Abstract
Introduction:
Many adult smokers have tried electronic cigarettes (e-cigarettes) as a less harmful alternative to combustible cigarettes. There is limited evidence, however, for the extent to which switching to e-cigarettes is associated with better health and functioning among nicotine users approaching their 40s—the beginning of midlife—when many health issues become more evident. This study examined the adoption of e-cigarette use (“vaping”) among smokers in their 30s, and its association with diverse measures of healthy and successful aging at age 39.
Methods:
Data were from the Seattle Social Development Project, a panel study of 808 diverse participants with high retention (88%−91%). A subsample of 156 who used combustible cigarettes (smoked) at age 30 and smoked or vaped at age 39 was selected for analysis. A measure of vaping frequency, relative to combustible cigarette use, was computed from self-reports of past-month vaping and smoking at age 39. Nine measures of health and functioning in the past year were computed at age 39, with nine corresponding measures at age 30.
Results:
Among smokers at age 30, 36% adopted vaping some or all of the time by age 39. Higher relative vaping frequency was related to 4 of 9 outcomes examined, including significantly more exercise, more constructive engagement, better physical health, and higher SES at age 39, accounting for prior behaviors at age 30.
Conclusions:
Findings suggest that, among smokers in their 30s, replacing combustible cigarettes with vaping may be associated with key markers of healthy and successful aging to age 39.
Keywords: Electronic cigarettes, Smoking, Health consequences, Adult functioning, Aging, Midlife
1. Introduction
Electronic cigarettes (e-cigarettes) entered the market in the United States in 2007, and by 2018 approximately 10% of adult combustible cigarette smokers used e-cigarettes and 6% had made a full switch from combustible cigarettes to e-cigarettes (Bao et al., 2020). E-cigarettes typically produce a nicotine-containing aerosol that is inhaled by the user, also known as “vaping” (we use “smoking” to refer only to combustible cigarette use). There is ongoing debate about the harms and benefits of e-cigarettes for public health. Although e-cigarettes contain a number of hazardous substances and there is substantial evidence that they increase risk of smoking initiation among youth and young adults, e-cigarettes are less harmful to the user than combustible cigarettes (National Academies of Sciences, 2018).
Studies on effects of vaping in adults have focused mainly on physical health (e.g., cardiovascular risk, respiratory function), mental health (e.g., depression), and behavioral health (e.g., exercise, alcohol use) (Gotts et al., 2019; National Academies of Sciences, 2018; Pokhrel et al., 2020; Saeed et al., 2020; Wang, 2020). No e-cigarette studies to our knowledge have broadly examined adult wellbeing and functioning. An important question is the extent to which adult smokers might turn to e-cigarettes as a healthier form of nicotine use, and if there is evidence for better overall health and functioning as they approach their 40s, the beginning of midlife (Kanesarajah et al., 2018).
To examine this question, we drew on broad assessments of healthy and successful aging (Lu et al., 2019; Michel and Sadana, 2017) that include mental and physical health, as well as health-promoting behaviors, engaging in social and productive activities, and attaining higher education or income. These different domains are important because they can often interact to play a significant role in overall health and wellbeing beyond more narrow assessments (Kanesarajah et al., 2018; Mejía et al., 2017). Because of reduced stigma, odor, and physical harm, it is possible that vaping—relative to smoking—could increase opportunities (or reduce barriers) for health-promoting activities and adult health and wellbeing (Fairchild et al., 2014; Sweanor et al., 2007). For example, vaping (vs. smoking) may make it easier to exercise or to be in settings that encourage exercise, or to have nonsmoking peers and partners, potentially reducing opportunities for other substance use. Vaping may also enable more interaction with nonsmoking coworkers and community members, and may increase other opportunities that can lead to improved socioeconomic status (SES) (Kosterman et al., 2021). Alternatively, it is also possible that nicotine users with better health and functioning to begin with are more likely to adopt vaping as a healthier choice for nicotine intake. Whether health and wellbeing influence vaping choice or vice versa (or reciprocal influence), evidence for either association would suggest an important role for vaping in healthy aging among nicotine users.
