Abstract
Objective:
We developed a novel, nurse practitioner–run Thoracic Survivorship Program to aid in long-term follow-up. Patients with non–small cell lung cancer who were disease-free at least 1 year after resection could be referred to the Thoracic Survivorship Program by their surgeon. Our objectives were to summarize follow-up compliance and assess long-term outcomes between Thoracic Survivorship Program enrollment and non–Thoracic Survivorship Program.
Methods:
Patients who underwent R0 resection for stages I to IIIA between 2006 and 2016 were stratified by enrollment in Thoracic Survivorship Program versus surgeon only follow-up (non–Thoracic Survivorship Program). Follow-up included 6-month chest computed tomography scans for 2 years and then annually. Lack of follow-up compliance was defined by 2 or more consecutive delayed annual computed tomography scans/visits ± 90 days. Relationships between Thoracic Survivorship Program and second primary non–small cell lung cancers, extrathoracic cancers, and survival were quantified using multivariable Cox proportional hazards regression with time-varying covariate reflecting timing of enrollment.
Results:
A total of 1162 of 3940 patients (29.5%) were enrolled in the Thoracic Survivorship Program. The median time to enrollment was 2.3 years; 3279 of 3940 (83%) had complete computed tomography scan data, and 60 of 3279 (1.8%) had 2 or more delayed scans; 323 of 9082 (3.6%) non–Thoracic Survivorship Program visits were noncompliant versus 132 of 4823 (2.7%) of Thoracic Survivorship Program visits (P = .009); 136 of 1146 Thoracic Survivorship Program patients developed second primary non–small cell lung cancer, and 69 of 1123 developed extrathoracic cancer, whereas 322 of 2794 of non–Thoracic Survivorship Program patients developed second primary non–small cell lung cancer and 225 of 2817 patients developed extrathoracic cancer. In multivariable analyses, Thoracic Survivorship Program enrollment was associated with improved disease-free survival (hazard ratio, 0.57; 95% confidence interval, 0.48-0.67; P < .001).
Conclusions:
Our novel nurse practitioner–run Thoracic Survivorship Program is associated with high patient compliance and outcomes not different from those seen with physician-based follow-up. These results have important implications for health care resource allocation and costs.
Keywords: lung cancer follow-up, survivorship
Graphical Abstract
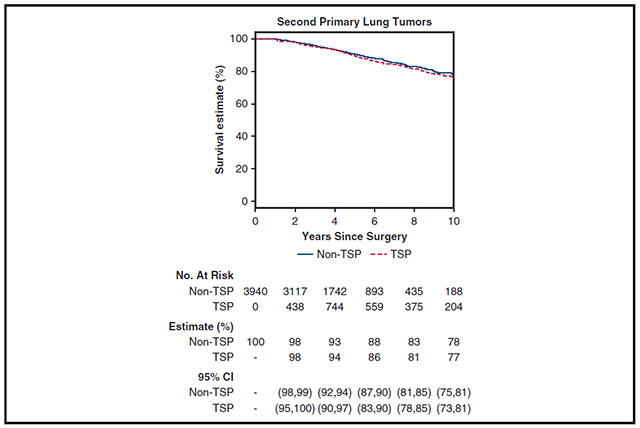
Survival curves for second lung primary tumors with TSP enrollment status as a time-varying covariate.
Starting in 2015, the American College of Surgeons required cancer centers to have a survivorship program to receive Commission on Cancer accreditation.1 As initially proposed by the Institute of Medicine in 2006, the goal of these survivorship programs included long-term coordinated ongoing care for patients with cancer focusing on optimal health and quality of life.2-4
Patients with lung cancer who have undergone surgical resection have a 5-year risk for locoregional recurrent disease of approximately 38% and a 3% to 5% risk per year of a second lung primary.5-7 Therefore, lifelong follow-up for patients with lung cancer after resection is critically important.8
Although various institutions have implemented individualized approaches for following patients with lung and thoracic cancer postoperatively, there are minimal data about a standardized survivorship program and the optimal way to provide continued, comprehensive follow-up.9 At our institution, based on multidisciplinary consensus, we developed the Thoracic Survivorship Program (TSP) in 2006, focusing on lung, esophageal, and mediastinal tumors, as part of a larger institutional survivorship initiative. We previously reported the initial development and outcomes of the TSP program (Table 1).10
TABLE 1.
Thoracic survivorship program features
| • Systematic clinical and radiologic follow-up with CT scan and intravenous contrast every 6 mo for the first 2 y followed by annual CT scan without contrast |
| • Standardized follow-up and electronic documentation of each visit |
| • Enhanced patient experience with specially trained nurse practitioner involved in running the program |
| • Close collaboration with primary surgeon with patients being referred back to the primary surgeon should significant radiologic or clinical abnormalities develop |
| • Close contact with referring physicians from outside of the institution |
| • Enrollment in the program is at the discretion of the primary surgeon, radiation oncologist, or medical oncologist |
| • Eligibility included patients with multiple thoracic malignancies including lung, thymic, and esophageal cancers. |
| • NSCLC– Eligibility started after 1 y disease-free postresection (stage I) and 2 y disease-free postresection (stage II/IIIa) |
CT, Computed tomography; NSCLC, non–small cell lung cancer.
Leveraging 15 years of experience, we assessed the updated outcomes of the TSP in our patients with lung cancer. The objectives of the study are to summarize TSP enrollment and follow-up compliance, and quantify the associations between TSP enrollment and long-term outcomes (recurrence, second lung primary malignancies, and second extrathoracic primary malignancies), as well as overall and disease-free survival.
