Abstract
Background/objective
The effect of glenoid version on the severity of glenoid bone loss is not completely understood, although the variation of glenoid version angles is considered to reflect the degree of glenoid bone loss in anterior shoulder instability cases. The objective of this retrospective case-control study is to determine the relationship of the glenoid version and the severity of glenoid bone loss in a group of previously documented recurrent anterior shoulder dislocation patients.
Methods
We retrospectively collected magnetic resonance arthrogram (MRA) data from 72 patients with unidirectional recurrent anterior shoulder instability. The best-fit circle method was used to identify the percentage of glenoid bone loss. Measurements of glenoid labral, chondral, and bony versions were performed using the Friedman method.
Results
Using univariate regression analysis, it was found that a retroversion angle of more than 4 degrees was associated with an increased risk ratio for the occurrence of a critical glenoid defect by approximately 5 times.
Conclusions
24 Univariate logistic regression analysis, used to determine the presence of a critical glenoid bone defect, showed that both the bony version angle and the number of previous dislocations were significantly associated with the extent of glenoid bone loss. A retroversion angle of more than 4 degrees was associated with an approximately five-fold increase in the odds ratio for the presence of a critical glenoid defect. Surgeons may use the value of the measured glenoid version in prediction the required version of the reconstructive treatment.
Key Terms: Anterior shoulder instability, Critical glenoid bone loss, Glenoid bone loss, Glenoid morphology, Glenoid version, Shoulder dislocation
1. Background
The glenohumeral joint is an inherently unstable joint which is restrained by a combination of both capsulolabral and the bony structures.1 Once an anterior dislocation has occurred, a lesion at the anterior glenoid structure is created. Any defect or deficit along the anterior glenoid margin results in a shallower, less resistant surface with a shorter glenoid arc length. This defect may predispose the joint to dislocation anteriorly more easily and may impact the anterior glenoid, leading to further bone loss.2
The relationship between a glenoid bone defect and the recurrence of shoulder dislocation has been well studied. The presence of a defect with more than 25% glenoid bone loss is significantly associated with the recurrence of dislocation.1,3,4 An understanding of the threshold for critical glenoid bone loss is important for proper treatment selection for patients with shoulder instability. In most cases, the threshold serves as the determining factor between arthroscopic soft-tissue stabilization and an open or arthroscopic glenoid augmentation procedure, e.g., a Latarjet procedure or an iliac or tibial bone graft procedure.5, 6, 7, 8, 9
The relationship between the glenoid version and the instability of the shoulder has been well documented in previous studies.10, 11, 12, 13, 14, 15, 16, 17 Recent reports have suggested a strong connection between glenoid retroversion and posterior instability.11, 12, 13,15, 16, 17
In contrast to posterior shoulder instability, there have been few studies describing the relationship between the glenoid version and anterior shoulder instability. One study by Hohmann et al. strongly suggests that anteversion of the glenoid increases in patients with established anterior shoulder instability.10
As mentioned above, both the capsule and labrum as well as the osteology of the shoulder have an important role in glenohumeral instability, with two factors, an increasing number of dislocations and age at first dislocation, being the strongest predictors of the presence of a glenoid bone defect and its size.18
Although the effect of the glenoid version on shoulder stability has been well documented, the effect of the version on glenoid bone loss has not yet been extensively evaluated. Knowledge of that effect could affect treatment decisions for patients with shoulder stability which could be based in part on the specific glenoid defect.
The purpose of this study was to determine the relationship between the glenoid version and the severity of glenoid bone loss by studying the records of patients with documented recurrent anterior shoulder dislocation. We hypothesized that patients with a high degree of glenoid bone loss, especially those with critical glenoid bone loss, may have greater glenoid retroversion.
2. Materials and methods
The study was designed as a retrospective case-control study.
2.1. Patient selection
This study was approved by the local Institutional Review Board. In this retrospective chart review, the medical records of all patients with anterior shoulder instability between January 2009 and December 2019 at Chiangmai university hospital were evaluated for inclusion in our study.
