Abstract
Background:
Sexual minority women (SMW) report higher rates of heavy episodic drinking (HED) and alcohol-related outcomes, including poor mental health, than heterosexual women. These disparities indicate a greater need for behavioral and mental health treatment for SMW. This study examined associations between alcohol outcomes, behavioral and mental health help-seeking, and treatment satisfaction among SMW by age, sexual identity, race/ethnicity, and income.
Methods:
Participants included a community sample of 695 SMW (Mage = 40.0, SD = 14.1; 74.1% lesbian, 25.9% bisexual; 37.6% White, 35.8% Black, 23.2% Latinx; 26.3% annual income $14,999 or less). We used bivariate analyses to characterize the sample’s demographic characteristics and multivariable logistic regression analyses to examine associations among variables.
Results:
SMW subgroups based on age, race/ethnicity, and annual income differed in alcohol outcomes (i.e., HED, DSM-IV alcohol dependence, alcohol-related problem consequences, alcohol problem recognition, and motivation to reduce drinking); help-seeking; and treatment satisfaction. SMW who engaged in help-seeking for alcohol-related concerns, compared to those who did not, were more likely to meet criteria for DSM-IV alcohol dependence (adjusted odds ratio [aOR] = 7.13; 95% CI = 2.77; 18.36), endorse alcohol-related problem consequences (aOR = 11.44; 95% CI = 3.88; 33.71), recognize problematic drinking (aOR = 14.56; 95% CI = 3.37; 62.97), and report motivation to reduce drinking (aOR = 5.26; 95% CI = 1.74; 15.88). SMW’s alcohol outcomes did not differ based on their satisfaction with treatment or with providers.
Conclusions:
This study’s findings confirm SMW’s elevated risk for HED and other alcohol-related outcomes and underscore the importance of identity-affirmative and accessible behavioral and mental health treatment for young, Black, and low-income SMW. Clinicians and intervention scientists should develop or enhance existing brief behavioral and mental health treatments for SMW engaging in HED who may not recognize problematic drinking or who are not motivated to reduce drinking.
Keywords: sexual minority women, alcohol use, subgroup differences, help-seeking, treatment satisfaction
Introduction
Heavy episodic drinking (HED; defined as four or more drinks in one day for women; U.S. Department of Health and Human Services, 2015) and other alcohol-related outcomes (e.g., alcohol dependence, alcohol-related problem consequences) place individuals at risk for poor health, representing a serious public health problem in the United States (U.S.; Linden-Carmichael et al., 2017). Rates of HED vary among women. Sexual minority women (SMW; e.g., lesbian, bisexual) are substantially more likely than heterosexual women to report HED (Hughes et al., 2020). For example, findings from a U.S. national sample demonstrated that compared to heterosexual women, SMW are nearly four times as likely to engage in HED (Fish et al., 2018). Another national study using probability sampling methods found that SMW are also 11 times more likely than heterosexual women to meet criteria for alcohol dependence (Drabble and Trocki, 2005). Given these disparities and that women with alcohol use disorders in the general population are less likely than men with alcohol use disorders to seek help (McCrady, 2020), it is essential to understand alcohol outcomes among SMW and identify which SMW are more likely to seek help, which are more likely to be satisfied with the help they receive, and the relationship between help-seeking and treatment satisfaction and alcohol outcomes.
SMW’s Sociodemographic Differences in Alcohol Use
Minority stressors (i.e., discrimination and associated stress reactions; Brooks, 1981; Meyer, 2003) account for some proportion of SMW’s higher risk of HED, alcohol dependence, and alcohol-related problem consequences (Evans-Polce et al., 2020; Hughes et al., 2020; Meyer, 2003). For instance, one study documented prospective associations between minority stress and alcohol-related problem consequences among 18 to 25-year-old SMW (Wilson et al., 2016). SMW’s risk of HED, alcohol dependence, and alcohol-related problem consequences likely varies across age, sexual identity, race/ethnicity, and income. Documenting sociodemographic differences related to these alcohol outcomes among SMW may confirm needed health disparities-reduction initiatives for this population (Terry-McElrath and Patrick, 2020).
In the general population researchers consistently find higher rates of HED among younger women than older women (Tucker et al., 2020). This pattern is also evident among SMW. For instance, a recent review demonstrated that rates of HED, alcohol dependence, and alcohol-related problem consequences were higher among younger than older SMW (Hughes et al., 2020). However, research on alcohol use and HED tend to show lower and slower age-related declines among SMW than heterosexual women (Hughes et al., 2006; Veldhuis et al., 2017).
Recent studies using nationally representative samples provide consistent evidence of within-group heterogeneity in HED and other alcohol-related outcomes across SMW’s sexual identity (Gattis et al., 2012). For example, findings from the 2015–2017 National Survey on Drug Use and Health demonstrate that relative to monosexual SMW (i.e., lesbian), bisexual women had elevated odds of HED and alcohol use disorder (Schuler and Collins, 2020). Bisexual women’s risk of HED and other alcohol-related outcomes may be attributed to stressors that are more prevalent among bisexual women than lesbian women (e.g., anti-bisexual prejudice, sexual assault) (McConnell and Messman-Moore, 2019; Scheer et al., 2019). Nevertheless, many researchers aggregate data across SMW subgroups, potentially masking unique risks for bisexual women (Hughes et al., 2020).
Rates of HED, alcohol dependence, and alcohol-related problem consequences also vary by race/ethnicity among SMW (Hughes et al., 2020). For example, one study using a community sample found that adult Black SMW were two to three times as likely as White SMW to report heavy drinking and were almost twice as likely to report drinking-related consequences (Hughes et al., 2006). Another study demonstrated that Latinx SMW were nearly three times as likely to report alcohol dependence as White SMW (Jeong et al., 2016). However, Balsam and colleagues found no racial/ethnic differences in a national online study of young SMW’s alcohol use (Balsam et al., 2015).
There is a dearth of literature on income-based disparities in HED and other alcohol-related outcomes among SMW (Schuler et al., 2019). Nonetheless, there appears to be an income-based discrepancy between women in the general population who consume more alcohol and those at greater risk of alcohol-attributable harms. For instance, although low-income women engage in HED at lower rates, they report alcohol-related problem consequences at higher rates than women with higher incomes – also referred to as the “alcohol harm paradox” (Mulia and Bensley, 2020). However, no studies have investigated whether this alcohol harm paradox exists among SMW.
Motivation to Reduce Drinking Among SMW
Alcohol harm reduction approaches focus on minimizing harm caused by excessive alcohol consumption with or without reductions in alcohol use (Witkiewitz et al., 2020). Nevertheless, reduced drinking is associated with improved quality of life among those with alcohol use disorders (Witkiewitz et al., 2019). Although prior research has documented SMW’s drinking motives (e.g., to increase positive affect, reduce negative affect, obtain social rewards, avoid social rejection; Dworkin et al., 2020), few studies have examined SMW’s motivation to reduce drinking.
Individuals’ varying levels of motivation to change their drinking patterns can influence the delivery and effectiveness of alcohol treatment (Witkiewitz et al., 2010). For example, motivational interviewing is more effective than behavioral skills training in reducing alcohol consumption for low-motivated clients (Witkiewitz et al., 2010). Moreover, whether SMW’s motivation to reduce drinking varies by age, sexual identity, race/ethnicity, or income has received little attention.
SMW’s Help-Seeking
Approximately 70% of people with an alcohol use disorder reduce or resolve their drinking problem without intervention (Tucker et al., 2020). However, engaging in treatment improves alcohol outcomes, including remission and recovery (Timko et al., 2006). Individuals with alcohol-related problems seek help from alcohol treatment programs and mental health providers, among other services (e.g., clergy assistance, mutual aid programs; Bourdon et al., 2020). Those with problematic alcohol use are more likely to seek mental health treatment than alcohol treatment (Edlund et al., 2012). In addition, individuals who engage in HED but do not meet criteria for an alcohol use disorder may benefit from early intervention approaches, such as Screening, Brief Intervention, and Referral to Treatment (Babor et al., 2007).
Perceived need for services robustly predicts help-seeking for alcohol-related concerns (Lewis et al., 2016; Tucker et al., 2020; Tuithof et al., 2016). Yet, fewer than 25% of individuals who perceive a need for treatment (e.g., those who report comorbid mental health and substance use concerns, those with greater levels of alcohol dependence) utilize services for alcohol and related problems (Schuler et al., 2015; Tucker et al., 2020). Research using data from the National Epidemiologic Survey on Alcohol and Related Conditions highlighted that only 7.5% of individuals who met criteria for DSM-IV alcohol abuse and 24.7% who met criteria for alcohol dependence reported seeking help at some point in their lifetime (Oleski et al., 2010).
The large and chronic gap between the perceived need for treatment and help-seeking is particularly pronounced among women (Tucker et al., 2020). For example, compared to men, women who met DSM-IV diagnostic criteria for alcohol abuse or dependence had one-third to one-half the odds of seeking alcohol treatment services (Gilbert et al., 2019). Barriers to help-seeking (e.g., anticipated stigma, childcare issues, cost) may help explain the treatment gap between women who express concern about their drinking or who desire to reduce alcohol-related harm and women who access treatment (Pinedo et al., 2020; Schuler et al., 2015).
