Abstract
Background
Efforts aimed at preventing premature mortality for people with Down syndrome are hindered by the practice of reporting disability as the underlying cause of death. Prior research suggests this form of diagnostic overshadowing may be the result of increased uncertainty surrounding the death.
Methods
This study uses bivariable analysis and multivariable logistic regression models to investigate associations between sociodemographic characteristics, comorbidities, and death context and processing characteristics with the reporting of Down syndrome as the underlying cause of death in 2005–2017 US Multiple Cause of Death data files.
Results
The reporting of Down syndrome as the underlying cause of death was associated with characteristics indicative of an increased amount of uncertainty surrounding the death. Results also suggest other mechanisms may inform inaccurate reporting, such as racial bias, and the continued conflation of disability and health.
Conclusion
Medical personnel certifying death certificates should strive for accuracy when reporting the causes of death. To ensure this outcome, even in the midst of increased uncertainty, Down syndrome should not be reported as the underlying cause of death unless the decedent was diagnosed with Alzheimer’s disease or unspecified dementia. Future research should further explore the possibility that increased death certification errors for adults with Down syndrome, or other developmental disabilities, is associated with racial bias.
Keywords: Down syndrome, death certificates, diagnostic overshadowing, clinical uncertainty, false equivalence, racial bias
Background
People with intellectual and developmental disabilities (IDD) are underrepresented in public health and medical research and often are subjected to disparities in access to and quality of health care (Krahn & Fox, 2014; Krahn, Walker, & Correa-De-Araujo, 2015; Spong & Bianchi, 2018). On average, people with IDD have poorer health and an earlier age at death than the general population (Havercamp, Scandlin, & Roth, 2004; Havercamp & Scott, 2015; Landes, McDonald, Wilmoth, & Carter Grosso, 2021; Landes, Stevens, & Turk, 2019a). One practice that research pinpoints as contributing to these disparities is diagnostic overshadowing – the stereotypical attribution of mental or physical health issues to disability – which results in the underdiagnosis and undertreatment of actual diseases or illnesses distinct from the disability (Ali et al., 2013; Jopp & Keys, 2001; Peña-Guzmán & Reynolds, 2019). The act of diagnostic overshadowing reduces the quality of medical care people with IDD receive throughout the life course (Ali et al., 2013; Hollins, Attard, von Fraunhofer, McGuigan, & Sedgwick, 1998; Ouellette-Kuntz, 2005).
There is evidence that diagnostic overshadowing occurs postmortem for people with IDD. The US began using a standardized death certification form in the early 1900s that uses the International Classification of Diseases (ICD) to report information on causes of death and comorbidities present at the time of death (National Research Council Committee on National Statistics, 2009; Percy & Dolman, 1978). Early versions of the ICD included vague, and often offensive codes for intellectual and developmental disabilities, with these codes gaining specificity and generally becoming less objectionable over the years. For instance in relation to this study, the ICD did not include a code for Down syndrome prior to 1948, introduced a code for “Mongolism” in 1948, then changed the terminology for this code to “Down’s syndrome” in 1965, and “Down syndrome” in 2021 (Wolfbane Cybernetic Ltd., 2021). Thus, the reporting of Down syndrome on the death certificate was not possible using the ICD system until 1948.
In 1990, researchers in Canada expressed concern that intellectual disability and Down syndrome were being reported as the underlying cause of death (UCOD) (Baird & Sadovnick, 1990), which is the disease or injury identified on the death certificate as having started the chain of events leading to death (National Center for Health Statistics, 2017). In their 1990 study, Baird and Sadovnick asserted that reporting intellectual disability and Down syndrome as the UCOD was an inaccurate practice as these disabilities are not illnesses or diseases that ‘cause’ death (Baird & Sadovnick, 1990, pp. 458, 460). Subsequent to the Baird and Sadovnick study, researchers in the US, UK, Australia, and France documented similar practices in death certification for people with intellectual and developmental disability, expressing shared concerns about the inaccuracy of this practice (Duruflé-Tapin et al., 2014; Landes & Peek, 2013; Trollor, Srasuebkul, Xu, & Howlett, 2017; Tyrer & McGrother, 2009). In effect, the practice of reporting an intellectual or developmental disability as the UCOD is an instance of diagnostic overshadowing as it ‘obscured’ the actual disease or injury that started the process leading to death among this population (Landes, Stevens, & Turk, 2019b; Trollor et al., 2017).
The latest study from the US documents that between 2012 and 2016, 25.9% of death certificates for adults with IDD reflected diagnostic overshadowing by reporting IDD as the underlying cause of death (UCOD) (Landes et al., 2019b). For people with one particular type of developmental disability, Down syndrome, 59% of death certificates reported their disability as the UCOD (Landes et al., 2019b). As it falsely equates disability with disease, this practice is inaccurate (Landes, Turk, & Lauer, 2020). Down syndrome is a genetic disorder characterised by higher prevalence and/or earlier onset of particular health conditions such as congenital heart defects, respiratory diseases, and Alzheimer’s disease (Landes, Stevens, & Turk, 2020; O’Leary, Hughes-McCormack, Dunn, & Cooper, 2018; Prasher & Janicki, 2019; Rubin & Crocker, 2006; Stephanie L. Santoro et al., 2021). Yet, while associated with increased risk of developing particular comorbidities, it is imperative to understand that Down syndrome is a disability, not a disease or injury that causes death (Baird & Sadovnick, 1990; Landes et al., 2019b; Landes, Turk, et al., 2020; Trollor et al., 2017), and should not be reported as the UCOD.
The only caveat to not reporting Down syndrome as the UCOD regards Alzheimer’s disease or unspecified dementia with the presence of Down syndrome. There is mounting evidence of a causal pathway between Down syndrome and the development of neuropathology typical of Alzheimer’s disease (Snyder et al., 2020; Wiseman et al., 2015). In response to this evidence, beginning in 2014 the Centers for Disease Control and Prevention (CDC) guidance on reporting the UCOD specified that “Unspecified dementia (F03) and Alzheimer’s disease (G30) should be considered an obvious consequence of Down’s syndrome (Q90)” (CDC, 2014, p. 23). It is important to note that the CDC’s instruction to report Down syndrome as the UCOD is only in instances when the decedent was diagnosed with Alzheimer’s disease or unspecified dementia, not for any other disease or injury.
The inaccurate reporting of Down syndrome as the UCOD is a missed opportunity for prevention efforts aimed at reducing premature mortality among this population (Landes, Turk, et al., 2020). Adults with Down syndrome in the US die at ages 19–25 years earlier than adults without this disability (Landes et al., 2019a), frequently from preventable causes of death (Landes, Stevens, et al., 2020). Inaccurately reporting Down syndrome as the UCOD obscures higher rates of preventable causes of death such as pneumonitis, choking, influenza and pneumonia (Landes et al., 2019b). Because public health efforts focused on understanding population health trends and reducing premature death rely upon death certificate data in general, and underlying cause of death trends in particular to understand mortality trends (Jha, 2012), it is crucial to eliminate the inaccurate practice of reporting Down syndrome as the UCOD.
Research demonstrates that the amount of uncertainty surrounding the death impacts the accuracy of death certification (Landes & Peek, 2013; Landes, Turk, & Bisesti, 2021; Wall, Huang, Oswald, & McCullen, 2005). Typically, the amount of uncertainty surrounding a death is associated with the amount and availability of information about the decedent’s medical history present at the time of death. There are two distinct factors identified as being associated with limited available medical history that may result in increased uncertainty when completing death certification: 1) fewer reported or non-specific comorbidities on the death certificate, often a sign of less information regarding the decedent’s medical history (Landes & Peek, 2013; Landes, Turk, et al., 2021; Lenfant & Thom, 1998; Wall et al., 2005); and 2) the place of death being in a non-medical as opposed to medical location which can determine access to medical history (Bercovitz & Pearson, 2006; McGivern, Shulman, Carney, Shapiro, & Bundock, 2017). Research also indicates that sociodemographic characteristics are associated with less frequent or lower quality of lifetime physician-patient interaction, which may result in a less thorough medical history available at the time of death (Ong, de Haes, Hoos, & Lammes, 1995). These include younger age (Wall et al., 2005), Hispanic ethnicity (De Alba & Sweningson, 2006; Mayo, Sherrill, Sundareswaran, & Crew, 2007; Seijo, Gomez, & Freidenberg, 1991), and lower levels of education (Verlinde, De Laender, De Maesschalck, Deveugele, & Willems, 2012; Willems, De Maesschalck, Deveugele, Derese, & De Maeseneer, 2005).