International Classification of Disease 9 (ICD-9) codes were used to identify patients within the defined time frame with anterior shoulder instability. We identified 120 patients diagnosed with anterior shoulder instability according to ICD-9. Each case was then manually reviewed. After excluding patients with multidirectional instability and those who had imperfections in their MRA data in the CMU PAC system, 40 patients excluded as 5 patients with multi directional instability and 43 patients with imperfection MRA in database a total of 72 patients were included in our study.
2.2. Outcome measures
Standard MRA shoulder images were obtained using a 3-T system. The mixed solution of gadolinium 0.1 ml combined with 3 ml of iodinate contrast and 20 ml of water was injected into the shoulder joint via spinal needle no.22 under fluoroscopic guidance. All scans were performed by the same radiology technician following a pre-established protocol. All images were obtained with the patient supine and the arm placed at the side of the body with the forearm supinated and the hand under the hip to maintain the appropriate humeral position during the examination. The MRA study included sagittal, axial, and oblique coronal images. The coronal oblique images were taken in a plane parallel to the supraspinatus tendon. All images were used in the calculation of the glenoid version and extent of glenoid bone loss.
2.3. Version
A total of 72 magnetic resonance arthrograms of samples with unidirectional recurrent anterior shoulder instability were reviewed, and measurements of glenoid, labral, chondral, and bone versions were made using the CMU PAC system.
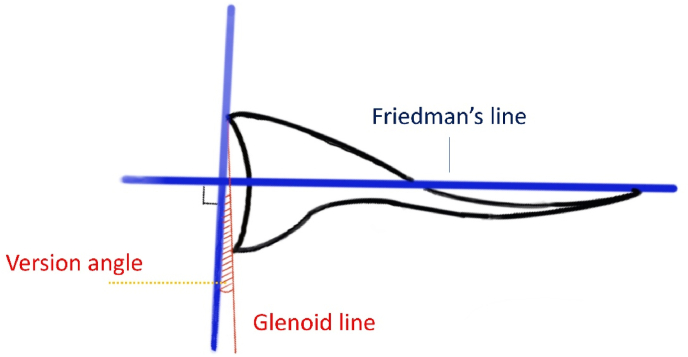
The glenoid version was measured using the technique described by Friedman.19 The axial image immediately inferior to the supraspinatus muscle where the posterior border of the scapular neck is clearly visible was selected. A line was then drawn along the axis of the glenoid surface (Glenoid line). The scapular axis (Friedman's line) was defined as a line drawn from the midpoint of the glenoid to a point on the medial rim of the scapular blade. The glenoid version angle was calculated by subtracting 90° from the angle formed by the glenoid line and Friedman's line.20 (Fig. 1).
Fig. 1.
Glenoid version measurement using Friedman's method.