The gap between problematic alcohol use and help-seeking behavior may be even greater among SMW. Despite their increased health risks (Cerezo et al., 2021) and overall greater unmet mental health needs and perceived need for services (Filice and Meyer, 2018), SMW are less likely than heterosexual and sexual minority men to engage in alcohol treatment, but engage in alcohol treatment at about the same rates as heterosexual women (Batchelder et al., 2021). Recent findings also demonstrate that SMW, particularly bisexual women, report more barriers to accessing behavioral and mental health treatment than heterosexual women (Williams et al., 2021). Delayed help-seeking and unmet behavioral and mental health needs among SMW may be compounded by a lack of identity-affirmative care (Cerezo et al., 2021).
Help-seeking behaviors also likely vary within the SMW population. Understanding subgroup differences in help-seeking is essential to identify those in greatest need of services, develop culturally competent interventions, and reduce alcohol-related harms among SMW (Fish et al., 2021). However, research documenting SMW’s help-seeking is sparse (Cerezo et al., 2021; McCabe et al., 2013; Mulia and Bensley, 2020). Results from the few existing studies are inconsistent (Fish et al., 2021; Jeong et al., 2016). For example, one study found no interaction between race/ethnicity and sexual identity on service use (Filice and Meyer, 2018). Another study demonstrated that Latinx SMW accessed alcohol treatment at lower rates than White SMW (Jeong et al., 2016).
SMW’s Treatment Satisfaction
As identified recently in the general population (e.g., Kendra et al., 2015), treatment satisfaction is a critical component of patient-centered care. For example, clients who were more satisfied with their substance use treatment reported better treatment outcomes, including lower alcohol-related morbidity and dropout rates, reduced drinking days, and higher therapeutic alliance scores (Kendra et al., 2015; McCallum et al., 2016; Windle et al., 2020). Women’s treatment dissatisfaction is associated with individual factors (e.g., financial difficulties), program characteristics (e.g., lack of gender-responsive services), and systemic factors (e.g., the societal stigma surrounding women’s substance use) (Gilbert et al., 2019).
Among women who seek alcohol treatment, SMW report lower levels of treatment satisfaction than heterosexual women (McCabe et al., 2013; Senreich, 2021); this is especially true for bisexual women (Beard et al., 2017). Similar findings have been reported among SMW accessing mental health services (Filice and Meyer, 2018; Williams et al., 2021). SMW report treatment dissatisfaction related to providers’ limited knowledge about SMW’s needs and discriminatory attitudes toward sexual minorities, as well as lack of programming tailored to SMW’s needs (Allen and Mowbray, 2016; McCabe et al., 2013). Bisexual women and SMW of color report lower satisfaction with healthcare than monosexual SMW and White SMW, likely due to compounding effects of perceived and enacted biphobia, homophobia, and racism on the part of providers (Fish et al., 2021).
Help-Seeking, Treatment Satisfaction and Alcohol Outcomes among SMW
Findings regarding the relationship between help-seeking and alcohol problem severity are inconsistent. Some results show a strong positive association between help-seeking and alcohol use disorder severity (Grella et al., 2009), while others show a negative association (Tucker et al., 2020). Yet, the extent to which these findings apply to SMW is unknown. Moreover, given that alcohol problem recognition may be the first step toward behavioral change (Prochaska and DiClemente, 1982), there have been calls for research examining the role of help-seeking in promoting alcohol problem recognition and motivation to reduce drinking (Glass et al., 2015). Despite this promising line of inquiry, no studies have examined SMW’s help-seeking in the context of alcohol problem recognition and motivation to reduce drinking. Moreover, whether alcohol outcomes among SMW vary based on behavioral and mental health treatment satisfaction and satisfaction with providers remains poorly understood.
SMW’s Self-Perceptions of Problematic Drinking
Motivation to change is critical to engaging in drinking-reduction strategies, including help-seeking (Chang et al., 2021). Likewise, alcohol problem recognition, a cognitive dimension of motivation, is critical to promoting behavior change (Miller and Rollnick, 2012; Prochaska and DiClemente, 1982). Findings suggest that many people who report HED and other alcohol-related outcomes do not recognize harms associated with their drinking (Chang et al., 2021). In addition, prior studies have mainly focused on the extent to which drinking expectancies influence drinking behavior (Madden and Clapp, 2019). Facilitating SMW’s accurate perceptions of their drinking and readiness to change (Morgenstern et al., 2016) represent essential treatment targets in reducing alcohol-related harms among SMW. Yet virtually no studies have examined SMW’s alcohol problem recognition and motivation to change in the context of HED and other alcohol-related outcomes (i.e., alcohol dependence and alcohol-related problem consequences).
The Present Study
Aims of the current study were to examine: (1) whether alcohol outcomes (i.e., HED, DSM-IV alcohol dependence, alcohol-related problem consequences, alcohol problem recognition, and motivation to reduce drinking) varied by SMW’s age, sexual identity, race/ethnicity, and income; (2) sociodemographic correlates of behavioral and mental health help-seeking, including for alcohol problems, and satisfaction with treatment and with treatment providers: a) in general, and b) after controlling for alcohol outcomes; and (3) associations between SMW’s help-seeking and treatment satisfaction and alcohol outcomes, adjusting for sociodemographic characteristics. Our fourth, exploratory aim, was to examine bivariate associations among alcohol outcomes, adjusting for sociodemographic characteristics. Figure 1 represents a conceptual model of the hypothesized directionality of variables in the first three study aims.
Figure 1.
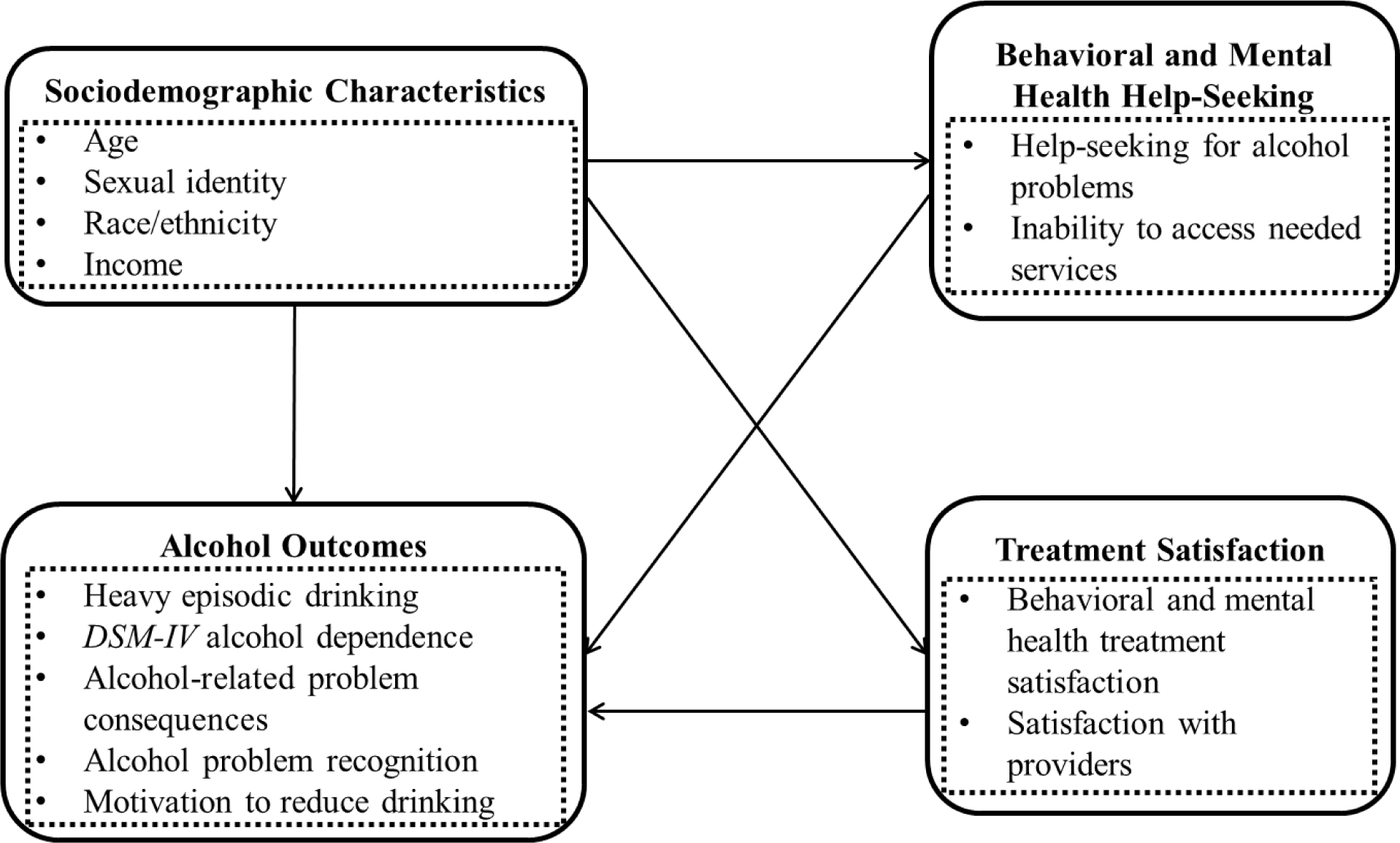
Conceptual model of sociodemographic characteristics, alcohol outcomes, behavioral and mental health help-seeking, and treatment satisfaction.
Defining alcohol dependence and alcohol-related problem consequences is necessary to make meaningful comparisons in epidemiological research (Stickel et al., 2017). The current study used DSM-IV criteria of alcohol dependence, including tolerance to the physical effects of alcohol, physiological withdrawal, preoccupation with alcohol, difficulty controlling alcohol use, and continued consumption despite harmful consequences (American Psychiatric Association, 1994). Alcohol-related problem consequences were defined as adverse harms and risk behaviors related to alcohol use (Keyes et al., 2019).