We used prospective longitudinal data to examine those who were smokers at age 30 (in 2005, prior to e-cigarette availability), and the extent to which they adopted e-cigarette use as a proportion of their total smoking and vaping at age 39. We then modeled changes in a set of physical and mental health and adult functioning measures from ages 30 to 39, and tested the degree to which participants’ level of vaping at age 39, compared to smoking, was associated with those changes. We hypothesized that more vaping, relative to smoking, would be associated with more improvement (or less decline) in health behaviors, functioning, health outcomes, and success across the 30s. Given limited research on vaping among adults beyond their 20s, findings may add to understanding of vaping’s role in healthy aging among those who use nicotine.
2. Materials and methods
2.1. Sample
Data were from the Seattle Social Development Project (SSDP), a longitudinal panel study established in 1985 from a population of all students (N = 1053) entering Grade 5 in 18 Seattle public schools serving higher crime neighborhoods. Of these students, 808 (77%) youth and their parents consented to participate in the longitudinal study. Analyses reported here were based on two survey waves conducted at ages 30 and 39 (in 2005 and 2014); retention of still-living participants from the original panel was 91% (N = 719) and 88% (N = 677), respectively (37 participants were deceased by age 39). Analyses examined those who reported smoking at age 30 and smoking or vaping at age 39 (N = 156). This sample was 54% male; 49% were European American, 26% African American, 15% Asian American, and 11% Native American—across race, 6% were of Hispanic ethnicity. The study was approved by the Human Subjects Review Committee at the University of Washington and participants provided informed consent.
2.2. Measures
Combustible cigarette use
Combustible cigarette use at ages 30 and 39 was assessed with, “How many times have you smoked cigarettes in the past month?” coded 0 (“not at all”) to 1 for a pack (20 cigarettes) a day or more; responses between 0 and 1 were coded proportionally (e.g., half a pack coded to .5) (all measures were coded to a 0–1 scale to use a consistent metric). E-cigarette use at age 39 was assessed with, “How many times in the past month have you used smokeless or electronic cigarettes (‘e-cigarettes,’ ‘vaping,’ or ‘ENDS’)?” Numeric responses were recoded to 0 to 1, with 1 indicating 30 or more times (95% reported 30 or fewer times; e-cigarette assessments were not available prior to age 39).
Relative vaping frequency
Relative vaping frequency at age 39 was computed as vaping frequency divided by the total of vaping plus smoking in the past month. Because smoking and vaping were each coded to a 0 to 1 scale with 1 equivalent to a daily vaper or pack-a-day smoker, the resulting continuous measure represents the relative vaping frequency such that 0 indicates smoking only with no vaping, 1 indicates vaping only with no smoking, and scores between 0 and 1 indicate the relative level of e-cigarette use (e.g., .5 indicates one occasion of vaping for every cigarette pack smoked).
Adult health and functioning
Adult health and functioning in the past year at age 39, along with corresponding measures at age 30, was assessed with nine continuous scales adapted from Kosterman et al. (2019). To aid in interpretation, each scale was coded to 0 to 1 with 1 indicating the healthiest or most positive outcome. Measures included: exercise (minutes, frequency and intensity of weekly exercise where 0 is no exercise and 1 is meeting CDC activity guidelines; U.S. Department of Health and Human Services, 2008); fewer alcohol problems and fewer drug problems (for each, reverse-coded count of DSM disorder symptoms where 0 is meeting disorder criteria and 1 is no symptoms; American Psychiatric Association, 2013); constructive engagement (sum of typical time spent at work, school, and homemaking where 0 is none and 1 is full-time equivalent); civic engagement (sum of activities where 0 is none and 1 is participation in voting, volunteering, community involvement, and advocacy); nonsmoking partner and peers (where 0 is partner and three closest peers all smoke cigarettes and 1 is none smoke); mental health (reverse-coded count of major depression and generalized anxiety DSM disorder symptoms where 0 is meeting disorder criteria for both and 1 is no symptoms; American Psychiatric Association, 2013); physical health (where 0 is self-report of poor or “worst possible” and 1 is excellent or “best possible” physical health); and socioeconomic status (where 0 is at or below U.S. median education and household income and 1 is above median for both). Additional covariates included gender, ethnicity, and years of education, as well as smoking quantity at age 30.
