Abstract
Objective:
To assess the utility of rapid parathyroid hormone (PTH) values in predicting transient post-operative hypocalcemia in patients with unplanned parathyroidectomy during total or completion thyroidectomy.
Methods:
All patients who underwent total or completion thyroidectomy between January 2010 and January 2015 were reviewed. Incidences of post-operative hypocalcemia were compared in patients with and without unplanned parathyroidectomy. Unplanned parathyroidectomy was defined as intra-operative incidental or intentional parathyroidectomy. Logistic regression assessed for predictors of hypocalcemia and optimum amount of calcium supplementation.
Results:
Thirty-eight (13.6%) patients had evidence of incidental parathyroidectomy and 39/280 (13.9%) patients had parathyroid autotransplantation intra-operatively. Central neck dissection and malignancy were identified as risk factors for unplanned parathyroidectomy (p = 0.001, p = 0.060). Patients with unplanned parathyroidectomy were more likely to have hypocalcemia (p = 0.002) and hypoparathyroidism (p < 0.0005). PTH value was the only significant predictor of hypocalcemia in these patients. In patients with a post-operative PTH of ≤15, initial calcium supplementation ≥ 1000 mg decreased the risk of hypocalcemia (p < 0.05).
Conclusion:
Post-operative PTH value predicts hypocalcemia in patients undergoing total and completion thyroidectomy with unplanned parathyroidectomy. In patients with a post-operative PTH <15, initial calcium supplementation with ≥1000 mg of elemental calcium is recommended.
Keywords: Incidental parathyroidectomy, Parathyroid autotransplantation, Hypocalcemia, Calcium supplementation, Parathyroid hormone, Hypoparathyroidism
1. Introduction
Unplanned parathyroidectomy, which occurs in 13.4–24.9% of patients undergoing total or completion thyroidectomy, is a significant risk factor for both postoperative transient and permanent hypocalcemia [1-6]. Intentional parathyroidectomy is secondary to devascularization, and incidental parathyroidectomy occurs when glands are found on pathology post-operatively. It has been previously established that the risk of postoperative hypoparathyroidism increases with extent of thyroidectomy, completion procedures, and central neck dissection [7]. Predicting and managing hypocalcemia may be significantly more difficult in patients with unplanned parathyroidectomy, whether inadvertent or intentional. These decisions include the need, timing, and amount of calcium supplementation and whether there is utility in obtaining parathyroid hormone (PTH) levels to guide this decision. In cases where removal of the gland is planned or recognized, parathyroid autotransplantation can be utilized to reduce the risk of permanent hypocalcemia; however, this does not affect transient post-operative hypocalcemia, as reimplanted glands achieve normal function after 3 to 14 weeks [8-10]. Patients with parathyroid removal are deemed high-risk for post-operative hypocalcemia and may benefit from a standardized post-operative management protocol to decrease risk of hypocalcemia and improve outcomes after thyroidectomy [11,12].
Previous studies have focused on incidence and risk factors leading to incidental parathyroidectomy and/or autotransplantation. There is no specific data on predicting and managing hypocalcemia in patients with unplanned parathyroidectomy. In this study, we evaluated the risk of post-operative hypocalcemia and hypoparathyroidism in patients when unplanned parathyroidectomy occurred during total or completion thyroidectomy. Secondly, we assessed whether post-operative PTH levels were associated with hypocalcemia in patients after unplanned parathyroidectomy. Lastly, we aimed to identify the optimum amount of calcium supplementation required to significantly decrease risk of resultant hypocalcemia to create a standardized post-operative management protocol. We hypothesized a significantly higher risk for transient hypoparathyroidism and hypocalcemia in the post-operative period with unplanned parathyroidectomy and would require supplemental calcium in the vast majority of cases obviating the value of obtaining postoperative PTH levels.
