Abstract
Background:
Thyroid cancer has become increasingly prevalent and threatens human health. Few studies have explored the incidence of thyroid cancer in Asia and its relationship with social-progress factors.
Methods:
We analyzed Global Burden of Disease (GBD) Study 2019 data specific to thyroid cancer. Incidence, prevalence, mortality, and disability-adjusted life year (DALY) rates were used to evaluate the burden of thyroid cancer.
Results:
The age-standardized incidence, prevalence, and DALY rates per 100,000 population were 1.34% (95% UI, 2.44–3.07), 2.79% (95% UI, 18.82–23.77) and 16.49% (95% UI, 14.6–18), respectively, for all of Asia in 2019. In 2019, the DALY rate of thyroid cancer in the High-income Asia-Pacific region was the highest and mortality due to thyroid cancer in the High-income Asia-Pacific region was also the highest. The growth trend of DALYs in the High-income Asia-Pacific region was much steeper than those in other Asian regions. In all Asian regions and in the High-income Asia-Pacific region, the incidence, prevalence, mortality and DALY rates of thyroid cancer in female patients were drastically higher than those in male patients. Among Asian patients with thyroid cancer, the DALY rate was higher in men aged 80–89 years than in women. The DALY rate gradually increased with age. In the High-income Asia-Pacific region, the mortality rate of patients with thyroid cancer decreased with age. The prevalence was highest in those aged 40–79 years.
Conclusion:
The disease burden of thyroid cancer in the High-income Asia-Pacific region was significantly higher than those in other regions, which may be due to overdiagnosis. The increasing incidence of thyroid cancer seems to indicate that thyroid cancer is still a public health problem in Asia. Therefore, some health policy adjustments will be meaningful.
Keywords: disability-adjusted life year, GBD study, thyroid cancer
Introduction
Thyroid cancer is the most frequently occurring endocrine tumour, with a high incidence rate, especially in women. 1 Thyroid cancer has received increasing attention worldwide. Thyroid cancer, the most frequent endocrine malignancy, accounts for approximately 1.5% of newly diagnosed cancers in Europe. 2 Some studies have shown that following current trends, thyroid cancer will become the fourth most common cancer in the United States by 2030. 3
Binh Hyang reported that the cancer burden will become a very serious public health challenge in the Asia-Pacific region, which encompasses Asia and the Pacific islands. 4 Recently, many stomach cancer collaborators of the Global Burden of Disease (GBD) Study 2017, including Arash Etemadi, reported that the highest age-standardized incidence rate of stomach cancer in 2017 was in the High-income Asia-Pacific region. 5 However, the relevant epidemiological characteristics of thyroid cancer in Asia and the High-income Asia-Pacific region have not been well studied. The incidence of thyroid cancer has increased annually over the past 40 years from 4.9 per 100,000 people in 1975 to 14.3 per 100,000 people in 2009. 6 Thus, an increasing number of studies on thyroid cancer will be performed, especially in Asia.
The GBD Study 2019, which included 204 countries and locations and areas from 1990 to 2019, furnished a complete evaluation of the loss of human health attributable to 369 diseases and injuries. 7 The GBD 2019 added updated and additional data to the GBD database and the updated data are recent, so it is more representative. Given that the current coronavirus disease 2019 (COVID-19) pandemic has caused delays and interruptions in cancer screening, diagnosis and treatment worldwide, accelerating research progress is important. 8 The GBD Study 2019 is a comprehensive study on health and health-related losses to society due to illness and injury can be observed. 9 The gradual progression of GBD research has allowed meaningful discussions about changes in health challenges associated with thyroid cancer in Asia.10,11 Currently, few studies have analyzed GBD Study data on thyroid cancer, and emphasizing thyroid cancer in the Asian region is necessary.
The prevalence of most cancers increases with age, 12 and the burden of thyroid cancer in countries with severely ageing populations is unknown. In Asia, specifically in the High-income Asia-Pacific region, the population is ageing rapidly. Thyroid cancer incidence rates have increased significantly in some wealthy countries in recent decades. 13 Especially in developed countries, such as Korea, thyroid cancer has become a significant contributor to the number of disability-adjusted life years (DALYs). 14 Therefore, this region is important in the assessment of the dynamics of the thyroid cancer burden.
The purpose of this study was to assess the thyroid cancer disease burden in the High-income Asia-Pacific region and perform a detailed comparison of different sex- and age-related indicators of thyroid cancer in Asia and the High-income Asia-Pacific region. These study results can be utilized by countries with different economic levels in different regions to reduce the unnecessary burden of thyroid cancer.
Methods
This study analyzed data from the GBD Study 2019 to explore the epidemiology of thyroid cancer in Asia.
The GBD research group developed the DALYs indicator to assess the burden of disease. 15 Thyroid cancer statistics (1990–2019) according to sex, age, region and year are available from the Institute for Health Metrics and Evaluation (IHME) global health data exchange (GHDx) website, and the data are accumulated and analyzed through the global health data exchange tool. Details of the methodology used in the GBD Study 2019 are described on the official Internet website (http://ghdx.healthdata.org/gbd-results-tool). 16 The GBD Study 2019 provided the annual prevalence, incidence, and mortality rates; years of life lost (YLLs); years lived with disability (YLDs); and DALYs attributable to thyroid cancer from 1990 to 2019. The DALY rate is the sum of YLLs and YLDs, so DALYs take into account the premature death and health-related suffering to represent the total years of healthful existence lost to all causes. 17 The purpose of this study was to analyze thyroid cancer prevalence, incidence and mortality rates, DALYs and other related indicators of thyroid cancer and compare those in the Asian region with those in the High-income Asia-Pacific region. To examine the incidence rates among multiple populations or time points, we defined the age-standardized rate as a comprehensive indicator to analyze the specific age-related incidence rate in different years. The age-standardized rate of thyroid cancer results is primarily based on the age data of the GBD Study 2019.15 The analysis of age data in this study was performed considering 5-year intervals from 1990 to 2019 and 20 age groups (ranging from 1 to 95 plus years old). A statistical description of the experimental data was performed using GraphPad software.
