Abstract
Successful campaigns to combat the COVID-19 pandemic depend, in part, on people's willingness to be vaccinated. It is therefore critical to understand the factors that determine people's vaccination intentions. We applied a reasoned action approach - the theory of planned behavior - to explore these factors. We used data from an online survey of adults (18–74 years; n = 5044) conducted in Germany between April 9 and April 28, 2021 and found that attitudes toward getting vaccinated predicted vaccination intentions, while normative and control beliefs did not. In turn, positive attitudes toward getting vaccinated were supported by trust in science and fear of COVID-19 whereas negative attitudes were associated with acceptance of conspiracy theories and skepticism regarding vaccines in general. We advise policymakers, physicians, and health care providers to address vaccination hesitancy by emphasizing factors that support positive attitudes toward getting vaccinated, such as prevention of serious illness, death, and long-term health detriments, as opposed to exerting social pressure or pointing to the ease of getting vaccinated.
Keywords: COVID-19, Theory of planned behavior, Vaccination intentions, Institutional trust, Fear of COVID-19, Conspiracy beliefs and denial of COVID-19, Skepticism toward vaccines
1. Introduction
Vaccination is deemed a key to successfully combat the COVID-19 pandemic (e.g., Das et al., 2020; Pandey et al., 2020; Sarwar et al., 2020). Effective vaccines have been rapidly developed and have become readily available in most developed countries in 2021 (Kashte et al., 2021; see also https://ourworldindata.org/covid-vaccinations). However, vanquishing the pandemic depends not only on the availability of effective and safe vaccines but also on peoples’ willingness to be vaccinated (e.g., Dror et al., 2020). Although in most developed countries a considerable proportion of the eligible population has by now been vaccinated, vaccination acceptance rates vary greatly both between and within countries (e.g., Neumann-Böhme et al., 2020; Sallam, 2021). To date, the goal of achieving herd immunity appears out of reach as many individuals are reluctant to be vaccinated or are outright hostile to vaccination campaigns.
The vaccination campaign in Germany began officially on December 27, 2020 (Federal Ministry of Health, 2021). People from the highest priority group (e.g., people aged 80 and above, people with pre-existing conditions, residents and staff of care facilities, medical and nursing staff) were the first to get vaccinated. Beginning in April 2021 (with some variations among German states), individuals belonging to the second priority group (e.g., individuals over age 70, people with trisomy 21, dementia patients, people who have undergone organ transplants, police and law enforcement personnel, close contacts of people in need of care, pregnant women, and people living or working in refugee or homeless facilities) were vaccinated. Vaccination was organized via an appointment system of the German federal states and carried out by mobile vaccination teams in nursing homes, in state-organized vaccination centers, or – later – also by general practitioners. The national supervisory authority (Robert Koch-Institute; www.rki.de/EN/Home/) reports that, despite the ready availability of vaccines, the rate of COVID-19 vaccination in Germany decreased considerably during the summer of 2021. Measures proposed to counteract vaccination resistance included incentives to get vaccinated, preferential treatment of vaccinated persons, and sanctioning of those who refused to be vaccinated. However, developing effective intervention strategies requires a better understanding of the factors that determine people's willingness (or unwillingness) to be vaccinated (Michie et al., 2021; Van Bavel et al., 2020).
To explore the factors that determine vaccination intentions, the current study relies on the theory of planned behavior (TPB; Ajzen, 1991; 2012), a reasoned action approach (Fishbein and Ajzen, 2010). The conceptual framework of the TPB considers attitudes, subjective norms, and perceived behavioral control to be direct antecedents of intentions and also allows us to examine more distal background factors. The latter include beliefs about the coronavirus, concerns regarding the available vaccines, trust in institutions, religious and left-right political orientations (see Piurko et al. 2011; Wojcik et al., 2021), and socioeconomic and demographic factors.
In the following section we provide a brief description of the theory of planned behavior and a review of the major findings from the international literature on vaccination intentions and hesitancy.
2. Intentions to receive a vaccination against COVID-19
2.1. The theory of planned behavior
As in other “reasoned action” approaches (see Fishbein and Ajzen, 2010), the immediate antecedent of behavior in the TPB is the intention to perform the behavior in question. The stronger the intention, the more likely it is that the behavior will follow. Thus, all else equal, intentions to get vaccinated should be predictive of actual behavior (for a general discussion of the relation between intention and behavior, see Fishbein and Ajzen, 2010, pp. 43–64).
According to the TPB, three kinds of considerations guide the formation of intentions. One set of considerations are instrumental and experiential beliefs about the performance of the behavior (behavioral beliefs). For example, people may believe that getting vaccinated reduces the likelihood of contracting the coronavirus (a positive consequence) but, at the same time, also believe that getting the shot is painful (a negative experience). In their aggregate, behavioral beliefs lead to the formation of a favorable or unfavorable attitude toward the behavior (for a general discussion of beliefs as the basis of attitudes, see Fishbein and Ajzen, 2010, pp. 96–103).
A second type of consideration are beliefs about the expectations and behaviors of significant social referents (e.g., spouse or partner, family, close friends, coworkers), which produce perceived social pressure to engage or not to engage in the behavior, or subjective norm (for a general discussion of beliefs as the basis of subjective norms, see Fishbein and Ajzen, 2010, pp. 134–148). Thus, for example, people may believe that their physicians think they should get vaccinated against COVID-19 (an injunctive normative belief supportive of the behavior) but that most of their friends do not intend to get the vaccine (a deterring descriptive normative belief).
Finally, the third type of consideration are beliefs about factors that may facilitate or impede performance of the behavior (control beliefs), which result in perceived behavioral control or a sense of self-efficacy (Bandura, 1997). Thus, people may believe that getting vaccinated is time consuming (an impeding control belief) but that a family member will provide a ride to a vaccination center (a facilitating control belief) (for a general discussion of control beliefs as a basis of perceived behavioral control, see Fishbein and Ajzen, 2010, pp. 170–177).
Due to space limitations in the questionnaire, in the present study we operationalized only the three direct predictors of intentions, i.e., attitudes, subjective norms, and perceived behavioral control, but not the behavioral, normative, and control beliefs that, from a theoretical perspective, provide the basis for these predictors. In most applications of the TPB, the three direct predictors of intentions have been treated as additive factors, although in the original formulation of the theory Ajzen (1985) discussed the possibility that perceived behavioral control moderates the effects of attitudes and subjective norms on intentions. Indeed, in the theory's most recent formulation (Fishbein and Ajzen, 2010), favorable attitudes and supportive subjective norms are assumed to motivate people to perform the behavior, but this motivation leads them to form an intention to engage in the behavior only to the extent that they believe that they can perform the behavior in question. Several empirical studies have provided evidence in support of the proposed interaction effects (e.g., Hukkelberg et al., 2014; La Barbera and Ajzen, 2020; Yzer & van den Putte, 2014).
The TPB has been used to predict and explain a variety of behaviors among which health-related behaviors are the most frequently studied domain (e.g., Bosnjak et al., 2020; Fishbein and Ajzen, 2010; Steinmetz et al., 2016; Winkelnkemper et al., 2018). A meta-analysis (Winkelnkemper et al., 2018) has shown that health-related behavioral intentions are the strongest predictors of health-related behaviors and that these intentions are predicted by attitudes, subjective norms, and perceived behavioral control (see also Godin and Kok, 1996; McEachan et al., 2011). Of direct relevance to the present study, the TPB has been applied to explain vaccination intentions concerning diseases other than COVID-19 (e.g., Agarwal, 2014; Fisher et al., 2013) showing that attitudes, subjective norms, and perceived behavioral control are consistently related to behavioral intentions, with attitudes often being the strongest predictor. This result was also found for COVID-19 vaccine uptake intentions in studies that tested the TPB (e.g., Guidry et al., 2021; Wolff, 2021) or integrated approaches using some of the TPB's predictor variables (e.g., Chu and Liu, 2021; Graupensperger et al., 2021; Mo et al., 2021; Shmueli, 2021).
2.2. Background factors relevant to COVID-19 vaccination intentions
Various factors that are not an integral part of the TPB may be related indirectly to intentions to get vaccinated against COVID-19. These background factors can be personal in nature (e.g., general attitudes, personality traits, values, emotions), informational (e.g., experience, knowledge, media exposure), and demographic (e.g., age, gender, race, ethnicity, education, income, religion). These factors are assumed to have no direct effects on intentions but can influence them indirectly via the more proximal antecedents of intentions specified in the theory (Fishbein and Ajzen, 2010). Thus, exploration of background factors can greatly enhance our understanding of the sociological and social psychological foundation of vaccination intentions, its primary predictors, and associated health outcomes (see also Godin et al., 2010; Hagger and Hamilton, 2021; de Leeuw et al., 2015; McKinley et al., 2020).
Institutional trust. Institutional trust refers to citizens' beliefs that institutions (e.g., government, the justice system, the medical establishment, science) act in a predictable, equitable, fair, and transparent manner and in ways that serve the citizens’ interests (e.g., Fukuyama, 1995; Putnam et al., 1993). Trust in institutions is related to perceived legitimacy of institutions (Khodyakov, 2007) and compliance with formal and informal norms (Tyler, 2006). Thus, people who trust their institutions may be expected to have a more positive attitude toward getting vaccinated against COVID-19, because they are more likely to believe that official information regarding the safety and effectiveness of vaccines is accurate. By way of contrast, institutional distrust is linked to many negative outcomes such as political extremism (Algan et al., 2017), deviant behavior (Lindström, 2008), and legal permissiveness (Marien and Hooghe, 2011). People who distrust institutions may therefore be more likely to reject vaccination because they may question the safety and effectiveness of vaccines. Recent studies have found that trust in both political institutions and science were associated with positive attitudes toward the COVID-19 vaccination and a higher willingness to be vaccinated (Allington et al., 2021; Jennings et al., 2021; Jensen et al., 2021; Petravić et al., 2021; Thaker, 2021; Troiano and Nardi, 2021). In contrast, distrust in science has been found to be associated with negative attitudes and vaccination hesitancy (Al-Qerem and Jarab, 2021; Byrne et al., 2021; Chen et al., 2021; Guidry et al., 2021; Janssens et al., 2021; Jennings et al., 2021; Karlsson et al., 2021; Kreps et al., 2021; Latkin et al., 2021c; Machida et al., 2021; Malesza and Wittmann, 2021; Mo et al., 2021; Paul et al., 2021; Petravić et al., 2021; Sherman et al., 2021; Soares et al., 2021; Thaker, 2021; Troiano and Nardi, 2021).