2. Materials and methods
2.1. Study samples
After approval by The Ohio State University Wexner Medical Center (OSUWMC) Institutional Review Board, a retrospective study was conducted on patients who underwent total or completion thyroidectomy at our institution between January 2010 and January 2015. The parathyroid glands were routinely identified intra-operatively and excessive manipulation was avoided if possible. Unplanned parathyroidectomy was defined as 1) incidental parathyroidectomy where parathyroid glands are either discovered on the permanent pathology post-operatively or recognized intra-operatively on the thyroid specimen and subsequently autotransplanted into separate muscle pockets in the sternocleidomastoid muscle; and 2) as intentional parathyroid autotransplantation secondary to significant devascularization of parathyroid tissue. Patients were excluded if they were under the age of 18, had a subtotal thyroidectomy, or had a combined single stage thyroidectomy with planned parathyroidectomy.
2.2. Study variables
Data collected includes demographics, clinical and surgical details, post-operative lab values, and comorbidities. The primary outcome, hypocalcemia, was defined as one reading in the post-operative period of ionized calcium < 4.0 mg/dL or regular calcium < 8.0 mg/dL. Serum intact PTH was obtained in the post-anesthesia care unit. PTH was measured using the ADVIA Centaur® PTH assay (SEIMENS). The normal PTH level in our laboratory ranges from 14.0 to 72.0 pg/mL.
We also evaluated the independent variables age, sex, history of hypocalcemia, prior neck surgery, concurrent central neck dissection, surgeon experience (< 20 vs 20–60 vs > 60 cases over study period), and pathology (benign vs malignant) as predictors of hypocalcemia in patients with unplanned parathyroidectomy.
Additionally, we evaluated the correlation between post-operative hypocalcemia and amount of initial calcium supplementation (none vs < 1000 mg vs ≥1000 mg). A patient was considered to have zero initial calcium supplementation if the administration was after the development of hypocalcemia.
2.3. Statistical analysis
Descriptive statistics were used to characterize the study population, stratified by unplanned parathyroidectomy. Comparisons between patients undergoing total or completion thyroidectomy with and without parathyroidectomy were assessed via two-sample t-tests for continuous variables and chi-squared or Fisher's exact tests for categorical variables. Univariable logistic regression models were used to assess association between independent predictors of hypocalcemia in patients with unplanned parathyroidectomy. Odds ratio (OR) and 95% confidence intervals (CI) are reported. A regression tree was conducted to assess patients at high risk of developing hypocalcemia in our patient population. Multivariable logistic regression was used to identify the optimum amount of initial calcium supplementation required to decrease the risk of hypocalcemia, with adjustments for age, sex, central neck dissection and serum PTH. Interaction between PTH and amount of calcium supplementation was further analyzed while adjusting for these variables. Statistical analysis was conducted in SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) and SPSS version 24 (IBM, Armok, NY).
3. Results
3.1. Patient characteristics
Two-hundred eighty patients underwent total or completion thyroidectomy (Table 1). Seventy-seven (27.5%) patients had evidence of unplanned parathyroidectomy. Specifically, 38/280 (13.6%) of patients had evidence of parathyroid tissue on the permanent pathology post-operatively. An additional 39/280 (13.9%) of patients had a parathyroid gland intentionally removed and autotransplanted secondary to evidence of devascularization or unintentionally removed with the thyroid specimen and subsequently autotransplanted. In the sample of 77 patients, 68/77 (88.3%) had total thyroidectomy while the remaining 9/77 (11.7%) had a completion thyroidectomy. The mean age of patients with unplanned parathyroidectomy was 48.5 ± 14.1. Most patients, 61/77 (79.2%) were female. Additionally, only 5/77 (6.5%) and 7/77 (9.1%) of patients had a history of abnormal calcium or prior neck surgery, respectively. Pathology of thyroid was malignant in 51/77 (66.2%) of cases and benign in 26/77 (33.8%) of cases.
Table 1.
