Abstract
Objectives
To investigate public perspectives on brain health.
Design
Cross-sectional multilanguage online survey.
Setting
Lifebrain posted the survey on its website and social media and shared it with stakeholders. The survey was open from 4 June 2019 to 31 August 2020.
Participants
n=27 590 aged ≥18 years from 81 countries in five continents completed the survey. The respondents were predominantly women (71%), middle aged (41–60 years; 37%) or above (>60 years; 46%), highly educated (69%) and resided in Europe (98%).
Main outcome measures
Respondents’ views were assessed regarding factors that may influence brain health, life periods considered important to look after the brain and diseases and disorders associated with the brain. We run exploratory linear models at a 99% level of significance to assess correlates of the outcome variables, adjusting for likely confounders in a targeted fashion.
Results
Of all significant effects, the respondents recognised the impact of lifestyle factors on brain health but had relatively less awareness of the role socioeconomic factors might play. Most respondents rated all life periods as important for the brain (95%–96%), although the prenatal period was ranked significantly lower (84%). Equally, women and highly educated respondents more often rated factors and life periods to be important for brain health. Ninety-nine per cent of respondents associated Alzheimer’s disease and dementia with the brain. The respondents made a connection between mental health and the brain, and mental disorders such as schizophrenia and depression were significantly more often considered to be associated with the brain than neurological disorders such as stroke and Parkinson’s disease. Few respondents (<32%) associated cancer, hypertension, diabetes and arthritis with the brain.
Conclusions
Differences in perceptions of brain health were noted among specific segments of the population. Policies providing information about brain-friendly health behaviours and targeting people less likely to have relevant experience may be needed.
Keywords: health policy, mental health, dementia, preventive medicine, public health
Strengths and limitations of this study.
We recruited online an unusually large international sample of people to interrogate about their perceptions of brain health.
The survey was developed in collaboration with representatives from national brain councils, brain foundations and research registries interested in brain health and was made available online in 14 languages.
The survey responders were not representative of the general population being mostly middle aged or older, highly educated, female and probably already interested in brain health.
The knowledge gaps observed in this sample of largely highly educated individuals are likely to be an issue, and perhaps even to a greater degree, in the broader population.
Introduction
Many neurological and mental conditions affect the brain’s structure and function like dementia, stroke, depression and schizophrenia, and significantly contribute to the global burden of non-communicable diseases.1 The US National Institute on Aging recently described brain health as the ability to ‘remember, learn, plan, concentrate, and handle challenges […] and be mentally and emotionally in balance, […] making the most of the brain and taking care of it’.2 There is increasing evidence that adopting healthy lifestyles including physical activity, having a healthy diet and good cardiovascular control, restraining from substance use, avoiding chronic stress and perhaps getting enough sleep may reduce risk of developing some brain diseases, although such impacts are not conclusively understood.3 4
Knowledge regarding how people perceive brain health, and what actions they are willing to take to maintain a healthy brain, is needed. In Europe, surveys aiming to investigate public perceptions of cognitive health have been conducted in Ireland,5 6 the Netherlands7 and the UK,8 and suggest limited knowledge and awareness of dementia, dementia risk and factors contributing to cognitive decline. Studies conducted in France9 and the UK10 reported a lack of understanding of some mental disorders such as schizophrenia, bipolar disorders and autism. In Slovenia, a recent survey reported that, despite awareness of the importance of brain health, laypeople were unlikely to adopt purposefully behaviours beneficial for the brain due to lack of time and information.11 Qualitative studies conducted in the UK12 13 and elsewhere in Europe14 showed varying awareness of actions beneficial for the brain, and emphasised the importance of providing people with evidence-based and trustworthy information to encourage adoption of brain-friendly behaviours. Studies conducted in Australia and New Zealand have also reported limited knowledge about cognitive health and Alzheimer’s disease (AD)15 and potential measures to reduce risk of dementia and cognitive decline.16–19 A 2015 systematic review of public perceptions about risk and protective factors for cognitive health and impairment concluded that although some awareness was present regarding risk factors for cognitive impairment, efforts should be made to provide the general public with accurate information regarding risk-reducing strategies.20
These studies offer useful insights to understand public perceptions of brain health but usually were conducted at national level and included samples of limited size. They often focused on one specific aspect of brain health, such as cognitive health or a mental illness, used different measures and instruments and did not share a common definition of brain health, making a comparison of results between studies challenging. Investigating perceptions of brain health in a larger sample and exploring how views may differ depending on gender, age and education will provide new and useful knowledge to guide brain health promotion. If there is a mismatch between what people consider important and what the best available evidence suggests, there may be considerable public health gains to explain the benefits or dangers of certain factors, especially those that could be acted on by the individual.
In June 2019, the Lifebrain consortium21 launched the ‘Global Brain Health Survey’.22 Lifebrain is a European consortium including 16 partners and data from brain imaging cohorts in eight European countries, totalling approximately 6000 research participants.23 We aimed to investigate the perspectives of participants in the Lifebrain cohorts and members of the public on brain health. The survey was conducted online and featured as ‘global’ to invite anyone interested in the topic of brain health to take the survey irrespective of geographical location. The survey included four overall themes: perception of some aspects of brain health (reported here), interest in undertaking brain health tests, motivations to look after one’s brain24 and support needed to make lifestyle changes beneficial for the brain.25 In this paper, we report responses to survey questions relating to: (1) factors believed to influence brain health, (2) specific life periods considered important to look after one’s brain, and (3) diseases and disorders associated with the brain. Whereas extrapolating from responses in this convenience sample to the general population will not be feasible considering the sample characteristics in different countries, we adjust the results for confounding variables, such as age and education, where appropriate.
Methods
A detailed description of the survey’s background and design, technical platform as well as a summary of the main questionnaire has been published elsewhere.22 In brief, the survey included 16 multiple-choice questions addressing brain health perceptions and 12 questions on demographics. The questions were developed using an interview guide from a previous qualitative interview study, where we investigated Lifebrain research participants’ perceptions of brain health.26 The survey was translated to 14 languages, including English, Danish, Spanish, French, Norwegian, Catalan, German, Swedish, Hungarian, Ukrainian, Italian, Dutch, Chinese (simplified Mandarin) and Turkish. The study applied the procedure of back translation. The survey was made freely available online from the Lifebrain website www.lifebrain.uio.no, was anonymous and took approximately 15–20 min to complete. No financial compensation was provided to respondents. On the introductory survey page, the US National Institute on Aging’s description of brain health was provided.2 The survey was available from June 2019 and was closed on 31 August 2020. To be able to submit their questionnaire, the respondents had to consent to the use of their data for research and complete at least five multiple-choice questions and the 12 demographic questions.
Patient and public involvement
The draft survey questionnaire was shared and discussed with representatives from patient organisations and national brain councils27 in Europe, Lifebrain researchers and cohort participants, and members of the public who participated in Lifebrain stakeholder workshops and public lectures in Spain, Norway and the UK. Their suggestions for improvement were integrated in later versions of the questionnaire. The questionnaire was also shared with national brain councils in Norway, Belgium and Germany, and brain foundations, and some agreed to become official co-organisers of the survey.
Sampling
The survey was primarily distributed via the Lifebrain cohorts’ websites, social media and E-newsletters, and with help from approximately 20–25 European organisational stakeholders in the consortium network. National brain councils, brain foundations, universities, research projects, professional societies, patient organisations and charities, and research registries, whose mission is to match interested volunteers with research groups, invited their members to take the survey. In addition, Lifebrain researchers posted the survey on their websites and social media, and distributed leaflets presenting the survey at conferences, scientific events, in public libraries and hospital waiting rooms. The survey was also featured in Scandinavian media.28 29 As the survey was freely available online, it is likely that it has been shared by other stakeholders outside of Europe.
Measures
We used three of the 16 multiple-choice questions in the survey questionnaire providing information about perceptions of brain health, and 12 demographic questions. The three multiple-choice questions were not mandatory and could be skipped by the respondents, whereas the 12 demographic questions were mandatory. For each multiple-choice question, respondents could endorse any number of items.
Factors influencing brain health
The first question was: ‘In your opinion, to what extent do the following influence brain health?’. A list of 11 factors was provided including physical health, diet, physical environment (eg, air pollution, noise), social environment (eg, family, social network), education, profession, family income, genetics and family medical history, substance use (eg, alcohol, smoking and drugs), sleeping habits and having goals that make life meaningful. The respondents could rate the factors using a 5-item Likert scale (very strong, strong, moderate, weak or no influence).