Results
As indicated in Table 1, which lists the total number of thyroid cancer cases and related age-standardized rates in Asia and various regions in Asia in 2019, the age-standardized incidence rate, prevalence rate, and DALY rate per 100,000 population were estimated to be 1.34% (95% uncertainty interval (UI), 2.44–3.07), 2.79% (95% UI, 18.82–23.77) and 16.49% (95% UI, 14.6–18), respectively, for all of Asia in 2019. The region with the highest incidence of thyroid cancer in Asia in 2019 was East Asia, at 41,579.53 (95% UI, 34,750.62–50,204.07), and the region with the lowest incidence was Oceania, at 161.67 (95% UI, 113.9–219.59). The area with the highest age-standardized incidence rate of thyroid cancer was Oceania, at 11.30% (95% UI, 8.23–15.62). Interestingly, the age-standardized incidence rate in the High-income Asia-Pacific region reached a maximum value of 8.36% (95% UI, 7.01–9.64). In 2019, the DALY rate of thyroid cancer in the High-income Asia-Pacific region was the highest, at 26.17% (95% UI, 22.24–29.19), and the mortality rate of thyroid cancer in the High-income Asia-Pacific region was the highest, at 1.47% (95% UI, 1.14–1.64). In addition, thyroid cancer caused 49,019.24 (95% UI, 41,648.17–54,668.39) DALYs in 2019.
Table 1.
Number and age-standardized prevalence, incidence, mortality, YLLs, YLDs and DALY rates in 2019 for thyroid cancer in Asia.
| South Asia | Southeast Asia | High-income Asia-Pacific | Oceania | |||||
|---|---|---|---|---|---|---|---|---|
| Age-standardized rate per 100,000 | Total | Age-standardized rate per 100,000 | Total | Age-standardized rate per 100,000 | Total | Age-standardized rate per 100,000 | Total | |
| DALYS | 16.15 (14.09–18.32) |
291,574.64 (254,403.38–330,796.42) |
24.39 (20.26–27.90) |
164,303.52 (136,533.58–187,955.55) |
26.17 (22.24–29.19) |
49,019.24 (41,648.17–54,668.39) |
1.22 (0.86–1.65) |
1576.43 (1156.35–2176.44) |
| DEATHS | 0.51 (0.44–0.58) |
9195.55 (7978.03–10,476.58) |
0.87 (0.74–0.99) |
5862.06 (4999.36–6646.13) |
1.47 (1.14–1.64) |
2754.35 (2127.72–3071.31) |
0.38 (0.28–0.51) |
50.20 (37.29–68.12) |
| Prevalence | 12.55 (10.48–14.61) |
226,466.71 (189,125.73–263,768.63) |
28.93 (22.85–34.25) |
194,898.69 (153,975.46–230,803.05) |
65.97 (56.07–76.34) |
123,548.32 (105,011.59–142,979.40) |
11.87 (8.71–16.39) |
1114.43 (765.4–1521.53) |
| Incidence | 1.75 (1.47–2.02) |
31,533.90 (26,591.47–36,439.30) |
3.80 (3.05–4.44) |
25,581.44 (20,569.12–29,885.75) |
8.36 (7.01–9.64) |
15,659.75 (13,134.42–18,056.29) |
11.30 (8.23–15.62) |
161.67 (113.9–219.59) |
| YLDS | 0.80 (0.54–1.12) |
14,455.20 (9657.83–20,221.79) |
1.82 (1.20–2.55) |
12,235.22 (8065.08–17,164.50) |
4.10 (2.76–5.78) |
7677.56 (5160.56–10,820.34) |
0.57 (0.35–0.89) |
76.05 (45.84–118.68) |
| YLLS | 15.35 (13.42–17.49) |
277,119.44 (242,233.44–315,799.76) |
22.57 (18.76–25.90) |
152,068.30 (126.427.00–174.530.60) |
22.07 (18.37–24.16) |
41,341.68 (34,412.42–45,253.98) |
8.39 (5.77–11.46) |
1500.38 (1092.36–2073.39) |
| Asia | Central Asia | East Asia | ||||||
| Age-standardized rate per 100,000 | Total | Age-standardized rate per 100,000 | Total | Age-standardized rate per 100,000 | Total | |||
| DALYS | 16.49 (14.6–18) |
750,983.75 (665,082.63–819,813.37) |
9.87 (8.77–11.04) |
9231.30 (8202.92–10,321.49) |
13.40 (11.22–15.52) |
197,337.06 (165,223.90–228,530.15) |
||
| DEATHS | 0.59 (0.53–0.65) |
26,982.24 (23,978.01–29,390.85) |
0.33 (0.30–0.36) |
308.74 (278.41–340.85) |
0.52 (0.43–0.60) |
7620.95 (6346.14–8874.16) |
||
| Prevalence | 2.79 (18.82–23.77) |
127,008.06 (857,343.77–1,082,418.36) |
12.25 (10.83–13.87) |
11,453.95 (10,131.17–12,975.29) |
22.46 (18.66–27.41) |
330,694.28 (274,742.67–403,528.00) |
||
| Incidence | 1.34 (2.44–3.07) |
61,060.65 (111,148.68–139,719.56) |
1.57 (1.40–1.76) |
1467.37 (1305.66–1649.90) |
2.82 (2.36–3.41) |
41,579.53 (34,750.62–50,204.07) |
||
| YLDS | 21.57 (0.91–1.83) |
982,341.15 (41,231.73–83,495.88) |
0.77 (0.52–1.06) |
719.03 (488.29–995.01) |
1.38 (0.91–1.99) |
20,386.07 (13,431.75–29,297.95) |
||
| YLLS | 15.15 (13.42–16.6) |
689,923.10 (611,277.65–756,008.82) |
9.10 (8.15–10.13) |
8512.26 (7624.29–9470.82) |
12.02 (10.07–14.09) |
176,950.98 (148,178.28–207,487.06) |
||
DALYs, disability-adjusted life year; YLDs, years lived with disability; YLLs, years of life lost.