Clinical characteristics – patients with and without parathyroidectomy.
| Clinical characteristics | Parathyroidectomy | No parathyroidectomy | Total | p-Value | |
|---|---|---|---|---|---|
| N (%) or mean (SD) | (n = 77) | (n = 203) | (n = 280) | ||
| Age | 48.5 (14.1) | 47.5 (14.1) | 47.8 (14.1) | 0.592 | |
| Sex | Male | 16 (20.8) | 57 (28.1) | 73 (26.1) | |
| Female | 61 (79.2) | 146 (71.9) | 207 (73.9) | 0.227 | |
| History of hypocalcemia | 5 (6.5) | 9 (4.4) | 14 (5.0) | 0.541 | |
| Prior neck surgery | 7 (9.1) | 18 (8.9) | 25 (8.9) | 1.000 | |
| Thyroidectomy | Total | 68 (88.3) | 182 (89.7) | 250 (89.3) | 1.000 |
| Completion | 9 (11.7) | 21 (10.3) | 30 (10.7) | ||
| Central neck dissection | 24 (38.1) | 38 (17.5) | 62 (22.1) | 0.001 | |
| Pathology | Benign | 26 (33.8) | 94 (46.3) | 120 (42.9) | |
| Malignant | 51 (66.2) | 109 (53.7) | 160 (57.1) | 0.060 | |
| Hypocalcemia | 36 (46.8) | 54 (26.6) | 90 (32.1) | 0.002 | |
| PTH obtained? | 56 (72.7) | 109 (53.7) | 165 (58.9) | 0.004 | |
| PTH value (n = 165) | 18.3 (21.6) | 28.6 (23.9) | 25.1 (23.6) | 0.006 |
Notes: SD, standard deviation.
Patients with evidence of parathyroidectomy were more likely to have had a concurrent central neck dissection (38.1% vs. 17.5%, p = 0.001). Malignancy was a marginally significant predictor of parathyroidectomy (66.2% vs 53.7%, p = 0.060). Additionally, patients with parathyroidectomy were statistically significantly more likely to have hypocalcemia (46.8% vs. 26.6%, p = 0.002), get a post-operative intact PTH measurement (72.7% vs. 53.7%, p = 0.004), and have a lower PTH value (18.3 ± 21.6 vs 28.6 ± 23.9, p = 0.006).
3.2. Univariable analysis predicting hypocalcemia
In patients with unplanned parathyroidectomy, univariable logistic regression identified PTH value (OR, 0.933; 95% CI, 0.882–0.988; p = 0.017) as the only statistically significant variable (Table 2). Other variables had a p-value of at least 0.25. Therefore, a multivariable logistic regression model was deemed unnecessary.
Table 2.
Univariable analysis to predict hypocalcemia in patients undergoing total thyroidectomy with parathyroidectomy.
| Predictor | Level | Parathyroidectomy (n = 77) |
||
|---|---|---|---|---|
| OR | 95% CI | p-Value | ||
| Age | 0.990 | 0.959–1.023 | 0.554 | |
| Sex | Female | Ref | ||
| Male | 1.166 | 0.385–3.534 | 0.787 | |
| History of hypocalcemia | 0.745 | 0.117–4.729 | 0.756 | |
| Prior neck surgery | 0.424 | 0.077–2.331 | 0.323 | |
| Central neck dissection | 0.994 | 0.397–2.490 | 0.990 | |
| Surgeon experience | < 20 cases | Ref | ||
| 20–60 cases | 0.847 | 0.194–3.693 | 0.752 | |
| > 60 cases | 0.520 | 0.117–2.304 | 0.270 | |
| Pathology | Benign | Ref | ||
| Malignant | 1.037 | 0.402–2.673 | 0.940 | |
| PTH value (n = 56) | 0.933 | 0.882–0.988 | 0.017 | |
3.3. Regression tree
In our sample, regression tree analysis identified the same variable from univariate analysis, PTH value, as the only significant predictor of hypocalcemia. After PTH value, further splitting of the data does not explain enough variance to be relevant in predicting hypocalcemia. A PTH value of 15.5 was found to maximize the decrease in impurity in the terminal nodes of the regression tree and best predict risk of hypocalcemia in our patients.