2.3. Analyses
Model analyses used Mplus 8.4 with full-information maximum likelihood missing data estimation (Muthén and Muthén, 1998–2017). Standardized coefficients and two-tailed tests of significance are presented. As in prior SSDP analyses (Kosterman et al., 2021), because part of the sample had been assigned to a preventive intervention in the elementary grades, we examined covariance equivalence across intervention and control groups among variables in tested models. Differences in just two relationships were observed (stronger association of vaping with fewer alcohol problems, and higher stability in physical health among full-intervention participants), which did not substantively change the pattern or interpretation of full-sample results that are presented.
3. Results
A total of 253 participants were smokers at age 30 (M = .29 packs per day), 156 of whom reported smoking and/or vaping in the past month at age 39 and constitute the analysis sample. Of these, 64% only smoked at age 39 (M = .46 packs per day), 8% only vaped (M = .36 times per day), and 28% were dual users (M = .50 packs and M = .38 times vaping per day).
To examine the association of vaping with changes in health and functioning from ages 30 to 39, we tested separate models for each health/functioning measure corresponding to the pathways illustrated in Figure 1. Results in Table 1, C paths, indicate that higher vaping frequency, relative to smoking, was associated with significantly more exercise, more constructive engagement, better self-reported physical health, and higher SES at age 39, as well as a marginal association with more civic engagement. No significant associations were found for alcohol or other drug problems, nonsmoking partner and peers, or mental health. These findings accounted for significant stability in the respective health and functioning measures (A paths); the association of prior health and functioning with relative vaping frequency (B paths); as well as gender, ethnicity, education, and prior smoking.