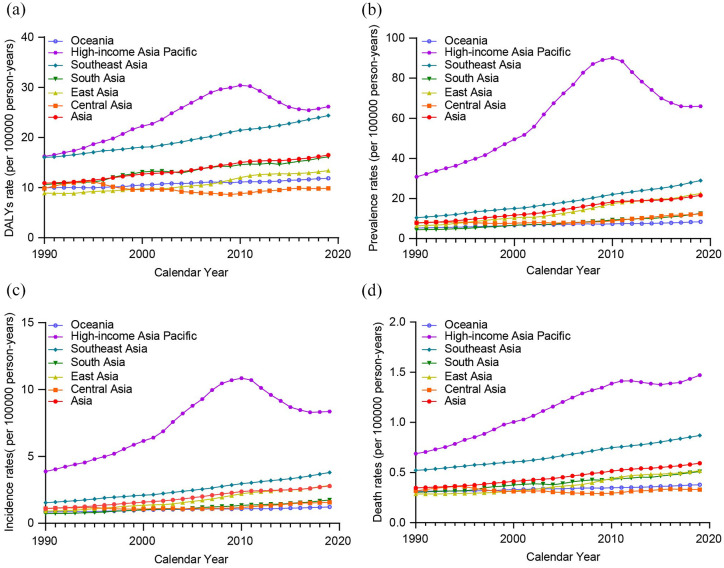
Trends of the age-standardized DALY, prevalence, incidence and mortality rates of thyroid cancer in Asia from 1990 to 2019 are shown in Figure 1. Figure 1(a) shows that the DALY rates of thyroid cancer in all Asian regions increased gradually from 1990 to 2019. The growth trend of DALYs in the High-income Asia-Pacific region was much steeper than those in other Asian regions, peaking at 30.40 (95% UI, 22.21–33.54) per 100,000 people in 2010. The DALY rate of thyroid cancer gradually declined after 2010 and gradually increased after reaching the minimum value of 25.45 (95% UI, 21.63–28.21) per 100,000 people in 2017. Figure 1(b)–(d) shows that the incidence, prevalence and mortality rates in the High-income Asia-Pacific region showed the same tendencies, with increases in 1990 and gradual decreases after 2010. As shown in Figure 1, the prevalence, incidence, mortality and DALY rates in other Asian regions increased linearly annually.
Figure 1.
Trends in age-standardized rates for (a) DALYs, (b) prevalence, (c) incidence, and (d) deaths for thyroid cancer in Asia from 1990 to 2019.
DALY, disability-adjusted life year.
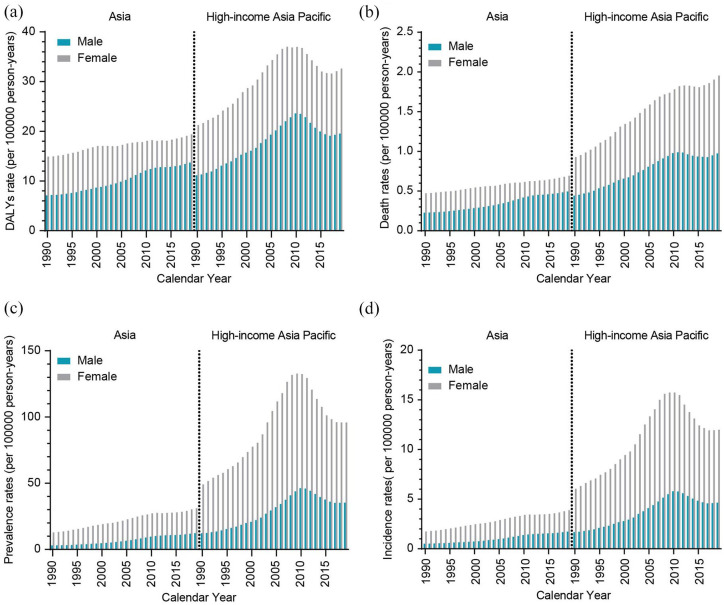
Figure 2 shows the change trends of thyroid cancer in Asia and the High-income Asia-Pacific region from 1990 to 2019 by sex. In Asia and in the High-income Asia-Pacific region, the incidence, prevalence, mortality and DALY rates of thyroid cancer in female patients were appreciably higher than those in male patients. On the left of the dotted line in the figure is the Asian region and on the right side is the High-income Asia-Pacific region. The incidence, prevalence, mortality and DALY rates of thyroid cancer have increased linearly in the past 30 years. Interestingly, the incidence of thyroid cancer in females in the High-income Asia-Pacific region increased annually from 1990 to 2009 and peaked at 15.73% (95% UI, 10.31–17.54) in 2009. After 2009, it declined annually, but in recent years, it has shown a gradual upwards trend. The incidence of thyroid cancer in males peaked at 5.79% (95% UI, 3.79–6.42) in 2010. The thyroid cancer mortality rates in men and women in the High-income Asia-Pacific region did not show significant decreases. Consistent with that shown in Figure 1, the DALY rates of thyroid cancer in High-income regions within the Asia-Pacific region confirmed a considerable upwards trend from 1990 to 2010. Among them, the DALY rate of thyroid cancer was highest in 2010 [males 23.60% (95% UI, 15.75–25.63) and females 36.98% (95% UI, 27.14–41.71)]; there was a downwards trend starting in 2010; however, an upwards trend was observed for the last 3 years.
