Abstract
Purpose of Review
Climate change has manifested itself in multiple environmental hazards to human health. Older adults and those living with cardiovascular diseases are particularly susceptible to poor outcomes due to unique social, economic, and physiologic vulnerabilities. This review aims to summarize those vulnerabilities and the resultant impacts of climate-mediated disasters on the heart health of the aging population.
Recent Findings
Analyses incorporating a wide variety of environmental data sources have identified increases in cardiovascular risk factors, hospitalizations, and mortality from intensified air pollution, wildfires, heat waves, extreme weather events, rising sea levels, and pandemic disease. Older adults, especially those of low socioeconomic status or belonging to ethnic minority groups, bear a disproportionate health burden from these hazards.
Summary
The worldwide trends responsible for global warming continue to worsen climate change–mediated natural disasters. As such, additional investigation will be necessary to develop personal and policy-level interventions to protect the cardiovascular wellbeing of our aging population.
Keywords: Environmental health, Climate change, Aging, Cardiovascular disease
Introduction
Our modern era, beginning with the Third Industrial Revolution in the closing decades of the twentieth century, has been characterized by a global expansion of economic development and trade that has reached even the most remote corners of the world [1, 2]. Although the resultant demographic transition has been experienced by most societies as an impressive increase in life expectancy, it has also led to a surge in cardiovascular disease burden coupled with an acceleration of climate change-mediated environmental hazards [3–6, 7•, 8–10].
As of 2019, 703 million people in the world were over 65 years of age, and that number is projected to grow to 1.5 billion, or one in six people globally, by 2050 [11]. This phenomenon has taken place not just in rich nations but also in most low- and middle-income countries upon the background of an atherogenic, obesogenic milieu typified by the proliferation of cheap processed foods high in salt, sugar, and saturated fats; increased white-collar work and urban living leading to reduced physical activity; and higher per capita income incentivizing maladaptive behavioral risk factors such as tobacco and alcohol consumption [12–15]. It is thus no surprise that global cardiovascular disease (CVD) prevalence has nearly doubled from 271 to 523 million cases between 1990 and 2019, with the majority of this burden shouldered by people over 60 years old [16]. Meanwhile, Earth’s average surface temperature has risen 1.2 °C (approximately 2.2°F) in the past century due to man-made sources of greenhouse gases [17]. This global warming has not only accelerated the unpredictability of cyclic worldwide climate events like El Niño, but has also increased the frequency and severity of seasonal regional weather phenomena such as extreme heat waves, flash floods, and hurricanes [17, 18].
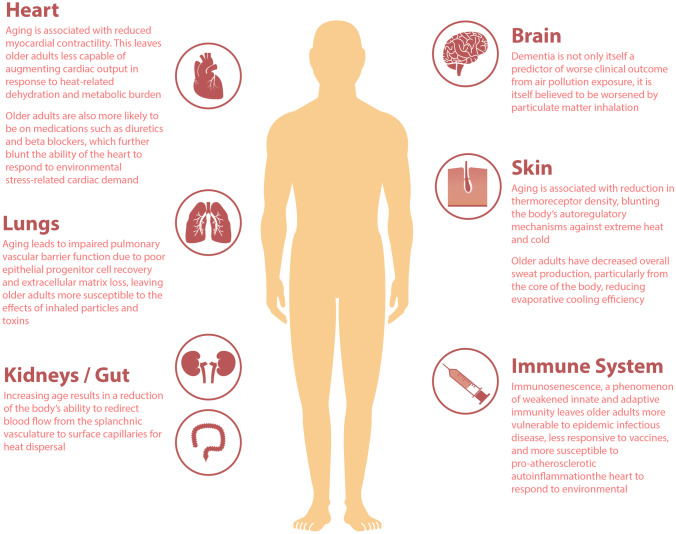
The growing global population of older adults finds itself particularly vulnerable to these climate consequences, as was tragically demonstrated in 2005 when nearly half of the 971 deaths from Hurricane Katrina in the USA befell individuals over the age of 75 [19]. Aside from the immediate casualties of the physical devastation imposed by these events, however, this group of people also experience a greater proportion of the health impacts of climate change, particularly CVD complications (Table 1). For example, nearly one in ten of the aforementioned Katrina mortalities was attributable to cardiovascular causes [19]. This surprising finding is due to a number of reasons, including both medical and societal factors: Older individuals have greater rates of pre-existing CVD and risk factors such as coronary artery disease, heart failure, stroke, obesity, and diabetes, leaving them at greater risk of decompensation from these conditions [20–22]. Additionally, aging is associated with changes in circulatory physiology, leaving older adults less able to adapt to sudden changes in their surroundings (Fig. 1). These include the inability to rapidly augment cardiac output in response to environmental stresses such as high temperatures and dehydration, vascular dysfunction leading to more sluggish heat dispersal at surface capillaries, and diminished capacity to redirect central blood stores to peripheral organs during sudden fluid loss [23]. Furthermore, frailty, a well-known syndrome of aging defined as a lack of physiologic reserve, is not only hypothesized to be accelerated by environmental pollutants, but is also itself an independent determinant of poor health outcomes from both heart disease as well as response to noxious ambient exposures [24–27]. Lastly, the reduced mobility of older people, a result of both physical and cognitive limitations and greater social isolation, makes them less able (and sometimes, less willing) to evacuate in a timely manner during natural disasters, leaving them to experience the worst direct and indirect effects of these climate catastrophes [28–30].
Table 1.
Select environmental manifestations of climate change and their impacts on the cardiovascular health of older adults
| Phenomenon | Cardiovascular impacts | Impacts and vulnerabilities relevant to older adults |
|---|---|---|
| Air pollution and wildfires | Climate change worsens ground-level air pollution by reducing air circulation, while increasing the frequency and severity of wildfires | Older adults have both higher underlying prevalence of cardiovascular conditions as well as reduced pulmonary vascular barrier functions, increasing their vulnerability to inhaled toxins |
| Particulate matter and ozone have both been tied to exacerbations of underlying cardiac conditions as well as chronic atherosclerotic and metabolic disease | Air conditioners can mitigate much of the harmful effects of airborne pollutants, but are less likely to be used by older adults, even when available | |
| Heat waves | Extreme heat not only leads to dehydration, it also stresses the myocardium with increased cardiac output requirements for skin-level circulatory heat dispersal | The majority of temperature-related deaths during heat waves are due to cardiovascular stress in older adults |
| Older adults are more likely to be on medications such as diuretics for heart failure and chronic kidney disease, reducing their body’s fluid volume reserve | ||
| Extreme weather events and natural disasters | Natural disasters, including hurricanes and blizzards, are associated with stress-related acute coronary events | Older adults often lack the physical and social mobility to evacuate in a timely manner from natural disasters |
| Widespread physical devastation can disrupt cardiovascular care infrastructure such as pharmacies, dialysis/infusion centers, and catheterization laboratories | The reduced circulatory reserve of older adults amplifies their susceptibility to the myocardial and metabolic demands imposed by physical activity in cold weather conditions and snow | |
| Pandemic and epidemic diseases | Global warming has increased the risk of zoonotic infectious disease transmission by increasing vector species’ habitat ranges, while exacerbating seasonal infectious disease epidemics such as influenza | Aging is associated with immunosenescence, which not only lowers resistance to infections, but also reduces vaccine effectiveness and induces pro-atherosclerotic autoinflammation |
| Pandemic disease disrupts cardiovascular care systems by delaying interventional procedures and diagnostic tests |
CVD cardiovascular disease
Fig. 1.
Aging-associated physiological changes predisposing older adults to harm from climate change–mediated phenomena
Given the ongoing nature of global warming and economic globalization, it is unlikely that we will see a reversal in the above trends [3, 17, 18]. As such, policymakers, researchers, and clinicians should pay greater attention to the unique cardiovascular risks posed by climate change to our aging population. Thus, in this review, we will attempt to summarize the major manifestations of our unstable planet on the heart health of our elders, while briefly offering some suggestions for how key stakeholders can begin to address these challenges.
