Abstract
Inherited thrombophilia is an important cause of venous thrombosis. The Factor V Leiden (FVL) is the most commonly encountered mutation, followed by the prothrombin G20210A gene mutation (PTM). The typical venous thrombotic events (VTEs) associated with PTM mutations are deep vein thrombosis (DVT) and pulmonary embolisms (PE). The PTM is inherited in an autosomal dominant pattern with variable penetrance. While heterozygous PTM mutations are more frequent and well documented in the literature, rare cases of homozygous PTM mutations are also reported. In this report, we discuss a 56-year-old male with a past medical history of homozygous prothrombin gene mutation (G20210A) who presented with an unprovoked DVT of the right lower extremity involving both the proximal and distal veins associated with multiple bilateral PEs. This case is unique in terms of the homozygous PTM inheritance, the age at which the patient presented (usually presentation is earlier in life), and the fact that he had a recurrence of both DVT and PE simultaneously.
Keywords: prothrombin mutation, pulmonary embolism, deep venous thrombosis
Introduction
The prothrombin G20210A gene mutation (PTM) is the second most commonly inherited thrombophilia after Factor V Leiden (FVL) and was first described by Poort and colleagues in 1996. 1 Their paper identified a missense mutation in the 3’ untranslated region of the prothrombin gene associated with thromboembolic events and an elevated level of serum prothrombin. The mutation results from a substitution of guanine for adenine at position 20210 of the prothrombin gene on chromosome 11. 2 There is evidence that the hypercoagulable state is due to the increased efficiency of the polyadenylation site, leading to an increase in prothrombin mRNA and protein expression. 3 Although hyperprothrombinemia may also be found among the normal population, Castoldi and colleagues demonstrated that the concurrent elevation of all liver-synthesized factors including protein S and antithrombin precludes a hypercoagulable state. 4 PTM is accordingly classified as an autosomal dominant mutation with variable penetrance.
Estimates of the prevalence of PTM heterozygotes range between 1% and 6%, with an overall prevalence estimate of 2% of the general population.5,6 Prothrombin G20210A gene mutation homozygotes, such as our patient, are even less common, and indeed, there is a paucity of reports in the literature regarding homozygotes. As of 2006, only 70 cases of homozygotes were highlighted in the literature. 7 The mutation also appears to have an ethnic predisposition. While there is a preponderance of the allele among persons of Southern European heritage, the allele frequency drops significantly among persons of African or Asian descent. 6
Multiple studies have explored the relationship between PTM and the occurrence of venous thromboembolism (VTE). Decidedly, there is a 3 to 4-fold increased risk of thrombosis among PTM patients, with odds ratios in the range of 3.13 to 3.7 after excluding patients with coexisting FVL.8-10 When the co-occurrence of PTM with FVL is examined, a synergism is unveiled with odds ratios for VTE in the range of 11.8 to 58.6.11-13 The typical VTE events encountered among PTM patients are deep vein thrombosis (DVT) and pulmonary embolism (PE). However, there have been reports of thrombosis occurring at atypical sites, including portal, hepatic or cerebral veins.14,15
The gold standard for the diagnosis of PTM remains genetic testing via polymerase chain reaction (PCR). Since there is a significant overlap between the distributions of serum prothrombin concentration within the normal population versus PTM patients, coagulation testing for the disorder is unreliable for the diagnosis of PTM. The mainstay of management remains anticoagulation for 3 to 6 months, with indefinite anticoagulation considered based on other factors such as sex, family history, homozygosity, or whether the index event was provoked or unprovoked.
Here, we present the case of a PTM homozygote who developed recurrent DVT/PE 4 years following a provoked VTE event in the setting of trauma.
