Abstract
Background & Aims
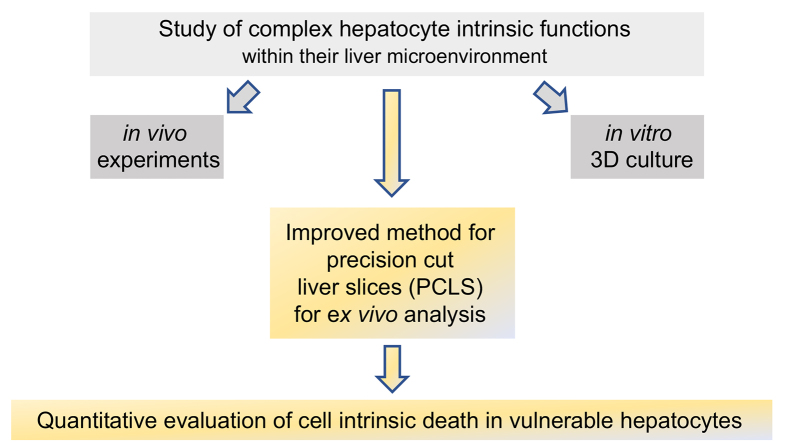
Increased sensitivity towards tumor necrosis factor (TNF)-induced cell death in virus-infected hepatocytes has revealed a so far unrecognized hepatocyte-intrinsic antiviral immune surveillance mechanism, for which no in vitro or ex vivo model is available. We aimed to establish precision-cut liver slices (PCLS) as a model system to study hepatocyte-intrinsic regulation of apoptosis.
Methods
Preparation of PCLS from mouse and human liver tissue was optimized for minimal procedure-associated apoptosis. Functionality of liver cells in PCLS was characterized using extracellular flux analysis to determine mitochondrial respiration, and viral infection with recombinant adenovirus and lymphocytic choriomeningitis virus (LCMV) was used to probe for hepatocyte-intrinsic sensitivity towards apoptosis in PCLS. Apoptosis was detected by immunohistochemical staining for cleaved-caspase 3 and quantified by detection of effector caspase activity in PCLS.
Results
We established an optimized protocol for preparation of PCLS from human and mouse models using agarose-embedding of liver tissue to improve precision cutting and using organ-protective buffer solutions to minimize procedure-associated cell death. PCLS prepared from virus-infected livers showed preserved functional metabolic properties. Importantly, in PCLS from adenovirus- and LCMV-infected livers we detected increased induction of apoptosis after TNF challenge ex vivo.
Conclusion
We conclude that PCLS can be used as model system to ex vivo characterize hepatocyte-intrinsic sensitivity to cell death. This may also enable researchers to characterize human hepatocyte sensitivity to apoptosis in PCLS prepared from patients with acute or chronic liver diseases.
Lay summary
Virus-infected hepatocytes in vivo show an increased sensitivity towards induction of cell death signaling through the TNF receptor. Studying this hepatocyte-intrinsic antiviral immune surveillance mechanism has been hampered by the absence of model systems that reciprocate the in vivo finding of increased apoptosis of virus-infected hepatocytes challenged with TNF. Herein, we report that an optimized protocol for generation of precision-cut liver slices can be used to study this hepatocyte-intrinsic surveillance mechanism ex vivo.
Keywords: TNF-induced apoptosis, precision-cut liver slices, anti-viral immunity
Abbreviations: IP3, inositol-3-phosphate; LCMV, lymphocytic choriomeningitis virus; PCLS, precision-cut liver slices; PLCg, phospholipase C gamma; ROS, reactive oxygen species; TNF, tumor necrosis factor
Graphical abstract
Highlights
-
•
Precision-cut liver slices (PCLS) can be used to study hepatocyte-intrinsic regulation of cell death ex vivo.
-
•
Increased induction of apoptosis is detected in PCLS from adenovirus- and LCMV-infected livers after TNF challenge ex vivo.
-
•
Optimized protocol may enable the characterization of human hepatocyte sensitivity to apoptosis in PCLS from patients with liver diseases.