Air Pollution and Wildfires
Air pollution is responsible for 6.7 million global deaths each year, making it the greatest environmental determinant of human morbidity and mortality [31–33]. Half of these deaths are from CVD and over half are in people over the age of 65 years [31, 32]. Airborne environmental exposures can be classified as either chronic (from both outdoor and indoor ambient sources) or acute (from singular personal and population-level exposures). Due to the immense number of sources of air pollution, there are thousands of distinct inhalable compounds that can be found in poor air. Briefly, the solid components are classified by particulate matter under 10 μm in diameter (PM10), 2.5 μm in diameter (PM2.5), and < 0.1 μm in diameter (ultrafine particles) [34]. These contaminants are often measured in conjunction with the most common gaseous pollutants, which include sulfur dioxide (SO2), carbon monoxide (CO), nitrogen dioxide (NO2), and ozone (O3). Encounters with all of these substances have been reported to affect human CVD outcomes to varying degrees. Short-term inhalation injury has been tied to escalations in cardiovascular hospitalization rates for acute complications such as myocardial infarction, stroke, and heart failure exacerbations [34, 35]. Simultaneously, long-term airborne exposures have been correlated with the progression of chronic heart diseases like coronary atherosclerosis and cardiometabolic risk factors such as hypertension and diabetes [33–36]. The pathophysiologic dynamics governing these phenomena differ considerably depending on the toxin combination, but they are believed to be complex processes involving varying degrees of autonomic imbalance, endothelial dysfunction, systemic inflammation, hypothalamus–pituitary–adrenal axis instability, and prothrombotic pathway activations [34].
Climate change has been linked to worsened air quality through several mechanisms. On the most global level, increased worldwide temperatures are predicted to lead to reduced wind speed and slower air circulation, concentrating existing urban air pollution locally [37, 38]. Next, it is believed that global warming has contributed to elevated ground-level ozone levels, which have been noted to interact with PM2.5 to worsen cardiovascular health status and mortality [31, 39–43]. Additionally, warmer weather and greater rainfall in certain regions have led to increased airborne pollen and mold spore counts, which have been linked to surges in emergency room visits for myocardial infarctions and strokes, as well as all-cause cardiovascular mortality [44–47].
The aging process is associated with impaired pulmonary vascular epithelial barrier function, likely a multifactorial process that includes reduced regenerative capacity of progenitor epithelial cells and poorer extracellular matrix recovery from acute inflammatory insults [48, 49]. The result is that older adults are less capable of protecting the air-blood barrier and are thus more susceptible to inhaled toxins. As such, it is no surprise that longitudinal ecological studies of both acute and chronic exposures to a variety of inhaled airborne pollutants have consistently found an elevation in cardiovascular events and mortality specifically among older individuals [50–56]. Furthermore, frailty and dementia, conditions of physiological and cognitive decline that accompany aging, are not only themselves connected to poor cardiovascular outcome from air pollution exposure, but are believed to themselves be worsened by airborne particulate matter inhalation [24, 26, 57–60].
Most noticeably, however, climate change has been linked to an acceleration in the frequency, intensity, and duration of seasonal extreme weather event–related deteriorations in air quality [17, 18, 61]. These include wildfires and dust storms, which can rapidly raise PM2.5 levels by orders of magnitude for hundreds of miles about their epicenters [10, 17, 18, 61]. Statewide investigations of wildfire smoke plume exposure in California have shown that adults 65 years of age and older have over twofold higher odds of suffering a cardiac arrest and 15% higher risk of finding themselves in the emergency room from a wide array of cardiovascular complications [62•, 63]. Unfortunately, older people often lack the mobility, transportation resources, and technology proficiency to rapidly evacuate from natural disasters such as wildfires [28, 29, 64, 65]. This is because they are more likely to suffer from disability or dementia, or reside in institutional settings such as nursing homes. That said, independently living elders are also more likely to live alone and less likely to be able to drive themselves [3, 29, 66]. Furthermore, even when older adults have in-home air conditioning, which can be used to help filter airborne particulate matter and mitigate some of its health risks, they are less likely to use it, frequently citing financial considerations as barriers to their use [67, 68]. Unfortunately, demographic trends do not favor a shift away from these concerns, as US census–based investigations suggest that aging populations may disproportionately reside in regions at highest risk of wildfire [69].
Heat Waves
Similarly to its effect on wildfires, global warming has worsened the severity, frequency, and duration of heat wave events, with multiple continents recording their highest ever temperatures in the past decade [17, 18]. Heat waves directly claim thousands of lives each year, with nearly two thousand lost due to heat-related causes annually in the USA alone, making them deadlier than hurricanes, floods, blizzards, and tornadoes [70–73]. Older adults are by far the most vulnerable group to extreme heat events, as the highest percentage of heat wave-attributable mortalities are in individuals over the age of 65 years [70, 72, 74, 75]. Tragically illustrative of this example was a historic heat wave that struck continental Europe in 2003, killing 30,000 people [23]. The vast majority of the fatalities were in those over 75 years of age [76]. Again, the physical and socioeconomic limitations to the mobility of older adults prevent them from leaving regions of high heat in a prompt manner, relocating to air-conditioned spaces, or using air conditioning even when available [28, 29, 64–68]. The growing proportion of the world’s older individuals living in urban centers and megacities are at further risk from “heat islands” that form from thermal trapping in manmade structures of concrete and steel [77, 78].
A number of physiological changes from the aging process raise the predisposition of older people to heat-related circulatory collapse. First, aging is tied to reductions in evaporative cooling efficiency due to decreased overall sweat production, particularly from the core of the body [79, 80]. This problem is exacerbated by the fact that elders are less able to redirect blood flow away from the deep splanchnic vasculature to the skin to facilitate cooling [81, 82]. Second, aging is associated with weaker contractile force of the heart in response to heat, meaning that older hearts are less capable of maintaining sufficient cardiac output in response to drops in blood pressure and left ventricular preload (say, from dehydration) than younger hearts [81]. Lastly, there is a reduction in surface thermoreceptor density in older adults, meaning that the heat releasing autoregulatory mechanisms of the body are less likely to be triggered with advancing age [83, 84].
This sensitivity to heat and fluid loss is particularly intensified in older adults with CVD. One reason is the effect of certain medications commonly used to treat these conditions. Diuretics, frequently employed to maintain optimal cardiac preload in patients with heart failure and chronic kidney disease, increase vulnerability to dehydration by reducing total resting blood volume. Beta blockers, utilized for managing hypertension, coronary disease, cardiomyopathies, and arrhythmias, further reduce the ability of the heart to augment its rate and stroke volume in response to increased circulatory demand [85, 86•]. Furthermore, patients living with disorders that limit myocardial contractility such as heart failure or obstructive coronary atherosclerosis, are more likely to develop cardiac ischemia at peak stress from heat exertion, increasing the risk of precipitating cardiogenic shock or myocardial infarction [23].
These factors make it understandable why the majority of deaths from heat waves are actually not due to the direct effects of heat (i.e., heat stroke, heat exhaustion) but rather from cardiovascular and cerebrovascular complications from the extreme strain placed upon the aging heart. For example, of the 692 excess deaths from the 1995 Chicago heat wave, only 4.7% were directly attributable to heat stroke, while 93.7% of excess deaths listed underlying CVD as a contributing factor [87]. Similarly, it is believed that over half (and possibly nearly two-thirds) of the mortalities from the 1995 and 1997 Milwaukee heat waves were directly precipitated by cardiovascular causes [88]. These findings are made mechanistically plausible by the fact that elevated cardiac troponin levels in blood samples of overheated patients are an independent prognostic marker of poor outcome from heat illness, particularly among the older individuals [89, 90].
Extreme Weather Events and Rising Sea Levels
Among the most striking effects of climate change are the intensification of seasonal environmental phenomena, chief among them severe weather anomalies such as hurricanes, tornadoes, severe thunderstorms, and winter storms or blizzards [17, 18]. These aberrant events carry the capacity for immense physical destruction to buildings, roads, and power lines, thus crippling healthcare delivery systems. Elders with CVD, who are particularly dependent on pharmacies, clinics, and hospitals, can find themselves cut off from these resources during these crises [91]. Furthermore, the immense emotional trauma inflicted by such natural disasters has been associated with surges in acute CVD complications. New Orleans area hospitals experienced a nearly threefold increase in myocardial infarction admissions immediately following Hurricane Katrina, with the rise in cases persisting for years following the catastrophe [92–95].