Figure 1.
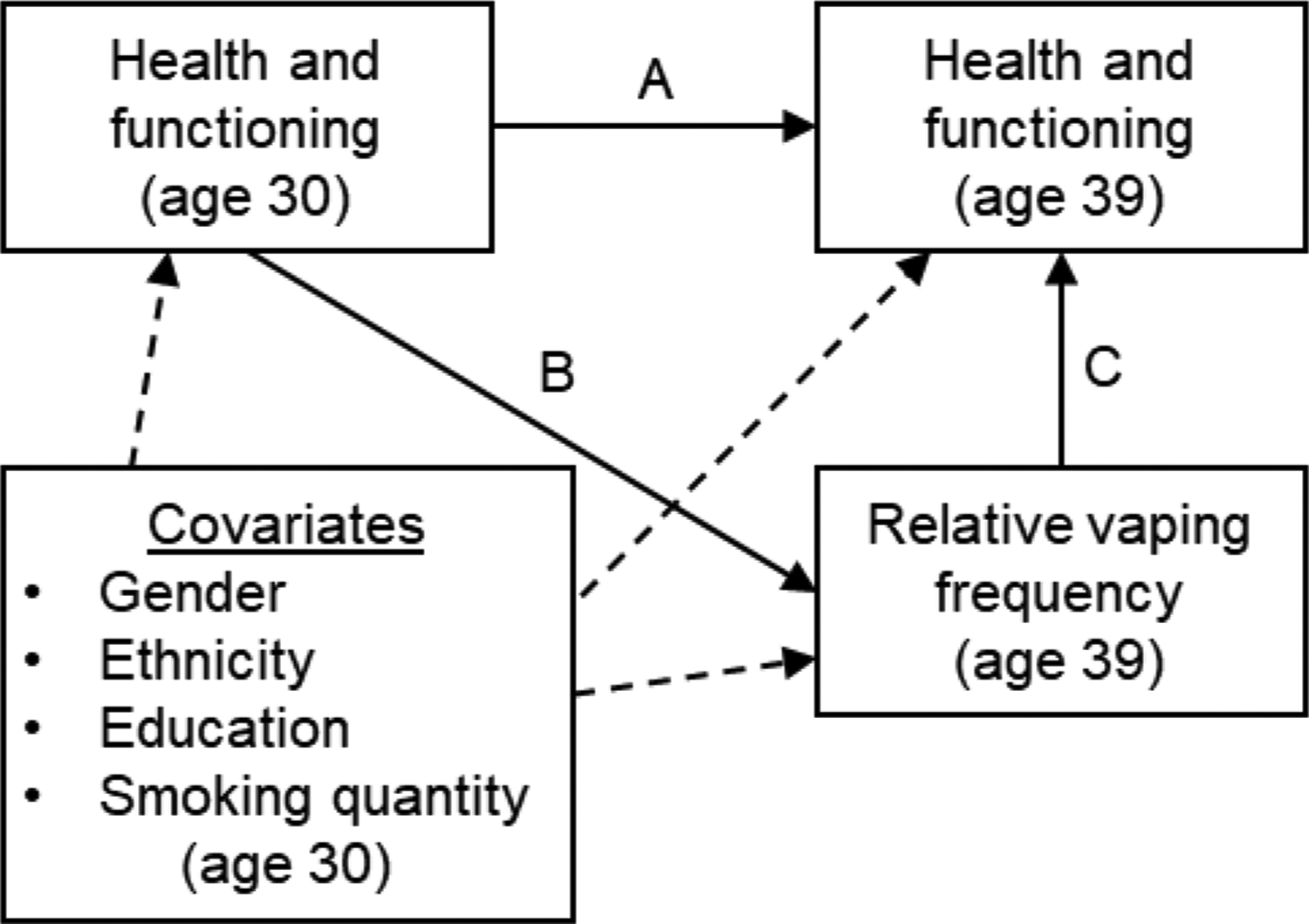
Illustration of path model used to examine the association of relative frequency of vaping with changes in health and functioning from ages 30 to 39. Paths A, B, and C correspond to columns in Table 1.
Table 1.
Association of Relative Frequency of Vaping With Health and Functioning at Age 39
| Model pathways | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Health/func. age 30 → Health/func. age 39 (A paths) |
Health/func. age 30 → Relative vaping freq. (B paths) |
Relative vaping freq. → Health/func. age 39 (C paths) |
|||||||
| Health and functioning measures | β | (SE) | p | β | (SE) | p | β | (SE) | p |
| Health behavior | |||||||||
| Exercise | .33*** | (.09) | <.001 | −.06 | (.08) | .501 | .18* | (.09) | .036 |
| Fewer alcohol problems | .37*** | (.08) | <.001 | .03 | (.08) | .681 | −.08 | (.08) | .361 |
| Fewer drug problems | .33*** | (.09) | <.001 | .06 | (.08) | .419 | .05 | (.05) | .365 |
| Adult functioning | |||||||||
| Constructive engagement | .24* | (.10) | .016 | .03 | (.06) | .674 | .13** | (.05) | .009 |
| Civic engagement | .27*** | (.07) | <.001 | .05 | (.08) | .556 | .15+ | (.08) | .067 |
| Nonsmoking partner and peers | .36*** | (.08) | <.001 | .03 | (.08) | .702 | .02 | (.08) | .820 |
| Adult health and success | |||||||||
| Mental health | .35*** | (.08) | <.001 | −.10 | (.08) | .199 | .07 | (.07) | .371 |
| Physical health | .34*** | (.08) | <.001 | −.16* | (.06) | .011 | .18* | (.07) | .013 |
| Socioeconomic status | .61*** | (.04) | <.001 | .25** | (.08) | .001 | .16** | (.06) | .007 |
Notes. Path coefficients are standardized betas (standard errors in parentheses). Health and functioning measures were labeled and coded such that higher scores indicated better health or functioning. Paths A, B, and C correspond to pathways in Figure 1. func. = functioning; freq. = frequency.
p < .10,
p < .05,
p < .01,
p < .001.
