Abstract
Odontomas are the most common odontogenic benign tumors categorized as hamartomas. Odontoma is primarily made up of enamel and dentin, although it may also contain cementum and pulp tissue in various forms. It is known for having slow-growth and non-aggressive nature. It is made up of either dental tissues categorized as a complex or a compound odontoma based on radiological and histological characteristics. Complex odontomas are less prevalent among them, and they usually show as a tiny, silent radiopaque mass enclosed by a radiolucent border, seen on routine radiographic examinations. To avoid tooth eruption disturbances and additional clinical problems, odontomas should be managed and surgically removed once they have been detected. The present study describe a rare case of giant complex odontoma in the posterior mandible with an unusual dimension in a 16-year-old Iranian female patient referred to the Department of Oral and Maxillofacial, Mashhad Dental School, Mashhad, Iran, in May 2021. The case was effectively treated with surgical curettage and tumor enucleation, emphasizing the significance of early detection to minimize complications. Additionally, the clinical, radiological, and histopathological aspects and probable surgical treatments were discussed.
Key Words: Odontogenic tumors, Odontoma, Mandible, Tooth eruption, Curettage
INTRODUCTION
Odontomas are the most frequent odontogenic tumors of the jaw1-5. These lesions account for 22% of all odontogenic tumors2, 4, 6, 7. They are formed from epithelial and ectomesenchymal components of the dental apparatus and contribute to the formation of dentin and enamel and are thought to be hamartoma rather than an actual neoplasm5, 7-9. The etiology of odontomas is still unclear. It has been linked to various clinical situations such as trauma, infection, inherited diseases (like Gardner’s syndrome), and gene mutations8, 10, 11. Odontomas are benign tumors that usually appear in the second decade of life and have no gender preference4, 12-14.
Odontomas are categorized as complex or compound tumors according to the WHO, which published its classification of odontogenic tumors in Jan 20173, 15. To distinguish these two types, the appearance of tooth-like features or the disordered mass of dental tissue is used5. In compound Odontoma, enamel, dentin, and pulp are all normally organized and enclosed in follicular connective tissue like a normal tooth1, 10. However, the complex type appears with various densities and it is unidentifiable as dental structures5, 10.
Notably, odontomas are usually slow-growing and painless intra-bony lesions5, 16. They are normally asymptomatic, only found by chance in radiographic tests obtained in conjunction with impacted teeth, or when they become exposed in the oral cavity via perforating the mucosa8, 16. Compound odontomas usually affect the anterior maxilla, whereas complex odontomas mainly affect the posterior mandible defined by a chaotic mass of dental tissues1, 5. Complex and compound odontomas include some radiographic differential diagnoses; the complex type appears as a calcified mass with radio-density of tooth structures and a thin radiolucent zone5. Compound odontoma, on the other hand, has a radiopaque look with uneven borders and a radiolucent zone containing numerous, tiny, calcified structures that resemble natural teeth4. To avoid tooth eruption abnormalities, early detection and surgical removal of these hamartomas are recommended2.
The majority of odontomas are found to be between 1 and 2 cm in diameter, with those greater than 3 cm being referred to as giant odontomas4, 17. Giant complex odontoma is a rare disorder8, 10, 17. To the best of our knowledge, no published reports discussed a case of giant complex Odontoma in the equal or more massive size of our case in Iran. Thus, the purpose of this study was to represent a rare case of a giant mandible complex odontoma in a 16-year-old Iranian female patient. Additionally, the clinical, radiological, and histological characteristics of the tumor were discussed, as well as the possibility of systemic disorders and the chosen therapy strategy.