3.4. Management of hypocalcemia
In patients with parathyroidectomy, univariable analysis identified initial calcium supplementation ≥ 1000 mg (vs none) (OR, 0.16; 95% CI 0.04–0.64; p = 0.01) to significantly decrease risk of hypocalcemia (Fig. 1). Particularly, in patients with parathyroidectomy who had a post-operative PTH ≤ 15, initial calcium supplementation ≥ 1000 mg (vs none) (OR, 0.08; 95% CI, 0.01–0.91; p = 0.042) decreases risk of hypocalcemia (Fig. 2). In contrast, in patients where PTH was not obtained, calcium supplementation did not decrease risk of hypocalcemia (p > 0.05). In this subset, none of the patients with PTH > 15 had an initial calcium supplementation ≥ 1000 mg, though an initial calcium supplementation < 1000 mg (vs none) (OR, 3.19; 95% CI, 0.32–31.77; p = 0.32) did not significantly reduce incidence of hypocalcemia in these patients.
Fig. 1. Probability of hypocalcemia in patients with unplanned parathyroidectomy stratified by amount of initial calcium supplementation.
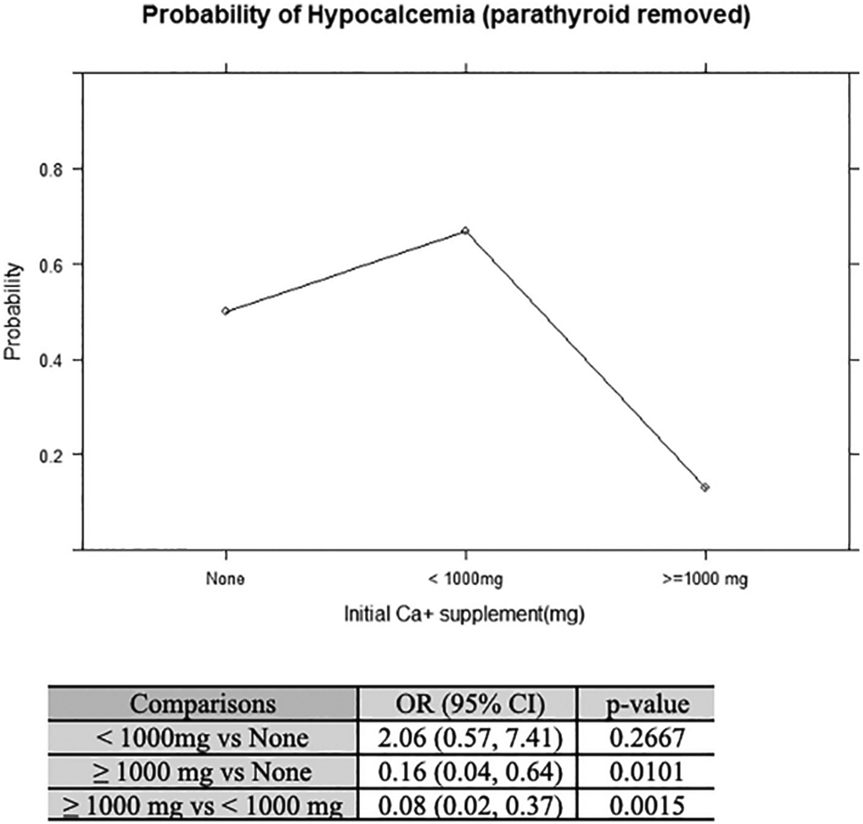
Initial calcium supplementation of ≥1000 mg significantly decreases risk of hypocalcemia compared to initial calcium supplementation of < 1000 mg or no calcium supplementation (p < 0.05).
Fig. 2. Probability of hypocalcemia in patients with unplanned parathyroidectomy stratified by PTH levels.