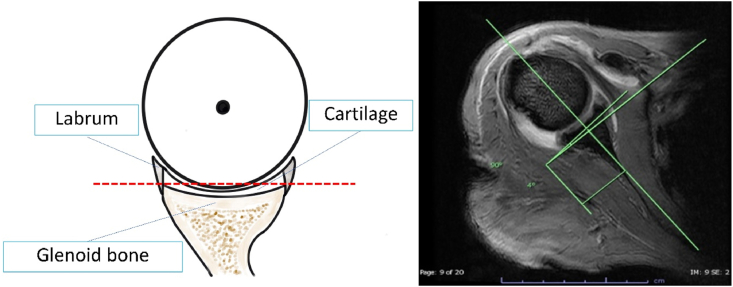
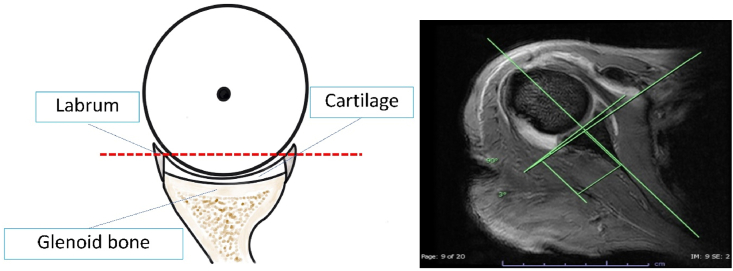
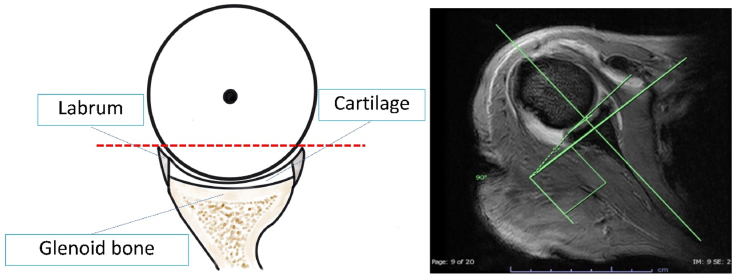
We measured the glenoid version, the bony version, the chondral version and the labral version three time each. We described retroversion by negative angles and anteversion by positive angles. All three measurements of each version were made using the same axial image. The labral version was also measured as described by Kim et al.21 and was defined as the angle formed by a line perpendicular to the reference line and a line connecting the apex of the anterior and posterior labrum. The chondral version was measured by a line connecting the apex of the chondral surfaces at the chondrolabral junctions anteriorly and posteriorly. The bony version was measured by a line connecting the apex of the subchondral bone anteriorly and posteriorly (Fig. 2, Fig. 3, Fig. 4).
Fig. 2.
Bony version measurement.
Fig. 3.
Chondral version measurement.
Fig. 4.
Labral version measurement.
Mizuno et al.22 analyzed Bankart lesions extending from the central anterior edge of the glenohumeral joint to the inferior margin, lesions which had been created by an anteroinferior force vector during a traumatic dislocation event. In this study to avoid the area of glenoid erosion, measurement of the glenoid version was made at the superior third of the glenoid MRI axial cut immediately inferior to the supraspinatus muscle where the posterior border of the scapular neck is clearly visible.
2.4. Glenoid bone loss measurement
Three dimensionally reconstructed computed tomography (3DCT) images with the humeral head digitally subtracted have been considered the gold standard for assessing glenoid morphology.23 Several authors have suggested replacing CT with MRI to reduce the cost of imaging studies and to avoid possible radiation exposure. Many authors have reported that quantification using sagittal images of MRI is equally accurate as using 3DCT.24, 25, 26, 27, 28
Several methods have been described for grouping defects based on the linear Bankart length measurement.29, 30, 31, 32 Among these methods, the best-fit circle method appears to be the simplest technique to understand and the most convenient to use when attempting to quantify glenoid bone loss during imaging.24 With the Sugaya method, a best-fit circle is drawn along the inferior aspect of the glenoid to identify the percentage of glenoid bone loss. In this study, glenoid bone loss of more than 25% is defined as critical glenoid bone loss.32 (Fig. 5).
Fig. 5.
Best-fit circle method for measuring glenoid bone loss.
To establish interobserver and intraobserver reliability in the current study, 20 random MRAs were selected. Two investigators used the methods described above to calculate correlation coefficients for those MRAs. The correlation coefficients for interobserver reliability were 0.84 for version and 0.89 for glenoid bone loss. Intraobserver correlation coefficients were 0.97 for version and 0.94 for glenoid bone loss. Given the comparative nature of the project and the high intraobserver reliability scores, selection of MRIs and all subsequent measurements were performed by the same independent research associate.
3. Statistical analysis
Categorical variables are reported as frequencies and percentages. Continuous variables were non-parametric and are reported as medians and interquartile ranges (IQR). In bivariate analysis, the association between glenoid bone loss and the categorical variables was calculated using Fisher's exact test; associations among continuous variables were calculated using the Mann-Whitney U test. P-values of less than 0.05 were considered statistically significant.
