Abstract
Background
Alternative scientometric measures have introduced a novel view of the scientific literature. This study aimed to identify the top 50 most-cited recent articles in the field of knee and hip arthroplasty, characterize their traditional and alternative scientometric measures, and determine the relationship between traditional and alternative scientometric measures.
Material and methods
The 50 most-cited articles with the term “arthroplasty” in the title that were published between 2015 and 2019 were retrieved from the Scopus database. Alternative scientometric parameters such as Altmetric Attention Score (AAS) from Altmetrics bookmarklet (Altmetrics.com) were retrieved. Scientometric variables such as journal impact factor, first author H-index, and keywords were also extracted.
Results
The 50 most-cited papers accrued 7955 total citations, with a mean of 159.10 ± 56.4 citations per article. The overall mean AAS across the papers was 63.4 ± 164.8. The mean first author’s H-index was 23.8 ± 18.9. Papers published in 2017 and 2018 had a significantly higher mean AAS than those published in 2015 and 2016 (35.1 vs 22.5, P = .009). Citation count was weakly correlated with the AAS (correlation coefficient = 0.379, P = .009). Also, AAS had significant correlations with the journal’s impact factor (P < .001).
Conclusion
We found that the AAS was highest in more recently published papers, while citation count had the opposite trend. The AAS was significantly correlated with the journal’s impact factor and citation count, but the correlation is weak. This suggests that the alternative scientometric measures are complementary to, and not substitutes for, complement traditional measures such as citation count and impact factor.
Keywords: Altmetric, Arthroplasty, Bibliometric, Joint, Scientometric
Background
Traditional scientometric measures, such as citation count, journal impact factor, and the H-index, are extensively used to quantify the distribution and impact of the published scientific literature. While such metrics have proven useful, several drawbacks limit their validity and reliability [1,2]. Furthermore, there is a substantial lead time between the publication of a study and the traditional scientometric measures, meaning that there is a delay of 12-24 months from the time a study is published to the time that such metrics detect the utilization and impact of the study [3].
Alternative scientometric measures have been introduced to complement the traditional measures and minimize the lead time [4,5]. These alternative measures are designed to provide a different view of the effect of scientific publications, namely the social media attention and distribution. The alternative scientometric measures have emerged in response to the ubiquitous use of social media and online forums and nontraditional news outlets by the authors, their audience, and the laypeople. The Altmetric Attention Score (AAS) was developed by the Altmetric Institute (Altmetric.com) and introduced in 2010, as a tool to evaluate the attention garnered by an article on online platforms [3,5]. AAS includes Twitter, Facebook, Google Plus, LinkedIn, news outlets, scientific blogs, Wikipedia, Reddit, policy documents, patents, YouTube, Publons and PubPeer, and online reference managers Mendeley and CiteULike. AAS is an overall weighted index of how widely an article is mentioned on social media.
Joint arthroplasty is one of the most common elective surgical procedures globally, and the volume of primary and revision total joint arthroplasty (TJA) has skyrocketed in recent decades. It is important to know the implications of the rapid increase of joint arthroplasty volume for current research in this area [[6], [7], [8]]. The joint arthroplasty literature is an ever-expanding field with a considerable number of published studies and active researchers. The social media outreach of the current arthroplasty literature is largely unknown. Therefore, the purpose of this study was to identify the top 50 most-cited recent articles in the field of joint arthroplasty and characterize their traditional and alternative scientometric measures. We also sought to determine the relationship between traditional and alternative scientometric measures. We hypothesized that the citation count and AAS would not show a strong correlation in the arthroplasty literature, similar to previously reported data in other fields.
Material and methods
Study selection
The Scopus database was searched for articles published in English between January 2015 and December 2019 that had the term “Arthroplasty” in their title. The 50 most-cited papers were selected from this. The Scopus database was selected because it provides a broader and more comprehensive list of journals, papers, and citation numbers. Two reviewers (S.P.M. and M.S.) screened this list of papers to exclude studies not related to hip or knee arthroplasty. Conflicts were resolved by consensus. The same reviewers extracted the Altmetric data subsequently into an excel sheet. This study did not include patient data and was exempt from institutional review board approval.
Data extraction
Publication year and citation count, as well as the journal’s impact factor, first author’s H-index, and keywords, were extracted from the Scopus database and academic-accelerator.com. The citation density, defined as the number of citations per year, was also calculated. Each article was reviewed, and the main topic and study population were identified. The Altmetric data were extracted from the Altmetric bookmarklet (Altmetrics.com) and included AAS and social media coverage. ResearchGate interest score was also recorded for each article from researchgate.net. Data were entered into a Microsoft Excel sheet. All data were extracted during week 1 (May 01, 2022, to November 01, 2022) to minimize missed data. Level of evidence was extracted as same as mentioned in the included studies. If the study does not mention the level of evidence, Journal of Bone & Joint Surgery guidelines were used to assign level of evidence [9].
AAS contribution
AAS is calculated as the weighted sum of the article’s mentions across different media platforms, with a larger AAS indicating a higher level of social media attention. Table 1 summarizes the platforms contributing to the AAS and their corresponding coefficient value. Unlisted platforms do not contribute to the AAS [10].
Table 1.
Media platforms contributing to the Altmetric Attention Score and their respective weight coefficient.
| Platform | Weight per mention |
|---|---|
| News media | 8 |
| Blogs | 5 |
| Wikipedia | 3 |
| Policy documents | 3 |
| 1 | |
| F1000/Publons/PubPeer | 1 |
| Open syllabus | 1 |
| Google+ | 1 |
| 0.25 | |
| YouTube | 0.25 |
| 0.25 |
Statistical analysis
Quantitative variables are reported as mean ± standard deviation, and categorical variables are reported as frequency. Continuous variables are compared between 2 groups by the Mann-Whitney test and between >2 groups by Kruskal-Wallis Test due to the nonparametric nature of the data. Data normality was assessed by observing the histogram with a normality curve. For discovering the correlation between continuous variables, the Spearman correlation test was used. The level of significance was set at P < .05. SPSS version 22.0 for windows (IBM, Armonk, NY) was used for all the statistical analyses.
Results
After excluding shoulder [[11], [12], [13], [14], [15], [16]] and disc [10], the 50 most-cited recently published papers were retrieved. All of them were in English, and all were available for a full-text review. Bibliographic data of the selected articles are represented in Table 2. The alternative metrics data are shown in Table 3.
Table 2.
List of the 50 most-cited articles in Scopus, 2015-2019 with “Arthroplasty” in the title.