Fear of COVID-19. The COVID-19 pandemic has severe detrimental effects on peoples’ physical and mental health (Giuntella et al., 2021). The severity of the disease, the required precautionary measures, and the possibility of being hospitalized and die are associated with increased feelings of anxiety and perceptions of threat from COVID-19, especially among vulnerable people, such as older adults, healthcare workers and caregivers, immigrants, victims of domestic violence, and people with mental health conditions or disabilities (Quadros et al., 2021; Rodríguez-Hidalgo et al., 2020). Thus, people who feel anxious about COVID-19 may be more likely to have a positive attitude toward getting vaccinated, simply because the vaccine can effectively reduce fear by providing protection from a severe or even deadly course of the disease. Recent studies have shown that the fear of infection and perceived vulnerability are indeed positively related with attitudes toward getting vaccinated against COVID-19 and vaccination intentions (Bendau et al., 2021; Chu and Liu, 2021; Fridman et al., 2021; Guidry et al., 2021; Jennings et al., 2021; Karlsson et al., 2021; Kourlaba et al., 2021; Malesza and Wittmann, 2021; Ruiz and Bell, 2021; Troiano and Nardi, 2021).
Conspiracy beliefs, denial of COVID-19 and skepticism toward vaccines. Conspiracy beliefs are narratives “in which the ultimate cause of an event is believed to be due to a plot by multiple actors working together with a clear goal in mind, often unlawfully and in secret” (Swami and Furnham, 2014, p. 220). Such beliefs are reinforced by confirmation bias (McHoskey, 1995), the tendency to search for and accept arguments and evidence that confirm one's own position on a subject while disregarding contradictory evidence. Similarly, denialism refers to rejection of the consensus on well-established scientific propositions, which is characterized by rejecting data and scientific literature, accusing scientists of conspiracy, relying on fake experts, selective picking and quoting, creating exaggerated expectations of science to scientific uncertainty, and using misrepresentation and logical fallacies (Diethelm and McKee, 2009). Conspiracy beliefs and denialism are most prevalent among people with extreme political positions (Washburn and Skitka, 2018) and those who distrust science (Lewandowsky et al., 2013). Thus, people who believe that COVID-19 is the result of a conspiracy and reject scientific consensus on the health dangers of the virus and the effectiveness and safety of vaccines are likely to have a more negative attitude toward vaccination. Recent studies have found that conspiracy beliefs and denialism regarding COVID-19 and vaccinations are related to negative attitudes and lower intentions to be vaccinated (Allington et al., 2021; Bertin et al., 2020; Freeman et al., 2021; Jensen et al., 2021; Kourlaba et al., 2021; Ruiz and Bell, 2021; Sallam et al., 2021; Sherman et al., 2021).
Socioeconomic and demographic factors, self-rated health, religiosity and left-right political orientation. Socioeconomic status is related to health behaviors such as getting vaccinated via the “barriers to immunization” mechanism (Link and Phelan, 1995; Ward and Raude, 2014). A lower socioeconomic status (e.g., low education and income, immigration background) may limit access to healthcare services and lead to poor health, lower life-expectancies, delayed vaccination, and opposition to vaccination (Kawachi et al., 1997; Peretti-Watel et al., 2014; Prislin et al., 1998; Wilkinson and Pickett, 2006; Winston et al., 2006). Indeed, recent studies indicated that higher education and other demographic factors such as older age, being male, and marriage are associated with a more positive attitude toward COVID-19 vaccination and higher vaccination intentions, while negative attitudes and vaccination hesitancy were reported for people with lower income, living with children, and having an immigrant background (Alabdulla et al., 2021; Allington et al., 2021; Byrne et al., 2021; Green et al., 2021; Kourlaba et al., 2021; Latkin et al., 2021b, 2021c; Machida et al., 2021; Paul et al., 2021; Petravić et al., 2021; Robertson et al., 2021; Ruiz and Bell, 2021; Sallam et al., 2021; Salmon et al., 2021; Soares et al., 2021; Thaker, 2021; Troiano and Nardi, 2021). Moreover, religiosity and right-wing political orientation are found to be related to negative attitudes and a lower willingness to get vaccinated against COVID-19 (Latkin et al., 2021a, 2021b; Ruiz and Bell, 2021; Troiano and Nardi, 2021), while pre-existing health conditions are related to a higher vaccination likelihood (Ruiz and Bell, 2021).
2.3. Hypotheses
We derive the following hypotheses regarding vaccination intentions based on the TPB and the background factors discussed above.
-
•
Intentions to get vaccinated against COVID-19 can be predicted from attitude toward getting vaccinated (H1), subjective norm regarding this behavior (H2), and perceived behavioral control (H3).
-
•
Perceived behavioral control moderates the relation between attitude and intention (H4) and between subjective norm and intention (H5). The strength of these relations increases with perceived behavioral control.
As noted, in the TPB, background factors are assumed to affect vaccination intentions indirectly. The following hypothesized correlations of background factors with intentions are therefore expected to be mediated by the intentions’ proximal antecedents, that is, by attitude, subjective norm, and/or perceived behavioral control with respect to getting vaccinated.
-
•
Institutional trust (H6) and fear of COVID-19 (H7) correlate positively with vaccination intentions.
-
•
Conspiracy beliefs/denial of COVID-19 (H8) and skepticism toward vaccines (H9) correlate negatively with vaccination intentions.
-
•
Poor health (H10) correlates positively with vaccination intentions.
-
•
Religiosity (H11) and right-wing orientation (H12) correlate negatively with vaccination intentions.
-
•
Older age (H13), being male (H14), high education (H15) and income (H16), being married or living in a partnership (H17) correlate positively with vaccination intentions.
-
•
Living with children (H18) and immigrant background (H19) correlate negatively with vaccination intentions.
3. Data, measures, and methods of analysis
3.1. Data
An ongoing German online access panel by the market research institute Respondi AG (https://www.respondi.com/EN/) was used to collect the data. Panel participants were recruited online through various channels (campaigns, marketers and by self-recruitment) and, after registering, were invited by an e-mail from the company to take part in the study. The sample for the current study included 5044 participants aged 18 to 74 residing in Germany. Quotas were implemented to achieve rates for gender, age, education, income, and immigration background comparable to those in the German population (German Federal Statistical Office, 2021). With the exception of immigration background (17% in the sample, 25% in the German microcensus data) the quotas were met. Participation was voluntary and participants did not sign a separate consensus form for this study. They were paid 75 cents for their participation. The survey was conducted between April 9 and April 28, 2021 in Germany, with the approval of the ethics committee of the Faculty of Management, Economics and Social Sciences, University of Cologne, Germany (reference: 210005DS).
At the time of the survey, 19.4% of the respondents reported that they had already received at least one vaccine against COVID-19, which matched the official vaccination rate reported by the Robert Koch-Institute (e.g., 19.6% on April 17). The remaining 80.6% (n = 4061) of participants who were not yet vaccinated responded to the part of the questionnaire that contained the indicators for the TPB. We deleted careless participants (Meade and Craig, 2012) who took less than 5 min to complete the questionnaire or who gave the same answer repeatedly. The median survey completion duration was 19 min, and the final sample size included 3532 respondents.
3.2. Measures
All TPB-related questions were presented to the respondents with the request that they assume they can get an appointment for a vaccination quickly. Intentions, attitudes toward the behavior, subjective norms, and perceived behavioral control were measured using several reflective indicators for each construct.
The dependent variable intention to receive a vaccination (INT) against COVID-19 was measured by three indicators (int1-int3). Attitude (ATT), subjective norm (SN), and perceived behavioral control (PBC) were measured by four indicators each (att1-att4, sn1-sn4, pbc1-pbc4). All answers were given on 7-point scales.
The survey contained measures of various background factors: COVID-19 conspiracy beliefs (CCB – 8 indicators), general conspiracy mindedness (GCM – 5 indicators), skepticism toward vaccines (SKV - 3 indicators), skepticism toward doctors (SKD – 3 indicators), fear of COVID-19 (FCV – 3 indicators), trust in politics (TPO – 6 indicators) and trust in science (TSC – 4 indicators). In addition, we measured self-rated health, self-rated risk of a severe course of COVID-19, religiosity, political orientation and socioeconomic and demographic variables (age, gender, education, income, immigration background, partnership status, living with children). The indicators measuring the constructs, the socioeconomic and demographic variables, and descriptive statistics are shown in the Online Appendix (A1).
3.3. Methods of analysis
We applied exploratory factor analysis (EFA) and confirmatory factor analysis (CFA) to test the relationships between the unobserved latent variables and measured indicators (Brown, 2015) and structural equation modeling (Bollen, 1989) to test the substantive hypotheses. The latent interaction effects were estimated using the residual centering approach (Little et al., 2006; Steinmetz et al., 2011). For calculations we used R 3.6.1 (R Core Team, 2019) and the packages lavaan (Rosseel, 2012), psych (Revelle, 2021), and semTools (Jorgensen et al., 2021). Post-hoc power analysis was carried out using the semPower package (Moshagen and Erdfelder, 2016). We used maximum likelihood estimation with standard errors and test statistics (Satorra and Bentler, 1994; Yuan and Bentler, 2000) that are robust with respect to non-normality in the data (MLR in lavaan) and we treated missing values (whose rate was low for most variables) using full information estimation. The data used in this analysis and R codes can be retrieved from https://osf.io/7rjmp/. In addition, codes and outputs are available in the Online Appendix.