Interestingly, although heat waves have been linked to increased cardiovascular sequelae among older people, so have extreme cold weather events, and in general, global cooling patterns are correlated with a significant number of CVD mortalities [96, 97]. It has been long recognized that major snowstorms are followed by ischemic heart disease–attributable deaths and cardiac admissions [97, 98]. Further investigation is necessary to understand the mechanism of these findings, although it is hypothesized that the reduced circulatory reserve of older adults amplifies their susceptibility to the myocardial and metabolic demands imposed by physical activity in cold weather conditions and snow.
Another very prominent environmental concern stemming from climate change is that of melting polar ice caps and subsequently elevated global sea levels [17, 18]. In conjunction with the worsened storm seasons noted above, rising sea levels have augmented the severity and frequency of flooding in coastal zones, which again hold major implications for less-mobile elders [99]. Flooding not only physically disrupts cardiovascular care infrastructure, it also increases the risk of vector-borne diarrheal diseases, which will affect older populations, who are more vulnerable to cardiac stresses from dehydration and more likely to be on diuretic medications, more severely [100, 101].
Perhaps most insidiously, however, rising sea levels in these regions are encroaching on underground wells and other sources of groundwater for human consumption [102, 103]. The resultant increase in drinking water salinity carries population-level implications for sodium ingestion–related hypertension [104, 105]. Additionally, the contaminated water is projected to reduce crop yield in the millions of acres of coastal farms (particularly for subsistence farmers in alluvial floodplains), jeopardizing the long-term availability of fresh produce critical for good cardiovascular health [106–108].
Pandemic and Epidemic Infectious Diseases
The devastation caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and its resultant coronavirus disease 2019 (COVID-19) have made the consequences of human environmental impacts on global health stark, given the likely zoonotic origin of the contagion [109–111]. Nevertheless, COVID-19 is not the first infectious pathogen to make the jump from animal to human, and will not be the last to do so. Indeed, the preceding decades have been characterized by potential pandemic warning signs posed not just by coronaviruses, but also by influenza viruses and paramyxoviruses with well-established animal vectors [109, 112–115].
Climate change has elevated the risk of pandemic infections in a number of ways, including increased human-animal contact (thus escalating the possibility of zoonotic disease transmission) by shifting wildlife habitats towards human settlements, and by the warming of tropics making new regions suitable for inhabitation by disease vectors such as arboviruses and their insect hosts [109, 110, 116]. Furthermore, warm winters have been associated with “rebound” flu seasons of unusual severity, leading researchers to postulate that global warming may result in longer, harsher influenza seasons when they do occur [109, 117]. This is particularly concerning for older adults, as advanced age and pre-existing heart disease are both independent predictors for all-cause and cardiovascular mortality from influenza in this group [118–120]. Much of this may be due to immunosenescence, an age-related phenomenon consisting of deterioration of both the innate and adaptive immune responses, which lead to increased susceptibility to infection, poor response to vaccination, and a pro-atherosclerotic autoinflammatory state [121, 122].
COVID-19, in particular, has laid bare the vulnerabilities of our healthcare system to pandemic-associated disruptions for both older individuals and patients living with chronic CVD. Nursing homes and long-term care facilities were among the first outbreak zones to record massive casualties from the coronavirus, and CVD treatment infrastructure such as cardiac catheterization laboratories were among the first to be shut down due to quarantine and exposure protocols [123]. Indeed, even critical emergency care for ST-elevation myocardial infarctions were compromised, with some institutions reporting significant delays in lifesaving procedural door-to-balloon time therapies [124]. Fears of contracting the disease have led to postponing of even important operations and cardiovascular screening studies, both during the initial pandemic outbreak as well as during subsequent surges, with major implications for the timely management of these debilitating conditions [125–127].
Vulnerable Populations
Although older adults living with heart disease are a generally vulnerable population, certain subgroups are likely to disproportionately suffer from the cardiovascular impacts of climate change. Multiple analyses have demonstrated both advanced age and low socioeconomic status to be independent determinants of poor cardiovascular outcome from air pollution, wildfires, heat waves, and natural disasters [20, 27, 32, 69, 128]. This may be attributable to greater baseline ambient pollution exposure, higher baseline prevalence of cardiovascular comorbidities and disease severity, and reduced financial access to specialty healthcare. Indeed, indigent elders are more likely to live near highways, and to have been engaged in jobs with occupational air pollution exposure [129–132]. Per US census data, both older individuals and the impoverished are more likely to live in regions vulnerable to wildfire [69].
Additionally, epidemiologic analyses have revealed that the structural racism experienced by Black and Native American communities lead to higher risk of exposure to environmental pollutants, natural disasters, and their associated mortality [19, 69, 74, 87, 133, 134]. Indigenous populations globally, many of whom depend on subsistence agriculture and farming, will be further impacted by the loss of generational farmlands and fisheries needed for a heart-healthy diet, while tribal elders suffer unduly during disaster evacuations due to the cultural shocks of displacement [133, 135–137].
These factors are further intensified for older people living in low- and middle-income countries, where rapid industrialization has led to intensification of unhealthy average air quality, particularly in urban centers [34, 138]. The annual average PM2.5 exposure levels in China and Bangladesh are currently over 50 and 70 μg/m3, respectively, which well exceed the recently updated World Health Organization guideline recommended annual average concentration of 5 μg/m3 [34, 139, 140••]. Many older women in poor countries are often tasked with cooking on traditional biomass-burning stoves [32, 35, 138]. This source of household air pollution, especially in inadequately ventilated homes, is a potent and concentrated source of cardiotoxic particulate matter linked to significant CVD morbidity [16, 31, 32, 35]. By 2050, it is estimated that 80% of people over the age of 60 in the world will live in low- and middle-income countries, nations whose health systems are still emerging from overcoming infectious epidemic diseases, and are having to fight both these transmissible illnesses and the rising tide of cardiovascular disorders simultaneously [3, 141].
Future Directions
Although the ongoing threat of further climate change leaves the future uncertain, there are measures that policymakers, researchers, and healthcare providers can take to mitigate the risks that our warming globe poses to the heart health of our elders. First, we must be steadfast in our advocacy for carbon emission reductions and environmentally sustainable practices from governments and corporations. On a more individual level, though yet sparse, there is emerging data that personal protective tools such as facemasks, portable air purifiers, and air conditioners can reduce the burden of airborne pollutants and heat stress [34, 36, 142]. Healthcare providers should thus screen older patients, particularly the frail, indigent, and those with multiple pre-existing cardiac comorbidities, for harmful environmental exposures such as chronic air pollution and acute heat/fire risks. If present (or for those living in regions of the world with seasonal wildfires and heat waves), clinicians should advise such patients on personal risk mitigation strategies as noted above. Emergency preparedness authorities and clinicians should also counsel high-risk older adults on disaster contingency planning preceding storm, heat, and fire seasons, including having medications and critical personal belongings prepared for evacuation. Indeed, both the US Centers for Disease Control and Environmental Protection Agency recommend that older individuals and those living with chronic cardiovascular conditions should have an emergency plan with medications and personal protective equipment ready, while avoiding excessive activity during such events [143, 144]. Currently, two-thirds of Americans over the age of 65 report having no such plan in the event of a disaster [66].
Researchers in the fields of Earth systems studies, public health, and cardiovascular science should also focus further investigations on the unique physiologic aspects of the aging process that increase the susceptibility of older adults to environmental insults. These should be paired with examinations of the socioeconomic and demographic trends that synergistically amplify this relationship. Additionally, high-quality randomized clinical trials are needed to determine the efficacy of personal-level protective equipment and policy-level risk mitigation strategies on reducing acute cardiovascular decompensation risk among elders during extreme weather events.
That said, it is critical that older individuals be involved in the development of strategies to mitigate these challenges. Despite the physical limitations imposed by age, many have developed mental resiliency that society can leverage. These include community leadership, family cohesiveness, the ability to mobilize social capital, and longitudinal perspective from living through previous disasters [66, 140••]. Indeed, older survivors of Hurricane Katrina cited having withstood prior hurricanes (in addition to the full extent of life’s hardships) as sources of strength during their most trying times [145]. Most importantly, many older adults espouse the phenomenon of “legacy thinking”, where they are able to utilize their transgenerational knowledge to campaign for and prioritize the needs of their children and grandchildren during times of crisis [146]. Future directions in policy and clinical decision-making can incorporate these foundations of resilience into creating a socio-medical-environmental culture that better protects the cardiovascular wellbeing of our elders as well as the planet they live in.