This study identified the sociodemographic characteristics, comorbidities, and death context and processing characteristics associated with the inaccurate reporting of Down syndrome as the UCOD. Based on findings from similar studies on adults with intellectual disability (Landes & Peek, 2013; Landes, Turk, et al., 2021), we hypothesised that the inaccurate reporting of Down syndrome as the UCOD will be more likely to occur in situations associated with a higher degree of uncertainty surrounding the death.
Methods
Data
This study used restricted National Vital Statistics System 2005–2017 US Multiple Cause of Death files inclusive of geographic identifiers. Multiple years were used to ensure adequate cell counts per variable. As analysis focused on predictors of Down syndrome as the UCOD among adults, it only included the death certificates of adults, ages 18 and over, who had an ICD-10 code for Down syndrome (Q90) reported as the underlying or a multiple cause of death, and who died in their state of residence between January 1, 2005 and December 31, 2017 (N=23,514).
Measures
We conceptualised accurate reporting as death certificates that reported Down syndrome as a multiple cause of death on the death certificate, but did not report this disability as the UCOD (hereafter Down syndrome not reported as UCOD). We identified two types of inaccurate reporting: 1) exclusive reporting of Down syndrome; and 2) the reporting of Down syndrome as the UCOD, but with additional comorbidities reported. The exclusive reporting of Down syndrome is a rare but severe example of diagnostic overshadowing in which decedents have Down syndrome reported on their death certificate as the UCOD, with no other comorbidities reported. The second type of inaccurate reporting, Down syndrome as the UCOD with additional comorbidities listed on the death certificate (hereafter Down syndrome as the UCOD), is more common. Based upon this typology of inaccurate reporting, the outcome measure included the categories of exclusive reporting of Down syndrome, Down syndrome as UCOD, and Down syndrome not reported as UCOD.
Factors associated with increased uncertainty surrounding the cause of death fit within three broad categories: sociodemographic characteristics, comorbidities, and death context and processing characteristics
Sociodemographic characteristics:
Three measures indicated sociodemographic characteristics: age (18–29; 30–39; 40–49; 50–59; 60–69; 70–103); race-ethnicity [Non-Hispanic White (here White); Non-Hispanic Black (here Black); Hispanic; Non-Hispanic Other (here Other)]; and level of education (0–8 years; 9 or more years; missing). As one study identifies more death certificate errors for females than males (Lloyd-Jones, Martin, Larson, & Levy, 1998), we also control for biological sex (female; male).
Comorbidities:
Fourteen measures indicated comorbidities reported on the death certificate. The first is the number of multiple causes of death reported on the death certificate, quartiled into the categories of 1, 2, 3, and 4–13. The other 13 are binary measures (yes; no) that document whether specific ICD-10 codes were reported on the death certificate. Ten of the ICD-10 measures accounted for the top causes of death for adults with Down syndrome, inclusive of one external cause (choking) of death and ten internal causes of death (see Table 1 for full listing and corresponding ICD-10 codes). One ICD-10 measure indicated whether non-specific conditions, indicated with an R-code – ‘symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified’ – were reported on the death certificate. Two remaining measures indicated comorbid developmental disabilities of intellectual disability or cerebral palsy.
Table1 :
Distribution of study variables across reporting categories among decedents who had Down syndrome reported on the death certificate, 2005–2017 US Multiple Cause of Death files, N=23,514
| Inaccurate reporting | Accurate reporting | |||
|---|---|---|---|---|
| Variable | Categories | Exclusive reporting of Down syndrome (n=767) % (N) |
Down syndrome as UCOD (n=11,452) % (N) |
Down syndrome not UCOD (n=11,295) % (N) |
| Sociodemographic characteristics | ||||
| Age | 18–29 | 3.78 (29) | 3.56 (408) | 4.33 (489) |
| 30–39 | 4.69 (36) | 4.23 (484) | 6.26 (707) | |
| 40–49 | 16.04 (123) | 13.19 (1,511) | 15.05 (1,700) | |
| 50–59 | 45.37 (348) | 44.76 (5,126) | 40.69 (4,596) | |
| 60–69 | 27.25 (209) | 30.79 (3,526) | 26.33 (2,974) | |
| 70–103 | 2.87 (22) | 3.47 (397) | 7.34 (829) | |
| Sex | Female | 53.32 (409) | 48.50 (5,554) | 48.35 (5,461) |
| Male | 46.68 (358) | 51.50 (5,898) | 51.65 (5,834) | |
| Race-ethnicity | White | 82.92 (636) | 83.87 (9,605) | 84.04 (9,492) |
| Black | 9.52 (73) | 8.10 (928) | 7.80 (881) | |
| Hispanic | 5.87 (45) | 6.37 (729) | 6.52 (736) | |
| Other | 1.69 (13) | 1.66 (190) | 1.65 (186) | |
| Education | 0–8 years | 56.71 (435) | 55.06 (6,306) | 53.01 (5,988) |
| 9+ years | 29.60 (227) | 32.43 (3,714) | 34.48 (3,894) | |
| Missing | 13.69 (105) | 12.50 (1,432) | 12.51 (1,413) | |
| Comorbidities | ||||
| Number of comorbidities | 1 | 27.65 (3,167) | 14.56 (1,645) | |
| 2 | 31.28 (3,582) | 24.90 (2,813) | ||
| 3 | 21.30 (2,439) | 23.75 (2,682) | ||
| 4–13 | 19.77 (2,264) | 36.79 (4,155) | ||
| Alzheimer’s disease/Unspecified dementia (ICD-10 G30, F03) | 28.09 (3,217) | 29.38 (3,318) | ||
| Heart disease (ICD-10 I00-I09, I11, I13, I20-I51) | 26.55 (3,040) | 37.77 (4,266) | ||
| Influenza/Pneumonia (ICD-10 J09-J18) | 30.49 (3,492) | 14.19 (1,603) | ||
| Pneumonitis (ICD-10 J69) | 15.29 (1,751) | 19.45 (2,197) | ||
| Cerebrovascular diseases (ICD-10 I60-I69) | 2.40 (275) | 7.16 (809) | ||
| Respiratory failure (ICD-10 J69.0, J69.1, J69.8) | 16.72 (1,915) | 15.05 (1,700) | ||
| Genitourinary diseases (ICD-10 N00-N07, N17-N19, N25-N27, N39) | 6.13 (702) | 9.41 (1,063) | ||
| Choking (ICD-10 W78-W80) | 4.03 (462) | 4.78 (766) | ||
| Malignant neoplasms (ICD-10 C00-C97) | 0.35 (40) | 5.34 (603) | ||
| Congenital heart (ICD-10 Q20-Q28) | 2.97 (340) | 3.28 (371) | ||
| Non-specific conditions (ICD-10 R00-R99) | 34.72 (3,976) | 27.94 (3,156) | ||
| Cerebral palsy (ICD-10 G80) | 0.35 (40) | 0.80 (90) | ||
| Intellectual disability (ICD-10 F70–79) | 520 (4.54) | 573 (5.07) | ||
| Death context and processing | ||||
| Place of death | Hospital inpatient | 7.04 (54) | 31.32 (3,587) | 35.94 (4,059) |
| Outpatient/ER/DOA | 8.34 (64) | 4.89 (560) | 6.44 (727) | |
| Home | 42.37 (325) | 23.31 (2,670) | 22.71 (2,565) | |
| Nursing home | 31.68 (243) | 29.65 (3,395) | 25.52 (2,883) | |
| Other/Unknown | 10.56 (81) | 10.83 (1,240) | 9.39 (1,061) | |
| Autopsy | Yes | 4.95 (38) | 2.48 (284) | 4.27 (482) |
| No | 84.62 (649) | 90.10 (10,318) | 88.54 (10,001) | |
| Unknown | 10.43 (80) | 7.42 (850) | 7.19 (812) | |
| Year of death – Median (IQR) | 2005 | 5.62 (50) | 6.62 (758) | 7.70 (870) |
| 2006 | 7.95 (61) | 5.65 (647) | 7.96 (899) | |
| 2007 | 8.08 (62) | 5.86 (671) | 8.34 (942) | |
| 2008 | 7.04 (54) | 6.57 (752) | 8.40 (949) | |
| 2009 | 7.04 (54) | 6.13 (702) | 10.14 (1,145) | |
| 2010 | 6.39 (49) | 5.71 (654) | 8.10 (915) | |
| 2011 | 6.26 (48) | 7.05 (807) | 7.84 (886) | |
| 2012 | 7.43 (57) | 7.29 (835) | 8.03 (907) | |
| 2013 | 7.95 (61) | 7.96 (912) | 8.00 (904) | |
| 2014 | 7.17 (55) | 9.31 (1,066) | 6.33 (715) | |
| 2015 | 8.47 (65) | 10.43 (1,195) | 5.75 (650) | |
| 2016 | 9.39 (79) | 10.70 (1,225) | 6.42 (725) | |
| 2017 | 10.30 (79) | 10.72 (1,228) | 6.98 (788) | |
Based on chi-square analysis, all associations were statistically significant for difference at the p<.05 level excluding race-ethnicity, congenital heart, and intellectual disability. UCOD = Underlying cause of death.