4. Results
4.1. Exploratory factor analysis (EFA) and confirmatory factor analysis (CFA)
We performed EFA for the TPB constructs and background factors and kept indicators that demonstrated high factor loadings and no cross-loadings (see Online Appendix A2). CFA models for the constructs fitted the data well and all standardized factor loadings were above 0.70 (see Online Appendix A3). Although we observed strong correlations among some constructs, they still exhibited acceptable discriminant validity (correlations below 0.85, Brown, 2015). Omega coefficients (McDonald, 1999) were satisfactory with the exception of the value for skepticism toward doctors, which was somewhat lower: ωTPO = 0.957, ωCCB = 0.943, ωATT = 0.940, ωSKV = 0.925, ωTSC = 0.907, ωGCM = 0.895, ωFCV = 0.841, ωSN = 0.816, ωPBC = 0.776, ωSKD = 0.720.
4.2. Structural equation models
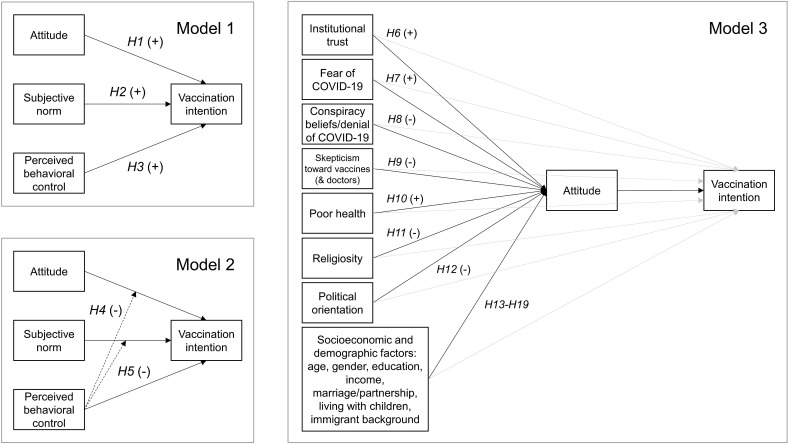
We estimated three models to test our hypothesis (see Fig. 1, Fig. 2 ).
Fig. 1.
Models specified to test hypotheses H1–H19. Solid black arrows indicate direct relationships between constructs. Dashed black arrows (Model 2) indicate moderation of relationships. Solid gray arrows (Model 3) indicate direct relationships between background factors and vaccination intention (not expected to be significant based on the TPB).
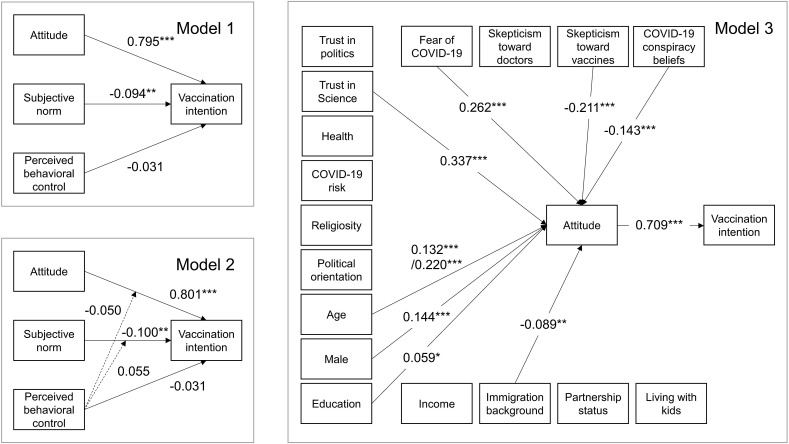
Fig. 2.
SEM results (standardized coefficients), model 1: n = 3507, model 2: n = 3507, model 3: n = 3110. Different sample sizes are due to missing values on indicators (model 1 and model 2) and predictors (model 3). For clarity, correlations among predictors are not shown and only significant paths are shown for model 3. *p ≤ 0.05, **p ≤ 0.01, ***p ≤ 0.001.
The first model (Model 1) only considered the prediction of vaccination intentions from attitudes, subjective norms, and perceived behavioral control. The results are presented in Table 1 (see also Online Appendix A4). According to standard SEM goodness of fit statistics (West et al., 2012) the model fitted the data well (χ2 = 27.274, df = 9, p = 0.001; CFI = 0.999; RMSEA = 0.026; SRMR = 0.006). Attitudes predicted intentions, and the standardized coefficient (β = 0.795) indicated a strong effect. Thus, the more favorable people's attitudes toward getting vaccinated, the stronger their intentions. Subjective norms had a significant and negative but very weak effect on intentions (β = −0.094), which could indicate a suppression effect due to the high correlation between subjective norms and attitudes (r = 0.849).
Table 1.
SEM estimates predicting vaccination intention.
| Path coefficients predicting INT | Estimate | Std. Err. | z-value | P (>|z|) | Standardized estimate |
|---|---|---|---|---|---|
| ATT | 1.002 | 0.050 | 20.022 | 0.000 | 0.795 |
| SN | −0.133 | 0.046 | −2.880 | 0.004 | −0.094 |
| PBC |
−0.053 |
0.043 |
−1.212 |
0.226 |
−0.031 |
| Covariances/correlations among predictors |
Estimate |
Std. Err. |
z-value |
P (>|z|) |
Standardized estimate |
| ATT ↔ SN | 2.880 | 0.077 | 37.581 | 0.000 | 0.849 |
| ATT ↔ PBC | 2.210 | 0.084 | 26.326 | 0.000 | 0.796 |
| SN ↔ PBC | 1.710 | 0.074 | 23.090 | 0.000 | 0.690 |
Notes: n = 3507 (25 cases had missing values on all indicators), estimator = MLR, INT = intention, ATT = attitude, SN = subjective norm, PBC = perceived behavioral control.
In a second model (Model 2) we tested the hypothesized interaction effects between perceived behavioral control and attitudes as well as between perceived behavioral control and subjective norms. The model fitted the data well (χ2 = 255.015, df = 65, p = 0.000; CFI = 0.993; RMSEA = 0.043; SRMR = 0.032). However, we found no indication of interactions (see Online Appendix A8). Thus, for the current sample hypothesis H1 was supported, whereas hypotheses H2 to H5 were not. This shows that readiness to get vaccinated against COVID-19 was largely a matter of personal attitudes toward vaccination, and that perceived social pressures and barriers were of minor importance.
In the third model (Model 3), we retained attitudes as the only TPB predictor of vaccination intentions and entered the background factors as predictors of both attitudes and intentions (general conspiracy mindedness was omitted due to collinearity among predictors). In this way, we were able to test whether the background factors were indirect predictors of vaccination intentions, as postulated in the TPB, or had direct effects. The fit of the model was acceptable (χ2 = 5357.172, df = 701, p = 0.000; CFI = 0.931; RMSEA = 0.050; SRMR = 0.061). Consistent with the theory, attitudes were the only direct predictor of vaccination intentions exerting a strong effect (β = 0.709), and no other variable had a significant direct impact (Table 2 ). However, several background factors influenced attitudes toward getting a COVID-19 vaccination. Fear of COVID-19 (β = 0.262) and trust in science (β = 0.337) had positive and moderately sized effects on attitudes supporting our hypotheses H6 and H7. The resulting (standardized) indirect effects were positive and significant and moderate in size (β = 0.186 and β = 0.239, respectively; Online Appendix A9 shows the decomposition of the effects). By way of contrast, beliefs in a COVID-19 conspiracy (β = −0.143) and skepticism toward vaccines (β = −0.211) had weak and moderate negative effects on attitudes, empirically supporting our hypotheses H8 and H9. Their indirect effects on intention were significant and weak (β = −0.101 and β = −0.149, respectively). Older people had more positive attitudes than younger people with weak and moderate effects, respectively (age 30 to 59: β = 0.132, age 60 and above: β = 0.220, H13). Compared to females, males had more positive attitudes (with a weak effect of β = 0.144, H14). People with high levels of education had more positive attitudes than those with low education levels (with a very weak effect of β = 0.059, H15). Immigrants (H19) had slightly more negative attitudes than non-immigrants (with a very weak effect of β = −0.089). The indirect effects of some of these sociodemographic factors were statistically significant, small in size, and positive (age 30 to 59: β = 0.094, age 60 and above: β = 0.156, compared to individuals younger than 30; males: β = 0.102; high education: β = 0.042). The indirect effect of immigration background was significant, weak, and negative (β = −0.063). In sum, the results show that several background factors correlated, as predicted, with vaccination intentions and that these correlations were fully mediated by attitudes.
Table 2.