MATERIALS AND METHODS
We performed a retrospective review of a prospectively maintained institutional database of patients treated between January 2006 and July 2016. Patients included in this analysis underwent a R0 resection for non–small cell lung cancer (NSCLC) clinical stages I to IIIA. All patients included had to survive at least 2 years, were disease-free for at least 1 year, and had follow-up for at least 2 years postoperatively. If patients had multiple operations for distinct lung primary tumors, only the first operation was included. Memorial Sloan Kettering Cancer Center Institutional Review Board approved the study as a retrospective research protocol (Institutional Review Board No. 20-054, approved February 12, 2020) and waived the need for patient informed consent.
Categorization of Thoracic Survivorship Program and Non–Thoracic Survivorship Program
For assessment of patient demographics, tumor characteristics, and treatment, patients were divided into 2 cohorts depending on whether they were eventually enrolled in the TSP versus being followed by their surgeons (non-TSP). TSP visits were performed by a nurse practitioner specifically trained in thoracic survivorship care who collaborated closely with the operating surgeon, and non-TSP visits were performed by the operating surgeon only. For patients ultimately enrolled in TSP, time from surgery to enrollment into the TSP was recorded. Eligibility for the TSP started after 1 year disease-free postresection (stage I disease) and 2-year disease-free postresection (stages II-IIIA.) When patients were transferred to the TSP, the regular interval for follow-up was maintained. For analysis of compliance, recurrence, second lung primary, and extrathoracic second primary malignancies, only data after the first TSP appointment were included in the analysis of the TSP cohort. To ensure enrollment into TSP was not influenced by how long the program had been functioning, we assessed enrollment before and on or after 2012, a date at which the program was considered mature based on experience and stability in nurse practitioner staff.
Demographics
Patient demographics collected included age, gender, smoking history, Zubrod score, prior cancer history, clinical tumor stage, pulmonary function tests, neoadjuvant therapy, surgical approach, tumor histology and pathologic stage, and year of operation.
Follow-up
Follow-up computed tomography (CT) scans and visit with date were noted for all patients. Time from surgery to follow-up CT scan and visit was used for compliance analysis. Routine follow-up included systematic clinical and radiologic follow-up with CT scan and intravenous contrast every 6 months for the first 2 years, followed by annual CT scan without contrast (Table 1). For patients enrolled in TSP, there was close collaboration between the primary surgeon and the nurse practitioner, with patients being referred back to the primary surgeon should significant radiological or clinical abnormalities develop.
Recurrence, Second Primary Lung Cancers, Extrathoracic Second Primary Cancers
Local recurrence was defined as a new tumor adjacent to a staple line, to the bronchial stump, or in the residual lobe (in cases of sublobar resection). Regional recurrences involved lymph nodes stations 1 to 14 or the ipsilateral lung. Distant metastasis was defined as a disease outside the ipsilateral hemithorax.
Second primary lung cancer was defined according to the criteria of Martini and Melamed11: (1) different histology from the index tumor; (2) same histology as the index tumor but diagnosed at least 2 years later; (3) same histology as the index tumor and diagnosed within 2 years, but located in a different lobe or segment, with no positive intervening lymph nodes and no evidence of metastasis. Confirmation of clonal relatedness, as published by our group,12 was used when genomic data were available.
Extrathoracic second primary cancers were defined as primary malignancies that occurred outside of the chest cavity. Only extrathoracic primary malignancies identified during postoperative follow-up after resection of first primary lung cancer were included. Recurrences, second primary lung cancer, and extrathoracic second primary cancer were analyzed separately. For summary of each outcome, patients were attributed to TSP or non-TSP depending on when the outcome occurred compared with enrollment into TSP.
Statistical Analyses
Data are summarized as frequency (percentage) or median (25th, 75th percentile). Enrollment into TSP was summarized as absolute proportion in the entire cohort and at 5 years postresection as 5-year cumulative incidence of enrollment due to variable time to TSP enrollment. Enrollment patterns were also summarized separately among patients who received surgery before 2012 versus on or after 2012 to reflect the maturity of the TSP program.
Summaries of compliance only included CT visits that occurred before any known date of recurrence and excludes visits in the first 2 years after surgery. CT visits that occurred on the date of TSP enrollment were considered non-TSP visits. Duration between 2 visits were calculated, and if the subsequent visit is 1 year or more + 90 days apart, then the subsequent visit is considered noncompliant (“delayed” or “missed”). The proportion of visits that were considered noncompliant are summarized by the type of visit (TSP or non-TSP) and compared between the 2 types by chi-square test.
Median duration of follow-up was estimated using reverse Kaplan–Meier approach from the time of surgery. Outcomes of interest (recurrence, second primary, extrathoracic second primary) and long-term survival (overall survival and disease-free survival) were analyzed using a time-to-event approach from the time of surgery. To account for variable time to TSP enrollment from surgery, TSP enrollment was considered a time-varying covariate such that all patients contribute information to the non-TSP cohort from the time of surgery until the day they enrolled in TSP, at which point they contribute information to the TSP cohort. Overall survival was estimated from the time of surgery to the time of death; disease-free survival was estimated from the time of surgery to the time of progression or death. Patients who did not experience the events of interest were censored at the time of last follow-up. Survival estimates for the second lung primary end point were summarized by TSP status using the Kaplan–Meier approach with TSP as time-varying covariate. The relationships between TSP enrollment status and each end point were quantified using extended Cox proportional hazards regression with time-varying covariate reflecting the timing of patient’s enrollment into the TSP.13 Adjusted hazard ratios (HRs) and corresponding 95% confidence intervals (CIs) for TSP enrollment were estimated in a multivariable model adjusting for a set of variables determined a priori (age, smoking status, gender, American Society of Anesthesiology Physical Status Classification System, prior cancer, forced expiratory volume in 1 second (%), diffusing capacity for carbon monoxide (%), induction therapy, procedure performed, approach, tumor location, histology, pathologic stage, adjuvant therapy, and year of surgery.) All models were stratified by surgeon to account for correlations between patients treated by the same surgeon and any potential referral patterns at the surgeon level.