Method
Participants and Procedures
Data are from Wave 3 of the Chicago Health and Life Experiences of Women (CHLEW) study (see Hughes et al., 2021 for more details), a community-based, 21-year, five-wave longitudinal study of SMW aged 18 and older. Wave 3 data were collected in 2010–2012 (N = 353 women were retained [response rate= 79%] from the original cohort). By Wave 3, approximately 100 participants had moved out of the Chicago metropolitan area. A modified version of respondent-driven sampling was used to recruit a supplemental sample of bisexual women, younger (18–25 years) SMW, and Black and Latinx SMW (N = 373). Notably, some SMW of color in Wave 3 were recruited in Wave 1. We used data from Wave 3 because it includes the largest and most diverse sample (N = 726; 353 SMW from the original cohort and 373 SMW from the supplemental cohort). Of these, four SMW who were believed to have misrepresented their sexual identity were not included in this study. Consistent with our prior research, women who identified as mostly heterosexual, only heterosexual, or other were also excluded from analyses, leaving a final sample of 695. Data were collected using computer-assisted in-person or telephone interviews (Hughes et al., 2021). The Institutional Review Board of the University of Illinois at Chicago (UIC) approved study procedures.
Measures
Help-seeking.
Behavioral and mental health help-seeking, including for alcohol problems, was assessed with two questions. First, help-seeking for alcohol problems was assessed using responses to the question, “During the past five years, have you gone to anyone – a treatment agency, Alcoholics Anonymous, anyone at all – for help with a drinking problem of your own?” (0 = no; 1 = yes). Second, inability to access needed services for a behavioral or mental health problem, including alcohol use, (hereafter, “inability to access needed services”), was characterized by an affirmative response to, “During the past five years, has there been a mental health problem, including alcohol use, for which you wanted or needed services that you were unable to obtain?” (0 = no, 1 = yes).
Treatment satisfaction.
Treatment satisfaction for behavioral and mental health problems (hereafter, “treatment satisfaction”) was assessed by asking participants who received help to what extent their needs were met. Response options were: none of my needs were met (0), only a few of my needs were met (1), most of my needs were met (2), or almost all my needs were met (3). Responses were dichotomized as no needs were met (0) vs. at least a few needs were met (1). Satisfaction with mental health providers was assessed with the question, “Thinking about the mental health provider(s) you saw most recently, did the services… hurt you a lot (0), hurt you a little (1), make no difference (2), help you a little (3), help you a little (4) or help you a lot (5).” Responses were dichotomized as services hurt or did not help (0) vs. helped at least a little (1).
Alcohol outcomes.
The National Institute on Alcohol Abuse and Alcoholism’s (NIAAA’s) current definition of HED among women is ≥4 drinks in one day (U.S. Department of Health and Human Services, 2015). Because the CHLEW study replicated a 20-year longitudinal study of alcohol use among women in the general population, the alcohol quantity question used “6 or more drinks” as the cut-off for HED (a threshold that was adopted from the Alcohol Use Disorders Identification Test; Bradley et al., 2003; Wilsnack et al., 1984). Thus, we combined responses to this question with responses to a question asking about the typical number of drinks participants consumed on drinking days to increase our measure’s sensitivity for detecting NIAAA-defined HED while also maintaining its specificity for identifying this particular drinking behavior. Participants were classified as having past-12-month HED if they consumed either ≥6 drinks on one or more days in the past 12 months or if they typically consumed ≥4 drinks on drinking days (1 = at least one episode of consuming ≥6 drinks on one or more days in the past 12 months or consuming ≥4 drinks on drinking days, 0 = neither).
Participants who endorsed three or more past-year DSM-IV alcohol dependence symptoms (e.g., continued alcohol use despite drinking-related consequences) from five criteria were coded as meeting study criteria for past-year DSM-IV alcohol dependence (Cronbach’s α = .74; Hasin et al., 2003).
An eight-item scale was used to assess past-year alcohol-related problem consequences (e.g., drunk driving; Cronbach’s α = .65; Midanik, 1982; Wilsnack et al., 1984). We created a binary variable indicating the presence of fewer than two (0) vs. two or more alcohol-related problem consequences (1).
Lifetime alcohol problem recognition was determined by whether participants indicated that they had ever wondered if they were developing a drinking problem (0 = no, 1 = yes).
Motivation to reduce drinking was defined based on whether participants endorsed wanting or trying to cut down or stop drinking alcohol in the past year (0 = no, 1 = yes).
Sociodemographic characteristics.
Participants reported their age, sexual identity (lesbian, bisexual), race/ethnicity (White, Black, Latinx), income (annual income over $14,999 vs. annual income $14,999 or less), parental status (non-parent vs. parent), and relationship status (currently in a relationship vs. not currently in a relationship). Response options for sexual identity included ‘only lesbian/gay,’ ‘mostly lesbian/gay,’ ‘bisexual,’ ‘mostly heterosexual,’ ‘only heterosexual/straight,’ and ‘other.’ We created a dummy variable to represent those who identified as ‘only lesbian/gay’ or ‘mostly lesbian/gay’ (0) or ‘bisexual’ (1). Income was assessed with the following question: “For the last tax year, which of these categories represents your total household income, from all sources? Household means everyone living in your house that you consider part of your family.” Response options ranged from ‘under $1,000’ to ‘$200,000 or more.’ Consistent with prior studies on barriers to help-seeking for alcohol-related problems, we used a dichotomous variable (0 = above lowest quartile [> $14,999]); 1 = under lowest quartile [≤ $14,999]; Gayman et al., 2011).
Statistical Analysis
Descriptive statistics, including means, standard deviations, and proportions, were used to characterize the sample’s demographics. Bivariate analyses were used to examine associations among sociodemographic characteristics. Next, in separate multivariable logistic regression models, we examined associations between sociodemographic characteristics and alcohol outcomes. Then, in separate multivariable logistic regression models, we regressed help-seeking and treatment satisfaction variables (i.e., help-seeking for alcohol problems, inability to access needed services, treatment satisfaction, satisfaction with providers), respectively, on sociodemographic characteristics. Only participants who accessed services were asked about treatment satisfaction and satisfaction with providers. Finally, in separate logistic regression models, we regressed alcohol outcomes on behavioral and mental health help-seeking and treatment satisfaction. As an exploratory aim, logistic regression analyses examined bivariate associations among alcohol outcomes.
Sample sizes depended on the amount of missing data for each model. Missing data for explanatory variables and covariates ranged from 0 for age to 31 (4.5%) for income. Missing data for alcohol outcomes, behavioral and mental health help-seeking, and treatment satisfaction variables ranged from 0 for inability to access needed services to 97 (14.0%) for motivation to reduce drinking. We used complete case analysis (i.e., missing data were handled using pairwise deletion; Jamshidian and Mata, 2007). Only SMW who sought help for behavioral or mental health problems, including alcohol use, were included in the treatment satisfaction models. Specifically, 57.1% (n = 397) of the total sample were included in the treatment satisfaction models and 58.7% (n = 408) were included in the satisfaction with provider models. Additional sample size information for each model is presented in Tables 1–4 and in Supplemental Tables 1 and 2.
Table 1.
Sociodemographic characteristics, Chicago Health and Life Experiences of Women (CHLEW; N = 695)
| Sexual Identity | Race/Ethnicity | Incomea | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||||
| Sociodemographic Characteristics | Total sample n (%) |
Lesbian, n (%) |
Bisexual, n (%) |
Chi-Sq, t-, or F-statistic | White n (%) |
Black n (%) |
Latinx n (%) |
Chi-Sq, t-, or F-statistic | Annual income over $14,999 n (%) |
Annual income $14,999 or less n (%) |
Chi-Sq, t-, or F-statistic |
|
| |||||||||||
| Age, M [SD] | 40.0 [14.1] | 41.9 [14.2] | 34.6 [12.4] | 6.54*** | 42.9 [16.0] | 39.9 [13.1] | 35.4 [11.4] | 14.68*** | 42.0 [13.4] | 36.1 [14.4] | 4.81*** |
| Sexual identity | |||||||||||
| Lesbian | 515 (74.1) | ||||||||||
| Bisexual | 180 (25.9) | ||||||||||
| Race/Ethnicity | 0.83 | ||||||||||
| White | 261 (37.6) | 199 (38.6) | 62 (34.4) | ||||||||
| Black | 249 (35.8) | 183 (35.5) | 66 (36.7) | ||||||||
| Latinx | 161 (23.2) | 117 (22.7) | 44 (24.4) | ||||||||
| Income | |||||||||||
| Annual income over $14,999 | 481 (69.2) | 382 (74.2) | 99 (55.0) | 24.41*** | 212 (81.2) | 134 (53.8) | 115 (71.4) | 45.90*** | |||
| Annual income $14,999 or less | 183 (26.3) | 111 (21.6) | 72 (40.0) | 41 (15.7) | 102 (41.0) | 36 (22.4) | |||||
| Parental Status | 1.73 | 43.32*** | 0.48 | ||||||||
| Non-parent | 430 (61.9) | 326 (63.3) | 104 (57.8) | 190 (72.8) | 115 (46.2) | 112 (69.6) | 298 (62.0) | 108 (59.0) | |||
| Parent | 265 (38.1) | 189 (36.7) | 76 (42.2) | 71 (27.2) | 134 (53.8) | 49 (30.4) | 183 (38.0) | 75 (41.0) | |||
| Relationship Status | 12.15*** | 7.52* | 10.95*** | ||||||||
| Not in a relationship | 270 (38.8) | 181 (35.2) | 89 (49.4) | 85 (32.6) | 110 (44.2) | 63 (39.1) | 168 (34.9) | 90 (49.2) | |||
| In a relationship | 422 (60.7) | 333 (64.8) | 89 (49.4) | 175 (67.0) | 137 (55.0) | 98 (60.9) | 310 (64.4) | 93 (50.8) | |||
Note. Percentages may not equal 100 due to missing data.