Case Presentation
A 56-year-old man with a history of underlying homozygous prothrombin gene mutation G20210A and prior provoked bilateral lower extremity DVTs and PE presented to the emergency department post-acute onset of palpitations in February 2020. His past medical history was notable for a motorcycle accident in 2017 for which he had shoulder surgery, after which he developed a DVT and PE and was discharged on rivaroxaban. Hypercoagulability workup including FVL, Prothrombin G20210A mutation, and deficiencies of antithrombin, protein C and protein S, only revealed homozygous prothrombin G20210A mutation. In June 2020 patient had a negative venous duplex, and a CT angiogram of the chest was negative for PE. He has been off anticoagulation for about 1 year after recommendations to be discontinued due to negative radiographic imaging. The patient reported that he is not on any current medications. Family history was negative for thrombosis or bleeding disorders. He was tachycardic with a heart rate of 120-130 beats per min, normotensive 139/78, hypoxic at 88% on room air upon initial presentation to the emergency department. Physical examination was otherwise unremarkable. Electrocardiogram showed sinus tachycardia, S1Q3T3, incomplete RBBB, right heart strain pattern evidenced by T wave inversions in V1-V3 as seen in Figure 1. Lab studies were as follows: Hb 15 g/dl (normal range 14-18 g/dl), platelets 190,000/ ul (normal range 130-400 x 10^3), troponin I 1.15 ng/ml (normal range < 0.5), Cr 1 mg/dl (0.5-1.2 mg/dl), BNP < 15 pg/ml (normal range <100), D-dimer (DDU) > 5000 ng/ml (normal range < 230), PT/INR 15.7/1.3 (PT normal range 12.6-14.6), PTT 30s (normal range 23-38). Chest x-ray was unremarkable, as seen in Figure 2. CT pulmonary angiogram showed extensive bilateral PEs with evidence of right heart strain (Figure 3-4). Echocardiogram confirmed right heart strain with moderate to severe enlargement of the right ventricle. The right ventricle was severely hypokinetic (positive McConnell sign), severe right ventricular pressure overload with a shift of interventricular septum to the left, and hyperdynamic left ventricle with an ejection fraction of 70-75%. Given the right heart strain and elevated troponin, PE was considered submassive intermediate-high risk PE. Interventional radiology (IR) consultation was obtained for catheter-directed thrombolysis. The patient was taken within 4 hours to IR, where he had catheter insertion followed by infusion of 0.5 mg of Alteplase (TPA) via 2 ports of both catheters for a total of 1 mg/hr for 24 hours and 700 unit/hr heparin. Coagulation profile and hemoglobin were monitored every 6-8 hours. Venous duplex scan demonstrated acute deep venous thrombosis of the right common femoral, femoral, popliteal, gastrocnemius, and peroneal veins and long-term DVT of the left posterior tibial vein. The patient had bleeding from the catheter site that resolved after the interventional radiologist removed the catheter after 24 hours. The patient had a significant drop in hemoglobin from 14 to 7.7 g/dl. The patient received a transfusion of 2 units of packed RBCs. No active source of bleeding was found. Hemolytic and DIC workup were negative as follows: serum LDH 200 u/l (normal range 98-192), reticulocyte count 2.6%, corrected for Hct is 1.2% (normal range 0.5-1.5%) and peripheral smear was normal, fibrinogen 305 mg/dl (normal range 270-500), Fibrin split products negative, PTT 27s, PT 15. Fecal occult blood was negative. CT scan of the chest, abdomen, and pelvis failed to show any evidence of internal bleeding. It was presumed that the drop in hemoglobin was due to the late equilibration of the blood loss that the patient had at the time of the catheter-directed thrombolysis. Physical therapy evaluated the patient as he was noted to become tachycardic up to 150 beats/min with ambulation and recommended subacute rehabilitation and cardiac rehabilitation. Therefore, the patient was discharged to subacute rehabilitation on rivaroxaban 20 mg daily with outpatient hematology and cardiology follow-up.
Figure 1.
EKG showing sinus tachycardia, S1Q3T3, incomplete RBBB, right heart strain pattern evidenced by T wave inversions in V1-V3.
Figure 2.

Chest x-ray shows no cardiopulmonary process.
Figure 3.
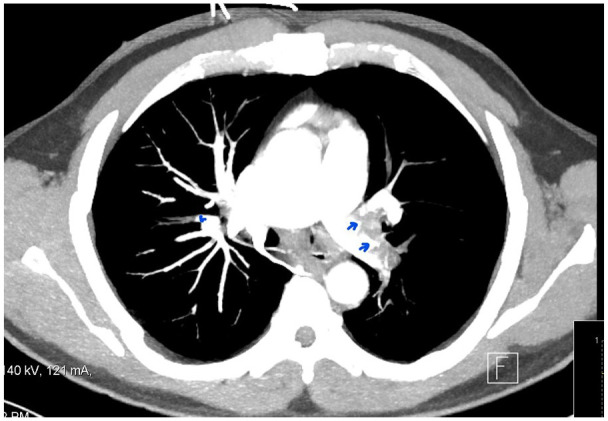
CT pulmonary Angiogram showing bilateral pulmonary embolisms (arrows).
Figure 4.

CT pulmonary angiogram shows extensive bilateral pulmonary embolisms with evidence of right heart enlargement.
Discussion
Since the description of PTM in 1996, many studies have explored the relationship between the mutation and the development of VTE. PTM heterozygosity increases the risk of VTE 3 to 4-fold.8-10 We postulate that the risk of VTE may be even greater for homozygotes on account of a further increase in serum prothrombin concentration. Our patient developed postoperative DVT/PE following a motorcycle accident. The patient’s status as a PTM homozygote naturally lends itself to the patient’s hypercoagulable state, but the patient’s VTE was provoked in the setting of trauma and postoperative immobility. Indeed, Stralen and colleagues determined that minor leg injuries, even those as innocuous as a sprain, can predispose to the development of venous thrombosis in the absence of other risk factors. 16 Furthermore, they found that patients with leg trauma and FVL carry a 50-fold increased risk of thrombosis. 16 Therefore, there may also be an underlying synergism between trauma and PTM. Although our patient required shoulder surgery in the aftermath of his accident, he conceivably suffered minor trauma to the lower extremities.