The relationships between bony, chondral, labral versions and glenoid bone loss were evaluated using logistic regression analysis. Predictors considered to be potential confounding factors were gender, age at first dislocation, and total number of dislocations.
The power of the statistical analysis of the association between a variable and the outcome were calculated using two independent proportions. We calculated the statistical power to be > 0.8. Univariate regression was used to calculate risk ratios using binomial families and were adjusted for confounders. Statistical significance was set at P values < 0.05.
4. Results
This retrospective study of 72 shoulders included 76.38% male subjects (n = 62) and 23.62% female subjects (n = 10). Their mean age was 31 years old. The mean age at the first dislocation was 23 years. The average number of dislocations was 26, the mean bony version retroversion was 3.34°, the mean chondral version retroversion was 3.8° and the mean labral version retroversion was 5.65° (Table 1). Ten of the 72 patients had critical glenoid bone loss.
Table 1.
Patient characteristics and other factors included in study.
| Variable | Mean |
|---|---|
| Age at first dislocation | 23 years |
| Number of dislocations | 26 |
| Bony version | Retroversion 3.34° |
| Critical bone loss group (10) | Retroversion 5.88° |
| Non critical bone loss group (62) | Retroversion 2.93° |
| Chondral version | Retroversion 3.80° |
| Critical bone loss group (10) | Retroversion 6.30° |
| Non critical bone loss group (62) | Retroversion 3.40° |
| Labral version | Retroversion 5.65° |
| Critical bone loss group (10) | Retroversion 8.80° |
| Non critical bone loss group (62) | Retroversion 5.14° |
Evaluation of confounding factors for the extent of a glenoid bone defect found that the number of dislocations had a significant influence on the extent of the glenoid bone loss, especially in cases of critical glenoid bone loss. However, other confounding factors identified in a previous study18 were not found to be statistically significant (Table 2).
Table 2.
Univariate characteristics of confounders for the presence of critical glenoid bone defect.
| Variable | Glenoid Bone loss |
P-value | |
|---|---|---|---|
| <25% | >25% (critical) | ||
| Gender, n (%) | |||
| Male | 53 (83) | 9 (90) | 0.7030 |
| Female | 9 (17) | 1 (10) | |
| Age at first dislocation | |||
| median (IQR) | 23 (13.8) | 22 (8.86) | 0.3197 |
| Number of dislocations | |||
| median (IQR) | 19 (64) | 53 (96.5) | 0.0001 |
Univariate logistic regression analysis, used to determine the presence of a critical glenoid bone defect, showed that both the bony version angle and the number of previous dislocations were significantly associated with the extent of glenoid bone loss. A retroversion angle of more than 4° was associated with an approximately five-fold increase in the odds ratio for the presence of a critical glenoid defect (Table 3).
Table 3.
Univariate characteristics of the glenoid version: presence of critical glenoid bone defect.
| Variable | Odds Ratio | 95% CI | P-value |
|---|---|---|---|
| 4° or more of glenoid bony retroversion | 5.18 | 1.02–26.43 | 0.04 |
| 4° or more of glenoid chondral retroversion | 1.58 | 0.41–6.05 | 0.50 |
| 4° or more of glenoid labral retroversion | 2.1 | 0.54–8.09 | 0.28 |
5. Discussion
This study presents the relationship between glenoid version and severity of glenoid bone loss, especially in anterior shoulder instability patients. The version angle range most closely associated with the occurrence of critical glenoid bone loss was 4° or more of bony retroversion. A history of multiple dislocations was also a strong predictor of critical glenoid bone loss. Chondral version and labral version did not demonstrate a significant association although there was a relationship between these angles and glenoid bone loss.