Lowest quartile was used to calculate low-income status (1 = ≤ $14,999 annually)
p < .05
p < .001.
Table 4.
Logistic regression analyses assessing help-seeking and treatment satisfaction as predictors of alcohol outcomes
| Heavy Episodic Drinking | DSM-IV Alcohol Dependence | Alcohol-Related Problem Consequences | Alcohol Problem Recognition | Motivation to Reduce Drinking | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| Help-Seeking and Treatment Satisfaction Variables | aOR (95% CI) | FDR-adjusted p-value | aOR (95% CI) | FDR-adjusted p-value | aOR (95% CI) | FDR-adjusted p-value | aOR (95% CI) | FDR-adjusted p-value | aOR (95% CI) | FDR-adjusted p-value |
|
| ||||||||||
| n = 503 | n = 502 | n = 491 | n = 503 | n = 443 | ||||||
| help-seeking for alcohol problems | ||||||||||
| No help-seeking for alcohol problems | ref | ref | ref | ref | ref | |||||
| help-seeking for alcohol problems | 1.68 (0.69, 4.13) | 0.44 | 7.13** (2.77, 18.36) | 0.01 | 11.44** (3.88, 33.71) | 0.01 | 14.56** (3.37, 62.97) | 0.01 | 5.26** (1.74, 15.88) | 0.01 |
| n = 635 | n = 634 | n = 617 | n = 635 | n = 555 | ||||||
| Inability to access Needed services | ||||||||||
| Able to access needed services | ref | ref | ref | ref | ref | |||||
| Unable to access needed services | 1.32 (0.81, 2.15) | 0.38 | 1.71 (0.89, 3.27) | 0.21 | 1.77 (0.96, 3.29) | 0.14 | 1.03 (0.64, 1.65) | 0.91 | 1.53 (0.91, 2.59) | 0.22 |
| n = 365 | n = 365 | n = 354 | n = 367 | n = 320 | ||||||
| Treatment satisfaction | ||||||||||
| No needs were met | ref | ref | ref | ref | ref | |||||
| At least a few needs were met | 0.68 (0.28, 1.66) | 0.69 | 0.97 (0.30, 3.11) | 0.96 | 0.94 (0.32, 2.81) | 0.91 | 1.79 (0.78, 4.17) | 0.34 | 1.40 (0.53, 3.70) | 0.50 |
| n = 376 | n = 376 | n = 364 | n = 378 | n = 329 | ||||||
| Satisfaction with mental health providers | ||||||||||
| Providers hurt or did not help | ref | ref | ref | ref | ref | |||||
| Providers helped at least a little | 0.76 (0.40, 1.43) | 0.69 | 0.60 (0.27, 1.37) | 0.30 | 0.67 (0.30, 1.50) | 0.44 | 1.27 (0.71, 2.26) | 0.56 | 0.77 (0.40, 1.47) | 0.50 |
Note. aOR = adjusted odds ratio; CI = confidence interval; ref = reference group. All models adjusted for age, sexual identity, race/ethnicity, income, parental status, and relationship status.
FDR-adjusted refers to the Benjamini-Hochberg procedure used to correct for the false discovery rate.
p < .01.
We present exponentiated coefficients (adjusted odds ratios [aORs]), 95% confidence intervals (Cis), and p-values. Analyses were conducted in SPSS version 27. We also performed a post-hoc adjustment of p values using Benjamini-Hochberg procedures, given that we examined multiple regression models (Benjamini and Hochberg, 1995).
Three post-hoc sensitivity analyses were conducted. First, we assessed SMW who reported four or more (vs. one) episodes of past-year HED based on NIAAA’s criteria for women (≥4 drinks in one day; U.S. Department of Health and Human Services, 2015). Sensitivity analyses were conducted for all models; these analyses revealed negligible differences in results (below). Second, we regressed help-seeking and treatment satisfaction variables, respectively, on sociodemographic characteristics after accounting for differences in alcohol outcomes, given the well-established relationship between alcohol outcomes and help-seeking across epidemiologic studies (Tucker et al., 2020). Third, we regressed help-seeking and treatment satisfaction variables, respectively, on sociodemographic characteristics among SMW who reported past-12-month HED.
Results
Sample Characteristics
Participants were, on average, 40.0 years of age (SD = 14.1; range = 18 to 82). The majority identified as lesbian (74.1%); 25.9% identified as bisexual (see Table 1). Relatively equal percentages of participants identified as White (37.6%) and Black (35.8%); fewer (23.2%) identified as Latinx. More than a fourth (26.3%) of the sample reported annual incomes of $14,999 or less. The majority of participants did not have children (61.9%) and were currently in a relationship (60.7%).
Compared with bisexual women, lesbian women were older, more likely to report annual incomes over $14,999, and more likely to be in a current relationship. Similarly, White SMW were older, more likely to report annual incomes over $14,999, more likely to be in a current relationship, and less likely to have children than SMW of color. SMW who reported annual incomes over $14,999 were older and more likely to be in a current relationship than those who reported annual incomes of $14,999 or less.
Of the total sample, 292 (43.0%) reported past-year HED, 72 (10.4%) met study criteria for past-year DSM-IV alcohol dependence, 82 (11.8%) reported two or more past-year alcohol-related problem consequences, 271 (39.0%) reported lifetime alcohol problem recognition, and 153 (22.0%) reported past-year motivation to reduce drinking.
Of the total sample, 27 (3.9%) reported seeking help for alcohol-related problems; 519 (74.7%) did not indicate that they had sought help for alcohol-related problems. Rates of help-seeking for alcohol-related problems were the same when restricting the sample to those who reported past-year HED. Of the total sample, 96 (13.8%) reported being unable to access needed services for a behavioral or mental health problem, including alcohol use, whereas 599 (86.2%) did not report being unable to access needed services for a behavioral or mental health problem, including alcohol use. Of those who received help, 365 (52.5%) reported that at least a few needs were met and 32 (4.6%) reported that no needs were met. Less than half (339; 48.8%) reported that their providers helped at least a little; and 69 (9.9%) reported that their providers hurt or did not help them.
Associations between Sociodemographic Characteristics and Alcohol Outcomes
Older SMW were less likely than younger SMW to report HED (aOR = 0.95; 95% CI = 0.94; 0.96) and alcohol-related problem consequences (aOR = 0.95; 95% CI = 0.93; 0.97; see Table 2). Black SMW were four times as likely as White SMW to meet study criteria for DSM-IV alcohol dependence (aOR = 4.08; 95% CI = 1.95; 8.54) and two times as likely to report motivation to reduce drinking (aOR = 2.01; 95% CI = 1.25; 3.25). Latinx SMW were less likely than White SMW to report alcohol problem recognition (aOR = 0.62; 95% CI = 0.40; 0.95). Alcohol outcomes did not vary by sexual identity or income.
Table 2.
Logistic regression analyses assessing sociodemographic characteristics and alcohol outcomes
| Heavy Episodic Drinkinga | DSM-IV Alcohol Dependenceb | Alcohol-Related Problem Consequencesc | Alcohol Problem Recognitiond | Motivation to Reduce Drinkinge | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| Sociodemographic Characteristics | aOR (95% CI) | FDR-adjusted p-value | aOR (95% CI) | FDR-adjusted p-value | aOR (95% CI) | FDR-adjusted p-value | aOR (95% CI) | FDR-adjusted p-value | aOR (95% CI) | FDR-adjusted p-value |
|
| ||||||||||
| Sample size | n = 635 | n = 634 | n = 617 | n = 635 | n = 555 | |||||
|
| ||||||||||
| Age | 0.95*** (0.94, 0.96) | <0.001 | 0.98 (0.96, 1.01) | 0.11 | 0.95** (0.93, 0.97) | .01 | 1.01 (1.00, 1.03) | 0.10 | 0.98 (0.97, 1.00) | 0.13 |
| Sexual Identity | ||||||||||
| Lesbian | ref | ref | ref | ref | ref | |||||
| Bisexual | 1.04 (0.70, 1.56) | 0.87 | 1.27 (0.71, 2.27) | 0.47 | 1.86 (1.08, 3.21) | 0.06 | 1.16 (0.78, 1.72) | 0.57 | 0.90 (0.57, 1.43) | 0.66 |
| Race/Ethnicity | ||||||||||
| White | ref | ref | ref | ref | ref | |||||
| Black | 1.18 (0.78, 1.81) | 0.75 | 4.08** (1.95, 8.54) | 0.01 | 1.26 (0.66, 2.39) | 0.60 | 0.68 (0.46, 1.02) | 0.10 | 2.01* (1.25, 3.25) | 0.02 |
| Latinx | 1.47 (0.95, 2.29) | 0.21 | 2.29 (1.02, 5.15) | 0.11 | 1.17 (0.61, 2.26) | 0.63 | 0.62 (0.40, 0.95) | 0.10 | 1.17 (0.69, 1.98) | 0.66 |
| Income | ||||||||||
| Annual income over $14,999 | ref | ref | ref | ref | ref | |||||
| Annual income $14,999 or less | 1.04 (0.70, 1.55) | 0.87 | 1.50 (0.86, 2.61) | 0.24 | 0.76 (0.42, 1.36) | 0.58 | 0.92 (0.63, 1.36) | 0.68 | 1.14 (0.73, 1.80) | 0.66 |
Note. aOR = adjusted odds ratio; CI = confidence interval; ref = reference group. All models also adjusted for parental status and relationship status.