Acknowledgements
Figure 1 includes graphics acquired and modified from designs by Macrovector/Ibrandify/Freepik.
Compliance with Ethical Standards
Conflict of Interest
Dr. Odden reports personal fees from Cricket Health, Inc., outside the submitted work. The other authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Global Cardiovascular Health
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Andrew Y. Chang, Email: aychang@stanford.edu
Michelle C. Odden, Email: modden@stanford.edu
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Philbeck T, Davis N. The Fourth Industrial Revolution: shaping a new era. J Int Aff. 2018;72:17–22. [Google Scholar]
- 2.Wade RH. Is globalization reducing poverty and inequality? Int J Health Serv. 2004;34:381–414. doi: 10.2190/G8F1-01FL-MEDW-JVG1. [DOI] [PubMed] [Google Scholar]
- 3.Bloom DE, Canning D, Lubet A. Global population aging: facts, challenges, solutions & perspectives. Daedalus. 2015;144:80–92. doi: 10.1162/DAED_a_00332. [DOI] [Google Scholar]
- 4.Bergh A, Nilsson T. Good for living? On the relationship between globalization and life expectancy. World Dev. 2010;38:1191–1203. doi: 10.1016/j.worlddev.2010.02.020. [DOI] [Google Scholar]
- 5.Yang X, Li N, Mu H, Zhang M, Pang J, Ahmad M. Study on the long-term and short-term effects of globalization and population aging on ecological footprint in OECD countries. Ecol Complex. 2021;47:100946. doi: 10.1016/j.ecocom.2021.100946. [DOI] [Google Scholar]
- 6.O’Brien KL, Leichenko RM. Double exposure: assessing the impacts of climate change within the context of economic globalization. Glob Environ Chang. 2000;10:221–232. doi: 10.1016/S0959-3780(00)00021-2. [DOI] [Google Scholar]
- 7.• Gersh BJ, Sliwa K, Mayosi BM, Yusuf S. Novel therapeutic concepts. Eur Heart J. 2010;31:642–8. The epidemic of cardiovascular disease in the developing world: global implications. [DOI] [PubMed]
- 8.McDermott MM. The international pandemic of chronic cardiovascular disease. JAMA. 2007;297:1253. doi: 10.1001/jama.297.11.1253. [DOI] [PubMed] [Google Scholar]
- 9.Fuster V. Global burden of cardiovascular disease. J Am Coll Cardiol. 2014;64:520–522. doi: 10.1016/j.jacc.2014.06.1151. [DOI] [PubMed] [Google Scholar]
- 10.Chang AY, Barry M, Harrington RA. The need to expand the framework of environmental determinants of cardiovascular health from climate change to planetary health: trial by wildfire. Circulation. 2021;143:2029–2031. doi: 10.1161/CIRCULATIONAHA.120.051892. [DOI] [PubMed] [Google Scholar]
- 11.United Nations . World population ageing 2019: Highlights. New York: UN; 2019. [Google Scholar]
- 12.Popkin BM. Global changes in diet and activity patterns as drivers of the nutrition transition. In: Kalhan SC, Prentice AM, Yajnik CS, editors. Nestlé nutrition institute workshop series: pediatric program. Basel: KARGER; 2009. pp. 1–14. https://www.karger.com/Article/FullText/209967. Cited 16 Sep 2020. [DOI] [PubMed]
- 13.Popkin BM. The nutrition transition and its health implications in lower-income countries. Public Health Nutr. 1998;1:5–21. doi: 10.1079/PHN19980004. [DOI] [PubMed] [Google Scholar]
- 14.Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 2012;70:3–21. doi: 10.1111/j.1753-4887.2011.00456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anand SS, Hawkes C, de Souza RJ, Mente A, Nugent R, et al. Food consumption and its impact on cardiovascular disease: importance of solutions focused on the globalized food system: a report from the workshop convened by the World Heart Federation. J Am Coll Cardiol. 2015;66:1590–1614. doi: 10.1016/j.jacc.2015.07.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2019;2020(76):2982–3021. doi: 10.1016/j.jacc.2020.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Meteorological Organization. State of the Global Climate 2020. 2021. https://library.wmo.int/doc_num.php?explnum_id=10618. Accessed 28 Aug 2021.
- 18.IPCC. Climate Change 2021: The physical science basis. Contribution of working group I to the sixth assessment report of the intergovernmental panel on climate change. 2021. https://www.ipcc.ch/report/ar6/wg1/downloads/report/IPCC_AR6_WGI_Full_Report.pdf. Accessed 5 Sept 2021.
- 19.Brunkard J, Namulanda G, Ratard R. Hurricane Katrina deaths, Louisiana, 2005. Disaster Med Public Health Prep. 2008;2:215–223. doi: 10.1097/DMP.0b013e31818aaf55. [DOI] [PubMed] [Google Scholar]
- 20.Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, et al. Heart Disease and Stroke Statistics–2021 Update: A report from the American Heart Association. Circulation. 2021;143. https://www.ahajournals.org/doi/10.1161/CIR.0000000000000950. Cited 3 Sep 2021. [DOI] [PubMed]
- 21.Yazdanyar A, Newman AB. The burden of cardiovascular disease in the elderly: morbidity, mortality, and costs. Clin Geriatr Med. 2009;25:563–577. doi: 10.1016/j.cger.2009.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rodgers JL, Jones J, Bolleddu SI, Vanthenapalli S, Rodgers LE, Shah K, et al. Cardiovascular risks associated with gender and aging. J Cardiovasc Dev Dis. 2019;6:E19. doi: 10.3390/jcdd6020019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kenney WL, Craighead DH, Alexander LM. Heat waves, aging, and human cardiovascular health. Med Sci Sports Exerc. 2014;46:1891–1899. doi: 10.1249/MSS.0000000000000325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee W-J, Liu C-Y, Peng L-N, Lin C-H, Lin H-P, Chen L-K. PM2.5 air pollution contributes to the burden of frailty. Sci Rep. 2020;10:14478. doi: 10.1038/s41598-020-71408-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Eckel SP, Louis TA, Chaves PHM, Fried LP, Margolis AHG. Modification of the association between ambient air pollution and lung function by frailty status among older adults in the cardiovascular health study. Am J Epidemiol. 2012;176:214–223. doi: 10.1093/aje/kws001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stewart R. Cardiovascular disease and frailty: what are the mechanistic links? Clin Chem. 2019;65:80–86. doi: 10.1373/clinchem.2018.287318. [DOI] [PubMed] [Google Scholar]
- 27.Bell ML, Zanobetti A, Dominici F. Evidence on vulnerability and susceptibility to health risks associated with short-term exposure to particulate matter: a systematic review and meta-analysis. Am J Epidemiol. 2013;178:865–876. doi: 10.1093/aje/kwt090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rosenkoetter MM, Covan EK, Cobb BK, Bunting S, Weinrich M. Perceptions of older adults regarding evacuation in the event of a natural disaster. Public Health Nurs. 2007;24:160–168. doi: 10.1111/j.1525-1446.2007.00620.x. [DOI] [PubMed] [Google Scholar]
- 29.McGuire LC, Ford ES, Okoro CA. Natural disasters and older US adults with disabilities: implications for evacuation. Disasters. 2007;31:49–56. doi: 10.1111/j.1467-7717.2007.00339.x. [DOI] [PubMed] [Google Scholar]
- 30.National Association of Area Agencies on Aging, National Council on Aging, and UnitedHealthcare. The United States of Aging Survey. 2012. https://www.aarp.org/content/dam/aarp/livable-communities/learn/research/the-united-states-of-aging-survey-2012-aarp.pdf. Accessed 5 Sept 2021.
