Abstract
Background
This study examined the impact of COVID‐related disruptions on mental health and substance use in young people residing in a state with an initially lower COVID burden and earlier reopening of in‐person learning than other states.
Methods
Data come from Waves 3 (Fall 2019) and 4 (Fall 2020) of the Policy and Communication Evaluation (PACE) Vermont, an online cohort study of adolescents (ages 12–17) and young adults (ages 18–25). Participants in Wave 4 (212 adolescents; 662 young adults) completed items on COVID‐related stressors, the impact of the pandemic on their substance use, brief mental health scales, and past 30‐day substance use. Analyses examined correlational and longitudinal relationships between COVID‐related stressors, mental health symptoms, and substance use.
Results
More than 60% of participants noted negative effects of the pandemic on their physical, emotional, and social well‐being, with greater impacts of COVID‐related stressors in young adults than adolescents. There were significant increases in depressive (OR 1.31, 95% CI 1.03, 1.66) and anxiety symptoms (OR 1.34; 95% CI 1.10, 1.64) in young adults between Fall 2019 and Fall 2020. Higher overall COVID Impact scores were associated with higher odds of depressive and anxiety symptoms, as well as past 30‐day electronic vapor product use, in adjusted cross‐sectional and longitudinal models.
Conclusions
Robust associations between COVID‐related distress, mental health, and substance use outcomes in young people signal the opportunity to increase evidence‐based interventions while adding novel approaches to minimize longer‐term harms of the pandemic on mental health in adolescents and young adults.
Keywords: Adolescent, youth, young adult, COVID‐19, mental health, substance use, anxiety, depression
Key Practitioner Message.
Findings detail increases in anxiety and depressive symptoms in adolescents and young adults in the fall of 2020, compared with a similar sample a year earlier.
COVID‐related stressors were positively correlated with an overall measure of COVID impacts. Where there were differences by age group in COVID‐related stressors, young adults reported a greater impact of these stressors on their lives, compared with adolescents.
Higher COVID Impact scores were associated with higher odds of depressive and anxiety symptoms, as well as past 30‐day use of electronic vapor products in both cross‐sectional and longitudinal analyses, controlling for potential confounders.
A sizeable proportion of past 30‐day substance users reported increases in substance use since they learned about the coronavirus pandemic.
Screening young people for COVID distress and mental health in schools, workplaces, and clinical settings may reduce the potential impact of mental health issues on social and educational functioning. This may be particularly important in higher education, given greater distress experienced by young adults.
Beyond individual screenings, class, school, or population‐level interventions promoting community and mental health wellness (e.g., sleep, nutrition, and exercise) may mitigate the negative impacts of COVID distress on mental health and substance use.
Introduction
The social and economic impacts of the COVID‐19 pandemic are likely to have both direct and indirect effects on the health of youth and young adults over the long‐term, with mental health symptoms and substance use playing an important role in long‐term COVID‐related morbidity and mortality. COVID‐19 has been identified as significantly increasing substance use and its related risks among adults (Volkow, 2020). National studies document increases in mental health symptoms in response to COVID‐related stressors (Czeisler et al., 2020; Fitzpatrick, Drawve, & Harris, 2020; McGinty, Presskreischer, Anderson, Han, & Barry, 2020). Mental health symptoms, in turn, are correlated with tobacco and substance use in adolescents (Conway et al., 2013, 2017; Silveira, Green, Iannaccone, Kimmel, & Conway, 2019) and adults (Conway et al., 2017; Parker, Sigmon, & Villanti, 2019; Parker & Villanti, 2021). Increases in substance use prevalence and frequency during the COVID‐19 pandemic have been documented through surveys (Klemperer, West, Peasley‐Miklus, & Villanti, 2020) and clinical lab testing (Niles, Gudin, Radcliff, & Kaufman, 2020), with concurrent increases in drug overdoses (Alter & Yeager, 2020). Federal data have also highlighted the first increase in annual cigarette sales in twenty years in 2020 (Federal Trade Commission, 2021), as well as increases in suicides in young adults in 2020 compared with 2019 (Curtin, Hedegaard, & Ahmad, 2021).
Disruptions in social interactions typical of adolescence and young adulthood during the COVID pandemic may have resulted in reductions in peer and school influences that impact substance use (Richter, 2020). However, the consequences of social deprivation in youth have been identified by researchers as a concern during the pandemic, given the importance of peer interactions in development during adolescence (Orben, Tomova, & Blakemore, 2020; Waselewski, Waselewski, & Chang, 2020). Reductions in these prosocial influences may induce feelings of social isolation; greater time at home may also result in greater exposure to parental or household substance use (Richter, 2020). Both of these factors are likely to put young people at risk for greater mental health symptoms and substance use.
Few studies have addressed direct impacts of the COVID‐19 pandemic on changes in substance use among adolescents and young adults. Two Canadian studies documented reductions in substance use among adolescents in clinical and community cohorts (Dumas, Ellis, & Litt, 2020; Hawke et al., 2020), though one of them noted greater frequency of alcohol and marijuana use among continuing users (Dumas et al., 2020). The latter study also documented a high prevalence of substance use with parents during COVID (42%) and the strong correlation between depression and solitary substance use, supporting concerns about increased risk for substance use resulting from more time at home (Dumas et al., 2020).