4. Discussion
Most smokers at age 30 who continued to use nicotine used only combustible cigarettes at age 39, although over one third (36%) used e-cigarettes some or all of the time. We found that a higher frequency of vaping, relative to one’s level of smoking, was associated with significantly better health and functioning in 4 out of 9 indicators examined at age 39 accounting for changes from age 30. Vaping, relative to smoking, may particularly facilitate active social engagements that would explain higher levels of constructive and civic engagement, exercise and, ultimately, better physical health and SES. Whereas more sedentary (substance use), domestic (partner smoking status), or individual (mental health) domains were not associated with vaping. Notably, there was little relationship of prior health and functioning with adoption of e-cigarette use, with the exception of physical health and SES. One unexpected finding was that better physical health at age 30 was associated with less relative vaping frequency at age 39 (β = −.16, r = −.14). It is possible that those who reported their prior health as poor were more motivated to try a safer mode of nicotine intake as they approached midlife.
Limitations of this study include a community sample, originating from Seattle, potentially narrowing its generalizability. By age 39, however, participants had dispersed across diverse communities throughout the U.S., with only 30% remaining in Seattle. Another caveat is that the data pre-date the introduction of JUUL and some other major e-cigarette manufacturers and may not reflect the most recent technology (Huang et al., 2019; National Academies of Sciences, 2018). Also, vaping was assessed concurrently with health and functioning at age 39. It is possible that better health and functioning promoted more vaping rather than the reverse. Such an interpretation would remain an important finding, however, consistent with a significant role for vaping in healthy aging among nicotine users. Further, this report did not examine those who quit nicotine use entirely; future research may want to compare the health and functioning of vapers with quitters.
The study also had important strengths, including a prospective longitudinal design spanning 9 years of adulthood, and the ability to account for parallel measures of each outcome and other key covariates prior to e-cigarette availability. Diverse indicators of healthy and successful aging were examined, which is necessary for a comprehensive understanding of health and wellbeing (Lu et al., 2019; Michel and Sadana, 2017). The age of the study cohort was particularly well suited to this analysis, being old enough to witness the introduction of e-cigarettes in their 30s—as existing smokers—yet likely young enough to remain amenable to adopting a new technology (Vogels, 2019). They may have also been at an advantageous age to recognize growing health risks with continued smoking as they approached midlife, and to understand that e-cigarettes are a less harmful alternative (Bao et al., 2020; Viscusi, 2016).
This study is among the first to investigate the adoption of e-cigarette use among smokers in their 30s and its association with diverse indicators of adult health and functioning. Findings suggest that smokers who opt to vape may not only reduce their intake of toxins and carcinogens, but may also improve or reinforce opportunities for healthy activities and engagement, and for better physical health and success in adulthood.
Highlights.
Over one third of smokers in their 30s took up vaping after e-cigarettes became available.
Vaping, relative to combustible smoking, was associated with better health and wellbeing.
Smokers who opt to vape may have more opportunities for healthy engagement.
These opportunities can promote healthier aging among nicotine users approaching midlife.
Acknowledgments
We thank our funders, the study participants, and the staff of the Social Development Research Group who contributed to data collection and administration of the project.
Role of Funding Source
This work was supported by the National Cancer Institute (NCI; grant number R37CA225690 to M.E.), the National Institute on Aging (NIA; grant number R01AG069024 to M.E.), and the National Institute on Drug Abuse (NIDA; grant numbers R01DA033956 to R.K., and R01DA009679 to J.D.H.). Content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies. NCI and NIDA played no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; nor in the decision to submit the article for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
No conflict declared.