CASE PRESENTATION
A 16-year-old female was referred to the Department of Oral and Maxillofacial, Mashhad Dental School, Mashhad, Iran, in May 2021 due to suffering from excessive pressure and pain sensation in the area of the right posterior mandible. The patient had no history of systemic diseases and her laboratory tests revealed no abnormal changes and no history of blood or pus from the lesion was noted. Extra-oral clinical examination did not indicate any signs of inflammation or cervical lymphadenopathy. At the intraoral clinical examination, a well-defined erythematous swelling was noted in the right side of the mandibular vestibule and the lesion showed itself as a rhomboidal calcified mass. Moreover, there was a free edentulous space beyond the first molar (Figure 1).
Fig. 1.
Pre-operative clinical examination of the lesion
In the panoramic radiograph, the presence of an amorphous, radio-opaque mass was detected measuring approximately 4.5×4 cm surrounded by a radiolucent rim with obliteration of inferior border of the mandible. Moreover, the lesion had caused the mesial movement of right lower first molar, along with a hard osseous expansion in the inferior alveolar nerve (IAN) area of the right posterior mandible. The giant mass was over the erupting pathway of an unerupted second molar tooth with mesioangular impaction (Figure 2). Cone-beam computed tomography (CBCT) images were beneficial in showing the extensiveness and the invasion of the tumor. Furthermore, 3D reconstruction indicates a better three-dimensional understanding of the lesion, being more accurate to the vastness and involvement of adjacent anatomical structures, which facilitates the treatment planning (Figure 2).
Fig. 2.
Panoramic radiograph and CBCT scan of the lesion
The diagnosis of complex odontoma was confirmed for this case, based on the clinical, radiographic discoveries, and an incisional biopsy (under local anesthesia) report.
Upon obtaining informed consent and explaining the surgical planning and the lesion type to the patient in compliance with the ethical code of Mashhad University of Medical Sciences, Mashhad, Iran (IR.MUMS.REC.1400.177), a second surgical procedure was performed under general anesthesia.
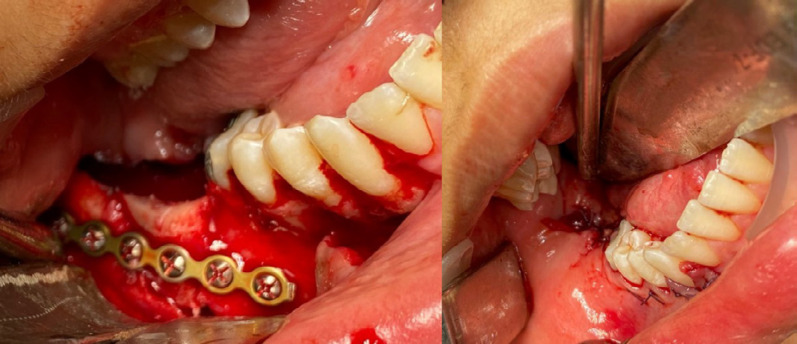
Briefly, for total lesion excision, a vestibular incision was made in the lower right vestibule fundus to access the lesion, and then a mucoperiosteal flap was elevated to access the massive tumor (Figure 3). Performing complete curettage of the odontoma added to the enucleation procedure, the massive lesion (4.5 × 4 cm) was divided into smaller pieces by using the surgical bur and osteotome. Then, the tumor was completely removed. The impacted lower right second molar was also extracted. Surgically removed mass shows a chaotic mass of calcification as well as surrounding soft tissues (Figure 3). Afterward, the reconstruction of the affected area of posterior mandible with a monocortical anterior iliac bone graft was performed (Figure 4). An iliac block bone was fixed in position with a mini-plate and 6 mini-screws. The maxillomandibular fixation (MMF) was carried out using IMF screws and wires. Finally, the mandibular mucosal flap was sutured using Vicryl 3.0 suture (Vicryl, Ethicon, Johnson and Johnson, UK) with no tension (Figure 4).
Fig. 3.
a) View of the tumor extensiveness, b) Tumor enucleation and curettage, c) Macroscopic view of the tumor mass
Fig. 4.
