Abstract
Benign mesenchymal odontogenic tumors are lesions derived from the mesenchymal components of the tooth-forming apparatus and are consequently found within the jawbone. Benign fibro-osseous tumors are part of this category of lesions in which normal bone is substituted, initially by fibrous tissue and within time become infiltrated by osteoid and cementoid elements. They are asymptomatic, slow-growing lesions and remain undiagnosed until swelling of the face becomes prominent and they share similar radiological characteristics. Herein, we report three cases of ossifying fibroma, cemento-osseous fibroma and periapical cemento-osseous dysplasia and analyze all the correlating factors, clinical history, radiological and histological features, intraoperative appearance, and treatment with a 3-year follow-up period. Despite the advances in the identification of these pathologies, clinicians still face difficulties in their classification and the diagnosis due to overlap in both histological and radiographic findings. An accurate final diagnosis is essential for appropriate treatment and an informative prognosis.
Keywords: Benign fibroosseous lesions, cemento-osseous fibroma, jawbones, mesenchymal, odontogenic tumors, ossifying fibroma, periapical cemento-osseous dysplasia
INTRODUCTION
Benign mesenchymal odontogenic tumors are derived from the mesenchymal elements of the tooth-forming apparatus and are consequently found within the jawbone or soft tissue overlying teeth. Benign fibro-osseous lesions (BFOLs) are part of these lesions.[1] BFOLs of the jawbones are illustrated by the replacement of normal bone with fibrous connective tissue.[2,3] They are a modified group of intraosseous benign bone tumors that share histological features.[1,2,3,4] BFOL of the craniofacial bones involves pathologic heterogeneous ossifications and calcifications in association with a collagenous stroma rich with fibroblastic elements.[1,2] The clinical appearances and the radiological images are challenging, although the final diagnosis is based on histology.[3]
Fibrous dysplasia (FD), ossifying fibroma (OF), desmoplastic fibroma (DF), periapical cemento-osseous dysplasia (PCOP) and cemento-osseous fibroma (COF) are classified as major forms of BFOLs. COF and PCOD are limited to the tooth-bearing areas, OF and DF are benign tumors of the craniofacial region, and FD is often found in the jawbones.[1]
Although the lesions share some histological findings, they have different clinical and radiological appearances, thus they are treated in different ways.[1,2,3,4]
The objective of this paper is to describe three clinical cases of fibrous osseous lesions OF, COF and PCOP with the clinical, radiological and histological findings and to discuss the diagnosis analysis and treatment modalities adopted.
CASE REPORTS
Case 1
A 34-year-old female patient with no pathological history of interest was referred to our department by her dentist for implant placement to restore her first mandibular right molar extracted 2 months ago.
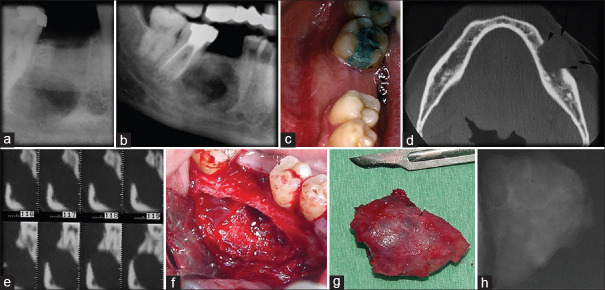
The intraoral radiograph showed the non-healed alveolar bone of the extracted molar along with a radiolucency image of the apical area [Figure 1a].
Figure 1.
(a) Intra-oral radiograph showing the radiolucency of the lesion and alveolar bone of the extracted molar. (b) Two-dimensional panoramic at 3 months revealed a well-demarcated unilocular mixed lesion: the center of the lesion was radiolucent, and the edge was more radiopaque. (c) swelling of the vestibular cortex of the mandible. (d) Axial image of computed tomography scan showed an alteration of the continuity of the cortical buccal bone was observed, and the lesion was extended to surrounding the soft tissue. (e) Para-axial image revealed that the lesion displaced the mandibular canal toward the basilar border of the mandible. (f) Surgical site after excision of the lesion. (g) The specimen. (h) X-ray of the lesion showing the calcification inside the lesion
Three months later, a two-dimensional (2D) panoramic radiograph revealed a well-demarcated unilocular mixed lesion with a radiolucent center, a relatively more radiopaque edge in comparison with the body of the mandible and a healed alveolar bone of the extracted molars [Figure 1b].
On clinical examination, an approximately 2 cm painless, hard, bulge of the vestibular cortex of the mandible was observed between the right second molar and second premolar. The appearance of the gum that covered it was normal [Figure 1c].
In computed tomography (CT) scan, the axial images showed an alteration of the continuity of the cortical buccal bone and the lesion was extending to the surrounding soft tissue [Figure 1d]. The para-axial images revealed that the lesion displaced the mandibular canal toward the basilar border of the mandible [Figure 1e].