Vermont was an early national leader in COVID management and in March 2020, ‘Stay Home, Stay Safe’ orders were issued, with schools closing for the remainder of the academic year and colleges transitioning to remote learning for the end of the spring semester. Vermont phased in the reopening of schools in fall 2020 (State of Vermont, 2020), with most Vermont middle and high schools adopting a hybrid (in‐person/remote) learning model, many students in school 2 days/week, and competitive high school sports underway. Vermont colleges also brought students back to campus in Fall 2020, with hybrid course models and rigorous COVID testing. The result of these changes was a gradual reintroduction to normal school and work routines for young people across the state, preceding many other US states. Increased socialization may have reduced feelings of social isolation and yet, provided more opportunities for substance use with peers; it may also have increased anxiety for young people. Returning to regular routines amidst rising COVID‐19 cases or during widespread vaccination may introduce new stressors for young people as well.
The goal of our study was to examine the prevalence of COVID‐related distress in Vermont adolescents and young adults in Fall 2020 and to explore the relationships between COVID‐related distress, mental health symptoms, and substance use in this population in both cross‐sectional and longitudinal analyses.
Methods
Data for the current analyses come from Waves 3 and 4 of the Policy and Communication Evaluation (PACE) Vermont study, an online cohort recruited via digital and print ads, as well as participant referrals. Wave 3 took place from September to October 2019, approximately 5 months before the onset of the COVID‐19 pandemic in the United States and included 1095 participants (350 adolescents ages 12–17 and 745 young adults ages 18–25). Wave 4 was conducted from September to October 2020, approximately 6 months following the beginning of the COVID‐19 pandemic in the United States and subsequent statewide ‘Stay Home, Stay Safe’ executive order in Vermont. Of the 874 participants in Wave 4, 212 were adolescents and 662 were young adults; 314 (36%) had also completed Wave 3 (88 adolescents and 226 young adults). At the time of enrollment, all participants provided consent electronically; adolescents required parental consent in an online form sent directly to a parent contact prior to providing assent in their own form. This research was approved by the University of Vermont’s Institutional Review Board (STUDY00000810) and received a Certificate of Confidentiality from the National Institutes of Health. Details of recruitment and study methods have been described elsewhere (Villanti et al., 2020).
Measures
COVID‐related distress
Table 1 presents 20 items on COVID‐related stress captured in Wave 4 adapted from the COVID‐19 Exposure and Family Impact Survey for Adolescents and Young Adults (CEFIS‐AYA, 2020) and the National Institutes of Health's Coronavirus Health Impact Survey (CRISIS, 2020). Three items from the CRISIS asked participants how difficult the following things in their life had been since the start of the COVID‐19 pandemic: cancellation of important events (such as graduation, prom, vacation, etc.); changes in daily activities (e.g., afterschool activities, online school, and sports); and financial (money) problems for you and your family. Three other CRISIS items asked participants to what degree they had been concerned about the following: the stability of your living situation (or having to move); the impact of COVID‐19 on your school or work; and whether your food would run out because of a lack of money. All six CRISIS items were assessed on a five‐point Likert scale, with response options ‘not at all’, ‘slightly’, ‘moderately’, ‘very’, and ‘extremely’. Responses were recoded as dichotomous with ‘very’ and ‘extremely’ collapsed as 1 and ‘not at all’, ‘slightly’, and ‘moderately’ collapsed as 0.
Table 1.
Adolescent and young adult response to COVID‐related stressors, PACE Vermont Study, September 2020 (n = 874)
| Adolescents | Young adults | Total | p‐value | ||||
|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | ||
| Since the start of the COVID‐19 pandemic, how much have the following things in your life been difficult for you? (Percent reporting ‘very’ or ‘extremely’ difficult) | |||||||
| Cancellation of important events | 100 | 47.2 | 323 | 48.8 | 423 | 48.4 | .681 |
| Changes in daily activities | 126 | 59.4 | 422 | 63.7 | 548 | 62.7 | .258 |
| Financial (money) problems for you or your family a | 22 | 10.4 | 169 | 25.6 | 191 | 21.9 | <.001 |
| Since the start of the COVID‐19 pandemic, to what degree have you been concerned about the following? (Percent reporting ‘very’ or ‘extremely’ concerned) | |||||||
| Stability of your living situation | 11 | 5.2 | 140 | 21.1 | 151 | 17.3 | <.001 |
| Impact of COVID‐19 on your school or work | 93 | 43.9 | 437 | 66.0 | 530 | 60.6 | <.001 |
| Whether your food would run out a | 8 | 3.8 | 85 | 12.9 | 93 | 10.7 | <.001 |
| COVID‐19 may have many impacts on you and your family life. In general, how has the COVID‐19 pandemic affected each of the following? (Percent reporting made it ‘a little’ or ‘a lot’ worse) | |||||||
| How family/household members get along a | 101 | 47.9 | 283 | 42.7 | 384 | 44.0 | .192 |
| Ability to care for your health a | 62 | 29.4 | 298 | 45 | 360 | 41.2 | <.001 |
| Ability to be independent a | 77 | 36.5 | 319 | 48.2 | 396 | 45.4 | .003 |
| Ability to care for others in your family a | 39 | 18.5 | 258 | 39 | 297 | 34.0 | <.001 |
| Your physical well‐being | |||||||
| Sedentary behavior a | 161 | 76.3 | 523 | 79 | 684 | 78.4 | .407 |
| Exercise/physical activity a | 112 | 53.1 | 421 | 63.6 | 533 | 61.1 | .006 |
| Eating b | 110 | 52.4 | 435 | 65.7 | 545 | 62.5 | .001 |
| Sleeping a | 102 | 48.3 | 385 | 58.2 | 487 | 55.8 | .012 |
| Substance use a | 26 | 12.3 | 304 | 45.9 | 330 | 37.8 | <.001 |
| Your emotional well‐being | |||||||
| Anxiety/worry a | 151 | 71.6 | 579 | 87.5 | 730 | 83.6 | <.001 |
| Mood a | 143 | 67.8 | 558 | 84.3 | 701 | 80.3 | <.001 |
| Loneliness a | 167 | 79.1 | 542 | 81.9 | 709 | 81.2 | .377 |
| Your social well‐being | |||||||
| Relationships with friends b | 140 | 66.4 | 501 | 75.8 | 641 | 73.5 | .007 |
| Romantic relationships a | 66 | 31.3 | 400 | 60.4 | 466 | 53.4 | <.001 |
n = 1 observation missing.
n = 2 observations missing.
