Abstract
The new coronavirus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was declared a pandemic on 11 March 2020 by the World Health Organization (WHO). The impacts of COVID-19 have changed over the past year globally. There were 116 million confirmed cases of COVID-19 in more than 220 countries, including 2.5 million deaths, as reported at the end of the first week of March 2021. Throughout this time, different variants of SARS-CoV-2 have emerged. In early March, the United States of America (USA) led in both confirmed cases and casualties, while India followed in the number of confirmed cases and Brazil in the number of deaths. Vaccines are available in the USA and worldwide to help combat COVID-19. The level of preparedness among multisectoral communities played a role in transmission rates; therefore, lessons learned from past outbreaks, alongside this pandemic, are crucial in establishing policies and regulations to reduce and/or prevent the spread. This narrative literature review provides an update on the global spread of the COVID-19 outbreak, and the current impact of the pandemic 1-year after the declaration, preparedness, and mitigation efforts since the outbreak.
Keywords: COVID-19, SARS-CoV-2 variants, Global Health, pandemic, disease outbreak
Introduction
When China reported 44 cases of pneumonia to the World Health Organization (WHO) between December 31, 2019, and January 3, 2020, the causal organism was unknown. 1 A novel coronavirus (2019-nCoV) was later identified as the agent responsible for the outbreak that evolved into a global pandemic. Coronaviruses (CoV) are single-stranded positive-sense RNA viruses that belong to the Coronaviridae family. They infect a wide range of hosts, affect multiple organ systems, and cause diseases in humans extending from the common cold to more serious respiratory diseases such as severe acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS), and the current coronavirus disease 2019 (COVID-19). 2 When comparing the genome of 2019-nCoV with SARS-CoV, the International Committee on Taxonomy of Viruses (ICTV) found that both strains are related, hence the new name of 2019-nCoV, severe acute respiratory syndrome 2 (SARS-CoV-2). SARS-CoV, MERS-CoV, and SARS-CoV-2 belong to the same genus Betacoronavirus which originates from bats. 2 Even though these viruses belong to the same lineage, they are genetically distinct. SARS-CoV-2 is 79% similar to SARS-CoV and 50% like MERS-CoV. 2 Structural analysis of SARS-CoV-2 demonstrates that while it uses the same cell entry receptor, angiotensin-converting enzyme 2 (ACE2), as SARS-CoV, it has a higher binding affinity. 3 This may explain why SARS-CoV-2 is more infectious.
The first mode of transmission of SARS-CoV-2 was assumed to be animal-to-human with supplemental human-to-human propagation. This was evident in the ever-changing epicenter of the pandemic. Initially, China was the epicenter of the SARS-CoV-2 pandemic with burdensome morbidity and mortality from the disease. The virus then made its way to Europe, where Italy was severely affected by the pandemic. One-year after the declaration, the United States of America (USA) had the highest number of cases and deaths. 2 Through March 7, 2021, there were a total of 116 166 652 confirmed cases of COVID-19 and 2 582 528 deaths across more than 220 countries. 4 The number infected with the virus continues to rise each day. The recently estimated reproductive number (R0) of 2.24 to 3.58 was higher than the initial WHO R0 estimate of 1.4 to 2.5, demonstrating that the dynamics of disease transmission are complex. 2 This could be attributed to the fact that asymptomatic individuals secrete viral loads similar to those who are symptomatic. 2 Furthermore, there have been increasing reports of SARS-CoV-2 in sewage and wastewater, raising concerns about fecal-oral transmission. 2 Vertical transmission may also be a possibility, as there have been reports of high levels of SARS-CoV-2 IgM antibodies in newborns born to mothers with COVID-19; viral RNA detected in the breast milk of lactating mothers, and a newborn tested positive for SARS-CoV-2 36 hours after being born to a mother with COVID-19.5,6 Reports of virus variants have also raised concerns about changes in transmissibility. By June 2020, a new variant of SARS-CoV-2 with a mutation D614G had become the dominant strain due to its increased infectivity and transmission. 7 December 14, 2020, the United Kingdom (UK) reported a variant referred to as SARS-CoV-2 VOC 202012/01 (Variant of Concern, the year 2020, month 12, variant 01), and on 18 December 2020, South Africa announced a new variant named 501Y.V2, because of an N501Y mutation. 7 Preliminary findings suggest that both variants are associated with increased transmissibility.