Bosler and colleagues investigated the existing case reports of homozygotes and attempted to categorize each according to categories such as age, index event, and risk factors. 7 In this article, we attempt to expand on the work undertaken by Bosler and colleagues to include individual cases reported in the literature between 2005 and 2021. Table 1 shows the reported cases of homozygous prothrombin G20210A patients during this time period. While many were asymptomatic, the most common VTE event was isolated DVT. In contrast, our patient suffered a concurrent DVT/PE during both the initial event and recurrence 4 years later. Intriguingly, while our patient had no other identifiable genetic coagulopathies, all except one of the previously reported patients with concurrent DVT/PE carried an additional inherited risk factor such as FVL, Protein S deficiency, Protein C deficiency, or antithrombin deficiency. Furthermore, our patient’s first VTE occurred at 52 years of age. Strikingly, the index event of only 12 of the 73 reported cases occurred over age 50 years. We believe that these aspects of the patient’s disease course align with the phenotypic heterogeneity among PTM homozygotes discussed by Bosler and colleagues. In addition, during the recurrent VTE episode, our patient suffered DVT of the common femoral, femoral, and popliteal veins. Thus, the patient’s presentation supports the findings of Dentali and colleagues, whose data suggest that there is a slight increase in the risk of proximal DVT versus distal DVT among PTM patients. 61
Table 1.
Prothrombin G20210A Homozygous Case Reports.
| Publication | Age/sex | Event | Acquired risk factors | Family history | Additional risk factors |
|---|---|---|---|---|---|
| Scott et al 17 | 18, female | DVT, ileo-femoral | Pregnancy | Negative | Negative |
| Howard et al 18 | 24, male | Myocardial infarction; subsequent DVT; PE | Smoking, surgery, and immobilization | Negative | FVL het |
| Kyrle et al 19 | 56, male | DVT, right leg; phlebitis | Not reported | Positive | Negative |
| 52, female | Phlebitis, bilateral legs, recurrent | Pregnancy | Positive | Negative | |
| González Ordóñez et al 20 | 65, male | Thrombotic transient ischemic attacks; DVT, femoro-iliac | Surgery | Not reported | Negative |
| Zawadzki et al 21 | 48, male | DVT; PE; mesenteric venous thrombosis | Not reported | Positive | MTHFR C677T het a |
| 30, female | PE | Not reported | Positive | MTHFR C677T het a | |
| Morange et al 22 | 44, male | DVT, left popliteal; PE | Not reported | Positive | MTHFR C677T het a |
| 74, female | Asymptomatic | Pregnancies | Positive | MTHFR C677T hom a | |
| 33-43, female (3 cases) | Asymptomatic | Pregnancy, surgery | Positive | MTHFR C677T a (2 hom, 1 het) | |
| Alatri et al 23 | 72, male | Asymptomatic | Surgeries | Positive | Negative |
| Girolami et al 24 | 29, male | Asymptomatic | Surgery | Negative | Not reported |
| 39, male | Asymptomatic | OC, pregnancies | Negative | Not reported | |
| Girolami et al 25 | 21, female | Asymptomatic | Surgery | Positive | Not reported |
| 15, female | Asymptomatic | Negative | Positive | Not reported | |
| Giordano et al 26 | 31, female | Phlebitis, left leg; TIAs; ischemic stroke | Negative | Negative | Anticardiolipin antibodies |
| Eikelboom et al 27 | 66, female | DVT, left leg | Minor surgery | Positive | Negative |
| 68, male | Asymptomatic | Not reported | Positive | Not reported | |
| Souto et al 28 | 51, male | Asymptomatic | Negative | Positive | Negative |
| 19, female | Asymptomatic | Negative | Positive | Negative | |
| Akar and Eğin 29 | 73, male | Asymptomatic | Diabetes, carcinoma | Not reported | Not reported |
| Meinardi et al 30 | 34, male | DVT | Negative | Negative | FVL hom |
| Halbmayer et al 31 | 23, male | DVT, left popliteal; PE | Negative | Positive | FVL het |
| 26, female | PE | Surgery | Positive | FVL het | |
| 20, female | Asymptomatic | Negative | Positive | Negative | |
| Kling et al 32 | 44, male | Retinal vein and retinal artery occlusion | Lymphoma | Positive | Negative |
| Corral et al 33 | 45, female | DVT | Surgery | Positive | FVL het |
| 43, male | DVT, PE | Trauma, vascular injury | Positive | FVL het | |