Specific life periods to look after one’s brain
The second question was: ‘In your opinion, at what stages in life is it important to look after one’s brain?’. Respondents could rate six life periods: in the womb (before birth), childhood (from birth to 12 years), adolescence (13–18 years), young adulthood (19–45 years), middle age (46–65 years) and old age (over 65 years), using a 4-item Likert scale (very important, important, moderately important, not important).
Diseases and disorders associated with the brain
The third question was: ‘Which of the following diseases/disorders do you associate with the brain?’. A list of 13 disorders was provided, of which 10 are recognised brain disorders (ie, AD and other forms of dementia, bipolar disorder, schizophrenia, Parkinson’s disease, addiction, stroke, depression, migraine, anxiety, cancer), and three are known to have an impact on the brain (ie, diabetes, arthritis and hypertension). When listing cancer, we did not specify whether it referred to brain cancer or other types of cancer.
Demographic questions
The respondents were asked about their age category (18–25, 26–40, 41–60, 61–70, 71–80, over 80), gender (male, female, other, prefer not to tell), highest attained educational qualification (primary school, special educational school, secondary school, vocational training, university/college degree), relationship/civil status (single, in a stable relationship but not married, married, divorced or separated, or widowed) and occupational status (employed for wages or self-employed, unemployed, home maker, student, retired, unable to work, or doing unpaid or voluntary work). The respondents were also asked to rate their ability to think, remember and learn (hereafter referred to as self-reported cognitive health) as well as their ability to be mentally and emotionally in balance (hereafter referred to as self-reported mental health) using a 5-item Likert scale (excellent, above average, average, below average, very poor). Finally, we asked for information about country of residence, previous experience of participating in brain research (yes, no), educational or work experience in healthcare (yes, no), experience of long-standing illness, disability or health problem (yes, no) and experience of looking after a family member with brain disease (yes, no).
Statistical analysis
Exploratory linear models were performed on all survey questions presented applying R V.4.1.0.30 Ten models were used per response category, exploring the relationship between demographic characteristics and responses. We report binarised responses and ORs for the purposes of communication and simplicity. However, we are aware of the potential pitfalls,31 so for purposes of robustness, we also report the data modelled as continuous in the online supplemental materials, and note the general agreement between the binary and continuous models (see online supplemental material 1). Complete detailed descriptive statistics are provided for all questions in online supplemental material 2 and the continuous, binary and ordinal models for question 1 and question 2 are provided in online supplemental material 3. Only responses from submitted questionnaires were used in the analysis.
bmjopen-2021-057999supp001.pdf (316.7KB, pdf)
bmjopen-2021-057999supp002.pdf (229.5KB, pdf)
bmjopen-2021-057999supp003.pdf (359.3KB, pdf)
For the first question (factors influencing brain health), responses of ‘very strong’ and ‘strong’ were classified as indicating an association between the question and response category, while the remaining options (‘moderate’, ‘weak’ and ‘no influence’) were categorised as indicating no association. Similarly, in the second question (life periods to take care of one’s brain), responses of ‘very important’ and ‘important’ were classified as indicating that respondents considered the life period as important to take care of the brain, indicating a positive association between the question and response category, whereas responses of the remaining ‘moderately important’ and ‘not important’ were classified as indicating that the respondents considered the life period as not so important or not important. The third question was already on a binary scale, where responses were logged by selecting from a list of diseases and disorders associated with brain health. For each category, separate predictive logistic regression models for (1) age, (2) gender, (3) education, (4) relationship status, (5) experience or education in healthcare, (6) experience with illness, (7) experience of being a caregiver for someone with a brain disease, (8) rating of own cognitive health, and (9) rating of own mental health as predictors were computed.
Demographic variables with more than three response categories were reduced to aid interpretation of results. Education was reduced to whether the subject had higher education (university degree) or not. Age was reduced to three categories: ‘youngest’ (those below 40 years), ‘middle-aged’ (those between 40 and 60 years) and ‘oldest’ (those above 60 years, the largest response group). Gender was reduced to three categories: ‘woman’, ‘man’ and ‘other/prefer not to tell’. The ratings of subjects’ own mental and cognitive health were reduced to two categories: one for those rating their health as average or above, and those rating their health as below average. Relationship was reduced to those being in a stable relationship (married and domestic partnerships) or not. The base comparison groups for each predictor variable were set as the category where there was the highest number of subjects.
The very large sample size with high statistical power made it very likely that group differences apparent on inspection of numbers were statistically significant. This means that many statistically significant results may not be of practical importance. We report results significant at the 1% level of probability, with false discovery rate correction across all models and covariates for each outcome variable. We used multivariable testing with logistic regression to adjust results only for questions 1 and 2 adjusting the observed sex effect for age and education. Similarly, in question 3, we controlled the ‘stable relationship effect’ for age and education. Finally, the Strengthening the Reporting of Observational Studies in Epidemiology cross-sectional reporting guidelines were used.32
Results
Respondent characteristics
In total, 27 590 respondents from 81 countries completed the survey. 99.9% of respondents (n=27 552) completed the first question, 99.8% (n=27 536) completed the second question and 99.8% (n=27 530) completed the third question. All respondents completed the demographic questions.
Table 1 provides an overview of the number of respondents by country. The respondents predominantly lived in Europe (98%), including the UK (36.8%), the Netherlands (25.5%), Norway (12.9%), Spain (7.6%), Denmark (4.0%), Germany (3.8%) and Sweden (2.8%). Respondents outside Europe primarily resided in the USA (0.6%) and Turkey (0.5%). Due to large variation in the number of responses between countries, and varying recruitment strategies from one country to another, making meaningful comparisons of responses between countries is hardly feasible. We thus only provide below the results for the whole sample across countries.
Table 1.
Number of respondents by country
| Country | Respondents (n) | % of total |
| UK | 10 160 | 36.8 |
| The Netherlands | 7023 | 25.5 |
| Norway | 3549 | 12.9 |
| Spain | 2095 | 7.6 |
| Denmark | 1101 | 4.0 |
| Germany | 1060 | 3.8 |
| Sweden | 760 | 2.8 |
| Italy | 311 | 1.1 |
| Ukraine | 311 | 1.1 |
| Hungary | 187 | 0.7 |
| USA | 165 | 0.6 |
| Slovenia | 148 | 0.5 |
| Turkey | 139 | 0.5 |
| Belgium | 115 | 0.4 |
| Other (<100 respondents per country) | 466 | 1.7 |
| Total | 27 590 | 100 |
Table 2 provides an overview of the demographic characteristics of the whole sample. The respondents were predominantly middle aged (41–60: 37.4%) or older (>60: 46.2%), women (71.1%), married or in a relationship (71.8%) and highly educated (68.6%). About half of the respondents (51.4%) reported being in paid employment and a third (38.5%) having an educational or employment experience in healthcare. The respondents largely rated their cognitive health (93.9%) and their mental health (86.8%) as average or above average. 40.4% of respondents reported having a long-standing illness, disability or health problem. 46.5% reported having an experience of looking after a family member with brain disease, and 43.2% an experience of participating in brain research. A majority of respondents (57%) had been recruited through the research registries Join Dementia Research33 in the UK and Hersenonderzoek.nl34 in the Netherlands. The demographic characteristics of respondents in the seven European countries with most responses are provided in online supplemental material 4.
Table 2.