References
- American Psychiatric Association, 2013. Diagnostic and statistical manual of mental disorders, 5th ed. Author, Arlington, VA. [Google Scholar]
- Bao W, Liu B, Du Y, Snetselaar LG, Wallace RB, 2020. Electronic cigarette use among young, middle-aged, and older adults in the United States in 2017 and 2018. JAMA Intern Med 180(2), 313–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairchild AL, Bayer R, Colgrove J, 2014. The renormalization of smoking? E-cigarettes and the tobacco “endgame”. N Engl J Med 370(4), 293–295. [DOI] [PubMed] [Google Scholar]
- Gotts JE, Jordt S-E, McConnell R, Tarran R, 2019. What are the respiratory effects of e-cigarettes? BMJ 366, l5275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang J, Duan Z, Kwok J, Binns S, Vera LE, Kim Y, Szczypka G, Emery SL, 2019. Vaping versus JUULing: How the extraordinary growth and marketing of JUUL transformed the US retail e-cigarette market. Tob Control 28(2), 146–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanesarajah J, Waller M, Whitty JA, Mishra GD, 2018. Multimorbidity and quality of life at mid-life: A systematic review of general population studies. Maturitas 109, 53–62. [DOI] [PubMed] [Google Scholar]
- Kosterman R, Epstein M, Bailey JA, Oesterle S, Furlong M, Hawkins JD, 2021. Adult social environments and the use of combustible and electronic cigarettes: Opportunities for reducing smoking in the 30s. Nicotine Tob Res 23(3), 518–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosterman R, Hawkins JD, Hill KG, Bailey JA, Catalano RF, Abbott RD, 2019. Effects of social development intervention in childhood on adult life at ages 30 to 39. Prevention Science 20(7), 986–995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu W, Pikhart H, Sacker A, 2019. Domains and measurements of healthy aging in epidemiological studies: A review. Gerontologist 59(4), e294–e310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mejía ST, Ryan LH, Gonzalez R, Smith J, 2017. Successful aging as the intersection of individual resources, age, environment, and experiences of well-being in daily activities. The Journals of Gerontology: Series B 72(2), 279–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michel J-P, Sadana R, 2017. “Healthy aging” concepts and measures. Journal of the American Medical Directors Association 18(6), 460–464. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO, 1998–2017. Mplus user’s guide, 8th ed. Muthén & Muthén, Los Angeles, CA. [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine, 2018. Public health consequences of e-cigarettes. The National Academies Press, Washington, DC. [PubMed] [Google Scholar]
- Pokhrel P, Schmid S, Pagano I, 2020. Physical activity and use of cigarettes and e-cigarettes among young adults. Am J Prev Med 58(4), 580–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saeed OB, Chavan B, Haile ZT, 2020. Association between e-cigarette use and depression in US adults. J Addict Med 14(5), 393–400. [DOI] [PubMed] [Google Scholar]
- Sweanor D, Alcabes P, Drucker E, 2007. Tobacco harm reduction: How rational public policy could transform a pandemic. Int J Drug Policy 18(2), 70–74. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, 2008. 2008 physical activity guidelines for Americans. https://health.gov/paguidelines/pdf/paguide.pdf.
- Viscusi WK, 2016. Risk beliefs and preferences for e-cigarettes. Am J Health Econ 2(2), 213–240. [Google Scholar]
- Vogels EA, 2019. Millennials stand out for their technology use, but older generations also embrace digital life. https://www.pewresearch.org/fact-tank/2019/09/09/us-generations-technology-use/. (Accessed July 27, 2021.
- Wang Q, 2020. High-intensity binge drinking is associated with cigarette smoking and e-cigarette use among US adults aged 40–64 years: Findings from the 2017 BRFSS survey. Tob Induc Dis 18(54), 54. [DOI] [PMC free article] [PubMed] [Google Scholar]