Data were collected using Excel (Microsoft Corp), and all analyses were conducted with Stata 15.1 (StataCorp) and R 3.6.1 (R Core Team). Time-varying covariate data were translated into counting process style and merged using the tmerge function within the R package Survival. Statistical tests were 2 sided and P < .05 was considered statistically significant.
RESULTS
Study Population
Of the 7430 patients who underwent lung resection in our institution between 2006 and 2016, a total of 3940 patients met study criteria (Figures 1 and 2) and 1162 of 3940 (29.5%) were ultimately enrolled in the TSP. Median (25th, 75th percentile) time to TSP enrollment was 2.3 years (1.7-3.6), and median follow-up duration from time of surgery was 6.4 years (4.1-9.5). The 5-year cumulative incidence of survivorship enrollment was 25.3% (95% CI, 24.0-26.7) (Figure E1). To assess whether the TSP enrollment differed by maturity of the TSP program, we stratified TSP enrollment before or after the year of surgery being 2012. Median time to enrollment into TSP was similar regardless of whether year of surgery was before versus on or after 2012 (before: 2.1 [25th, 75th percentile; 1.4, 4.3] years; on or after: 2.5 [1.9, 3.2] years). Enrollment rate into TSP was similar regardless of year of surgery before or after 2012 (5-year estimates: 24.0% [2006-2011], 28.7% [2012-2016]).
FIGURE 1.
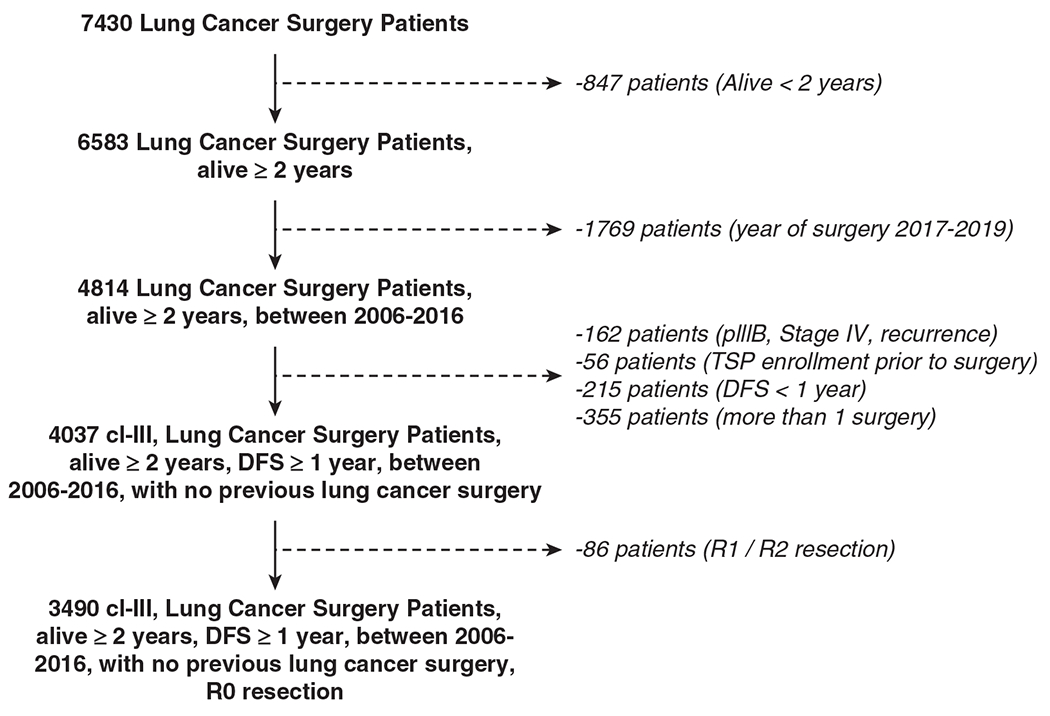
CONSORT diagram. TSP, Thoracic Survivorship Program; DFS, disease-free survival.
FIGURE 2.
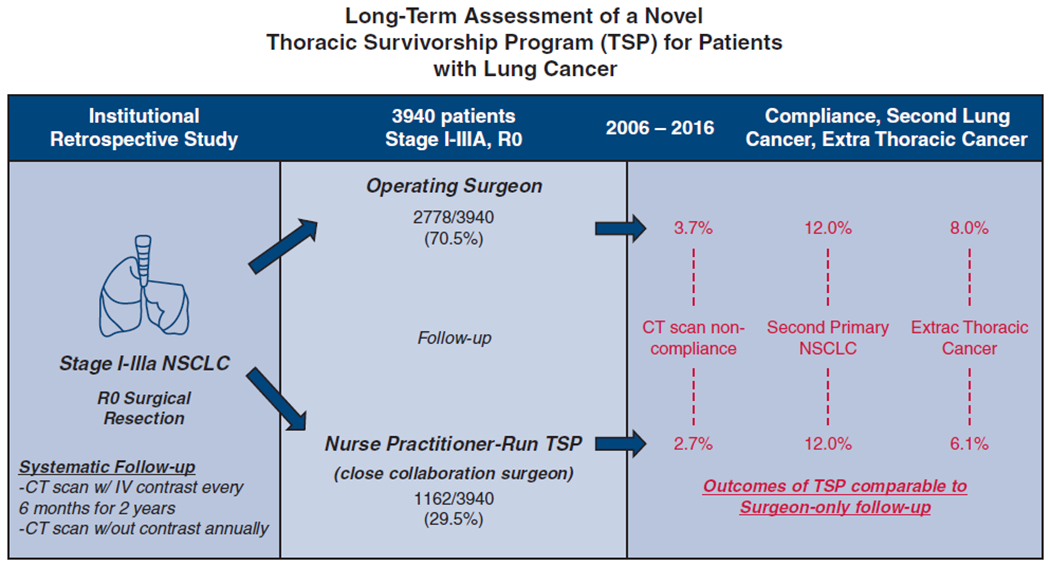
Long-term assessment of a novel TSP for patients with lung cancer showing patient enrollment and outcomes. NSCLC, Non–small cell lung cancer; CT, computed tomography; IV, intravenous.