Demographic characteristics of the whole sample
| Respondents | Respondents (n) | % of total |
| Gender | ||
| Women | 19 626 | 71.1 |
| Men | 7833 | 28.4 |
| Other | 131 | 0.5 |
| Total | 27 590 | 100.0 |
| Age range (years) | ||
| 18–40 | 4502 | 16.4 |
| 41–60 | 10 328 | 37.4 |
| >60 | 12 760 | 46.2 |
| Education | ||
| Higher education | 18 925 | 68.6 |
| Lower education | 8665 | 31.4 |
| Relationship status | ||
| Yes | 19 819 | 71.8 |
| No | 7771 | 28.2 |
| Occupation* | ||
| Employed for wages | 14 181 | 51.4 |
| Retired | 10 550 | 38.2 |
| Other | 9708 | 35.2 |
| Employment and/or education in healthcare | ||
| No | 16 955 | 61.5 |
| Yes | 10 635 | 38.5 |
| Participation in brain research | ||
| No | 15 671 | 56.8 |
| Yes | 11 919 | 43.2 |
| Self-rated cognitive health | ||
| Below average | 1661 | 6.1 |
| Average or above average | 25 929 | 93.9 |
| Self-rated mental health | ||
| Below average | 3632 | 13.2 |
| Average or above average | 23 958 | 86.8 |
| Experience of illness, disability or health problem | ||
| No | 16 451 | 59.6 |
| Yes | 11 139 | 40.4 |
| Experience as caregiver of patient with brain disease | ||
| No | 14 762 | 53.5 |
| Yes | 12 828 | 46.5 |
*Percentages add up to >100% and n>27 590 because multiple responses were allowed.
bmjopen-2021-057999supp004.pdf (82.9KB, pdf)
Factors influencing brain health
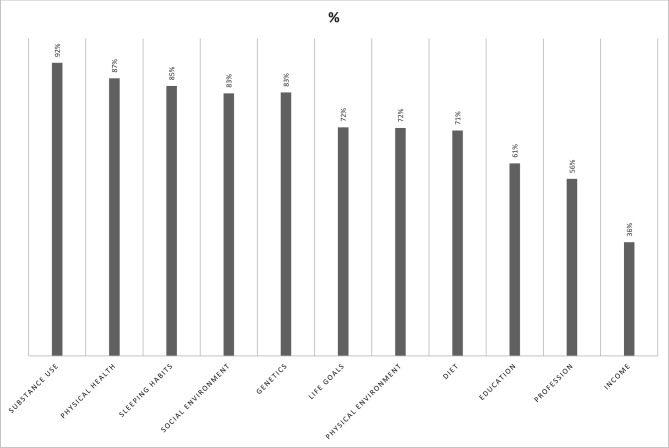
Figure 1 shows how many respondents rated each factor as having strong or very strong influence on brain health. Most respondents rated substance use (92% of participants), physical health (87%), sleeping habits (85%), social environment (83%) and genetics (83%) as having a strong/very strong influence on brain health, followed by life goals (72%), physical environment (72%), diet (71%) and socioeconomic factors such as education (61%), profession (56%) and income (36%). Other respondents rated the factors as having a moderate, weak or no influence on brain health. A detailed description of how factors were rated by all respondents according to a 5-item Likert scale is provided in the online supplemental material 2, sections 1.1–1.11.
Figure 1.
Factors believed to have a strong influence on brain health. % indicates proportion of participants rating this factor as having a ‘strong’ or ‘very strong’ influence on brain health, with the remainder of participants rating it as ‘moderate’, ‘weak’ or ‘no influence’.
Differences in response patterns were observed between demographic groups of respondents (table 3). Men were less likely than women to consider factors such as substance use (OR 0.66, 99% CI 0.58 to 0.74), sleeping habits (OR 0.68, 99% CI 0.62 to 0.74) and diet (OR 0.70, 99% CI 0.65 to 0.75) as having strong or very strong influence on the brain. In contrast, men were more prone to rate profession (OR 1.18, 99% CI 1.10 to 1.27) and education (OR 1.13, 99% CI 1.05 to 1.21) as important. After controlling for education level and age, these effects remained significant. Respondents with low education put less emphasis on factors such as education (OR 0.62, 99% CI 0.58 to 0.66), physical health (OR 0.73, 99% CI 0.66 to 0.81), profession (OR 0.75, 99% CI 0.71 to 0.81) and substance use (OR 0.75, 99% CI 0.67 to 0.85) as compared with highly educated respondents. However, they had higher odds of considering income (OR 1.11, 99% CI 1.04 to 1.19) and physical environment (OR 1.06, 99% CI 0.98 to 1.14) as having a strong/very strong influence on brain health.
Table 3.
Factors believed to have a strong influence on brain health by demographic groups
| Variable | Characteristics | Substance use | Genetics | Physical health | ||||||
| % | OR | 99% CI | % | OR | 99% CI | % | OR | 99% CI | ||
| Gender | Women | 93.3 | 83.4 | 88.3 | ||||||
| Men | 90.1 | 0.66 | 0.58 to 0.74 | 80.0 | 0.79 | 0.73 to 0.87 | 85.3 | 0.77 | 0.70 to 0.85 | |
| Other/undisclosed | 85.8 | 0.44 | 0.23 to 0.84 | 69.8 | 0.46 | 0.28 to 0.76 | 85.0 | 0.75 | 0.39 to 1.43 | |
| Age (years) | >60 | 90.5 | 83.4 | 86.6 | ||||||
| 41–60 | 94.2 | 1.70 | 1.49 to 1.95 | 83.6 | 1.01 | 0.92 to 1.11 | 88.1 | 1.14 | 1.03 to 1.26 | |
| <40 | 93.2 | 1.43 | 1.20 to 1.69 | 76.6 | 0.65 | 0.58 to 0.72 | 88.4 | 1.17 | 1.02 to 1.34 | |
| Education | Higher education | 93.0 | 82.6 | 88.6 | ||||||
| Lower education | 90.9 | 0.75 | 0.67 to 0.85 | 81.8 | 0.94 | 0.87 to 1.03 | 85.0 | 0.73 | 0.66 to 0.81 | |
| Experience or education in health care | No | 91.3 | 81.7 | 85.7 | ||||||
| Yes | 94.0 | 1.50 | 1.32 to 1.70 | 83.4 | 1.12 | 1.03 to 1.22 | 90.2 | 1.53 | 1.39 to 1.70 | |
| Variable | Characteristics | Sleeping habits | Social environment | Life goals | ||||||
| % | OR | 99% CI | % | OR | 99% CI | % | OR | 99% CI | ||
| Gender | Women | 86.5 | 84.1 | 73.5 | ||||||
| Men | 81.3 | 0.68 | 0.62 to 0.74 | 79.2 | 0.72 | 0.66 to 0.79 | 71.1 | 0.89 | 0.82 to 0.96 | |
| Other/undisclosed | 87.4 | 1.08 | 0.54 to 2.16 | 90.4 | 1.79 | 0.81 to 3.91 | 70.9 | 0.88 | 0.53 to 1.46 | |
| Age (years) | >60 | 79.6 | 79.9 | 74.3 | ||||||
| 41–60 | 89.0 | 2.06 | 1.87 to 2.28 | 84.1 | 1.33 | 1.22 to 1.46 | 73.3 | 0.95 | 0.88 to 1.03 | |
| <40 | 91.6 | 2.78 | 2.39 to 3.23 | 87.3 | 1.73 | 1.52 to 1.97 | 67.2 | 0.71 | 0.64 to 0.78 | |
| Education | Higher education | 85.8 | 83.6 | 73.2 | ||||||
| Lower education | 83.4 | 0.83 | 0.76 to 0.91 | 80.9 | 0.83 | 0.76 to 0.91 | 71.9 | 0.94 | 0.87 to 1.01 | |
| Healthcare experience | No | 83.6 | 80.6 | 70.9 | ||||||
| Yes | 87.3 | 1.35 | 1.23 to 1.48 | 86.1 | 1.48 | 1.36 to 1.62 | 75.7 | 1.28 | 1.19 to 1.37 | |
| Variable | Characteristics | Physical environment | Diet | Education | ||||||
| % | OR | 99% CI | % | OR | 99% CI | % | OR | 99% CI | ||
| Gender | Women | 72.7 | 73.7 | 59.8 | ||||||
| Men | 69.6 | 0.86 | 0.80 to 0.93 | 66.2 | 0.70 | 0.65 to 0.75 | 62.7 | 1.13 | 1.05 to 1.21 | |
| Other/undisclosed | 77.8 | 1.31 | 0.76 to 2.29 | 72.4 | 0.94 | 0.56 to 1.57 | 64.6 | 1.22 | 0.76 to 1.98 | |
| Age (years) | >60 | 69.8 | 66.7 | 60.9 | ||||||
| 41–60 | 74.3 | 1.25 | 1.16 to 1.35 | 75.6 | 1.54 | 1.43 to 1.67 | 59.2 | 0.93 | 0.87 to 1.00 | |
| <40 | 71.7 | 1.10 | 0.99 to 1.21 | 76.1 | 1.59 | 1.44 to 1.77 | 63.4 | 1.11 | 1.01 to 1.22 | |
| Education | Higher education | 71.5 | 73.1 | 64.3 | ||||||
| Lower education | 72.6 | 1.06 | 0.98 to 1.14 | 68.2 | 0.79 | 0.73 to 0.85 | 52.6 | 0.62 | 0.58 to 0.66 | |
| Healthcare experience | No | 70.5 | 69.0 | 58.0 | ||||||
| Yes | 74.0 | 1.19 | 1.11 to 1.28 | 75.6 | 1.39 | 1.29 to 1.49 | 64.8 | 1.33 | 1.25 to 1.42 | |
| Variable | Characteristics | Profession | Income | ||||
| % | OR | 99% CI | % | OR | 99% CI | ||
| Gender | Women | 54.6 | 36.2 | ||||
| Men | 58.7 | 1.18 | 1.10 to 1.27 | 35.0 | 0.95 | 0.88 to 1.02 | |
| Other/undisclosed | 54.3 | 0.99 | 0.62 to 1.57 | 40.2 | 1.18 | 0.74 to 1.89 | |
| Age (years) | >60 | 53.2 | 36.8 | ||||
| 41–60 | 57.0 | 1.16 | 1.08 to 1.24 | 36.3 | 0.98 | 0.91 to 1.05 | |
| <40 | 60.2 | 1.33 | 1.21 to 1.46 | 32.0 | 0.81 | 0.73 to 0.89 | |
| Education | Higher education | 58.0 | 35.1 | ||||
| Lower education | 51.0 | 0.75 | 0.71 to 0.81 | 37.5 | 1.11 | 1.04 to 1.19 | |
| Healthcare experience | No | 53.9 | 33.5 | ||||
| Yes | 58.8 | 1.23 | 1.15 to 1.31 | 39.6 | 1.30 | 1.22 to 1.39 | |
Univariate ORs and 99% CIs.