Figure 2.
Disease burden of thyroid cancer among males and females in Asia and High-income Asia-Pacific regions from 1990 to 2019. (a) DALYs rate of thyroid cancer in Asia and High-income Asia-Pacific from 1990 to 2019, (b) Deaths rates of thyroid cancer in Asia and High-income Asia-Pacific from 1990 to 2019, (c) Prevalence rates of thyroid cancer in Asia and High-income Asia-Pacific from 1990 to 2019., and (d) Incidence rates of thyroid cancer in Asia and High-income Asia-Pacific from 1990 to 2019.
DALY, disability-adjusted life year.
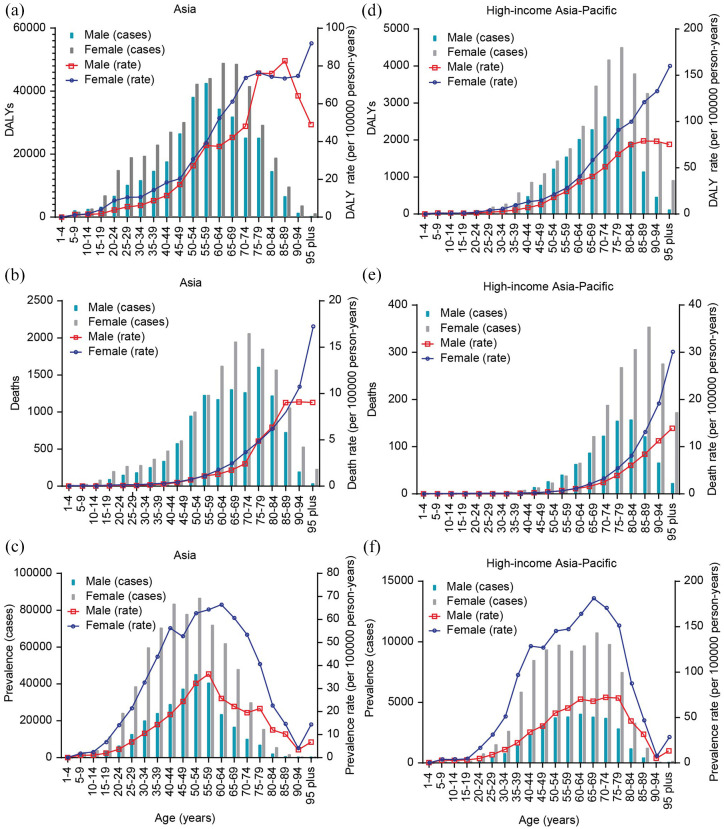
Figure 3 shows the DALY, prevalence mortality rates and the total number of thyroid cancer cases in Asia and the High-income Asia-Pacific region in 2019 by age. In terms of age, the middle-aged and elderly populations had the highest rates of thyroid cancer in Asia, especially those aged 40–59 years. Among all the age groups, with the exception of the 60–94 years age group, the age-standardized prevalence steadily increased with age. The 50–54 years age group had the largest number of patients, both male and female, in Asia. In the Asian region, the mortality rate of elderly male patients aged 80–89 years was higher than that of female patients. The age-standardized mortality rates in the other age groups gradually increased with age, and mortality in female patients was higher than that in male patients. Among Asian patients with thyroid cancer, the DALY rate in men in the 80–89 years age group was higher than that in women, while for the other age groups, the DALY rate was higher in women.
Figure 3.
Age-specific counts and rate of DALYs, prevalence and deaths in Asia and High-income Asia-Pacific regions by gender in 2019.
Age-specific counts and rate of (a) DALYs, (b) deaths and (c) prevalence in Asia by gender. Age-specific counts and rate of (d) DALYs, (e) deaths and (f) prevalence in High-income Asia-Pacific regions by gender.
DALY, disability-adjusted life year.
In the High-income Asia-Pacific region, the mortality rate of patients with thyroid cancer also increased with age, as shown in Figure 3(e). The prevalence of thyroid cancer in the High-income Asia-Pacific region was mainly concentrated in the 40–79 years age group. The prevalence rate in the 65–94 years age group showed a downwards trend with increasing age, while the prevalence rates in the rest of the age groups increased with age. Regardless of age, the prevalence in females was significantly higher than that in males. The DALY rate of thyroid cancer in the High-income Asia-Pacific region gradually increased with age, and the DALY rate in women was greater than that in men.