The glenoid version can be measured by various methods. One of the standard methods is the “Friedman method” that be done with either CT or MRA scans.19 The advantage of MRA over CT scans is that MRA can provide more detail, not only of the bony version but also of the soft tissue version. A high signal intensity layer between the labrum, chondral cartilage and osseous can be evaluated separately. We decided to use MRA for this study because it allowed us to evaluate each version independently.
Previous studies have reported varying average degrees of the glenoid version angle, with the average glenoid version being between 2° anteversion and 7° retroversion depending on the location and measurement method.33, 34, 35, 36 The results of our cohort study are in concordance with previous studies. In this study we found the average bony version to be a retroversion of 3.34°. The bony version was found to have a significant correlation with critical glenoid bone loss. Univariate regression analysis of the size of the glenoid bone defect showed that bony retroversion of more than 4° was significantly associated with critical glenoid bone loss: the occurrence of critical glenoid bone loss in patients who had a retroversion angle of 4° or more was 5 times higher than in the more anteversion groups.
Eichinger et al.34 demonstrated that a linear relationship can be observed between the glenoid version and the force required to dislocate the glenohumeral joint. They found that for each 1° increase in retroversion, between retroversion 5° and anteversion 5° of glenoid version, the force required for dislocation increased by 6% per degree, and the energy needed to dislocate increased by 10% per degree. That study suggested that increasing the retroversion of the glenoid might increase the force needed to dislocate the shoulder which might explain why greater extent of glenoid bone damage is found with higher degrees of glenoid retroversion.
Milano et al. reported that both the total number of dislocations and a younger age at first dislocation were important factors associated with greater glenoid bone loss.18 We therefore analyzed these two factors as confounding factors. But due to small number of sample size in critical glenoid bone loss group so we decided not to calculate multivariate logistic regression analysis.
Previous studies12,21 have reported that there is normally greater retroversion at the superior glenoid level compared to the lower glenoid level. In this study, because the mid to lower glenoid level was destroyed when the shoulders were dislocated, we measured the retroversion of the upper glenoid level, then used the previously reported average difference between the upper and lower glenoid level retroversion to estimate the value for the mid to lower glenoid level which should be approximately 4–6° more anteversion than the version of the upper glenoid.37
The clinical relevance of this study is that it may help predict the importance of the glenoid version after an anterior instability especially those who have a high degree of bone loss which indicates a higher retroversion than normal. This could also affect the surgical technique which previously emphasized the restoration of the glenoid surface area. The version of the reconstructed glenoid may have to be taken into account. Further study needs to be done to prove the effectiveness of the glenoid reconstruction procedure relates to the version of the glenoid. Also, the study is needed to evaluate other aspects of glenoid morphology, e.g., glenoid inclination and glenoid width, which may also play an important role in glenoid bone loss. Similarly, the study of potential bone loss on the humeral head using glenoid morphology is required as well.
A limitation of this study is the small sample size. Some of the factors had an insufficient sample size to be statistically significant although relationship trends were found to exist between those factors and glenoid bone loss.
6. Conclusions
The critical glenoid bone loss might be related to glenoid morphology. The occurrence of critical glenoid bone loss was found to be approximately 5 times higher in patients with more than 4° of glenoid retroversion compared to patients with the same risk factors but with anteversion. Surgeons might be able to evaluate the urgency of treatment in part based on characteristics of the glenoid version.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors, and no material support of any kind was received.
Authorship
Conception and design of study: N. Paopongthong, C. Phornphutkul.
Acquisition of data: N. Paopongthong, P. Atthakomol, C. Phornphutkul, analysis and/or interpretation of data: N. Paopongthong, P. Atthakomol, C. Phornphutkul.
Drafting the manuscript: N. Paopongthong, P. Atthakomol.
Revising the manuscript critically for important intellectual content: C. Phornphutkul.
Approval of the version of the manuscript to be published (the names of all authors must be listed): N. Paopongthong, P. Atthakomol, C. Phornphutkul.