Of the 16 items on the CEFIS‐AYA Impact scale, 14 asked about the impact of the COVID‐19 pandemic on participants and their families, addressing their ability to care for their own health and others; ability to be independent; and their physical, emotional, and social well‐being. The one item excluded from the scale related to ‘parenting your children’, as it was deemed unlikely to be applicable to the majority of the sample. Response options were ‘made it a lot better’ (1), ‘made it a little better’ (2), ‘made it a little worse’ (3), ‘made it a lot worse’ (4), and ‘not applicable’ (0). The final item from the CEFIS‐AYA asked ‘overall, how much distress have you experienced related to COVID‐19’? with responses on a 10‐point Likert scale from 1 (No distress) to 10 (Extreme distress); we describe this measure as ‘overall COVID distress’. First, the CEFIS‐AYA COVID Impact Score was calculated by summing all 15 responses per recommended scoring (CEFIS‐AYA, 2020). Next, responses to the 14 categorical items were recoded as dichotomous with ‘made it a little worse’ and ‘made it a lot worse’ categorized as 1, ‘made it a little better’, ‘made it a lot better’, and ‘not applicable’ as 0.
Mental health symptoms
Waves 3 and 4 of the PACE Vermont Study included measures of depressive symptoms using the Patient Health Questionnaire‐2 (PHQ‐2) and anxiety using the Generalized Anxiety Disorder 2‐item (GAD‐2) scales (Kroenke, Spitzer, & Williams, 2003; Kroenke, Spitzer, Williams, Monahan, & Lowe, 2007). Analyses used a scoring cutoff of ≥3 on the scale to be classified as having depressive (PHQ‐2) or anxiety (GAD‐2) symptoms.
Substance use
Waves 3 and 4 of the PACE Vermont Study included measures on past 30‐day substance use, including cigarette, electronic vapor product (EVP), alcohol, and marijuana use as in our previous studies (Villanti et al., 2020). Additional items were developed at Wave 4 to capture changes in substance use due to COVID‐19 among participants who reported ever use of cigarettes, EVPs, alcohol, or marijuana; for each substance, respondents were asked to report any changes in use of each of the products since they learned about the coronavirus pandemic, with response choices of ‘my [cigarette] use has increased’, ‘my [cigarette] use has stayed the same’, ‘my [cigarette] use has decreased’, or ‘other (please specify)’.
Other covariates
All participants responded to items assessing their age, sex, gender identity, sexual identity, and current enrollment in school or a degree program at Wave 4. Age group was a categorical variable with two‐levels: adolescents (ages 12–17) and young adults (ages 18–25). Education completed was assessed among young adults only. Socioeconomic status among adolescents was assessed using the MacArthur Scale of Subjective Social Status–Youth Version (Goodman et al., 2001) and among young adults, using a validated subjective financial status measure (Williams et al., 2017). Rural residence was determined by county of residence using the list created by the Federal Office of Rural Health Policy (Health Resources & Services Administration, 2018).
Analyses
Analyses were conducted in Stata, Version 15. Bivariate analyses described the characteristics of the Wave 4 PACE Vermont sample and the prevalence of COVID‐related stressors, past 30‐day substance use, and change in substance use resulting from COVID in adolescents compared with young adults. Linear regression models assessed the relationships between demographics and COVID Impact Score in bivariate and multivariable models. Linear regression models examined the correlation between specific COVID‐related stressors and COVID Impact Score, alone and adjusted for correlates of COVID Impact Score (age group, sex, gender, sexual identity, race/ethnicity, and current enrollment in school/degree program). The overall prevalence of mental health symptoms and by age group was compared in the full Wave 3 and Wave 4 samples, accounting for repeated measures within subjects. Multivariable logistic regression analyses were conducted in participants completing both survey waves to determine the potential impact of COVID‐19 distress on changes in mental health symptoms and substance use between 2019 and 2020. Multivariable logistic regression models in the longitudinal sample also examined the association between mental health symptoms and past 30‐day substance use in Fall 2020, controlling for COVID Impact Score, correlates of COVID distress, and Fall 2019 substance use.
Results
Demographics
In total, 874 Vermont adolescents (n = 212) and young adults (n = 662) participated in Wave 4 of the PACE Vermont study. Table S1 describes the characteristics of the included sample. The majority of participants were female (71%, n = 614), cisgender (94%; n = 819), white (82%; n = 717), and reported being straight/heterosexual (67%; n = 589). Seven percent (n = 64) were non‐white/other race and 11% (n = 92) were Hispanic. The mean age of adolescent participants was 15.0 years [standard deviation (SD) 1.6] and the mean age of young adult participants was 21.5 years (SD 2.2). Compared with Vermont population statistics from 2019 (Vermont Department of Health, 2020b), the PACE Vermont 2020 sample had a higher proportion of females (adolescents: 64% vs. 49%; young adults: 73% vs. 49%) and a lower proportion of rural residents (adolescents: 55% vs. 65%; young adults: 47% vs. 54%). The breakdown for other demographic variables (race/ethnicity and gender identity) was similar to the Vermont’s Youth Risk Behavior Survey (Vermont Department of Health, 2020a).