Death context and processing:
Three measures accounted for aspects of the context and processing of the death: 1) location of death (home, hospital inpatient hospital outpatient/ER/DOD, nursing home, unknown/other); 2) autopsy status (yes, no, unknown); and 3)year of death (coded in single years).
Analytic strategy
Initial analysis compared the distributions of sociodemographic characteristics and death processing for each category of the outcome measure (N=23,514). We then created two separate binary outcome measures for multivariable analysis, each with the same null category. The first binary variable compared exclusive reporting of Down syndrome (coded 1) with Down syndrome not reported as the UCOD (coded 0). The second binary variable compared Down syndrome as the UCOD (coded 1) with Down syndrome not reported as the UCOD (coded 0). We employed this strategy of dividing the outcome measure into two separate binary variables with the same null category, as opposed to a multinomial modeling strategy, in order to fully examine the association between reported comorbidities (which were not present for decedents with the exclusive reporting of Down syndrome) and Down syndrome as the UCOD. We used a logistic regression model to examine associations of sociodemographic characteristics and death context and processing with the first binary outcome measure: exclusive reporting of Down syndrome versus Down syndrome not reported as the UCOD (n=12,062). We then specified a logistic regression model to examine the association of all study variables with the second binary outcome measure: Down syndrome as UCOD versus Down syndrome not reported as the UCOD (n=22,747).
We provided sensitivity analysis to account for the 2014 shift in CDC policy regarding reporting Down syndrome as the UCOD in instances when the decedent had a diagnosis of Alzheimer’s disease or unspecified dementia. Using cases for decedents who did/did not have Down syndrome reported as the UCOD (n=22,747), we first specified a model that included an interaction term for Alzheimer’s disease or unspecified dementia by year of death. We then plotted predicted probabilities of Down syndrome as UCOD across year of death for three groups: all cases, all cases with Alzheimer’s disease or unspecified dementia reported (28.7%; n=6,535), all cases without Alzheimer’s disease or unspecified dementia reported (71.3%; n=16,212). Finally, we specified a logistic regression model to examine the association of all study variables with the reporting of Down syndrome as UCOD only for cases that did not report Alzheimer’s disease or unspecified dementia on the death certificate (n=16,212).
For all models, the most salient predictors of the inaccurate reporting of Down syndrome were identified through estimation of squared semipartial correlations. Analysis was conducted with STATA 17.0 (College Station, TX).
Results
For the time period of the study, 23,514 out of 31,649,684 death certificates had Down syndrome reported on their death certificate. This Down syndrome prevalence rate of 7.4 per 10,000 in the study corresponds with recent estimates of the size of this population in the US to be 6.7 per 10,000 and 8.3 per 10,000 (de Graaf, Buckley, & Skotko, 2017; Presson et al., 2013).
Among all decedents, 52% had Down syndrome reported as the UCOD – 3.3% with the exclusive reporting of Down syndrome, 48.7% with Down syndrome as the UCOD. Comparisons of the distributions of sociodemographic characteristics and death processing for all three possible outcomes are provided in Table 1. The most noticeable differences were a disproportionate percentage of females and home deaths among decedents with exclusive reporting of Down syndrome, and a shift starting in 2014, as the percentage of both inaccurate reporting outcomes eclipsed the percentage of cases that did not have inaccurate reporting. Table 1 also includes the distribution of comorbidities for the decedents with Down syndrome as the UCOD, and those with Down syndrome not reported as the UCOD. The most noticeable differences were that influenza/pneumonia and non-specific conditions were more common, and heart disease and malignant neoplasms were less common among those who had Down syndrome reported as the UCOD.
Results from the logistic regression model examining associations with the exclusive reporting of Down syndrome, as opposed to Down syndrome not reported as the UCOD, are provided in Table 2. The exclusive reporting of Down syndrome was more likely among: females (OR, 1.18; 95% CI, 1.02–1.37) compared to males, Black (OR, 1.34; 95% CI, 1.03–1.74) compared to White decedents, those who died in settings other than hospital inpatient (Outpatient/ER/DOA OR, 6.59; 95% CI, 4.52–9.60; Home OR, 9.96; 95% CI, 7.42–13.36; Nursing home OR, 7.05; 95% CI, 5.21–9.56; Other/unknown setting OR, 5.78; 95% CI, 4.05–8.23), and those with an unknown autopsy status (OR, 1.65; 95% CI, 1.28–2.13). The inaccurate practice of exclusive reporting of Down syndrome was also more likely in 2015 (OR, 1.83; 95% CI, 1.23–2.71), 2016 (OR, 1.94; 95% CI, 1.25–1.70), and 2017 (OR, 1.88; 95% CI, 1.29–2.75) compared to 2005. Exclusive reporting was less likely among decedents age 70–103 (OR, 0.36; 95% CI, 0.20–0.64) compared to those age 18–29, and among decedents with 9 or more years of education (OR, 0.74; 95% CI, 0.61–0.88) compared to those with 1–8 years of education. Based on analysis of squared semipartial correlations, the strongest predictors or exclusive reporting, each explaining more than 1% of the variance in the outcome, were home and nursing home deaths.
Table 2 :
Logistic regression analysis of the exclusive reporting of Down syndrome, 2005–2017 US Multiple Cause of Death files, n=12,062
| Variable | OR | 95% CI |
|---|---|---|
| Sociodemographic characteristics | ||
| Age (ref: 18–29) | ||
| 30–39 | 0.92 | (0.55, 1.54) |
| 40–49 | 1.12 | (0.72, 1.74) |
| 50–59 | 1.02 | (0.67, 1.56) |
| 60–69 | 0.90 | (0.58, 1.40) |
| 70–103 | 0.36** | (0.20, 0.64) |
| Female | 1.18* | (1.02, 1.37) |
| Race-ethnicity (ref: White) | ||
| Black | 1.34* | (1.03, 1.74) |
| Hispanic | 0.91 | (0.66, 1.26) |
| Other | 1.23 | (0.68, 2.21) |
| Education (ref: 0–8 years) | ||
| 9+ years | 0.74** | (0.61, 0.88) |
| Missing | 0.99 | (0.79, 1.24) |
| Death context and processing | ||
| Place of death (ref: hospital inpatient) | ||
| Outpatient/ER/DOA | 6.59*** | (4.52, 9.60) |
| Home | 9.96*** | (7.42, 13.36) |
| Nursing home | 7.05*** | (5.21, 9.56) |
| Other/Unknown | 5.78*** | (4.05, 8.23) |
| Autopsy (ref: no) | ||
| Yes | 1.12 | (0.78, 1.61) |
| Unknown | 1.65*** | (1.28, 2.13) |
| Year of death (ref: 2005) | ||
| 2006 | 1.20 | (0.81, 1.78) |
| 2007 | 1.11 | (0.75, 1.63) |
| 2008 | 0.98 | (0.66. 1.47) |
| 2009 | 0.86 | (0.58, 1.29) |
| 2010 | 0.91 | (0.60, 1.37) |
| 2011 | 0.87 | (0.57, 1.31) |
| 2012 | 1.01 | (0.68, 1.51) |
| 2013 | 1.16 | (0.78, 1.72) |
| 2014 | 1.48 | (0.99, 2.22) |
| 2015 | 1.83** | (1.23, 2.71) |
| 2016 | 1.94** | (1.25, 1.70) |
| 2017 | 1.88** | (1.29, 2.75) |
| Intercept | 0.01*** | (0.01, 0.02) |
Note:
p < .05,
p < .01,
p < .001.
Bold text = predictor accounted for > 1% of variance in outcome, sr2>.01.