SEM estimates predicting intention and attitude.
| Path coefficients predicting INT | Estimate | Std. Err. | z-value | P (>|z|) | Standardized estimate |
|---|---|---|---|---|---|
| ATT | 0.895 | 0.032 | 28.358 | 0.000 | 0.709 |
| CCB | 0.062 | 0.039 | 1.603 | 0.109 | 0.030 |
| SKV | −0.015 | 0.042 | −0.368 | 0.713 | −0.009 |
| SKD | 0.026 | 0.048 | 0.534 | 0.593 | 0.012 |
| FCV | 0.020 | 0.032 | 0.644 | 0.519 | 0.013 |
| TPO | 0.014 | 0.031 | 0.458 | 0.647 | 0.011 |
| TSC | −0.065 | 0.056 | −1.164 | 0.244 | −0.035 |
| health | 0.013 | 0.043 | 0.306 | 0.759 | 0.005 |
| risk2a | −0.003 | 0.080 | −0.041 | 0.968 | −0.001 |
| risk3a | −0.142 | 0.115 | −1.227 | 0.220 | −0.058 |
| rel | −0.001 | 0.018 | −0.080 | 0.936 | −0.001 |
| pol | 0.009 | 0.017 | 0.521 | 0.602 | 0.007 |
| age2b | −0.043 | 0.089 | −0.477 | 0.633 | −0.017 |
| age3b | 0.087 | 0.116 | 0.748 | 0.455 | 0.036 |
| malec | −0.105 | 0.069 | −1.522 | 0.128 | −0.043 |
| edud | 0.024 | 0.087 | 0.270 | 0.787 | 0.010 |
| ince | 0.017 | 0.084 | 0.205 | 0.838 | 0.007 |
| immf | −0.041 | 0.093 | −0.442 | 0.658 | −0.017 |
| partg | −0.042 | 0.074 | −0.577 | 0.564 | −0.017 |
| kidsh |
0.024 |
0.082 |
0.297 |
0.766 |
0.010 |
| Path coefficients predicting ATT |
Estimate |
Std. Err. |
z-value |
P (>|z|) |
Standardized estimate |
| CCB | −0.232 | 0.034 | −6.803 | 0.000 | −0.143 |
| SKV | −0.292 | 0.037 | −7.861 | 0.000 | −0.211 |
| SKD | −0.045 | 0.036 | −1.227 | 0.220 | −0.026 |
| FCV | 0.334 | 0.027 | 12.199 | 0.000 | 0.262 |
| TPO | 0.016 | 0.022 | 0.747 | 0.455 | 0.015 |
| TSC | 0.503 | 0.047 | 10.667 | 0.000 | 0.337 |
| health | −0.032 | 0.033 | −0.969 | 0.333 | −0.015 |
| risk2a | 0.020 | 0.058 | 0.337 | 0.736 | 0.010 |
| risk3a | 0.122 | 0.086 | 1.428 | 0.153 | 0.063 |
| rel | −0.013 | 0.014 | −0.958 | 0.338 | −0.013 |
| pol | 0.017 | 0.014 | 1.200 | 0.230 | 0.017 |
| age2b | 0.255 | 0.070 | 3.653 | 0.000 | 0.132 |
| age3b | 0.425 | 0.088 | 4.834 | 0.000 | 0.220 |
| malec | 0.278 | 0.051 | 5.483 | 0.000 | 0.144 |
| edud | 0.113 | 0.056 | 2.020 | 0.043 | 0.059 |
| ince | 0.071 | 0.058 | 1.235 | 0.217 | 0.037 |
| immf | −0.171 | 0.067 | −2.574 | 0.010 | −0.089 |
| partg | −0.013 | 0.056 | −0.225 | 0.822 | −0.007 |
| kidsh | −0.116 | 0.061 | −1.908 | 0.056 | −0.060 |
Notes: n = 3110 (422 cases had missing values on predictors), estimator = MLR, INT = intention, ATT = attitude, CCB=COVID-19 conspiracy beliefs, SKV = skepticism toward vaccines, SKD = skepticism toward doctors, FCV = fear of COVID-19, TPO = trust in politics, TSC = trust in science, health = self-rated health, risk2 & risk3 = COVID-19 risk, rel = religiosity, pol = political orientation, age2 & age3 = age, male = gender, edu = education, inc = income, imm = immigration background; part = partnership status, kids = living with kids. Reference categories (see also Online Appendix A1): a low risk, b age <30, c female, d below tertiary, e ≤ 4000€, f no immigration background, g single/divorced/widowed, h no. Correlations among predictors are not shown (see Online Appendix A9). Standardized estimates for binary predictors are standardized with respect to the dependent variable only (“std.nox” in lavaan).
Model 3 (the most comprehensive model) was also tested with regard to statistical power (Moshagen and Erdfelder, 2016). First, we assessed the achieved power of an effect (post-hoc power analysis), i.e., the probability of correctly rejecting a model when it is actually wrong. We defined the effect in terms of the RMSEA fit statistic (Steiger, 1990), which is assumed to indicate a non-acceptable discrepancy between observed and estimated covariances if RMSEA >0.05. Given the effect, the sample size and complexity of Model 3 (N = 3110; df = 701), and an alpha error level of 0.05 the estimated power was >0.999. Thus, the probability to correctly rejecting an ill-fitting model is very high. Second, we assessed a critical value of the χ2 test statistic (compromise power analysis), which provides a decision rule about whether the estimated model is in line with the null hypothesis (i.e., perfect fit) or the alternative hypothesis (i.e., RMSEA >0.05). Given proportional alpha and beta error probabilities and the sample size and complexity of Model 3 the analysis returned a critical value of χ2 = 13964.40, which was above the observed value (χ2 = 5357.172). This suggests that the estimated model is in line with the null hypothesis of no (or negligible) discrepancy between observed and estimated covariances (for details see Online Appendix A11).
Finally, we specified four additional models to test how COVID-19 conspiracy beliefs, skepticism toward vaccines, fear of COVID-19, and trust in science are related to the socioeconomic and demographic factors, health variables, political orientation, and religiosity (see Online Appendix A12). COVID-19 conspiracy beliefs were prevalent among participants who believed that they were at moderate risk of suffering severe sickness from an infection (β = 0.103) as well as among religious individuals (β = 0.082) and those on the right of the political spectrum (β = 0.197), among people with an immigrant background (β = 0.147), and people living with children (β = 0.174). People of older age (age 30 to 59: β = −0.131, age 60 and above: β = −0.279), with a higher education (β = −0.304), and with higher income (β = −0.297) were less likely to endorse such beliefs. Skepticism toward vaccines was higher for religious people (β = 0.050), those on the right of the political spectrum (β = 0.185), people with an immigration background (β = 0.150), and people living with children (β = 0.112). People with higher education (β = −0.382) and those with a higher income (β = −0.261) were less skeptical of vaccines. Fear of COVID-19 was higher for people who believed that they were at medium or high risk of a severe course of the sickness (β = 0.306 and β = 0.543, respectively), religious people (β = 0.092), people with higher education (β = 0.205), and people living with a partner (β = 0.152). Fear was lower for people with better health (β = −0.151), those on the right of the political spectrum (β = −0.141), males (β = −0.091), and people living with children (β = −0.103). Trust in science was higher for people with better health (β = 0.071), people at medium risk of severe course of the sickness (β = 0.091), people in the oldest age group (β = 0.210), males (β = 0.198), and with higher education (β = 0.394) and income (β = 0.206). Trust was lower for those on the right of the political spectrum (β = −0.196) and people living with children (β = −0.152). Several robustness analyses are reported in the Online Appendix (A5-A7, A10).
5. Summary and discussion
Achieving a high rate of vaccination is deemed a key to successfully combat the COVID-19 pandemic. Efforts have been made in many countries to distribute vaccines against the virus to people at high risk of a severe or fatal course of the disease as well as to the rest of the population (Mullard, 2020; Sharma et al., 2021). However, high vaccination rates are not solely the result of availability, effectiveness, and safety of vaccines, but also of people's willingness to get vaccinated. Based on the theory of planned behavior, we assessed the factors that contribute to people's vaccination intentions with data from Germany that reflect the situation in the second half of April 2021 in which the vaccination campaign “had picked up speed”. Vaccination intentions were assumed to be a function of people's attitudes toward the vaccination, perceived social pressures to get vaccinated, and perceived barriers to vaccination. Moreover, background factors such as institutional trust, fear of COVID-19, conspiracy beliefs, denial of COVID-19, skepticism toward vaccines, health-status, religiosity, political orientation, and socioeconomic and demographic characteristics were hypothesized to influence vaccination intentions indirectly via attitudes, subjective norms, and/or perceived behavioral control.
The only direct predictor of vaccination intention was the attitude toward getting vaccinated and no interaction was found between attitudes and perceived behavioral control and between subjective norm and perceived behavioral control. These findings imply that the formation of an intention to get or not get vaccinated may largely be based on personal beliefs that performance of the behavior will result in positive or negative outcomes. This implication derives from the TPB's “expectancy-value-model of attitudes” (Fishbein, 1963, 1967; Fishbein and Ajzen, 1975, 2010), according to which a person's attitude toward a behavior is a function of readily accessible behavioral beliefs, i.e., of the perceived likelihood that performing the behavior will lead to certain valued outcomes and experiences. Specifically, the perceived likelihood of each anticipated outcome or experience is weighted (multiplied) by its subjective value, and the resulting products are summed (Fishbein and Ajzen, 2010, pp. 96–103). When the behavior is perceived to produce mostly positive outcomes and experiences, the attitude will be favorable and the likelihood of forming an intention to perform the behavior increases. When most behavioral beliefs are negative, however, the attitude will not be in favor of the behavior and the likelihood of forming an intention to perform the behavior decreases (Fishbein and Ajzen, 2010, pp. 203–205).
Contrary to our second hypothesis, subjective norms were found to make no significant contribution to the prediction of intentions to get vaccinated. This is somewhat surprising considering the important role often attributed to social media in shaping people's readiness to get vaccinated. However, it is conceivable that exposure to social media merely provides information (correct or misleading) on which people's attitudes are based. It is also possible, however, that in the case of a behavior that is of great personal significance, such as getting vaccinated, other people's wishes and behaviors decline in importance.