Demographics
While the time to TSP enrollment varies, when assessing patients ultimately enrolled in TSP, the majority of patients in both cohorts were women (TSP: 729/1162, 63%; non-TSP: 1723/2778, 62%) with a similar distribution of age (median [25th, 75th percentile]: TSP: 67 years [60,73]; non-TSP: 68 [61,74]). Most patients were former/current smokers (TSP: 909/1162, 78%; non-TSP: 2199/2788, 79%); did not have a previous cancer (TSP: 251/1162, 65%; non-TSP: 1702/2778, 61%); and those with a known Zubrod score of 0/1 (TSP: 645/656, 98%; non-TSP: 1602/1631, 98%) (Table 2).
TABLE 2.
Patient demographic and clinical characteristics
| Overall N = 3940 | Non-TSP (N = 2778; 71%) | TSP (N = 1162; 29%) | |
|---|---|---|---|
| Age, y | 68 (61-74) | 68 (61-74) | 67 (60-73) |
|
| |||
| Smoking status | |||
| Never | 835 (21) | 579 (21) | 253 (22) |
| Former/current | 3116 (79) | 2199 (79) | 909 (78) |
|
| |||
| Sex | |||
| Female | 2456 (62) | 1723 (62) | 729 (63) |
| Male | 1495 (38) | 1055 (38) | 433 (37) |
|
| |||
| Zubrod Score (N = 2287) | |||
| Zubrod 0/1 | 2254 (98) | 1602 (98) | 645 (98) |
| Zubrod 2/3/4 | 40 (1.7) | 29 (1.8) | 11 (1.7) |
|
| |||
| ASA | |||
| ASA I/II | 764 (19) | 512 (18) | 251 (22) |
| ASA III/IV | 3187 (81) | 2266 (82) | 911 (78) |
|
| |||
| Prior cancer | |||
| No | 2471 (63) | 1702 (61) | 760 (65) |
| Yes | 1480 (37) | 1076 (39) | 402 (35) |
|
| |||
| FEV1 (%) (N = 3824) | 91 (78-104) | 89 (77-103) | 94 (81-105) |
|
| |||
| Diffusion (%) (N = 3698) | 82 (68-96) | 80 (66-94) | 85 (71-99) |
|
| |||
| Induction | |||
| No | 3508 (89) | 2413 (87) | 1084 (93) |
| Yes | 443 (11) | 365 (13) | 78 (7) |
|
| |||
| Procedure performed | |||
| Lobectomy | 2643 (67) | 1809 (65) | 827 (71) |
| Sublobar | 1145 (29) | 840 (30) | 301 (26) |
| Bilobectomy | 84 (2.1) | 63 (2.3) | 21 (1.8) |
| Pneumonectomy | 79 (2.0) | 66 (2.4) | 13 (1.1) |
|
| |||
| Approach | |||
| Open | 1744 (44) | 1397 (50) | 343 (30) |
| VATS/RATS | 2207 (56) | 1381 (50) | 819 (70) |
|
| |||
| Tumor location | |||
| Left | 1543 (39) | 1085 (39) | 454 (39) |
| Right | 2408 (61) | 1693 (61) | 708 (61) |
|
| |||
| Pathology | |||
| Adenocarcinoma | 2867 (73) | 1988 (72) | 879 (76) |
| Squamous cell | 519 (13) | 389 (14) | 130 (11) |
| Small cell | 44 (1) | 32 (1.2) | 12 (1.0) |
| Carcinoid | 340 (9) | 240 (8.6) | 100 (8.6) |
| Other/large/pleomorphic | 170 (4) | 129 (4.6) | 41 (3.5) |
|
| |||
| Pathologic stage | |||
| 0 | 73 (2) | 60 (2) | 9 (1) |
| I | 2831 (72) | 1858 (67) | 975 (84) |
| II | 629 (16) | 493 (18) | 135 (11) |
| IIIA | 411 (10) | 367 (13) | 43 (4) |
|
| |||
| In-house complications | |||
| No | 3000 (76) | 2089 (75) | 911 (78) |
| Yes | 940 (24) | 689 (25) | 251 (22) |
|
| |||
| Grade of complication (n = 940) | |||
| 1-2 | 841 (89) | 606 (89) | 235 (89) |
| 3-4 | 104 (11) | 75 (11) | 29 (11) |
|
| |||
| Complication type (n = 940) | |||
| Respiratory | 394 (42) | 285 (41) | 109 (44) |
| Cardiac | 276 (29) | 206 (30) | 70 (28) |
| Renal | 108 (11) | 79 (11) | 29 (12) |
| Other | 162 (17) | 119 (17) | 43 (17) |
|
| |||
| Adjuvant therapy (n = 3890) | |||
| Systemic only | 547 (14) | 428 (16) | 119 (10) |
| Radiation only | 81 (2) | 72 (2) | 9 (1) |
| Systemic and radiation | 81 (2) | 75 (3) | 6 (1) |
| None | 3181 (82) | 2156 (79) | 1025 (88) |
Time to TSP enrollment after surgery may vary; values are reported as N (%) or median [25th, 75th percentiles]. TSP, Thoracic Survivorship Program; ASA, American Society of Anesthesiology Physical Status Classification System; FEV1, forced expiratory volume in 1 second; VATS, video-assisted thoracic surgery; RATS, robot-assisted thoracic surgery.