Introduction
Immune effector cell populations like virus-specific T cells and natural killer cells, that recognize and kill virus-infected hepatocytes, contribute to successful immune surveillance in the liver.1 The selective elimination of virus-infected hepatocytes was considered to rely entirely on the ability of virus-specific effector cell populations to execute their killing activity. Consequently, research aiming to understand successful or failing immune surveillance against viral infection in the liver has mainly focused on studying the numbers and the breadth of effector function of virus-specific T cells.2,3 Recently it has become evident, however, that hepatocytes themselves contribute to immune surveillance by developing a unique state of responsiveness towards death signals.4 Virus-infected but not healthy hepatocytes selectively respond to tumor necrosis factor (TNF) receptor signaling with induction of caspase-induced cell death, i.e., apoptosis. This reveals the existence of hepatocyte-intrinsic antiviral surveillance that is independent of cytolytic T cell effector function and that leads to death of hepatocytes.4,5
Currently, there are no in vitro or ex vivo models in place to study the contribution and mechanistic aspects of this increased sensitivity to apoptosis in hepatocytes in liver diseases. Hepatocytes function within their microenvironment, which may be important to sustain their metabolic and immune functions and may explain why certain functions observed in vivo are not observed in vitro in isolated primary hepatocytes.6,7 The necessity to study organ context-dependent functions of cells has been recognized as a general challenge, and has led to the development of experimental model systems in many organ-specific research fields that allow for contextual analysis of cell functions in tissues.8 For the liver, different 3D cell culture models have been developed, which simulate the hepatic microanatomy like liver scaffolds and facilitate the growth of different liver cell populations in defined 3D-structures.9 Stem cell-derived liver cells were also used to construct human liver tissue.10 Yet, all these approaches require sophisticated technologies. A more direct approach to generate 3D tissue models, which reflect the complexity of tissue organization, for the study of tissue context-dependent cell functions is the generation of precision-cut tissue slices.11,12 Precision-cut liver slice (PCLS) models were used in the past to explore pathophysiological mechanisms underlying chronic liver damage,[13], [14], [15] and mechanisms underlying hepatic steatosis, steatohepatitis or drug metabolism.[16], [17], [18], [19], [20], [21] Herein, we report on an improved PCLS model that enables the ex vivo analysis of hepatocyte-intrinsic mechanisms, which determine sensitivity of virus-infected hepatocytes towards death signaling.
Materials and methods
Mouse and human liver
C57BL/6J mice were purchased from Charles River (Germany). All mice used in the experiments were maintained under specific pathogen-free conditions according to the guidelines of the Federation of Laboratory Animal Science Association. Animal experiments were approved by local authorities (ROB-55.2.2532.Vet_02-18-16). Experiments with human liver samples were approved by and performed in accordance with the regulations of the Ethics committee at the Technical University of Munich (86/17S) and the ethical guidelines of the World Medical Association Declaration of Helsinki. Informed written consent was obtained from each patient.
Preparation of PCLS
Murine livers were removed from anesthetized mice (2.5% isoflurane) and human liver tissue was obtained from patients undergoing liver resection for colorectal tumor metastasis. PCLS were generated as described here in short. After resection, liver tissue was immediately stored in the organ-preservation buffer solution custodiol® at 4°C (Köhler, Germany) and was immersed in 4% low-melting agarose. Agarose-stabilized liver tissue enabled the generation of PCLS using a vibratome Leica VT 1000S (Leica Biosystems, Germany). The freshly generated PCLS were maintained in Williams E Medium (PAN-Biotech, Germany), with gentle orbital shaking (80 times/min) at 37°C in a CO2 incubator to ensure tissue oxygenation and consistent exposure to reagents during experiments (please visit our detailed protocol for generation of PCLS in the supplementary information).
Results
Improved preparation of mouse and human PCLS
In vivo the induction of apoptosis in hepatocytes infected with a recombinant adenovirus coding for the marker genes GFP and luciferase (Ad-CMV-GL, 5x108 infectious units per mouse) occurred within 2 hours after TNF challenge (Fig. 1A,B). However, TNF-induced cell death after in vitro infection of hepatocytes with Ad-CMV-GL, required more than 5 hours, measured by loss of electrical impedance of the hepatocyte cell layer in a 96-well plate (Fig. 1C). Since it is not possible to isolate viable virus-infected hepatocytes for mechanistic in vitro studies of induction of cell death,4,5 we set out to establish a PCLS model that could enable the ex vivo characterization of the unique responsiveness of virus-infected hepatocytes in vivo within the liver to die by apoptosis.