Post discussion with the patient and after she signed the consent form, a surgical biopsy was decided on as the next step in the management. The differential diagnosis was in favor of a fibro-osseous lesion.
Under loco-regional analgesia, total excision of the bony lesion was performed. Its consistency was soft, and the X-ray revealed fibrous tissue with some calcifications [Figure 1f-h].
The histological examination of the lesion showed a highly cellular fibroblastic stoma along with a mineralized tissue similar to bone of various sizes randomly distributed. The histological diagnosis was in favor of an of [Figure 2a]. No signs of malignancy were evident in any of the remitted fragments.
Figure 2.
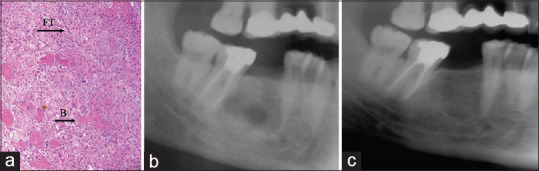
(a) H&E, ×10 showing a highly cellular fibroblastic tissue (FT), and a mineralized tissue similar to the bone of various sizes (B), (b) Cropped panoramic radiograph at one year, (c) cropped panoramic radiograph 3 years later
The patient was followed closely for 6 months, and bone healing was achieved one year later. A panoramic radiograph 3 years later revealed stabilization of bone healing. To note that the patient refused to undergo implant placement, she still has a removable prosthesis [Figure 2b and c].
Case 2
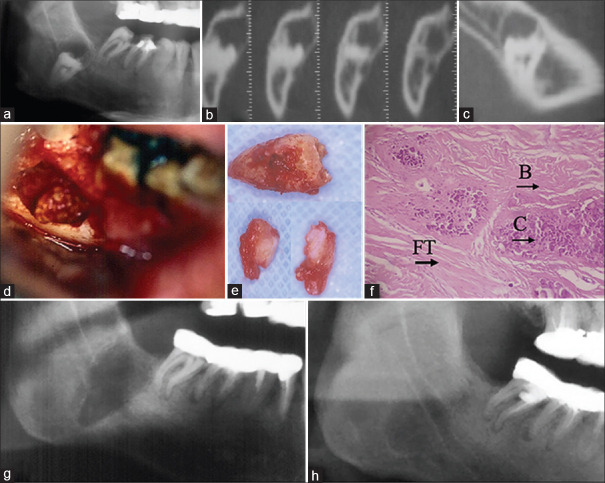
A 31-year-old male patient was referred to our department by his general dentist for extraction of impacted mandibular right third molar before crown placement on the same side. A 2D panoramic radiograph revealed an impacted third molar that was displaced toward the border of the mandible and the crown showed a well-demarcated unilocular lesion [Figure 3a]. The para-axial images of the CT scan demonstrated a displaced third molar, completely surrounded by bone. Coronally, a radiolucent image is reported without any cortical discontinuities [Figure 3b]. Sagittal reconstruction image of the CT scan showed that the mandibular canal was in a lingual position [Figure 3c].
Figure 3.
(a) Cropped panoramic radiograph revealed that the impacted third molar was displaced toward the border of the mandible and the crown showed a well-demarcated unilocular lesion. (b) Para-axial images of the computed tomography scan showed that the displaced third molar was completely surrounded by bone and coronally a radiolucent image exists without any cortical discontinuities. (c) Sagittal reconstruction image of the computed tomography scan showed that the mandibular canal was in a lingual position. (d) Surgical site. (e) The lesion with a fibrous consistency and the retained removed tooth. (f) Histology H&E, ×10 of the lesion showed a cellular fibrous tissue, woven or lamellar bone with varying amounts of mineralized material look like bone (B) and cementum (C). (g) Cropped panoramic X-ray one year later. (h) Cropped panoramic three years later showing the complete bone healing
The surgical extraction of the impacted molar along with the excision of the associated lesion represents the treatment plan proposed to the patient. After the agreement, a consent form was signed before the surgery.
The differential diagnosis included a dentigerous cyst and a fibro-osseous lesion.
Under loco-regional analgesia, surgical extraction was done buccally. First, the lesion with a noted fibrous consistency was excised, then the retained tooth was removed [Figures 3d and e]. The histology of the lesion displayed cellular fibrous tissue and woven or lamellar bone with varying amounts of mineralized material that look like bone and cementum. Thus, the histological diagnosis was in favor of a cement-osseous fibroma [Figure 3f].
A 2D-panoramic x-ray at the 1-year and 3-year follow-up showed complete bone healing, and the trajectory of the mandibular canal was well-delineated [Figure 3g and h].