- 31.Murray CJL, Aravkin AY, Zheng P, Abbafati C, Abbas KM, Abbasi-Kangevari M, et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1223–1249. doi: 10.1016/S0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Landrigan PJ, Fuller R, Acosta NJR, Adeyi O, Arnold R, Basu N (Nil), et al. The Lancet Commission on pollution and health. Lancet. 2018;391:462–512. [DOI] [PubMed]
- 33.Brauer M, Casadei B, Harrington RA, Kovacs R, Sliwa K, WHF Air Pollution Expert Group Taking a stand against air pollution-the impact on cardiovascular disease: a joint opinion from the World Heart Federation, American College of Cardiology, American Heart Association, and the European Society of Cardiology. Circulation. 2021;143:e800–e804. doi: 10.1161/CIRCULATIONAHA.120.052666. [DOI] [PubMed] [Google Scholar]
- 34.Rajagopalan S, Al-Kindi SG, Brook RD. Air pollution and cardiovascular disease: JACC State-of-the-Art Review. J Am Coll Cardiol. 2018;72:2054–2070. doi: 10.1016/j.jacc.2018.07.099. [DOI] [PubMed] [Google Scholar]
- 35.Newby DE, Mannucci PM, Tell GS, Baccarelli AA, Brook RD, Donaldson K, et al. Expert position paper on air pollution and cardiovascular disease. Eur Heart J. 2015;36:83–93. doi: 10.1093/eurheartj/ehu458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brook RD, Rajagopalan S, Pope CA, Brook JR, Bhatnagar A, Diez-Roux AV, et al. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation. 2010;121:2331–2378. doi: 10.1161/CIR.0b013e3181dbece1. [DOI] [PubMed] [Google Scholar]
- 37.Held IM, Soden BJ. Robust responses of the hydrological cycle to global warming. J Clim. 2006;19:5686–5699. doi: 10.1175/JCLI3990.1. [DOI] [Google Scholar]
- 38.Hong C, Zhang Q, Zhang Y, Davis SJ, Tong D, Zheng Y, et al. Impacts of climate change on future air quality and human health in China. Proc Natl Acad Sci USA. 2019;116:17193–17200. doi: 10.1073/pnas.1812881116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Garthwaite R, Fowler D, Stevenson D, Cox P, Ashmore M, Grennfelt P, et al. Ground level ozone in the 21st century: trends, interactions with climate and environmental impacts. IOP Conf Ser Earth Environ Sci. 2009;6:282002. doi: 10.1088/1755-1307/6/28/282002. [DOI] [Google Scholar]
- 40.Kinney PL. Climate change, air quality, and human health. Am J Prev Med. 2008;35:459–467. doi: 10.1016/j.amepre.2008.08.025. [DOI] [PubMed] [Google Scholar]
- 41.Bell ML, Goldberg R, Hogrefe C, Kinney PL, Knowlton K, Lynn B, et al. Climate change, ambient ozone, and health in 50 US cities. Clim Change. 2007;82:61–76. doi: 10.1007/s10584-006-9166-7. [DOI] [Google Scholar]
- 42.Bell ML, Dominici F, Samet JM. A meta-analysis of time-series studies of ozone and mortality with comparison to the national morbidity, mortality, and air pollution study. Epidemiology. 2005;16:436–445. doi: 10.1097/01.ede.0000165817.40152.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Malik AO, Jones PG, Chan PS, Peri-Okonny PA, Hejjaji V, Spertus JA. Association of long-term exposure to particulate matter and ozone with health status and mortality in patients after myocardial infarction. Circ: Cardiovascular Quality and Outcomes. 2019;12. https://www.ahajournals.org/doi/10.1161/CIRCOUTCOMES.119.005598. Cited 5 Sep 2021. [DOI] [PMC free article] [PubMed]
- 44.Beggs PJ. Impacts of climate change on aeroallergens: past and future. Clin Exp Allergy. 2004;34:1507–1513. doi: 10.1111/j.1365-2222.2004.02061.x. [DOI] [PubMed] [Google Scholar]
- 45.Weichenthal S, Lavigne E, Villeneuve PJ, Reeves F. Airborne pollen concentrations and emergency room visits for myocardial infarction: a multicity case-crossover study in Ontario, Canada. Am J Epidemiol. 2016;183:613–621. doi: 10.1093/aje/kwv252. [DOI] [PubMed] [Google Scholar]
- 46.Low RB, Bielory L, Qureshi AI, Dunn V, Stuhlmiller DFE, Dickey DA. The relation of stroke admissions to recent weather, airborne allergens, air pollution, seasons, upper respiratory infections, and asthma incidence, September 11, 2001, and Day of the Week. Stroke. 2006;37:951–957. doi: 10.1161/01.STR.0000214681.94680.66. [DOI] [PubMed] [Google Scholar]
- 47.Brunekreef B, Hoek G, Fischer P, Spieksma FT. Relation between airborne pollen concentrations and daily cardiovascular and respiratory-disease mortality. Lancet. 2000;355:1517–1518. doi: 10.1016/S0140-6736(00)02168-1. [DOI] [PubMed] [Google Scholar]
- 48.Schuliga M, Read J, Knight DA. Ageing mechanisms that contribute to tissue remodeling in lung disease. Age Res Rev. 2021;70:101405. doi: 10.1016/j.arr.2021.101405. [DOI] [PubMed] [Google Scholar]
- 49.Parrish AR. The impact of aging on epithelial barriers. Tissue Barriers. 2017;5:e1343172. doi: 10.1080/21688370.2017.1343172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Koken PJM, Piver WT, Ye F, Elixhauser A, Olsen LM, Portier CJ. Temperature, air pollution, and hospitalization for cardiovascular diseases among elderly people in Denver. Environ Health Perspect. 2003;111:1312–1317. doi: 10.1289/ehp.5957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schwartz J, Morris R. Air pollution and hospital admissions for cardiovascular disease in Detroit, Michigan. Am J Epidemiol. 1995;142:23–35. doi: 10.1093/oxfordjournals.aje.a117541. [DOI] [PubMed] [Google Scholar]
- 52.Barnett AG, Williams GM, Schwartz J, Best TL, Neller AH, Petroeschevsky AL, et al. The effects of air pollution on hospitalizations for cardiovascular disease in elderly people in Australian and New Zealand Cities. Environ Health Perspect. 2006;114:1018–1023. doi: 10.1289/ehp.8674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chuang K-J, Yan Y-H, Chiu S-Y, Cheng T-J. Long-term air pollution exposure and risk factors for cardiovascular diseases among the elderly in Taiwan. Occup Environ Med. 2011;68:64–68. doi: 10.1136/oem.2009.052704. [DOI] [PubMed] [Google Scholar]
- 54.Jalaludin B, Morgan G, Lincoln D, Sheppeard V, Simpson R, Corbett S. Associations between ambient air pollution and daily emergency department attendances for cardiovascular disease in the elderly (65+ years), Sydney, Australia. J Expo Sci Environ Epidemiol. 2006;16:225–237. doi: 10.1038/sj.jea.7500451. [DOI] [PubMed] [Google Scholar]
- 55.Morris RD, Naumova EN, Munasinghe RL. Ambient air pollution and hospitalization for congestive heart failure among elderly people in seven large US cities. Am J Public Health. 1995;85:1361–1365. doi: 10.2105/AJPH.85.10.1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yang Y, Tang R, Qiu H, Lai P-C, Wong P, Thach T-Q, et al. Long term exposure to air pollution and mortality in an elderly cohort in Hong Kong. Environ Int. 2018;117:99–106. doi: 10.1016/j.envint.2018.04.034. [DOI] [PubMed] [Google Scholar]
- 57.Gerber Y, Myers V, Broday DM, Steinberg DM, Yuval. Koton S, et al. Frailty status modifies the association between air pollution and post-myocardial infarction mortality: a 20-year follow-up study. J Am Coll Cardiol. 2014;63:1698–1699. doi: 10.1016/j.jacc.2014.01.026. [DOI] [PubMed] [Google Scholar]
- 58.Tan AX, Shah SJ, Sanders JL, Psaty BM, Wu C, Gardin JM, et al. Association between myocardial strain and frailty in CHS. Circ: Cardiovascular Imaging. 2021;14. https://www.ahajournals.org/doi/10.1161/CIRCIMAGING.120.012116. Cited 6 Sep 2021. [DOI] [PMC free article] [PubMed]
- 59.Myers V, Broday DM, Steinberg DM, Yuval. Drory Y, Gerber Y. Exposure to particulate air pollution and long-term incidence of frailty after myocardial infarction. Ann Epidemiol. 2013;23:395–400. doi: 10.1016/j.annepidem.2013.05.001. [DOI] [PubMed] [Google Scholar]
- 60.Grande G, Ljungman PLS, Eneroth K, Bellander T, Rizzuto D. Association between cardiovascular disease and long-term exposure to air pollution with the risk of dementia. JAMA Neurol. 2020;77:801. doi: 10.1001/jamaneurol.2019.4914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Reid CE, Brauer M, Johnston FH, Jerrett M, Balmes JR, Elliott CT. Critical review of health impacts of wildfire smoke exposure. Environ Health Perspect. 2016;124:1334–1343. doi: 10.1289/ehp.1409277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.• Jones CG, Rappold AG, Vargo J, Cascio WE, Kharrazi M, McNally B, et al. Out-of-hospital cardiac arrests and wildfire-related particulate matter during 2015–2017 California Wildfires. JAHA. 2020;9. https://www.ahajournals.org/doi/10.1161/JAHA.119.014125. Cited 23 Sep 2020. This analysis linked National Oceanic and Atmospheric Administration (NOAA) satellite data of wildfire plume presence and intensity with Cardiac Arrest Registry to Enhance Survival (CARES) outcomes to detect a deleterious impact of wildfire-associated air pollution on out-of-hospital cardiac arrests. Increasing age and lower socioeconomic status were also found to be an important modifier of the relationship.