Fig. 1.
Absence of cell death in murine and human PCLS.
(A) Serum ALT levels in mice after injection of TNF (400 ng/mouse) at d2 after infection with Ad-CMV-GL (5x108 infectious units/mouse). (B) H&E staining of liver sections at 4 h after TNF-injection in Ad-CMV-GL-infected mice, scale bar: 100 μm. (C) Primary mouse hepatocytes were grown to confluence in 2D-culture and were infected with Ad-CMV-GL before challenge with TNF 2 days later; time kinetics of hepatocyte death after TNF challenge was determined by measuring change in electrical impedance of healthy, healthy/TNF challenged, Ad-CMV-GL-infected and Ad-CMV-GL-infected/TNF challenged hepatocytes. (D) H&E staining of murine and human PCLS directly after preparation and after 2 h of incubation at 37°C, scale bar 100 μm. (E) Time kinetics of LDH release from murine PCLS after incubation at 37°C; lysed PCLS as positive control and culture medium alone as negative control. (F) Immunohistochemistry of PCLS for detection of cleaved-caspase 3 to identify apoptotic cells directly after preparation and after 2 hours of incubation at 37°C. (G) Quantification of cleaved-caspase 3-positive cells in human and murine PCLS (≥3,150 hepatocytes analyzed for each parameter) from (F). (A-G) Representative data from at least 3 separate experiments are shown as mean ± SEM. Statistical significance was calculated using unpaired t test, ∗p ≤0.05, ∗∗p ≤0.01 and ∗∗∗p ≤0.001. LDH, lactate dehydrogenase; PCLS, precision-cut liver slices; sALT, serum alanine aminotransferase; TNF, tumor necrosis factor.
We improved the generation of PCLS by stabilizing mouse and human liver tissue in a low-melting agarose to allow for gentle precision cutting of liver tissue into slices and by reducing tissue damage during this procedure through use of an organ-protective buffer solution (see detailed protocol for preparation of PCLS). Histomorphological analysis demonstrated that neither generation of PCLS nor subsequent incubation at 37°C for a period of 2 hours led to detectable cell damage in mouse and human PCLS (Fig. 1D). Consequently, we did not detect a release of lactate dehydrogenase, a marker for cell death, from PCLS after cutting or after incubation at 37°C (Fig. 1E). To confirm the absence of apoptotic cell death in the improved PCLS, we quantified induction of apoptosis by measuring cleaved-caspase 3, which is the apoptosis inducing active form of the effector caspase 3. We found very few cleaved-caspase 3-positive cells by immunohistochemistry in murine and human PCLS (Fig. 1F,G) compared to a higher number of apoptotic cells in PCLS generated by the conventional method (Fig. S1). Numbers of cleaved-caspase 3-positive hepatocytes were slightly higher in human PCLS (0.54% ± 0.27) compared to murine PCLS (0.23% ± 0.5). Taken together, these results demonstrated that the improved method for generating PCLS yielded viable liver tissue without generation of procedure-associated apoptotic cells (Fig. 1).
PCLS as ex vivo model system to study hepatocyte sensitivity to apoptosis
Establishing PCLS that did not bear high numbers of apoptotic cells allowed us to investigate whether these PCLS could be employed to study ex vivo the apoptotic response of infected hepatocytes observed in vivo. We first evaluated whether hepatocytes infected in vivo were detected in PCLS ex vivo. To this end, we generated a recombinant adenovirus coding for the fluorescence reporter gene iRFP720 (Ad-CMV-GIRO) that enables the detection of in vivo fluorescence activity of Ad-CMV-GIRO-infected hepatocytes due to the high tissue-penetration of light with high wavelength (>700 nm) emitted from iRFP720. In vivo fluorescence imaging of Ad-CMV-GIRO-infected mice demonstrated successful adenoviral transduction of the liver (Fig. 2A). Importantly, iRFP720-fluorescence was also ex vivo detected in PCLS from livers of mice infected with Ad-CMV-GIRO (Fig. 2B,C). No fluorescence signal was detected from uninfected livers in vivo or from PCLS prepared from these livers ex vivo (Fig. 2A-C). Histomorphological analysis of PCLS from infected livers compared to non-infected livers by H&E staining or staining for apoptotic cells (detection of cleaved-caspase 3) did not reveal tissue damage after infection (Fig. 2D). Taken together, these results demonstrated that virus-infected cells were present in PCLS generated from Ad-CMV-GIRO-infected liver.