Results from initial logistic regression models examining associations with the reporting of Down syndrome as UCOD, as opposed to Down syndrome not reported as the UCOD, are reported in Table 3. Model 1 includes all study variables, Model 2 adds the Alzheimer’s disease/unspecified dementia by year interaction term. As there were no substantial changes in the ORs from Model 1 to Model 2 – slight changes in the ORs for 30–39 and Hispanic resulted in these factors becoming statistically significant – we focus our summary on the interaction term in Model 2. To improve ease of interpretation, we used Model 2 from Table 3 to plot the predicted probabilities of Down syndrome as the UCOD across all years of the studies for: 1) the overall sample; 2) decedents with Alzheimer’s disease or unspecified dementia; and 3) decedents without Alzheimer’s disease or unspecified dementia. As is apparent, the statistically significant differences in the reporting of Down syndrome as UCOD across the years of the study were largely explained by patterns related to Alzheimer’s disease/unspecified dementia. For decedents without this diagnosis (Panel 3, Figure 1), there was only a slight increase in the reporting of Down syndrome as UCOD in 2013, 2015, and 2016. For decedent’s with Alzheimer’s disease or unspecified dementia (Panel 2, Figure 1), patterns of reporting Down syndrome as UCOD were lowest in 2006–2010, moderately higher in 2005 as well as 2011–2013, then substantially higher starting in 2014, the year the CDC specified that Down syndrome should be reported as the UCOD when the decedent had Alzheimer’s disease or unspecified dementia.
Table 3:
Logistic regression analysis of Down syndrome as underlying cause of death, 2005–2017 US Multiple Cause of Death files, n=22,747
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Sociodemographic Characteristics | ||||
| Age (ref: 18–29) | ||||
| 30–39 | 0.84 | (0.69, 1.02) | 0.81* | (0.66, 0.99) |
| 40–49 | 0.96 | (0.81, 1.14) | 0.96 | (0.80, 1.14) |
| 50–59 | 0.99 | (0.84, 1.17) | 0.99 | (0.83, 1.17) |
| 60–69 | 1.01 | (0.85, 1.20) | 0.99 | (0.83, 1.18) |
| 70–103 | 0.51*** | (0.42, 0.64) | 0.54*** | (0.44, 0.68) |
| Female | 0.99 | (0.93, 1.05) | 0.99 | (0.93, 1.05) |
| Race-ethnicity (ref: White) | ||||
| Black | 1.23*** | (1.10, 1.37) | 1.24*** | (1.11, 1.39) |
| Hispanic | 1.10 | (0.98, 1.25) | 1.15* | (1.02, 1.30) |
| Other | 1.22 | (0.96, 1.53) | 1.20 | (0.95, 1.53) |
| Education (ref: 0–8 years) | ||||
| 9+ years | 0.98 | (0.92, 1.05) | 0.97 | (0.90, 1.04) |
| Missing | 0.96 | (0.88, 1.05) | 0.98 | (0.89, 1.08) |
| Comorbidities | ||||
| Number of comorbidities (ref: 1) | ||||
| 2 | 0.49*** | (0.45, 0.54) | 0.48*** | (0.44, 0.53) |
| 3 | 0.29*** | (0.26, 0.32) | 0.28*** | (0.25, 0.31) |
| 4–13 | 0.13*** | (0.12, 0.15) | 0.12*** | (0.10, 0.13) |
| Alzheimer’s disease/Unspecified dementia | 0.86*** | (0.80, 0.93) | 0.67** | (0.52, 0.86) |
| Heart disease | 0.93* | (0.86, 1.00) | 0.91* | (0.84, 0.98) |
| Influenza/pneumonia | 3.83*** | (3.53, 4.17) | 4.10*** | (3.76, 4.47) |
| Pneumonitis | 0.98 | (0.90, 1.06) | 0.94 | (0.86, 1.03) |
| Cerebrovascular diseases | 0.38*** | (0.33, 0.45) | 0.37*** | (0.32, 0.43) |
| Respiratory disease | 1.50*** | (1.37, 1.63) | 1.57*** | (1.44, 1.72) |
| Genitourinary diseases | 0.99 | (0.88, 1.11) | 0.99 | (0.88, 1.11) |
| Choking | 1.04 | (0.90, 1.18) | 1.05 | (0.92, 1.21) |
| Congenital heart defect | 1.55*** | (1.31, 1.83) | 1.51*** | (1.27, 1.79) |
| Malignant neoplasms | 0.06*** | (0.05, 0.09) | 0.06*** | (0.04, 0.09) |
| Non-specific conditions (R-code) | 2.40*** | (2.23, 2.58) | 2.50*** | (2.32, 2.70) |
| Cerebral palsy | 0.54** | (0.36, 0.81) | 0.53** | (0.35, 0.79) |
| Intellectual disability | 1.52*** | (1.33, 1.75) | 1.51*** | (1.31, 1.74) |
| Death context and processing | ||||
| Place of death (ref: Hospital inpatient) | ||||
| Hospital outpatient/ER/DOA | 1.09 | (0.95, 1.25) | 1.09 | (0.94, 1.25) |
| Home | 1.23*** | (1.13, 1.34) | 1.26*** | (1.15, 1.38) |
| Nursing home | 1.32*** | (1.22, 1.43) | 1.37*** | (1.26, 1.49) |
| Other/Unknown | 1.21** | (1.09, 1.35) | 1.21*** | (1.08, 1.36) |
| Autopsy (ref: No) | ||||
| Yes | 0.65*** | (0.55, 0.78) | 0.61*** | (0.51, 0.73) |
| Unknown | 1.11 | (0.99, 1.24) | 1.11 | (0.99, 1.25) |
| Year of death (ref: 2005) | ||||
| 2006 | 0.82* | (0.71, 0.97) | 1.03 | (0.86, 1.23) |
| 2007 | 0.80** | (0.68, 0.93) | 1.08 | (0.91, 1.30) |
| 2008 | 0.87 | (0.75, 1.01) | 1.14 | (0.96, 1.36) |
| 2009 | 0.71*** | (0.61, 0.82) | 1.01 | (0.85, 1.20) |
| 2010 | 0.75*** | (0.65, 0.88) | 1.07 | (0.89, 1.29) |
| 2011 | 1.03 | (0.89, 1.20) | 1.08 | (0.90, 1.29) |
| 2012 | 1.08 | (0.93, 1.25) | 1.08 | (0.90, 1.29) |
| 2013 | 1.13 | (0.97, 1.31) | 1.21* | (1.01, 1.44) |
| 2014 | 1.96*** | (1.68, 2.28) | 1.18 | (0.99, 1.41) |
| 2015 | 2.36*** | (2.03, 2.74) | 1.30** | (1.09, 1.56) |
| 2016 | 2.27*** | (1.95, 2.63) | 1.29** | (1.08, 1.55) |
| 2017 | 2.22*** | (1.91, 2.58) | 1.16 | (0.97, 1.38) |
| Alzheimer’s disease/Unspecified
dementia X Year of death |
0.36*** | (0.24, 0.53) | ||
| 2006 | 0.26*** | (0.18. 0.39) | ||
| 2007 | 0.30*** | (0.21, 0.44) | ||
| 2008 | 0.21*** | (0.14, 0.31) | ||
| 2009 | 0.25*** | (0.17, 0.37) | ||
| 2010 | 0.90 | (0.64, 1.27) | ||
| 2011 | 1.07 | (0.76, 1.50) | ||
| 2012 | 0.85 | (0.60, 1.18) | ||
| 2013 | 6.08*** | (4.26, 8.68) | ||
| 2014 | 8.91*** | (6.15, 12.91) | ||
| 2015 | 6.56*** | (4.63, 9.30) | ||
| 2016 | 10.91*** | (7.59, 15.67) | ||
| 2017 | 1.40*** | (1.12, 1.75) | ||
| Intercept | 1.30* | (1.05, 1.61) | 1.40*** | (1.12, 1.75) |
Note:
p < .05,
p < .01,
p < .001.
Bold text = predictor accounted for > 1% of variance in outcome, sr2>.01.