| Rank | Year | Title and reference | First author and Scopus H-index | Journal | 2-y-Impact factor 2020 | Study design | Country | Subject | Level of evidence | Cited by | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2018 | Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030 [7] | Sloan M. | 9 | Journal of Bone and Joint Surgery, American volume | 5.284 | Retrospective observational | USA | TJA volume projection | 3 | 452 |
| 2 | 2015 | The epidemiology of revision total knee and hip arthroplasty in England and Wales: A comparative analysis with projections for the United States. A study using the national joint registry data set [17] | Patel A. | 6 | The Bone & Joint Journal | 5.082 | Retrospective observational | UK | TJA volume projection | 3 | 260 |
| 3 | 2015 | Predictors of persistent pain after total knee arthroplasty: A systematic review and meta-analysis [18] | Lewis G.N. | 28 | British Journal of Anesthesia | 9.166 | Meta-analysis | New Zealand | Complications | 3 | 242 |
| 4 | 2016 | Trends and predictors of opioid use after total knee and total hip arthroplasty [19] | Goesling J. | 17 | Pain | 6.961 | Prospective observational | USA | Opioid use | 2 | 238 |
| 5 | 2017 | Projected increase in total knee arthroplasty in the United States—an alternative projection model [20] | Inacio M.C.S. | 43 | Osteoarthritis and Cartilage | 6.576 | Retrospective observational | Australia | TJA volume projection | 3 | 231 |
| 6 | 2015 | Comparative Epidemiology of Revision Arthroplasty: Failed THA Poses Greater Clinical and Economic Burdens Than Failed TKA [21] | Bozic K.J. | 64 | Clinical Orthopedics and Related Research | 4.176 | Retrospective observational | USA | Epidemiology | 3 | 229 |
| 7 | 2015 | Future projections of total hip and knee arthroplasty in the UK: Results from the UK Clinical Practice Research Datalink [22] | Culliford D. | 23 | Osteoarthritis and Cartilage | 6.576 | Retrospective observational | UK | TJA volume projection | 3 | 205 |
| 8 | 2017 | Patient Dissatisfaction Following Total Knee Arthroplasty: A Systematic Review of the Literature [23] | Gunaratne R. | 2 | Journal of Arthroplasty | 4.757 | Systematic review | Australia | Outcome | 3 | 189 |
| 9 | 2016 | Early Results of Medicare's Bundled Payment Initiative for a 90-Day Total Joint Arthroplasty Episode of Care [24] | Iorio R. | 49 | Journal of Arthroplasty | 4.757 | Retrospective observational | USA | Health-care economics | 3 | 185 |
| 10 | 2017 | Current Epidemiology of Revision Total Knee Arthroplasty in the United States [25] | Delanois R.E. | 35 | Journal of Arthroplasty | 4.757 | Retrospective observational | USA | Epidemiology | 3 | 183 |
| 11 | 2016 | Patient-related risk factors for periprosthetic joint infection after total joint arthroplasty: A systematic review and meta-analysis [26] | Kunutsor S.K. | 41 | PLoS ONE | 3.24 | Meta-analysis | UK | Complications | 3 | 183 |
| 12 | 2017 | Current Epidemiology of Revision Total Hip Arthroplasty in the United States: National Inpatient Sample 2009 to 2013 [27] | Gwam C.U. | 17 | Journal of Arthroplasty | 4.757 | Retrospective observational | USA | Epidemiology | 3 | 181 |
| 13 | 2017 | Fully porous 3D printed titanium femoral stem to reduce stress-shielding following total hip arthroplasty [28] | Arabnejad S. | 8 | Journal of Orthopedic Research | 3.494 | Instrumentation | Canada | Instrumentation | NA | 177 |
| 14 | 2018 | Aspirin or rivaroxaban for VTE prophylaxis after hip or knee arthroplasty [29] | Anderson D.R. | 68 | New England Journal of Medicine | 91.245 | Randomized clinical trial | Canada | Thromboembolism | 1 | 168 |
| 15 | 2016 | Patient satisfaction after total knee arthroplasty [30] | Choi Y.-J. | 5 | Knee Surgery & Related Research | NA | Narrative review | South Korea | Outcome | 5 | 166 |
| 16 | 2015 | Anterior vs Posterior Approach for Total Hip Arthroplasty, a Systematic Review and Meta-analysis [31] | Higgins B.T. | 3 | Journal of Arthroplasty | 4.757 | Meta-analysis | Lebanon | Outcome | 3 | 166 |
| 17 | 2015 | Patient-reported outcomes after total and unicompartmental knee arthroplasty: A study of 14 076 matched patients from the national joint registry for England and Wales [32] | Liddle A.D. | 22 | The Bone & Joint Journal | 5.082 | Retrospective observational | UK | Outcome | 3 | 165 |
| 18 | 2015 | Lifetime medical costs of knee osteoarthritis management in the United States: Impact of extending indications for total knee arthroplasty [33] | Losina E. | 78 | Arthritis Care & Research | 4.794 | Retrospective observational | USA | Health-care economics | 3 | 165 |
| 19 | 2015 | The clinical outcome of minimally invasive Phase 3 Oxford unicompartmental knee arthroplasty [34] | Pandit H. | 50 | The Bone & Joint Journal | 5.082 | Retrospective observational | UK | Outcome | 2 | 154 |
| 20 | 2015 | Computer navigation for total knee arthroplasty reduces revision rate for patients less than 65 years of age [35] | De Steiger R.N. | 28 | Journal of Bone and Joint Surgery—American Volume | 5.284 | Retrospective observational | Australia | Complications | 3 | 151 |
| 21 | 2015 | Pain catastrophizing as a risk factor for chronic pain after total knee arthroplasty: A systematic review [36] | Burns L.C. | 9 | Journal of Pain Research | 3.133 | Meta-analysis | Canada | Complications | 2 | 147 |
| 22 | 2015 | Current failure mechanisms after knee arthroplasty have changed: Polyethylene wear is less common in revision surgery [37] | Thiele K. | 9 | Journal of Bone and Joint Surgery—American Volume | 5.284 | Retrospective observational | Germany | Complications | 3 | 147 |
| 23 | 2016 | Discharge Destination After Total Joint Arthroplasty: An Analysis of Postdischarge Outcomes, Placement Risk Factors, and Recent Trends [38] | Keswani A. | 14 | Journal of Arthroplasty | 4.757 | Retrospective observational | USA | Outcome | 3 | 142 |
| 24 | 2015 | Quantifying the Burden of Revision Total Joint Arthroplasty for Periprosthetic Infection [39] | Kamath A.F. | 28 | Journal of Arthroplasty | 4.757 | Retrospective observational | USA | Epidemiology | 3 | 142 |
| 25 | 2015 | Surgical approach in primary total hip arthroplasty: Anatomy, technique and clinical outcomes [40] | Petis S. | 11 | Canadian Journal of Surgery | 2.089 | Narrative review | UK | Outcome | 5 | 140 |
| 26 | 2016 | Hypoalbuminemia Independently Predicts Surgical Site Infection, Pneumonia, Length of Stay, and Readmission After Total Joint Arthroplasty [41] | Bohl D.D. | 37 | Journal of Arthroplasty | 4.757 | Retrospective observational | USA | Complications | 3 | 138 |
| 27 | 2016 | Robotics in Arthroplasty: A Comprehensive Review [42] | Jacofsky D.J. | 28 | Journal of Arthroplasty | 4.757 | Narrative review | USA | Robotics | 5 | 137 |
| 28 | 2015 | What Is the Learning Curve for the Anterior Approach for Total Hip Arthroplasty? [43] | de Steiger R.N. | 28 | Clinical Orthopedics and Related Research | 4.176 | Retrospective observational | Australia | Outcome | 3 | 136 |
| 29 | 2015 | A Subject-Specific Musculoskeletal Modeling Framework to Predict in Vivo Mechanics of Total Knee Arthroplasty [44] | Marra M.A. | 7 | Journal of Biomechanical Engineering | 2.097 | Biomechanical study | Netherland | Biomechanic | NA | 136 |
| 30 | 2016 | Enhanced recovery after surgery for primary hip and knee arthroplasty: A review of the evidence [45] | Soffin E.M. | 11 | British Journal of Anaesthesia | 9.166 | Narrative review | USA | Recovery & rehabilitation | 5 | 135 |
| 31 | 2016 | The epidemiology of failure in total knee arthroplasty avoiding your next revision [46] | Khan M. | 5 | The Bone & Joint Journal | 5.082 | Narrative review | UK | Complications | 5 | 135 |
| 32 | 2016 | Improved accuracy of component positioning with robotic-assisted unicompartmental knee arthroplasty [47] | Bell S.W. | 8 | Journal of Bone and Joint Surgery—American Volume | 5.284 | Randomized clinical trial | UK | Robotics | 1 | 134 |
| 33 | 2015 | Systematic Review of Patient-specific Instrumentation in Total Knee Arthroplasty: New but Not Improved [48] | Sassoon A. | 15 | Clinical Orthopedics and Related Research | 4.176 | Systematic review | USA | Instrumentation | 3 | 134 |
| 34 | 2017 | Effect of genotype-guided warfarin dosing on clinical events and anticoagulation control among patients undergoing hip or knee arthroplasty: The GIFT randomized clinical trial [49] | Gage B.F. | 57 | JAMA—Journal of the American Medical Association | 56.272 | Randomized clinical trial | USA | Thromboembolism | 1 | 133 |
| 35 | 2015 | Cup position alone does not predict risk of dislocation after hip arthroplasty [50] | Esposito C.I. | 19 | Journal of Arthroplasty | 4.757 | Retrospective observational | USA | Complications | 3 | 130 |
| 36 | 2016 | Preoperative Reduction of Opioid Use Before Total Joint Arthroplasty [51] | Nguyen L.-C.L. | 5 | Journal of Arthroplasty | 4.757 | Retrospective observational | USA | Opioid use | 3 | 129 |
| 37 | 2017 | Effect of Bundled Payments and Health Care Reform as Alternative Payment Models in Total Joint Arthroplasty: A Clinical Review [52] | Siddiqi A. | 8 | Journal of Arthroplasty | 4.757 | Narrative review | USA | Health-care economics | 5 | 128 |
| 38 | 2017 | Dislocation of a primary total hip arthroplasty is more common in patients with a lumbar spinal fusion [53] | Buckland A.J. | 16 | The Bone & Joint Journal | 5.082 | Retrospective observational | USA | Complications | 3 | 126 |
| 39 | 2015 | Rapid recovery protocols for primary total hip arthroplasty can safely reduce length of stay without increasing readmissions [54] | Stambough J.B. | 24 | Journal of Arthroplasty | 4.757 | Retrospective observational | USA | Recovery & rehabilitation | 3 | 126 |
| 40 | 2017 | Opioid Use After Total Knee Arthroplasty: Trends and Risk Factors for Prolonged Use [55] | Bedard N.A. | 25 | Journal of Arthroplasty | 4.757 | Retrospective observational | USA | Opioid use | 3 | 125 |
| 41 | 2016 | Validation of the KOOS, JR: A Short-form Knee Arthroplasty Outcomes Survey [56] | Lyman S. | 54 | Clinical Orthopedics and Related Research | 4.176 | Retrospective observational | USA | Outcome | 3 | 122 |
| 42 | 2015 | Pelvic Tilt in Patients Undergoing Total Hip Arthroplasty: When Does it Matter? [57] | Maratt J.D. | 8 | Journal of Arthroplasty | 4.757 | Retrospective observational | USA | Preoperative planning | 3 | 120 |
| 43 | 2015 | General compared with spinal anesthesia for total hip arthroplasty [58] | Basques B.A. | 33 | Journal of Bone and Joint Surgery—American Volume | 5.284 | Retrospective observational | USA | Anesthesia | 3 | 118 |
| 44 | 2015 | The Otto Aufranc Award: Modifiable vs Nonmodifiable Risk Factors for Infection After Hip Arthroplasty [59] | Maoz G. | 5 | Clinical Orthopedics and Related Research | 4.176 | Retrospective observational | USA | Complications | 4 | 117 |
| 45 | 2015 | In-home telerehabilitation compared with faceto-face rehabilitation after total knee arthroplasty: A noninferiority randomized controlled trial [60] | Moffet H. | 28 | Journal of Bone and Joint Surgery—American Volume | 5.284 | Randomized clinical trial | Canada | Recovery & rehabilitation | 1 | 117 |
| 46 | 2016 | Patient-reported outcome measures in arthroplasty registries: Report of the Patient-Reported Outcome Measures Working Group of the International Society of Arthroplasty RegistriesPart II. Recommendations for selection, administration, and analysis [61] | Rolfson O. | 25 | Acta Orthopaedica | 3.717 | Comment | Sweden | Outcome | 5 | 116 |
| 47 | 2015 | Effect of adductor canal block vs femoral nerve block on quadriceps strength, mobilization, and pain after total knee arthroplasty: A randomized, blinded study [62] | Grevstad U. | 10 | Regional Anesthesia and Pain Medicine | 6.288 | Randomized clinical trial | Denmark | Outcome | 1 | 115 |
| 48 | 2015 | Does varus alignment adversely affect implant survival and function 6 years after kinematically aligned total knee arthroplasty? [63] | Howell S.M. | 49 | International Orthopedics | 3.075 | Prospective observational | USA | Outcome | 3 | 114 |
| 49 | 2017 | Alignment options for total knee arthroplasty: A systematic review [64] | Rivière C. | 16 | Orthopedics and Traumatology: Surgery & Research | 2.256 | Systematic review | UK | Surgery technique | 1 | 113 |
| 50 | 2017 | The minimal clinically important difference for Knee Society Clinical Rating System after total knee arthroplasty for primary osteoarthritis [65] | Lee W.C. | 4 | Knee Surgery, Sports Traumatology, Arthroscopy | 4.342 | Retrospective observational | Singapore | Outcome | 4 | 113 |
(citation number was retrieved from the Scopus, February 2022).