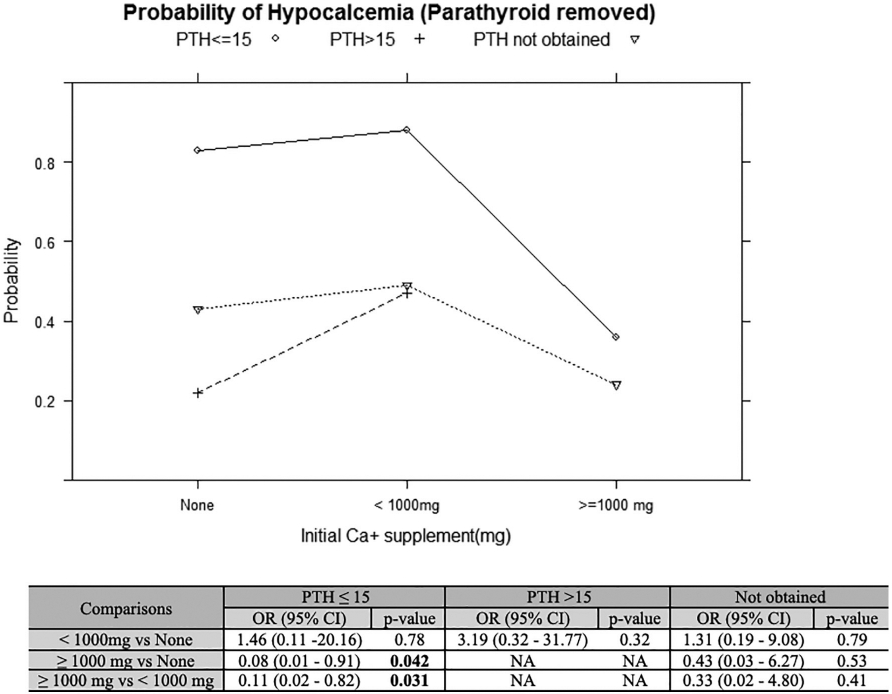
In patients with PTH ≤ 15, initial calcium supplementation of ≥ 1000 mg significantly decreases risk of hypocalcemia compared to initial calcium supplementation of < 1000 mg or no calcium supplementation (p < 0.05). Calcium supplementation in patients with PTH > 15 or PTH not obtained does not alter probability of hypocalcemia.
4. Discussion
To our knowledge, this is the first report to describe the utility of using a postoperative PTH value to predict transient hypocalcemia in patients with unplanned parathyroidectomy and to guide management with appropriate calcium supplementation. We evaluated this approach as an alternative to watchful waiting or immediate presumptive supplementation of all patients without use of laboratory values to guide treatment. Particularly, in patients with unplanned parathyroidectomy, PTH value (p = 0.001) was the only significant predictor of hypocalcemia. In patients with PTH ≤15, initial calcium supplementation ≥ 1000 mg elemental calcium was found to decrease the risk of hypocalcemia (p < 0.05).
Thyroid malignancy, nodal metastasis, and central neck dissection have been previously defined as risk factors for unplanned parathyroidectomy [2-5]. Applewhite et al. showed an odds ratio of 3.88 (95% CI, 2.29–6.58) and 3.50 (95% CI, 1.83–6.72) of developing hypocalcemia in patients with thyroid malignancy and concurrent central neck dissection, respectively [3]. In malignant cases, discerning thyroid and parathyroid tissue can be difficult due to disease extension and loss of normal tissue planes. Additional dissection in patients with malignancy or lymph node metastasis requiring neck dissection increases the risk of inadvertent tampering, devascularization, and removal of parathyroid tissue. In cases with extensive nodal metastasis within the central neck, it may be difficult to separate viable parathyroid tissue from diseased lymph nodes.
In this study, patients with parathyroidectomy were more likely to have post-operative hypocalcemia (p = 0.002) and hypoparathyroidism (p < 0.0005). Previous studies have been inconsistent on the correlation between unplanned parathyroidectomy and resultant hypocalcemia [6,13,14]. Sakorafas et al. found no difference in the incidence of post-operative hypocalcemia between patients with and without incidental parathyroidectomy (21% vs 23%, p = 0.33) in a cohort of 158 patients undergoing thyroid surgery [6]. This study excluded patients with intentional autotransplantation secondary to devascularization of parathyroid tissue, and patients with recurrent disease requiring reoperation. Furthermore, this study included patients who underwent total and subtotal lobectomy whereas our study included both total and completion thyroidectomy cases. In contrast, recent studies with a larger sample size and similar study design to ours have also confirmed that patients with parathyroidectomy were more likely to have hypocalcemia and hypoparathyroidism [5,14,15]. Because this subset of patients is at a significantly increased risk for post-operative hypocalcemia, they are at risk for associated complications related their metabolic derangement the associated treatment required. They may also have an increased length of hospital stay required to manage and treat transient hypocalcemia.