Surgical Reconstruction of the defect with the iliac bone graft and tension-free closure of the soft tissue flap
Afterward, the mass was submitted for a thorough histopathological examination using H&E staining. Under light microscope evaluation with the magnification of 200 X, the sections showed an irregular arrangement of dental tissues such as tubular dentin, cementoid areas, enamel matrix, and pulp-like connective tissue in a matrix of collagen fibers with blood vessels. During decalcification, the enamel tissues were dissected (Figures 5-a, 5-b). These findings confirmed the primary diagnosis.
Fig. 5 a,b.
Histopathology View of the tumor (200X Magnification under Microscope (Lambred, American)); D: dentin, P: pulp cavity, C: cementoid, DE: dissolved enamel, Preparing a photograph of the desired areas in the slides by a HP microscope equipped with a camera. (Canon,650D)
Interestingly, after the surgical procedure patient did not experience walking difficulties, an impaired sensation of iliac skin, or mental nerve paresthesia. The post-operative radiographic view was shown in Figure 6. The maxillomandibular fixation (MMF) was removed after one month, postoperatively.
The post-operative period was uneventful and the patient completed a six-month follow-up without any signs of tumor recurrence and no operative complications or infection was detected in the follow-up sessions.
DISCUSSION
Odontogenic tumors of the jaw are a group of lesions that originate from remnants of epithelium or ectomesenchyme associated with teeth development and ranges from hamartomas to real tumors1.Odontogenic tumors are classified as benign or malignant in the fourth edition of the WHO histological classification system15. They are then categorized as epithelial, ectomesenchymal, or mixed cells, depending on the cell of origin15.
Odontomas are the most frequent common odontogenic tumors, which constitute about 22% of all these neoplasms1-5, 10, 12, 16. They are classified as tumor-like malformations (hamartomas) made up of hard and soft dental tissues, enamel, and dentine, with varying amounts of pulp and cement2, 3, 12.Paul Broca created the term “odontoma” in 1867, and it was first used to designate any odontogenic tumor or tumor-like disorder2, 9, 18. The terminology of odontoma has changed over time because of new findings, and since 2017, it has been classified by WHO as a group of benign mixed odontogenic tumors constitute of both epithelial and mesenchymal tissues along with ameloblastic fibro-Odontoma, which is thought to be an immature originator of complex Odontoma3, 10, 12, 15.
Regarding WHO classification based on the radiographic features and tumor gross, compound and complex odontomas are described3, 10, 12, 15. Mixed odontomas are a form of odontoma that combines the characteristics of a compound and complex odontomas12, 19. Compound odontomas are tooth-like structures with pulp tissue in the core, dentin shells around them, and enamel components partially covering them. However, complex odontomas are clumped masses of dentin, enamel, enamel matrix, pulp tissue, and cementum that lack normal organization2. The prevalence of compound Odontoma is twofold of the complex type3, 7, 12. Although odontomas can occur everywhere in the dental arches, the canine and incisor portions of the maxillary arch show more compound odontomas, but the posterior parts, notably the mandible, show the most complex odontomas4, 14, 17.
The etiology of these tumors is still unrevealed2-4, 12. Local trauma, inflammatory processes, and chronic infections have all been identified as possible variables during ontogenesis in several studies. Other possible causes include genetic backgrounds, such as odontoblastic hyperactivity, or inherited syndromes like Gardner’s and Hermann’s syndrome12, 14, 15.
Odontoma can develop at any age, but it is mostly diagnosed in the second decade of life2, 4, 20. Moreover, it peaks around the age of 1412. Our patient was a 16-year-old girl. There was no gender predisposition4, 12, 14. In contrast, it is slightly more common in women1, 5, 21.