Adenocarcinoma was the predominant histology in both cohorts (TSP:879/1162, 76%; non-TSP: 1988/2778, 72%). Patients in the TSP cohort had a lower pathologic stage with 984 of 1162 patients (85%) being stage 0 to 1 versus 1918 of 2778 patients (69%) in the non-TSP cohort. Only 43 of 1162 patients (3.7%) in the TSP cohort were stage IIIA versus 367 of 2778 patients (13.0%) in the non-TSP cohort. There was a higher proportion of patients receiving neoadjuvant therapy in the non-TSP cohort (365/2778, 13%) compared with the TSP cohort (78/1162, 6.7%). The majority of both patients in both cohorts underwent a lobectomy (TSP 827/1162, 71%; non-TSP 1809/2778, 65%). More patients in the TSP cohort (819/1161, 70%) underwent a minimally invasive approach with video-assisted thoracoscopic surgery (robotic or nonrobotic) compared with the non-TSP cohort (1381/2778, 50%) (Table 2). Postoperative median length of stay was similar between both cohorts at 4 days. In-hospital complications occurred in 251 of 1162 patients (22%) in the TSP cohort and 689 of 2778 patients (22%) in the non-TSP cohort, with the majority of patients having a grade 1 to 2 complication (89%) (Table 2).
Follow-up Compliance
A total 3279 of 3940 patients (83%) had complete CT scan and follow-up visit data. Some patients did not have full CT scan data because scans were performed outside of Memorial Sloan Kettering Cancer Center; 327 of 3279 (10.0%) had 1 delayed visit and 60 of 3279 (1.8%) had 2 or more delayed visits. Of the total number of visits, 323 of 9082 (3.6%) non-TSP visits were deemed noncompliant versus 132 of 4823 (2.7%) TSP visits (P = .009).
Recurrence
Recurrence of disease occurred in 549 of 2787 patients in the non-TSP cohort compared with 80 of 1153 in the TSP cohort. Similar location of recurrence was noted in both cohorts, with approximately one-third having a local recurrence only (Tables 3 and E1). In a multivariable analysis (Table E2) adjusting for demographics, tumor characteristics, surgical characteristics, stage, induction therapy, adjuvant therapy, and year of surgery, TSP enrollment was not significantly associated with the hazard of recurrence (HR, 0.91; 95% CI, 0.65-1.26; P = .6).
TABLE 3.
Recurrence rates, second lung primary tumors, and extrathoracic primary tumors and survivorship enrollment
| Non-TSP | TSP | |
|---|---|---|
| Recurrence | [2787] | [1153] |
| Yes | 549 | 80 |
|
| ||
| Recurrence location (n = 629) | ||
| Distant | 298 | 41 |
| Locoregional | 153 | 25 |
| Distant + locoregional | 98 | 14 |
|
| ||
| Second lung primary malignancy | [2794] | [1146] |
| Yes | 322 | 136 |
|
| ||
| Clinical stage of second lung primary (n = 458) | ||
| IA | 262 | 112 |
| IB | 11 | 5 |
| II | 16 | 3 |
| IIIA | 16 | 6 |
| IIIB/C/IV | 17 | 10 |
|
| ||
| Treatment of second lung primary | ||
| Local (surgery or radiation) | 277 | 118 |
| Local and systemic | 19 | 6 |
| Systemic | 10 | 6 |
| Observation | 16 | 6 |
|
| ||
| Second extrathoracic malignancy | [2817] | [1123] |
| Yes | 225 | 69 |
|
| ||
| Site of second extrathoracic malignancy (n = 294) | ||
| Prostate/kidney/urologic | 48 | 17 |
| Breast | 33 | 12 |
| Thyroid | 29 | 6 |
| Other | 115 | 35 |
Each outcome was analyzed separately with regards to TSP enrollment at the time of outcome; thus the number of patients in TSP is different depending on outcome. [ ] Indicates total patients in TSP or non-TSP analyzed for each outcome. TSP, Thoracic Survivorship Program
Second Primary
The frequency in detection of second primary lung cancers was the same across TSP (136/1146, 12%) and non-TSP (322/2794, 12%) groups. In multivariable analysis (Table E3) adjusting for demographics, tumor characteristics, surgery, stage, adjuvant therapy, and year of surgery, there was no significant association between TSP enrollment and the hazard of a second primary lung tumor (HR, 0.98; 95% CI, 0.87-1.11; P = .8). The stage at diagnosis of the second primary lung cancer was similar, with the overwhelming number of patients (TSP 86.0%, non-TSP 84.4%) having a clinical stage I tumor (Table 3).
Extrathoracic Second Primary Malignancy
Extrathoracic second primary malignancy was detected among 69 of 1123 in the TSP cohort and 225 of 2817 in the non-TSP cohort. The most frequent sites of extrathoracic second primary sites were prostate (TSP 25%, non-TSP 21%), breast (17%, 15%), and thyroid (8.7%, 13%). Thirty-nine patients had their extrathoracic malignancy discovered before enrolling in TSP and were included in the non-TSP cohort with regard to detection of extrathoracic primary. In multivariable analysis (Table E4) accounting for time to extrathoracic second primary malignancy, TSP status was significantly associated with greater hazard of extrathoracic second primary malignancies (HR, 1.31; 95% CI, 1.04-1.66; P = .023) (Table 3).