Wave 3 participants who continued in Wave 4 (n = 314) were less likely to report past 30‐day cigarette use (8% vs. 13%), EVP use (13% vs. 23%), and marijuana use (23% vs. 31%; all p < .05) than those who did not continue. Those retained did not differ from those lost to follow‐up by age, sex, gender identity, sexual identity, race/ethnicity, current enrollment in school/degree program, rural residence, mental health symptoms, or past 30‐day alcohol use.
COVID‐related distress
Table 1 presents the prevalence of COVID‐related stressors by age group. In general, >60% of young people noted worse conditions during COVID for nine of the 20 items assessed: this included difficulty with changes in daily activities since the start of the COVID‐19 pandemic (62.7%), as well as concern about the impact of COVID‐19 on school and work (60.6%), and reporting that the pandemic made many aspects of physical, emotional, and social well‐being worse. Where there were differences in COVID‐related stressors by age group, they favored a worse experience among young adults compared with adolescents, with important differences by financial problems (25.6% in young adults vs. 10.4% in adolescents) and food insecurity (12.9% vs. 3.8%). Young adults reported a higher prevalence of COVID worsening exercise/physical activity, eating, sleeping, substance use, anxiety/worry, mood, relationships with friends, and romantic relationships compared with adolescents. Young adults also endorsed higher COVID Impact scores (mean 42.4, SD 9.8) than adolescents (mean 35.4, SD 10.6). Age, sex, sexual identity, race/ethnicity were correlated with COVID Impact Score in bivariate and multivariable models; gender identity and current enrollment in school or a degree program were correlated with higher COVID Impact Scores in bivariate analyses only (Table S2). Endorsement of each of the dichotomized CRISIS and CEFIS‐AYA items was associated with a 3.75–12.96‐point increase in the COVID Impact Score, controlling for age, sex, gender identity, sexual identity, race/ethnicity, and current enrollment in school/degree program (Table S3). In adjusted analyses, endorsing worse anxiety/worry, mood, or loneliness as a result of COVID was correlated with a more than 12‐point higher COVID Impact Score than those who reported that their emotional well‐being was better during COVID.
COVID‐19 and mental health symptoms
Figure 1 shows higher levels of depressive (p = .002) and anxiety symptoms (p < .001) in adolescents and young adults in the fall of 2020 (Wave 4) compared with the fall of 2019 (Wave 3), with significant increases seen in depressive (OR 1.31, 95% CI 1.03, 1.66) and anxiety symptoms (OR 1.34; 95% CI 1.10, 1.64) in young adults, accounting for repeated measures. In the Wave 4 sample, there were strong correlations between COVID Impact Score and mental health symptoms, such that a one‐point increase in the COVID Impact Score was correlated with a 8% higher odds of anxiety symptoms (95% CI 1.06, 1.10) and a 9% higher odds of depressive symptoms (95% CI 1.07, 1.12), controlling for covariates (Table 2). Analyses of the subsample of participants completing both waves showed that COVID Impact Score was similarly associated with higher odds of depressive and anxiety symptoms at Wave 4 controlling for Wave 3 symptoms and other covariates.
Figure 1.
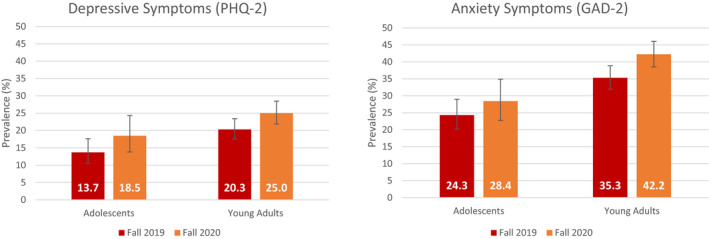
Percentage of adolescents and young adults reporting depressive or anxiety symptoms in Fall 2019 versus Fall 2020, PACE Vermont Study
Table 2.
Associations between COVID Impact score, mental health symptoms, and past 30‐day substance use in adolescents and young adults, PACE Vermont Study, September 2020 (n = 865)
| COVID Impact score | ||||||
|---|---|---|---|---|---|---|
| Unadjusted | Adjusted a | |||||
| n | OR | (95% CI) | n | AOR | (95% CI) | |
| Mental health outcomes | ||||||
| Depressive symptoms | ||||||
| Wave 4 sample | 873 | 1.10** | (1.08–1.12) | 867 | 1.09** | (1.07–1.12) |
| Longitudinal sample b | 314 | 1.09** | (1.05–1.13) | 313 | 1.10** | (1.05–1.14) |
| Anxiety symptoms | ||||||
| Wave 4 sample | 873 | 1.10** | (1.08–1.12) | 867 | 1.08** | (1.06–1.10) |
| Longitudinal sample b | 314 | 1.10** | (1.06–1.13) | 313 | 1.08** | (1.04–1.11) |
| Substance use outcomes | ||||||
| Past 30‐day cigarette use | ||||||
| Wave 4 sample | 874 | 1.05** | (1.02–1.07) | 868 | 1.02 | (0.99–1.05) |
| Longitudinal sample b | 314 | 1.05 | (0.99–1.11) | 313 | 1.03 | (0.97–1.10) |
| Past 30‐day EVP use | ||||||
| Wave 4 sample | 874 | 1.06** | (1.04–1.08) | 868 | 1.05** | (1.02–1.07) |
| Longitudinal sample b | 314 | 1.05* | (1.01–1.09) | 302 | 1.05* | (1.01–1.10) |
| Past 30‐day alcohol use | ||||||
| Wave 4 sample | 871 | 1.05** | (1.04–1.07) | 865 | 1.04** | (1.02–1.05) |
| Longitudinal sample b | 308 | 1.03* | (1.00–1.06) | 307 | 1.02 | (0.99–1.05) |
| Past 30‐day marijuana use | ||||||
| Wave 4 sample | 871 | 1.03** | (1.01–1.04) | 866 | 1.01 | (0.99–1.03) |
| Longitudinal sample b | 309 | 1.05* | (1.02–1.10) | 308 | 1.05* | (1.01–1.10) |
*p < .05, **p < .01.