Table 3.
Altmetric indices for the 50 most-cited articles published 2015-2019.
| Rank | First author | Year | Cited by | Research interest score | Altmetric attention score (AAS) | Dimensions | Mendeley | Policy source | News outlet | Blogs | Patent | Wikipedia | Research highlight platform | Redditors | Google user | CiteULike | Connotea | Video uploaders | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Sloan M. [7] | 2018 | 452 | 299.3 | 85 | 8 | 594 | 512 | 1 | 1 | ||||||||||
| 2 | Patel A. [17] | 2015 | 260 | 158 | Altmetric hasn't picked up any sharing activity around this article yet. | |||||||||||||||
| 3 | Lewis G.N. [18] | 2015 | 242 | 153.6 | Altmetric hasn't picked up any sharing activity around this article yet. | |||||||||||||||
| 4 | Goesling J. [19] | 2016 | 238 | 137.2 | 223 | 26 | 270 | 251 | 3 | 28 | 1 | |||||||||
| 5 | Inacio M.C.S. [20] | 2017 | 231 | 141.5 | 23 | 13 | 264 | 320 | 1 | 2 | ||||||||||
| 6 | Bozic K.J. [21] | 2015 | 229 | 137.5 | 5 | 8 | 264 | 261 | 1 | |||||||||||
| 7 | Culliford D. [22] | 2015 | 205 | 129.2 | 24 | 3 | 238 | 304 | 2 | 1 | ||||||||||
| 8 | Gunaratne R. [23] | 2017 | 189 | 122.9 | 27 | 18 | 236 | 252 | 2 | |||||||||||
| 9 | Iorio R. [24] | 2016 | 185 | 98.8 | 3 | 214 | 138 | 1 | ||||||||||||
| 10 | Delanois R.E. [25] | 2017 | 183 | 122.1 | 2 | 3 | 225 | 274 | ||||||||||||
| 11 | Kunutsor S.K. [26] | 2016 | 183 | 106.4 | 13 | 1 | 215 | 322 | 1 | 1 | ||||||||||
| 12 | Gwam C.U. [27] | 2017 | 181 | 122.4 | 35 | 238 | 208 | 5 | ||||||||||||
| 13 | Arabnejad S. [28] | 2017 | 177 | 118.2 | 82 | 3 | 199 | 432 | 2 | 8 | 2 | 2 | 1 | |||||||
| 14 | Anderson D.R. [29] | 2018 | 168 | 98 | 657 | 844 | 198 | 446 | 24 | 10 | 5 | 3 | 1 | 1 | ||||||
| 15 | Choi Y.-J. [30] | 2016 | 166 | 102.2 | 62 | 52 | 180 | 339 | 2 | |||||||||||
| 16 | Higgins B.T. [31] | 2015 | 166 | 99.6 | 12 | 8 | 194 | 286 | 1 | 1 | ||||||||||
| 17 | Liddle A.D. [32] | 2015 | 165 | 90.6 | 35 | 41 | 181 | 155 | 2 | |||||||||||
| 18 | Losina E. [33] | 2015 | 165 | 96.1 | 12 | 5 | 187 | 258 | 1 | |||||||||||
| 19 | Pandit H. [34] | 2015 | 154 | 84.9 | 16 | 23 | 169 | 84 | 2 | |||||||||||
| 20 | De Steiger R.N. [35] | 2015 | 151 | 89.2 | 14 | 4 | 176 | 149 | 2 | 1 | ||||||||||
| 21 | Burns L.C. [36] | 2015 | 147 | 86.8 | 12 | 12 | 155 | 228 | 1 | 1 | ||||||||||
| 22 | Thiele K. [37] | 2015 | 147 | 88 | 10 | 1 | 171 | 139 | 1 | 1 | ||||||||||
| 23 | Keswani A. [38] | 2016 | 142 | 76.1 | 12 | 3 | 170 | 182 | 1 | |||||||||||
| 24 | Kamath A.F. [39] | 2015 | 142 | 82.8 | Altmetric hasn't picked up any sharing activity around this article yet. | |||||||||||||||
| 25 | Petis S. [40] | 2015 | 140 | 97.5 | 4 | 4 | 168 | 500 | 2 | |||||||||||
| 26 | Bohl D.D. [41] | 2016 | 138 | 80.7 | 1 | 2 | 161 | 145 | ||||||||||||
| 27 | Jacofsky D.J. [42] | 2016 | 137 | 93.6 | 5 | 4 | 186 | 316 | 1 | |||||||||||
| 28 | de Steiger R.N. [43] | 2015 | 136 | 84.5 | 8 | 11 | 164 | 132 | ||||||||||||
| 29 | Marra M.A. [44] | 2015 | 136 | 86.9 | 2 | 1 | 151 | 298 | 1 | 1 | ||||||||||
| 30 | Soffin E.M. [45] | 2016 | 135 | 82.1 | 8 | 10 | 163 | 269 | 1 | |||||||||||
| 31 | Khan M. [46] | 2016 | 135 | 85.2 | 71 | 97 | 153 | 118 | 2 | |||||||||||
| 32 | Bell S.W. [47] | 2016 | 134 | 113.9 | 5 | 3 | 170 | 107 | 1 | |||||||||||
| 33 | Sassoon A. [48] | 2015 | 134 | 75.8 | 6 | 7 | 151 | 158 | 1 | |||||||||||
| 34 | Gage B.F. [49] | 2017 | 133 | 41.1 | 850 | 191 | 150 | 193 | 3 | 1 | 89 | 8 | 5 | 2 | ||||||
| 35 | Esposito C.I. [50] | 2015 | 130 | 74.3 | 2 | 2 | 148 | 145 | ||||||||||||
| 36 | Nguyen L.-C.L. [51] | 2016 | 129 | 76.1 | 8 | 13 | 160 | 129 | 1 | |||||||||||
| 37 | Siddiqi A. [52] | 2017 | 128 | 90.6 | 6 | 2 | 162 | 183 | 2 | 1 | ||||||||||
| 38 | Buckland A.J. [53] | 2017 | 126 | 81.7 | 99 | 148 | 165 | 155 | 3 | |||||||||||
| 39 | Stambough J.B. [54] | 2015 | 126 | 76.9 | 405 | 2 | 143 | 158 | 51 | |||||||||||
| 40 | Bedard N.A. [55] | 2017 | 125 | 35.6 | 5 | 8 | 152 | 101 | 1 | |||||||||||
| 41 | Lyman S. [56] | 2016 | 122 | 79.4 | 6 | 9 | 148 | 199 | 1 | |||||||||||
| 42 | Maratt J.D. [57] | 2015 | 120 | 65.3 | 10 | 1 | 142 | 153 | 1 | 1 | ||||||||||
| 43 | Basques B.A. [58] | 2015 | 118 | 63.5 | 6 | 4 | 127 | 167 | 1 | 1 | 1 | |||||||||
| 44 | Maoz G. [59] | 2015 | 117 | 66.3 | 5 | 2 | 130 | 152 | 1 | 1 | ||||||||||
| 45 | Moffet H. [60] | 2015 | 117 | 88.2 | 23 | 17 | 147 | 334 | 1 | 1 | 1 | 1 | ||||||||
| 46 | Rolfson O. [61] | 2016 | 116 | 77.2 | 1 | 1 | 139 | 161 | ||||||||||||
| 47 | Grevstad U. [62] | 2015 | 115 | 74.2 | 11 | 16 | 143 | 175 | 4 | |||||||||||
| 48 | Howell S.M. [63] | 2015 | 114 | 64.7 | 3 | 125 | 126 | 1 | ||||||||||||
| 49 | Rivière C. [64] | 2017 | 113 | 103.9 | 2 | 2 | 135 | 218 | ||||||||||||
| 50 | Lee W.C. [65] | 2017 | 113 | 72.3 | Altmetric hasn't picked up any sharing activity around this article yet. |
(Altmetric indices were retrieved from the Scopus, February 2022).