| 34, female | DVT | Pregnancy | Positive | FVL het | |
| Bauduer et al 34 | 40, male | Mesenteric venous thrombosis | Obesity | Positive | Negative |
| Martlew et al 35 | 31, female | Asymptomatic | Pregnancies | Negative | MTHFR C677T het a |
| Acquila et al 36 | 22, female | DVT, left leg | Pregnancy | Negative | Negative |
| Sivera et al 37 | 28, female | DVT, femoral-iliac | OC, systemic lupus | Negative | Anticardiolipin antibodies |
| 2, male | Asymptomatic | Not reported | Positive | Negative | |
| Soria et al 38 | 9, male | DVT, right popliteal | Negative | Negative | FVL hom, MTHFR C677T hom a |
| Wulf et al 39 | 18, male | Superficial thrombosis | Negative | Positive | FVL hom |
| 15, female | Asymptomatic | Not reported | Positive | Negative | |
| Vayá et al 40 | 19, female | DVT, recurrent | OC, smoker | Unknown | Negative |
| Kosch et al 41 | 13, male | DVT, bilateral legs; PE, recurrent | Immobilization | Positive | Protein S deficiency |
| 19, male | Asymptomatic | Not reported | Positive | Protein S deficiency | |
| Boinot et al 42 | 13, male | DVT, bilateral femoral; PE, bilateral | Immobilization | Positive | Protein C deficiency, Protein S deficiency |
| Kurkowska-Jastrzebska et al 43 | 29, female | Cerebral venous thrombosis | OC | Negative | FVL het |
| Klein et al 44 | 29, female | Eclampsia, HELLP syndrome | Pregnancy | Negative | Negative |
| WBH Klein et al 45 | Neonate, female | Cerebral venous sinus thrombosis, PE | None | None noted | MTHFR C677T het a , low antithrombin |
| Bosler et al 7 | 33, female | DVT leg, PE | OC, former smoker | Yes, father DVT | MTHFR A1298C het a |
| 63, male | Recurrent DVTs arm, subsequent DVT leg | Former smoker | Yes, mother PE | MTHFR C677T het a | |
| 43, male | DVT leg | Former smoker | None noted | Low antithrombin | |
| Leonard et al 46 | 22, female | DVT | OC | Positive | FVL hom |
| Germanakis et al 47 | 4, male | Stroke | Glenn anastomosis for double inlet left ventricle | Positive | MTHFR C677T hom a |
| Sogawa et al 48 | 16, male | Stroke, DVT, PE | Negative | Positive | FVL het |
| Beretta et al 49 | 30, female | DVT | Pregnancy | Positive | FVL hom |
| Uthman et al 50 | 34, female | DVT | Behcet’s disease, OC | None noted | Negative |
| Touma et al 51 | 34, female | Longitudinal myelitis; Stroke | Negative | Negative | Anticardiolipin antibodies, MTHFR C677T het a |
| Di Micco et al 52 | 27, female | DVT | OC | Negative | Negative |
| 34, female | Recurrent miscarriage | Pregnancy | Negative | Negative | |
| 42, male | Acute myocardial infarction | Negative | Positive | Negative | |
| 48, male | Asymptomatic | Negative | Positive | Negative | |
| 60, female | Stroke | Negative | Negative | Negative | |
| 40, male | Asymptomatic | Negative | Positive | Negative | |
| Roman-Gonzalez et al 53 | 32, male | DVT, PE | Sedentary | Positive | Not reported |
| 33, female | Asymptomatic | OC, Pregnancy | Positive | Not reported | |
| 31, female | DVT | Negative | Positive | Not reported | |
| 31, female | Asymptomatic | Negative | Positive | Not reported | |
| Velarde-Félix et al 54 | 48, female | Budd-Chiari Syndrome; DVT, recurrent | Negative | Positive | FVL het, JAK-2 V617F mutation |
| Yoon et al 55 | 15, male | Bilateral superficial femoral artery thrombosis | Negative | None noted | Antiphospholipid syndrome |
| Stoeva and Koleva 56 | 25, male | PE | Negative | Positive | PAI-1 4G/5G, MTHFR A1298C and C677T het a |
| 24, female | Asymptomatic | Negative | Positive | MTHFR A1298C and C677T het a | |
| George and Kent 57 | 15, female | DVT, PE | OC, Obesity | Positive | FVL het |
| Costa et al 58 | 25, male | PE | Not reported | None noted | FVL het |
| Fiore et al 59 | 31, unknown | PE, Internal iliac vein thrombosis | Not reported | None noted | Antiphospholipid syndrome |
| TRMC, not previously reported | 56, male | DVT, PE | Trauma, surgery, immobility | None noted | Negative |
Abbreviations: DVT, deep vein thrombosis; PE, pulmonary embolism; FVL, Factor V Leiden mutation; OC, oral contraceptive use; het, heterozygous; hom, homozygous; WBH, William Beaumont Hospital cases; TRMC, Trinitas Regional Medical Center.