Discussion
Thyroid cancer is a frequent malignant tumour of the endocrine system. 18 In 2014, Noda’s Natural History of Thyroid Cancer mentioned that although thyroid cancer is a malignant tumour, the degree of malignancy is not high enough to cause death. 19 Therefore, the disease burden imposed by thyroid cancer on the population is worthy of discussion. Morbidity and mortality attributable to thyroid cancer are increasing worldwide. Previous studies have explored the incidence and mortality rates by analysing out-of-date thyroid cancer data, as information related to thyroid cancer in Asia is scarce. Therefore, we verified key findings and viewpoints regarding thyroid cancer based on the GBD Study 2019. Although some studies have estimated the disease burden of thyroid cancer in Asia, in this study, we evaluated the burden and trend of thyroid cancer in Asia, especially the High-income Asia-Pacific region, and discussed the correlations of sex and age with thyroid cancer in the High-income Asia-Pacific region. By providing annual updates of estimated data on thyroid cancer in Asia, future GBD studies will assist in elucidating the disease burden of thyroid cancer in Asia and help guide the development of strategies that are conducive to positive results. 5
In our study, the age-standardized incidence, prevalence, mortality and DALY rates of thyroid cancer in the High-income Asia-Pacific region were much higher in women than in men. This end result is very comparable to that of Zhai’s research. 20 In contrast to other study results, in some age groups in our study, mainly the elderly population, the prevalence of thyroid cancer was higher in men than in women. Women are expected to have a higher thyroid cancer burden than men, likely because women live longer than men, not because women have a higher incidence of thyroid cancer-related disability. 21 In Asia and the Pacific islands, women live longer but spend a larger percentage of their existence with disability than men. 22 A previous study in 2015 pointed out that among all cancer patients, 36.9% of Chinese cancer patients survived for at least 5 years after diagnosis, and the survival rate in female patients was much higher than that in male patients. 23 However, the combined impact of life expectancy and the prevalence of severity-weighted disability effects resulted in a higher DALY rate in females than in males in all regions. 21 In our study, we found that in the High-income Asia-Pacific region, the change in the DALY rate in men was slightly larger than that in women in some age groups. In the elderly population, men seemed to have an excessive risk of thyroid cancer. 24 Nilubol et al. 25 suggested comparable results; among the aged population, male sex appears to be strongly correlated with the risk of thyroid cancer. Men have a higher disease burden than women, especially in East Asia and the wealthy Asia-Pacific region. This may also be explained by advertisements for health check-ups and cancer screening programmes in these countries. 26 Another study noted differences in oestrogen receptor subtype expression based on thyroid cancer histological factors. 27 These findings can also explain the sex differences in disability and mortality in patients with thyroid cancer in the High-income Asia-Pacific region, especially in elderly people.
Thyroid cancer has been indicated to be a tumour with a large effect on DALYs. 14 In general, the increase in the disease burden of thyroid cancer can be explained by annual increases in the ageing population in the High-income Asia-Pacific region. The countrywide disease burden has shifted over the years from acute to persistent chronic illnesses and from younger to older individuals. 28 In recent years, studies have shown that thyroid cancer is one of the most common cancers in adolescents and young people.29,30 In addition to the effects related to ageing, the cost of living of patients diagnosed with thyroid cancer is higher than that of healthy people; associated costs include drugs, examinations, other treatment-related items and follow-ups. Moreover, the psychological impact of thyroid cancer in surviving patients has not yet been properly studied, but it is a significant burden on many patients and may have an impact on the disease burden of thyroid cancer in Asia.
In the GBD Study 2019, the High-income Asia-Pacific region included four developed countries: Japan, Singapore, Republic of Korea and Brunei Darussalam. Overall, the incidence, prevalence, mortality and DALY rates of thyroid cancer in most people in all Asian regions increased from 1990 to 2019. Consistent with Sabrina Jegerlehner’s findings, 31 the incidence of thyroid cancer has increased, but in the current study, we observed a decline in thyroid cancer-related mortality in Asia. 31 In our study, we did not observe that thyroid cancer had a relatively stable growth trend. The relatively stable mortality rate despite an increasing morbidity rate can be attributed to improvements in treatment effects. This explanation is theoretically feasible. 6
In the previous three decades, the number of humans diagnosed with thyroid cancer globally has increased dramatically.26,30,32,33 These findings show that the increase in the number of detected thyroid cancer cases is due to overdiagnosis, resulting in overtreatment. Overdiagnosis and overtreatment are harmful to some extent. The impacts of overdiagnosis may be lifelong and affect patients’ well-being, capability to obtain medical insurance, physical health and even life expectancy. 34 In the High-income Asia-Pacific region, South Korea serves as an interesting example of the harm caused by the increased disease burden due to excessive clinical examinations. 26 Kaliszewski et al. 35 summarized the increased prevalence, increased burden of disease and unnecessary life and financial burdens caused by overdiagnosis. Due to the possible harm caused by overdiagnosis, the United States has also formulated recommendations for the prevention of thyroid cancer. 31 Overdiagnosis is the most likely explanation for the increase in thyroid cancer DALYS in the High-income Asia-Pacific region. Aschebrook-Kilfoy et al. 36 found that thyroid cancer has imposed a substantial scientific and financial burden on the United States, and the economic burden of thyroid cancer in some developing countries, especially those in East Asia, has increased. In summary, regardless of whether the increasing disease burden of thyroid cancer is due to overdiagnosis, it is reasonable to develop more rational and appropriate diagnostic and treatment methods to decrease the disease burden of thyroid cancer and prevent resource waste.