FDR-adjusted refers to the Benjamini–Hochberg procedure used to correct for the false discovery rate.
Past-year heavy episodic drinking (1 = ≥ 6 drinks on one or more days in the past year or ≥ 4 drinks on a typical drinking day, 0 = < 6 drinks on one or more days in the past year and < 4 drinks on a typical drinking day; Bradley et al., 2003; U.S. Department of Health and Human Services, 2015; Wilsnack et al., 1984)
Past-year DSM-IV alcohol dependence (1 = ≥ 3 DSM-IV symptoms of alcohol dependence, 0 = < 3 DSM-IV symptoms of alcohol dependence; Hasin et al., 2003)
Past-year alcohol-related problem consequences (1 = ≥ 2 alcohol problem consequence in the past year, 0 = < 2 alcohol-related problem consequences in the past year; Midanik, 1982; Wilsnack et al., 1984)
Lifetime alcohol problem recognition (1 = wondered if developing a drinking problem; 0 = never wondered if developing a drinking problem)
Past-year motivation to reduce drinking (1 = wanting to or trying to cut down or stop drinking alcohol in the past year; 0 = not wanting to or not trying to cut down or stop drinking alcohol in the past year)
p < .05
p < .01
p < .001.
Our first post-hoc sensitivity analysis examining SMW who reported four or more (vs. one) episodes of past-year HED based on NIAAA’s definition of HED among women revealed consistent findings across SMW’s age, sexual identity, and income. However, with respect to race/ethnicity, Black SMW were more likely than White SMW to report four or more episodes of past-year HED (aOR = 1.77; 95% CI = 1.02; 3.09). Similarly, Latinx SMW were more than twice as likely as White SMW to report four or more episodes of past-year HED (aOR = 2.22; 95% CI = 1.27; 3.89).
Associations between Sociodemographic Characteristics and Help-Seeking and Treatment Satisfaction
Compared to younger SMW, older SMW were less likely to report inability to access needed services (aOR = 0.97; 95% CI = 0.95; 0.99). Older SMW who received help were more likely than younger SMW to report treatment satisfaction (aOR = 1.08; 95% CI = 1.03; 1.13) and satisfaction with mental health providers (aOR = 1.05; 95% CI = 1.02; 1.08; see Table 3). These patterns persisted when adjusting for alcohol outcomes (see Supplemental Table 1).
Table 3.
Logistic regression analyses assessing sociodemographic characteristics, help-seeking, and treatment satisfaction
| Help-Seeking for Alcohol Problemsa | Inability to Access Needed Servicesb | Treatment Satisfactionc | Satisfaction with Mental Health Providersd | |||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Sociodemographic Characteristics | aOR (95% CI) | FDR-adjusted p-value | aOR (95% CI) | FDR-adjusted p-value | aOR (95% CI) | FDR-adjusted p-value | aOR (95% CI) | FDR-adjusted p-value |
|
| ||||||||
| Sample size | n = 505 | n = 637 | n = 367 | n = 378 | ||||
|
| ||||||||
| Age | 1.01 (0.98, 1.04) | 0.66 | 0.97** (0.95, 0.99) | 0.01 | 1.08*** (1.03, 1.13) | <0.001 | 1.05*** (1.02, 1.08) | <0.001 |
| Sexual Identity | ||||||||
| Lesbian | ref | ref | ref | ref | ||||
| Bisexual | 1.89 (0.75, 4.75) | 0.44 | 1.39 (0.84, 2.31) | 0.35 | 1.73 (0.68, 4.39) | 0.42 | 1.18 (0.63, 2.23) | 0.76 |
| Race/Ethnicity | ||||||||
| White | ref | ref | ref | ref | ||||
| Black | 1.51 (0.58, 3.95) | 0.66 | 0.60 (0.33, 1.08) | 0.23 | 0.31* (0.12, 0.82) | 0.05 | 0.57 (0.28, 1.15) | 0.19 |
| Latinx | 0.67 (0.18, 2.56) | 0.66 | 0.92 (0.52, 1.63) | 0.92 | 1.09 (0.34, 3.46) | 0.88 | 0.90 (0.42, 1.92) | 0.79 |
| Income | ||||||||
| Annual income over $14,999 | ref | ref | ref | ref | ||||
| Annual income $14,999 or less | 2.26 (0.92, 5.55) | 0.38 | 0.97 (0.57, 1.66) | 0.92 | 0.86 (0.36, 2.06) | 0.88 | 0.44** (0.24, 0.79) | 0.01 |
Note. aOR = adjusted odds ratio; CI = confidence interval; ref = reference group. All models also adjusted for parental status and relationship status. All help-seeking and treatment satisfaction variables were assessed within the past five years.
FDR-adjusted refers to the Benjamini–Hochberg procedure used to correct for the false discovery rate.
help-seeking for alcohol problems (1 = participants who endorsed seeking help for alcohol-related problems, 0 = participants who did not endorse seeking help for alcohol-related problems)
Inability to access needed services (1 = participants who reported having a behavioral or mental health problem for which they wanted or needed services that they were unable to obtain, 0 = participants who reported not having a behavioral or mental health problem for which they wanted or needed services that they were unable to obtain)
Treatment satisfaction (1 = participants who reported that at least a few of their needs were met, 0 = participants who reported that none of their needs were met)
Satisfaction with mental health providers (1 = participants who reported that their provider(s) helped them at least a little, 0 = participants who reported that their provider(s) hurt or did not help them)
p < .05
p < .01
p < .001.
We found no differences in help-seeking or treatment satisfaction by sexual identity even when accounting for differences in alcohol outcomes. However, over and above the effects of sociodemographic characteristics and alcohol outcomes, Black SMW were less likely than White SMW to report inability to access needed services (aOR = 0.42; 95% CI = 0.22; 0.83). Black SMW were also less likely than White SMW to report satisfaction with treatment (aOR = 0.31; 95% CI = 0.12; 0.82); this finding held after adjusting for alcohol outcomes. We found no differences in help-seeking or treatment satisfaction between Latinx SMW and White SMW with and without adjusting for alcohol outcomes.
Compared to SMW with annual incomes over $14,999, those whose incomes were $14,999 or less were less likely to report satisfaction with mental health providers (aOR = 0.44; 95% CI = 0.24; 0.79); this finding held after adjusting for alcohol outcomes. Over and above the effects of alcohol outcomes, compared to SMW with annual incomes over $14,999, those whose incomes were $14,999 or less were more than eight times as likely to report help-seeking for alcohol-related problems (aOR = 8.06; 95% CI = 1.93; 33.73).
These patterns persisted when examining associations between sociodemographic characteristics and help-seeking and treatment satisfaction only among SMW who reported engaging in HED in the past 12 months.
The Role of Help-Seeking and Treatment Satisfaction in SMW’s Alcohol Outcomes
Table 4 displays results from logistic regression models examining associations between help-seeking and treatment satisfaction and alcohol outcomes, adjusting for sociodemographic characteristics. Help-seeking for alcohol problems was positively associated with DSM-IV alcohol dependence (aOR = 7.13; 95% CI = 2.77; 18.36), alcohol-related problem consequences (aOR = 11.44; 95% CI = 3.88; 33.71), alcohol problem recognition (aOR = 14.56; 95% CI = 3.37; 62.97), and motivation to reduce drinking (aOR = 5.26; 95% CI = 1.74; 15.88). Inability to access needed services, treatment satisfaction, and satisfaction with mental health providers were not associated with alcohol outcomes. However, our post-hoc sensitivity analysis revealed that inability to access needed services was positively associated with reporting four or more episodes of past-year HED (aOR = 1.79; 95% CI = 1.05; 3.07).
Associations among SMW’s Alcohol Outcomes
We also examined associations among alcohol outcomes. As shown in Supplemental Table 2, HED was associated with DSM-IV alcohol dependence (aOR = 12.49; 95% CI = 5.44; 28.67) and alcohol-related problem consequences (aOR = 8.57; 95% CI = 4.06; 18.08). DSM-IV alcohol dependence was positively associated with alcohol-related problem consequences (aOR = 9.85; 95% CI = 5.19; 18.68). Alcohol problem recognition was associated with HED (aOR = 2.32; 95% CI = 1.61; 3.33), DSM-IV alcohol dependence (aOR = 7.78; 95% CI = 4.20; 14.42), and alcohol-related problem consequences (aOR = 3.25; 95% CI = 1.91; 5.53), and motivation to reduce drinking (aOR = 3.63; 95% CI = 2.41; 5.48). SMW who were motivated to reduce drinking were more likely than those who were not to report HED (aOR = 3.48; 95% CI = 2.24; 5.41), DSM-IV alcohol dependence (aOR = 50.61; 95% CI = 20.79; 123.24), and alcohol-related problem consequences (aOR = 3.36; 95% CI = 1.97; 5.72).
Discussion
Extending previous research (Evans-Polce et al., 2020; Hughes et al., 2020), the current study highlights heterogeneity in SMW’s alcohol outcomes, behavioral and mental health help-seeking, and treatment satisfaction.