Declaration of competing interest
A conflict of interest occurs when an individual's objectivity is potentially compromised by a desire for financial gain, prominence, professional advancement or a successful outcome. AP-SMART Editors strive to ensure that what is published in the Journal is as balanced, objective and evidence-based as possible. Since it can be difficult to distinguish between an actual conflict of interest and a perceived conflict of interest, the Journal requires authors to disclose all and any potential conflicts of interest.
Acknowledgments
All persons who have made substantial contributions to the work reported in the manuscript (e.g., technical help, writing and editing assistance, general support), but who do not meet the criteria for authorship, are named in the Acknowledgements and have given us their written permission to be named. If we have not included an Acknowledgements in our manuscript, then that indicates that we have not received substantial contributions from nonauthors.
Contributor Information
Nattakorn Paopongthong, Email: Peanutkub@hotmail.com.
Pichitchai Atthakomol, Email: p.atthakomol@gmail.com.
Chanakarn Phornphutkul, Email: berkbann@hotmail.com.
References
- 1.Rowe C., Zarins B., Ciullo J. Recurrent anterior dislocation of the shoulder after surgical repair. Apparent causes of failure and treatment. J Bone Jt Surg Am Vol. 1984;66(2):159–168. [PubMed] [Google Scholar]
- 2.Itoi E., Lee S.-B., Berglund L.J., Berge L.L., An K.-N. The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: a cadaveric study. JBJS. 2000;82(1):35–46. doi: 10.2106/00004623-200001000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Boileau P., Villalba M., Héry J.-Y., Balg F., Ahrens P., Neyton L. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. JBJS. 2006;88(8):1755–1763. doi: 10.2106/JBJS.E.00817. [DOI] [PubMed] [Google Scholar]
- 4.Burkhart S.S., De Beer J.F. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthrosc J Arthrosc Relat Surg. 2000;16(7):677–694. doi: 10.1053/jars.2000.17715. [DOI] [PubMed] [Google Scholar]
- 5.Helfet A.J. Coracoid transplantation for recurring dislocation of the shoulder. The Journal of bone and joint surgery British. 1958;40(2):198–202. doi: 10.1302/0301-620X.40B2.198. [DOI] [PubMed] [Google Scholar]
- 6.Latarjet M. Treatment of recurrent dislocation of the shoulder. Lyon Chir. 1954;49(8):994–997. [PubMed] [Google Scholar]
- 7.Piasecki D.P., Verma N.N., Romeo A.A., Levine W.N., Bach B.R., Jr., Provencher M.T. Glenoid bone deficiency in recurrent anterior shoulder instability: diagnosis and management. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2009;17(8):482–493. doi: 10.5435/00124635-200908000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Provencher C.M.T., Bhatia S., Ghodadra N.S., et al. Recurrent shoulder instability: current concepts for evaluation and management of glenoid bone loss. JBJS. 2010;92(Supplement_2):133–151. doi: 10.2106/JBJS.J.00906. [DOI] [PubMed] [Google Scholar]
- 9.Warner J.J., Gill T.J., O'Hollerhan J.D., Pathare N., Millett P.J. Anatomical glenoid reconstruction for recurrent anterior glenohumeral instability with glenoid deficiency using an autogenous tricortical iliac crest bone graft. Am J Sports Med. 2006;34(2):205–212. doi: 10.1177/0363546505281798. [DOI] [PubMed] [Google Scholar]