Perceived behavioral control also had no significant effect on intentions to get vaccinated and, contrary to our hypotheses IV and V, it did not moderate the effects of attitude or subjective norm on intentions (see also Hagger et al., 2021). However, recall that in this particular study all TPB-related questions were presented to participants with the request to assume that they can get an appointment for a vaccination quickly. In retrospect, these instructions may have led the respondents to discount any perceived barriers to vaccination and may thus have reduced the potential impact of perceived behavioral control.
Consistent with the TPB and our hypotheses, none of the background factors directly affected vaccination intentions. However, several factors had an indirect effect via their direct effects on attitudes toward getting vaccinated. We found that people who hold COVID-19 conspiracy beliefs and people who are skeptical toward vaccines were less favorably inclined toward getting vaccinated against COVID-19. Thus, conspiracy beliefs and vaccine skepticism have the potential to reduce vaccination readiness, especially in segments of society where these ideas are prevalent. The results indicate that this may be the case among people on the political right, immigrants, people with less education and lower income, younger people, and people with children in kindergarten or school. Conspiratorial ideas and opposition to vaccination have been promoted by parties and representatives of the far political right in Germany, which may have affected their followers. This may go along with a general tendency to resist governmental efforts to contain the pandemic (including the vaccination campaign), which can be observed in the so-called “Querdenker” movement that tends to be open to radical right-wing positions and science denialism (Nachtwey et al., 2020). Conspiracy beliefs and vaccination skepticism were also somewhat more common among people with an immigrant background (although this particular effect was very weak), presumably among those who have limited health care access due to a lack of knowledge of the health care system and language and cultural barriers (Crawshaw et al., 2021). Information deficits may also explain the effect of low education (and income). Moreover, younger people may be more skeptical of vaccines because their risk of serious symptoms is low. At the same time, they are strongly affected by the measures to contain the pandemic (contact restrictions, curfews, and school closures), increasing their risk of suffering from mental health problems (Batra et al., 2021; Meherali et al., 2021). The negative effects of parenthood may be explained by parents’ concerns about vaccine safety and the low risk of children to suffer severely from the disease. To date, the role of children and schools as drivers of the pandemic is controversial (Oh et al., 2021) and may lead parents to adopt a defensive stance regarding vaccination of their children.
The results also confirm that people who are more trusting in science and fear suffering from COVID-19 are in favor of getting the vaccination. People with higher education (and income) and of older age had more trust in science, and people identifying with the far political right were less trusting. In line with the argumentation on conspiracy beliefs and skepticism toward vaccines, we connect the lower trust in science with a right-wing political orientation. People with a higher level of education are more inclined to believe in science because of their educational experience, whereas older people may be more trusting because they are more likely to have experienced successful medical treatments with the passage of time. Finally, more highly educated people and those at a high risk of getting seriously ill are more concerned about COVID-19 and thus are more likely to have a positive attitude toward getting vaccinated.
Our findings outline several implications for both policy makers and health care providers (for an overview in the UK, see Michie et al., 2021). First, the effect of attitudes toward getting vaccinated on vaccination intentions suggests that people are particularly concerned with personal benefits of vaccination (as opposed to collective benefits). Thus, efforts to fight vaccination hesitancy should highlight protection from serious illness, hospitalization, death, and long-term health detriments (see also Ashworth et al., 2021; Freeman et al., 2021). Approaches that emphasize social norms to get vaccinated or the ease of obtaining the vaccine may turn out to be less effective, but this may change in later stages of the pandemic, for instance, if mandatory vaccination and sanctions for noncompliance are implemented.
Second, the effect of trust in science on attitudes towards getting vaccinated suggests that messaging should be scientifically credible, precise, and persuasive, and at the same time easy to understand. Especially in the context of public debates (e.g., in the media), scientists and active researchers should be (even more) involved to support knowledge transfer. However, the development and systematic tests of such theory-driven and evidence-based interventions are still underdeveloped (Ajzen and Schmidt, 2020; Michie et al., 2021).
5.1. Limitations
The current study is not without limitations. First, we were unable to control for unobserved confounding factors (e.g., personality traits, medical preconditions), because our data was cross-sectional. Thus, randomization (as in experiments) or elimination of stable confounding variables (as with panel data) was impossible. Second, it is impossible to empirically distinguish our models from equivalent models that may be estimated with the same data (MacCallum et al., 1993). Although the structure of our analytical models was based on established theoretical considerations and alternative models may contradict theory, many alternatives may exist that could equally well fit the data and result in different conclusions. In fact, causal inference (with cross-sectional data) may be problematic. For example, contrary to the assumed mechanism, unfavorable vaccination intentions may induce a selective search for information about negative consequences of vaccination and therefore influence attitudes (reversed causality). Third, our sample may be selective in terms of who was willing to participate (Schaurer and Weiβ, 2020) and with regard to the age of the respondents (adults aged 74 and above were not considered). These factors may limit the generalizability of our findings. Finally, it remains to be seen if intentions to get vaccinated will result in people carrying out the behavior once they have the opportunity. Even though it is theoretically plausible that intentions to get vaccinated are predictive of actual behavior, unforeseen events or other barriers to performing the behavior during the pandemic may weaken the effect of intention on behavior.
Credit author statement
Daniel Seddig: Conceptualization, Methodology, Validation, Formal analysis, Data curation, Writing – original draft Preparation, Visualization, Supervision, Project administration, Funding acquisition. Dina Maskileyson: Conceptualization, Methodology, Writing – original draft Preparation, Project administration, Funding acquisition. Eldad Davidov: Conceptualization, Methodology, Writing – original draft Preparation, Project administration, Funding acquisition. Icek Ajzen: Methodology, Writing – review & editing, Project administration. Peter Schmidt: Methodology, Writing – review & editing, Project administration.
Acknowledgements
The study was generously supported by a grant from the Fritz Thyssen Foundation, Germany. The authors would like to thank the Department of Psychosomatic Medicine and Psychotherapy, University Medical Center Mainz, Germany, for supplying the fees for open access publication. The authors would like to thank Leona Przechomski for helping prepare the manuscript. Eldad Davidov would like to thank the University of Zurich Research Priority Program Social Networks, Switzerland, for support during work on this study.
Biographies
Daniel Seddig is a senior researcher at the Institute of Sociology and Social Psychology at the University of Cologne and interims professor for empirical social research at the University of Passau (2021–2022). His research interests are social behaviors, attitudes, and norms regarding health, crime, immigration, and political orientations, and their association with cultural values, personal values, and socio-demographic variables across cultures and the life course. He is currently an Associate Editor for the European Journal of Criminology and the journal Survey Research Methods and member of the Coordination Group International Surveys of the GESIS Institute. https://orcid.org/0000-0003-1595-6948
Dina Maskileyson is a postdoctoral researcher at the Institute of Sociology and Social Psychology at the University of Cologne. As a sociologist studying health, she is interested in an in-depth understanding of the sources and consequences of health inequality within a comparative perspective between different population groups and across different countries. Her current research seeks to address four themes interrelated with health: immigration, socioeconomic inequality, population ageing, and gender. Her work involves both statistical analysis of large-sample secondary data and primary data collection involving experimental survey design. https://orcid.org/0000-0002-5687-8336
Eldad Davidov is professor at the Institute for Sociology and Social Psychology at the University of Cologne, Germany, and the Department of Sociology at the University of Zurich, Switzerland, and co-director of the University of Zurich Research Priority Program “Social Networks”. He was president of the European Survey Research Association (ESRA) between 2015 and 2017. His research interests are applications of structural equation modeling to survey data, especially in cross-cultural research. Applications include human values and attitudes toward immigrants and other minorities. https://orcid.org/0000-0002-3396-969X