% indicates proportion of participants rating this factor as having a ‘strong’ or ‘very strong’ influence on brain health, with the remainder of participants rating it as ‘moderate’, ‘weak’ or ‘no influence’.
Respondents older than 60 years gave more importance to income than participants below 40 years of age (OR 0.81, 99% CI 0.73 to 0.89) and respondents aged 41–60 years (OR 0.98, 99% CI 0.91 to 1.05). The same was observed for having meaningful goals in life. In contrast, importance given to sleep decreased with age and respondents below 40 years of age (OR 2.78, 99% CI 2.39 to 3.23), and respondents aged 41–60 years (OR 2.06, 99% CI 1.87 to 2.28) more often rated sleep as having a strong/very strong influence on brain health as compared with the respondents older than 60 years. The same accounted for factors such as social environment, diet and profession.
Respondents with a higher education level, respondents with a reported education or experience in healthcare, respondents who self-rated their cognitive and mental health as average or above and women were more prone to rate all factors as having a strong or very strong influence on brain health (see online supplemental material 5, section 1). In contrast, respondents who self-rated their cognitive and mental health as below average were less likely to rate all factors as having a strong or very strong influence on brain health, with one notable exception. Respondents rating their mental health as below average were more likely to rate sleep as important (OR 1.33, 99% CI 1.16 to 1.53) as compared with respondents rating their mental health as average or above. Likewise, respondents in a stable relationship were less prone to rate sleep as important (OR 0.81, 99% CI 0.74 to 0.89), and more prone to rate genetics as important (OR 1.20, 99% CI 1.11 to 1.31) as compared with other respondents not in a stable relationship.
bmjopen-2021-057999supp005.pdf (148.5KB, pdf)
Life periods to look after ones’ brain
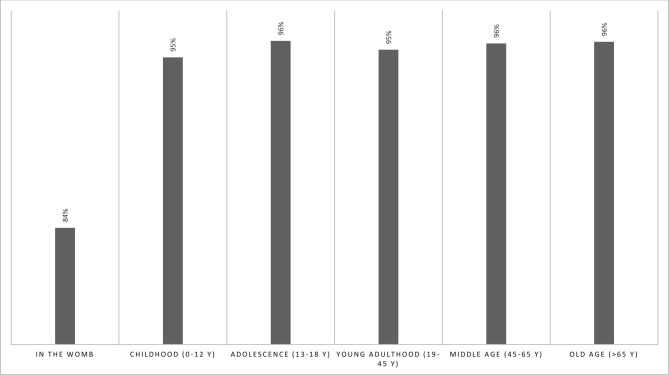
Figure 2 shows that the respondents rated most life periods as important or very important for the brain (95%–96%), whereas the prenatal stage (in the womb/before birth) was rated as important or very important by 84% of respondents (online supplemental material 2, section 2).
Figure 2.
Life periods considered important to take care of one’s brain. % indicates proportion of participants rating this life period as ‘important’ or ‘very important’, with the remainder of participants rating it as ‘not important’ or ‘moderately important’.
Table 4 shows that men were less likely to consider life periods such as the middle age (OR 0.41, 99% CI 0.35 to 0.48) and old age (OR 0.41, 99% CI 0.35 to 0.49) as important as compared with women. This was also observed when controlling for age and education. Respondents with lower education were also less likely to rate life periods as important as compared with higher educated respondents, except for young adulthood (OR 1.06, 99% CI 0.90 to 1.24). The youngest respondents (<40) were less likely to consider middle age (OR 0.82, 99% CI 0.67 to 1.00) and old age as important (OR 0.55, 99% CI 0.45 to 0.67) compared with the oldest respondents (>60). Rather, the youngest respondents were more likely to consider childhood (OR 1.89, 99% CI 1.51 to 2.37) and adolescence important (OR 2.14, 99% CI 1.60 to 2.85) as compared with the oldest respondents (>60).
Table 4.
Life periods considered important to take care of one’s brain by demographic groups
| Variable | Characteristics | In the womb | Childhood (0–12) | Adolescence (13–18) | ||||||
| % | OR | 99% CI | % | OR | 99% CI | % | OR | 99% CI | ||
| Gender | Women | 85.9 | 95.7 | 97.0 | ||||||
| Men | 78.0 | 0.58 | 0.53 to 0.63 | 93.0 | 0.59 | 0.51 to 0.69 | 95.6 | 0.68 | 0.57 to 0.81 | |
| Other/undisclosed | 86.4 | 1.04 | 0.53 to 2.04 | 95.2 | 0.89 | 0.30 to 2.63 | 96.0 | 0.75 | 0.23 to 2.44 | |
| Age (years) | >60 | 80.7 | 93.4 | 95.5 | ||||||
| 41–60 | 86.2 | 1.49 | 1.36 to 1.64 | 96.2 | 1.78 | 1.51 to 2.09 | 97.3 | 1.71 | 1.41 to 2.08 | |
| <40 | 86.1 | 1.48 | 1.31 to 1.68 | 96.4 | 1.89 | 1.51 to 2.37 | 97.9 | 2.14 | 1.60 to 2.85 | |
| Education | Higher education | 86.0 | 95.8 | 97.0 | ||||||
| Lower education | 78.5 | 0.59 | 0.54 to 0.65 | 92.9 | 0.57 | 0.50 to 0.66 | 95.6 | 0.67 | 0.56 to 0.80 | |
| Healthcare experience | No | 80.5 | 93.7 | 95.9 | ||||||
| Yes | 88.8 | 1.91 | 1.74 to 2.10 | 96.8 | 2.06 | 1.74 to 2.43 | 97.7 | 1.79 | 1.48 to 2.18 | |
| Variable | Characteristics | Young adulthood (19–45) | Middle age (45–65) | Old age (>65) | ||||||
| % | OR | 99% CI | % | OR | 99% CI | % | OR | 99% CI | ||
| Gender | Women | 96.2 | 97.0 | 97.1 | ||||||
| Men | 93.4 | 0.56 | 0.48 to 0.65 | 93.0 | 0.41 | 0.35 to 0.48 | 93.2 | 0.41 | 0.35 to 0.49 | |
| Other/undisclosed | 92.8 | 0.51 | 0.21 to 1.24 | 88.8 | 0.24 | 0.12 to 0.51 | 92.0 | 0.35 | 0.15 to 0.82 | |
| Age (years) | >60 | 94.5 | 95.3 | 96.2 | ||||||
| 41–60 | 96.5 | 1.59 | 1.34 to 1.89 | 97.2 | 1.68 | 1.40 to 2.03 | 96.8 | 1.19 | 0.98 to 1.43 | |
| <40 | 95.4 | 1.21 | 0.98 to 1.50 | 94.3 | 0.82 | 0.67 to 1.00 | 93.3 | 0.55 | 0.45 to 0.67 | |
| Education | Higher education | 95.3 | 95.9 | 96.2 | ||||||
| Lower education | 95.6 | 1.06 | 0.90 to 1.24 | 95.6 | 0.93 | 0.78 to 1.09 | 95.3 | 0.80 | 0.67 to 0.94 | |
| Healthcare experience | No | 94.7 | 95.2 | 95.4 | ||||||
| Yes | 96.6 | 1.60 | 1.36 to 1.89 | 96.8 | 1.53 | 1.29 to 1.82 | 96.7 | 1.41 | 1.19 to 1.68 | |
Univariate OR and 99% CI.