- 10.Hohmann E., Tetsworth K. Glenoid version and inclination are risk factors for anterior shoulder dislocation. J Shoulder Elbow Surg. 2015;24(8):1268–1273. doi: 10.1016/j.jse.2015.03.032. [DOI] [PubMed] [Google Scholar]
- 11.Hurley J.A., Anderson T.E., Dear W., Andrish J.T., Bergfeld J.A., Weiker G.G. Posterior shoulder instability: surgical versus conservative results with evaluation of glenoid version. Am J Sports Med. 1992;20(4):396–400. doi: 10.1177/036354659202000405. [DOI] [PubMed] [Google Scholar]
- 12.Inui H., Sugamoto K., Miyamoto T., et al. Glenoid shape in atraumatic posterior instability of the shoulder. Clin Orthop Relat Res. 2002;403:87–92. doi: 10.1097/00003086-200210000-00014. [DOI] [PubMed] [Google Scholar]
- 13.Mauro C.S., McClincy M.P., Bradley J.P. Effect of glenoid version and width on outcomes of arthroscopic posterior shoulder stabilization. Am J Sports Med. 2016;44(4):941–947. doi: 10.1177/0363546516631738. [DOI] [PubMed] [Google Scholar]
- 14.Owens B.D., Campbell S.E., Cameron K.L. Risk factors for anterior glenohumeral instability. Am J Sports Med. 2014;42(11):2591–2596. doi: 10.1177/0363546514551149. [DOI] [PubMed] [Google Scholar]
- 15.Owens B.D., Campbell S.E., Cameron K.L. Risk factors for posterior shoulder instability in young athletes. Am J Sports Med. 2013;41(11):2645–2649. doi: 10.1177/0363546513501508. [DOI] [PubMed] [Google Scholar]
- 16.Privitera D.M., Siegel E.J., Miller L.R., Sinz N.J., Higgins L.D. Glenoid version and its relationship to glenohumeral instability and labral tears. J Shoulder Elbow Surg. 2016;25(7):1056–1063. doi: 10.1016/j.jse.2015.11.013. [DOI] [PubMed] [Google Scholar]
- 17.Wirth M.A., Seltzer D.G., Rockwood C.A., Jr. Recurrent posterior glenohumeral dislocation associated with increased retroversion of the glenoid. A case report. Clin Orthop Relat Res. 1994;308:98–101. [PubMed] [Google Scholar]
- 18.Milano G., Grasso A., Russo A., et al. Analysis of risk factors for glenoid bone defect in anterior shoulder instability. Am J Sports Med. 2011;39(9):1870–1876. doi: 10.1177/0363546511411699. [DOI] [PubMed] [Google Scholar]
- 19.Friedman R.J., Hawthorne K., Genez B. The use of computerized tomography in the measurement of glenoid version. JBJS. 1992;74(7):1032–1037. [PubMed] [Google Scholar]
- 20.Tetreault P., Krueger A., Zurakowski D., Gerber C. Glenoid version and rotator cuff tears. J Orthop Res. 2004;22(1):202–207. doi: 10.1016/S0736-0266(03)00116-5. [DOI] [PubMed] [Google Scholar]
- 21.Kim S.-H., Kim H.-K., Sun J.-I., Park J.-S., Oh I. Arthroscopic capsulolabroplasty for posteroinferior multidirectional instability of the shoulder. Am J Sports Med. 2004;32(3):594–607. doi: 10.1177/0363546503262170. [DOI] [PubMed] [Google Scholar]
- 22.Mizuno K., Nabeshima Y., Hirohata K. Analysis of Bankart lesion in the recurrent dislocation or subluxation of the shoulder. Clin Orthop Relat Res. 1993;(288):158–165. [PubMed] [Google Scholar]
- 23.Sugaya H., Moriishi J., Dohi M., Kon Y., Tsuchiya A. Glenoid rim morphology in recurrent anterior glenohumeral instability. JBJS. 2003;85(5):878–884. doi: 10.2106/00004623-200305000-00016. [DOI] [PubMed] [Google Scholar]
- 24.Gyftopoulos S., Hasan S., Bencardino J., et al. Diagnostic accuracy of MRI in the measurement of glenoid bone loss. Am J Roentgenol. 2012;199(4):873–878. doi: 10.2214/AJR.11.7639. [DOI] [PubMed] [Google Scholar]