HED, DSM-IV alcohol dependence, and alcohol-related problem consequences varied among SMW by age and race/ethnicity, but not by sexual identity or income. Specifically and aligned with prior findings (Hughes et al., 2020; Schuler and Collins, 2020), younger SMW were more likely than older SMW to report HED and alcohol-related problem consequences. Also consistent with existing research (Balsam et al., 2015; Hughes et al., 2006; Hughes et al., 2020), Black and Latinx SMW were more likely than White SMW to report HED and to meet criteria for DSM-IV alcohol dependence, but no more likely to report alcohol-related problem consequences. In fact, Black and Latinx SMW were more likely to report four or more episodes of HED in the past year. The finding that Black and Latinx SMW were no more likely than White SMW to report alcohol-related consequences differs from research with general population samples which indicates that racial/ethnic minorities report more severe alcohol-related problem consequences than White individuals (Witbrodt et al., 2014). Future studies should examine potential moderators, such as drinking to cope with heterosexist, racist, and sexist discrimination, to identify SMW of color who may be particularly vulnerable to alcohol-problem consequences (Cerezo and Ramirez, 2020). SMW reported similar HED and other alcohol outcomes regardless of sexual identity or income. Thus, we found no evidence of the “alcohol harm paradox” (i.e., low-income people engage in HED at lower rates but report alcohol-related problem consequences at higher rates than people with higher incomes; Mulia and Bensley, 2020). Additional research is needed to examine whether alcohol outcomes vary among SMW across sexual attraction or behavior and other socioeconomic factors, including financial distress and access to health insurance.
SMW differed in their motivation to reduce drinking only across race/ethnicity. Specifically, although Black SMW were less likely than White SMW to report alcohol-related problems, they were more than twice as likely to report being motivated to reduce drinking. Future studies should examine whether anticipated stigma from interviewers and normative beliefs (e.g., perceptions of others’ approval of drinking levels; Blevins et al., 2018) might influence SMW’s likelihood of recognizing or disclosing problematic drinking to interviewers.
This study also extended previous findings (McCabe et al., 2013; Mulia and Bensley, 2020) by demonstrating heterogeneity in SMW’s behavioral and mental health help-seeking and treatment satisfaction across sociodemographic characteristics. For example, older SMW were more likely than younger SMW to report accessing needed behavioral or mental health services and being satisfied with treatment and providers, even after accounting for alcohol outcomes. In addition, consistent with some research (Filice and Meyer, 2018; Jeong et al., 2016), Black SMW were more likely to report accessing needed services but were less likely to report treatment satisfaction than White SMW. Similar patterns have been observed in the general population, with research indicating that people of color are less likely than White people to receive high-quality and culturally sensitive care, likely due to implicit provider biases and institutional racism (Mays et al., 2017).
We found significant differences in help-seeking for alcohol-related problems based on income. When accounting for alcohol outcomes, SMW whose incomes were $14,999 or less were more than eight times as likely to report help-seeking for alcohol-related problems but were less likely to report satisfaction with mental health providers than SMW whose incomes were over $14,999. Few people living in poverty report satisfaction with healthcare services (Willie et al., 2020) and access to high-quality services (Funk et al., 2009). SMW living in poverty may not benefit from behavioral and mental health treatment to the same extent as SMW with higher incomes (Hodgkinson et al., 2017). Moreover, low-income SMW may be more likely to access alcohol services than SMW with higher incomes because they may be more likely to have coverage for substance use disorder treatment (e.g., through Medicaid), yet this expansion of coverage may not translate to increased access to identity-affirmative treatment (Olfson et al., 2018).
We also examined behavioral and mental health help-seeking and treatment satisfaction by sociodemographic characteristics in a subsample restricted to SMW who reported past-month HED. Findings suggest that young, Black, and low-income SMW who engage in HED but do not meet criteria for an alcohol use disorder may benefit from increased access to brief behavioral and mental health interventions (e.g., Screening, Brief Intervention, and Referral to Treatment; Babor et al., 2007) with identity-affirmative providers.
When examining associations between help-seeking and alcohol outcomes we found that SMW who sought help for alcohol-related problems were more than seven times as likely to meet study criteria for DSM-IV alcohol dependence and more than 11 times as likely to report alcohol-related problem consequences than SMW who did not seek help. This study extends prior research that has primarily applied self-selection models to explain why HED and other alcohol-related outcomes influence help-seeking (Moos and Moos, 2004). For example, one study found that individuals with elevated risk of HED were more likely to seek help than those with less severe alcohol-related problems (Witkiewitz et al., 2019). The current study is among the first to find that an inability to access needed behavioral and mental health services was associated with four or more episodes of past-year HED. Future studies should build on these results and examine whether continued treatment engagement is associated with a reduction in alcohol-related problems among those who seek behavioral and mental health services.
SMW who engaged in help-seeking for alcohol-related problems were more than 14 times as likely to report alcohol problem recognition and were more than five times as likely to be motivated to reduce drinking. These findings are supported by the transtheoretical model (Prochaska and DiClemente, 1982). For instance, SMW who sought help for alcohol-related problems may have decreased or resolved their ambivalence about drinking (Rice et al., 2014). It could also be that participants who chose to seek help for alcohol-related problems were already less ambivalent about needing to change their drinking behavior. Other psychological factors, including self-efficacy and help-seeking attitudes, may also contribute to recognizing problematic drinking and being motivated to reduce drinking (Glass et al., 2015).
Among individuals in the general population who misuse alcohol, many do not recognize alcohol-attributable harms (Chang et al., 2021). However, we found that SMW who reported HED, met study criteria for DSM-IV alcohol dependence, and reported two or more alcohol-related problem consequences were more likely to report alcohol problem recognition than SMW who did not report HED and other alcohol-related outcomes. Similarly, SMW who were motivated to reduce drinking were over three times as likely to report HED, meet study criteria for DSM-IV alcohol dependence, report two or more alcohol-related problem consequences, and report alcohol problem recognition. SMW who engage in HED and report other alcohol-related outcomes seem to accurately recognize problems associated with their drinking. SMW may respond well to motivational interviewing approaches that are tailored to their awareness of drinking problems and level of motivation to reduce drinking (Miller and Rollnick, 2012).
Clinical and Policy Implications
Our findings offer support for person-centered and multimodal treatment approaches tailored to SMW’s unique needs (e.g., psychoeducation about alcohol-related consequences, motivation to reduce drinking) and individual characteristics (e.g., age, race/ethnicity, income). Evidence-based, coordinated care is also needed to improve communication and shared decision-making – promising treatment strategies that can enhance healthcare quality among low-income people (Santiago et al., 2013), and SMW in particular (Steele et al., 2017). Reimbursement for comprehensive addiction treatment among SMW who access public insurance plans is also needed. Recognizing problematic drinking behavior could serve as a treatment target for SMW, given the overlap of SMW who wondered whether they were developing a drinking problem and those who reported high-risk drinking (e.g., HED) and who were motivated to reduce drinking. Tailored behavioral and mental health interventions that match SMW’s motivation level in reducing drinking may also prove helpful (Witkiewitz et al., 2010).
Limitations and Future Research Directions
Several limitations should be considered. Whether our results generalize to SMW living outside of the Chicago Metropolitan Area in Illinois remains unknown. Data were cross-sectional, and measures used inconsistent timeframes, limiting our ability to address temporal sequencing among study variables. Further, data were collected in 2010–2012. Societal attitudes toward sexual minorities appear to have improved; SMW today may report fewer barriers to and greater satisfaction with treatment. Newer studies need to determine whether this is the case or whether our findings are replicated, particularly for younger SMW, bisexual women, racial/ethnic minority SMW, and SMW living in poverty.
This study utilized retrospective self-report measures and several measures were single-item indicators. There were no measures of the reasons SMW utilized services, or of services or provider characteristics. For example, individuals with problematic alcohol use are more likely to seek mental health treatment than alcohol treatment (Edlund et al., 2012). This study did not distinguish among substance use disorder treatment, general mental health providers, and other support sources. Also, our HED measure may not have identified HED among SMW who typically drank three or fewer drinks, but occasionally consumed four or more.
Several directions for future research are reviewed below. To improve understanding of help-seeking and treatment satisfaction among SMW, additional research is needed to compare our results with those from samples of SMW who are in recovery or who engage in high-intensity HED. Future research should also consider including SMW who are not exclusively cisgender and who report a broader range of sexual identities and racial/ethnic identities. Other variables not included in this study, such as mental health comorbidities and prior help-seeking experiences, may be associated with help-seeking and treatment satisfaction among SMW (Allen and Mowbray, 2016; Hughes et al., 2020; McCabe et al., 2013). Longitudinal studies are needed to test prospective associations between help-seeking, treatment satisfaction, and alcohol outcomes among SMW. Future studies could build on our findings by exploring the potential role of ambivalence in reducing drinking among SMW and whether different mechanisms (e.g., alcohol craving, alcohol expectancies, alcohol cue reactivity) influence alcohol problem recognition and motivation to reduce drinking across SMW’s sociodemographic characteristics.
Interventions are needed that enhance treatment motivation among SMW, particularly those who are ambivalent about changing their behavior – for example, by eliciting client statements for change (Kuerbis et al., 2018). Also, no studies to date have examined whether SMW benefit from receiving treatment tailored to their perceptions of problematic drinking or their motivation to reduce drinking (i.e., modularized treatment approaches; Witkiewitz et al., 2010). Researchers should also aim to understand SMW’s goals for treatment (e.g., moderate drinking vs. abstinence) to help develop tailored behavioral and mental health interventions for this population (Pachankis et al., 2020; Scheer et al., in press). Finally, determining whether the timing of SMW’s help-seeking impacts alcohol outcomes could identify resources for those who delay needed treatment compared to those who report repeated treatment episodes.