Table 4 illustrates the citation and AAS data broken down by year, country of origin, and journal characteristics. Overall, the 50 most-cited papers accrued 7955 total citations, with a mean of 159.10 ± 56.4 (range 113-452) citations per article and 32.7 ± 19.6 citations per year per article. The overall mean AAS across the papers was 63.4 ± 164.8 (median = 10.5). The mean first author’s H-index was 23.8 ± 18.9, and each paper had a mean of 6.5 ± 4.7 authors. Not surprisingly, 24 articles on our list were published in 2015. However, the 2 papers with the highest AAS were published in 2018. Furthermore, papers published in 2017 and 2018 (most recent papers) had a significantly higher mean AAS than those published in 2015 and 2016 (149.5 ± 273.1 vs 29.5 ± 77.7, P = .030). No significant difference was observed between them regarding citation number (175.3 ± 87.0 vs 152.8 ± 38.6, P = .75).
Table 4.
Citation and Altmetric Attention Score (AAS) data broken down by variables of interest.
| Frequency (percent) | Citations (mean ± SD) | AAS (mean ± SD) | |
|---|---|---|---|
| Overall | 50 (100%) | 159.10 ± 56.4 | 63.4 ± 164.8 |
| Year | |||
| 2015 | 24 (48%) | 153.2 ± 41.0 | 29.8 ± 86.4 |
| 2016 | 13 (26%) | 150.8 ± 33.9 | 32.1 ± 61.7 |
| 2017 | 11 (22%) | 154.5 ± 39.1 | 113.1 ± 261.1 |
| 2018 | 2 (4%) | 310.0 ± 200.8 | 371.0 ± 404.5 |
| 2019 | 0 | - | - |
| P valuea | .36 | .12 | |
| Country | |||
| USA | 25 (50%) | 159.1 ± 56.4 | 75.1 ± 188.8 |
| UK | 9 (18%) | 165.4 ± 45.1 | 21.3 ± 23.0 |
| Australia | 4 (8%) | 176.8 ± 42.5 | 18.0 ± 8.6 |
| Canada | 4 (8%) | 152.3 ± 26.7 | 193.5 ± 310.5 |
| Others (N = 1 for Denmark, Germany, Lebanon, Netherland, New Zealand, South Korea, Singapore, Sweden) | 8 (16%) | 150.1 ± 43.0 | 16.3 ± 22.9 |
| P valuea | .44 | .23 | |
| Article type | |||
| Original | 37 (74%) | 160.5 ± 62.7 | 79.1 ± 189.5 |
| Retrospective observational | 27 (54%) | 166.4 ± 69.0 | 34.6 ± 82.6 |
| Randomized clinical trial | 5 (10%) | 133.4 ± 21.2 | 309.2 ± 411.3 |
| Others (N = 1 for Biomechanical study, comment, instrumentation) | 3 (6%) | 143.0 ± 31.1 | 28.3 ± 46.5 |
| Prospective observational | 2 (4%) | 176.0 ± 87.7 | 113.0 ± 155.6 |
| Review | 13 (26%) | 155.0 ± 34.3 | 19.0 ± 23.2 |
| Narrative review | 6 (12%) | 140.2 ± 13.3 | 26.0 ± 31.5 |
| Meta-analysis | 4 (8%) | 184.5 ± 41.1 | 12.3 ± 0.57 |
| Systematic review | 3 (6%) | 145.3 ± 39.2 | 11.7 ± 13.4 |
| P valueb (comparing review vs original articles) | .57 | .81 | |
| P valuea (among review article types) | .11 | .63 | |
| Open access | |||
| Yes | 4 (8%) | 144.8 ± 28.5 | 420.7 ± 210.4 |
| No | 46 (92%) | 160.3 ± 58.2 | 119.5 ± 18.4 |
| P valueb | .72 | .73 | |
| Site | |||
| Knee | 22 (44%) | 149.9 ± 35.9 | 17.4 ± 19.2 |
| Knee and hip | 17 (34%) | 187.4 ± 79.9 | 129.0 ± 262.4 |
| Hip | 11 (22%) | 133.8 ± 20.3 | 57.6 ± 164.8 |
| P valuea | .014∗ | .66 | |
| Topic | |||
| Outcome | 13 (26%) | 141.4 ± 25.0 | 16.4 ± 17.5 |
| Complication | 10 (20%) | 151.6 ± 36.5 | 25.2 ± 34.9 |
| Epidemiologic | 4 (8%) | 183.8 ± 35.6 | 14.0 ± 18.2 |
| TJA volume projection | 4 (8%) | 287.0 ± 112.3 | 44.0 ± 35.5 |
| Others (N = 1 for anesthesia, biomechanics, preoperative planning, surgery technique) | 4 (8%) | 121.8 ± 9.9 | 5.0 ± 3.8 |
| Recovery & rehabilitation | 3 (6%) | 126.0 ± 9.0 | 145.3 ± 225.0 |
| Health-care economics | 3 (6%) | 159.3 ± 28.9 | 7.0 ± 4.6 |
| Opioid use | 3 (6%) | 164.0 ± 64.1 | 78.7 ± 125.0 |
| Robotics | 2 (4%) | 135.5 ± 2.1 | 5.0 ± 0.0 |
| Instrumentation | 2 (4%) | 155.5 ± 30.4 | 44.0 ± 53.7 |
| Thromboembolism | 2 (4%) | 150.5 ± 24.7 | 753.5 ± 136.5 |
| P valuea | .03∗ | .11 | |
| Journal | |||
| Journal of Arthroplasty | 15 (30%) | 148.1 ± 25.2 | 38.1 ± 106.1 |
| Journal of Bone and Joint Surgery | 6 (12%) | 186.5 ± 130.8 | 23.83 ± 30.7 |
| Clinical Orthopedics and Related Research | 5 (10%) | 147.6 ± 46.2 | 6.0 ± 1.2 |
| Bone and Joint Journal | 5 (10%) | 168.0 ± 53.7 | 55.3 ± 37.0 |
| Others | 19 (38%) | 159.1 ± 56.4 | 117.0 ± 247.9 |
| P valuea | .90 | .09 |
Asterisk indicates that P-value is <.05 and statistically significant.
Bold indicates the significantly different value (P < .05) from other values in the table.
Kruskal-Wallis test.
Mann-Whitney test.
The mean and median level of evidence was 3.0 for articles, comprising 6/3/30/2/7 papers with a level 1/2/3/4/5 of evidence, respectively. Regarding 2 popular social media platforms, Twitter and Facebook, a median of 7 (range 0-843) and 1 (range 1-23) post was published, respectively. The median impact factor of journals was 4.8 (range 2.1 to 91.2).
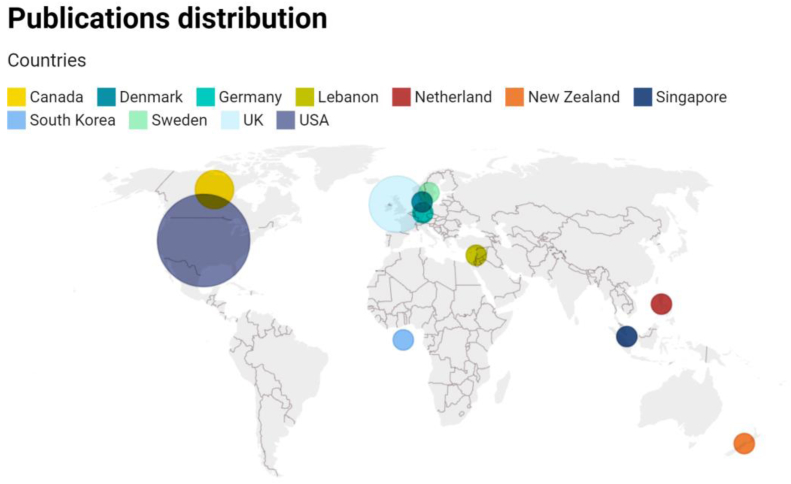
With 25 publications, the United States institutions contributed the greatest number of papers to our list, followed by the United Kingdom [9], Australia [4], and Canada [4]. Figure 1 illustrates the country of origin of the articles assessed in this study.