Odontomas present as tiny, asymptomatic lesions, and in the majority of patients, X-ray findings account for more than half of the cases2, 8, 13. In particular, our case was accidentally diagnosed by her CBCT and panoramic radiographs. Cases of odontomas that are greater than 3 cm are referred to as giant odontomas4. Hardly, any published reports have been found about giant complex odontomas in the posterior mandible in Iran since 5 years ago. A thorough literature review of several cases of giant complex odontoma of the mandible in the world was summarized (Table 1).
Table 1.
A summary of Giant complex odontoma in mandible from 2017 to 2021
| Authors/Reference | Year | Case (Age/sex) | Signs and symptoms | Impacted Teeth |
Tumor
Size(cm) |
Surgical treatment | Follow-up |
|---|---|---|---|---|---|---|---|
| Ladani et al. 7 | 2017 | 22/female | pain and swelling | Second lower molar | 2 x 4 | tumor excision- closure of surgical site | 4-month Completed- good bone formation |
| Akerzoul et al. 14 | 2017 | 35/male | swelling | none | 6 x 6 | Enucleation | One month Completed |
| Park et al. 17 | 2018 | 28/female | pain | Third lower molar | 3× 2.5 ×2 | Enucleation- left iliac bone grafts | Completed-no major complications |
| Niazmand et al. 11 | 2019 | 18/female | none | Second lower molar | 5 × 1 | Surgical resection | Completed, unevenful |
| Kumar et al. 9 | 2019 | 40/female | swelling | Second lower molar | 2 x 2 | Enucleation | unknown |
| Saravanan et al. 21 | 2019 | 12/female | swelling | Second lower molar | 4 x 3 | Partial tumor excision | Completed- without any recurrence. |
| Bueno et al. 10 | 2020 | 42/male | limitation of mouth opening and asymptomatic swelling | none | unknown | Enucleation and curettage | unknown |
| Unni et al. 13 | 2020 | 26/male | Pain and swelling | Third lower molar | 5 × 5 × 4 | tumor excision | 3-month Completed- persistence of paresthesia |
| Adhikari et al. 16 | 2021 | 8/female | swelling | Second lower molar | 2.5 x 2.5 | Surgical excision | unknown |
| Aschaitrakool et al. 22 | 2021 | 19/female | swelling | Third lower molar | 4 x 3 | Enucleation-reconstruction plate | 12-month Completed- no pain or paresthesia |
Giant odontomas can result in cortical bone expansion with facial asymmetry and swelling, as well as pain, limited mouth opening, and tooth dislocation4, 10, 23, 24. Conservative surgical excision is considered the appropriate surgical approach to remove the possibility of recurrence and the need for bone reconstruction should be regarded based upon clinical and radiographic features of the lesion10, 17, 26. Total excision of the tumor known as enucleation, curettage with removing 1-2 mm of surrounding bone, resection of the jaw due to the mass expansion as well as reconstruction of the mandible by bone grafts could be possible treatment strategies17, 27.
Complex odontoma is a calcified irregular mass encircled by a thin radiolucent zone with a smooth outer border2-5. They are made up of haphazard assemblages of dentin, enamel, enamel matrix, cementum, and pulp tissue2, 4. As a result, the internal material has no tooth morphology4. Histological examination of the case confirmed the mentioned features.
Radiographically, the appearance of a complex odontoma is determined by the tumor development stage and the degree of mineralization. The initial staging is radiolucent due to the absence of calcification. Partial mineralization is noticed in the second or middle stage. In the next stage, the lesion emerges radiopaque, with an amorphous concentration of dental hard tissue encircled by a narrow radiolucent rim3, 5, 6, 9, 10. According to the X-ray assessment of our patient, the third stage seemed to be verifiable.
The adjacent affected permanent tooth may resorb because of the odontoma enlargement. It is more difficult to save impacted teeth in patients with older ages, bigger odontomas, and longer medical backgrounds3. Therefore, early diagnosis and treatment are recommended likewise the current case.