- 63.Wettstein ZS, Hoshiko S, Fahimi J, Harrison RJ, Cascio WE, Rappold AG. Cardiovascular and cerebrovascular emergency department visits associated with wildfire smoke exposure in California in 2015. JAHA. 2018;7. https://www.ahajournals.org/doi/10.1161/JAHA.117.007492. Cited 2021 Aug 17. [DOI] [PMC free article] [PubMed]
- 64.DeSalvo K, Petrin C. From Katrina to wildfires: leveraging technology in disaster response. Health Affairs (Blog); 2017. [Google Scholar]
- 65.Wong SD, Broader JC, Shaheen SA. Can Sharing economy platforms increase social equity for vulnerable populations in disaster response and relief? A case study of the 2017 and 2018 California Wildfires. Transp Res Interdiscip Perspect. 2020;5:100131. [Google Scholar]
- 66.Shih RA, Acosta JD, Chen EK, Carbone EG, Xenakis L, Adamson DM, et al. Improving disaster resilience among older adults: insights from public health departments and aging-in-place efforts. Rand Health Q. 2018;8:3. [PMC free article] [PubMed] [Google Scholar]
- 67.Gao Y, Chan EYY, Lam HCY, Wang A. Perception of potential health risk of climate change and utilization of fans and air conditioners in a representative population of Hong Kong. Int J Disaster Risk Sci. 2020;11:105–118. doi: 10.1007/s13753-020-00256-z. [DOI] [Google Scholar]
- 68.Hansen A, Bi P, Nitschke M, Pisaniello D, Newbury J, Kitson A. Perceptions of heat-susceptibility in older persons: barriers to adaptation. Int J Environ Res Public Health. 2011;8:4714–4728. doi: 10.3390/ijerph8124714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Masri S, Scaduto E, Jin Y, Wu J. Disproportionate impacts of wildfires among elderly and low-income communities in California from 2000–2020. IJERPH. 2021;18:3921. doi: 10.3390/ijerph18083921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Robine J-M, Cheung SLK, Le Roy S, Van Oyen H, Griffiths C, Michel J-P, et al. Death toll exceeded 70,000 in Europe during the summer of 2003. C R Biol. 2008;331:171–178. doi: 10.1016/j.crvi.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 71.Barriopedro D, Fischer EM, Luterbacher J, Trigo RM, García-Herrera R. The hot summer of 2010: redrawing the temperature record map of Europe. Science. 2011;332:220–224. doi: 10.1126/science.1201224. [DOI] [PubMed] [Google Scholar]
- 72.United States Environmental Protection Agency. Climate change indicators: heat-related deaths. 2021. https://www.epa.gov/climate-indicators/climate-change-indicators-heat-related-deaths#ref10. Accessed 6 Sept 2021.
- 73.Kalkstein LS, Greene JS. An evaluation of climate/mortality relationships in large U.S. cities and the possible impacts of a climate change. Environ Health Perspect. 1997;105:84–93. doi: 10.1289/ehp.9710584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Medina-Ramón M, Zanobetti A, Cavanagh DP, Schwartz J. Extreme temperatures and mortality: assessing effect modification by personal characteristics and specific cause of death in a multi-city case-only analysis. Environ Health Perspect. 2006;114:1331–1336. doi: 10.1289/ehp.9074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Antonia K, Glen PK, Andreas DF. The impact of heat waves on mortality among the elderly: a mini systematic review. J Geriatr Med Gerontol. 2018;4. https://www.clinmedjournals.org/articles/jgmg/journal-of-geriatric-medicine-and-gerontology-jgmg-4-053.php?jid=jgmg. Cited 6 Sep 2021.
- 76.Toulemon L, Barbieri M. The mortality impact of the August 2003 heat wave in France: investigating the ‘harvesting’ effect and other long-term consequences. Popul Stud. 2008;62:39–53. doi: 10.1080/00324720701804249. [DOI] [PubMed] [Google Scholar]
- 77.Laaidi K, Zeghnoun A, Dousset B, Bretin P, Vandentorren S, Giraudet E, et al. The impact of heat islands on mortality in Paris during the August 2003 heat wave. Environ Health Perspect. 2012;120:254–259. doi: 10.1289/ehp.1103532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Arnberger A, Allex B, Eder R, Ebenberger M, Wanka A, Kolland F, et al. Elderly resident’s uses of and preferences for urban green spaces during heat periods. Urban For Urban Green. 2017;21:102–115. doi: 10.1016/j.ufug.2016.11.012. [DOI] [Google Scholar]
- 79.Anderson RK, Kenney WL. Effect of age on heat-activated sweat gland density and flow during exercise in dry heat. J Appl Physiol. 1985;1987(63):1089–1094. doi: 10.1152/jappl.1987.63.3.1089. [DOI] [PubMed] [Google Scholar]
- 80.Smith CJ, Alexander LM, Kenney WL. Nonuniform, age-related decrements in regional sweating and skin blood flow. Am J Physiol Regul Integr Comp Physiol . 2013;305:R877–R885. doi: 10.1152/ajpregu.00290.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Minson CT, Wladkowski SL, Cardell AF, Pawelczyk JA, Kenney WL. Age alters the cardiovascular response to direct passive heating. J Appl Physiol. 1985;1998(84):1323–1332. doi: 10.1152/jappl.1998.84.4.1323. [DOI] [PubMed] [Google Scholar]
- 82.Minson CT, Wladkowski SL, Pawelczyk JA, Kenney WL. Age, splanchnic vasoconstriction, and heat stress during tilting. Am J Physiol. 1999;276:R203–212. doi: 10.1152/ajpregu.1999.276.1.r203. [DOI] [PubMed] [Google Scholar]
- 83.Blatteis CM. Age-dependent changes in temperature regulation - a mini review. Gerontology. 2012;58:289–295. doi: 10.1159/000333148. [DOI] [PubMed] [Google Scholar]
- 84.Guergova S, Dufour A. Thermal sensitivity in the elderly: a review. Ageing Res Rev. 2011;10:80–92. doi: 10.1016/j.arr.2010.04.009. [DOI] [PubMed] [Google Scholar]
- 85.Westaway K, Frank O, Husband A, McClure A, Shute R, Edwards S, et al. Medicines can affect thermoregulation and accentuate the risk of dehydration and heat-related illness during hot weather. J Clin Pharm Ther. 2015;40:363–367. doi: 10.1111/jcpt.12294. [DOI] [PubMed] [Google Scholar]
- 86.• Layton JB, Li W, Yuan J, Gilman JP, Horton DB, Setoguchi S. Heatwaves, medications, and heat-related hospitalization in older Medicare beneficiaries with chronic conditions. PLoS ONE. 2020;15:e0243665.Utilizing US Medicare data with zip code level climate data for surface air temperature from the Meteorological Forcing Dataset for Land Surface Modeling and Daymet Daily Surface Weather Data, the authors of this analysis noted not only a substantial increase in heat-related hospitalizations among subjects 65 years or older living with chronic conditions during heat waves, but also significantly increased risk of hospitalization for elders taking ACE-inhibitors/ARBs, anticholinergic agents, antipsychotics, and loop diuretics. [DOI] [PMC free article] [PubMed]