The world population is committed to physical separation, the use of appropriate personal protective equipment (PPE), frequent handwashing, proper cough etiquette, and standard cleaning and disinfecting procedures to prevent the transmission of infectious respiratory droplets. To help mitigate exportation, importation, and further transmission of SARS-CoV-2, the Centers for Disease Control and Prevention (CDC) 8 has ordered that all international air passengers arriving in the USA are tested 3 days or earlier before flight departure and documentation must be presented before boarding, effective January 26, 2021. Efforts, such as vaccinations, to combat COVID-19 are in place by administering Johnson and Johnson, Pfizer-BioNTech, and Moderna, among citizens of the USA and those abroad. 9 Both Pfizer-BioNTech and Moderna employ mRNA technology to express the SARS-CoV-2 spike protein. The mRNA vaccines are more than 90% effective and protect against variants from the UK and South African. 9 USA-authorized vaccines, including Janssen’s viral vector technology, remain effective among circulating strains of COVID-19. 9 Additional vaccines from other pharmaceutical companies are expected to be approved as soon as possible. As of early March 2021, the USA has administered over 93.6 million total doses.10,11 While this is encouraging, vaccine equity is an issue. Despite mitigation methods and vaccination programs, healthcare services around the world have been overrun and are not prepared for a pandemic of this magnitude and its subsequent surges.12,13 In this narrative review, the global spread of COVID-19 is detailed and an update on the current impact 1-year after the declaration of the pandemic, preparedness, and mitigation efforts.
Methodology
An electronic literature search was performed on PubMed, Google Scholar, and MedLine Plus. The search was limited to peer-reviewed articles published from January 1, 2020, through a 1-year post-declaration of the pandemic. The articles were selected if they included keywords such as coronavirus, COVID-19, SARS-CoV-2, global outbreak, pandemic, variants, mutations, and transmissibility. The articles were then reviewed and included according to their applicability to the topic, to provide information on the global efforts made for the preparedness and mitigation of the COVID-19 pandemic aimed at combating the spread of the disease.
Global Spread, Preparedness, and Response
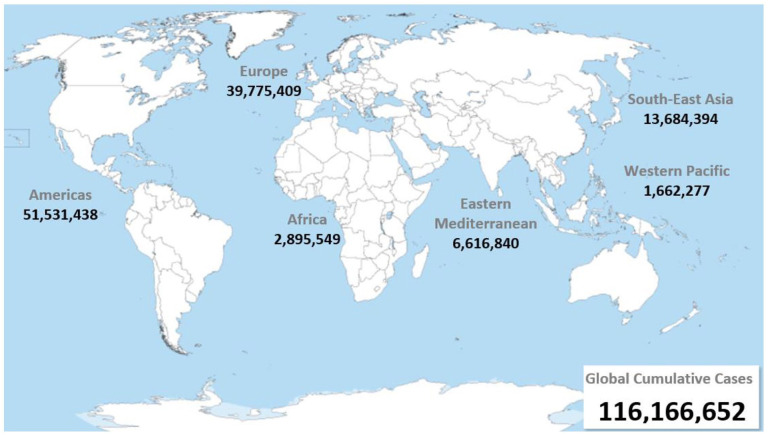
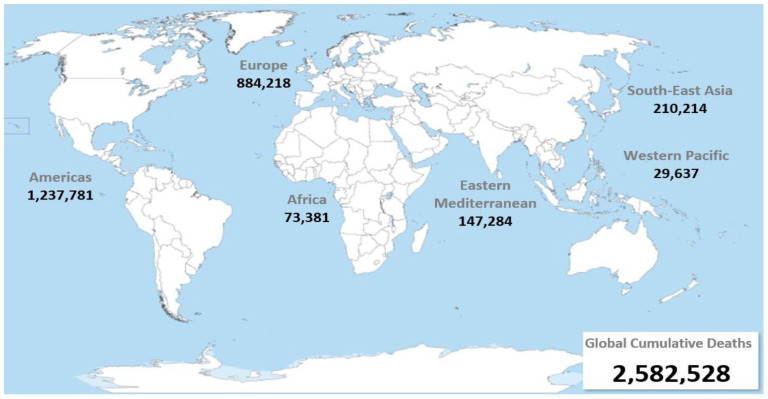
The upward trend of disease infectivity and mortality in 1-year demonstrates that more than 116 million people have been infected with the virus and more than 2 million casualties due to the continuous evolution of COVID-19.4,14,15 According to the global situation report, the countries with the highest cumulative cases are the following: the USA with 28 602 211, accounting for 25% of the world’s infected population (total 116 166 652 cases); India with 11 210 799 cases (10%); and Brazil with 10 869 227 cases (9%), as depicted in Figure 1.4,14,15 Furthermore, the countries with the highest number of deaths resulting from COVID-19 are the USA with 519 075 casualties, accounting for 20% of the total number of deaths worldwide associated with the disease (total 2 582 528 deaths); followed by Brazil with 262 770 deaths (10%); and Mexico with 189 578 deaths (7%), as depicted in Figure 2.4,14,15
Figure 1.