Figure 1.
Distribution of the country of origin among papers included in this study.
The majority of publications (74.0%) were original research, and retrospective observational studies were predominant with 27 papers. Meta-analyses had the highest mean citation count among all methodologies (184.5 ± 41.1). Studies on knee arthroplasty were more frequent [22], followed by hip and knee [17] and hip arthroplasty [12]. The Journal of Arthroplasty contributed the greatest number of papers [16], followed by the Journal of Bone and Joint Surgery [6], Clinical Orthopedics and Related Research [5], and Bone and Joint Journal [5].
Functional and radiological outcomes [14], complications [11], epidemiologic studies [4], and TJA volume projection [4] were the most frequent subject across the papers. TJA volume projection studies had a significantly higher number of citations among different topics (287.0 ± 112.3, P = .03).
Table 5 summarizes the frequent keywords out of 138 keywords that were used in the papers included in this study.
Table 5.
Keywords used in the papers included in this study (27/50 articles provided keywords, keywords that did not repeat were omitted).
| Keywords | Frequency |
|---|---|
| Total knee arthroplasty | 12 |
| Total hip arthroplasty | 7 |
| Arthroplasty | 7 |
| Epidemiology | 6 |
| Knee | 4 |
| Total knee replacement | 3 |
| Hip | 3 |
| Projections | 3 |
| Opioid | 3 |
| Alignment | 2 |
| Chronic pain | 2 |
| Incidence rates | 2 |
| Infection | 2 |
| National Inpatient Sample | 2 |
| Osteoarthritis | 2 |
| Patient-reported outcomes | 2 |
| Readmissions | 2 |
| Revision | 2 |
| Risk factors | 2 |
| Satisfaction | 2 |
Correlations
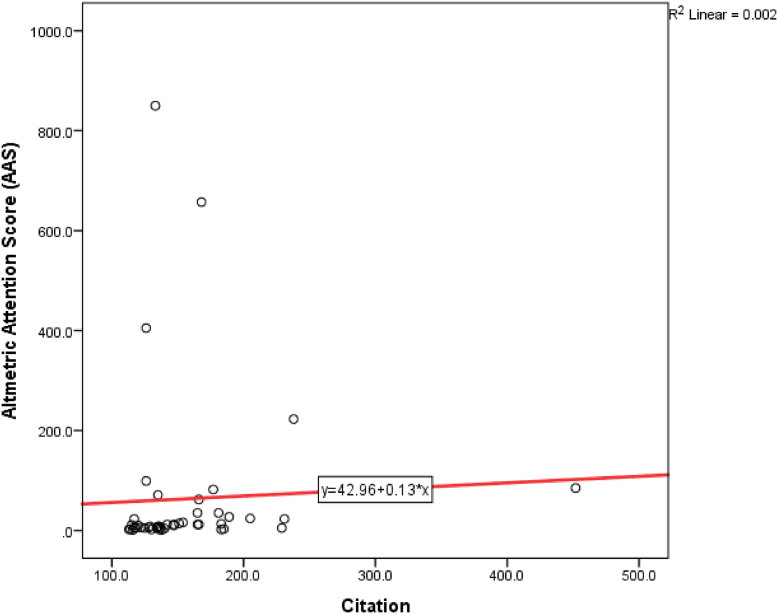
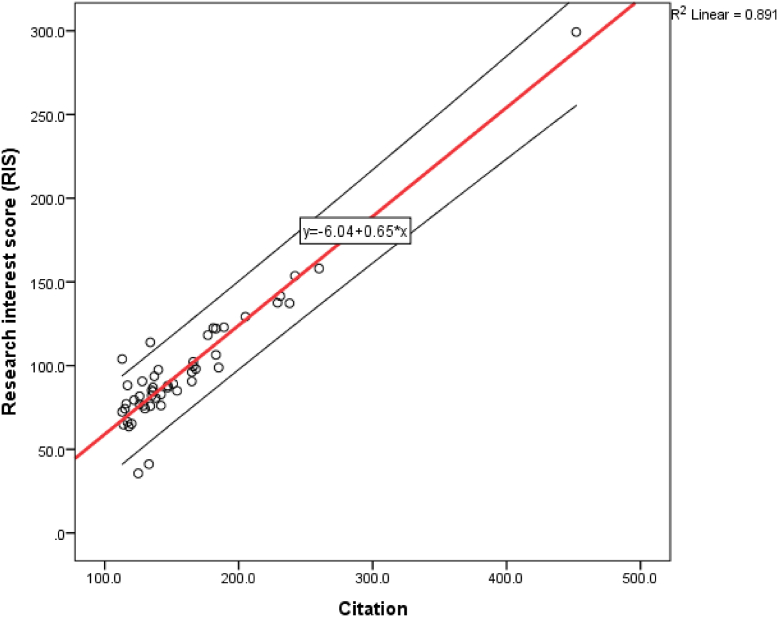
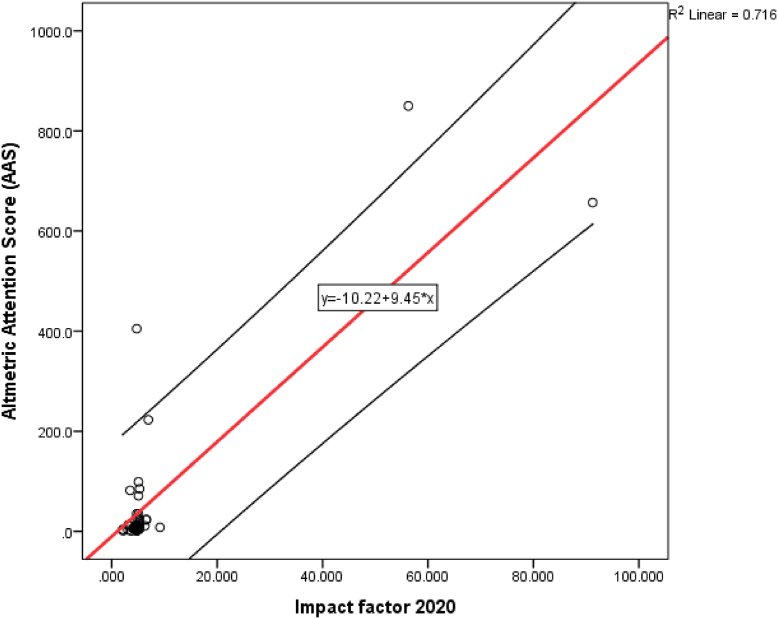
Using spearman correlation, we found a significant correlation between AAS and citation count. However, the correlation was weak (correlation coefficient = 0.379, P = .009, Fig. 2). Also, AAS had a significant correlation with Twitter (correlation coefficient = 0.601, P < .001), Facebook (correlation coefficient = 0.560, P = .004), news outlets (correlation coefficient = 0.951, P < .001), dimension (correlation coefficient = 0.381, P = .009), and blog (correlation coefficient = 0.82, P = .046) mentions. The citation count was also significantly and strongly correlated with ResearchGate interest score (correlation coefficient = 0.818, P < .001, Fig. 3), but not with the journal’s impact factor (P = .052). AAS was significantly correlated with the journal’s impact factor 2020 (correlation coefficient = 0.547, P < .001, Fig. 4). First author’s H-index was not significantly correlated with AAS or citation number (P = .66 and .44).
Figure 2.
Spearman correlation between citation count and Altmetric attention score (AAS).
Figure 3.
Spearman correlation between citation count and ResearchGate interest score (RIS).
Figure 4.
Spearman correlation between Altmetric attention score (AAS) and impact factor.
Discussion
With the popularity of social media platforms, these outlets have emerged as the primary source of news and information with arguably a larger audience than the traditional news sources. It is not surprising that researchers are also increasingly using social media to promote their research, report their findings, and collaborate with colleagues. Considering the limitations of traditional scientometric measures, alternative metrics have been introduced as complementary measures of the publication impact [66]. A growing number of researchers are cognizant of the alternative metrics, and the frequency of published articles with an Altmetric score is rapidly increasing [67]. In this study, we aimed to analyze the characteristics of the top 50 most-cited articles in the field of arthroplasty to investigate their breadth of dissemination through the traditional and alternative scientometric measures.
The top 50 most-cited studies in the arthroplasty literature have garnered a total of 7955 citations with a mean of 159.10 ± 56.4 citations per paper. At the same time, the mean AAS was 63.4 ± 164.8, and the median AAS was 10.5. Previous studies in other orthopedic specialties have found a median AAS of 4 to 235, depending on the topic and age of the publication [66,[68], [69], [70], [71]]. In line with other authors, we found a significant but weak correlation between the citation number and AAS across the included papers [[3], [67], [68], [69],[72], [73]]. Several studies have reported a weak correlation between citation count and AAS in orthopedics [68,69] and other fields [[3], [67],[72], [73]], and occasionally nonsignificant correlations [70], suggesting that Altmetrics do not represent the same measure as traditional scientometric measures. Instead, Altmetric measures could act as a complementary tool to inform the social and cultural impact of the literature.