Fig. 2.
TNF mediates cell death in PCLS from virus-infected liver.
(A) In vivo fluorescence imaging day 2 post infection (Ad-CMV-GIRO, 5x108 infectious units/mouse). (B) Fluorescence images of PCLS prepared from murine liver at day 2 post infection with Ad-CMV-GIRO (5x108 infectious units/mouse). (C) Quantification of fluorescence intensity (radiance) from PCLS (B). (D) H&E staining and immunohistochemistry for cleaved-caspase 3 in PCLS prepared from Ad-CMV-GIRO-infected livers or healthy livers. (E) Mitochondrial stress test of PCLS prepared from Ad-CMV-GIRO-infected livers (5x108 infectious units/mouse) or healthy livers. (F) Quantification of caspase 3 activity by luminescence detection assay in PCLS prepared from Ad-CMV-GIRO-infected liver (5x108 infectious units/mouse) at 2 h after ex vivo TNF challenge (20 ng/ml). (G, H) Quantification of caspase 3-activity in PCLS prepared from Ad-CMV-GIRO infected liver (5x108 infectious units/mouse) after incubation with pharmacological inhibitors of ROS (luteolin), IP3 receptor signaling (xestospongin), PLCg-signaling (edelfosin) and ex vivo TNF challenge (20 ng/ml). (I) Quantification of caspase 3-activity in PCLS prepared from LCMV strain WE-infected livers at 2 h after ex vivo TNF challenge (20 ng/ml and 100 ng/ml). (A-I) Representative data from at least 3 separate experiments are shown as mean ± SEM. Statistical significance was calculated using unpaired t test, ∗p ≤0.05, ∗∗p ≤0.01 and ∗∗∗p ≤0.001. IP3, inositol-3-phosphate; LCMV, lymphocytic choriomeningitis virus; PCLS, precision-cut liver slices; PLCg, phospholipase C gamma; ROS, reactive oxygen species; TNF, tumor necrosis factor.
Viral infection leads to rapid expression of viral genes that might cause changes in cellular metabolism.22 We therefore investigated whether metabolic mitochondrial activity was different in PCLS prepared from Ad-CMV-GIRO-infected livers compared to healthy livers. There was no difference in mitochondrial respiration activity measured by extracellular flux analysis of PCLS prepared from Ad-CMV-GIRO-infected compared to healthy livers (Fig. 2E, Fig. S2). In the absence of a change in mitochondrial respiration after Ad-CMV-GIRO infection, we next characterized the response of Ad-CMV-GIRO-infected cells to TNF challenge. Strikingly, in PCLS prepared from virus-infected livers we detected higher caspase 3 activity than in PCLS from uninfected livers at 2 hours after ex vivo TNF challenge (Fig. 2F). Since induction of apoptosis through TNF receptor signaling in virus-infected hepatocytes in vivo requires NADPH-oxidase and generation of reactive oxygen species (ROS),4 we addressed the question of whether blockade of ROS formation would rescue TNF-induced apoptosis in PCLS. Clearly, incubation of PCLS prepared from Ad-CMV-GIRO infected livers with the ROS-blocking agent luteolin prevented TNF-induced caspase activation (Fig. 2G). To further evaluate the involvement of signaling events downstream of ROS formation, we studied the relevance of phospholipase C gamma (PLCg) activation and inositol-3-phosphate (IP3)-receptor signaling for induction of apoptosis in Ad-CMV-GIRO-infected hepatocytes. Incubation with the pharmacological inhibitor of IP3-receptor signaling (xestospongin) prevented TNF-induced caspase 3 activation in PCLS prepared from Ad-CMV-GIRO-infected livers (Fig. 2G). Furthermore, pharmacological inhibition of PLCg-activation with edelfosin equally prevented caspase 3 activation in PCLS prepared from Ad-CMV-GIRO-infected livers at 2 hours after ex vivo TNF challenge (Fig. 2H). To demonstrate that increased sensitivity of hepatocytes to apoptosis in PCLS was not restricted to infection with recombinant adenoviruses, we used the lymphocytic choriomeningitis virus (LCMV) strain WE to infect the liver. PCLS prepared from LCMV-infected livers also showed caspase 3 activation at 2 hours after ex vivo TNF challenge and the extent of liver damage increased with higher TNF doses (Fig. 2I). Together, these results demonstrated that, in PCLS prepared from virus-infected livers ex vivo, a TNF challenge induced caspase 3 activation, which was prevented by inhibition of ROS formation and by interfering with PLCg-activation or IP3-receptor signaling (Fig. 2).