Global cumulative cases of COVID-19, through the end of the first week of March 2021.
Source: Data recreated using the number of confirmed cases reported by WHO. 4
Figure 2.
Global cumulative casualties of COVID-19, through the end of the first week of March 2021.
Source: Data recreated using the number of confirmed deaths reported by WHO. 4
Several factors should be considered when addressing concerns about the spread and progression of the virus and how the disease can be managed. 16 These factors consist of but are not limited to transmission types (ie, clusters of cases vs sporadic), population distributions in specific age groups, degrees of social distancing interventions, and implementation of work resumption. 17 Also, measures such as early testing and detection, social distancing, isolation practices, and healthcare responses play crucial roles in achieving the desired outcome.8,16,18-20 Personal protective measures such as the use of face masks and hand hygiene have also been included in public health guidelines.21,22 Although hand hygiene does not directly affect the transmission of the virus by respiratory droplets or aerosols, face masks have been shown to be effective in protecting others, particularly healthcare workers, from symptomatic individuals.21-23
Rampant disease transmission depends on the characteristics of the virus, the ability to spread from human to human, its severity in resulting illness, and other measures available to mitigate the impact of its destruction. 13 These additional measures may include the accessibility and effectiveness of vaccines or medications to combat the illness. 13
Italy was the first European country to be heavily hit during the first wave of this unprecedented crisis. 24 Notably, critical care treatment was severely affected in northern Italy due to a shortage of intensive care beds. 25 The failure of preparedness and effectiveness in emergency response led the Italian response team to re-evaluate the crisis from the first wave (March-May 2020) to relative stability, just before the second outbreak Italy experienced in October 2020. 24 Experiences gained from healthcare providers in this region during the pandemic can be used in establishing a response plan. 25 A study by Carenzo et al 25 suggested the following 3 interventions: (1) dedicate intensive care units (ICUs) for critically ill patients with COVID-19, (2) allocate a pre-triage facility to diagnose and isolate suspected and confirmed cases, and (3) provide adequate skills and knowledge to medical teams in managing ICU, patient management, the appropriate usage of PPE, and to be prepared to update protocols and procedures based on any disruptions that may arise.
Similarly, Daegu citizens of South Korea, experienced a large-scale outbreak during the first wave of the pandemic, particularly impacting patients who experience out-of-hospital cardiac arrest. 26 Among the interventions implemented, high-level PPE was introduced, and the standard method of cardiopulmonary resuscitation was changed to chest compressions using mechanical equipment. 26 Each of these heart patients was treated as suspected or confirmed COVID-19 cases, irrespective of their symptoms. 26 In response to the isolation of resuscitation units and the complete or partial closures of emergency centers, the number of medical personnel requiring self-isolation decreased and improved favorable outcomes for the patients. 26
Hospital preparedness, initial disease management, and surveillance of healthcare workers were explored in Tokyo, Japan. 27 Kaito et al 27 reported that each hospital should develop an incident management system for COVID-19, based on patient symptoms and/or risk history, which is then confirmed with diagnostic testing. Thus, disease management is carefully selected based on the patient’s needs. 27 The authors suggest further that contact tracking and quarantining those who have encountered COVID-19 can reduce clusters of new cases. 27
Like many other nations, Ecuador’s health system was severely overwhelmed by this pandemic and its main cause was due to limited emergency health planning responses. 12 Officials from Ecuador’s public health system learned early that it was necessary to mitigate the epidemic in the country and reduce mortality in the most vulnerable at-risk population; hence, the implementation of the WHO’s operational guideline in the strategic preparedness and response plan to COVID-19 served as a reference point in combating the outbreak. 12 It was noted that a country’s legislative capacity and government authority had control in addressing the social, economic, and health consequences related to the COVID-19 outbreak, as seen in the response to the pandemic. 28