Although the literature addresses the incidence and risk factors for incidental parathyroidectomy or parathyroid autotransplantation, there is minimal data on predictors of hypocalcemia after unplanned parathyroidectomy. In practice, the occurrence of parathyroidectomy during total or completion thyroidectomy place patients in a high-risk category for transient hypocalcemia and one may consider immediate post-operative calcium supplementation prophylactically to prevent complications as well as extended hospital stay. Interestingly, we found that PTH value predicts hypocalcemia in patients with parathyroidectomy after thyroidectomy. Specifically, patients with a PTH value of < 15.5 have a significantly elevated risk of developing hypocalcemia. We found that patients with parathyroidectomy and a PTH < 15 who were initially supplemented with ≥1000 mg of elemental calcium had a significantly decreased risk of post-operative hypocalcemia. Our results suggest identification and treatment of postoperative hypocalcemia guided by PTH value, regardless of the mechanism of parathyroid manipulation or injury.
A systematic review conducted by Alhefdhi et al., found that incidences of post-operative hypocalcemia were 10.1% versus 18.8% for patients supplemented with calcium versus those who had no intervention [12]. The authors highlighted the importance of calcium supplementation for all patients undergoing total thyroidectomy but did not comment on risk of hypercalcemia secondary to routine calcium supplementation in all patients.
One of the key strengths of our study is that it defines a high-risk patient population and standardizes treatment for patients based on rapidly acquired objective data. Standardizing early calcium supplementation can significantly decrease the risk of transient, post-operative hypocalcemia, decrease hospital stay and financial burdens on the patient and the institution, resulting in improved overall outcomes [11,12]. Secondly, this may prevent unnecessary treatment and may reduce the risk of adverse events from calcium supplementation.
The study is limited by the retrospective nature of the data. There is a selection bias in choosing to get a PTH post-operatively. For example, after evaluation of the surgical procedure, comorbidities, and indication for the total thyroidectomy, the surgeon might elect not to get PTH value post-operatively. Therefore, on multivariable analysis we focused on the subset of patients who had post-operative PTH labs (n = 56) to assess PTH value as a predictor of hypocalcemia. Furthermore, there is a selection bias in choosing the amount of initial calcium supplementation post-operatively. Therefore, analysis was done based on initial calcium supplementation only if started before the development of hypocalcemia; this decreases bias and elucidates a more accurate analysis of the direct effect of initial calcium supplementation on subsequent development of hypocalcemia. Finally, due to changing clinical practice over time, many important confounders may not have been accounted for in this sample. Nevertheless, our large sample size and multivariable analysis adjust for important confounders. Based on this institutional data, PTH is currently used post-operatively with standardized calcium supplementation at our institution reducing this bias for future analysis.
5. Conclusion
Patients with unplanned parathyroidectomy during total thyroidectomy or completion surgery are more likely to develop transient hypoparathyroidism and hypocalcemia and are deemed high-risk for such occurrence. Post-operative PTH levels of < 15 predict hypocalcemia and initial supplementation with ≥ 1000 mg of elemental calcium is recommended promptly. This has the potential to decrease length of stay and prevent overtreatment in patients who may have received prophylactic supplementation.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Abbreviations:
- CI
confidence intervals
- OR
odds ratio
- OSUWMC
Ohio State University Wexner Medical Center
- PTH
parathyroid hormone
- SD
standard deviation
Footnotes
Conflict of interest
The authors have no conflict of interest.
Declarations of interest: None.