Case 3
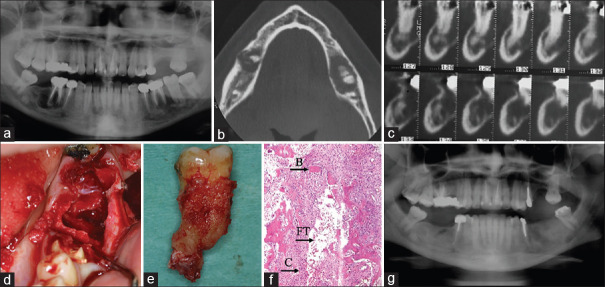
A 33-year-old female presented to our department with moderate bilateral mandibular swelling and mobility of teeth 36, 37 and 46 with deep periodontal pockets. Her medical history was nonrevealing she had no systemic diseases recorded.
A 2D panoramic radiograph showed that 36 and 46 had been devitalized and restored with crowns. Mixed lesions composed of radicular radiolucency associated with radiopacity surrounding the root apices of the teeth 36, 37 and 46 were noted [Figure 4a].
Figure 4.
(a) Panoramic X-ray revealing a mixed lesion composed of radicular radiolucency associated with radiopacity surrounding the root apices of the teeth 36, 37 and 46. (b) Axial image of the computed tomography scan showed no alteration of the continuity of the mandibular cortical bone and the presence of radiolucency lesions surrounding radiopaque elements. (c) Para-axial images revealing mixed radiolucency-radiopaque lesions apically to the tooth and the mandibular canal was displaced toward the mandibular border. (d and e) The surgical site with the extracted molar with calcification related to the apices. (f) H&E, ×10 revealed a stroma composed of spindle-shaped fibroblastic cells (FT) with a collagenous formation associated with mineralized calcifications similar to bone (B) and cement (C). (g) The two-dimensional panoramic X-ray showed a complete mandibular bone healing on both sides after 3 years
The axial image of the CT scan showed no alteration of the continuity of the mandibular cortical bone along with the presence of radiolucency lesions surrounding radiopaque elements [Figure 4b]. Para-axial images revealed mixed radiolucency-radiopaque lesions apically to the tooth and the mandibular canal was displaced toward the mandibular border [Figure 4c].
Clinical findings and radiographical images favored a diagnosis of periapical rarefying osteitis. The treatment plan proposed and accepted by the patient was teeth extraction with excision of the lesion for histopathological examination.
A consent form was signed, and the surgical procedure was performed under loco-regional analgesia [Figure 4d and e].
The histopathological examination revealed a stroma composed of spindle-shaped fibroblastic cells with a collagenous formation associated with mineralized calcifications similar to bone and cement [Figure 4f]. The patient was followed monthly. The 2D panoramic X-ray showed complete mandibular bone healing on both sides after 3 years postprocedure [Figure 4g].
DISCUSSION
BFOLs are a category of lesions characterized by an initial replacement of normal bone with fibrous tissue. Over a period of time, the lesions become infiltrated with osteoid and cementoid elements. They represent a particularly challenging group of pathologies for clinicians.
A useful approach to the definitive diagnosis of BFOLs requires analysis of all the correlating factors including, but not limited to, the clinical history, the radiological findings, the intraoperative appearance of the lesion, and most importantly, the histological examination of the specimen. The accuracy of the final diagnosis is necessary for proper treatment and an informative prognosis.
OF, COF and PCOD are classified as and behave like, a benign mesenchymal tumor subclassified as fibro-osseous lesions with the exception of COF which is considered a reactive process.[1,5]
OFs and PCODs disturb the jaws and bones of the craniofacial region, while COF is only allied with tooth-bearing areas of the jawbones and possibly originating within the periodontal ligament.[1] They appear in both jaws but more frequently arise in the mandible, especially the molar–premolar region.[6,7,8,9,10,11,12]
Most of these disorders are asymptomatic and are characterized by slow-growing lesions. Hence, they remain unrecognized and undiagnosed until swelling of the face becomes prominent, prompting the patient to seek care.[1,5,8,9,10,13]
OF and PCOD are observed in women more frequently than men,[11,12,14] while no sex prediction is seen in COF.[8] PCODs are described in both focal and florid types and the incidence of the familial type is very rare.[11]
Radiologically, on both panoramic radiographs and CT, these lesions are usually unilocular, well-circumscribed radiolucent lesions of bone with a well-delineated radiopaque edge. As they progress, they appear as mixed lesions with radiolucent and radiopaque areas.[2,9,11,13,14]
The three cases illustrated in the following report involve the mandible, are asymptomatic and their radiological appearances reflect the known descriptions of a unilocular and well-circumscribed mixed lesion with a well-demarcated border.