The challenges faced by sub–Saharan African countries (SSA) to control the spread of COVID-19 waves of infection include the lack of adequate resources and technology to effectively follow contact tracing, the dilemma of implementing lockdowns, and the impact of fake news. Other challenges are technical and capacity elements of testing, treatment, and the development and access to vaccines. 29 Lagos State in central Nigeria was the epicenter of the 2014 Ebola outbreak, as well as the main location for the COVID-19 epidemic. 30 Hence, the emergency preparedness lessons learned from the Ebola outbreak were used to guide COVID-19 from vastly spreading. 30 It is important to take note that public health interventions implemented in several African countries to lessen the gaps and control disease outbreaks, such as Ebola, may have strengthened the response in containing the current pandemic. 31 Zhang et al 32 explored the association between health care preparedness and the government response during the first and second COVID-19 waves that rolled through the African region. Initial cases were first detected in countries with urban populations, greater international travel, and those with better capability in diagnostic testing equipment. 32 Even those countries rated to have better preparedness with more resilient health care systems were affected by the pandemic 32 Moreover, predictors for the second wave were comparable to that of the first wave in the African region. 32 The first wave per capita mortality rate was greater in urban communities, in areas receiving foreign travel, and among those with the prevalence of human immunodeficiency virus (HIV). 31 Overall, African countries were reported to have seen lower infection and mortality rates than most countries in the Americas Europe, and Asia due to factors such as low rate of testing, poor documentation of the cause of death, younger age population, good vitamin D status from exposure to sunlight, cross-immunity from other viruses including coronaviruses, and lessons learned from other infectious diseases such as HIV and Ebola. 33 Thus, having a strategic guide to emergency preparedness and response is crucial for an improved outcome, as depicted in Table 1. 34
Table 1.
Strategic preparedness and response guide.
| WHO pillars | Actions |
|---|---|
| 1: Coordination, Planning, Financing, and Monitoring | Foundation for operational alignment throughout all pillars that allows for real-time actions and corrections for decision-making at a country, city, and community level. |
| 2: Risk Communication, Community Engagement, and Infodemic Management | Listening to whole communities and addressing health service barriers play a role in mitigating the impact of COVID-19. |
| 3: Surveillance, Epidemiological Investigation, Contact Tracing, and Adjustment of Public Health and Social Measures | Increasing testing capacities with efficient diagnostic equipment is imperative to stop the spread, along with sustained quarantine efforts and case investigation. |
| 4: Points of Entry, International Travel and Transport, and Mass Gatherings | Risk mitigation is key, and action includes but is not limited to self-monitoring, and surveillance at entry points with case-to-case management. |
| 5: Laboratories and Diagnostics | Investigations can only commence after testing has been conducted. Cost-effective strategies should be put in place to detect variants of concern through screening, sequencing, and sharing pertinent data amongst nations. |
| 6: Infection Prevention and Control, and Protection of the Health Workforce | Prevention is essential when combating COVID-19. Maintenance of essential health services and protection of healthcare workers are needed. |
| 7: Case Management, Clinical Operations, and Therapeutics | Countries should have access to multidisciplinary guidance and guidelines to maintain essential healthcare services at all levels of concern. |
| 8: Operational Support and Logistics, and Supply Chains | Supply chains must be able to meet supply and demand patterns to avoid shortages of medical and health products/services. |
| 9: Maintaining Essential Health Services and Systems | Strengthening essential public health functions and long-term health systems in a whole community takes prioritization in tackling demand and supply barriers. |
| 10: Vaccination | Availability, accessibility, and deployment of safe and effective vaccines are powerful tools to combat the pandemic. |
Data reproduced from the WHO, as of February 2021. 34
The common goal among the global population is to reduce the spread and the burden of COVID-19, and aid in the protection of those at high risk for severe illness8,10; therefore, continuous efforts are needed with an emphasis on public education.