- 87.Kaiser R, Le Tertre A, Schwartz J, Gotway CA, Daley WR, Rubin CH. The effect of the 1995 heat wave in Chicago on all-cause and cause-specific mortality. Am J Public Health. 2007;97(Suppl 1):S158–162. doi: 10.2105/AJPH.2006.100081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Weisskopf MG, Anderson HA, Foldy S, Hanrahan LP, Blair K, Török TJ, et al. Heat wave morbidity and mortality, Milwaukee, Wis, 1999 vs 1995: an improved response? Am J Public Health. 2002;92:830–833. doi: 10.2105/AJPH.92.5.830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hausfater P, Doumenc B, Chopin S, Le Manach Y, Santin A, Dautheville S, et al. Elevation of cardiac troponin I during non-exertional heat-related illnesses in the context of a heatwave. Crit Care. 2010;14:R99. doi: 10.1186/cc9034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Davido A, Patzak A, Dart T, Sadier MP, Méraud P, Masmoudi R, et al. Risk factors for heat related death during the August 2003 heat wave in Paris, France, in patients evaluated at the emergency department of the Hôpital Européen Georges Pompidou. Emerg Med J. 2006;23:515–518. doi: 10.1136/emj.2005.028290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ford ES, Mokdad AH, Link MW, Garvin WS, McGuire LC, Jiles RB, et al. Chronic disease in health emergencies: in the eye of the hurricane. Prev Chronic Dis. 2006;3:A46. [PMC free article] [PubMed] [Google Scholar]
- 92.Gautam S, Menachem J, Srivastav SK, Delafontaine P, Irimpen A. Effect of Hurricane Katrina on the incidence of acute coronary syndrome at a primary angioplasty center in New Orleans. Disaster Med Public Health Prep. 2009;3:144–150. doi: 10.1097/DMP.0b013e3181b9db91. [DOI] [PubMed] [Google Scholar]
- 93.Becquart N, Naumova E, Singh G, Chui K. Cardiovascular disease hospitalizations in Louisiana Parishes’ elderly before, during and after Hurricane Katrina. IJERPH. 2018;16:74. doi: 10.3390/ijerph16010074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Jiao Z, Kakoulides SV, Moscona J, Whittier J, Srivastav S, Delafontaine P, et al. Effect of Hurricane Katrina on incidence of acute myocardial infarction in New Orleans three years after the storm. Am J Cardiol. 2012;109:502–505. doi: 10.1016/j.amjcard.2011.09.045. [DOI] [PubMed] [Google Scholar]
- 95.Moscona JC, Peters MN, Maini R, Katigbak P, Deere B, Gonzales H, et al. The incidence, risk factors, and chronobiology of acute myocardial infarction ten years after Hurricane Katrina. Disaster Med Public Health Prep. 2019;13:217–222. doi: 10.1017/dmp.2018.22. [DOI] [PubMed] [Google Scholar]
- 96.Guo Y, Gasparrini A, Armstrong B, Li S, Tawatsupa B, Tobias A, et al. Global variation in the effects of ambient temperature on mortality: a systematic evaluation. Epidemiology. 2014;25:781–789. doi: 10.1097/EDE.0000000000000165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Glass RI, Zack MM. Increase in deaths from ischaemic heart-disease after blizzards. Lancet. 1979;1:485–487. doi: 10.1016/S0140-6736(79)90835-3. [DOI] [PubMed] [Google Scholar]
- 98.Bobb JF, Ho KKL, Yeh RW, Harrington L, Zai A, Liao KP, et al. Time-course of cause-specific hospital admissions during snowstorms: an analysis of electronic medical records from major hospitals in Boston, Massachusetts. Am J Epidemiol. 2017;185(4):283–294. doi: 10.1093/aje/kww219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Bukvic A, Gohlke J, Borate A, Suggs J. Aging in flood-prone coastal areas: discerning the health and well-being risk for older residents. IJERPH. 2018;15:2900. doi: 10.3390/ijerph15122900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Ohl CA. Flooding and human health. BMJ. 2000;321:1167–1168. doi: 10.1136/bmj.321.7270.1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Nasci R. Vector-borne disease surveillance and natural disasters. Emerg Infect Dis. 1998;4:333–334. doi: 10.3201/eid0402.980227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Abd-Elhamid HF, Javadi AA. Impact of sea level rise and over-pumping on seawater intrusion in coastal aquifers. J Water Clim Change. 2011;2:19–28. doi: 10.2166/wcc.2011.053. [DOI] [Google Scholar]
- 103.Sherif MM, Singh VP. Effect of climate change on sea water intrusion in coastal aquifers. Hydrol Process. 1999;13:1277–1287. doi: 10.1002/(SICI)1099-1085(19990615)13:8<1277::AID-HYP765>3.0.CO;2-W. [DOI] [Google Scholar]
- 104.Vineis P, Chan Q, Khan A. Climate change impacts on water salinity and health. J Epidemiol Glob Health. 2011;1:5–10. doi: 10.1016/j.jegh.2011.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Scheelbeek PFD, Khan AE, Mojumder S, Elliott P, Vineis P. Drinking water sodium and elevated blood pressure of healthy pregnant women in salinity-affected coastal areas. Hypertension. 2016;68:464–470. doi: 10.1161/HYPERTENSIONAHA.116.07743. [DOI] [PubMed] [Google Scholar]
- 106.Reinelt P. Seawater intrusion policy analysis with a numerical spatially heterogeneous dynamic optimization model: SEAWATER INTRUSION POLICY ANALYSIS. Water Resour Res. 2005;41. http://doi.wiley.com/10.1029/2004WR003111. Cited 8 Sep 2021.
- 107.Arslan H, Demir Y. Impacts of seawater intrusion on soil salinity and alkalinity in Bafra Plain, Turkey. Environ Monit Assess. 2013;185:1027–1040. doi: 10.1007/s10661-012-2611-3. [DOI] [PubMed] [Google Scholar]
- 108.Sarkar B, Islam A, Majumder A. Seawater intrusion into groundwater and its impact on irrigation and agriculture: evidence from the coastal region of West Bengal, India. Reg Stud Mar Sci. 2021;44:101751. doi: 10.1016/j.rsma.2021.101751. [DOI] [Google Scholar]
- 109.Hashimoto S, Hikichi M, Maruoka S, Gon Y. Our future: experiencing the coronavirus disease 2019 (COVID-19) outbreak and pandemic. Respir Investig. 2021;59:169–179. doi: 10.1016/j.resinv.2020.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Beyer RM, Manica A, Mora C. Shifts in global bat diversity suggest a possible role of climate change in the emergence of SARS-CoV-1 and SARS-CoV-2. Sci Total Environ. 2021;767:145413. doi: 10.1016/j.scitotenv.2021.145413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Everard M, Johnston P, Santillo D, Staddon C. The role of ecosystems in mitigation and management of Covid-19 and other zoonoses. Environ Sci Policy. 2020;111:7–17. doi: 10.1016/j.envsci.2020.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Butler D. Swine flu goes global. Nature. 2009;458:1082–1083. doi: 10.1038/4581082a. [DOI] [PubMed] [Google Scholar]
- 113.Pipper J, Inoue M, Ng LFP, Neuzil P, Zhang Y, Novak L. Catching bird flu in a droplet. Nat Med. 2007;13:1259–1263. doi: 10.1038/nm1634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.de Wit E, van Doremalen N, Falzarano D, Munster VJ. SARS and MERS: recent insights into emerging coronaviruses. Nat Rev Microbiol. 2016;14:523–534. doi: 10.1038/nrmicro.2016.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Luby SP, Gurley ES, Hossain MJ. Transmission of human infection with Nipah virus. CLIN INFECT DIS. 2009;49:1743–1748. doi: 10.1086/647951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Gould EA, Higgs S. Impact of climate change and other factors on emerging arbovirus diseases. Trans R Soc Trop Med Hyg. 2009;103:109–121. doi: 10.1016/j.trstmh.2008.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Towers S, Chowell G, Hameed R, Jastrebski M, Khan M, Meeks J, et al. Climate change and influenza: the likelihood of early and severe influenza seasons following warmer than average winters. PLoS Curr. 2013. https://currents.plos.org/influenza/article/climate-change-and-influenza-the-likelihood-of-early-and-severe-influenza-seasons-following-warmer-than-average-winters/. Cited 8 Sep 2021. [DOI] [PMC free article] [PubMed]