This condition is most common throughout adolescence, and parents and maxillofacial specialists should pay close attention if they notice unilateral deciduous teeth retention, permanent teeth lack, or tooth shifting, even if there is swelling or pain. Odontomas can be removed at an early stage, giving the affected teeth and tumor a better prognosis3.
CONCLUSION
This research has improved the knowledge of clinical and radiographic characteristics of complex odontomas. Early detection via panoramic radiography and clinical assessments and then surgical management of odontomas followed by meticulous follow-up are critical for eliminating eruption problems especially in extensive cases and avoiding later pathological complications. Complex odontomas are odontogenic tumors that are usually asymptomatic, are commonly discovered by chance in routine radiographic examinations, and usually are not linked to other illnesses. Nevertheless, large lesions can cause the jaws’ cortical plates to expand, resulting in facial asymmetry. As the onset of the tumor coincidence with the age of puberty, parents, and dentists should pay more attention to susceptible cases. To avoid complications such as the delayed eruption of the permanent teeth, over-retention, or possibility of tumor relapse, timely diagnosis as well as surgical enucleation followed by curettage are strongly recommended.
FUNDING
None. This study was self-funded.
CONFLICTING INTEREST
None.
ACKNOWLEDGMENTS
The authors gratefully acknowledge the assistance and financial support of Mashhad University of Medical Sciences and Student Research Committee of Mashhad University of Medical Sciences.
References
- 1.Labib A, Adlard RE. Tumors of The Jaws. 2021 Jul 17. In: StatPearls [Internet] Treasure Island (FL) StatPearls Publishing; 2021. [Google Scholar]
- 2.Sharifi Rayeni A, Samieirad S, Mianbandi V, Saghravanian N, Tohidi E. A rare case of maxillary compound odontoma with an unusual large number of denticles. JDMT. 2019;8(2):101–6. [Google Scholar]
- 3.Zhuoying C, Fengguo Y. Huge erupted complex odontoma in maxilla. Oral Maxillofac Surg Cases. 2019;5(1):100096. [Google Scholar]
- 4.Van HA, Nguyen TT, Vo NQ, Vo TH, Chansomphou V, Pham NT, Trinh CT, Aiuto R. Giant compound odontoma of the mandible in an adolescent. J Pediatr Surg Case Rep. 2021;65:101755. [Google Scholar]
- 5.Rajendra Santosh AB, Ogle OE. Odontogenic Tumors. Dent Clin North Am. 2020;64(1):121–138. doi: 10.1016/j.cden.2019.08.008. [DOI] [PubMed] [Google Scholar]
- 6.Lekshmy J, Padmashree S, Pandeshwar P. Unerupted Complex Odontoma of the Posterior Mandible: A case report. Int J Maxillofac Imaging. 2021;2(3):110–2. [Google Scholar]
- 7.Ladani P, Shetye A, Shah M. Dental rehabilitation of patient with complex odontoma: A case report and review of literature. J Dent Implant. 2017;7(1) [Google Scholar]
- 8.Kasami N, Popovski V. Giant Complex Odontoma of the Mandible: A case report and literature review. Acta Medica Balkanica. 2020;5(9-10):58–64. [Google Scholar]
- 9.Kumar BP, Koduru Nikhila GS, Devi VV. Complex Odontoma--A Case Report. Journal homepage: www. nacd. in Indian J Dent Adv. 2019;11(3):112–6. [Google Scholar]
- 10.Bueno NP, Bergamini ML, Elias FM, Braz-Silva PH, Ferraz EP. Unusual giant complex odontoma: A case report. J Stomatol Oral Maxillofac Surg. 2020;121(5):604–607. doi: 10.1016/j.jormas.2019.12.009. [DOI] [PubMed] [Google Scholar]
- 11.Niazmand M, Mokhtari S. Large erupted odontoma of the mandible: Report of a rare case. J Med Sci. 2019;39(4) [Google Scholar]