Discussion
Since December 2019, there have been multiple global initiatives to slow the spread of COVID-19. 16 The rate of transmission, the containment methods, the number of infected individuals, and the death rates varied and fluctuated between different countries. Due to the initial outbreak and the surge of infected individuals in affected countries, initial approaches to slowing the spread of the coronavirus were aimed at maintaining or decreasing the demand for hospital and critical care beds.35,36 Also, some institutions, like the USA government, have included free testing and employment rights as part of their policy, requiring that potentially exposed individuals stay at home for at least 14 days, with possible paid sick leave. 37
Although, at the beginning of the pandemic, the WHO did not recommend the use of travel bans to control SARS-CoV-2 based on considerations under the 2005 International Health Regulations (IHR) which has thus resulted in the slow response of some countries at the onset of the outbreak. However, countries like New Zealand, Australia, and Taiwan, which do not have porous land borders, have been able to use travel restrictions to slow incoming cases and enable quarantine and contact tracing. Therefore, allowing them to approach the elimination of the disease repeatedly. 38
The WHO has identified multiple variants of SARS-CoV-2 as a concern. In late January 2020, a variant of SARS-CoV-2 with a substitution for D614G emerged and replaced the initial strain that was identified in China. 7 Although this strain has not been shown to cause severe illness or have any effect on diagnostics, therapeutics, drug therapies, and public health preventive measures compared to the initial strain, it has demonstrated increased infectivity and transmission. 7 In December 2020, another variant with 23 nucleotide substitutions was identified in the UK, known as VOC 202012/01 or B.1.1.7. 39 Preliminary clinical findings also suggested that the strain B.1.1.7 has increased transmissibility; however, the analysis also indicated that there was no change in disease severity or recurrence of infection between the groups of CoVs that share an inherited set of distinctive mutations known as a variant.7,39 Furthermore, an increase in the number of deaths in January 2021 is associated with the B.1.1.7 variant. 39
Another worrying variant of SARS-CoV-2 was detected in South Africa and has spread rapidly to 3 provinces, known as 20H/501Y.V2 or B.1.351. 39 This mutation has been found to specifically affect the performance of polymerase chain reaction (PCR) assays with an S gene target. 7 However, most PCR assays used globally utilize multiple targets, thus making the impact of variants on diagnostics insignificant. 7 At this stage, there is no evidence that these new variants are associated with severe disease or worsening outcomes. 7 A variant isolate of E484K belonging to B.1.1.248 also known as 501.V3 or P.1, was reported in the first week of 2021 in Brazil.40,41 Other variants of concern include B.1.617, named the “Delta variant,” which is the predominant variant in India identified in October 2020 and responsible for the spread of deadly cases in the western state of Maharashtra. 41 It is vastly spreading in the UK, USA, and other locations. Another variant is found to be spreading in Bengal, B.1.618, also known as “triple mutant,” which is suspected to have evolved from B.1.617. 41 In addition, new variants discovered in the USA have been detected in California and have been reported in numerous states, including B.1.526 (lota), which has been spreading at an alarming rate in New York City since November 2020. 41
Therefore, the global circulation of the SARS-CoV-2 variants has expressed the need for local actions to slow the transmission with social control measures that are known to be effective in reducing transmissions such as reducing social contacts, effective testing and tracking, robust outbreak identification, and control, support to ensure effective isolation and quarantine, and population vaccination. In addition, public education about certain locations and behaviors in the community that is linked to a high risk transmission, as well as the continuing use of mitigation measures that will be required even after vaccination, are also necessary. 38 Furthermore, enhanced mitigation measures could be required based on the level of local community transmissions such as reinforcing the need for face coverings in all indoor public spaces, schools, workplaces, and crowded outdoor spaces; temporary closure of non-essential indoor spaces, where face coverings cannot be worn; increasing the distance on the 2 m (6 ft) rule; improving indoor ventilation, and addressing socioeconomic inequalities that are the major cause of community transmission in many countries. 38
In December 2020, the USA Food and Drug Administration (FDA) approved Moderna mRNA-1273 and Pfizer/BioNTech BNT162 vaccines for emergency use authorization (EUA).42,43 The vaccines are lipid nanoparticle-encapsulated mRNA and encode the perfusion-stabilized spike protein of the SARS-CoV-2. 43 Due to the similarities in the spike proteins of the SARS-CoV-2 variants, the efficacy of the vaccines remain unaffected, and will also target these variants. 43 Johnson and Johnson’s AD26/Janssen COVID-19 viral vector vaccine was granted EUA on 27 February 2021, as the third manufacturer available in the USA with more than 66% effectiveness in combating COVID-19.9,42,44 Likewise, since the declaration of the pandemic, several therapeutic agents, including antivirals that could potentially be repurposed or developed into effective interventions for COVID-19 infection, have undergone trials and some are still undergoing trial.45,46 Thus, physicians have more treatment options for patients hospitalized for COVID-19 1-year after the declaration of the pandemic with drugs that can speed up the recovery process and few that can improve survival.