- 118.Madjid M, Naghavi M, Litovsky S, Casscells SW. Influenza and cardiovascular disease: a new opportunity for prevention and the need for further studies. Circulation. 2003;108:2730–2736. doi: 10.1161/01.CIR.0000102380.47012.92. [DOI] [PubMed] [Google Scholar]
- 119.Warren-Gash C, Smeeth L, Hayward AC. Influenza as a trigger for acute myocardial infarction or death from cardiovascular disease: a systematic review. Lancet Infect Dis. 2009;9:601–610. doi: 10.1016/S1473-3099(09)70233-6. [DOI] [PubMed] [Google Scholar]
- 120.Nguyen JL, Yang W, Ito K, Matte TD, Shaman J, Kinney PL. Seasonal influenza infections and cardiovascular disease mortality. JAMA Cardiol. 2016;1:274. doi: 10.1001/jamacardio.2016.0433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Aw D, Silva AB, Palmer DB. Immunosenescence: emerging challenges for an ageing population. Immunology. 2007;120:435–446. doi: 10.1111/j.1365-2567.2007.02555.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Goronzy JJ, Weyand CM. Understanding immunosenescence to improve responses to vaccines. Nat Immunol. 2013;14:428–436. doi: 10.1038/ni.2588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Chang AY, Cullen MR, Harrington RA, Barry M. The impact of novel coronavirus COVID-19 on noncommunicable disease patients and health systems: a review. J Intern Med. 2020. [DOI] [PMC free article] [PubMed]
- 124.Tam C-CF, Cheung K-S, Lam S, Wong A, Yung A, Sze M, et al. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment–elevation myocardial infarction care in Hong Kong, China. Circ: Cardiovascular Quality and Outcomes. 2020. https://www.ahajournals.org/doi/10.1161/CIRCOUTCOMES.120.006631. Cited 29 Mar 2020. [DOI] [PMC free article] [PubMed]
- 125.Welt FGP, Shah PB, Aronow HD, Bortnick AE, Henry TD, Sherwood MW, et al. Catheterization laboratory considerations during the coronavirus (COVID-19) pandemic: from ACC’s Interventional Council and SCAI. J Am Coll Cardiol. 2020;S0735109720345666. [DOI] [PMC free article] [PubMed]
- 126.Yong CM, Spinelli KJ, Chiu ST, Jones B, Penny B, Gummidipundi S, et al. Cardiovascular procedural deferral and outcomes over COVID-19 pandemic phases: A multi-center study. Am Heart J. 2021;241:14–25. doi: 10.1016/j.ahj.2021.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Einstein AJ, Shaw LJ, Hirschfeld C, Williams MC, Villines TC, Better N, et al. International impact of COVID-19 on the diagnosis of heart disease. J Am Coll Cardiol. 2021;77:173–85. [DOI] [PMC free article] [PubMed]
- 128.Benevolenza MA, DeRigne L. The impact of climate change and natural disasters on vulnerable populations: a systematic review of literature. J Hum Behav Soc Environ. 2019;29:266–281. doi: 10.1080/10911359.2018.1527739. [DOI] [Google Scholar]
- 129.Boehmer TK, Foster SL, Henry JR, Woghiren-Akinnifesi EL, Yip FY, Centers for Disease Control and Prevention (CDC) Residential proximity to major highways - United States, 2010. MMWR Suppl. 2013;62:46–50. [PubMed] [Google Scholar]
- 130.Gan WQ, Tamburic L, Davies HW, Demers PA, Koehoorn M, Brauer M. Changes in residential proximity to road traffic and the risk of death from coronary heart disease. Epidemiology. 2010;21:642–649. doi: 10.1097/EDE.0b013e3181e89f19. [DOI] [PubMed] [Google Scholar]
- 131.Arif AA, Rohrer JE, Delclos GL. A population-based study of asthma, quality of life, and occupation among elderly Hispanic and non-Hispanic whites: a cross-sectional investigation. BMC Public Health. 2005;5:97. doi: 10.1186/1471-2458-5-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Torén K, Bergdahl IA, Nilsson T, Järvholm B. Occupational exposure to particulate air pollution and mortality due to ischaemic heart disease and cerebrovascular disease. Occup Environ Med. 2007;64:515–519. doi: 10.1136/oem.2006.029488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Mottershead KD, McGee TK, Christianson A. Evacuating a first nation due to wildfire smoke: the case of Dene Tha’ First Nation. Int J Disaster Risk Sci. 2020;11:274–286. doi: 10.1007/s13753-020-00281-y. [DOI] [Google Scholar]
- 134.Beverly JL, Bothwell P. Wildfire evacuations in Canada 1980–2007. Nat Hazards. 2011;59:571–596. doi: 10.1007/s11069-011-9777-9. [DOI] [Google Scholar]
- 135.Asfaw HW, McGee TK, Christianson AC. Indigenous elders’ experiences, vulnerabilities and coping during hazard evacuation: the case of the 2011 Sandy Lake First Nation Wildfire Evacuation. Soc Nat Resour. 2020;33:1273–1291. doi: 10.1080/08941920.2020.1745976. [DOI] [Google Scholar]
- 136.Kurashima N, Fortini L, Ticktin T. The potential of indigenous agricultural food production under climate change in Hawaiʻi. Nat Sustain. 2019;2:191–199. doi: 10.1038/s41893-019-0226-1. [DOI] [Google Scholar]
- 137.Weatherdon LV, Ota Y, Jones MC, Close DA, Cheung WWL. Projected scenarios for coastal first nations’ fisheries catch potential under climate change: management challenges and opportunities. PLoS One. 2016;11:e0145285. doi: 10.1371/journal.pone.0145285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Rajagopalan S, Brook RD. Indoor-outdoor air pollution continuum and CVD burden: an opportunity for improving global health. Glob Heart. 2012;7:207. doi: 10.1016/j.gheart.2012.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.World Health Organization. Burden of disease from ambient air pollution for 2012. 2014. https://www.who.int/airpollution/data/AAP_BoD_results_March2014.pdf. 22 Aug 2021.
- 140.•• World Health Organization. WHO global air quality guidelines: particulate matter (PM2.5 and PM10), ozone, nitrogen dioxide, sulfur dioxide and carbon monoxide: executive summary. Geneva: World Health Organization; 2021. https://apps.who.int/iris/handle/10665/345334. Cited 1 Nov 2021. The authors wish to highlight the recent change in WHO global air quality guidelines, which, among other recommendations, is notable for tightened standards on short-term exposure to particulate matter (PM2.5 and PM10), ozone, nitrogen dioxide, sulfur dioxide, and carbon monoxide, compared to their previous guidelines. [PubMed]
- 141.Shetty P. Grey matter: ageing in developing countries. The Lancet. 2012;379:1285–1287. doi: 10.1016/S0140-6736(12)60541-8. [DOI] [PubMed] [Google Scholar]
- 142.Bell ML, Ebisu K, Peng RD, Dominici F. Adverse health effects of particulate air pollution: modification by air conditioning. Epidemiology. 2009;20:682–686. doi: 10.1097/EDE.0b013e3181aba749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.US Centers for Disease Control. Chronic conditions and wildfire smoke. 2021. https://www.cdc.gov/air/wildfire-smoke/chronic-conditions.htm. Accessed 8 Sept 2021.
- 144.United States Environmental Protection Agency. How smoke from fires can affect your health. 2021. https://www.epa.gov/pm-pollution/how-smoke-fires-can-affect-your-health. Accessed 8 Sept 2021.
- 145.Adams V, Kaufman SR, van Hattum T, Moody S. Aging disaster: mortality, vulnerability, and long-term recovery among Katrina survivors. Med Anthropol. 2011;30:247–270. doi: 10.1080/01459740.2011.560777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Frumkin H, Fried L, Moody R. Aging, climate change, and legacy thinking. Am J Public Health. 2012;102:1434–1438. doi: 10.2105/AJPH.2012.300663. [DOI] [PMC free article] [PubMed] [Google Scholar]