% indicates proportion of participants rating this life period as ‘important’ or ‘very important’, with the remainder of participants rating it as ‘not important’ or ‘moderately important’.
Respondents with an education or experience in healthcare were more prone to consider the life periods as important, especially pregnancy (OR 1.91, 99% CI 1.74 to 2.10) and childhood (OR 2.06, 99% CI 1.74 to 2.43) as compared with other respondents with no experience (online supplemental material 5, section 2). Respondents with lower education were consistently less likely to consider the life periods as important as compared with respondents with higher education, except for young adulthood, which they were more likely to consider important as compared with the highly educated (OR 1.06, 99% CI 0.90 to 1.24). Respondents in a stable relationship were more prone to consider important taking care of the brain in old age (OR 1.21, 99% CI 1.03 to 1.41) as compared with respondents not in a stable relationship.
Diseases and disorders associated with the brain
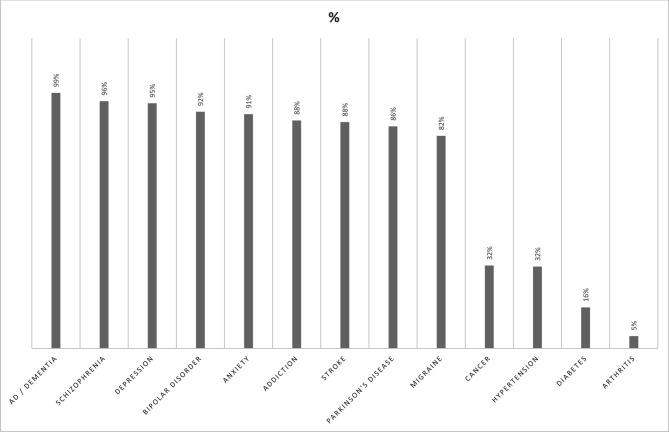
Figure 3 shows that 99% of the respondents associated AD and other forms of dementia with the brain. The next most often selected disorders were mental disorders like schizophrenia (96%), depression (95%), bipolar disorder (92%), anxiety (91%) and addiction (88%). Disorders least often associated with the brain included cancer (32%), hypertension (32%), diabetes (16%) and arthritis (5%).
Figure 3.
Diseases and disorders believed to be associated with the brain. % indicates proportion of participants rating this disorder or disease as ‘associated with the brain’, with the remainder of participants rating it as ‘not associated with the brain’. AD, Alzheimer’s disease.
Women were more likely than men to associate the diseases with the brain, and this was particularly observed for bipolar disorder (OR 0.47, 99% CI 0.42 to 0.53), stroke (OR 0.53, 99% CI 0.48 to 0.58) and schizophrenia (OR 0.64, 99% CI 0.54 to 0.75) (table 5). A similar trend was observed among lower educated respondents, who were less likely to select disorders such as bipolar disorder (OR 0.42, 99% CI 0.38 to 0.47) and AD/dementia (OR 0.48, 99% CI 0.34 to 0.67) as compared with highly educated respondents.
Table 5.
Diseases and disorders associated with the brain by demographic groups
| Variable | Characteristics | AD and dementia | Schizophrenia | Depression | ||||||
| % | OR | 99% CI | % | OR | 99% CI | % | OR | 99% CI | ||
| Gender | Women | 99.4 | 96.4 | 95.6 | ||||||
| Men | 98.5 | 0.40 | 0.29 to 0.56 | 94.5 | 0.64 | 0.54 to 0.75 | 93.8 | 0.70 | 0.60 to 0.81 | |
| Other/undisclosed | 100 | 95.2 | 0.74 | 0.25 to 2.18 | 96.0 | 1.11 | 0.34 to 3.61 | |||
| Age (years) | >60 | 99.3 | 95.1 | 94.2 | ||||||
| 41–60 | 99.4 | 1.08 | 0.71 to 1.65 | 96.6 | 1.47 | 1.23 to 1.75 | 96.1 | 1.51 | 1.29 to 1.78 | |
| <40 | 98.0 | 0.35 | 0.23 to 0.51 | 96.3 | 1.34 | 1.06 to 1.69 | 95.4 | 1.29 | 1.05 to 1.59 | |
| Education | Higher education | 99.3 | 96.5 | 95.6 | ||||||
| Lower education | 98.6 | 0.48 | 0.34 to 0.67 | 94.5 | 0.62 | 0.53 to 0.72 | 94.0 | 0.72 | 0.62 to 0.84 | |
| Healthcare experience | No | 98.9 | 95.3 | 94.6 | ||||||
| Yes | 99.5 | 2.37 | 1.57 to 3.56 | 96.9 | 1.52 | 1.28 to 1.81 | 96.0 | 1.38 | 1.18 to 1.61 | |
| Variable | Characteristics | Bipolar disorder | Anxiety | Addiction | ||||||
| % | OR | 99% CI | % | OR | 99% CI | % | OR | 99% CI | ||
| Gender | Women | 93.6 | 91.4 | 90.0 | ||||||
| Men | 87.3 | 0.47 | 0.42 to 0.53 | 89.4 | 0.79 | 0.71 to 0.89 | 84.4 | 0.60 | 0.54 to 0.67 | |
| Other/undisclosed | 93.7 | 1.01 | 0.39 to 2.60 | 95.2 | 1.88 | 0.64 to 5.55 | 90.5 | 1.05 | 0.48 to 2.31 | |
| Age (years) | >60 | 88.9 | 89.0 | 86.6 | ||||||
| 41–60 | 94.6 | 2.17 | 1.90 to 2.49 | 92.6 | 1.54 | 1.37 to 1.74 | 89.8 | 1.37 | 1.23 to 1.52 | |
| <40 | 93.8 | 1.90 | 1.59 to 2.26 | 92.1 | 1.44 | 1.23 to 1.70 | 90.6 | 1.50 | 1.29 to 1.74 | |
| Education | Higher education | 94.0 | 91.6 | 90.0 | ||||||
| Lower education | 87.0 | 0.42 | 0.38 to 0.47 | 89.1 | 0.75 | 0.67 to 0.84 | 85.0 | 0.63 | 0.57 to 0.69 | |
| Healthcare experience | No | 90.0 | 90.2 | 86.0 | ||||||
| Yes | 94.7 | 2.00 | 1.76 to 2.28 | 92.0 | 1.25 | 1.11 to 1.40 | 92.4 | 1.97 | 1.77 to 2.20 | |
| Variable | Characteristics | Stroke | Parkinson’s disease | Migraine | ||||||
| % | OR | 99% CI | % | OR | 99% CI | % | OR | 99% CI | ||
| Gender | Women | 89.9 | 86.9 | |||||||
| Men | 82.4 | 0.53 | 0.48 to 0.58 | 84.3 | 0.81 | 0.73 to 0.89 | 83.5 | |||
| Other/undisclosed | 89.7 | 0.98 | 0.46 to 2.08 | 84.9 | 0.85 | 0.45 to 1.62 | 79.7 | 0.78 | 0.71 to 0.85 | |
| Age (years) | >60 | 87.7 | 86.1 | 77.6 | ||||||
| 41–60 | 89.3 | 1.16 | 1.04 to 1.29 | 87.5 | 1.13 | 1.25 to 1.02 | 86.0 | 1.78 | 1.62 to 1.95 | |
| <40 | 84.5 | 0.76 | 0.67 to 0.87 | 83.2 | 0.80 | 0.71 to 0.91 | 88.3 | 2.18 | 1.91 to 2.48 | |
| Education | Higher education | 88.3 | 87.9 | 84.3 | ||||||
| Lower education | 86.7 | 0.87 | 0.79 to 0.96 | 82.1 | 0.63 | 0.57 to 0.69 | 78.6 | 0.69 | 0.63 to 0.75 | |
| Healthcare experience | No | 84.5 | 83.1 | 79.5 | ||||||
| Yes | 93.0 | 2.44 | 2.18 to 2.73 | 90.9 | 2.04 | 1.85 to 2.26 | 87.2 | 1.76 | 1.61 to 1.92 | |
| Variable | Characteristics | Cancer | Hypertension | Diabetes | ||||||
| % | OR | 99% CI | % | OR | 99% CI | % | OR | 99% CI | ||
| Gender | Women | 33.8 | 33.7 | 16.7 | ||||||
| Men | 27.9 | 0.76 | 0.70 to 0.82 | 26.5 | 0.71 | 0.66 to 0.77 | 13.8 | 0.80 | 0.73 to 0.88 | |
| Other/undisclosed | 37.3 | 1.16 | 0.72 to 1.88 | 41.3 | 1.38 | 0.86 to 2.20 | 25.4 | 1.70 | 1.00 to 2.89 | |
| Age (years) | >60 | 28.5 | 34.2 | 15.3 | ||||||
| 41–60 | 34.1 | 1.30 | 1.21 to 1.40 | 31.5 | 0.88 | 0.82 to 0.95 | 17.2 | 1.15 | 1.05 to 1.27 | |
| <40 | 38.2 | 1.55 | 1.41 to 1.70 | 25.4 | 0.65 | 0.59 to 0.72 | 14.7 | 0.96 | 0.84 to 1.09 | |
| Education | Higher education | 34.2 | 33.5 | 17.3 | ||||||
| Lower education | 27.7 | 0.74 | 0.68 to 0.79 | 27.9 | 0.77 | 0.71 to 0.83 | 12.8 | 0.70 | 0.64 to 0.77 | |
| Healthcare experience | No | 27.4 | 24.9 | 10.6 | ||||||
| Yes | 39.7 | 1.74 | 1.63 to 1.87 | 42.6 | 2.24 | 2.09 to 2.39 | 24.3 | 2.71 | 2.49 to 2.96 | |
| Variable | Characteristics | Arthritis | ||
| % | OR | 99% CI | ||
| Gender | Women | 5.1 | ||
| Men | 3.9 | 0.75 | 0.63 to 0.89 | |
| Other/undisclosed | 6.3 | 1.25 | 0.49 to 3.23 | |
| Age (years) | >60 | 4.5 | ||
| 41–60 | 5.2 | 1.15 | 0.98 to 1.35 | |
| <40 | 4.6 | 1.01 | 0.81 to 1.25 | |
| Education | Higher education | 4.9 | ||
| Lower education | 4.6 | 0.94 | 0.80 to 1.11 | |
| Healthcare experience | No | 3.4 | ||
| Yes | 7.0 | 2.12 | 1.83 to 2.46 | |
Univariate OR and 99% CI.