Conclusion
The current study highlights heterogeneity in SMW’s alcohol outcomes, behavioral and mental health help-seeking, and treatment satisfaction across age, sexual identity, race/ethnicity, and income. Our findings underscore the importance of increasing SMW’s access to culturally sensitive and effective personalized behavioral and mental health treatment – especially SMW who are at heightened risk for HED and negative alcohol-related outcomes, who are unable to access needed services, and who are not satisfied with their treatment or providers. Delivering alcohol interventions that match SMW’s level of motivation to reduce drinking and identifying multi-level barriers to recognizing problematic alcohol use may be particularly important for younger SMW, SMW of color, and SMW with low incomes.
Supplementary Material
Acknowledgements:
The CHLEW study is supported by NIAAA (R01AA013328-15; PI: Hughes), which also supports Lauren Bochicchio’s postdoctoral fellowship. Jillian Scheer acknowledges support from the National Institute on Alcohol Abuse and Alcoholism under grant K01AA028239. Abigail Batchelder acknowledges support from the National Institute on Drug Abuse under grant K23DA043418. Jeremy Kidd acknowledges support from the National Institute on Alcohol Abuse and Alcoholism under grant K23AA028296. The research presented herein is the authors’ own and does not represent the views of the funders, including the National Institutes of Health.
Footnotes
Author Disclosure Statement
No competing financial interests exist.
References
- Allen JL, Mowbray O (2016) Sexual orientation, treatment utilization, and barriers for alcohol related problems: Findings from a nationally representative sample. Drug and Alcohol Dependence 161:323–330. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (1994) Diagnostic and Statistical Manual of Mental Disorders: DSM-IV - (4th ed.). Washington DC: American Psychiatric Association. [Google Scholar]
- Babor TF, McRee BG, Kassebaum PA, Grimaldi PL, Ahmed K, Bray J (2007) Screening, Brief Intervention, and Referral to Treatment (SBIRT) toward a public health approach to the management of substance abuse. Substance Abuse 28:7–30. [DOI] [PubMed] [Google Scholar]
- Balsam KF, Molina Y, Blayney JA, Dillworth T, Zimmerman L, Kaysen D (2015) Racial/ethnic differences in identity and mental health outcomes among young sexual minority women. Cultural Diversity & Ethnic Minority Psychology 21:380–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batchelder AW, Stanton AM, Kirakosian N, King D, Grasso C, Potter J, Mayer KH, O’Cleirigh C (2021) Mental health and substance use diagnoses and treatment disparities by sexual orientation and gender in a community health center sample. LGBT Health 8: 290–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beard C, Kirakosian N, Silverman AL, Winer JP, Wadsworth LP, Björgvinsson T (2017) Comparing treatment response between LGBQ and heterosexual individuals attending a CBT- and DBT-skills-based partial hospital. Journal of Consulting and Clinical Psychology 85:1171–1181. [DOI] [PubMed] [Google Scholar]
- Benjamini Y, Hochberg Y (1995) Controlling the False Discovery Rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society 57:289–300. [Google Scholar]
- Blevins CE, Walker DD, Stephens RS, Banes KE, Roffman RA (2018) Changing social norms: The impact of normative feedback included in motivational enhancement therapy on cannabis outcomes among heavy-using adolescents. Addictive Behaviors 76:270–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourdon JL, Tillman R, Francis MW, Dick DM, Stephenson M, Kamarajan C, ...McCutcheon VV (2020) Characterization of service use for alcohol problems across generations and sex in adults with alcohol use disorder. Alcoholism: Clinical and Experimental Research 44:746–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley KA, Bush KR, Epler AJ, Dobie DJ, Davis TM, Sporleder JL, Maynard C, Burman ML, Kivlahan DR (2003) Two brief alcohol-screening tests from the Alcohol Use Disorders Identification Test (AUDIT): Validation in a female Veterans Affairs patient population. Archives of Internal Medicine 163:821–829. [DOI] [PubMed] [Google Scholar]
- Brooks V (1981) Minority stress and lesbian women. Lexington, MA: Lexington Books. [Google Scholar]
- Cerezo A, Ching S, Ramirez A (2021) Healthcare access and health-related cultural norms in a community sample of Black and Latinx sexual minority gender expansive women. Journal of Homosexuality. [DOI] [PubMed] [Google Scholar]
- Cerezo A, Ramirez A (2020) Perceived discrimination, alcohol use disorder and alcohol-related problems in sexual minority women of color. Journal of Social Service Research 0:1–14. [Google Scholar]
- Chang C, Wang TJ, Chen MJ, Liang SY, Wu SF, Bai MJ (2021) Factors influencing readiness to change in patients with alcoholic liver disease: A cross-sectional study. Journal of Psychiatric and Mental Health Nursing 28:344–355. [DOI] [PubMed] [Google Scholar]
- Drabble L, Trocki K (2005) Alcohol consumption, alcohol-related problems, and other substance use among lesbian and bisexual women. Journal of Lesbian Studies 9:19–30. [DOI] [PubMed] [Google Scholar]
- Dworkin ER, Jaffe AE, Fitzpatrick S, Rhew IC, Kaysen D (2020) Daily relationships between posttraumatic stress symptoms, drinking motives, and alcohol consumption in trauma-exposed sexual minority women. Psychology of Addictive Behaviors 35:3–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edlund MJ, Booth BM, Han X (2012) Who seeks care where? Utilization of mental health and substance use disorder treatment in two national samples of individuals with alcohol use disorders. Journal of Studies on Alcohol and Drugs 73:635–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans-Polce RJ, Kcomt L, Veliz PT, Boyd CJ, McCabe SE (2020) Alcohol, tobacco, and comorbid psychiatric disorders and associations with sexual identity and stress-related correlates. American Journal of Psychiatry 177:1073–1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filice E, Meyer SB (2018) Patterns, predictors, and outcomes of mental health service utilization among lesbians, gay men, and bisexuals: A scoping review. Journal of Gay & Lesbian Mental Health 22:162–195. [Google Scholar]
- Fish JN, Turpin RE, Williams ND, Boekeloo BO (2021) Sexual identity differences in access to and satisfaction with health care: Findings from nationally representative data. American Journal of Epidemiology 190:1281–1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fish JN, Hughes TL, Russell ST (2018) Sexual identity differences in high-intensity binge drinking: Findings from a US national sample. Addiction 113:749–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Funk M, Lund C, Freeman M, Drew N (2009) Improving the quality of mental health care. International Journal for Quality in Health Care 21:415–420. [DOI] [PubMed] [Google Scholar]
- Gattis MN, Sacco P, Cunningham-Williams RM (2012) Substance use and mental health disorders among heterosexual identified men and women who have same-sex partners or same-sex attraction: Results from the national epidemiological survey on alcohol and related conditions. Archives of Sexual Behavior 41:1185–1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gayman MD, Cuddeback GS, Morrissey JP (2011) Help-seeking behaviors in a community sample of young adults with substance use disorders. The Journal of Behavioral Health Services & Research 38:464–477. [DOI] [PubMed] [Google Scholar]
- Gilbert PA, Pro G, Zemore SE, Mulia N, Brown G. (2019) Gender differences in use of alcohol treatment services and reasons for non-use in a national sample. Alcoholism, Clinical and Experimental Research 43:722–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glass JE, Grant JD, Yoon HY, Bucholz KK (2015) Alcohol problem recognition and help seeking in adolescents and young adults at varying genetic and environmental risk. Drug and Alcohol Dependence 153:250–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grella CE, Karno MP, Warda US, Moore AA, Niv N (2009) Perceptions of need and help received for substance dependence in a national probability survey. Psychiatric Services 60:1068–1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Schuckit MA, Martin CS, Grant BF, Bucholz KK, Helzer JE (2003) The validity of DSM-IV alcohol dependence: What do we know and what do we need to know? Alcoholism: Clinical and Experimental Research 27:244–252. [DOI] [PubMed] [Google Scholar]
- Hodgkinson S, Godoy L, Beers LS, Lewin A (2017) Improving mental health access for low-income children and families in the primary care setting. Pediatrics 139:e20151175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes TL, Wilsnack S, Martin K, Matthews A, Johnson T (2021). Alcohol use among sexual minority women: Methods used and lessons learned in the 20-Year Chicago Health and Life Experiences of Women Study. The International Journal of Alcohol and Drug Research 9:30–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes TL, Wilsnack S, Szalacha L, Johnson T, Bostwick W, Seymour R, Aranda F, Benson P, Kinnison K (2006) Age and racial/ethnic differences in drinking and drinking-related problems in a community sample of lesbians. Journal of Studies on Alcohol 67:579–590. [DOI] [PubMed] [Google Scholar]
- Hughes TL, Veldhuis CB, Drabble LA, Wilsnack SC (2020) Research on alcohol and other drug (AOD) use among sexual minority women: A global scoping review. PLoS One 15: e0229869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamshidian M, Mata M (2007) Advances in analysis of mean and covariance structure when data are incomplete. In Lee S-Y (Ed.), Handbook of Latent Variable and Related Models (pp. 21–44). North-Holland. [Google Scholar]
- Jeong YM, Veldhuis CB, Aranda F, Hughes TL (2016) Racial/ethnic differences in unmet needs for mental health and substance use treatment in a community-based sample of sexual minority women. Journal of Clinical Nursing 25:3557–3569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendra MS, Weingardt KR, Cucciare MA, Timko C (2015) Satisfaction with substance use treatment and 12-step groups predicts outcomes. Addictive Behaviors 40:27–32. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Jager J, Mal-Sarkar T, Patrick ME, Rutherford C, Hasin D (2019) Is there a recent epidemic of women’s drinking? A critical review of national studies. Alcoholism: Clinical and Experimental Research 43:1344–1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuerbis A, Houser J, Levak S, Shao S, Morgenstern J (2018) Exploration of treatment matching of problem drinker characteristics to motivational interviewing and non-directive client-centered psychotherapy. Journal of Substance Abuse Treatment 86:9–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis E, Jamison A, Ghaus S, Durazo E, Frayne S, Hoggatt K, Bean-Mayberry B, Timko C, Cucciare M (2016) Receptivity to alcohol-related care among US women veterans with alcohol misuse. Journal of Addictive Diseases 35:226–237. [DOI] [PubMed] [Google Scholar]