Icek Ajzen is a social psychologist and professor emeritus at the University of Massachusetts Amherst (USA). He received his doctorate from the University of Illinois at Urbana–Champaign and is best known for his work on the attitude-behavior relation and the theory of planned behavior. Professor Ajzen has been ranked the most influential individual scientist within social psychology in terms of cumulative research impact. He received the Distinguished Scientist Award from the Society of Experimental Social Psychology in 2013 and the Distinguished Scientific Contribution Award from the Society for Personality and Social Psychology in 2016. His work been cited over 350,000 times and has been influential across such diverse fields as health psychology, consumer behavior, work and leisure, education, political behavior, and environmental psychology. https://orcid.org/0000-0001-8101-6300
Peter Schmidt, Ph.D. 1977 in Sociology and Philosophy of Science at the University of Mannheim. 1981. Professor for empirical research and Methodology at the Faculty for Cultural and Social Sciences, University of Giessen 1981–2008 on leave 1994–2000 as Program Director for societal Monitoring at GESIS Mannheim (formerly ZUMA). Since 2008 Professor emeritus and Member at the Centre for International Development and Environment (ZEU) at the University of Giessen and since 2020 Research Fellow and Principal Investigator at the department of psychosomatics at the University of Mainz. https://orcid.org/0000-0001-6954-8590
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2022.114981.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Agarwal V. A/H1N1 vaccine intentions in college students: an application of the theory of planned behavior. J. Am. Coll. Health. 2014;62(6):416–424. doi: 10.1080/07448481.2014.917650. [DOI] [PubMed] [Google Scholar]
- Ajzen I. In: Action Control: from Cognition to Behavior. Kuhl J., Beckmann J., editors. Springer; Heidelberg, Germany: 1985. From intentions to actions: a theory of planned behavior; pp. 11–39. [DOI] [Google Scholar]
- Ajzen I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 1991;50(2):179–211. doi: 10.1016/0749-5978(91)90020-T. [DOI] [Google Scholar]
- Ajzen I. In: Lange P.A.M., Kruglanski A.W., Higgins E.T., editors. vol. 1. Sage; London, UK: 2012. The theory of planned behavior; pp. 438–459. (Handbook of Theories of Social Psychology). [DOI] [Google Scholar]
- Ajzen I., Schmidt P. In: The Handbook of Behavior Change (Cambridge Handbooks in Psychology. Hagger M., Cameron L., Hamilton K., Hankonen N., Lintunen T., editors. Cambridge University Press; Cambridge: 2020. Changing behavior using the theory of planned behavior; pp. 17–31. [DOI] [Google Scholar]
- Al-Qerem W.A., Jarab A.S. COVID-19 vaccination acceptance and its associated factors among a Middle Eastern population. Front. Public Health. 2021;9:34. doi: 10.3389/fpubh.2021.632914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alabdulla M., Reagu S.M., Al‐Khal A., Elzain M., Jones R.M. COVID‐19 vaccine hesitancy and attitudes in Qatar: a national cross‐sectional survey of a migrant‐majority population. Influenza Respir. Virus.s. 2021;15(3):361–370. doi: 10.1111/irv.12847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Algan Y., Guriev S., Papaioannou E., Passari E. The European trust crisis and the rise of populism. Brookings Pap. Econ. Activ. 2017:309–382. doi: 10.1353/eca.2017.0015. [DOI] [Google Scholar]
- Allington D., McAndrew S., Moxham-Hall V., Duffy B. Coronavirus conspiracy suspicions, general vaccine attitudes, trust and coronavirus information source as predictors of vaccine hesitancy among UK residents during the COVID-19 pandemic. Psychol. Med. 2021:1–12. doi: 10.1017/S0033291721001434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashworth M., Thunström L., Cherry T.L., Newbold S.C., Finnoff D.C. Emphasize personal health benefits to boost COVID-19 vaccination rates. Proc. Natl. Acad. Sci. 2021;118(32) doi: 10.1073/pnas.2108225118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Freeman; New York, NY: 1997. Self-efficacy: The Exercise of Control. [Google Scholar]
- Batra K., Sharma M., Batra R., Singh T.P., Schvaneveldt N. Assessing the psychological impact of COVID-19 among college students: an evidence of 15 countries. Healthcare. 2021;9(2):222. doi: 10.3390/healthcare9020222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendau A., Plag J., Petzold M.B., Ströhle A. COVID-19 vaccine hesitancy and related fears and anxiety. Int. Immunopharm. 2021;97:107724. doi: 10.1016/j.intimp.2021.107724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertin P., Nera K., Delouvée S. Conspiracy beliefs, rejection of vaccination, and support for hydroxychloroquine: a conceptual replication-extension in the COVID-19 pandemic context. Front. Psychol. 2020;11:2471. doi: 10.3389/fpsyg.2020.565128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bollen K.A. John Wiley & Sons; New York, NY: 1989. Structural Equations with Latent Variables. [DOI] [Google Scholar]
- Bosnjak M., Ajzen I., Schmidt P. The theory of planned behavior: selected recent advances and applications. Eur. J. Psychol. 2020;16(3):352. doi: 10.5964/ejop.v16i3.3107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown T.A. second ed. Guilford Press; New York, NY: 2015. Confirmatory Factor Analysis for Applied Research. [Google Scholar]
- Byrne T., Patel P., Shrotri M., Beale S., Michie S., Butt J., et al. 2021. Trends, Patterns and Psychological Influences on COVID-19 Vaccination Intention: Findings from a Large Prospective Community Cohort Study in England and Wales (Virus Watch). medRxiv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen M., Li Y., Chen J., Wen Z., Feng F., Zou H., et al. An online survey of the attitude and willingness of Chinese adults to receive COVID-19 vaccination. Hum. Vaccines Immunother. 2021;17(7):2279–2288. doi: 10.1080/21645515.2020.1853449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu H., Liu S. Integrating health behavior theories to predict American's intention to receive a COVID-19 vaccine. Patient Educ. Counsel. 2021 doi: 10.1016/j.pec.2021.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crawshaw A., Deal A., Rustage K., Forster A., Campos-Matos I., Vandrevala T., et al. What must be done to tackle vaccine hesitancy and barriers to COVID-19 vaccination in migrants? J. Trav. Med. 2021;28(4) doi: 10.1093/jtm/taab048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das G., Ghosh S., Garg S., Ghosh S., Jana A., Samat R., et al. An overview of key potential therapeutic strategies for combat in the COVID-19 battle. RSC Adv. 2020;10(47):28243–28266. doi: 10.1039/d0ra05434h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Leeuw A., Valois P., Ajzen I., Schmidt P. Using the theory of planned behavior to identify key beliefs underlying pro-environmental behavior in high-school students: implications for educational interventions. J. Environ. Psychol. 2015;42:128–138. doi: 10.1016/j.jenvp.2015.03.005. [DOI] [Google Scholar]
- Diethelm P., McKee M. Denialism: what is it and how should scientists respond? Eur. J. Publ. Health. 2009;19(1):2–4. doi: 10.1093/eurpub/ckn139. [DOI] [PubMed] [Google Scholar]
- Dror A., Eisenbach N., Taiber S., Morozov N., Mizrachi M., Zigron A., et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur. J. Epidemiol. 2020;35(8):775–779. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federal Ministry of Health . 2021. Ordinance on the Entitlement to Vaccination against the SARS-CoV-2 Coronavirus.https://www.bundesgesundheitsministerium.de/fileadmin/Dateien/3_Downloads/C/Coronavirus/Verordnungen/CoronaImpfV_EN_080221.pdf Retrieved. [Google Scholar]
- Fishbein M. An investigation of the relationships between beliefs about an object and the attitude toward that object. Hum. Relat. 1963;16(3):233–239. doi: 10.1177/001872676301600302. [DOI] [Google Scholar]
- Fishbein M. Wiley; New York, NY: 1967. Readings in Attitude Theory and Measurement. [Google Scholar]
- Fishbein M., Ajzen I. Addison-Wesley; Reading, MA: 1975. Belief, Attitude, Intention, and Behavior: an Introduction to Theory and Research. [Google Scholar]
- Fishbein M., Ajzen I. Psychology Press; New York, NY: 2010. Predicting and Changing Behavior: the Reasoned Action Approach. [DOI] [Google Scholar]
- Fisher W.A., Kohut T., Salisbury C.M., Salvadori M.I. Understanding human papillomavirus vaccination intentions: comparative utility of the theory of reasoned action and the theory of planned behavior in vaccine target age women and men. J. Sex. Med. 2013;10(10):2455–2464. doi: 10.1111/jsm.12211. [DOI] [PubMed] [Google Scholar]
- Freeman D., Loe B., Yu L.M., Freeman J., Chadwick A., Vaccari C., Shanyinde M., Harris V., Waite F., Rosebrock L., Petit A., Vanderslott S., Lewandowsky S., Larkin M., Innocenti S., Pollard A., McShane H., Lambe S. Effects of different types of written vaccination information on COVID-19 vaccine hesitancy in the UK (OCEANS-III): a single-blind, parallel-group, randomised controlled trial. Lancet Public Health. 2021;6(6):e416–e427. doi: 10.1016/S2468-2667(21)00096-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fridman A., Gershon R., Gneezy A. COVID-19 and vaccine hesitancy: a longitudinal study. PLoS One. 2021;16(4) doi: 10.1371/journal.pone.0250123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fukuyama F. The Free Press; New York, NY: 1995. Trust: the Social Virtues and the Creation of Prosperity. [Google Scholar]
- German Federal Statistical Office (Destatis) 2021. Database of the Federal Statistical Office of Germany (GENESIS-Online)https://www-genesis.destatis.de/genesis/online Retrieved from. [Google Scholar]
- Giuntella O., Hyde K., Saccardo S., Sadoff S. Lifestyle and mental health disruptions during COVID-19. Proc. Natl. Acad. Sci. 2021;118(9) doi: 10.1073/pnas.2016632118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godin G., Kok G. The theory of planned behavior: a review of its applications to health-related behaviors. Am. J. Health Promot. 1996;11(2):87–98. doi: 10.4278/0890-1171-11.2.87. [DOI] [PubMed] [Google Scholar]