Survival
Median follow-up duration from time of surgery was 6.4 (4.1-9.5) years. After adjusting for demographics, tumor characteristics, surgery, adjuvant therapy, and year of surgery in multivariable analysis (Tables E5 and E6), TSP status was associated with a lower hazard of death (HR, 0.42; 95% CI, 0.33-0.52; P <.001) and a lower hazard of progression or death (HR, 0.42; 95% CI, 0.47-0.67; P < .001).
Analysis Excluding Carcinoid
A total of 340 of 3940 patients were diagnosed with primary lung carcinoid tumor. Of patients ultimately enrolled in TSP, 100 of 1162 (8.6%) and 240 of 2778 (8.6%) in the non-TSP cohort had a pathologic diagnosis of carcinoid. Carcinoid tumors are thought to have a different disease process with better overall survival than lung cancer. To address this potential confounder, the association between TSP enrollment and recurrence, second lung primary, extrathoracic malignancies, and survival were examined in a sensitivity analysis after the exclusion of patients with carcinoid tumors. There was minimal change in the results (Table E1).
DISCUSSION
Both the American College of Surgeons Commission on Cancer1 and the National Cancer Center Network4,14,15 now consider survivorship programs integral to optimal cancer care. However, the methods of follow-up for patients with thoracic cancer are still debated and remain variable.9 Long-term follow-up of patients must include surveillance for both recurrence and second malignancies.16-18 Our novel TSP is associated with high patient compliance, early detection of second primary NSCLC, and excellent survival outcomes. As previously noted, this TSP model, coordinated by specialized nurse practitioners, allows for focused postoperative surveillance and assessment of related medical issues, with the collaborating primary surgeon becoming reinvolved with the patient’s care as needed to evaluate any new concerns.10,19 Patient compliance with follow-up in the TSP was high (97.3%) and better than with follow-up by the primary surgeon (96.4%, P = .009.)
The identification of second primary lung cancers is very important for patients who have undergone lung cancer resection, with 12% of patients in both the TSP and non-TSP cohorts developing a second primary lung cancer in our study. The overwhelming majority of these second lung cancers were found at an early clinical stage, making them amenable to early curative-intent local intervention with surgery or SBRT.7,19,20 Our results are consistent with recommendations from the American Cancer Society that detection of second primary lung cancers be part of follow-up care for patients who have undergone surgery.18,21
Recurrence rates were different between patients followed in the non-TSP cohorts versus the TSP cohort. Patients in the non-TSP cohort were more likely to have received neoadjuvant therapy and to have later-stage tumors, predisposing them to have a greater chance of recurrence. Because enrollment in our TSP program is based on the operating surgeon’s discretion, patients with more advanced disease may be followed more frequently by their primary surgeon, illustrating a selection bias. Although we tried to control for this in the multivariable analysis, this probable selection bias potentially explains why patients in the non-TSP cohort had a lower survival and greater recurrence rates. The approach to enrollment into the TSP at the discretion of the operating surgeon permits the surgeon to follow some patients closely while transitioning others to the nurse practitioner-based TSP. This helps offload the surgeon’s outpatient practice, allowing them to focus on more complex medical issues while ensuring safe and effective long-term care.10,22,23
The identification of extrathoracic malignancies, although relatively low (6.1% in TSP vs 8.0% in non-TSP), is another important aspect of any survivorship program. These malignancies may be found at any point in time during post-therapy surveillance and are a crucial part of the overall patient assessment. Routine cancer screening tests such as mammograms, colonoscopies, and prostate exams along with close coordination with primary care providers and oncologists are part of the cornerstone for a robust TSP.4,14,22-25 Our TSP nurse practitioners are trained to ensure that all patients undergo standard screening for extrathoracic malignancies.
Since the Coronavirus Disease 2019 pandemic, the TSP program has largely transitioned to a virtual platform. This transition to telemedicine has ensured continued follow-up care for our predominantly older patient population.26 Although we have not examined the details in this study, the TSP potentially offers savings in health care costs, exchanging the costs of a physician-based visit for a lower cost, independent nurse practitioner–based visit.27
Study Limitations
This analysis has all the limitations inherent in a retrospective study. There is selection bias of patients enrolled in the TSP. Surgeons decided which patients would be enrolled in the TSP and were more likely to continue personally following patients who had more advanced stage disease at diagnosis. In addition, some surgeons elected not to use the TSP, but preferred to follow their own patients long-term. We considered this in our analyses by incorporating potential surgeon effects as stratification factors within the models.
CONCLUSIONS
Overall, this study shows that our TSP, run by highly trained nurse practitioners in collaboration with the operating surgeon, is an excellent care model. This model can be adapted by smaller centers as a framework for survivorship care, even if the dedicated nurse practitioner has other responsibilities. The high level of patient compliance in the TSP speaks to the extent of patient satisfaction with this approach. Additional studies may verify the implications for health care costs.
Supplementary Material
CENTRAL MESSAGE.
We analyzed compliance and long-term outcomes for surgically resected patients with lung cancer enrolled in our TSP that included close coordination between nurse practitioners and surgeons. Outcomes were not significantly different between patients enrolled in TSP versus those not. This can have consequences on health care costs and resource use.
PERSPECTIVE.
Survivorship programs are now considered integral to optimal cancer care. However, methods of follow-up after resection of NSCLC remain variable. Based on 15 years of experience in more than 1100 patients, our novel TSP, managed by highly trained nurse practitioners, is associated with high patient compliance and excellent outcomes.