Discussion
Studying the response of hepatocytes within their liver microenvironment to signaling processes requires either an in vivo disease model, complex 3D cultures of hepatocytes mimicking the complex liver microenvironment for in vitro studies, or viable liver slice cultures for ex vivo studies. Herein, we demonstrate an improved method for preparation of PCLS that yields liver tissue slices that could be used to characterize ex vivo the hepatocyte-intrinsic response to induction of apoptosis. Improved cutting of liver tissue through immobilization of liver tissue in agarose blocks together with the use of a tissue-preservation solution used in liver transplantation enabled the preparation of PCLS from mouse and human liver tissue that showed almost no procedure-associated cell death. However, PCLS prepared from surgically resected human liver tissue showed few apoptotic cells, which may be related to longer time spans of tissue hypoxia before the start of PCLS preparation. In accordance with this assumption, we did not find a further increase in numbers of apoptotic cells over time after incubation of human PCLS.
Next, we investigated whether PCLS can be used to study liver cell functions ex vivo. Fluorescence activity in hepatocytes infected in vivo with recombinant Ad-CMV-GIRO was preserved ex vivo in PCLS prepared from these livers, which pointed towards conservation of functions of virus-infected hepatocytes. Similarly, mitochondrial respiration was intact in PCLS as determined by extracellular flux analysis of single mouse PCLS, and showed similarity to mitochondrial respiration detected from hepatocytes analyzed ex vivo,4 which further corroborates that liver cell functionality was maintained in PCLS. Most importantly, development of liver cell death was observed in PCLS prepared from virus-infected livers after TNF challenge ex vivo, which resembled the rapid response of virus-infected hepatocytes to TNF in vivo.4 Such sensitivity to apoptosis of liver cells in PCLS was not restricted to infection with adenoviruses, a DNA virus, but was also observed after infection with an RNA virus (LCMV) suggesting that the unique sensitivity of hepatocytes to apoptosis after TNF challenge might also be present during infection with other viruses. The development of an improved method to prepare PCLS may therefore allow for the characterization of the underlying mechanism of hepatocyte-intrinsic regulation of apoptosis induction in molecular detail using inhibitors that would exert systemic toxicity in vivo. Furthermore, since we have also shown that human PCLS can be generated with this protocol, PCLS-based analysis of hepatocyte sensitivity to cell death may be extended to human diseases like acute or chronic viral hepatitis,23,24,25 non-alcoholic steatohepatitis26 or drug-induced liver injury,27 where liver cell death is observed.
Financial support
German National Science Foundation, SFB TR 179.
Authors’ contributions
MB, SL, AS, KM, ML performed experiments; NH and DH provided essential study material; MB, ML, KS, DW, PK analyzed the data; MB, SE, PK designed the study; MB, DW and PK wrote the manuscript, all authors approved the manuscript.
Data availability statement
The data generated and analyzed are available from the corresponding author, MB, upon reasonable request.
Conflict of interest
The authors declare no conflict of interest.
Please refer to the accompanying ICMJE disclosure forms for further details.
Acknowledgments
We thank Silke Hegenbarth, Sava Michailidou, Michaela Müller, Marianne K. Janas (Institute of Molecular Immunology and Experimental Oncology) for technical support.
Footnotes
Author names in bold designate shared co-first authorship.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jhepr.2022.100463.
Contributor Information
Marcus Brugger, Email: marcus.brugger@tum.de.