While AAS was weakly correlated with citation count, it has moderate correlation with the journal’s impact factor (correlation coefficient = 0.547, P < .001, Fig. 4). This may stem from the reader’s tendency to share articles from the journals with a higher impact factor. Although a similar trend was found in total knee literature, a correlation between AAS and impact factor was not found in sports science and total hip arthroplasty literature [71,72,74]. High-impact journals may be more active in engaging with social media, or the quality of studies may play a role in this association. Kunze et al. found that high methodologic quality and a lower rate of bias were significant predictors of a higher AAS in the arthroplasty literature [68]. Compared with citation count, AAS is considered a quantitative variable assessing a paper’s more immediate impact attraction on readers and the intended audience [75]. However, since not every author is active on social media, more active authors will generate a higher AAS for their publications [68]. With the continued growth of the social media outreach of the scientific literature, this effect will likely be minimized in the future.
Citation count is classically delayed by 1-2 years after publication, which is not the case with Altmetric measures. Interestingly, we found that recently published papers (2017-2018) had a significantly higher AAS than papers published in 2015-2016 (149.5 ± 273.1 vs 29.5 ± 77.7, P = .030). This shows that not only the Altmetric measures do not suffer from the delay observed in traditional scientometric measures but also the authors could also be more attentive to social media recently [76].
We found that randomized controlled trials had a higher mean AAS (309.2 ± 411.3) although this did not reach statistical significance. Previous authors have also shown that prospective studies attract more interest on social media [66]. Interestingly, review articles, including meta-analyses, had the highest citation count, but not a higher AAS [77]. The Journal of Arthroplasty contributes to most of the included studies (30%), followed by The Journal of Bone and Joint Surgery (12%), Bone and Joint Journal (10%), and Clinical Orthopedics and Related Research (10%). In a scientometric study of arthroplasty researches by O’Neill et al., as high as 10.9% of all arthroplasty research articles from 2001 to 2016 was published in the Journal of Arthroplasty, similar to our study, while Clinical Orthopedics and Related Research and The Journal of Bone and Joint Surgery ranked second and third, respectively [78]. Kunze et al. analyzed the articles published between January and December 2016 in the 5 journals with the highest impact factor [68]. The mean AAS was 8.6, and the mean citation count was 15. AAS was significantly associated with citations (β = 0.16; P < .0001). They also found that publications from North America and studies concerning validity/reliability measurement gained more social media attention, as measured by AAS. They also noted that studies with more citations are more likely to be mentioned on Twitter, Facebook, and news outlets [68].
We acknowledge several limitations to our study. First, we only included articles with the term “arthroplasty” in their title, whereas it is possible that a highly cited publication did not have this term in its title. Also, we only searched through Scopus to minimize redundancies and duplicate citations, with the downside of being less comprehensive. However, we did not aim to do a systematic review. Finally, we included papers published in 2015-2019 in this study. While this may limit the traditional citation count, the alternative scientometric measures are relatively new and are not applicable to older studies. Despite these limitations, we managed to identify the most impactful articles in the field of arthroplasty. The authors suggest further studies to distinguish the most noteworthy articles in other fields of orthopedic surgery to guide future research.
Conclusions
In this study, the top 50 most-cited papers in the field of arthroplasty were identified. Traditional and alternative scientometric measures were extracted and compared between studies. We found that the AAS was highest in more recently published papers, while citation count had the opposite trend. Also, AAS was significantly correlated with the journal’s impact factor (moderate) and citation count (weak). Meta-analyses and volume projection studies garnered the most citations. Additionally, we found a weak correlation between AAS and citation count, which suggests that the alternative scientometric measures are complementary to, and not substitutes for, complement traditional measures such as citation count and impact factor.
Conflicts of interest
The authors declare that there are no conflicts of interest.
Footnotes
Ethics approval and consent to participate: This study did not review any patient data and was exempt from institutional review board approval.
Consent for publication: Not applicable.
Availability of data and materials: The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Funding: No funding was received for this study.
Appendix A. Supplementary data
References
- 1.Bornmann L., Haunschild R. Alternative article-level metrics: the use of alternative metrics in research evaluation. EMBO Rep. 2018;19(12):e47260. doi: 10.15252/embr.201847260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Butler J.S., Kaye I.D., Sebastian A.S., et al. The evolution of current research impact metrics: from bibliometrics to altmetrics? Clin Spine Surg. 2017;30(5):226. doi: 10.1097/BSD.0000000000000531. [DOI] [PubMed] [Google Scholar]
- 3.Patthi B., Prasad M., Gupta R., et al. Altmetrics–a collated adjunct beyond citations for scholarly impact: a systematic review. J Clin Diagn Res. 2017;11(6):ZE16. doi: 10.7860/JCDR/2017/26153.10078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Priem J., Groth P., Taraborelli D. The altmetrics collection. PLoS One. 2012;7(11):e48753. doi: 10.1371/journal.pone.0048753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Priem J., Taraborelli D., Groth P., Neylon C. altmetrics.org; 2011. Altmetrics: a manifesto. [Google Scholar]
- 6.Sheikhbahaei E., Mirghaderi S.P., Moharrami A., Habibi D., Motififard M., Javad Mortazavi S.M. Incidence of symptomatic COVID-19 in unvaccinated patients within one month after elective total joint arthroplasty: a multicentre study. Arthroplasty Today. 2022;14:110. doi: 10.1016/j.artd.2022.01.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sloan M., Premkumar A., Sheth N.P. Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am. 2018;100(17):1455. doi: 10.2106/JBJS.17.01617. [DOI] [PubMed] [Google Scholar]
- 8.Maradit Kremers H., Larson D.R., Crowson C.S., et al. Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am. 2015;97(17):1386. doi: 10.2106/JBJS.N.01141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marx R.G., Wilson S.M., Swiontkowski M.F. Updating the assignment of levels of evidence. J Bone Joint Surg Am. 2015;97(1):1. doi: 10.2106/JBJS.N.01112. [DOI] [PubMed] [Google Scholar]
- 10.Phillips F.M., Geisler F.H., Gilder K.M., Reah C., Howell K.M., McAfee P.C. Long-term outcomes of the US FDA IDE prospective, randomized controlled clinical trial comparing PCM cervical disc arthroplasty with anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 2015;40(10):674. doi: 10.1097/BRS.0000000000000869. [DOI] [PubMed] [Google Scholar]
- 11.Bacle G., Nové-Josserand L., Garaud P., Walch G. Long-term outcomes of reverse total shoulder arthroplasty: a follow-up of a previous study. J Bone Joint Surg Am. 2017;99(6):454. doi: 10.2106/JBJS.16.00223. [DOI] [PubMed] [Google Scholar]
- 12.Bohsali K.I., Bois A.J., Wirth M.A. Complications of shoulder arthroplasty. J Bone Joint Surg Am. 2017;99(3):256. doi: 10.2106/JBJS.16.00935. [DOI] [PubMed] [Google Scholar]
- 13.Boileau P. Complications and revision of reverse total shoulder arthroplasty. Orthop Traumatol Surg Res. 2016;102(1 Suppl):S33. doi: 10.1016/j.otsr.2015.06.031. [DOI] [PubMed] [Google Scholar]
- 14.Kiet T.K., Feeley B.T., Naimark M., et al. Outcomes after shoulder replacement: comparison between reverse and anatomic total shoulder arthroplasty. J Shoulder Elbow Surg. 2015;24(2):179. doi: 10.1016/j.jse.2014.06.039. [DOI] [PubMed] [Google Scholar]