Figure 1:
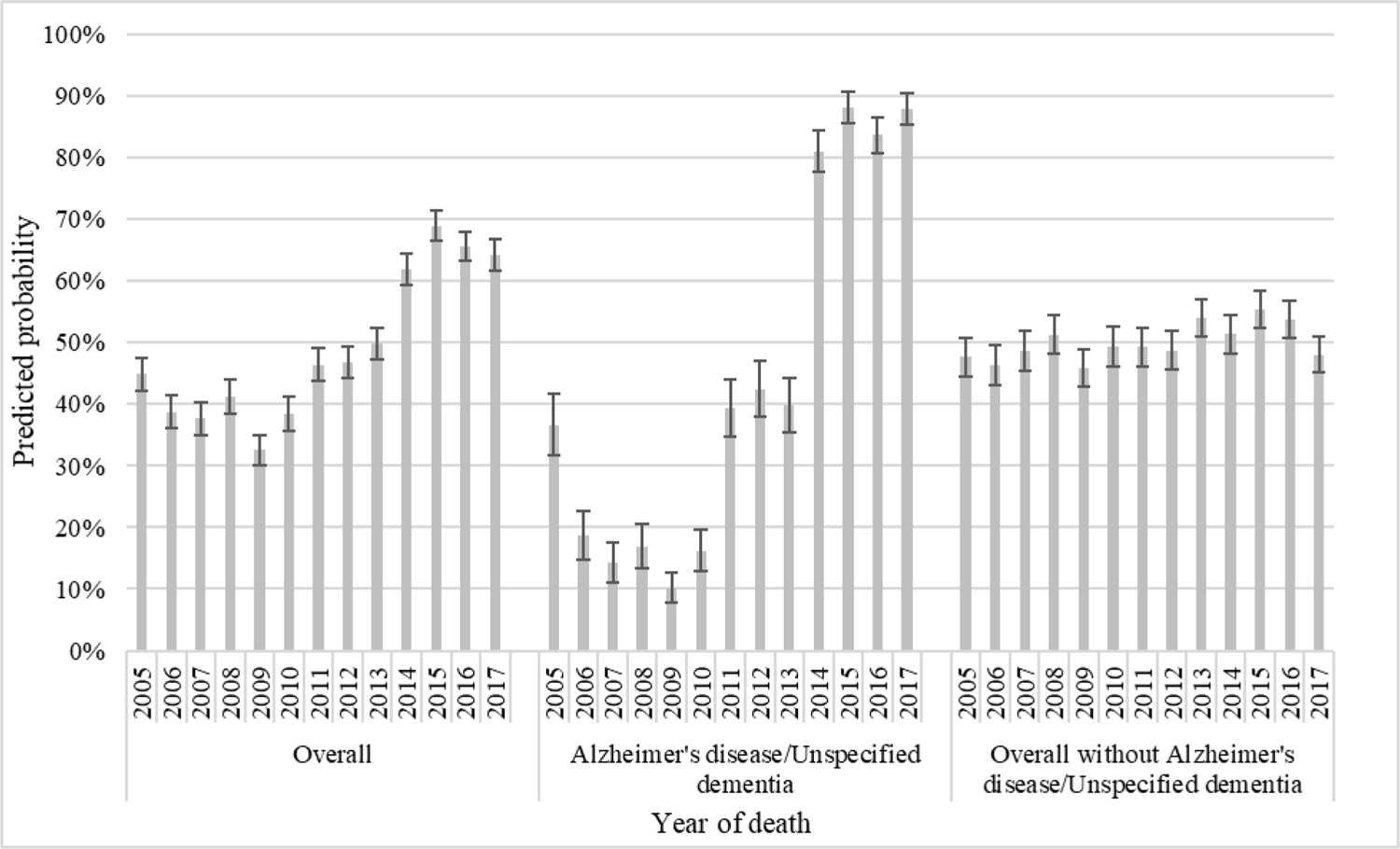
Predicted probabilities of Down syndrome as UCOD overall, and by Alzheimer’s disease/Unspecified dementia status.
Because the CDC stipulated that Down syndrome should be reported as the UCOD for decedents with Alzheimer’s disease or unspecified dementia, and the dissimilar patterns of reporting across years for decedents with/without Alzheimer’s disease or unspecified dementia, we specified a final model that examined factors predicting the inaccurate reporting of Down syndrome as the UCOD after excluding all cases of decedents with Alzheimer’s disease of unspecified dementia (Table 4). Inaccurate reporting of Down syndrome was more likely: for Black (OR, 1.25; 95% CI, 1.08–1.36) and Hispanic (OR, 1.16; 95% CI, 1.01–1.33) compared to White decedents; when decedents had a comorbidity of influenza/pneumonia (OR, 4.48; 95% CI, 4.46–4.94), respiratory disease (OR, 1.73; 95% CI 1.57–1.91), congenital heart defect (OR, 1.55; 95% CI, 1.31–1.85), or a non-specific condition (R-code) (OR, 2.76; 95% CI 2.53–3.01); and when death occurred at home (OR, 1.27; 95% CI, 1.15–1.41), in a nursing home (OR, 1.42; 95% CI 1.29–1.57), or in an other/unknown location (OR, 1.15; 95% CI 1.01–1.32) compared to the hospital inpatient setting. Inaccurate reporting was also more likely when the decedent with Down syndrome also had intellectual disability (OR, 1.64; 95% CI, 1.40–1.92) reported on the death certificate. Similar to results from Model 2 in Table 3, there was a slight increase in reporting of Down syndrome as UCOD in 2013 (OR, 1.22; 95% CI, 1.02–1.46), 2015 (OR, 1.32; 95% CI, 1.10–1.58), and 2016 (OR, 1.31; 95% CI, 1.09–1.57) compared to 2005.
Table 4:
Logistic regression analysis of Down syndrome as underlying cause of death, 2005–2017 US Multiple Cause of Death files excluding deaths with Alzheimer’s disease/Unspecified dementia, n=16,212
| OR | 95% CI | |
|---|---|---|
| Sociodemographic Characteristics | ||
| Age (ref: 18–29) | ||
| 30–39 | 0.81* | (0.66, 0.99) |
| 40–49 | 0.95 | (0.79, 1.13) |
| 50–59 | 0.94 | (0.79, 1.12) |
| 60–69 | 0.95 | (0.79, 1.14) |
| 70–103 | 0.56*** | (0.44, 0.71) |
| Female | 0.98 | (0.91, 1.05) |
| Race-ethnicity (ref: White) | ||
| Black | 1.24** | (1.09, 1.40) |
| Hispanic | 1.16* | (1.01, 1.33) |
| Other | 1.17 | (0.90, 1.51) |
| Education (ref: 0–8 years) | ||
| 9+ years | 0.97 | (0.89, 1.06) |
| Missing | 1.00 | (0.89, 1.12) |
| Comorbidities | ||
| Number of comorbidities (ref: 1) | ||
| 2 | 0.43*** | (0.39, 0.48) |
| 3 | 0.23*** | (0.21, 0.26) |
| 4–13 | 0.09*** | (0.08, 0.10) |
| Heart disease | 0.88** | (0.81, 0.96) |
| Influenza/pneumonia | 4.48*** | (4.46, 4.94) |
| Pneumonitis | 0.94 | (0.85, 1.04) |
| Cerebrovascular diseases | 0.37*** | (0.31, 0.44) |
| Respiratory disease | 1.73*** | (1.57, 1.91) |
| Genitourinary diseases | 0.97 | (0.85, 1.10) |
| Congenital heart defect | 1.55*** | (1.31, 1.85) |
| Choking | 1.04 | (0.89, 1.22) |
| Malignant neoplasms | 0.06*** | (0.04, 0.09) |
| Non-specific conditions (R-code) | 2.76*** | (2.53, 3.01) |
| Cerebral palsy | 0.52** | (0.34, 0.81) |
| Intellectual disability | 1.64*** | (1.40, 1.92) |
| Death context and processing | ||
| Place of death (ref: Hospital inpatient) | ||
| Hospital outpatient/ER/DOA | 1.11 | (0.96, 1.29) |
| Home | 1.27*** | (1.15, 1.41) |
| Nursing home | 1.42*** | (1.29, 1.57) |
| Other/Unknown | 1.15* | (1.01, 1.32) |
| Autopsy (ref: No) | ||
| Yes | 0.58*** | (0.48, 0.70) |
| Unknown | 1.09 | (0.96, 1.25) |
| Year of death | ||
| 2006 | 1.04 | (0.87, 1.25) |
| 2007 | 1.09 | (0.91, 1.31) |
| 2008 | 1.15 | (0.96, 1.37) |
| 2009 | 1.01 | (0.85, 1.21) |
| 2010 | 1.08 | (0.90, 1.30) |
| 2011 | 1.09 | (0.91, 1.31) |
| 2012 | 1.09 | (0.91 1.31) |
| 2013 | 1.22* | (1.02, 1.46) |
| 2014 | 1.20 | (1.00, 1.44) |
| 2015 | 1.32** | (1.10, 1.58) |
| 2016 | 1.31** | (1.09, 1.57) |
| 2017 | 1.17 | (0.98, 1.41) |
| Intercept | 1.56** | (1.23, 1.98) |
Note:
p < .05,
p < .01,
p < .001.
Bold text = predictor accounted for > 1% of variance in outcome, sr2>.01.