Per AHA, MTHFR variants are no longer considered a risk factor for VTE. 60
Following our patient’s initial and recurrent DVT/PE, he was prophylactically prescribed rivaroxaban. While the management of VTE among PTM patients is infrequently reported in the literature, Costa and colleagues reported the case of a PTM homozygote with coexisting FVL who was prescribed enoxaparin in the acute setting and placed on apixaban for indefinite anticoagulation. 58 The authors reported a favorable d-dimer response and suggested that this treatment option can be considered for unprovoked VTE in the context of inherited thrombophilia. Likewise, patients such as ours with elevated D-dimer levels >5000 mg/dL may be suitable candidates for trending the treatment response to anticoagulation with novel oral anticoagulants.
Conclusion
In summary, middle-aged or elderly patients may develop a provoked DVT/PE in the setting of isolated PTM homozygosity, despite being previously asymptomatic. This case is, therefore, worth reporting to expand upon the spectrum of presentations among PTM homozygotes encountered in practice. We urge our readers to conduct more research on the choice and duration of anticoagulation treatment needed to manage patients with prothrombotic mutations.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics approval: Ethics approval is not required for case reports in our institution.
Informed Consent: Verbal consent was obtained from the patient for their anonymised information to be published in this article
ORCID iD: Ramez Alyacoub  https://orcid.org/0000-0002-2968-2944
https://orcid.org/0000-0002-2968-2944
References
- 1. Poort SR, Rosendaal FR, Reitsma PH, et al. A common genetic variation in the 3’-untranslated region of the prothrombin gene is associated with elevated plasma prothrombin levels and an increase in venous thrombosis. Blood. 1996;88(10):3698-3703. [PubMed] [Google Scholar]
- 2. Jadaon MM. Epidemiology of prothrombin G20210A mutation in the Mediterranean region. Mediterr J Hematol Infect Dis. 2011;3(1):e2011054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ceelie H, Spaargaren-van Riel CC, Bertina RM, Vos HL. G20210A is a functional mutation in the prothrombin gene; effect on protein levels and 3’-end formation. J Thromb Haemost. 2004;2(1):119-127. [DOI] [PubMed] [Google Scholar]
- 4. Castoldi E, Simioni P, Tormene D, et al. Differential effects of high prothrombin levels on thrombin generation depending on the cause of the hyperprothrombinemia. J Thromb Haemost. 2007;5(5):971-979. [DOI] [PubMed] [Google Scholar]
- 5. Zivelin A, Rosenberg N, Faier S, et al. A single genetic origin for the common prothrombotic G20210A polymorphism in the prothrombin gene. Blood. 1998;92(4):1119-1124. [PubMed] [Google Scholar]
- 6. Rosendaal FR, Doggen CJ, Zivelin A, et al. Geographic distribution of the 20210 G to A prothrombin variant. Thromb Haemost. 1998;79(4):706-708. [PubMed] [Google Scholar]
- 7. Bosler D, Mattson J, Crisan D. Phenotypic heterogeneity in patients with homozygous prothrombin 20210AA Genotype. A paper from the 2005 William Beaumont Hospital Symposium on molecular pathology. J Mol Diagn. 2006;8(4):420-425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Leroyer C, Mercier B, Oger E, et al. Prevalence of 20210 A allele of the prothrombin gene in venous thromboembolism patients. Thromb Haemost. 1998;80(1):49-51. [PubMed] [Google Scholar]
- 9. Margaglione M, Brancaccio V, Giuliani N, et al. Increased risk for venous thrombosis in carriers of the prothrombin G–>A20210 gene variant. Ann Intern Med. 1998;129(2):89-93. doi: 10.7326/0003-4819-129-2-199807150-00003. [DOI] [PubMed] [Google Scholar]
- 10. Hillarp A, Zöller B, Svensson PJ, Dahlbäck B. The 20210 A allele of the prothrombin gene is a common risk factor among Swedish outpatients with verified deep venous thrombosis. Thromb Haemost. 1997;78(3):990-992. [PubMed] [Google Scholar]
- 11. Salomon O, Steinberg DM, Zivelin A, et al. Single and combined prothrombotic factors in patients with idiopathic venous thromboembolism: prevalence and risk assessment. Arterioscler Thromb Vasc Biol. 1999;19(3):511-518. [DOI] [PubMed] [Google Scholar]