Discussion.
Presenter: Dr Hari B. Keshava

Dr Paula A. Ugalde (Quebec City, Quebec, Canada). This is an interesting subject. Do you think this program is applicable to academic and nonacademic centers?

Dr Hari B. Keshava (New York, NY). I think it’s applicable to all types of centers. Of course, follow-up is needed. As we showed, second lung primaries or even second extrathoracic primary cancers do exist, and these patients need follow-up and surveillance for these second primary lung cancers. I think this can be done both in a setting of academia and a nonacademic setting.
Dr Ugalde. Do you think that the strength of your study is that you showed that the identification of second primaries were similar between both groups? Do you think that that’s the most important key factor to determine efficacy?
Dr Keshava. I agree exactly with what you’re saying. The fact that they are similar allows us to allocate resources appropriately. Surgeon clinics can get bogged down. You start following your patients lifelong, and it can become difficult to see these patients all the time. I think in a setting like we have shown here with this type of survivorship follow-up helps to allow close coordination with nurse practitioners—and with them sending the patients back once they notice something that has changed on the CT scans. These nurse practitioners are astute in looking at the CT scans themselves and noticing any differences. They know what to look for and what questions to ask the patients, and I think that it helps tremendously to have these types of programs set up and in practice.
Dr Ugalde. Great. Why do you think this is a cost-effective program? Is it because physicians are not required?
Dr Keshava. I think the time spent by nurse practitioners and the reimbursement rates, especially in the United States, are different between nurse practitioners and surgeons. And if you’re able to have specifically trained nurse practitioners spend the time with the patients (which surgeons may not be able to do because they’re in the operating room or seeing other types of patients), we can actually have our nurse practitioners help with those patients. Looking toward the future, we are starting to see more virtual visits being done, especially in this era of Coronavirus Disease 2019, and these nurse practitioners can help with those virtual visits—in assessing the patients, looking at the CT scans, and making sure everything is okay with those patients.
Dr Ugalde. When do you think it would be the perfect timing for either the surgeon or the clinic to enroll the patient? That’s my first question—perfect timing for followup of the patient. My second question is do the patients feel comfortable with this? Do the patients ask if they will see a physician? Is that a problem? Is that a limitation for the patients, in your opinion?
Dr Keshava. We actually showed in our first article about the thoracic survivorship program at Memorial Sloan-Kettering Cancer Center that enrollment into the program was helpful when you actually had both a surgeon and the nurse practitioner following these patients there, at the time of enrollment into the thoracic survivorship program.
Usually, this would occur at 2 years of follow-up. So at that point, we thought it was the optimal time to enroll these patients. The patients were receptive when they understood that they would get close follow-up and that there still would be close coordination with the nurse practitioners and the primary operating surgeon. As long as there’s a good dialogue with the patients, I think the patients are receptive to this.
Dr Ugalde. What would be the perfect timing? One-year follow-up? Two-year follow-up?
Dr Keshava. I think at the second-year follow-up, enrolling patients in the thoracic survivorship program is a perfect time because at that point, the chance of a recurrence is probably decreased. We’re starting to go to more annual visits and these specifically trained nurse practitioners know exactly what to ask, what to look for, and how to document what’s going on.
Dr Ugalde. Just out of curiosity, how many patients do you think that a nurse practitioner is able to see in a day?
Dr Keshava. I would say they could see anywhere from 8 to 10 patients in this type of setting, along with other patients who need to come into the clinic. So maybe some virtual, some coming into the clinic. I think that’s an appropriate volume for a thoracic survivorship nurse practitioner.
Dr Ugalde. Do you think you will be able to establish this program where you’re working in southern California?
Dr Keshava. I do think that. This research was done when I was a fellow at Memorial Sloan-Kettering. However, now in my new practice, I have been tasked with helping to start a survivorship program in our cancer center. I’m going to use and show these data to help get a nurse practitioner-run survivorship program at my current institution.
Dr Ugalde. That is the perfect way to align your training with your career. So hopefully, you’ll be successful in that.
Acknowledgments
This work was supported in part by National Institutes of Health/National Cancer Institute Cancer Center Support Grant P30 CA008748.
The study was approved by the Memorial Sloan Kettering Cancer Center Institutional Review Board, under a retrospective research protocol, Institutional Review Board No. 20-054, approved on February 12, 2020, with waiver for informed patient consent.
Abbreviations and Acronyms
- CI
confidence interval
- CT
computed tomography
- HR
hazard ratio
- NSCLC
non–small cell lung cancer
- TSP
Thoracic Survivorship Program
Footnotes
Webcast
You can watch a Webcast of this AATS meeting presentation by going to: https://aats.blob.core.windows.net/media/21%20AM/AM21_TH07/AM21_TH07_8.mp4.