- Godin G., Sheeran P., Conner M., Bélanger-Gravel A., Gallani M., Nolin B. Social structure, social cognition, and physical activity: a test of four models. British. J. Health Psychol. 2010;15(1):79–95. doi: 10.1348/135910709x429901. [DOI] [PubMed] [Google Scholar]
- Graupensperger S., Abdallah D.A., Lee C.M. Social norms and vaccine uptake: college students’ COVID vaccination intentions, attitudes, and estimated peer norms and comparisons with influenza vaccine. Vaccine. 2021;39(15):2060–2067. doi: 10.1016/j.vaccine.2021.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green M.S., Abdullah R., Vered S., Nitzan D. A study of ethnic, gender and educational differences in attitudes toward COVID-19 vaccines in Israel–implications for vaccination implementation policies. Isr. J. Health Pol. Res. 2021;10(1):1–12. doi: 10.1186/s13584-021-00458-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guidry J.P., Laestadius L.I., Vraga E.K., Miller C.A., Perrin P.B., Burton C.W., et al. Willingness to get the COVID-19 vaccine with and without emergency use authorization. Am. J. Infect. Control. 2021;49(2):137–142. doi: 10.1016/j.ajic.2020.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagger M., Hamilton K. Effects of socio-structural variables in the theory of planned behavior: a mediation model in multiple samples and behaviors. Psychol. Health. 2021;36(3):307–333. doi: 10.1080/08870446.2020.1784420. [DOI] [PubMed] [Google Scholar]
- Hagger M.S., Cheung M.W.L., Ajzen I., Hamilton K. Perceived behavioral control moderating effects in the theory of planned behavior: a meta-analysis. Health Psychol. 2021 doi: 10.1037/hea0001153. [DOI] [PubMed] [Google Scholar]
- Hukkelberg S.S., Hagtvet K.A., Kovac V.B. Latent interaction effects in the theory of planned behaviour applied to quitting smoking. Br. J. Health Psychol. 2014;19(1):83–100. doi: 10.1111/bjhp.12034. [DOI] [PubMed] [Google Scholar]
- Janssens U., Kluge S., Marx G., Hermes C., Salzberger B., Karagiannidis C. Einstellung zur Impfung gegen SARS-CoV-2. Med. Klin. Intensivmed. Notfallmed. 2021;116(5):421–430. doi: 10.1007/s00063-021-00821-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jennings W., Stoker G., Willis H., Valgardsson V., Gaskell J., Devine D., et al. 2021. Lack of Trust and Social Media Echo Chambers Predict COVID-19 Vaccine Hesitancy. medRxiv. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen E.A., Pfleger A., Herbig L., Wagoner B., Lorenz L., Watzlawik M. What drives belief in vaccination conspiracy theories in Germany? Front. Commun. 2021;6:105. doi: 10.3389/fcomm.2021.678335. [DOI] [Google Scholar]
- Jorgensen T.D., Pornprasertmanit S., Schoemann A.M., Rosseel Y. 2021. semTools: Useful Tools for Structural Equation Modeling.https://CRAN.R-project.org/package=semTools R package version 0.5-5. Retrieved from. [Google Scholar]
- Karlsson L.C., Soveri A., Lewandowsky S., Karlsson L., Karlsson H., Nolvi S., et al. Fearing the disease or the vaccine: the case of COVID-19. Pers. Indiv. Differ. 2021;172:110590. doi: 10.1016/j.paid.2020.110590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashte S., Gulbake A., El-Amin S., III, Gupta A. COVID-19 vaccines: rapid development, implications, challenges and future prospects. Hum. Cell. 2021;34(3):711–733. doi: 10.1007/s13577-021-00512-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I., Kennedy B.P., Lochner K., Prothrow-Stith D. Social capital, income inequality and mortality. Am. J. Publ. Health. 1997;87(9):1491–1498. doi: 10.2105/AJPH.87.9.1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khodyakov D. Trust as a process. Sociology. 2007;41(1):115–132. doi: 10.1177/0038038507072285. [DOI] [Google Scholar]
- Kourlaba G., Kourkouni E., Maistreli S., Tsopela C.G., Molocha N.M., Triantafyllou C., et al. Willingness of Greek general population to get a COVID-19 vaccine. Glob. Health Res. Pol. 2021;6(1):1–10. doi: 10.1186/s41256-021-00188-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreps S., Dasgupta N., Brownstein J.S., Hswen Y., Kriner D.L. Public attitudes toward COVID-19 vaccination: the role of vaccine attributes, incentives, and misinformation. npj Vaccines. 2021;6(1):1–7. doi: 10.1016/j.paid.2020.110590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Barbera F., Ajzen I. Control interactions in the theory of planned behavior: rethinking the role of subjective norm. Eur. J. Psychol. 2020;16(3):401–417. doi: 10.5964/ejop.v16i3.2056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin C., Dayton L.A., Yi G., Konstantopoulos A., Park J., Maulsby C., Kong X. COVID-19 vaccine intentions in the United States, a social-ecological framework. Vaccine. 2021;39(16):2288–2294. doi: 10.1016/j.vaccine.2021.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin C.A., Dayton L., Yi G., Colon B., Kong X. Mask usage, social distancing, racial, and gender correlates of COVID-19 vaccine intentions among adults in the US. PLoS One. 2021;16(2) doi: 10.1371/journal.pone.0246970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latkin C.A., Dayton L., Yi G., Konstantopoulos A., Boodram B. Trust in a COVID-19 vaccine in the US: a social-ecological perspective. Soc. Sci. Med. 2021;270:113684. doi: 10.1016/j.socscimed.2021.113684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewandowsky S., Gignac G.E., Oberauer K. The role of conspiracist ideation and worldviews in predicting rejection of science. PLoS One. 2013;8(10) doi: 10.1371/journal.pone.0075637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindström M. Social capital, political trust and purchase of illegal liquor: a population-based study in southern Sweden. Health Pol. 2008;86(2–3):266–275. doi: 10.1016/j.healthpol.2007.11.001. [DOI] [PubMed] [Google Scholar]
- Link B.G., Phelan J. Social conditions as fundamental causes of disease. J. Health Soc. Behav. 1995;35:80–94. doi: 10.2307/2626958. [DOI] [PubMed] [Google Scholar]
- Little T.D., Bovaird J.A., Widaman K.F. On the merits of orthogonalizing powered and product terms: implications for modeling interactions among latent variables. Struct. Equ. Model. 2006;13(4):497–519. doi: 10.1207/s15328007sem1304_1. [DOI] [Google Scholar]
- MacCallum R.C., Wegener D.T., Uchino B.N., Fabrigar L.R. The problem of equivalent models in applications of covariance structure analysis. Psychol. Bull. 1993;114(1):185–199. doi: 10.1037/0033-2909.114.1.185. [DOI] [PubMed] [Google Scholar]
- Machida M., Nakamura I., Kojima T., Saito R., Nakaya T., Hanibuchi T., et al. Acceptance of a COVID-19 vaccine in Japan during the COVID-19 pandemic. Vaccines. 2021;9(3):210. doi: 10.3390/vaccines9030210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malesza M., Wittmann E. Acceptance and intake of COVID-19 vaccines among older Germans. J. Clin. Med. 2021;10(7):1388. doi: 10.3390/jcm10071388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marien S., Hooghe M. Does political trust matter? An empirical investigation into the relation between political trust and support for law compliance. Eur. J. Polit. Res. 2011;50(2):267–291. doi: 10.1111/j.1475-6765.2010.01930.x. [DOI] [Google Scholar]
- McDonald R.P. Lawrence Erlbaum Associates Publishers; 1999. Test Theory: A Unified Treatment. [DOI] [Google Scholar]
- McEachan R.R.C., Conner M., Taylor N.J., Lawton R.J. Prospective prediction of health-related behaviours with the theory of planned behaviour: a meta-analysis. Health Psychol. Rev. 2011;5(2):97–144. doi: 10.1080/17437199.2010.521684. [DOI] [Google Scholar]
- McHoskey J.W. Case closed? On the John F. Kennedy assassination: biased assimilation of evidence and attitude polarization. Basic Appl. Soc. Psychol. 1995;17(3):395–409. doi: 10.1207/s15324834basp1703_7. [DOI] [Google Scholar]
- McKinley L., McAnally K., Moyers S., Hagger M. In: Handbook of Global Health. Haring R., Kickbusch I., Ganten D., Moeti M., editors. 2020. Behavioral health theories, equity, and disparities in global health; pp. 1–23. [DOI] [Google Scholar]
- Meade A.W., Craig S.B. Identifying careless responses in survey data. Psychol. Methods. 2012;17(3):437–455. doi: 10.1037/a0028085. [DOI] [PubMed] [Google Scholar]
- Meherali S., Punjani N., Louie-Poon S., Abdul Rahim K., Das J.K., Salam R.A., Lassi Z.S. Mental health of children and adolescents amidst COVID-19 and past pandemics: a rapid systematic review. Int. J. Environ. Res. Publ. Health. 2021;18(7):3432. doi: 10.3390/ijerph18073432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michie S., West R., Pidgeon N., Reicher S., Amlôt R., Bear L. Staying ‘Covid-safe’: proposals for embedding behaviours that protect against Covid-19 transmission in the UK. Br. J. Health Psychol. 2021 doi: 10.1111/bjhp.12557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mo P.K.H., Luo S., Wang S., Zhao J., Zhang G., Li L., et al. Intention to receive the COVID-19 vaccination in China: application of the diffusion of innovations theory and the moderating role of openness to experience. Vaccines. 2021;9(2):129. doi: 10.3390/vaccines9020129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moshagen M., Erdfelder E. A new strategy for testing structural equation models. Struct. Equ. Model. 2016;23:54–60. doi: 10.1080/10705511.2014.950896. [DOI] [Google Scholar]
- Mullard A. How COVID vaccines are being divvied up around the world. Nature. 2020 doi: 10.1038/d41586-020-03370-6. [DOI] [PubMed] [Google Scholar]
- Nachtwey O., Schäfer R., Frei N. 2020. Politische Soziologie der Corona-Proteste. December 20. [DOI] [Google Scholar]