Percy A. Knolle, Email: percy.knolle@tum.de.
Supplementary data
The following are the supplementary data to this article:
References
- 1.Protzer U., Maini M.K., Knolle P.A. Living in the liver: hepatic infections. Nat Rev Immunol. 2012;12:201–213. doi: 10.1038/nri3169. [DOI] [PubMed] [Google Scholar]
- 2.Maini M.K., Pallett L.J. Defective T-cell immunity in hepatitis B virus infection: why therapeutic vaccination needs a helping hand. Lancet Gastroenterol Hepatol. 2018;3:192–202. doi: 10.1016/S2468-1253(18)30007-4. [DOI] [PubMed] [Google Scholar]
- 3.Ficht X., Iannacone M. Immune surveillance of the liver by T cells. Sci Immunol. 2020;5 doi: 10.1126/sciimmunol.aba2351. [DOI] [PubMed] [Google Scholar]
- 4.Lampl S., Janas M.K., Donakonda S., Brugger M., Lohr K., Schneider A., et al. Reduced mitochondrial resilience enables non-canonical induction of apoptosis after TNF receptor signaling in virus-infected hepatocytes. J Hepatol. 2020;73(6):1347–1359. doi: 10.1016/j.jhep.2020.06.026. [DOI] [PubMed] [Google Scholar]
- 5.Wohlleber D., Kashkar H., Gärtner K., Frings M.K., Odenthal M., Hegenbarth S., et al. TNF-induced target cell killing by CTL activated through cross-presentation. Cell Rep. 2012;2:478–487. doi: 10.1016/j.celrep.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 6.Gebhardt R. Metabolic zonation of the liver: regulation and implications for liver function. Pharmacol Ther. 1992;53:275–354. doi: 10.1016/0163-7258(92)90055-5. [DOI] [PubMed] [Google Scholar]
- 7.Gola A., Dorrington M.G., Speranza E., Sala C., Shih R.M., Radtke A.J., et al. Commensal-driven immune zonation of the liver promotes host defence. Nature. 2021;589:131–136. doi: 10.1038/s41586-020-2977-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Godoy P., Hewitt N.J., Albrecht U., Andersen M.E., Ansari N., Bhattacharya S., et al. Recent advances in 2D and 3D in vitro systems using primary hepatocytes, alternative hepatocyte sources and non-parenchymal liver cells and their use in investigating mechanisms of hepatotoxicity, cell signaling and ADME. Arch Toxicol. 2013;87:1315–1530. doi: 10.1007/s00204-013-1078-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thanapirom K., Caon E., Papatheodoridi M., Frenguelli L., Al-Akkad W., Zhenzhen Z., et al. Optimization and validation of a novel three-dimensional co-culture system in decellularized human liver scaffold for the study of liver fibrosis and cancer. Cancers. 2021;13:4936. doi: 10.3390/cancers13194936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Takebe T., Sekine K., Enomura M., Koike H., Kimura M., Ogaeri T., et al. Vascularized and functional human liver from an iPSC-derived organ bud transplant. Nature. 2013;499:481–484. doi: 10.1038/nature12271. [DOI] [PubMed] [Google Scholar]
- 11.Palma E., Doornebal E.J., Chokshi S. Precision-cut liver slices: a versatile tool to advance liver research. Hepatol Int. 2019;13:51–57. doi: 10.1007/s12072-018-9913-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de Graaf I.A., Olinga P., de Jager M.H., Merema M.T., de Kanter R., van de Kerkhof E.G., et al. Preparation and incubation of precision-cut liver and intestinal slices for application in drug metabolism and toxicity studies. Nat Protoc. 2010;5:1540–1551. doi: 10.1038/nprot.2010.111. [DOI] [PubMed] [Google Scholar]
- 13.Wu X., Roberto J.B., Knupp A., Kenerson H.L., Truong C.D., Yuen S.Y., et al. Precision-cut human liver slice cultures as an immunological platform. J Immunol Methods. 2018;455:71–79. doi: 10.1016/j.jim.2018.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Othman A., Ehnert S., Dropmann A., Ruoß M., Nüssler A.K., Hammad S. Precision-cut liver slices as an alternative method for long-term hepatotoxicity studies. Arch Toxicol. 2020;94:2889–2891. doi: 10.1007/s00204-020-02861-9. [DOI] [PubMed] [Google Scholar]