Adjusted models control for age, sex, gender identity, sexual identity, race/ethnicity, and current enrollment in school/degree program.
Unadjusted and adjusted models in the longitudinal sample control for the outcome assessed in Fall 2019 (e.g., Wave 3 depressive symptoms included in the longitudinal models for Wave 4 depressive symptoms).
COVID‐19 and substance use
In the Wave 4 sample, 12% reported past 30‐day cigarette use, 21% EVP use, 57% alcohol use, and 24% marijuana use; for all substances, young adults had significantly higher prevalence of past 30‐day use than adolescents. Between 33% (marijuana) and 44% (alcohol) of past 30‐day substance‐using adolescents and young adults reported that their use of specific substances stayed the same since they learned about the coronavirus pandemic. However, 25% of past 30‐day cigarette users, 24% of past 30‐day EVP users, 34% of past 30‐day alcohol users, and 50% of past 30‐day marijuana users reported increased use since they learned about the coronavirus pandemic (data available upon request). Bivariate analyses in the Wave 4 sample suggested that a 1‐point increase in COVID Impact Score was correlated with higher odds of past 30‐day cigarette use (OR 1.05, 95% CI 1.02, 1.07), EVP use (OR 1.06; 95% CI 1.04, 1.08), alcohol use (OR 1.05, 95% CI 1.04, 1.07), and marijuana use (OR 1.03, 95% CI 1.01, 1.04; Table 2); COVID Impact Score remained correlated with past 30‐day EVP and alcohol use in multivariable models. Analyses of the subsample of participants completing both waves showed that the COVID Impact Score was similarly associated with higher odds of past 30‐day EVP and marijuana use at Wave 4 controlling for Wave 3 use and demographic covariates (Table 2). Adjusted results in the longitudinal subsample on the relationship between COVID Impact Score, past 30‐day EVP use, and past 30‐day marijuana use were not attenuated by the addition of Wave 4 depressive and anxiety symptoms to the model (results not shown).
Discussion
The current observational study describes significant negative impacts of the COVID‐19 pandemic on distress and physical, emotional, and social well‐being in Vermont adolescents and young adults, approximately six months after early restrictions and the closure of schools, but concurrent with the reopening of limited in‐person learning in the state. Importantly, where there were differences by age group in COVID‐related stressors, young adults reported a greater impact of these stressors on their lives, compared with adolescents. Earlier findings in a sample of Vermont college students documented decreases in mood during the semester in which the COVID‐19 pandemic began (Copeland et al., 2021); findings from our study detail increases in anxiety and depressive symptoms in young adults in the fall of 2020, compared with a similar sample a year earlier. COVID‐related stressors were positively correlated with COVID Impact Score, particularly items assessing the impact of COVID on anxiety/worry, mood, and loneliness. Similarly, there were strong positive and consistent correlations between COVID Impact Score and mental health symptoms, even after controlling for known confounders and symptoms a year prior.
A sizeable proportion of past 30‐day substance users in our sample reported increases in use since they learned about the coronavirus pandemic. This is noteworthy since drug use in adolescence is often social and COVID disrupted some of those social opportunities for use. Associations between COVID Impact Score and past 30‐day substance use were present across all four substances in bivariate analyses of the Wave 4 sample, but were limited to past 30‐day EVP and alcohol use after controlling for confounders. Longitudinal models found a relationship between COVID Impact Score and higher odds of past 30‐day EVP use and marijuana use, controlling for use of those substances a year earlier. Novel findings from our study show that the greater the impact of COVID on the lives of young people, the more likely they were to use EVPs. These results are consistent with work by Dumas et al. on solitary substance use and research on the relationship between negative affect and cigarette smoking escalation in adolescents (Weinstein & Mermelstein, 2013).
Strengths of this study include timely data collection in a large sample of adolescents and young adults prior to and during the COVID pandemic. Longitudinal analyses strengthen the internal validity of study findings seen in our cross‐sectional sample. Limitations of this study include the lack of probability‐based sampling, the cross‐sectional nature of COVID data collected in this study, the use of screening rather than diagnostic tools for mental health symptoms, and the homogeneity of the sample. While PACE Vermont participants generally reflect the population of Vermont teens and young adults, findings from this study may not be generalizable to other populations. Additionally, increases in mental health symptoms using two‐item screeners may not reflect clinically meaningful changes in anxiety and depression diagnoses in participants; these increases may be a temporary indication of reaction to stress. Assessing these symptoms 6 months following the start of the COVID pandemic, however, likely captures enduring effects of the pandemic on the lives of young people. The CEFIS‐AYA items asked only in Wave 4 also assessed how COVID‐19 has impacted emotional well‐being, which included anxiety and mood; out of all the CEFIS‐AYA constructs, emotional well‐being had the largest proportion reporting ‘a little’ or ‘a lot’ worse. Together with the screener items, self‐appraisals of the impact of COVID on emotional well‐being suggest the effect of the pandemic on mental health in adolescents and young adults was meaningful. The use of recommended, but not validated, measures of COVID‐related distress is both a strength and a limitation. Multiple scales were created to rapidly assess potential impacts of COVID on mental health, thus our results are comparable with other studies using these measures (Aminoff et al., 2021; Feldman et al., 2021; Mansueto, Lopes, Grassi, & Cosci, 2021; Nikolaidis et al., 2021; Perl, Oren, Klein, & Shechner, 2021). However, rigorous measure development will be needed to disaggregate COVID‐related stress from other stressors as the pandemic resolves and to better understand the long‐term effects of the pandemic on adolescents and young adult mental health and substance use.