The response to the COVID-19 pandemic is constantly evolving and many nations have been exposed to severe limitations in managing such an outbreak of this magnitude. 47 The WHO and the IHR Committee have fundamentally revised and will continue to update their protocols to minimize the gaps in global governance. 47 Moreover, most countries still do not yet have an IHR core health system capacity to detect and alert the global community about novel outbreaks. 47 Correspondingly, a country’s success in controlling the COVID-19 pandemic varies based on political and economic status, cultural and social needs, demographic and geographic resources, and the nation’s policy orientation. 48 In SSA, where the poverty rate is high and many people live in overcrowded slums, African cultural norms and daily social life activities hinder the control of Covid-19 in addition to the difficulty in implementing behavioral practices that are required to manage COVID-19, such as maintaining a social distance of at least 1 m and frequent handwashing. 29 Furthermore, government strategies as well as law and order, have been demonstrated in Sweden to have an impact on the spread of the pandemic. 49
An urgent need to guide communities is necessary to recover from this unprecedented outbreak. 50 Of utter significance, providing support and celebrating success, developing clear guidelines, preparing for future emergencies, reevaluating priorities, maximizing performance, sustaining learning and communication, and periodic consultation with public health officials and leaders across all platforms is crucial to provide integrated care during an outbreak. 50 For SSA countries, international coordination is critical to strengthening the health system and coordinated intra African collaboration. 38
Addressing advanced care planning and engaging in communication with patients’ families proved to be a struggle during these unprecedented times. 51 Digital interventions through remote monitoring and training could offer many opportunities to strengthen the health care system; in addition, offering home diagnostic and screening equipment to minimize the spread of this communicable disease. 52
In some countries, long-term care facilities, nursing homes, and home health care agencies experienced a higher incidence of cases of COVID-19, of which these residents were more likely to be hospitalized and die.53-55 More than half of the nursing homes across the USA had separate plans to combat this disaster, but all plans focused on training staff, restricting visitors and outside consultants, implementing policies regarding sick employees, and guidance on this evolutionary outbreak. 54 Most facilities even had policies to identify visitors and maintaining a clear line of communication and relationship with local hospitals and public health officials. 54 Data reproduced by Quigley et al 54 identified that 66% or two-thirds of nursing homes reported having access to COVID-19 tests, 100% of those tests allocated for patients and 53% for employees. However, 72% or three-fourths reported inadequate supplies (ie, N-95 respirators, alcohol-based sanitizer, gowns, face guards, surgical masks, and gloves). 54 Furthermore, 83% or five-sixths expected employee shortages. 54 The consensus among nursing home management teams was their concern for lack of supplies (43%), staff shortage (34%), and the safety of their patients (14%), indicating that emergency preparedness strategies need to be continuously refined. 54 Similarly, home health care agencies across the USA faced challenges caring for the vulnerable patient population during this pandemic. 55 The majority of these agencies had their emergency preparedness plan (76%); allocating an employee in charge of outbreak preparedness (84%) and providing employees with continuous education and training as the disease evolved (97%). 55
Conclusion
Globally, nations have faced many challenges to respond to the pandemic, due to shortages of PPE and disinfectants; as well as the general public’s lack of perception of the risks posed by communicable diseases, such as COVID-19. Lessons learned from past and present outbreaks should be shared globally to help nations identify best practices to combat such resilient disease(s). Changes in PPE strategies and the introduction of isolated resuscitation units narrowed the gap between infection and mortality rates. Implementing policies and regulations have helped reduce and/or prevent the spread of the pathogen among communities and health care facilities. In addition, appropriate education for all communities, particularly those that suffer from inequalities, is a strategy to promote appropriate behavioral changes and improve risk management. Furthermore, it is crucial to stay ahead of this ever-changing communicable disease by using diagnostics quickly, keeping track of variants of concern, and administering management and therapeutic approaches to those at risk.
Footnotes
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: All authors contributed substantially to the conception, drafting, and final approval of the manuscript.