Conflict of Interest Statement
The authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
References
- 1.American College of Surgeons Commission on Cancer. 2020 Standards and Resources. Website. Accessed April 22, 2021. https://www.facs.org/quality-programs/cancer/coc/standards/2020
- 2.Hewitt ME, Greenfield S, Stovall E. The National Cancer Policy Board. From Cancer Patient to Cancer Survivor: Lost in Transition. National Academies Press; 2006. [Google Scholar]
- 3.Stricker CT, O’Brien M. Implementing the Commission on Cancer standards for survivorship care plans. Clin J Oncol Nurs. 2014;18(Suppl):15–22. [DOI] [PubMed] [Google Scholar]
- 4.McGrath EB, Schaal A, Pace C. The integration of survivorship care planning at a comprehensive cancer center. J Adv Pract Oncol. 2019;10:461–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lou F, Sima CS, Rusch VW, Jones DR, Huang J. Differences in patterns of recurrence in early-stage versus locally advanced non-small cell lung cancer. Ann Thorac Surg. 2014;98:1755–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Martini N, Bains MS, Burt ME, Zakowski MF, McCormack P, Rusch VW, et al. Incidence of local recurrence and second primary tumors in resected stage I lung cancer. J Thorac Cardiovasc Surg. 1995;109:120–9. [DOI] [PubMed] [Google Scholar]
- 7.Ripley RT, McMillan RR, Sima CS, Hasan SM, Ahmad U, Lou F, et al. Second primary lung cancers: smokers v. nonsmokers after resection of stage I lung adenocarcinoma. Ann Thorac Surg. 2014;98:968–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Varlotto JM, Recht A, Flickinger FW, Medford-Davis LN, Dyer A-M, DeCamp MM. Varying recurrence rates and risk factors associated with different definitions of local recurrence in patients with surgically resected, stage I non-small cell lung cancer. Cancer. 2010;116:2390–400. [DOI] [PubMed] [Google Scholar]
- 9.Calman L, Beaver K, Hind D, Lorigan P, Roberts C, Lloyd-Jones M. Survival benefits from follow-up of patients with lung cancer. J Thorac Oncol. 2011;6: 1993–2004. [DOI] [PubMed] [Google Scholar]
- 10.Huang J, Logue AE, Ostroff JS, Park BJ, McCabe M, Jones DR, et al. Comprehensive long-term care of patients with lung cancer: development of a novel thoracic survivorship program. Ann Thorac Surg. 2014;98:955–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Martini N, Melamed MR. Multiple primary lung cancers. J Thorac Cardiovasc Surg. 1975;70:606–12. [PubMed] [Google Scholar]
- 12.Chang JC, Alex D, Bott M, Tan KS, Seshan V, Golden A, et al. Comprehensive next-generation sequencing unambiguously distinguishes separate primary lung carcinomas from intrapulmonary metastases: comparison with standard histopathologic approach. Clin Cancer Res. 2019;25: 7113–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang Z, Reinkainen J, Adeleke KA, Pieterse ME, Groothuis-Oudshoorn CGM. Time-varying covariates and coefficients in Cos regression models. Ann Transl Med. 2018;6:121–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Krebs P, Coups EJ, Feinstein MB, Burkhalter JE, Steingart RM, Logue A, et al. Health behaviors of early-stage non-small cell lung cancer survivors. J Cancer Surviv. 2012;6:637–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Denlinger CS, Sanft T, Mosiehi JJ, Overholser L, Armenian S, Baker KS, et al. NCCN guidelines insights: survivorship, version 2.2020. J Natl Compr Canc Netw. 2020;18:1016–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brown C, Cataldo J. Explorations of lung cancer stigma for female long term survivors. Nurs Inq. 2013;20:352–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Korst RJ, Kansler AL, Port JL, Lee PC, Altorki NK. Accuracy of surveillance computed tomography in detecting recurrent or new primary lung cancer in patients with completely resected lung cancer. Ann Thorac Surg. 2006;82: 1009–15. [DOI] [PubMed] [Google Scholar]
- 18.Pozo CLP, Morgan MA, Gray JE. Survivorship issues for patients with lung cancer. Cancer Control. 2014;21:40–50. [DOI] [PubMed] [Google Scholar]
- 19.Lou F, Huang J, Sima CS, Dycoco J, Rusch V, Bach PB. Patterns of recurrence and second primary lung cancer in early-stage lung cancer survivors followed with routine computed tomography surveillance. J Thorac Cardiovasc Surg. 2013;145:75–82. [DOI] [PubMed] [Google Scholar]
- 20.Steber CR, Hughes RT, Soike MH, Helis CA, Nieto K, Jacobson T, et al. Stereotactic body radiotherapy for synchronous early stage non-small cell lung cancer. Acta Oncol. 2021;60:605–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith T, Stein KD, Mehta CC, Kaw C, Kepner JL, Buskirk T, et al. The rationale, design, and implementation of the American Cancer Society’s studies of cancer survivors. Cancer. 2007;109:1–12. [DOI] [PubMed] [Google Scholar]
- 22.Moore S, Corner J, Haviland J, Wells M, Salmon E, Normand C, et al. Nurse led follow up and conventional medical follow up in management of patients with lung cancer: randomised trial. Br Med J. 2002;325:1145–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moore S, Wells M, Plant H, Fuller F, Wright M, Corner J. Nurse specialist led follow-up in lung cancer: the experience of developing and delivering a new model of care. Eur J Oncol Nurs. 2006;10:364–77. [DOI] [PubMed] [Google Scholar]
- 24.Cowens-Alvarado R, Sharpe K, Pratt-Chapman M, Willis A, Gansler T, Ganz PA, et al. Advancing survivorship care through the National Cancer Survivorship Resource Center. CA Cancer J Clin. 2013;63:147–50. [DOI] [PubMed] [Google Scholar]
- 25.Nekhlyudov L, Aziz NM, Lerro C, Virgo KS. Oncologists’ and primary care physicians’ awareness of late and long-term effects of chemotherapy: implications for care of the growing population of survivors. J Oncol Pract. 2014;10: e29–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hill-Kayser CE, Vachani C, Hampshire MK, Jacobs LA, Metz JM. Utilization of internet-based survivorship care plans by lung cancer survivors. Clin Lung Cancer. 2009;10:347–52. [DOI] [PubMed] [Google Scholar]
- 27.Rosales AR, Byrne D, Burnham C, Watts L, Clifford K, Zuckerman DS, et al. Comprehensive survivorship care with cost and revenue analysis. J Oncol Pract. 2014;10:e81–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