Importantly, stressors related to COVID‐19 have not been experienced uniformly by adolescents and young adults and the experience of the COVID‐19 pandemic in Vermont has differed significantly from other states, which may impact the generalizability of our findings. Vermont routinely reported the lowest number of cases and deaths due to COVID‐19 (Centers for Disease Control and Prevention, 2021) and unemployment rates below the national average (Congressional Research Service, 2021). States and individual school districts also vary widely in their approaches to online, in‐person, and hybrid learning (EducationWeek, 2020). Despite the lower per capita number of COVID‐19 cases and deaths as well as unemployment relative to other states, Vermont adolescents and young adults experienced significant negative effects of the pandemic, particularly with regard to social, emotional, and physical well‐being; given the Vermont context, our findings may underestimate the broader impact of COVID on mental health of U.S. young people. Continued monitoring of the impacts of COVID‐19 on adolescents and young adults by state and local authorities, including school districts and colleges, will be needed to respond to community needs.
Conclusion
Findings from our study of Vermont adolescents and young adults suggest young adults experienced greater COVID distress than adolescents which may be partially explained by greater job loss, housing changes, food insecurity, and less family support experienced by this age group (Fry, Passel, & Cohn, 2020; Owens et al., 2020). The instability and social isolation of the pandemic, combined with greater risk for substance use (Arnett, 2005) and onset of mental disorders in young adulthood (Kessler et al., 2007), highlights that young adults may be a group with highest risk for mental health‐related effects of COVID. Young adults are also less likely than adolescents to receive treatment for mental health problems (Copeland et al., 2015), likely due to lack of screening and referral systems embedded in family, school, and health care systems present in adolescence. Screening young people for COVID distress and mental health in schools, workplaces, employment centers, and clinical settings will be necessary to intervene before mental health issues affect social and educational functioning. This may be particularly important in higher education, given greater distress experienced by young adults. Beyond individual screenings, class, school, or population‐level interventions promoting community and mental health wellness (e.g., sleep, nutrition, and exercise) may mitigate the negative impacts of COVID distress on mental health and substance use (Copeland et al., 2021). Our study suggests that broad intervention efforts will likely be needed for all adolescents and young adults, though more intensive efforts may be needed for young adults who may bear a disproportionate burden of the social, economic, and mental health impacts and upheaval of the pandemic.
Ethical information
This research was approved by the University of Vermont’s Institutional Review Board and received a Certificate of Confidentiality from the National Institutes of Health. At the time of enrollment, all participants provided consent electronically; adolescents required parental consent in an online form sent directly to a parent contact prior to providing assent in their own form.
Supporting information
Table S1. Characteristics of adolescent and young adult participants, PACE Vermont Study, September 2020 (n = 874)
Table S2. Demographic correlates of COVID Impact Score, PACE Vermont Study, September 2020
Table S3. Linear regression models of COVID Impact score on individual COVID‐related stressors
Acknowledgements
Research reported in this publication was supported by the National Institute on Drug Abuse of the National Institutes of Health under Award Number R21DA051943, the Vermont Department of Health, the University of Vermont Cancer Center, and the University of Vermont Larner College of Medicine. A.C.V. was also supported in part by Health Resources and Services Administration (HRSA) center of the U.S. Department of Health and Human Services (HHS; grant number UD9 RH33633) from the U.S. Department of Health and Human Services. Although this work product was funded in whole or in part with monies provided by or through the State of Vermont, the State does not necessarily endorse the researchers' findings and/or conclusions. The findings and/or conclusions may be inconsistent with the State's policies, programs, and objectives. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Health Resources and Services Administration. A.C.V. designed and directed the project. A.C.V. and S.E.L. performed the analyses. A.C.V. wrote the first draft of the manuscript and all authors provided feedback and edits on the manuscript. We would like to acknowledge edits on an earlier draft from colleagues in the Alcohol and Drug Abuse Program and Health Surveillance at the Vermont Department of Health. The authors have declared no competing or potential conflicts of interest.
References
- Alter, A. & Yeager, C. (2020). COVID‐19 impact on US national overdose crisis. Available from: http://www.odmap.org/Content/docs/news/2020/ODMAP‐Report‐June‐2020.pdf [last accessed 3 December 2020].
- Aminoff, V. , Sellén, M. , Sörliden, E. , Ludvigsson, M. , Berg, M. , & Andersson, G. (2021). Internet‐based cognitive behavioral therapy for psychological distress associated with the COVID‐19 pandemic: A pilot randomized controlled trial. Frontiers in Psychology, 12, 684540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnett, J.J. (2005). The developmental context of substance use in emerging adulthood. Journal of Drug Issues, 35, 235–254. [Google Scholar]
- Centers for Disease Control and Prevention . (2021). United States COVID‐19 cases and deaths by state over time. Available from: https://data.cdc.gov/Case‐Surveillance/United‐States‐COVID‐19‐Cases‐and‐Deaths‐by‐State‐o/9mfq‐cb36 [last accessed 12 January 2021].
- Congressional Research Service . (2021). Unemployment rates during the COVID‐19 pandemic: In brief. Available from: https://fas.org/sgp/crs/misc/R46554.pdf [last accessed 12 January 2021].