- 25.Huijsmans P.E., Haen P.S., Kidd M., Dhert W.J., van der Hulst V.P., Willems W.J. Quantification of a glenoid defect with three-dimensional computed tomography and magnetic resonance imaging: a cadaveric study. J Shoulder Elbow Surg. 2007;16(6):803–809. doi: 10.1016/j.jse.2007.02.115. [DOI] [PubMed] [Google Scholar]
- 26.Lee R.K., Griffith J.F., Tong M.M., Sharma N., Yung P. Glenoid bone loss: assessment with MR imaging. Radiology. 2013;267(2):496–502. doi: 10.1148/radiol.12121681. [DOI] [PubMed] [Google Scholar]
- 27.Owens B.D., Burns T.C., Campbell S.E., Svoboda S.J., Cameron K.L. Simple method of glenoid bone loss calculation using ipsilateral magnetic resonance imaging. Am J Sports Med. 2013;41(3):622–624. doi: 10.1177/0363546512472325. [DOI] [PubMed] [Google Scholar]
- 28.Stecco A., Guenzi E., Cascone T., et al. MRI can assess glenoid bone loss after shoulder luxation: inter-and intra-individual comparison with CT. La radiologia medica. 2013;118(8):1335–1343. doi: 10.1007/s11547-013-0927-x. [DOI] [PubMed] [Google Scholar]
- 29.Barchilon V.S., Kotz E., Barchilon Ben-Av M., Glazer E., Nyska M. A simple method for quantitative evaluation of the missing area of the anterior glenoid in anterior instability of the glenohumeral joint. Skeletal Radiol. 2008;37(8):731–736. doi: 10.1007/s00256-008-0506-8. [DOI] [PubMed] [Google Scholar]
- 30.Chuang T.-Y., Adams C.R., Burkhart S.S. Use of preoperative three-dimensional computed tomography to quantify glenoid bone loss in shoulder instability. Arthrosc J Arthrosc Relat Surg. 2008;24(4):376–382. doi: 10.1016/j.arthro.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 31.Gerber C., Nyffeler R.W. Classification of glenohumeral joint instability. Clin Orthop Relat Res. 2002;400:65–76. doi: 10.1097/00003086-200207000-00009. [DOI] [PubMed] [Google Scholar]
- 32.Sugaya H. Techniques to evaluate glenoid bone loss. Curr Rev Musculoskel Med. 2014;7(1):1–5. doi: 10.1007/s12178-013-9198-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Churchill R.S., Brems J.J., Kotschi H. Glenoid size, inclination, and version: an anatomic study. J Shoulder Elbow Surg. 2001;10(4):327–332. doi: 10.1067/mse.2001.115269. [DOI] [PubMed] [Google Scholar]
- 34.Eichinger J.K., Massimini D.F., Kim J., Higgins L.D. Biomechanical evaluation of glenoid version and dislocation direction on the influence of anterior shoulder instability and development of Hill-Sachs lesions. Am J Sports Med. 2016;44(11):2792–2799. doi: 10.1177/0363546516659281. [DOI] [PubMed] [Google Scholar]
- 35.Mallon W.J., Brown H.R., Vogler J., 3rd, Martinez S. Radiographic and geometric anatomy of the scapula. Clin Orthop Relat Res. 1992;(277):142–154. [PubMed] [Google Scholar]
- 36.Nyffeler R.W., Jost B., Pfirrmann C.W., Gerber C. Measurement of glenoid version: conventional radiographs versus computed tomography scans. J Shoulder Elbow Surg. Sep-Oct 2003;12(5):493–496. doi: 10.1016/s1058-2746(03)00181-2. [DOI] [PubMed] [Google Scholar]
- 37.Kim H., Yoo C.H., Park S.B., Song H.S. Difference in glenoid retroversion between two-dimensional axial computed tomography and three-dimensional reconstructed images. Clin Shoulder Elb. Jun 2020;23(2):71–79. doi: 10.5397/cise.2020.00122. [DOI] [PMC free article] [PubMed] [Google Scholar]