% indicates proportion of participants rating this disorder or disease as ‘associated with the brain’, with the remainder of participants rating it as ‘not associated with the brain’.
AD, Alzheimer’s disease.
The youngest respondents (aged <40) were less likely to associate with the brain diseases often appearing in old age such as AD/dementia (OR 0.35, 99% CI 0.23 to 0.51), stroke (OR 0.76, 99% CI 0.67 to 0.87), hypertension (OR 0.65, 99% CI 0.59 to 0.72) and Parkinson’s disease (OR 0.80, 99% CI 0.71 to 0.91), as compared with respondents aged >60. In contrast, they more often selected disorders such as migraine (OR 2.18, 99% CI 1.91 to 2.48) and bipolar disorder (OR 1.90, 99% CI 1.59 to 2.26), addiction (OR 1.50, 99% CI 1.29 to 1.74) or anxiety (OR 1.44, 99% CI 1.23 to 1.70) as compared with respondents aged >60.
Respondents who self-assessed their mental health to be below average were less likely to associate the given diseases/disorders above with the brain as compared with other respondents, although they had higher odds of considering mental disorders such as anxiety (OR 1.51, 99% CI 1.26 to 1.82), depression (OR 1.40, 99% CI 1.10 to 1.78), bipolar disorder (OR 1.29, 99% CI 1.07 to 1.55) and addiction (OR 1.12, 99% CI 0.97 to 1.30) as associated with the brain. Respondents with an experience of disease were more likely, as compared with others with no such experience, to associate disorders such as arthritis (OR 1.59, 99% CI 1.38 to 1.84), diabetes (OR 1.25, 99% CI 1.15 to 1.37) and hypertension (OR 1.20, 99% CI 1.12 to 1.29) with the brain (online supplemental material 5, section 3). Respondents in a stable relationship were more likely to associate AD with the brain (OR 1.91, 99% CI 1.36 to 2.68) as compared with respondents not in a stable relationship. However, this association did not hold when controlling for age and education level.
Discussion
Summary of findings
To the best of our knowledge, this study was the first and largest survey to investigate public perceptions of brain health across countries using an online questionnaire available in multiple languages. Our respondents considered certain behaviours such as substance use (ie, smoking, drugs and alcohol consumption) and factors such as lifestyle, physical health, genetics and social environment important for brain health. Other factors included, in decreasing order of importance, diet, the physical environment and having goals that make life meaningful, followed by socioeconomic factors such as income, profession and education. The respondents rated all life periods as important for the brain although taking care of the brain in the womb (before birth) received relatively less attention. This question aimed to describe the life period during which one can take care of the fetal brain during pregnancy. It is possible that some respondents interpreted this life period as taking care of the mother’s brain during pregnancy. However, regardless of how it was interpreted, taking care of the mother’s and the fetus’s brain is important and deserves attention.
Awareness was high of AD and dementia affecting the brain. Our respondents more frequently associated mental disorders such as schizophrenia and depression with the brain as compared with neurological disorders such as stroke and Parkinson’s disease, although it should be noted that both classes were most often ranked as associated. Since we partly relied on our network of stakeholders working in fields of relevance for brain health to recruit survey respondents, it is likely that our sample was more interested in cognitive and psychological aspects of brain health than the general population. Disorders that are not defined as brain diseases but have an impact on the brain, such as hypertension, diabetes and arthritis, were perceived to be associated with the brain only to a small extent. Overall, women and highly educated respondents more often rated items as important than men and less educated participants. Men and women also differed in which factors they considered important for brain health.
Relevance to previous research
The high ranking of substance use as a factor influencing brain health is consistent with data from surveys in Australia and the USA19 35 but not from previous surveys in Ireland5 or the Netherlands7 where other factors like cognitive activity were given more importance. A recent scoping review of studies examining public perceptions of risk and protective factors related to cognitive health and impairment reported that genetics was the most identified risk factor for AD and dementia.20 In our survey, genetics was considered highly important for brain health. Likewise, our respondents’ high ranking of sleep corroborates results from a recent UK-wide survey in which respondents perceived sleep as important for maintaining or improving cognitive skills.36
Physical health was rated as highly important in our study in contrast to what previous surveys found,7 18 19 which reported limited awareness of how high blood pressure, coronary heart disease, obesity and plasma cholesterol levels influence brain health. Although our respondents rated physical health as important, paradoxically, they associated hypertension with the brain to a limited extent. In our questionnaire, we did not provide any example of what physical health entails, so we do not know exactly how our respondents interpreted the question. Results across studies may also be difficult to compare due to differences in the measures and instruments used. Our respondents less often deemed diet to be of very strong importance for brain health relative to other lifestyle factors, in line with previous studies.5 37 Although the topic has been little explored, our participants’ limited emphasis on socioeconomic factors is in line with results from an Australian survey on cognitive health.19 With few exceptions, most of our participants resided in high-income countries or upper middle-income countries such as Turkey. Views regarding the importance of socioeconomic factors for brain health may differ in low and middle-income countries.
To our knowledge, few studies have investigated what life periods people consider important for taking care of the brain. A recent global Ipsos survey (2021) looked at the perceptions of the importance of early life for a person’s health and happiness in adulthood38 and found that people did not consider the early (first 5) years as important for later health, compared with other periods of life. Previous research has shown that focus is often put on old age, as it might be considered as a risk factor for cognitive decline.39 In contrast, our respondents attributed high importance to childhood although they tended to rank age ranges closer to their own as more important. Similarly, we have not found studies specifically investigating which diseases people associate with the brain. Other surveys have shown public awareness of dementia,15 as confirmed by our results, despite limited knowledge of disease mechanisms and risk and protective factors,5 little concern regarding risk of developing dementia16 and limited public awareness of the prevalence and characteristics of mental illnesses such as schizophrenia and bipolar disorders.9 10
Implications for policymakers
Our sample was highly educated, mostly women probably interested in brain health and therefore not representative of the general population. Our survey, however, highlights that even in such population, there are some knowledge gaps to be filled. Detailed information should be provided about dietary habits and physical activity beneficial for physical health and for the brain. Our findings indicate that people may underestimate the importance of risk factors such as diabetes and poor vascular health for brain health, suggesting an avenue for improved public health messaging. Previous research has shown that unmarried people are at higher risk of dementia as compared with people living in stable relationships.40 We observed that awareness of AD was higher among our respondents living in stable relationships. This may suggest the need for targeted brain health information to single people and those living alone. Men and women differed in their perceptions of factors influencing brain health. Educational campaigns might need to consider these differences and leverage them for more personalised messages.