- 15.Padegimas E.M., Maltenfort M., Lazarus M.D., Ramsey M.L., Williams G.R., Namdari S. Future patient demand for shoulder arthroplasty by younger patients: national projections. Clin Orthop Relat Res. 2015;473(6):1860. doi: 10.1007/s11999-015-4231-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tashjian R.Z., Hung M., Keener J.D., et al. Determining the minimal clinically important difference for the American Shoulder and Elbow Surgeons score, Simple Shoulder Test, and visual analog scale (VAS) measuring pain after shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26(1):144. doi: 10.1016/j.jse.2016.06.007. [DOI] [PubMed] [Google Scholar]
- 17.Patel A., Pavlou G., Mújica-Mota R.E., Toms A.D. The epidemiology of revision total knee and hip arthroplasty in England and Wales: a comparative analysis with projections for the United States. A study using the National Joint Registry dataset. Bone Joint J. 2015;97-b(8):1076. doi: 10.1302/0301-620X.97B8.35170. [DOI] [PubMed] [Google Scholar]
- 18.Lewis G.N., Rice D.A., McNair P.J., Kluger M. Predictors of persistent pain after total knee arthroplasty: a systematic review and meta-analysis. Br J Anaesth. 2015;114(4):551. doi: 10.1093/bja/aeu441. [DOI] [PubMed] [Google Scholar]
- 19.Goesling J., Moser S.E., Zaidi B., et al. Trends and predictors of opioid use after total knee and total hip arthroplasty. Pain. 2016;157(6):1259. doi: 10.1097/j.pain.0000000000000516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Inacio M.C.S., Paxton E.W., Graves S.E., Namba R.S., Nemes S. Projected increase in total knee arthroplasty in the United States - an alternative projection model. Osteoarthritis Cartilage. 2017;25(11):1797. doi: 10.1016/j.joca.2017.07.022. [DOI] [PubMed] [Google Scholar]
- 21.Bozic K.J., Kamath A.F., Ong K., et al. Comparative epidemiology of revision arthroplasty: failed THA poses greater clinical and economic burdens than failed TKA. Clin Orthop Relat Res. 2015;473(6) doi: 10.1007/s11999-014-4078-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Culliford D., Maskell J., Judge A., Cooper C., Prieto-Alhambra D., Arden N.K. Future projections of total hip and knee arthroplasty in the UK: results from the UK Clinical Practice Research Datalink. Osteoarthritis Cartilage. 2015;23(4):594. doi: 10.1016/j.joca.2014.12.022. [DOI] [PubMed] [Google Scholar]
- 23.Gunaratne R., Pratt D.N., Banda J., Fick D.P., Khan R.J.K., Robertson B.W. Patient dissatisfaction following total knee arthroplasty: a systematic review of the literature. J Arthroplasty. 2017;32(12):3854. doi: 10.1016/j.arth.2017.07.021. [DOI] [PubMed] [Google Scholar]
- 24.Iorio R., Clair A.J., Inneh I.A., Slover J.D., Bosco J.A., Zuckerman J.D. Early results of medicare's bundled payment initiative for a 90-day total joint arthroplasty episode of care. J Arthroplasty. 2016;31(2):343. doi: 10.1016/j.arth.2015.09.004. [DOI] [PubMed] [Google Scholar]
- 25.Delanois R.E., Mistry J.B., Gwam C.U., Mohamed N.S., Choksi U.S., Mont M.A. Current epidemiology of revision total knee arthroplasty in the United States. J Arthroplasty. 2017;32(9):2663. doi: 10.1016/j.arth.2017.03.066. [DOI] [PubMed] [Google Scholar]
- 26.Kunutsor S.K., Whitehouse M.R., Blom A.W., Beswick A.D. Patient-related risk factors for periprosthetic joint infection after total joint arthroplasty: a systematic review and meta-analysis. PLoS One. 2016;11(3):e0150866. doi: 10.1371/journal.pone.0150866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gwam C.U., Mistry J.B., Mohamed N.S., et al. Current epidemiology of revision total hip arthroplasty in the United States: national inpatient sample 2009 to 2013. J Arthroplasty. 2017;32(7):2088. doi: 10.1016/j.arth.2017.02.046. [DOI] [PubMed] [Google Scholar]
- 28.Arabnejad S., Johnston B., Tanzer M., Pasini D. Fully porous 3D printed titanium femoral stem to reduce stress-shielding following total hip arthroplasty. J Orthop Res. 2017;35(8):1774. doi: 10.1002/jor.23445. [DOI] [PubMed] [Google Scholar]
- 29.Anderson D.R., Dunbar M., Murnaghan J., et al. Aspirin or rivaroxaban for VTE prophylaxis after hip or knee arthroplasty. N Engl J Med. 2018;378(8):699. doi: 10.1056/NEJMoa1712746. [DOI] [PubMed] [Google Scholar]
- 30.Choi Y.-J., Ra H.J. Patient satisfaction after total knee arthroplasty. Knee Surg Relat Res. 2016;28(1):1. doi: 10.5792/ksrr.2016.28.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Higgins B.T., Barlow D.R., Heagerty N.E., Lin T.J. Anterior vs. posterior approach for total hip arthroplasty, a systematic review and meta-analysis. J Arthroplasty. 2015;30(3):419. doi: 10.1016/j.arth.2014.10.020. [DOI] [PubMed] [Google Scholar]
- 32.Liddle A.D., Pandit H., Judge A., Murray D.W. Patient-reported outcomes after total and unicompartmental knee arthroplasty: a study of 14,076 matched patients from the National Joint Registry for England and Wales. Bone Joint J. 2015;97-b(6):793. doi: 10.1302/0301-620X.97B6.35155. [DOI] [PubMed] [Google Scholar]
- 33.Losina E., Paltiel A.D., Weinstein A.M., et al. Lifetime medical costs of knee osteoarthritis management in the United States: impact of extending indications for total knee arthroplasty. Arthritis Care Res (Hoboken) 2015;67(2):203. doi: 10.1002/acr.22412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pandit H., Hamilton T.W., Jenkins C., Mellon S.J., Dodd C.A., Murray D.W. The clinical outcome of minimally invasive Phase 3 Oxford unicompartmental knee arthroplasty: a 15-year follow-up of 1000 UKAs. Bone Joint J. 2015;97-b(11):1493. doi: 10.1302/0301-620X.97B11.35634. [DOI] [PubMed] [Google Scholar]
- 35.de Steiger R.N., Liu Y.L., Graves S.E. Computer navigation for total knee arthroplasty reduces revision rate for patients less than sixty-five years of age. J Bone Joint Surg Am. 2015;97(8):635. doi: 10.2106/JBJS.M.01496. [DOI] [PubMed] [Google Scholar]
- 36.Burns L.C., Ritvo S.E., Ferguson M.K., Clarke H., Seltzer Z., Katz J. Pain catastrophizing as a risk factor for chronic pain after total knee arthroplasty: a systematic review. J Pain Res. 2015;8:21. doi: 10.2147/JPR.S64730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Thiele K., Perka C., Matziolis G., Mayr H.O., Sostheim M., Hube R. Current failure mechanisms after knee arthroplasty have changed: polyethylene wear is less common in revision surgery. J Bone Joint Surg Am. 2015;97(9):715. doi: 10.2106/JBJS.M.01534. [DOI] [PubMed] [Google Scholar]
- 38.Keswani A., Tasi M.C., Fields A., Lovy A.J., Moucha C.S., Bozic K.J. Discharge destination after total joint arthroplasty: an analysis of postdischarge outcomes, placement risk factors, and recent trends. J Arthroplasty. 2016;31(6):1155. doi: 10.1016/j.arth.2015.11.044. [DOI] [PubMed] [Google Scholar]
- 39.Kamath A.F., Ong K.L., Lau E., et al. Quantifying the burden of revision total joint arthroplasty for periprosthetic infection. J Arthroplasty. 2015;30(9):1492. doi: 10.1016/j.arth.2015.03.035. [DOI] [PubMed] [Google Scholar]
- 40.Petis S., Howard J.L., Lanting B.L., Vasarhelyi E.M. Surgical approach in primary total hip arthroplasty: anatomy, technique and clinical outcomes. Can J Surg. 2015;58(2):128. doi: 10.1503/cjs.007214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bohl D.D., Shen M.R., Kayupov E., Della Valle C.J. Hypoalbuminemia independently predicts surgical site infection, pneumonia, length of stay, and readmission after total joint arthroplasty. J Arthroplasty. 2016;31(1):15. doi: 10.1016/j.arth.2015.08.028. [DOI] [PubMed] [Google Scholar]
- 42.Jacofsky D.J., Allen M. Robotics in arthroplasty: a comprehensive review. J Arthroplasty. 2016;31(10):2353. doi: 10.1016/j.arth.2016.05.026. [DOI] [PubMed] [Google Scholar]
- 43.de Steiger R.N., Lorimer M., Solomon M. What is the learning curve for the anterior approach for total hip arthroplasty? Clin Orthop Relat Res. 2015;473(12):3860. doi: 10.1007/s11999-015-4565-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Marra M.A., Vanheule V., Fluit R., et al. A subject-specific musculoskeletal modeling framework to predict in vivo mechanics of total knee arthroplasty. J Biomech Eng. 2015;137(2):020904. doi: 10.1115/1.4029258. [DOI] [PubMed] [Google Scholar]
- 45.Soffin E.M., YaDeau J.T. Enhanced recovery after surgery for primary hip and knee arthroplasty: a review of the evidence. Br J Anaesth. 2016;117(suppl 3):iii62. doi: 10.1093/bja/aew362. [DOI] [PubMed] [Google Scholar]
- 46.Khan M., Osman K., Green G., Haddad F.S. The epidemiology of failure in total knee arthroplasty: avoiding your next revision. Bone Joint J. 2016;98-b(1 Suppl A):105. doi: 10.1302/0301-620X.98B1.36293. [DOI] [PubMed] [Google Scholar]