Inaccurate reporting was less likely: at age 30–39 (OR, 0.81; 95% CI, 0.66–0.99) and 70–103 (OR, 0.49; 95% CI, 0.40–0.60) compared to age 18–29; for decedents with 2 (OR, 0.43; 95% CI, 0.39–0.48), 3 (OR, 0.23; 95% CI, 0.21–0.26), and 4–13 (OR, 0.09; 95% CI, 0.08–0.10) comorbidities compared to those with 1 comorbitity; when the decedent had a comorbidity of heart disease (OR, 0.88; 95% CI, 0.81–0.96), cerebrovascular disease (OR, 0.37; 95% CI, 0.31–0.44), or malignant neoplasm (OR, 0.06; 95% CI, 0.04–0.09); and when an autopsy was performed (OR, 0.58; 95% CI, 0.48–0.70). Based on analysis of squared semipartial correlations, the strongest predictors of the inaccurate reporting of Down syndrome as UCOD, each explaining more than 1% of the variance in the outcome, were number of comorbidities reported, as well as influenza/pneumonia, malignant neoplasms, and non-specific conditions.
Discussion
This study conceptualized inaccurate reporting of Down syndrome as either 1) the exclusive reporting of Down syndrome on the death certificate (with no other comorbidities reported) and 2) the reporting of Down syndrome as the UCOD in the presence of additional reported comorbidities, but without the presence of a diagnosis forAlzheimer’s disease or unspecified dementia. Results demonstrate that the inaccurate reporting of Down syndrome as the UCOD is associated with sociodemographic characteristics, comorbidities, and death context and processing characteristics. The majority of the strongest predictors of each type of inaccurate reporting indicated increased uncertainty surrounded the death: 1) for exclusive reporting, non-medical places of death which have less immediate access to medical records; and 2) for Down syndrome as UCOD, a lower number of reported comorbidities characteristic of a less thorough medical history present at the time of death, and the presence of a non-specific condition (R-code) on the death certificate. In addition, the association between cancer, a highly specified disease, and less likelihood of reporting of Down syndrome as UCOD also points to the role of certainty/uncertainty. Despite the fact that uncertainty does appear to play a role in inaccurate reporting, other trends were present that suggest this is not the only determinant.
Though not the strongest predictor, race/ethnicity was associated with both types of inaccurate reporting. Black decedents were more likely to have the exclusive reporting of Down syndrome than White decedents, and Black and Hispanic decedents more likely to have Down syndrome reported as the UCOD when compared to White decedents. Black Americans have historically experienced marginalization, mistreatment, and exclusion from the US health care system during life, and post-mortem (Washington, 2006), and continue to face ongoing marginalization (Taylor, 2019). Healthcare marginalization is also common among Hispanics, especially when recently immigrated to the US (Derose, Escarce, & Lurie, 2007). Thus, it is possible that Black and Hispanic adults with Down syndrome experience an intersectional layering of inequality (Turan et al., 2019) during their lives and at the time of death that results in an increased likelihood of inaccurate cause of death reporting. Results from this study revealing increased likelihood of inaccurate reporting of Down syndrome on death certificates for racial/ethnic minority decedents underscores the importance of ensuring that medical providers rely on empirical information in the death certification process of adults with developmental disabilities. This is especially the case for Black decedents, as opposed to either implicit or explicit racial biases (Balsa & McGuire, 2001, 2003). In addition, future research should explore the possibility of racial/ethnic bias in death certification reporting for this population.
In addition, it is important to draw attention to findings from this study indicating that certifiers may be reporting Down syndrome as the UCOD in instances when the decedent had a comorbidity that is more prevalent among this population – such as influenza/pneumonia, congenital heart defect, or a respiratory disease. As discussed earlier, the CDC recommends that Down syndrome be reported as the UCOD when the decedent was diagnoses with Alzheimer’s disease or unspecified dementia. However, these are the only comorbid conditions for which the CDC provides this instruction. Results from this study demonstrate that when a decedent with Down syndrome has a comorbidity that is more common among this population, such as influenza/pneumonia or a congenital heart defect, some certifiers are concluding that Down syndrome was the ‘cause’ of these diseases. While it is understandable that a medical provider may arrive at this conclusion, it is important to understand that this is inaccurate for diseases other than Alzheimer’s disease or unspecified dementia, and as such, constitutes a false equivalence. While there is indeed increased prevalence of congenital heart defects and respiratory diseases among people with Down syndrome (Barlow et al., 2001; Stephanie L. Santoro et al., 2021; Stephanie L Santoro & Steffensen, 2021), unlike Alzheimer’s disease, the evidence to date is not sufficient to suggest causality. Thus, it is important to understand that to date, outside of the link with Alzheimer’s disease, Down syndrome does not ‘cause’ death (Baird & Sadovnick, 1990; Landes, Turk, et al., 2020). In instances when the medical professional who is certifying the death certificate suspects that a medical condition (other than Alzheimer’s disease or unspecified dementia) that started the sequence of events leading to death is more prevalent among people with Down syndrome, Down syndrome should not be reported as the UCOD. Doing so is counterproductive as it hinders public health efforts to fully understand the actual cause of death trends in this population.
As results from this study demonstrate that the inaccurate reporting of Down syndrome on death certificates – inclusive of both the exclusive reporting of Down syndrome and the reporting of Down syndrome as the UCOD – is persistent over time, it is necessary to provide recommendations for death certifiers to begin rectifying this problematic practice. The summary recommendations here echo those provided in more detail in a recent article (Landes, Turk, et al., 2020), and are applicable in instances when the decedent did not have a diagnosis of Alzheimer’s disease or unspecified dementia. It is important for certifiers to understand that Down syndrome is not a disease or injury and thus not appropriate as the UCOD, but is a condition present “at the time of death and may have contributed to death” (National Center for Health Statistics 2003). For many decedents, the contribution of Down syndrome to the death process may be obvious, especially in cases when more prevalent diseases such a congenital heart defect at a younger age is present (Rubin and Crocker 2006). In these instances, after accurately reporting an appropriate medical cause of death as the UCOD, it is important for the person certifying the death certificate to also document the disability on the death certificate (Landes, Turk, et al., 2020).
It is also necessary to understand that nongenetic or nonphysiological factors of disability - such as lower SES, increased social isolation, and disparities in access to and receipt of quality health and daily care – often contribute directly or indirectly to the death of people with intellectual and developmental disabilities (Landes, Turk, et al., 2020). As it accounts for the ways in which disability may directly and indirectly contribute to death, we recommend that certifiers report Down syndrome on the death certificate even in instances when the link between this disability and the actual cause of death is not direct. While the CDC instructs to report Down syndrome as the UCOD in Part I of the death certificate when the decedent had a diagnosis of Alzheimer’s disease or unspecified dementia on rare occasions, for all other decedents with Down syndrome, the best practice is to report this disability in Part II of the death certificate (Landes, Turk, et al., 2020). As it is likely that some certifiers will continue to report Down syndrome as the UCOD, increased specification of guidance for reporting Down syndrome may be necessary in the CDC’s coding rules for standardised death certification to address inaccurate reporting (Landes, Turk, et al., 2020).
Though not engaging the topic of Down syndrome, recently there has been some debate regarding whether a different developmental disability, cerebral palsy, should be reported as the UCOD on death certificates (Landes, 2019; Ryan et al., 2019; Ryan, Ryan, & Peterson, 2020). Though not the same disability, we think this discussion is informative for the topic at hand. While the researchers disagreed as to whether characterizing the reporting of cerebral palsy as the UCOD was always an inaccurate practice, there was consensus that doing so reduced the epidemiological usefulness of death certificate data for this population. Though firm in our perspective that Down syndrome should not be reported as the UCOD except in instances when a diagnosis of Alzheimer’s disease or unspecified dementia are present at the time of death, we acknowledge that other researchers may have different opinions on this topic.
Limitations
The primary limitations of this study relate to the data. First and foremost, the data from the study is from the US. Results cannot be generalized to other countries due to differences in the death certification process. Errors and omissions are common among death certificates in general, both pertaining to demographic characteristics and cause of death data (Messite & Stellman, 1996; Nielsen, Bjornsson, & Jonasson, 1991; Rostron, Boies, & Arias, 2010). Thus, as with other characteristics of the decedent, while Down syndrome is typically recognizable, there may be instances when medical professionals certifying the death certificate do not to report this disability. Although the prevalence rate of Down syndrome among decedents during the course of the study is similar to recent estimates, our assumption is that some decedents with Down syndrome did not have their disability reported on the death certificate. While problematic in and of itself, it is not possible to know how often this occurs, but due to this possibility, it is important to emphasize that results from this study describe determinants of inaccurate reporting only among decedents with Down syndrome that had their disability reported on the death certificate. In addition, missing data for autopsy status and certifier is problematic. We made the conscious choice to maintain these cases and include a missing category for these measures as they indicate a distinct amount of uncertainty, or at least lack of thoroughness, in the death processing that may influence inaccurate reporting. This was indeed the case as both were associated with increased risk of inaccurate reporting.