- 12. Zoller B, Svensson PJ, Dahlback B, et al. The A20210 allele of the prothrombin gene is frequently associated with the factor V Arg 506 to Gln mutation but not with protein S deficiency in thrombophilic families. Blood. 1998;91(6):2210-2211. [PubMed] [Google Scholar]
- 13. Emmerich J, Rosendaal FR, Cattaneo M, et al. Combined effect of factor V Leiden and prothrombin 20210A on the risk of venous thromboembolism–pooled analysis of 8 case-control studies including 2310 cases and 3204 controls. Study group for pooled-analysis in venous thromboembolism [published correction appears in Thromb Haemost. 2001;86(6):1598]. Thromb Haemost. 2001;86(3):809-816. [PubMed] [Google Scholar]
- 14. Zhang P, Zhang J, Sun G, et al. Risk of Budd-Chiari syndrome associated with factor V Leiden and G20210A prothrombin mutation: a meta-analysis. PLoS ONE. 2014;9(4):e95719. doi: 10.1371/journal.pone.0095719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gonzalez JV, Barboza AG, Vazquez FJ, Gándara E. Prevalence and geographical variation of prothrombin G20210A mutation in patients with cerebral vein thrombosis: a systematic review and meta-analysis. PLoS ONE. 2016;11(3):e0151607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. van Stralen KJ, Rosendaal FR, Doggen CJ. Minor injuries as a risk factor for venous thrombosis. Arch Intern Med. 2008;168(1):21-26. doi: 10.1001/archinternmed.2007.5. [DOI] [PubMed] [Google Scholar]
- 17. Scott C, Hanley J, Ludlam C, et al. Homozygosity for a factor II polymorphism associated with thrombosis during pregnancy. Thromb Haemostasis. 1997;77(Suppl. Abstract):770. [Google Scholar]
- 18. Howard TE, Marusa M, Channell C, Duncan A. A patient homozygous for a mutation in the prothrombin gene 3’-untranslated region associated with massive thrombosis. Blood Coagul Fibrinolysis. 1997;8(5):316-319. [DOI] [PubMed] [Google Scholar]
- 19. Kyrle PA, Mannhalter C, Béguin S, et al. Clinical studies and thrombin generation in patients homozygous or heterozygous for the G20210A mutation in the prothrombin gene. Arterioscler Thromb Vasc Biol. 1998;18(8):1287-1291. doi: 10.1161/01.atv.18.8.1287. [DOI] [PubMed] [Google Scholar]
- 20. González Ordóñez AJ, Medina Rodriguez JM, Fernández Alvarez CR, Macias Robles MD, Coto García E. A patient homozygous for mutation 20210A in the prothrombin gene with venous thrombosis and transient ischemic attacks of thrombotic origin. Haematologica. 1998;83(11):1050-1051. [PubMed] [Google Scholar]
- 21. Zawadzki C, Gaveriaux V, Trillot N, et al. Homozygous G20210A transition in the prothrombin gene associated with severe venous thrombotic disease: two cases in a French family. Thromb Haemost. 1998;80(6):1027-1028. [PubMed] [Google Scholar]
- 22. Morange PE, Barthet MC, Henry M, et al. A three-generation family presenting five cases of homozygosity for the 20210 G to A prothrombin variant. Thromb Haemost. 1998;80(5):859-860. [PubMed] [Google Scholar]
- 23. Alatri A, Franchi F, Moia M. Homozygous G20210A prothrombin gene mutation without thromboembolic events: a case report. Thromb Haemost. 1998;80(6):1028-1029. [PubMed] [Google Scholar]
- 24. Girolami A, Simioni P, Manfrin D, et al. Asymptomatic homozygous nt 20210 G to A prothrombin polymorphism in two blood donors belonging to two different kindreds. Clin Appl Thromb Hemost. 1999;5(1):48-51. [DOI] [PubMed] [Google Scholar]
- 25. Girolami A, Simioni P, Tormene D, et al. Two additional homozygous patients for the 20210 prothrombin polymorphism with no venous thrombosis. Thromb Res. 1999;96(5):415-417. [DOI] [PubMed] [Google Scholar]
- 26. Giordano P, De Lucia D, Coppola B, Iolascon A. Homozygous prothrombin gene mutation and ischemic cerebrovascular disease: a case report. Acta Haematol. 1999;102(2):101-103. doi: 10.1159/000040979. [DOI] [PubMed] [Google Scholar]
- 27. Eikelboom JW, Ivey L, Ivey J, Baker RI. Familial thrombophilia and the prothrombin 20210A mutation: association with increased thrombin generation and unusual thrombosis. Blood Coagul Fibrinolysis. 1999;10(1):1-5. [PubMed] [Google Scholar]