- 47.Bell S.W., Anthony I., Jones B., MacLean A., Rowe P., Blyth M. Improved accuracy of component positioning with robotic-assisted unicompartmental knee arthroplasty: data from a prospective, randomized controlled study. J Bone Joint Surg Am. 2016;98(8):627. doi: 10.2106/JBJS.15.00664. [DOI] [PubMed] [Google Scholar]
- 48.Sassoon A., Nam D., Nunley R., Barrack R. Systematic review of patient-specific instrumentation in total knee arthroplasty: new but not improved. Clin Orthop Relat Res. 2015;473(1):151. doi: 10.1007/s11999-014-3804-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gage B.F., Bass A.R., Lin H., et al. Effect of genotype-guided warfarin dosing on clinical events and anticoagulation control among patients undergoing hip or knee arthroplasty: the GIFT randomized clinical trial. JAMA. 2017;318(12):1115. doi: 10.1001/jama.2017.11469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Esposito C.I., Gladnick B.P., Lee Y.Y., et al. Cup position alone does not predict risk of dislocation after hip arthroplasty. J Arthroplasty. 2015;30(1):109. doi: 10.1016/j.arth.2014.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nguyen L.C., Sing D.C., Bozic K.J. Preoperative reduction of opioid use before total joint arthroplasty. J Arthroplasty. 2016;31(9 Suppl):282. doi: 10.1016/j.arth.2016.01.068. [DOI] [PubMed] [Google Scholar]
- 52.Siddiqi A., White P.B., Mistry J.B., et al. Effect of bundled payments and health care reform as alternative payment models in total joint arthroplasty: a clinical review. J Arthroplasty. 2017;32(8):2590. doi: 10.1016/j.arth.2017.03.027. [DOI] [PubMed] [Google Scholar]
- 53.Buckland A.J., Puvanesarajah V., Vigdorchik J., et al. Dislocation of a primary total hip arthroplasty is more common in patients with a lumbar spinal fusion. Bone Joint J. 2017;99-b(5):585. doi: 10.1302/0301-620X.99B5.BJJ-2016-0657.R1. [DOI] [PubMed] [Google Scholar]
- 54.Stambough J.B., Nunley R.M., Curry M.C., Steger-May K., Clohisy J.C. Rapid recovery protocols for primary total hip arthroplasty can safely reduce length of stay without increasing readmissions. J Arthroplasty. 2015;30(4):521. doi: 10.1016/j.arth.2015.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bedard N.A., Pugely A.J., Westermann R.W., Duchman K.R., Glass N.A., Callaghan J.J. Opioid use after total knee arthroplasty: trends and risk factors for prolonged use. J Arthroplasty. 2017;32(8):2390. doi: 10.1016/j.arth.2017.03.014. [DOI] [PubMed] [Google Scholar]
- 56.Lyman S., Lee Y.Y., Franklin P.D., Li W., Cross M.B., Padgett D.E. Validation of the KOOS, JR: a short-form knee arthroplasty outcomes survey. Clin Orthop Relat Res. 2016;474(6):1461. doi: 10.1007/s11999-016-4719-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Maratt J.D., Esposito C.I., McLawhorn A.S., Jerabek S.A., Padgett D.E., Mayman D.J. Pelvic tilt in patients undergoing total hip arthroplasty: when does it matter? J Arthroplasty. 2015;30(3):387. doi: 10.1016/j.arth.2014.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Basques B.A., Toy J.O., Bohl D.D., Golinvaux N.S., Grauer J.N. General compared with spinal anesthesia for total hip arthroplasty. J Bone Joint Surg Am. 2015;97(6):455. doi: 10.2106/JBJS.N.00662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Maoz G., Phillips M., Bosco J., et al. The Otto Aufranc Award: modifiable versus nonmodifiable risk factors for infection after hip arthroplasty. Clin Orthop Relat Res. 2015;473(2):453. doi: 10.1007/s11999-014-3780-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Moffet H., Tousignant M., Nadeau S., et al. In-home telerehabilitation compared with face-to-face rehabilitation after total knee arthroplasty: a noninferiority randomized controlled trial. J Bone Joint Surg Am. 2015;97(14):1129. doi: 10.2106/JBJS.N.01066. [DOI] [PubMed] [Google Scholar]
- 61.Rolfson O., Bohm E., Franklin P., et al. Patient-reported outcome measures in arthroplasty registries report of the patient-reported outcome measures working group of the international society of arthroplasty registries Part II. Recommendations for selection, administration, and analysis. Acta Orthop. 2016;87 Suppl 1(Suppl 1):9. doi: 10.1080/17453674.2016.1181816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Grevstad U., Mathiesen O., Valentiner L.S., Jaeger P., Hilsted K.L., Dahl J.B. Effect of adductor canal block versus femoral nerve block on quadriceps strength, mobilization, and pain after total knee arthroplasty: a randomized, blinded study. Reg Anesth Pain Med. 2015;40(1):3. doi: 10.1097/AAP.0000000000000169. [DOI] [PubMed] [Google Scholar]
- 63.Howell S.M., Papadopoulos S., Kuznik K., Ghaly L.R., Hull M.L. Does varus alignment adversely affect implant survival and function six years after kinematically aligned total knee arthroplasty? Int Orthop. 2015;39(11):2117. doi: 10.1007/s00264-015-2743-5. [DOI] [PubMed] [Google Scholar]
- 64.Rivière C., Iranpour F., Auvinet E., et al. Alignment options for total knee arthroplasty: a systematic review. Orthop Traumatol Surg Res. 2017;103(7):1047. doi: 10.1016/j.otsr.2017.07.010. [DOI] [PubMed] [Google Scholar]
- 65.Lee W.C., Kwan Y.H., Chong H.C., Yeo S.J. The minimal clinically important difference for Knee Society Clinical Rating System after total knee arthroplasty for primary osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2017;25(11):3354. doi: 10.1007/s00167-016-4208-9. [DOI] [PubMed] [Google Scholar]
- 66.Parrish J.M., Jenkins N.W., Brundage T.S., Hrynewycz N.M., Singh K. The top 100 spine surgery articles on social media: an altmetric study. Spine (Phila Pa 1976) 2020;45(17):1229. doi: 10.1097/BRS.0000000000003508. [DOI] [PubMed] [Google Scholar]
- 67.Costas R., Zahedi Z., Wouters P. Do “altmetrics” correlate with citations? Extensive comparison of altmetric indicators with citations from a multidisciplinary perspective. J Assoc Inf Sci Technol. 2015;66(10):2003. [Google Scholar]
- 68.Kunze K.N., Polce E.M., Vadhera A., et al. What is the predictive ability and academic impact of the altmetrics score and social media attention? Am J Sports Med. 2020;48(5):1056. doi: 10.1177/0363546520903703. [DOI] [PubMed] [Google Scholar]
- 69.Yoshimura R., Grant M.C., Gardiner M.D., Wade R.G. Disseminating hand surgery research using social media: the relationship between altmetrics and citations. J Hand Surg Am. 2021;46(9):740. doi: 10.1016/j.jhsa.2021.03.028. [DOI] [PubMed] [Google Scholar]
- 70.Levy K.H., Huddleston H., Kurtzman J.S., Aibinder W.R., Koehler S.M. The 50 most cited papers in chronic scapholunate reconstruction: a bibliometric analysis. Eur J Orthop Surg Traumatol. 2021;31(6):995. doi: 10.1007/s00590-020-02864-3. [DOI] [PubMed] [Google Scholar]
- 71.Ramamurti P., Gu A., Fassihi S.C., et al. Correlation between altmetric score and traditional bibliometrics in total joint arthroplasty research. Arthroplasty Today. 2021;7:225. doi: 10.1016/j.artd.2020.12.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nocera A.P., Boyd C.J., Boudreau H., Hakim O., Rais-Bahrami S. Examining the correlation between altmetric score and citations in the urology literature. Urology. 2019;134:45. doi: 10.1016/j.urology.2019.09.014. [DOI] [PubMed] [Google Scholar]
- 73.Chang J., Desai N., Gosain A. Correlation between altmetric score and citations in pediatric surgery core journals. J Surg Res. 2019;243:52. doi: 10.1016/j.jss.2019.05.010. [DOI] [PubMed] [Google Scholar]
- 74.de Oliveira Silva D., Taborda B., Pazzinatto M.F., Ardern C., Barton C.J. Altmetric score has a stronger relationship with article citations than journal impact factor and open access status: a cross-sectional analysis of 4,022 sports science articles. J Orthop Sports Phys Ther. 2021;51(11):536. doi: 10.2519/jospt.2021.10598. [DOI] [PubMed] [Google Scholar]
- 75.Baheti A., Bhargava P. Altmetrics: a measure of social attention toward scientific research. Curr Probl Diagn Radiol. 2017;46:391. doi: 10.1067/j.cpradiol.2017.06.005. [DOI] [PubMed] [Google Scholar]
- 76.Finch T., O'Hanlon N., Dudley S.P. Tweeting birds: online mentions predict future citations in ornithology. R Soc Open Sci. 2017;4(11):171371. doi: 10.1098/rsos.171371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zhang S., Fan H., Zhang Y. The 100 top-cited studies on dyslexia research: a bibliometric analysis. Front Psychiatry. 2021;12:714627. doi: 10.3389/fpsyt.2021.714627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.O'Neill C.J., Cassar-Gheiti A.J., Harty J.A. Arthroplasty and global research output: a bibliometric analysis. J Orthop. 2020;17:187. doi: 10.1016/j.jor.2019.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.