It is worth noting that the mortality rate of thyroid cancer in some areas of Asia is no longer increasing despite increases in incidence rates and DALY rates. Interestingly, thyroid cancer-related mortality in the High-income Asia-Pacific region showed a slightly increasing or a stable trend during this period compared with mortality in Asia as a whole. However, the explanation for the higher mortality rate of thyroid cancer in the High-income Asia-Pacific region than in Asia as a whole cannot be explained by overdiagnosis alone 37 because in a population in which overdiagnosis occurs, appropriate treatment is also offered. Treatment affects the mortality rate of thyroid cancer; thus, this finding indicates that overdiagnosis is not the only explanation.26,37 Studies have shown that the increases in mortality rates in Japan and South Korea may have strong relationships with the increases in imaging tests for thyroid cancer in South Korea and Japan. As Shibuya et al. 37 mentioned in a study on thyroid cancer screening in Japan, thyroid cancer may be affected by radiation exposure. Other risk factors might also be related to the incidence of and mortality due to thyroid cancer, such as ageing, obesity, smoking and race. 38 Zhai’s et al. 20 study showed that developed countries had the highest proportions of deaths related to high body mass index (BMI). One study found that obesity has a greater impact on mortality than morbidity. Further research found a direct relationship between the aggressiveness and anaplasticity of thyroid cancer and obesity and diet.
Asia is the most populous continent in the world and has a vast territory. The socioeconomic conditions, political regimes and medical systems among different Asian countries vary greatly. 39 In the second half of the 20th century, the ageing population in Japan began to increase rapidly. 40 Although not all countries are ageing at the same rate (due to differences in the level and time of population transformation), the trend of population ageing is quite obvious. This is especially evident in Japan and South Korea in the High-income Asia-Pacific region. This may be one explanation for thyroid cancer mortality being more pronounced in the elderly population in the High-income Asia-Pacific region. In a paper on the incidence of thyroid cancer in Japan, Magner 41 mentioned that the healthy lifestyle of Japanese people seemed to allow many Japanese people to live to an age of above 80 years. Therefore, it is not surprising that the majority of deaths due to thyroid cancer in the High-income Asia-Pacific region occur in those above the age of 80 years. However, if a patient is not actively treated, thyroid cancer will cause abnormalities in the secretion, metabolism and function of thyroid hormones, and as people age, 42 they develop immune and age-related genetic problems; this may increase the risk of thyroid cancer-related morbidity and mortality in elderly people.
A summary of the natural history of thyroid cancer revealed that some thyroid cancers are indeed malignant but do not lead to patient death; however, macrocell carcinomas in aged patients are more aggressive since they accumulate genetic alterations after repeated proliferation over decades. 19 The countrywide disease burden has shifted over time from acute to persistent chronic illnesses and from younger to older individuals. 28 In a genetic study, Lian et al. 43 found that two ageing-related genes, tnfrsf12a and chi3l1, were novel common risk genes associated with both ageing and thyroid cancer. The survival rates in patients with thyroid cancer are widely variable and are dependent on the histotype and degree of differentiation. 44 In our study, most thyroid cancers occurred in middle-aged and elderly patients, especially in East Asia and the Asia-Pacific region. Among elderly patients, the mortality rate of thyroid cancer in people aged above 70 years gradually increased. The reason for this phenomenon has much to do with the ageing population in Asia.
Since our study did not analyze risk factors for thyroid cancer, the explanation for the significant increase in thyroid cancer in the High-income Asia-Pacific region and the reasons for the higher thyroid cancer mortality rate than that in the total Asia-Pacific region cannot be discussed. Additional studies are needed to demonstrate outcomes associated with thyroid cancer risk factors.
Conclusion
As mentioned above, the burden of thyroid cancer continues to increase due to overtreatment. In addition, stress experienced by many thyroid cancer patients leads to overtreatment. Most thyroid cancer studies have proven that thyroid cancer is one of the most serious tumours affecting DALYs14,20,45 consistent with our study. The growing incidence of thyroid cancer and increasing burden of disease seem to indicate that thyroid cancer is still a public health problem in Asia. Therefore, thyroid cancer in Asia still requires attention. Some health policy adjustments are also needed. A focused discussion on the epidemiology of thyroid cancer in Asia and the High-income Asia-Pacific region is urgently needed to moderate the increasing trend of the burden of thyroid cancer due to overdiagnosis and treatment. Moreover, the population is ageing, so epidemiological thyroid cancer data need to be adjusted accordingly. The prevalence of thyroid cancer in the High-income Asia-Pacific region was concentrated mainly in the 40–79 years age group. This age group has a notably high prevalence of thyroid cancer. Therefore, although excessive screening and other examinations are of little significance, some health policy adjustments would be meaningful. Among patients with thyroid cancer, it is still necessary to distinguish between high-risk patients who want to undergo treatment and patients who may not need treatment, and this distinction depends on the epidemiology of thyroid cancer. 18 Improvements in the medical care system and the care of elderly patients, especially elderly male patients, also deserve more attention. Moreover, we also need to consider the economic situations of developing countries and developed countries in Asia, and policies should differ according to specific situations. The main goal is to reduce medical resource waste, excessive assessments and excessive interventions for the prognosis and treatment of thyroid cancer. Targeted measures to moderate the increasing disease burden should be developed.
Footnotes
Author contributions: Yike Li: Data curation; Formal analysis; Methodology; Project administration; Software; Visualization; Writing – original draft.
Yinqiong Huang: Data curation; Investigation; Methodology; Validation; Visualization; Writing – original draft.
Xue He: Funding acquisition; Investigation; Software; Supervision; Visualization; Writing – original draft.
Cheng Han: Data curation; Formal analysis; Funding acquisition; Methodology; Supervision; Writing – review & editing.
Wei Wu: Investigation; Validation; Visualization; Writing – original draft.