Conclusion
Cause of death data is essential in efforts to reduce premature mortality among adults with Down syndrome. Thus, it is imperative that medical providers accurately report the cause of death for this population. Results from this study provide further evidence that increased uncertainty surrounding a death is associated with the inaccurate reporting of intellectual or developmental disabilities as the UCOD (Landes, Turk, et al., 2021). In addition, results demonstrate that inaccurate reporting may be associated with racial bias, and the false equivalence of disability and health conditions. While no doubt that uncertainty will be present in all medical practice (Balsa & McGuire, 2003; Good, 1998; Timmermans & Angell, 2001), especially death certification (Timmermans, 2006), this should not be an excuse for inaccuracy in death certification. Instead, even in moments of uncertainty, medical providers should rely on empirical information, as opposed to assumptions or stereotypes about certain groups of people, especially marginalised groups such as adults with Down syndrome (Balsa & McGuire, 2001, 2003). Down syndrome is a disability, and is not an accurate cause of death other than instances when the decedent had a diagnosis of Alzheimer’s disease or unspecific dementia. Thus, even when increased uncertainty surrounds the death, medical personnel should not default to diagnostic overshadowing and report Down syndrome as the UCOD if the decedent did not have a diagnosis for Alzheimer’s disease or unspecific dementia. This ramifications of this type of stereotyping during the process of death certification extend beyond the immediate decedent as inaccurately reporting Down syndrome obscures cause of death patterns, and public health efforts to prevent premature mortality for this population (Landes et al., 2019b).
Funding sources:
Research reported in this publication was supported by the National Institute On Aging of the National Institutes of Health under Award Number R03AG065638. Research in this paper also benefited from National Institute On Aging Center grant (P30AG066583), Center for Aging Policy Studies, Syracuse University. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of interest statement: No conflicts of interest have been declared.
Study is not humans subjects research as data is publicly available and fully deidentified.
References
- Ali A, Scior K, Ratti V, Strydom A, King M, & Hassiotis A (2013). Discrimination and other barriers to accessing health care: perspectives of patients with mild and moderate intellectual disability and their carers. PLoS ONE, 8(8), e70855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baird PA, & Sadovnick AD (1990). Underlying cause of death in Down syndrome: Accuracy of British Columbia death certificate data. Canadian Journal of Public Health, 81(November/December), 456–461. [PubMed] [Google Scholar]
- Balsa AI, & McGuire TG (2001). Statistical discrimination in health care. Journal of Health Economics, 20(6), 881–907. doi: 10.1016/S0167-6296(01)00101-1 [DOI] [PubMed] [Google Scholar]
- Balsa AI, & McGuire TG (2003). Prejudice, clinical uncertainty and stereotyping as sources of health disparities. Journal of Health Economics, 22(1), 89–116. doi: 10.1016/S0167-6296(02)00098-X [DOI] [PubMed] [Google Scholar]
- Barlow GM, Chen X-N, Shi ZY, Lyons GE, Kurnit DM, Celle L, … Korenberg JR (2001). Down syndrome congenital heart disease: A narrowed region and a candidate gene. Genetics in Medicine, 3(2), 91–101. doi: 10.1097/00125817-200103000-00002 [DOI] [PubMed] [Google Scholar]
- Bercovitz AR, & Pearson WS (2006). Use of computerized medical records in home health and hospice agencies; United States, 2000. National Center for Health Statistics. Vital Health Statistics, 13(161), 1–21. [PubMed] [Google Scholar]
- CDC. (2014). ICD-10 Mortality Manual 2a - 2014. Retrieved from https://www.cdc.gov/nchs/data/dvs/2a_2014.pdf
- De Alba I, & Sweningson JM (2006). English proficiency and physicians’ recommendation of Pap smears among Hispanics. Cancer Detection and Prevention, 30(3), 292–296. doi: 10.1016/j.cdp.2006.05.003 [DOI] [PubMed] [Google Scholar]
- de Graaf G, Buckley F, & Skotko BG (2017). Estimation of the number of people with Down syndrome in the United States. Genetics in Medicine, 19(4), 439–447. doi: 10.1038/gim.2016.127 [DOI] [PubMed] [Google Scholar]
- Derose KP, Escarce JJ, & Lurie N (2007). Immigrants And Health Care: Sources Of Vulnerability. Health Affairs, 26(5), 1258–1268. doi: 10.1377/hlthaff.26.5.1258 [DOI] [PubMed] [Google Scholar]
- Duruflé-Tapin A, Colin A, Nicolas B, Lebreton C, Dauvergne F, & Gallien P (2014). Analysis of the medical causes of death in cerebral palsy. Annals of Physical and Rehabilitation Medicine, 57(1), 24–37. doi: 10.1016/j.rehab.2013.11.002 [DOI] [PubMed] [Google Scholar]
- Good M-JD (1998). American medicine: The quest for competence: Univ of California Press. [Google Scholar]
- Havercamp SM, Scandlin D, & Roth M (2004). Health disparities among adults with developmental disabilities, adults with other disabilities, and adults not reporting disability in North Carolina. Public Health Reports, 119(4), 418–426. doi: 10.2307/20056702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havercamp SM, & Scott HM (2015). National health surveillance of adults with disabilities, adults with intellectual and developmental disabilities, and adults with no disabilities. Disability and Health Journal, 8(2), 165–172. doi: 10.1016/j.dhjo.2014.11.002 [DOI] [PubMed] [Google Scholar]
- Hollins S, Attard MT, von Fraunhofer N, McGuigan S, & Sedgwick P (1998). Mortality in people with learning disability: Risks, causes, and death certification findings in London. Developmental Medicine & Child Neurology, 40(1), 50–56. doi: 10.1111/j.1469-8749.1998.tb15356.x [DOI] [PubMed] [Google Scholar]
- Jha P (2012). Counting the dead is one of the world’s best investments to reduce premature mortality. Hypothesis, 10(1), e3. [Google Scholar]
- Jopp DA, & Keys CB (2001). Diagnostic Overshadowing Reviewed and Reconsidered. American Journal on Mental Retardation, 106(5), 416–433. doi: [DOI] [PubMed] [Google Scholar]
- Krahn GL, & Fox MH (2014). Health disparities of adults with intellectual disabilities: What do we know? What do we do? Journal of Applied Research in Intellectual Disabilities, 27(5), 431–446. doi: 10.1111/jar.12067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krahn GL, Walker DK, & Correa-De-Araujo R (2015). Persons With Disabilities as an Unrecognized Health Disparity Population. American Journal of Public Health, 105(S2), S198–S206. doi: 10.2105/ajph.2014.302182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landes SD (2019). Mortality risk among adults with cerebral palsy: alarming findings and lingering questions. Developmental Medicine & Child Neurology, 61(8), 860–861. doi: 10.1111/dmcn.14221 [DOI] [PubMed] [Google Scholar]
- Landes SD, McDonald KE, Wilmoth JM, & Carter Grosso E (2021). Evidence of continued reduction in the age-at-death disparity between adults with and without intellectual and/or developmental disabilities. Journal of Applied Research in Intellectual Disabilities, 34(3), 916–920. doi: 10.1111/jar.12840 [DOI] [PubMed] [Google Scholar]
- Landes SD, & Peek CW (2013). Death by mental retardation? The influence of ambiguity on death certificate coding error for adults with intellectual disability. Journal of Intellectual Disability Research, 57(12), 1183–1190. doi: 10.1111/j.1365-2788.2012.01614.x [DOI] [PubMed] [Google Scholar]
- Landes SD, Stevens JD, & Turk MA (2019a). Heterogeneity in age at death for adults with developmental disability. Journal of Intellectual Disability Research, 63, 1482–1487. doi: 10.1111/jir.12672 [DOI] [PubMed] [Google Scholar]
- Landes SD, Stevens JD, & Turk MA (2019b). Obscuring effect of coding developmental disability as the underlying cause of death on mortality trends for adults with developmental disability: a cross-sectional study using US Mortality Data from 2012 to 2016. BMJ Open, 9(2), e026614. doi: 10.1136/bmjopen-2018-026614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landes SD, Stevens JD, & Turk MA (2020). Cause of Death in Adults with Down Syndrome in the US. Disability and Health Journal, 13(4), 1–9. doi: 10.1016/j.dhjo.2020.100947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landes SD, Turk MA, & Bisesti E (2021). Uncertainty and the reporting of intellectual disability on death certificates: a cross-sectional study of US mortality data from 2005 to 2017. BMJ Open, 11(1), e045360. doi: 10.1136/bmjopen-2020-045360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landes SD, Turk MA, & Lauer E (2020). Recommendations for Accurately Reporting Intellectual and Developmental Disabilities on Death Certificates. American Journal of Preventive Medicine, 59(6), 892–895. doi: 10.1016/j.amepre.2020.05.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenfant C, & Thom T (1998). Fifty years of death certificates: The Framingham Heart Study. Annals of Internal Medicine, 129(12), 1066–1067. [DOI] [PubMed] [Google Scholar]