ORCID iD: Gideon Dzando  https://orcid.org/0000-0001-8852-7680
https://orcid.org/0000-0001-8852-7680
References
- 1. Hasöksüz M, Kiliç S, Saraç F. Coronaviruses and SARS-COV-2. Turk J Med Sci. 2020;50:549-556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dhama K, Khan S, Tiwari R, et al. Coronavirus disease 2019–COVID-19. Clin Microbiol Rev. 2020;33:e00028-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Quan C, Li C, Ma H, Li Y, Zhang H. Immunopathogenesis of coronavirus-induced acute respiratory distress syndrome (ARDS): potential infection-associated hemophagocytic lymphohistiocytosis. Clin Microbiol Rev. 2020;34:e00074-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. WHO. Coronavirus disease (COVID-19) dashboard. March 10, 2021. Accessed March 9, 2021. https://www.who.int/publications/m/item/weekly-epidemiological-update—10-march-2021
- 5. Mukhra R, Krishan K, Kanchan T. Possible modes of transmission of novel coronavirus SARS-CoV-2: a review. Acta Biomed. 2020;91:e2020036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wang Y, Wang Y, Chen Y, Qin Q. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J Med Virol. 2020;92:568-576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. WHO. SARS-CoV-2 variants. December 31, 2020. Accessed March 10, 2021. https://www.who.int/emergencies/disease-outbreak-news/item/2020-DON305
- 8. CDC. Requirement for proof of negative COVID-19 test or recovery from COVID-19 for all air passengers arriving in the United States. Centers for Disease Control and Prevention. 2021. Accessed February 12, 2021. https://www.cdc.gov/coronavirus/2019-ncov/travelers/testing-international-air-travelers.html
- 9. FDA. Learn more about COVID-19 vaccines from the FDA. 2021. Accessed March 9, 2021. https://www.fda.gov/consumers/consumer-updates/learn-more-about-covid-19-vaccines-fda
- 10. CDC. COVID-19 vaccinations in the United States. 2021. Accessed March 10, 2021. https://covid.cdc.gov/covid-data-tracker/#vaccinations
- 11. AJMC Staff. Timeline of COVID-19 vaccine development in 2021. 2021. Accessed March 10, 2021. https://www.ajmc.com/view/a-timeline-of-covid-19-vaccine-developments-in-2021
- 12. Alava JJ, Guevara A. A critical narrative of Ecuador’s preparedness and response to the COVID-19 pandemic. Public Health Pract. 2021;2:100127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cvetković VM, Nikolić N, Radovanović Nenadić U, Öcal A, Noji EK, Zečević M. Preparedness and preventive behaviors for a pandemic disaster caused by COVID-19 in Serbia. Int J Environ Res Public Health. 2020;17:4124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Worldmeter. COVID-19 coronavirus pandemic. 2021. Accessed March 10, 2021. https://www.worldometers.info/coronavirus/
- 15. JHU. COVID-19 dashboard by the center for systems science and engineering (CSSE) at Johns Hopkins. 2021. Accessed March 9, 2021. https://coronavirus.jhu.edu/map.html
- 16. Sanyaolu A, Okorie C, Hosein Z, et al. Global pandemicity of COVID-19: situation report as of June 9, 2020. Infect Dis Res Treat. 2021;14:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Liu Y, Gu Z, Xia S, et al. What are the underlying transmission patterns of COVID-19 outbreak? An age-specific social contact characterization. Lancet. 2020;22:100354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. WHO. WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020. March 11, 2020. Accessed February 15, 2021. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020
- 19. Cavallo JJ, Donoho DA, Forman HP. Hospital capacity and operations in the coronavirus disease 2019 (COVID-19) pandemic—planning for the Nth patient. JAMA Health Forum. 2020;1:e200345. [DOI] [PubMed] [Google Scholar]
- 20. Le NK, Le AV, Parikh J, et al. Ecological and health infrastructure factors affecting the transmission and mortality of COVID-19. J Adv Virol Res. 2021;1:101. [Google Scholar]
- 21. Cowling BJ, Aiello AE. Public health measures to slow community spread of coronavirus disease 2019. J Infect Dis. 2020;221:1749-1751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Karaivanov A, En Lu S, Shigeoka H, et al. Face masks, public policies and slowing the spread of COVID-19: evidence from Canada. 2020. Accessed February 15, 2021. https://www.nber.org/system/files/working_papers/w27891/w27891.pdf [DOI] [PMC free article] [PubMed]
- 23. Lotfi M, Hamblin MR, Rezaei N. COVID-19: transmission, prevention, and potential therapeutic opportunities. Clin Chim Acta. 2020;508:254-266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bosa I, Castelli A, Castelli M, et al. Response to COVID-19: was Italy (un)prepared? Health Econ Policy Law. 2022;17:1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Carenzo L, Costantini E, Greco M, et al. Hospital surge capacity in a tertiary emergency referral centre during the COVID-19 outbreak in Italy. Anaesthesia. 2020;75:928-934. [DOI] [PubMed] [Google Scholar]