The mature lesions are radiopaque and delineated by a thin radiolucent border representing the fibrous interface separating pathological bone from adjacent normal bone. The calcifications displayed in the radiological images could be cementum-like or bone-like spherules.[2,8,9,11,13,14]
In the early stage of PCOD, radiolucency is noted at the root apex, it can be misdiagnosed as apical periodontitis and is associated with vital teeth, usually without any clinical sign or complaint.[11]
The lesions are treated with curettage or surgical excision depending on the size and location and recurrences are rarely observed.[3,6,7,14]
Histologically, they are composed of highly cellular fibroblastic stoma and a mineralized tissue comparable to bone, cementum or both.[6,7,8,11,12]
All the presented cases were treated by surgical excision and no recurrence was observed during 3-year follow-up period. To note, the first case was misdiagnosed initially due to the complexity of the lesions.
CONCLUSION
Despite the advances in the identification of these pathologies, clinicians still face difficulties in the classification, diagnosis, and managing of these lesions, in part due to the histological and radiographic similarities. Correlation between the biological behavior of the lesion and the collected clinical, radiological and histopathological data is crucial in order to reach a precise diagnosis which is primordial to choose the appropriate therapeutic action.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient (s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initial s will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.MacDonald DS. Classification and nomenclature of fibro-osseous lesions. Oral Surg Oral Med Oral Pathol Oral Radiol. 2021;131:385–9. doi: 10.1016/j.oooo.2020.12.004. [DOI] [PubMed] [Google Scholar]
- 2.Nelson BL, Phillips BJ. Benign fibro-osseous lesions of the head and neck. Head Neck Pathol. 2019;13:466–75. doi: 10.1007/s12105-018-0992-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mainville GN, Turgeon DP, Kauzman A. Diagnosis and management of benign fibro-osseous lesions of the jaws: A current review for the dental clinician. Oral Dis. 2017;23:440–50. doi: 10.1111/odi.12531. [DOI] [PubMed] [Google Scholar]
- 4.Eversole R, Su L, ElMofty S. Benign fibro-osseous lesions of the craniofacial complex. A review. Head Neck Pathol. 2008;2:177–202. doi: 10.1007/s12105-008-0057-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wright JM, Vered M. Update from the 4th Edition of the World Health Organization classification of head and neck tumours: Odontogenic and maxillofacial bone tumors. Head Neck Pathol. 2017;11:68–77. doi: 10.1007/s12105-017-0794-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Triantafillidou K, Venetis G, Karakinaris G, Iordanidis F. Ossifying fibroma of the jaws: A clinical study of 14 cases and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114:193–9. doi: 10.1016/j.tripleo.2011.07.033. [DOI] [PubMed] [Google Scholar]
- 7.Wang TT, Zhang R, Wang L, Chen Y, Dong Q, Li TJ. Two cases of multiple ossifying fibromas in the jaws. Diagn Pathol. 2014;9:75. doi: 10.1186/1746-1596-9-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sopta J, Dražić R, Tulić G, Mijucić V, Tepavčević Z. Cemento-ossifying fibroma of jaws-correlation of clinical and pathological findings. Clin Oral Investig. 2011;15:201–7. doi: 10.1007/s00784-010-0381-2. [DOI] [PubMed] [Google Scholar]
- 9.Bala TK, Soni S, Dayal P, Ghosh I. Cemento-ossifying fibroma of the mandible. A clinicopathological report. Saudi Med J. 2017;38:541–5. doi: 10.15537/smj.2017.5.15643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Katti G, Khan MM, Chaubey SS, Amena M. Cemento-ossifying fibroma of the jaw. BMJ Case Rep. 2016;2016:bcr2015214327. doi: 10.1136/bcr-2015-214327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shibata N, Inamoto K, Naitoh M, Ariji E. Clinical assessment of cemento-osseous dysplasia based on three-dimensional diagnostic imaging: A case report. Aust Endod J. 2021;47:105–12. doi: 10.1111/aej.12488. [DOI] [PubMed] [Google Scholar]
- 12.Brody A, Zalatnai A, Csomo K, Belik A, Dobo-Nagy C. Difficulties in the diagnosis of periapical translucencies and in the classification of cemento-osseous dysplasia. BMC Oral Health. 2019;19:139. doi: 10.1186/s12903-019-0843-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cavalcanti PH, Nascimento EH, Pontual ML, Pontual AD, Marcelos PG, Perez DE, et al. Cemento-osseous dysplasias: Imaging features based on cone beam computed tomography scans. Braz Dent J. 2018;29:99–104. doi: 10.1590/0103-6440201801621. [DOI] [PubMed] [Google Scholar]
- 14.MacDonald-Jankowski DS. Ossifying fibroma: A systematic review. Dentomaxillofac Radiol. 2009;38:495–513. doi: 10.1259/dmfr/70933621. [DOI] [PubMed] [Google Scholar]