- Conway, K.P. , Green, V.R. , Kasza, K.A. , Silveira, M.L. , Borek, N. , Kimmel, H.L. , … & Compton, W.M. (2017). Co‐occurrence of tobacco product use, substance use, and mental health problems among adults: Findings from Wave 1 (2013–2014) of the Population Assessment of Tobacco and Health (PATH) Study. Drug and Alcohol Dependence, 177, 104–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conway, K.P. , Vullo, G.C. , Nichter, B. , Wang, J. , Compton, W.M. , Iannotti, R.J. , & Simons‐Morton, B. (2013). Prevalence and patterns of polysubstance use in a nationally representative sample of 10th graders in the United States. Journal of Adolescent Health, 52, 716–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland, W.E. , McGinnis, E. , Bai, Y. , Adams, Z. , Nardone, H. , Devadanam, V. , … & Hudziak, J.J. (2021). Impact of COVID‐19 pandemic on college student mental health and wellness. Journal of the American Academy of Child and Adolescent Psychiatry, 60, 134–141 e132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland, W.E. , Shanahan, L. , Davis, M. , Burns, B.J. , Angold, A. , & Costello, E.J. (2015). Increase in untreated cases of psychiatric disorders during the transition to adulthood. Psychiatric Services, 66, 397–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- COVID‐19 Exposure and Family Impact Survey: Adolescent and Young Adult Version (CEFIS‐AYA). (2020, May 8). Available from: https://www.phenxtoolkit.org/toolkit_content/PDF/CPTS_CEFIS_AYA.pdf [last accessed 4 December 2020].
- Curtin, S.C. , Hedegaard, H. & Ahmad, F.B. (2021). Provisional numbers and rates of suicide by month and demographic characteristics: United States, 2020. Vital Statistics Rapid Release; no 16. National Center for Health Statistics; November 2021.
- Czeisler, M.E. , Lane, R.I. , Petrosky, E. , Wiley, J.F. , Christensen, A. , Njai, R. , … & Rajaratnam, S.M.W. (2020). Mental health, substance use, and suicidal ideation during the COVID‐19 pandemic – United States, June 24–30, 2020. MMWR. Morbidity and Mortality Weekly Report, 69, 1049–1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumas, T.M. , Ellis, W. , & Litt, D.M. (2020). What does adolescent substance use look like during the COVID‐19 pandemic? Examining changes in frequency, social contexts, and pandemic‐related predictors. Journal of Adolescent Health, 67, 354–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EducationWeek (2020, January 11, 2021). Map: Where are schools closed? Available from: https://www.edweek.org/leadership/map‐where‐are‐schools‐closed/2020/07 [last accessed 12 January 2021].
- Federal Trade Commission (2021, October 26). Federal Trade Commission Cigarette Report for 2020. Available from: https://www.ftc.gov/reports/federal‐trade‐commission‐cigarette‐report‐2016‐federal‐trade‐commission‐smokeless‐tobacco [last accessed 3 November 2021].
- Feldman, E.C.H. , Balistreri, K.A. , Lampert, S. , Durkin, L.K. , Bugno, L.T. , Davies, W.H. , & Greenley, R.N. (2021). Emerging adults' adherence to preventative health guidelines in response to COVID‐19. Journal of Pediatric Psychology, 46, 635–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzpatrick, K.M. , Drawve, G. , & Harris, C. (2020). Facing new fears during the COVID‐19 pandemic: The State of America's mental health. Journal of Anxiety Disorders, 75, 102291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fry, R. , Passel, J.S. , & Cohn, D.V. (2020, September 4). A majority of young adults in the U.S. live with their parents for the first time since the Great Depression. Pew Research Center. Available from: https://www.pewresearch.org/fact‐tank/2020/09/04/a‐majority‐of‐young‐adults‐in‐the‐u‐s‐live‐with‐their‐parents‐for‐the‐first‐time‐since‐the‐great‐depression/ [last accessed 2 December 2020]. [Google Scholar]
- Goodman, E. , Adler, N.E. , Kawachi, I. , Frazier, A.L. , Huang, B. , & Colditz, G.A. (2001). Adolescents' perceptions of social status: Development and evaluation of a new indicator. Pediatrics, 108, e31. [DOI] [PubMed] [Google Scholar]
- Hawke, L.D. , Barbic, S.P. , Voineskos, A. , Szatmari, P. , Cleverley, K. , Hayes, E. , … & Henderson, J.L. (2020). Impacts of COVID‐19 on youth mental health, substance use, and well‐being: A rapid survey of clinical and community samples: repercussions de la COVID‐19 sur la sante mentale, l'utilisation de substances et le bien‐etre des adolescents: un sondage rapide d'echantillons cliniques et communautaires. Canadian Journal of Psychiatry, 65, 701–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Resources & Services Administration, Office of Rural Health Policy (2018, December 31). List of rural counties and designated eligible census tracts in metropolitan counties. Available from: https://www.hrsa.gov/sites/default/files/hrsa/ruralhealth/resources/forhpeligibleareas.pdf [last accessed 19 February 2021].