Hui Shen: Data curation; Methodology; Software; Validation; Writing – original draft.
Yanbing Xu: Data curation; Investigation; Methodology; Software; Writing – original draft.
Yazhuo Liu: Conceptualization; Formal analysis; Investigation; Project administration; Resources; Supervision; Writing – review & editing.
Zizhao Zhu: Conceptualization; Formal analysis; Investigation; Software; Supervision; Validation; Writing – review & editing.
Conflict of interest statement: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by a National Natural Science Foundation of China (NSFC) grant (Grant No. 82100832) to Dr Cheng Han and a National Natural Science Foundation of China (NSFC) grant (Grant No. 82000754) to Dr Xue He.
ORCID iDs: Yinqiong Huang  https://orcid.org/0000-0001-9186-3896
https://orcid.org/0000-0001-9186-3896
Hui Shen  https://orcid.org/0000-0003-4807-9726
https://orcid.org/0000-0003-4807-9726
Yazhuo Liu  https://orcid.org/0000-0002-0311-3903
https://orcid.org/0000-0002-0311-3903
Contributor Information
Yike Li, Department of Clinical Nutrition and Metabolism, Affiliated Zhongshan Hospital of Dalian University, Dalian, China.
Yinqiong Huang, Department of Endocrinology, The Second Affiliated Hospital of Fujian Medical University, Quanzhou, China.
Xue He, Department of Laboratory Medicine, The First Affiliated Hospital of China Medical University, Shenyang, China.
Cheng Han, Department of Clinical Nutrition and Metabolism, Affiliated Zhongshan Hospital of Dalian University, Dalian, China.
Wei Wu, Department of General Surgery, The Sixth People’s Hospital of Shenyang, Shenyang, China.
Hui Shen, Department of Clinical Nutrition and Metabolism, Affiliated Zhongshan Hospital of Dalian University, Dalian, China.
Yanbing Xu, Department of Clinical Nutrition and Metabolism, Affiliated Zhongshan Hospital of Dalian University, Dalian, China.
Yazhuo Liu, Department of Clinical Nutrition and Metabolism, Affiliated Zhongshan Hospital of Dalian University, No. 6 Zhongshan District of Jiefang Route, Dalian 116001, Liaoning, China.
Zizhao Zhu, Department of General Surgery, The Sixth People’s Hospital of Shenyang, No. 85 Heping South Street, Heping District, Shenyang 110006, Liaoning, China.
References
- 1. Kent WD, Hall SF, Isotalo PA, et al. Increased incidence of differentiated thyroid carcinoma and detection of subclinical disease. CMAJ 2007; 177: 1357–1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, et al. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer 2013; 49: 1374–1403. [DOI] [PubMed] [Google Scholar]
- 3. Rahib L, Smith BD, Aizenberg R, et al. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res 2014; 74: 2913–2921. [DOI] [PubMed] [Google Scholar]
- 4. Yang BH, Parkin DM, Cai L, et al. Cancer burden and trends in the Asian Pacific Rim region. Asian Pac J Cancer Prev 2004; 5: 96–117. [PMC free article] [PubMed] [Google Scholar]
- 5. GBD 2017 Stomach Cancer Collaborators. The global, regional, and national burden of stomach cancer in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease study 2017. Lancet Gastroenterol Hepatol 2020; 5: 42–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Davies L, Welch HG. Current thyroid cancer trends in the United States. JAMA Otolaryngol Head Neck Surg 2014; 140: 317–322. [DOI] [PubMed] [Google Scholar]
- 7. Li Z, Wang L, Guan H, et al. Burden of eating disorders in China, 1990-2019: an updated systematic analysis of the global burden of disease study 2019. Front Psychiatry 2021; 12: 632418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kocarnik JM, Compton K, Dean FE, et al. Cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life years for 29 cancer groups from 2010 to 2019: a systematic analysis for the Global Burden of Disease study 2019. JAMA Oncol 2022; 8: 420–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. James SL, Abate D, Abate KH, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease study 2017. Lancet 2018; 392: 1789–1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Vos T, Abajobir AA, Abate KH, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease study 2016. Lancet 2017; 390: 1211–1259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Vos T, Lim SS, Abbafati C, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease study 2019. Lancet 2020; 396: 1204–1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Balducci L, Ershler WB. Cancer and ageing: a nexus at several levels. Nat Rev Cancer 2005; 5: 655–662. [DOI] [PubMed] [Google Scholar]
- 13. Regenstein M, Nocella K, Jewers MM, et al. The cost of residency training in teaching health centers. N Engl J Med 2016; 375: 612–614. [DOI] [PubMed] [Google Scholar]
- 14. Park JH, Lee KS, Choi KS. Burden of cancer in Korea during 2000-2020. Cancer Epidemiol 2013; 37: 353–359. [DOI] [PubMed] [Google Scholar]
- 15. Vos T, Allen C, Arora M, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease study 2015. Lancet 2016; 388: 1545–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Global Health Data Exchange https://ghdx.healthdata.org/gbd-results-tool (accessed 1 August 2019).