Our respondents made a clear connection between mental health and brain health, which may be due to their experience of the increasing societal burden of mental and addictive disorders.41 The outbreak of the COVID-19 pandemic in 2020, with strong implications for mental health,42 may also have influenced responses. However, we cannot verify this as the survey was anonymous and no time logs were recorded. Our results suggest that governments should give more attention to the reduction of preventable or modifiable mental health risk factors, for instance, by identifying individuals in early stages of disease or creating social environments promoting psychological well-being.43
Strengths and limitations
We believe that our study has several strengths. First, we consulted representatives from patient and civil society organisations such as patient organisations and national brain councils when developing the survey questionnaire. They are knowledgeable about how the public processes health-related information and helped strengthen the readability and relevance of our questions. The questions were also piloted in a previous study26 and at several public meetings. Second, we translated the survey into 14 languages, made it available online and promoted it in Europe and beyond. This enabled us to achieve a sample size up to 10 times larger than in previous comparable surveys.7 19 44 Third, our survey described brain health as encompassing both cognitive and mental health. This definition was more comprehensive than in other studies, which often focused solely on one aspect of brain health such as cognitive decline. This may make our results more relevant when discussing brain health promotion.
Our study has limitations. Our sample is not representative of the general population. Our respondents were predominantly highly educated, mostly women from the oldest segment of population reporting good cognitive and mental health. This is probably due to our recruitment strategy. Several of the Lifebrain cohorts23 as well as the research registries we used to recruit participants included more female educated volunteers.34 This may also be because women appear more concerned about cognitive decline and the maintenance of cognitive skills36 45 than men. Our respondents were probably more interested in, and knowledgeable about, brain health than the general population. Although we did not collect any ethnic data, we suspect that our sample was probably not ethnically and culturally diverse. We also do not know whether people in developing countries would manifest different perceptions to brain health, particularly the influence of socioeconomic factors. Another limitation of our study is that an online survey is more easily accessed by the most resourceful population groups with digital connection and competence. We were aware of this limitation when conceiving the study but aimed to reach a large international sample and include respondents from the Lifebrain consortium. Using an online tool was the most appropriate strategy due to our limited resources and it facilitated anonymous collection of data. Finally, although great care was taken in the translation and back-translation process22 and stakeholders in several countries helped adapt the survey to their local circumstances, there is a risk that our international respondents interpreted our questions slightly differently due to nuances in translations and the novelty of the concept of brain health.26
Conclusions and future directions
Our findings reflect a relatively good understanding of some facets of brain health. Awareness was higher among highly educated female respondents as compared with male and lowly educated respondents. Differences in perceptions of brain health were noted among specific segments of the population, suggesting that targeted policy actions towards these groups might be of relevance. Exploring how perceptions of brain health relate to intentions to follow brain-friendly lifestyles will also be of interest, knowing that such intentions may also depend on perceptions of risk46 47 and the socioeconomic, physical and technological contexts in which people navigate.48 Analysis of subsequent questions in this survey will provide some answers to this question.
Future research should investigate views on brain health of diverse ethnic groups in Europe, following recent calls for more diversity in research,49 as well as explore views on brain health in non-Western countries due to cultural variations.50 We did not compare results between countries due to varying sample size and recruitment strategies. Future research might investigate whether results differ between the three countries with most responses (UK, the Netherlands, Norway), and how any difference may have implications for brain health promotion at national levels. Future studies should also consider adopting alternative recruitment techniques and data collection platforms and include more men and respondents more representative of the general population.
Supplementary Material
Acknowledgments
We are grateful for the valuable help we received from many people to develop and disseminate the survey. This includes, but is not limited to, the Lifebrain research staff, the stakeholders who participated in Lifebrain workshops and public lectures, representatives from the Norwegian Brain Council, the Belgian Brain Council, the German Brain Council, the Brain Foundation Netherlands (Hersenstichting.nl), the Swedish Brain Foundation, the Women’s Brain Project, the National University of Ostroh Academy in Ukraine, Join Dementia Research, Hersenonderzoek, patient organisations and professional societies in Europe and elsewhere. We thank the survey respondents for their contribution.
Footnotes
Contributors: IBL, AMM, BBF, KPE, CAD, RBC, EZ, WFCB, KSM, AMF, RAK, PG, DB-F, LN, CS-P, KBW, SD, LZ, MFI and MTF were involved in the design and data collection of the study. AMM, KPE, ØS and EZ had full access to the raw data and conducted the statistical analysis. IBL, BBF, CAD, NAGF and RBC made substantial contribution to the analysis of the data. IBL drafted the manuscript. IBL, AMM, BBF, KPE, CAD, RBC, EZ, NAGF, ØS, WFCB, KSM, AMF, RAK, PG, DB-F, LN, CS-P, KBW, SD, LZ, MFI and MTF substantively revised the manuscript and approved the submitted version. IBL is the guarantor for the article.
Funding: This research was funded by the EU Horizon 2020 Grant: Healthy minds 0–100 years: Optimising the use of European brain imaging cohorts (Lifebrain) (grant agreement number: 732592).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. The data will be made available upon request until its deposited in an open science platform (deposit planned to take place before June 30).
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study involves human participants. The survey was reviewed by the Regional Committees for Medical and Health Research Ethics in Norway (2017/653 REK SørØst B) and approved for exemption from ethics approval according to the Norwegian Health Research Act. In addition, the survey was approved by the University of Oxford Medical Sciences Interdivisional Research Ethics Committee (R67364/RE001) and the Medical Ethics Review Committee of VU University Medical Center in the Netherlands as required for dissemination in the country’s research networks. Ethics approval was not required for dissemination in the other Lifebrain partner countries. Participants gave informed consent to participate in the study before taking part.
References
- 1.Raggi A, Leonardi M. Burden of brain disorders in Europe in 2017 and comparison with other non-communicable disease groups. J Neurol Neurosurg Psychiatry 2020;91:104–5. 10.1136/jnnp-2019-320466 [DOI] [PubMed] [Google Scholar]
- 2.National Institute on Aging U . What is brain health? : National Institute on Aging; 2019. Available: https://brainhealth.nia.nih.gov/ [Accessed 20 May 2019].