- 15.Starokozhko V., Vatakuti S., Schievink B., Merema M.T., Asplund A., Synnergren J., et al. Maintenance of drug metabolism and transport functions in human precision-cut liver slices during prolonged incubation for 5 days. Arch Toxicol. 2017;91:2079–2092. doi: 10.1007/s00204-016-1865-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van de Bovenkamp M., Groothuis G.M., Meijer D.K., Olinga P. Liver slices as a model to study fibrogenesis and test the effects of anti-fibrotic drugs on fibrogenic cells in human liver. Toxicol In Vitro. 2008;22:771–778. doi: 10.1016/j.tiv.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 17.Graaf I.A., Groothuis G.M., Olinga P. Precision-cut tissue slices as a tool to predict metabolism of novel drugs. Expert Opin Drug Metab Toxicol. 2007;3:879–898. doi: 10.1517/17425255.3.6.879. [DOI] [PubMed] [Google Scholar]
- 18.Hadi M., Westra I.M., Starokozhko V., Dragovic S., Merema M.T., Groothuis G.M. Human precision-cut liver slices as an ex vivo model to study idiosyncratic drug-induced liver injury. Chem Res Toxicol. 2013;26:710–720. doi: 10.1021/tx300519p. [DOI] [PubMed] [Google Scholar]
- 19.Westra I.M., Mutsaers H.A., Luangmonkong T., Hadi M., Oosterhuis D., de Jong K.P., et al. Human precision-cut liver slices as a model to test antifibrotic drugs in the early onset of liver fibrosis. Toxicol In Vitro. 2016;35:77–85. doi: 10.1016/j.tiv.2016.05.012. [DOI] [PubMed] [Google Scholar]
- 20.Guyot C., Lepreux S., Combe C., Sarrazy V., Billet F., Balabaud C., et al. Fibrogenic cell phenotype modifications during remodelling of normal and pathological human liver in cultured slices. Liver Int. 2010;30:1529–1540. doi: 10.1111/j.1478-3231.2010.02342.x. [DOI] [PubMed] [Google Scholar]
- 21.Duryee M.J., Willis M.S., Schaffert C.S., Reidelberger R.D., Dusad A., Anderson D.R., et al. Precision-cut liver slices from diet-induced obese rats exposed to ethanol are susceptible to oxidative stress and increased fatty acid synthesis. Am J Physiol Gastrointest Liver Physiol. 2014;306:G208–217. doi: 10.1152/ajpgi.00124.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sanchez E.L., Lagunoff M. Viral activation of cellular metabolism. Virology. 2015;479-480:609–618. doi: 10.1016/j.virol.2015.02.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Iannacone M., Guidotti L.G. Immunobiology and pathogenesis of hepatitis B virus infection. Nat Rev Immunol. 2021 doi: 10.1038/s41577-021-00549-4. [DOI] [PubMed] [Google Scholar]
- 24.Polakos N.K., Cornejo J.C., Murray D.A., Wright K.O., Treanor J.J., Crispe I.N., et al. Kupffer cell-dependent hepatitis occurs during influenza infection. Am J Pathol. 2006;168:1169–1178. doi: 10.2353/ajpath.2006.050875. quiz 1404-1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang Y., Liu S., Liu H., Li W., Lin F., Jiang L., et al. SARS-CoV-2 infection of the liver directly contributes to hepatic impairment in patients with COVID-19. J Hepatol. 2020;73:807–816. doi: 10.1016/j.jhep.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sutti S., Albano E. Adaptive immunity: an emerging player in the progression of NAFLD. Nat Rev Gastroenterol Hepatol. 2020;17:81–92. doi: 10.1038/s41575-019-0210-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Andrade R.J., Chalasani N., Björnsson E.S., Suzuki A., Kullak-Ublick G.A., Watkins P.B., et al. Drug-induced liver injury. Nat Rev Dis Primers. 2019;5:58. doi: 10.1038/s41572-019-0105-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data generated and analyzed are available from the corresponding author, MB, upon reasonable request.