- 12.Ćabov T, Fuchs PN, Zulijani A, Ćabov Ercegović L, Marelić S. Odontomas: pediatric case report and review of the literature. Acta Clin Croat. 2021;60(1):146–152. doi: 10.20471/acc.2021.60.01.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Unni JV, Daryani D, Kumar V, Uthkal MP. A large complex infected odontome: Case report and review of literature. J Indian Acad Oral Med Radiol. 2020;32(3):308. [Google Scholar]
- 14.Akerzoul N, Chbicheb S, El Wady W. Giant Complex Odontoma of Mandible: A Spectacular Case Report. Open Dent J. 2017;11:413–419. doi: 10.2174/1874210601711010413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wright JM, Vered M. Update from the 4th Edition of the World Health Organization Classification of Head and Neck Tumours: Odontogenic and Maxillofacial Bone Tumors. Head Neck Pathol. 2017;11(1):68–77. doi: 10.1007/s12105-017-0794-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Adhikari P, Chatterjee RP, Gayen S, Paul M, Sultana M, Mahmud SA, Das SK. Complex Odontoma: A Case Report. Eur J Dent. 2021;2(2):1–4. [Google Scholar]
- 17.Park JC, Yang JH, Jo SY, Kim BC, Lee J, Lee W. Giant complex odontoma in the posterior mandible: A case report and literature review. Imaging Sci Dent. 2018;48(4):289–293. doi: 10.5624/isd.2018.48.4.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Satish V, Prabhadevi MC, Sharma R. Odontome: A Brief Overview. Int J Clin Pediatr Dent. 2011;4(3):177–85. doi: 10.5005/jp-journals-10005-1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kämmerer PW, Schneider D, Schiegnitz E, Schneider S, Walter C, Frerich B, Kunkel M. Clinical parameter of odontoma with special emphasis on treatment of impacted teeth-a retrospective multicentre study and literature review. Clin Oral Investig. 2016;20(7):1827–35. doi: 10.1007/s00784-015-1673-3. [DOI] [PubMed] [Google Scholar]
- 20.Levi-Duque F, Ardila CM. Association between odontoma size, age and gender: Multivariate analysis of retrospective data. J Clin Exp Dent. 2019;11(8):e701–e706. doi: 10.4317/jced.55733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Saravanan R, Sathyasree V, Manikandhan R, Deepshika S, Muthu K. Sequential Removal of a Large Odontoma in the Angle of the Mandible. Ann Maxillofac Surg. 2019;9(2):429–433. doi: 10.4103/ams.ams_102_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aschaitrakool Y, Panyawaraphon T, Chinkrua C, Chamusri N, Wimardhani YS. Management of Large Odontoma in Mandible: A Rare Case Report. CM Dent J. 2021;42(2):120–7. [Google Scholar]
- 23.Gervasoni C, Tronchet A, Spotti S, Valsecchi S, Palazzolo V, Riccio S, D Aiuto A, Azzi L, Di Francesco A. Odontomas: review of the literature and case reports. J Biol Regul Homeost Agents. 2017;31(2 Suppl 1):119–125. [PubMed] [Google Scholar]
- 24.Cezairli B, Taşkesen F, Coşkun Ü, Cezairli NS, Tosun E. Surgical treatment of a large complex odontoma. Meandros Med Dent J . 2017;18(2) [Google Scholar]
- 25.Balaji SM, Balaji P. Large odontome compressing inferior alveolar nerve - A case report. Indian J Dent Res. 2021;32(1):124–126. doi: 10.4103/ijdr.ijdr_115_21. [DOI] [PubMed] [Google Scholar]
- 26.Maltagliati A, Ugolini A, Crippa R, Farronato M, Paglia M, Blasi S, Angiero F. Complex odontoma at the upper right maxilla: Surgical management and histomorphological profile. Eur J Paediatr Dent. 2020;21(3):199–202. doi: 10.23804/ejpd.2020.21.03.08. [DOI] [PubMed] [Google Scholar]