- Lloyd-Jones DM, Martin DO, Larson MG, & Levy D (1998). Accuracy of death certificates for coding coronary heart disease as the cause of death. Annals of Internal Medicine, 129(12), 1020–1026. doi: 10.7326/0003-4819-129-12-199812150-00005 [DOI] [PubMed] [Google Scholar]
- Mayo RM, Sherrill WW, Sundareswaran P, & Crew L (2007). Attitudes and perceptions of Hispanic patients and health care providers in the treatment of Hispanic patients: a review of the literature. Hispanic Health Care International, 5(2), 64–72. [Google Scholar]
- McGivern L, Shulman L, Carney JK, Shapiro S, & Bundock E (2017). Death Certification Errors and the Effect on Mortality Statistics. Public Health Reports, 132(6), 669–675. doi: 10.1177/0033354917736514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messite J, & Stellman SD (1996). Accuracy of death certificate completion: The need for formalized physician training. JAMA, 275(10), 794–796. doi: 10.1001/jama.1996.03530340058030 [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. (2017). Part 2 - Instructions for classifying the underlying and multiple causes of death. Retrieved from https://www.cdc.gov/nchs/nvss/instruction_manuals.htm
- National Research Council Committee on National Statistics. (2009). The US Vital Statistics System: A National Perspective. Paper presented at the Vital Statistics: Summary of a Workshop. [Google Scholar]
- Nielsen GP, Bjornsson J, & Jonasson JG (1991). The accuracy of death certificates. Implications for health statistics. Virchows Arch A Pathol Anat Histopathol, 419(2), 143–146. [DOI] [PubMed] [Google Scholar]
- O’Leary L, Hughes-McCormack L, Dunn K, & Cooper S-A (2018). Early death and causes of death of people with Down syndrome: A systematic review. Journal of Applied Research in Intellectual Disabilities, 0(0). doi:doi: 10.1111/jar.12446 [DOI] [PubMed] [Google Scholar]
- Ong LML, de Haes JCJM, Hoos AM, & Lammes FB (1995). Doctor-patient communication: A review of the literature. Social Science & Medicine, 40(7), 903–918. doi: 10.1016/0277-9536(94)00155-M [DOI] [PubMed] [Google Scholar]
- Ouellette-Kuntz H (2005). Understanding health disparities and inequities faced by individuals with intellectual disabilities. Journal of Applied Research in Intellectual Disabilities, 18(2), 113–121. doi: 10.1111/j.1468-3148.2005.00240.x [DOI] [Google Scholar]
- Peña-Guzmán DM, & Reynolds JM (2019). The harm of ableism: Medical error and epistemic injustice. Kennedy Institute of Ethics Journal, 29(3), 205–242. [DOI] [PubMed] [Google Scholar]
- Percy C, & Dolman A (1978). Comparison of the coding of death certificates related to cancer in seven countries. Public Health Reports, 93(4), 335. [PMC free article] [PubMed] [Google Scholar]
- Prasher VP, & Janicki MP (Eds.). (2019). Physical health of adults with intellectual and developmental disabilities (2nd ed.). New York: Springer. [Google Scholar]
- Presson AP, Partyka G, Jensen KM, Devine OJ, Rasmussen SA, McCabe LL, & McCabe ERB (2013). Current estimate of Down syndrome population prevalence in the United States. The Journal of Pediatrics, 163(4), 1163–1168. doi: 10.1016/j.jpeds.2013.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rostron BL, Boies JL, & Arias E (2010). Education reporting and classification on death certificates in the United States. National Center for Health Statistics. Vital and Health Statistics, 2(151). [PubMed] [Google Scholar]
- Rubin IL, & Crocker AC (2006). Medical care for children & adults with developmental disabilities (2nd Ed.). Baltimore, MD: Paul H. Brookes Publishing. [Google Scholar]
- Ryan JM, Peterson MD, Ryan N, Smith KJ, O’connell NE, Liverani S, … Allen E (2019). Mortality due to cardiovascular disease, respiratory disease, and cancer in adults with cerebral palsy. Developmental Medicine & Child Neurology, 61(8), 924–928. doi:doi: 10.1111/dmcn.14176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan JM, Ryan N, & Peterson MD (2020). Is cerebral palsy a cause of death? Developmental Medicine & Child Neurology, n/a(n/a). doi: 10.1111/dmcn.14440 [DOI] [PubMed] [Google Scholar]
- Santoro SL, Chicoine B, Jasien JM, Kim JL, Stephens M, Bulova P, & Capone G (2021). Pneumonia and respiratory infections in Down syndrome: A scoping review of the literature. American Journal of Medical Genetics Part A, 185(1), 286–299. doi: 10.1002/ajmg.a.61924 [DOI] [PubMed] [Google Scholar]
- Santoro SL, & Steffensen EH (2021). Congenital heart disease in Down syndrome–A review of temporal changes. Journal of Congenital Cardiology, 5(1), 1–14. [Google Scholar]
- Seijo R, Gomez H, & Freidenberg J (1991). Language as a Communication Barrier in Medical Care for Hispanic Patients. Hispanic Journal of Behavioral Sciences, 13(4), 363–376. doi: 10.1177/07399863910134001 [DOI] [Google Scholar]
- Snyder HM, Bain LJ, Brickman AM, Carrillo MC, Esbensen AJ, Espinosa JM, … Rafii MS (2020). Further understanding the connection between Alzheimer’s disease and Down syndrome. Alzheimer’s & Dementia, 16(7), 1065–1077. doi: 10.1002/alz.12112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spong CY, & Bianchi DW (2018). Improving Public Health Requires Inclusion of Underrepresented Populations in Research. JAMA, 319(4), 337–338. doi: 10.1001/jama.2017.19138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor J (2019). Racism, inequality, and health care for African Americans.
- Timmermans S (2006). Postmortem: How medical examiners explain suspicious deaths. Chicago: University of Chicago Press. [Google Scholar]
- Timmermans S, & Angell A (2001). Evidence-Based Medicine, Clinical Uncertainty, and Learning to Doctor. Journal of Health and Social Behavior, 42(4), 342–359. doi: 10.2307/3090183 [DOI] [PubMed] [Google Scholar]
- Trollor J, Srasuebkul P, Xu H, & Howlett S (2017). Cause of death and potentially avoidable deaths in Australian adults with intellectual disability using retrospective linked data. BMJ Open, 7(2), e013489. doi: 10.1136/bmjopen-2016-013489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turan JM, Elafros MA, Logie CH, Banik S, Turan B, Crockett KB, … Murray SM (2019). Challenges and opportunities in examining and addressing intersectional stigma and health. BMC Medicine, 17(1), 7. doi: 10.1186/s12916-018-1246-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyrer F, & McGrother C (2009). Cause-specific mortality and death certificate reporting in adults with moderate to profound intellectual disability. Journal of Intellectual Disability Research, 53(11), 898–904. doi: 10.1111/j.1365-2788.2009.01201.x [DOI] [PubMed] [Google Scholar]
- Verlinde E, De Laender N, De Maesschalck S, Deveugele M, & Willems S (2012). The social gradient in doctor-patient communication. International journal for equity in health, 11(1), 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wall M, Huang J, Oswald J, & McCullen D (2005). Factors associated with reporting multiple causes of death. BMC Medical Research Methodology, 5(1), 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Washington HA (2006). Medical apartheid: The dark history of medical experimentation on Black Americans from colonial times to the present. New York: Anchor Books. [Google Scholar]
- Willems S, De Maesschalck S, Deveugele M, Derese A, & De Maeseneer J (2005). Socio-economic status of the patient and doctor–patient communication: does it make a difference? Patient Education and Counseling, 56(2), 139–146. doi: 10.1016/j.pec.2004.02.011 [DOI] [PubMed] [Google Scholar]
- Wiseman FK, Al-Janabi T, Hardy J, Karmiloff-Smith A, Nizetic D, Tybulewicz VLJ, … Strydom A (2015). A genetic cause of Alzheimer disease: mechanistic insights from Down syndrome. Nature Reviews Neuroscience, 16(9), 564–574. doi: 10.1038/nrn3983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfbane Cybernetic Ltd. (2021). International Classification of Diseases. Retrieved from http://www.wolfbane.com/icd/index.html