- Neumann-Böhme S., Varghese N.E., Sabat I., Barros P.P., Brouwer W., van Exel J., et al. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur. J. Health Econ. 2020;21(7):977–982. doi: 10.1007/s10198-020-01208-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oh D.-Y., Böttcher S., Kröger S., von Kleist M. SARS-CoV-2-Übertragungswege und Implikationen für den Selbst- und Fremdschutz. Bundesgesundheitsblatt - Gesundheitsforsch. - Gesundheitsschutz. 2021 doi: 10.1007/s00103-021-03389-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandey S., Pande V., Sati D., Upreti S., Samant M. Vaccination strategies to combat novel corona virus SARS-CoV-2. Life Sci. 2020;256:117956. doi: 10.1016/j.lfs.2020.117956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul E., Steptoe A., Fancourt D. Attitudes towards vaccines and intention to vaccinate against COVID-19: implications for public health communications. Lancet Reg. Health Eur. 2021;1:100012. doi: 10.1016/j.lanepe.2020.100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peretti-Watel P., Raude J., Sagaon-Teyssier L., Constant A., Verger P., Beck F. Attitudes toward vaccination and the H1N1 vaccine: poor people's unfounded fears or legitimate concerns of the elite? Soc. Sci. Med. 2014;109:10–18. doi: 10.1016/j.socscimed.2014.02.035. [DOI] [PubMed] [Google Scholar]
- Petravić L., Arh R., Gabrovec T., Jazbec L., Rupčić N., Starešinič N., et al. Factors affecting attitudes towards COVID-19 vaccination: an online survey in Slovenia. Vaccines. 2021;9(3):247. doi: 10.3390/vaccines9030247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piurko Y., Schwartz S., Davidov E. Basic personal values and the meaning of left-right political orientations in 20 countries. Polit. Psychol. 2011;32(4):537–561. doi: 10.1111/j.1467-9221.2011.00828.x. [DOI] [Google Scholar]
- Prislin R., Dyer J.A., Blakely C.H., Johnson C.D. Immunization status and sociodemographic characteristics: the mediating role of beliefs, attitudes, and perceived control. Am. J. Publ. Health. 1998;88(12):1821–1826. doi: 10.2105/AJPH.88.12.1821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putnam R.D., Leonardi R., Nanetti R.Y. Princeton University Press; Princeton, NJ: 1993. Making Democracy Work: Civic Traditions in Modern Italy. [Google Scholar]
- Quadros S., Garg S., Ranjan R., Vijayasarathi G., Mamun M. Fear of COVID 19 infection across different cohorts: a scoping review. Front. Psychiatr. 2021;12 doi: 10.3389/fpsyt.2021.708430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2019. R: A Language and Environment for Statistical Computing.https://www.R-project.org/ [Google Scholar]
- Revelle W. Northwestern University; Evanston, Illinois: 2021. Psych: Procedures for Psychological, Psychometric, and Personality Research.https://CRAN.R-project.org/package=psych R package version 2.1.6. [Google Scholar]
- Robertson E., Reeve K.S., Niedzwiedz C.L., Moore J., Blake M., Green M., et al. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain Behav. Immun. 2021;94:41–50. doi: 10.1016/j.bbi.2021.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez-Hidalgo A.J., Pantaleón Y., Dios I., Falla D. Fear of COVID-19, stress, and anxiety in university undergraduate students: a predictive model for depression. Front. Psychol. 2020;11:3041. doi: 10.3389/fpsyg.2020.591797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosseel Y. lavaan: an R package for structural equation modeling. J. Stat. Software. 2012;48(2):1–36. doi: 10.18637/jss.v048.i02. [DOI] [Google Scholar]
- Ruiz J.B., Bell R.A. Predictors of intention to vaccinate against COVID-19: results of a nationwide survey. Vaccine. 2021;39(7):1080–1086. doi: 10.1016/j.vaccine.2021.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallam M. COVID-19 vaccine hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines. 2021;9(2):160. doi: 10.3390/vaccines9020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallam M., Dababseh D., Eid H., Al-Mahzoum K., Al-Haidar A., Taim D., et al. High rates of COVID-19 vaccine hesitancy and its association with conspiracy beliefs: a study in Jordan and Kuwait among other Arab countries. Vaccines. 2021;9(1):42. doi: 10.3390/vaccines9010042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salmon D.A., Dudley M.Z., Brewer J., Kan L., Gerber J.E., Budigan H., et al. COVID-19 vaccination attitudes, values and intentions among United States adults prior to emergency use authorization. Vaccine. 2021;39(19):2698–2711. doi: 10.1016/j.vaccine.2021.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarwar Z., Ahmad T., Kakar S. Potential approaches to combat COVID-19: a mini-review. Mol. Biol. Rep. 2020;47(12):9939–9949. doi: 10.1007/s11033-020-05988-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satorra A., Bentler P.M. In: Latent Variables Analysis: Applications for Developmental Research. von Eye A., Clogg C.C., editors. Sage; Thousand Oaks, CA: 1994. Corrections to test statistics and standard errors in covariance structure analysis; pp. 399–419. [DOI] [Google Scholar]
- Schaurer I., Weiß B. Investigating selection bias of online surveys on coronavirus-related behavioral outcomes. Surv. Res. Method. 2020;14(2):103–108. doi: 10.18148/srm/2020.v14i2.7751. [DOI] [Google Scholar]
- Sharma K., Koirala A., Nicolopoulos K., Chiu C., Wood N., Britton P. Vaccines for COVID-19: where do we stand in 2021? Paediatr. Respir. Rev. 2021;39:22–31. doi: 10.1016/j.prrv.2021.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman S.M., Sim J., Cutts M., Dasch H., Amlot R., Rubin J., et al. medRxiv; 2021. COVID-19 Vaccination Acceptability in the UK at the Start of the Vaccination Programme: a Nationally Representative Cross-Sectional Survey (CoVAccS Wave 2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shmueli L. Predicting intention to receive COVID-19 vaccine among the general population using the health belief model and the theory of planned behavior model. BMC Publ. Health. 2021;21(1):1–13. doi: 10.1101/2021.04.06.21254973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soares P., Rocha J.V., Moniz M., Gama A., Laires P.A., Pedro A.R., et al. Factors associated with COVID-19 vaccine hesitancy. Vaccines. 2021;9(3):300. doi: 10.3390/vaccines9030300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steiger J.H. Structural model evaluation and modification: an interval estimation approach. Multivariate Behav. Res. 1990;25(2):173–180. doi: 10.1207/s15327906mbr2502_4. [DOI] [PubMed] [Google Scholar]
- Steinmetz H., Davidov E., Schmidt P. Three approaches to estimate latent interaction effects: intention and perceived behavioral control in the theory of planned behavior. Methodol. Innovat. Online. 2011;6(1):95–110. doi: 10.4256/mio.2010.0030. [DOI] [Google Scholar]
- Steinmetz H., Knappstein M., Ajzen I., Schmidt P., Kabst R. How effective are behavior change interventions based on the theory of planned behavior? Z. für Psychol. 2016;224(3):216–233. doi: 10.1027/2151-2604/a000255. [DOI] [Google Scholar]
- Swami V., Furnham A. In: Power, Politics, and Paranoia: Why People Are Suspicious of Their Leaders. Prooijen J., Lange P., editors. Cambridge University Press; Cambridge: 2014. Political paranoia and conspiracy theories; pp. 218–236. [DOI] [Google Scholar]
- Thaker J. The persistence of vaccine hesitancy: COVID-19 vaccination intention in New Zealand. J. Health Commun. 2021;26(2):104–111. doi: 10.1080/10810730.2021.1899346. [DOI] [PubMed] [Google Scholar]
- Troiano G., Nardi A. Vaccine hesitancy in the era of COVID-19. Publ. Health. 2021;194:245–251. doi: 10.1016/j.puhe.2021.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyler T.R. Princeton University Press; Princeton. Princeton, NJ: 2006. Why People Obey the Law. [Google Scholar]
- Van Bavel J.J.V., Baicker K., Boggio P.S., Capraro V., Cichocka A., Cikara M., Crockett M.J., Crum A.J., Douglas K.M., Druckman J.N., Drury J., Dube O., Ellemers N., Finkel E.J., Fowler J.H., Gelfand M., Han S., Haslam S.A., Jetten J.…Willer R. Using social and behavioural science to support COVID-19 pandemic response. Nat. Human Behav. 2020;4(5):460–471. doi: 10.1038/s41562-020-0884-z. [DOI] [PubMed] [Google Scholar]
- Ward J., Raude J. Understanding influenza vaccination behaviors: a comprehensive sociocultural framework. Expet Rev. Vaccine. 2014;13(1):17–29. doi: 10.1586/14760584.2014.863156. [DOI] [PubMed] [Google Scholar]
- Washburn A.N., Skitka L.J. Science denial across the political divide: liberals and conservatives are similarly motivated to deny attitude-inconsistent science. Soc. Psychol. Personal. Sci. 2018;9(8):972–980. doi: 10.1177/1948550617731500. [DOI] [Google Scholar]
- West S.G., Taylor A.B., Wu W. In: Handbook of Structural Equation Modeling. Hoyle R.H., editor. The Guilford Press; New York, NY: 2012. Model fit and model selection in structural equation modeling; pp. 209–231. [Google Scholar]
- Wilkinson R.G., Pickett K.E. Income inequality and health: a review and explanation of the evidence. Soc. Sci. Med. 2006;62(7):1768–1784. doi: 10.1016/j.socscimed.2005.08.036. [DOI] [PubMed] [Google Scholar]
- Winkelnkemper P., Ajzen I., Schmidt P. 2018. The Theory of Planned Behavior: A Meta-Analysis and Structural Equation Modeling. (Unpublished manuscript. [Google Scholar]
- Winston C.A., Wortley P.M., Lees K.A. Factors associated with vaccination of medicare beneficiaries in five U.S. Communities: results from the racial and ethnic adult disparities in immunization initiative survey, 2003. J. Am. Geriatr. Soc. 2006;54(2):303–310. doi: 10.1111/j.1532-5415.2005.00585.x. [DOI] [PubMed] [Google Scholar]
- Wojcik A., Cislak A., Schmidt P. ‘The left is right’: left and right political orientation across Eastern and Western Europe. Soc. Sci. J. 2021;1–17 doi: 10.1080/03623319.2021.1986320. [DOI] [Google Scholar]
- Wolff K. COVID-19 vaccination intentions: the theory of planned behavior, optimistic bias, and anticipated regret. Front. Psychol. 2021;12:648289. doi: 10.3389/fpsyg.2021.648289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan K.-H., Bentler P.M. Three likelihood-based methods for mean and covariance structure analysis with nonnormal missing data. Socio. Methodol. 2000;30(1):165–200. doi: 10.1111/0081-1750.00078. [DOI] [Google Scholar]
- Yzer M., van den Putte B. Control perceptions moderate attitudinal and normative effects on intention to quit smoking. Psychol. Addict. Behav. 2014;28(4):1153–1161. doi: 10.1037/a0037924. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.