- 28. Souto JC, Mateo J, Soria JM, et al. Homozygotes for prothrombin gene 20210 A allele in a thrombophilic family without clinical manifestations of venous thromboembolism. Haematologica. 1999;84(7):627-632. [PubMed] [Google Scholar]
- 29. Akar N, Eğin Y. A further case of homozygous G20210A prothrombin gene mutation without thromboembolic events. Clin Appl Thromb Hemost. 1999;5(4):284. [DOI] [PubMed] [Google Scholar]
- 30. Mainardi JR, Pelsma PM, Koning H, et al. Double-homozygosity for factor V Leiden and the prothrombin gene G20210A variant in a young patient with idiopathic venous thrombosis. Blood. 1999;94(5):1828-1829. [PubMed] [Google Scholar]
- 31. Halbmayer WM, Kalhs T, Haushofer A, Breier F, Fischer M. Venous thromboembolism at a young age in a brother and sister with coinheritance of homozygous 20210A/A prothrombin mutation and heterozygous 1691G/A factor V Leiden mutation. Blood Coagul Fibrinolysis. 1999;10(5):297-302. [DOI] [PubMed] [Google Scholar]
- 32. Kling F, Macarez R, Robinet A, et al. Thrombose mixte rétinienne chez un patient porteur d’une mutation du gène de la prothrombine, à l’état homozygote [Mixed retinal thrombosis in a patient carrying prothrombin gene mutation in a homozygote state]. J Fr Ophtalmol. 1999;22(9):979-981. [PubMed] [Google Scholar]
- 33. Corral J, Zuazu-Jausoro I, Rivera J, González-Conejero R, Ferrer F, Vicente V. Clinical and analytical relevance of the combination of prothrombin 20210A/A and factor V Leiden: results from a large family. Br J Haematol. 1999;105(2):560-563. [PubMed] [Google Scholar]
- 34. Bauduer F, Claracq M, Orgogozo F, Mariescu M, Ducout L, Freyburger G. Mesenteric venous thrombosis in a 40-year-old man with homozygous factor II G20210A mutation. Blood Coagul Fibrinolysis. 2000;11(8):785-786. [DOI] [PubMed] [Google Scholar]
- 35. Martlew VJ, Perez-Casal M, Alfirevic Z, Toh CH. What clinical significance has the presence of the homozygous G20210A prothrombin gene mutation in a healthy woman? Thromb Haemost. 2000;84(2):355-356. [PubMed] [Google Scholar]
- 36. Acquila M, Bicocchi MP, Mori PG, Odino S, Valetto A, Bottini F. A homozygosity state for 20210A prothrombin variant in a young woman as cause of a deep venous thrombosis during pregnancy. Eur J Haematol. 2000;65(1):80-81. doi: 10.1034/j.1600-0609.2000.9l140.x. [DOI] [PubMed] [Google Scholar]
- 37. Sivera P, Bosio S, Bertero MT, Demaestri M, Mazza U, Camaschella C. G20210A homozygosity in antiphospholipid syndrome secondary to systemic lupus erythematosus. Haematologica. 2000;85(1):109-110. [PubMed] [Google Scholar]
- 38. Soria JM, Quintana R, Vallvé C, Iruin G, Cortés C, Fontcuberta J. A boy with venous thrombosis, homozygous for factor V Leiden, prothrombin G20210A and MTHFR C667t mutations, but belonging to an asymptomatic family. Haematologica. 2000;85(11):1230-1232. [PubMed] [Google Scholar]
- 39. Wulf GM, Van Deerlin VM, Leonard DG, Bauer KA. Thrombosis in a patient with combined homozygosity for the factor V Leiden mutation and a mutation in the 3’-untranslated region of the prothrombin gene. Blood Coagul Fibrinolysis. 1999;10(2):107-110. [DOI] [PubMed] [Google Scholar]
- 40. Vayá A, García M, Mira Y, et al. Homozygous 20210G/A prothrombin gene mutation associated with bilateral iliac vein thrombosis: a case report. Thromb Res. 2001;104(4):293-296. [DOI] [PubMed] [Google Scholar]
- 41. Kosch A, Junker R, Wermes C, et al. Recurrent pulmonary embolism in a 13-year-old male homozygous for the prothrombin G20210A mutation combined with protein S deficiency and increased lipoprotein (a). Thromb Res. 2002;105(1):49-53. [DOI] [PubMed] [Google Scholar]
- 42. Boinot C, Borgel D, Kitzis A, Guicheteau M, Aiach M, Alhenc-Gelas M. Familial thrombophilia is an oligogenetic disease: involvement of the prothrombin G20210A, PROC and PROS gene mutations. Blood Coagul Fibrinolysis. 2003;14(2):191-196. [DOI] [PubMed] [Google Scholar]
- 43. Kurkowska-Jastrzebska I, Wicha W, Dowzenko A, et al. Concomitant heterozygous factor V Leiden mutation and homozygous prothrombin gene variant (G20210A) in patient with cerebral venous thrombosis. Med Sci Monit. 2003;9(5):CS41-CS45. [PubMed] [Google Scholar]