- 3.Mintzer J, Donovan KA, Kindy AZ, et al. Lifestyle choices and brain health. Front Med 2019;6:204. 10.3389/fmed.2019.00204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Livingston G, Sommerlad A, Orgeta V, et al. Dementia prevention, intervention, and care. Lancet 2017;390:2673–734. 10.1016/S0140-6736(17)31363-6 [DOI] [PubMed] [Google Scholar]
- 5.Glynn RW, Shelley E, Lawlor BA. Public knowledge and understanding of dementia-evidence from a national survey in Ireland. Age Ageing 2017;46:865–9. 10.1093/ageing/afx082 [DOI] [PubMed] [Google Scholar]
- 6.Rosato M, Leavey G, Cooper J, et al. Factors associated with public knowledge of and attitudes to dementia: a cross-sectional study. PLoS One 2019;14:e0210543. 10.1371/journal.pone.0210543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Heger I, Deckers K, van Boxtel M, et al. Dementia awareness and risk perception in middle-aged and older individuals: baseline results of the MijnBreincoach survey on the association between lifestyle and brain health. BMC Public Health 2019;19:678. 10.1186/s12889-019-7010-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alzheimer’s Research UK . Dementia attitudes monitor. wave 1 2018. Shaping breakthroughs in public understanding of dementia and attitudes to research, 2018. [Google Scholar]
- 9.Durand-Zaleski I, Scott J, Rouillon F, et al. A first national survey of knowledge, attitudes and behaviours towards schizophrenia, bipolar disorders and autism in France. BMC Psychiatry 2012;12:128. 10.1186/1471-244X-12-128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cadge C, Connor C, Greenfield S. University students' understanding and perceptions of schizophrenia in the UK: a qualitative study. BMJ Open 2019;9:e025813. 10.1136/bmjopen-2018-025813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tomat N, Perovnik M, Vidmar G, et al. Lay public view of neuroscience and science-based brain health recommendations in Slovenia. Front Public Health 2021;9:690421. 10.3389/fpubh.2021.690421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Niechcial MA, Vaportzis E, Gow AJ. People’s views on preserving thinking skills in old age. Educ Gerontol 2019;45:341–52. 10.1080/03601277.2019.1627054 [DOI] [Google Scholar]
- 13.Bosco A, Jones KA, Di Lorito C, et al. Changing lifestyle for dementia risk reduction: inductive content analysis of a national UK survey. PLoS One 2020;15:e0233039. 10.1371/journal.pone.0233039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rosenberg A, Coley N, Soulier A, et al. Experiences of dementia and attitude towards prevention: a qualitative study among older adults participating in a prevention trial. BMC Geriatr 2020;20:99. 10.1186/s12877-020-1493-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anderson LA, Day KL, Beard RL, et al. The public's perceptions about cognitive health and Alzheimer's disease among the U.S. population: a national review. Gerontologist 2009;49(Suppl 1):S3–11. 10.1093/geront/gnp088 [DOI] [PubMed] [Google Scholar]
- 16.Smith BJ, Ali S, Quach H. Public knowledge and beliefs about dementia risk reduction: a national survey of Australians. BMC Public Health 2014;14:661. 10.1186/1471-2458-14-661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim S, Sargent-Cox KA, Anstey KJ. A qualitative study of older and middle-aged adults' perception and attitudes towards dementia and dementia risk reduction. J Adv Nurs 2015;71:1694–703. 10.1111/jan.12641 [DOI] [PubMed] [Google Scholar]
- 18.Barak Y, Gray AR, Rapsey C, et al. The dunedin dementia risk awareness project: pilot study in older adults. Int Psychogeriatr 2020;32:241–54. 10.1017/S1041610219000772 [DOI] [PubMed] [Google Scholar]
- 19.Hosking DE, Sargent-Cox KA, Anstey KJ. An Australian survey of cognitive health beliefs, intentions, and behaviours through the adult life course. Prev Med Rep 2015;2:498–504. 10.1016/j.pmedr.2015.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Friedman DB, Becofsky K, Anderson LA, et al. Public perceptions about risk and protective factors for cognitive health and impairment: a review of the literature. Int Psychogeriatr 2015;27:1263–75. 10.1017/S1041610214002877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.The Lifebrain Consortium . Lifebrain, 2018. Available: http://www.lifebrain.uio.no/
- 22.Budin-Ljøsne I, Friedman BB, Suri S, et al. The global brain health survey: development of a Multi-Language survey of public views on brain health. Front Public Health 2020;8:387. 10.3389/fpubh.2020.00387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Walhovd KB, Fjell AM, Westerhausen R, et al. Healthy minds from 0-100 years: Optimising the use of European brain imaging cohorts ("Lifebrain"). Eur Psychiatry 2018;47:76–7. 10.1016/j.eurpsy.2017.10.005 [DOI] [PubMed] [Google Scholar]
- 24.Lifebrain . What motivates people to look after their brain health? Insights from the global brain health survey. Oslo: Lifebrain, 2022. ISBN: 978-82-8406-267-9, 2022. [Google Scholar]
- 25.Lifebrain . How to promote citizens’ brain health? Insights from the Global Brain Health. Survey on citizen’s perceptions of brain health interventions”. Lifebrain, 2021. ISBN: 978-82-8406-223-5. [Google Scholar]
- 26.Friedman BB, Suri S, Solé-Padullés C, et al. Are people ready for personalized brain health? Perspectives of research participants in the Lifebrain Consortium. Gerontologist 2020;60:1050–9. 10.1093/geront/gnz155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mauguière F, Trejo J-L, Andjus P, et al. Ten priorities for national brain and mental health plans. Croat Med J 2019;60:152–5. 10.3325/cmj.2019.60.152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.WFCM B, Arnesen KS;, Carver M;, et al. I Brain researchers want to know how you take care of your brain, 2020. Available: https://sciencenordic.com/brain-denmark-researchers-zone/brain-researchers-want-to-know-how-you-take-care-of-your-brain/1621966
- 29.Baare WFCM KA, Carver M, Drevon RB. Hjælp forskerne: Hvordan passer du på din hjerne? : Forskerzonen, 2020. Available: https://videnskab.dk/krop-sundhed/hjaelp-forskerne-hvordan-passer-du-paa-din-hjerne
- 30.R Foundation for Statistical Computing . R: A Language and Environment for Statistical Computing [program], 2021
- 31.Altman DG, Royston P. The cost of dichotomising continuous variables. BMJ 2006;332:1080.1. 10.1136/bmj.332.7549.1080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.von Elm E, Altman DG, Egger M, et al. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 2007;335:806–8. 10.1136/bmj.39335.541782.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Join dementia research. Available: https://www.joindementiaresearch.nihr.ac.uk/
- 34.Hersenonderzoek.nl. Available: https://hersenonderzoek.nl/
- 35.American Society on Aging . ASA-MetLife Foundation attitudes and awareness of brain health poll, 2006.
- 36.Vaportzis E, Gow AJ. People's beliefs and expectations about how cognitive skills change with age: evidence from a U.K.-Wide aging survey. Am J Geriatr Psychiatry 2018;26:797–805. 10.1016/j.jagp.2018.03.016 [DOI] [PubMed] [Google Scholar]
- 37.Wilcox S, Sharkey JR, Mathews AE, et al. Perceptions and beliefs about the role of physical activity and nutrition on brain health in older adults. Gerontologist 2009;49(Suppl 1):S61–71. 10.1093/geront/gnp078 [DOI] [PubMed] [Google Scholar]
- 38.IPSOS . Attitudes towards the early years, 2021. [Google Scholar]
- 39.Maust DT, Solway E, Langa KM, et al. Perception of dementia risk and preventive actions among US adults aged 50 to 64 years. JAMA Neurol 2020;77:259–62. 10.1001/jamaneurol.2019.3946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sommerlad A, Ruegger J, Singh-Manoux A, et al. Marriage and risk of dementia: systematic review and meta-analysis of observational studies. J Neurol Neurosurg Psychiatry 2018;89:231–8. 10.1136/jnnp-2017-316274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rehm J, Shield KD. Global burden of disease and the impact of mental and addictive disorders. Curr Psychiatry Rep 2019;21:10. 10.1007/s11920-019-0997-0 [DOI] [PubMed] [Google Scholar]
- 42.Barzilay R, Moore TM, Greenberg DM, et al. Resilience, COVID-19-related stress, anxiety and depression during the pandemic in a large population enriched for healthcare providers. Transl Psychiatry 2020;10:291. 10.1038/s41398-020-00982-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Arango C, Díaz-Caneja CM, McGorry PD, et al. Preventive strategies for mental health. Lancet Psychiatry 2018;5:591–604. 10.1016/S2215-0366(18)30057-9 [DOI] [PubMed] [Google Scholar]
- 44.Mehegan LRC, Skufca L. Brain health and nutrition survey. AARP research 2018, 2017. Available: 10.26419/res.00187.001 [DOI]
- 45.Wu B, Goins RT, Laditka JN, et al. Gender differences in views about cognitive health and healthy lifestyle behaviors among rural older adults. Gerontologist 2009;49(Suppl 1):S72–8. 10.1093/geront/gnp077 [DOI] [PubMed] [Google Scholar]
- 46.Gaube S, Lermer E, Fischer P. The concept of risk perception in health-related behavior theory and behavior change. In: Raue M, Streicher B, Lermer E, eds. Perceived safety: a multidisciplinary perspective. Cham: Springer International Publishing, 2019: 101–18. [Google Scholar]
- 47.Ferrer R, Klein WM. Risk perceptions and health behavior. Curr Opin Psychol 2015;5:85–9. 10.1016/j.copsyc.2015.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wahl H-W, Hoppmann CA, Ram N, et al. Healthy Aging-Relevant goals: the role of Person-Context Co-construction. J Gerontol B Psychol Sci Soc Sci 2021;76:S181–90. 10.1093/geronb/gbab089 [DOI] [PubMed] [Google Scholar]
- 49.Farkas L. Data collection in the field of ethnicity. European Commission. Luxembourg: Publications Office of the European Union, 2017. [Google Scholar]
- 50.Wang Y, Pan Y, Li H. What is brain health and why is it important? BMJ 2020;371:m3683. 10.1136/bmj.m3683 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-057999supp001.pdf (316.7KB, pdf)
bmjopen-2021-057999supp002.pdf (229.5KB, pdf)
bmjopen-2021-057999supp003.pdf (359.3KB, pdf)
bmjopen-2021-057999supp004.pdf (82.9KB, pdf)
bmjopen-2021-057999supp005.pdf (148.5KB, pdf)
Data Availability Statement
Data are available upon reasonable request. The data will be made available upon request until its deposited in an open science platform (deposit planned to take place before June 30).