Presentation: Podium presentation at the Triological Society Combined Sections Meeting, January 18–20th, 2018 in Scottsdale, Arizona, USA.
References
- [1].Manatakis DK, Balalis D, Soulou VN, Korkolis DP, Plataniotis G, Gontikakis E. Incidental parathyroidectomy during total thyroidectomy: risk factors and consequences. Int J Endocrinol 2016;2016:7825305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Ozemir IA, Buldanli MZ, Yener O, et al. Factors affecting postoperative hypocalcemia after thyroid surgery: importance of incidental parathyroidectomy. North Clin of Istanb 2016;3:9–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Applewhite MK, White MG, Xiong M, et al. Incidence, risk factors, and clinical outcomes of incidental parathyroidectomy during thyroid surgery. Ann Surg Oncol 2016;23:4310–5. [DOI] [PubMed] [Google Scholar]
- [4].Hone RW, Tikka T, Kaleva AI, et al. Analysis of the incidence and factors predictive of inadvertent parathyroidectomy during thyroid surgery. J Laryngol Otol 2016;130:669–73. [DOI] [PubMed] [Google Scholar]
- [5].Ozogul B, Nuran Akcay M, Kisaoglu A, Atamanalp SS, Ozturk G, Aydinli B. Incidental parathyroidectomy during thyroid surgery: risk factors, incidence, and outcomes. Turk J Med Sci 2014;44:84–8. [PubMed] [Google Scholar]
- [6].Sakorafas GH, Stafyla V, Bramis C, Kotsifopoulos N, Kolettis T, Kassaras G. Incidental parathyroidectomy during thyroid surgery: an underappreciated complication of thyroidectomy. World J Surg 2005;29:1539–43. [DOI] [PubMed] [Google Scholar]
- [7].Barczynski M, Konturek A, Stopa M, Cichon S, Richter P, Nowak W. Total thyroidectomy for benign thyroid disease: is it really worthwhile? Ann Surg 2011;254:724–9. [DOI] [PubMed] [Google Scholar]
- [8].Friedman M, Vidyasagar R, Bliznikas D, Joseph NJ. Intraoperative intact parathyroid hormone level monitoring as a guide to parathyroid reimplantation after thryoidectomy. Laryngoscope 2005;115(1):34–8. [DOI] [PubMed] [Google Scholar]
- [9].Lo CY, Tam SC. Parathyroid autotransplantation durign thyroidectomy. Arch Surg 2001;136:1381–5. [DOI] [PubMed] [Google Scholar]
- [10].El-Sharaky MI, Kahalil MR, Sharaky O, et al. Assessment of parathyroid autotransplantation for preservation of parathyroid function after total thyroidectomy. Head Neck 2003;25:799–807. [DOI] [PubMed] [Google Scholar]
- [11].Stedman T, Chew P, Truran P, Lim CB, Balasubramanian SP. Modification, validation and implementation of a protocol for post-thyroidectomy hypocalcaemia. Ann R Coll Surg Engl 2017:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Alhefdhi A, Mazeh H, Chen H. Role of postoperative vitamin D and/or calcium routine supplementation in preventing hypocalcemia after thyroidectomy: a systematic review and meta-analysis. Oncologist 2013;18:533–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Tartaglia F, Blasi S, Giuliani A, et al. Parathyroid autotransplantation during total thyroidectomy. Results of a retrospective study. Int J Surg 2016;28(Suppl. 1):S79–83. [DOI] [PubMed] [Google Scholar]
- [14].Lin YS, Hsueh C, Wu HY, Yu MC, Chao TC. Incidental parathyroidectomy during thyroidectomy increases the risk of postoperative hypocalcemia. Laryngoscope 2017;127:2194–200. [DOI] [PubMed] [Google Scholar]
- [15].Edafe O, Antakia R, Laskar N, Uttley L, Balasubramanian SP. Systematic review and meta-analysis of predictors of post-thyroidectomy hypocalcaemia. Br J Surg 2014;101:307–20. [DOI] [PubMed] [Google Scholar]