- 44. Klein R, Howe JG, Magriples U, McPhedran P. Eclampsia in a woman homozygous for the prothrombin G20210A mutation. Thromb Haemost. 2004;91(1):201-202. [PubMed] [Google Scholar]
- 45. Klein L, Bhardwaj V, Gebara B. Cerebral venous sinus thrombosis in a neonate with homozygous prothrombin G20210A genotype. J Perinatol. 2004;24(12):797-799. doi: 10.1038/sj.jp.7211187. [DOI] [PubMed] [Google Scholar]
- 46. Leonard M, Gala JL, Verschuren F, Coche E, Deneys V, Hainaut P. Venous thromboembolism in a young woman with combined homozygosity for factor V Leiden and prothrombin G20210A mutations. Haematologica. 2005;90(Suppl.):ECR30. [PubMed] [Google Scholar]
- 47. Germanakis I, Sfyridaki C, Papadopoulou E, et al. Stroke following Glenn anastomosis in a child with inherited thrombophilia. Int J Cardiol. 2006;111(3):464-467. [DOI] [PubMed] [Google Scholar]
- 48. Sogawa Y, Libman R, Eviatar L, Kan L. Pulsatile tinnitus in a 16-year-old patient. Pediatr Neurol. 2005;33(3):214-216. doi: 10.1016/j.pediatrneurol.2005.03.012. [DOI] [PubMed] [Google Scholar]
- 49. Beretta AL, Bianchi M, Norchi S, Martinelli I. Pregnancy-associated deep vein thrombosis in a double homozygous carrier of factor V Leiden and prothrombin G20210A. Thromb Haemost. 2005;94(6):1329-1330. [DOI] [PubMed] [Google Scholar]
- 50. Uthman I, Otrock Z, Taher A. Deep venous thrombosis in a patient with Behçet’s disease and homozygous prothrombin (factor II) G20210A mutation on oral contraceptive pills. Rheumatol Int. 2006;26(8):758-759. [DOI] [PubMed] [Google Scholar]
- 51. Touma Z, Atweh SF, Kibbi L, Arayssi T. Longitudinal myelitis in patient with systemic lupus erythematosus, homozygous prothrombin G20210A and heterozygous MTHFR 677T. Lupus. 2007;16(7):517-520. [DOI] [PubMed] [Google Scholar]
- 52. Di Micco P, Di Fiore R, Niglio A, et al. Different outcome of six homozygotes for prothrombin A20210A gene variant. J Transl Med. 2008;6:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Roman-Gonzalez A, Cardona H, Cardona-Maya W, et al. The first homozygous family for prothrombin G20210A polymorphism reported in Latin America. Clin Appl Thromb Hemost. 2009;15(1):113-116. [DOI] [PubMed] [Google Scholar]
- 54. Velarde-Félix JS, Sanchez-Zazueta J, Gonzalez-Ibarra FP, et al. Budd-Chiari syndrome in a patient with JAK-2 V617F and factor V G1691A mutations. West Indian Med J. 2014;63(5):528-531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Yoon U, Kwok L, Flessenkaemper I. Bilateral superficial femoral artery thrombosis in a 15-year-old caucasian male with homozygous prothrombin G20210A genotype and associated antiphospholipid syndrome. Int J Angiol. 2016;25(5):e100-e105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Stoeva NY, Koleva VS. Homozygous carrier of prothrombin G20210A mutation with massive pulmonary embolism and his family: gender differences of susceptibility to mutation. Folia Med. 2016;58(1):64-66. [DOI] [PubMed] [Google Scholar]
- 57. George AP, Kent P. The impact of multiple risk factors for venous thromboembolism and its implications for management. Glob Pediatr Health. 2019;6:2333794X19859161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Costa RL, Triggs M, Cole SE, et al. Anticoagulation therapy in a patient with heterozygous factor V Leiden and coexisting homozygous prothrombin gene mutations. Cureus. 2020;12(12):e11949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Fiore JR, Ciarallo M, Di Stefano M, et al. Severe systemic thrombosis in a young COVID-19 patient with a rare homozygous prothrombin G20210A mutation. Infez Med. 2021;29(2):259-262. [PubMed] [Google Scholar]
- 60. Hickey SE, Curry CJ, Toriello HV. ACMG practice guideline: lack of evidence for MTHFR polymorphism testing [published correction appears in Genet Med. 2020 Jun 12:]. Genet Med. 2013;15(2):153-156. [DOI] [PubMed] [Google Scholar]
- 61. Dentali F, Pomero F, Borretta V, et al. Location of venous thrombosis in patients with FVL or prothrombin G20210A mutations: systematic review and meta-analysis. Thromb Haemost. 2013;110(1):191-194. [DOI] [PubMed] [Google Scholar]