- Kessler, R.C. , Amminger, G.P. , Aguilar‐Gaxiola, S. , Alonso, J. , Lee, S. , & Ustün, T.B. (2007). Age of onset of mental disorders: A review of recent literature. Current Opinion in Psychiatry, 20, 359–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klemperer, E.M. , West, J.C. , Peasley‐Miklus, C. , & Villanti, A.C. (2020). Change in tobacco and electronic cigarette use and motivation to quit in response to COVID‐19. Nicotine & Tobacco Research, 22, 1662–1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke, K. , Spitzer, R.L. , & Williams, J.B. (2003). The Patient Health Questionnaire‐2: Validity of a two‐item depression screener. Medical Care, 41, 1284–1292. [DOI] [PubMed] [Google Scholar]
- Kroenke, K. , Spitzer, R.L. , Williams, J.B. , Monahan, P.O. , & Lowe, B. (2007). Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Annals of Internal Medicine, 146, 317–325. [DOI] [PubMed] [Google Scholar]
- Mansueto, G. , Lopes, F.L. , Grassi, L. , & Cosci, F. (2021). Impact of COVID‐19 outbreak on Italian healthcare workers versus general population: Results from an online survey. Clinical Psychology & Psychotherapy, 28, 1334–1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinty, E.E. , Presskreischer, R. , Anderson, K.E. , Han, H. , & Barry, C.L. (2020). Psychological distress and COVID‐19‐related stressors reported in a longitudinal cohort of US adults in April and July 2020. JAMA, 324, 2555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikolaidis, A. , DeRosa, J. , Kass, M. , Droney, I. , Alexander, L. , DiMartino, A. , … Paksarian, D. (2021). Heterogeneity in COVID‐19 pandemic‐induced lifestyle stressors and predicts future mental health in adults and children in the US and UK. medRxiv. 10.1101/2021.08.10.21261860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niles, J.K. , Gudin, J. , Radcliff, J. , & Kaufman, H.W. (2020). The opioid epidemic within the COVID‐19 pandemic: Drug testing in 2020. Population Health Management, 24, S‐43–S‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orben, A. , Tomova, L. , & Blakemore, S.J. (2020). The effects of social deprivation on adolescent development and mental health. The Lancet Child & Adolescent Health, 4, 634–640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens, M.R. , Brito‐Silva, F. , Kirkland, T. , Moore, C.E. , Davis, K.E. , Patterson, M.A. , … & Tucker, W.J. (2020). Prevalence and social determinants of food insecurity among college students during the COVID‐19 pandemic. Nutrients, 12, 2515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker, M.A. , Sigmon, S.C. , & Villanti, A.C. (2019). Higher smoking prevalence among United States adults with co‐occurring affective and drug use diagnoses. Addictive Behaviors, 99, 106112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker, M.A. , & Villanti, A.C. (2021). Relationship between comorbid drug use disorders, affective disorders, and current smoking. Substance Use and Misuse, 56, 93–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perl, L. , Oren, A. , Klein, Z. , & Shechner, T. (2021). Effects of the COVID19 pandemic on transgender and gender non‐conforming adolescents' mental health. Psychiatry Research, 302, 114042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter, L. (2020). The effects of the COVID‐19 pandemic on the risk of youth substance use. Journal of Adolescent Health, 67, 467–468. [DOI] [PubMed] [Google Scholar]
- Silveira, M.L. , Green, V.R. , Iannaccone, R. , Kimmel, H.L. , & Conway, K.P. (2019). Patterns and correlates of polysubstance use among US youth aged 15–17 years: wave 1 of the Population Assessment of Tobacco and Health (PATH) Study. Addiction, 114, 907–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- State of Vermont, Agency of Education . (2020). Reopening status of Vermont Public Schools. Available from: https://education.vermont.gov/news/covid‐19‐guidance‐vermont‐schools/reopening‐status‐of‐vermont‐public‐schools [last accessed 12 January 2021].
- The CoRonavIruS Health Impact Survey (CRISIS) . (2020). V0.3: Adult self‐report baseline current form. Available from: https://www.nlm.nih.gov/dr2/CRISIS_Adult_Self‐Report_Baseline_Current_Form_V0.3.pdf [last accessed 4 December 2020].
- Vermont Department of Health . (2020a, March). 2019 Vermont youth risk behavior survey: Statewide results. Available from: https://www.healthvermont.gov/sites/default/files/documents/pdf/CHS_YRBS_statewide_report.pdf [last accessed 15 October 2020].
- Vermont Department of Health . (2020b, October 22). Population of Vermont counties by single year of age and sex, 2019. Available from: https://www.healthvermont.gov/sites/default/files/documents/xls/HS‐STAT‐Population‐of‐Vermont‐Counties‐by‐single‐year‐of‐age‐and‐sex‐2019.xls [last accessed 19 February 2021].
- Villanti, A.C. , Vallencourt, C.P. , West, J.C. , Peasley‐Miklus, C. , LePine, S.E. , McCluskey, C. , … & Williams, R. (2020). Recruiting and retaining youth and young adults in the Policy and Communication Evaluation (PACE) Vermont study: Randomized controlled trial of participant compensation. Journal of Medical Internet Research, 22, e18446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow, N.D. (2020). Collision of the COVID‐19 and addiction epidemics. Annals of Internal Medicine, 173, 61–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waselewski, E.A. , Waselewski, M.E. , & Chang, T. (2020). Needs and coping behaviors of youth in the U.S. during COVID‐19. Journal of Adolescent Health, 67, 649–652. [DOI] [PubMed] [Google Scholar]
- Weinstein, S.M. , & Mermelstein, R.J. (2013). Influences of mood variability, negative moods, and depression on adolescent cigarette smoking. Psychology of Addictive Behaviors, 27, 1068–1078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams, V.F. , Smith, A.A. , Villanti, A.C. , Rath, J.M. , Hair, E.C. , Cantrell, J. , … & Vallone, D.M. (2017). Validity of a subjective financial situation measure to assess socioeconomic status in US young adults. Journal of Public Health Management and Practice, 23, 487–495. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Characteristics of adolescent and young adult participants, PACE Vermont Study, September 2020 (n = 874)
Table S2. Demographic correlates of COVID Impact Score, PACE Vermont Study, September 2020
Table S3. Linear regression models of COVID Impact score on individual COVID‐related stressors