- Linden-Carmichael AN, Vasilenko SA, Lanza ST, Maggs JL (2017) High-intensity drinking versus heavy episodic drinking: Prevalence rates and relative odds of alcohol use disorder across adulthood. Alcoholism: Clinical and Experimental Research 41:1754–1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madden DR, Clapp JD (2019) The event-level impact of one’s typical alcohol expectancies, drinking motivations, and use of protective behavioral strategies. Drug and Alcohol Dependence 194:112–120. [DOI] [PubMed] [Google Scholar]
- Mays VM, Jones A, Delany-Brumsey A, Coles C, Cochran SD (2017) Perceived discrimination in healthcare and mental health/substance abuse treatment among Blacks, Latinos, and Whites. Medical Care 55:173–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Hughes TL, Bostwick WB, West BT, Boyd CJ (2009) Sexual orientation, substance use behaviors and substance dependence in the United States. Addiction 104:1333–1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCallum SL, Mikocka-Walus AA, Gaughwin MD, Andrews JM, Turnbull DA (2016) I’m a sick person, not a bad person: Patient experiences of treatments for alcohol use disorders. Health Expectations 19:828–841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McConnell AA, Messman-Moore TL (2019) Hazardous drinking, antibisexual prejudice, and sexual revictimization among bisexual women: A moderated mediation model. Psychology of Violence 9:526–535. [Google Scholar]
- McCrady BS (2020) Treatment interventions for women with alcohol use disorder. Alcohol Research: Current Reviews 40:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer I (2003) Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin 129:674–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Midanik L (1982) The validity of self-reported alcohol consumption and alcohol problems: A literature review. British Journal of Addiction 77:357–382. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S (2012) Motivational interviewing: Helping people change. Guilford Press. [Google Scholar]
- Moos RH, Moos BS (2004) The interplay between help-seeking and alcohol-related outcomes: Divergent processes for professional treatment and self-help groups. Drug and Alcohol Dependence 75:155–164. [DOI] [PubMed] [Google Scholar]
- Morgenstern J, Kuerbis A, Houser J, Muench F, Shao S, Treloar H (2016) Within-person associations between daily motivation and self-efficacy and drinking among problem drinkers in treatment. Psychology of Addictive Behaviors 30:630–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulia N, Bensley KM (2020) Alcohol-related disparities among women: Evidence and potential explanations. Alcohol Research: Current Reviews 40:09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oleski J, Mota N, Cox BJ, Sareen J (2010) Perceived need for care, help seeking, and perceived barriers to care for alcohol use disorders in a national sample. Psychiatric Services 61:1223–1231. [DOI] [PubMed] [Google Scholar]
- Olfson M, Wall M, Barry CL, Mauro C, Mojtabai R (2018) Impact of Medicaid expansion on coverage and treatment of low-income adults with substance use disorders. Health Affairs 37:1208–1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachankis JE, McConocha EM, Clark KA, Wang K, Behari K, Fetzner BK, Brisbin CD, Scheer JR, Lehavot K (2020) A transdiagnostic minority stress intervention for gender diverse sexual minority women’s depression, anxiety, and unhealthy alcohol use: A randomized controlled trial. Journal of Consulting and Clinical Psychology 88:613–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinedo M, Zemore S, Beltrán-Girón J, Gilbert P, Castro Y (2020) Women’s barriers to specialty substance abuse treatment: A qualitative exploration of racial/ethnic differences. Journal of Immigrant and Minority Health 22:653–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC (1982) Transtheoretical therapy: Toward a more integrative model of change. Psychotherapy: Theory, Research & Practice 19:276–288. [Google Scholar]
- Rice SL, Hagler KJ, Tonigan JS (2014) Longitudinal trajectories of readiness to change: Alcohol use and help-seeking behavior. Journal of Studies on Alcohol and Drugs 75:486–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santiago CD, Kaltman S, Miranda J (2013) Poverty and mental health: How do low-income adults and children fare in psychotherapy? Journal of Clinical Psychology 69:115–126. [DOI] [PubMed] [Google Scholar]
- Scheer JR, Clark KA, McConocha E, Wang K, Pachankis JE (in press). Toward cognitive-behavioral therapy for sexual minority women: Voices from stakeholders and community members. Cognitive and Behavioral Practice. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheer JR, McConocha E, Behari K, Pachankis JE (2021) Sexual violence as a mediator of sexual orientation disparities in alcohol use, suicidality, and sexual-risk behaviour among female youth. Psychology & Sexuality 12:37–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuler MS, Puttaiah S, Mojtabai R, Crum RM (2015) Perceived barriers to treatment for alcohol problems: A latent class analysis. Psychiatric Services 66:1221–1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuler MS, Collins RL (2020) Sexual minority substance use disparities: Bisexual women at elevated risk relative to other sexual minority groups. Drug and Alcohol Dependence 206:107755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuler MS, Stein BD, Collins RL (2019) Differences in substance use disparities across age groups in a national cross-sectional survey of lesbian, gay, and bisexual adults. LGBT Health 6:68–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senreich E (2021) Perceptions of treatment according to sexual orientation in urban substance use disorder (SUD) programs with mostly nonwhite client populations. Journal of Gay & Lesbian Social Services. [Google Scholar]
- Steele LS, Daley A, Curling D, Gibson MF, Green DC, Williams CC, Ross LE (2017) LGBT identity, untreated depression, and unmet need for mental health services by sexual minority women and trans-identified people. Journal of Women’s Health 26:116–127. [DOI] [PubMed] [Google Scholar]
- Stickel F, Moreno C, Hampe J, Morgan MY (2017) The genetics of alcohol dependence and alcohol-related liver disease. Journal of Hepatology 66:195–211. [DOI] [PubMed] [Google Scholar]
- Terry-McElrath YM, Patrick ME (2020) U.S. adolescent alcohol use by race/ethnicity: Consumption and perceived need to reduce/stop use. Journal of Ethnicity in Substance Abuse 19:3–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timko C, Debenedetti A, Billow R (2006) Intensive referral to 12-Step self-help groups and 6-month substance use disorder outcomes. Addiction 101:678–688. [DOI] [PubMed] [Google Scholar]
- Tucker JA, Chandler SD, Witkiewitz K (2020) Epidemiology of recovery from alcohol use disorder. Alcohol Research: Current Reviews 40:02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuithof M, ten Have M, van den Brink W, Vollebergh W, de Graaf R (2016) Treatment seeking for alcohol use disorders: Treatment gap or adequate self-selection? European Addiction Research 22:277–285. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (2015) Drinking levels defined. Retrieved from https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking. [DOI] [PubMed]
- Veldhuis CB, Talley AE, Hancock DW, Wilsnack SC, Hughes TL (2017) Alcohol use, age, and self-rated mental and physical health in a community sample of lesbian and bisexual women. LGBT Health 4:419–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams ND, Turpin RE, Akré ERL, Boekeloo BO, Fish JN (2021) Disparities in mental health care access among persons differing in sexual identity: Nationally representative findings. Psychiatric Services. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willie TC, Bastida C, Olavarrieta CD, Scolese A, Campos PA, Falb KL, Gupta J, (2020) Socioecological determinants of community resource utilisation among low-income women in Mexico City who experienced male-to-female intimate partner violence. Global Public Health 15:1627–1638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilsnack RW, Wilsnack SC, Klassen AD (1984) Women’s drinking and drinking problems: Patterns from a 1981 national survey. American Journal of Public Health 74:1231–1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson SM, Gilmore AK, Rhew IC, Hodge KA, Kaysen DL (2016) Minority stress is longitudinally associated with alcohol-related problems among sexual minority women. Addictive Behaviors, 80–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witbrodt J, Mulia N, Zemore SE, Kerr WC (2014) Racial/ethnic disparities in alcohol-related problems: Differences by gender and level of heavy drinking. Alcoholism: Clinical and Experimental Research 38:1662–1670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Wilson AD, Pearson MR, Montes KS, Kirouac M, Roos CR, Hallgren KA, Maisto SA (2019) Profiles of recovery from alcohol use disorder at three years following treatment: Can the definition of recovery be extended to include high functioning heavy drinkers? Addiction 114:69–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Heather N, Falk DE, Litten RZ, Hasin DS, Kranzler HR, Mann KF, O’Malley SS, Anton RF (2020) World Health Organization risk drinking level reductions are associated with improved functioning and are sustained among patients with mild, moderate and severe alcohol dependence in clinical trials in the United States and United Kingdom. Addiction 115:1668–1680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Hartzler B, Donovan D (2010) Matching motivation enhancement treatment to client motivation: Re-examining the Project MATCH motivation matching hypothesis. Addiction 105:1403–1413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Litten RZ, Leggio L (2019) Advances in the science and treatment of alcohol use disorder. Science Advances 5:eaax4043. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