- 17. Pham TM, Kubo T, Fujino Y, et al. Disability-adjusted life years (DALY) for cancer in Japan in 2000. J Epidemiol 2011; 21: 309–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. La Vecchia C, Malvezzi M, Bosetti C, et al. Thyroid cancer mortality and incidence: a global overview. Int J Cancer 2015; 136: 2187–2195. [DOI] [PubMed] [Google Scholar]
- 19. Takano T. Natural history of thyroid cancer [review]. Endocr J 2017; 64: 237–244. [DOI] [PubMed] [Google Scholar]
- 20. Zhai M, Zhang D, Long J, et al. The global burden of thyroid cancer and its attributable risk factor in 195 countries and territories: a systematic analysis for the Global Burden of Disease study. Cancer Med 2021; 10: 4542–4554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Murray CJL, Lopez AD. Regional patterns of disability-free life expectancy and disability-adjusted life expectancy: Global Burden of Disease study. Lancet 1997; 349: 1347–1352. [DOI] [PubMed] [Google Scholar]
- 22. Murray CJL, Lopez AD. Global mortality, disability, and the contribution of risk factors: Global Burden of Disease study. Lancet 1997; 349: 1436–1442. [DOI] [PubMed] [Google Scholar]
- 23. Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin 2016; 66: 115–132. [DOI] [PubMed] [Google Scholar]
- 24. Rukhman N, Silverberg A. Thyroid cancer in older men. Aging Male 2011; 14: 91–98. [DOI] [PubMed] [Google Scholar]
- 25. Nilubol N, Zhang L, Kebebew E. Multivariate analysis of the relationship between male sex, disease-specific survival, and features of tumor aggressiveness in thyroid cancer of follicular cell origin. Thyroid 2013; 23: 695–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mitman G. Ebola in a stew of fear. N Engl J Med 2014; 371: 1763–1765. [DOI] [PubMed] [Google Scholar]
- 27. Rahbari R, Zhang L, Kebebew E. Thyroid cancer gender disparity. Future Oncol 2010; 6: 1771–1779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Fries JF. Aging, illness, and health policy: implications of the compression of morbidity. Perspect Biol Med 1988; 31: 407–428. [DOI] [PubMed] [Google Scholar]
- 29. Massimino M, Evans DB, Podda M, et al. Thyroid cancer in adolescents and young adults. Pediatr Blood Cancer 2018; 65: e27025. [DOI] [PubMed] [Google Scholar]
- 30. Burgess JR. Temporal trends for thyroid carcinoma in Australia: an increasing incidence of papillary thyroid carcinoma (1982-1997). Thyroid 2002; 12: 141–149. [DOI] [PubMed] [Google Scholar]
- 31. Jegerlehner S, Bulliard JL, Aujesky D, et al. Overdiagnosis and overtreatment of thyroid cancer: a population-based temporal trend study. PLoS ONE 2017; 12: e0179387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ito Y, Nikiforov YE, Schlumberger M, et al. Increasing incidence of thyroid cancer: controversies explored. Nat Rev Endocrinol 2013; 9: 178–184. [DOI] [PubMed] [Google Scholar]
- 33. Leenhardt L, Grosclaude P, Cherie-Challine L, et al. Increased incidence of thyroid carcinoma in France: a true epidemic or thyroid nodule management effects? Report from the French Thyroid Cancer Committee. Thyroid 2004; 14: 1056–1060. [DOI] [PubMed] [Google Scholar]
- 34. Welch HG, Black WC. Overdiagnosis in cancer. J Natl Cancer Inst 2010; 102: 605–613. [DOI] [PubMed] [Google Scholar]
- 35. Kaliszewski K, Diakowska D, Wojtczak B, et al. Cancer screening activity results in overdiagnosis and overtreatment of papillary thyroid cancer: a 10-year experience at a single institution. PLoS ONE 2020; 15: e0236257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Aschebrook-Kilfoy B, Schechter RB, Shih YC, et al. The clinical and economic burden of a sustained increase in thyroid cancer incidence. Cancer Epidemiol Biomarkers Prev 2013; 22: 1252–1259. [DOI] [PubMed] [Google Scholar]
- 37. Shibuya K, Gilmour S, Oshima A. Time to reconsider thyroid cancer screening in Fukushima. Lancet 2014; 383: 1883–1884. [DOI] [PubMed] [Google Scholar]
- 38. Kitahara CM, Sosa JA. The changing incidence of thyroid cancer. Nat Rev Endocrinol 2016; 12: 646–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Leung WK, Wu MS, Kakugawa Y, et al. Screening for gastric cancer in Asia: current evidence and practice. Lancet Oncol 2008; 9: 279–287. [DOI] [PubMed] [Google Scholar]
- 40. Yap MT, Thang LL, Traphagan JW. Introduction: aging in Asia – perennial concerns on support and caring for the old. J Cross Cult Gerontol 2005; 20: 257–267. [DOI] [PubMed] [Google Scholar]
- 41. Magner JA. High thyroid cancer mortality rate in Japan: a result of nonaggressive treatment strategy, or just an aging population? Thyroid 2018; 28: 818–819. [DOI] [PubMed] [Google Scholar]
- 42. Mariotti S, Franceschi C, Cossarizza A, et al. The aging thyroid. Endocr Rev 1995; 16: 686–715. [DOI] [PubMed] [Google Scholar]
- 43. Lian M, Cao H, Baranova A, et al. Aging-associated genes TNFRSF12A and CHI3L1 contribute to thyroid cancer: an evidence for the involvement of hypoxia as a driver. Oncol Lett 2020; 19: 3634–3642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Raue F, Frank-Raue K. Thyroid cancer: risk-stratified management and individualized therapy. Clin Cancer Res 2016; 22: 5012–5021. [DOI] [PubMed] [Google Scholar]
- 45. Deng Y, Li H, Wang M, et al. Global burden of thyroid cancer from 1990 to 2017. JAMA Netw Open 2020; 3: e208759. [DOI] [PMC free article] [PubMed] [Google Scholar]