- 26. Cho JW, Jung H, Lee MJ, et al. Preparedness of personal protective equipment and implementation of new CPR strategies for patients with out-of-hospital cardiac arrest in the COVID-19 era. Resusc Plus. 2020;3:100015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kaito D, Matsumura K, Yamamoto R. Hospital preparedness for COVID-19: the known and the known unknown. Keio J Med. 2021;70:25-34. [DOI] [PubMed] [Google Scholar]
- 28. Srikanth Reddy K, Kumar Chattu V, Wilson K. Canada’s legal preparedness against the COVID-19 pandemic: a scoping review of federal laws and regulations. Can Public Adm. 2021;64:458-484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Agwanda B, Dagba G, Opoku P, Amankwa MO, Nyadera IN. Sub-Sahara Africa and the COVID-19 pandemic: reflecting on challenges and recovery opportunities. J Dev Soc. 2021;37:502-524. [Google Scholar]
- 30. Abayomi A, Balogun MR, Bankole M, et al. From Ebola to COVID-19: emergency preparedness and response plans and actions in Lagos, Nigeria. Global Health. 2021;17:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Umviligihozo G, Mupfumi L, Sonela N, et al. Sub-Saharan Africa preparedness and response to the COVID-19 pandemic: a perspective of early career African scientists. Wellcome Open Res. 2020;5:163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Zhang F, Karamagi H, Nsenga N, et al. Predictors of COVID-19 epidemics in countries of the World Health Organization African region. Nat Med. 2021;27:2041-2047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Okonji EF, Okonji OC, Mukumbang FC, Van Wyk B. Understanding varying COVID-19 mortality rates reported in Africa compared to Europe, Americas, and Asia. Trop Med Int Health. 2021;26:716-719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. WHO. COVID-19 strategic preparedness and response plan. February 1, 2021. Accessed March 10, 2021. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/strategies-and-plans
- 35. Shoukat A, Wells CR, Langley JM, Singer BH, Galvani AP, Moghadas SM. Projecting demand for critical care beds during COVID-19 outbreaks in Canada. Can Med Assoc J. 2020;192:E489-E496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Sahu K, Kumar R. Preventive and treatment strategies of COVID-19: from community to clinical trials. J Fam Med Prim Care. 2020;9:2149-2157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Berger ZD, Evans NG, Phelan AL, Silverman RD. COVID-19: control measures must be equitable and inclusive. BMJ. 2020;368:m1141. [DOI] [PubMed] [Google Scholar]
- 38. Grubaugh ND, Hodcroft EB, Fauver JR, Phelan AL, Cevik M. Public health actions to control new SARS-CoV-2 variants. Cell. 2021;184:1127-1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. CDC. COVID-19: emerging SARS-CoV-2 variants. 2021. Accessed February 15, 2021. https://www.cdc.gov/coronavirus/2019-ncov/more/science-and-research/scientific-brief-emerging-variants.html
- 40. NIID. Brief report: new variant strain of SARS-CoV-2 identified in travelers from Brazil. January 12, 2021. Accessed February 15, 2021. https://www.niid.go.jp/niid/en/2019-ncov-e/10108-covid19-33-en.html
- 41. Sanyaolu A, Okorie C, Marinkovic A, et al. The emerging SARS-CoV-2 variants of concern. Ther Adv Infect Dis. 2021;8:20499361211024372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. FDA. FDA issues emergency use authorization for third COVID-19 vaccine: action advances fight against COVID-19, follows comprehensive evaluation of available safety, effectiveness, and manufacturing quality information by FDA career scientists. 2021. Accessed March 10, 2021. https://www.fda.gov/news-events/press-announcements/fda-issues-emergency-use-authorization-third-covid-19-vaccine
- 43. Baden LB, El Sahly HM, Essink B, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2020;384:403-416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. CDC. Johnson & Johnson’s Janssen. 2021. Accessed March 10, 2021. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/different-vaccines/janssen.html
- 45. Chilamakuri R, Agarwal S. COVID-19: characteristics and therapeutics. Cells. 2021;10:206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Siddique R, Bai Q, Shereen MA, et al. Evidence and speculations: vaccines and therapeutic options for COVID-19 pandemic. Hum Vaccin Immunother. 2021;17:1113-1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Gostin LO, Halabi SF, Klock KA. An international agreement on pandemic prevention and preparedness. JAMA. 2021;326:1257-1258. [DOI] [PubMed] [Google Scholar]
- 48. Hendrix CS. The political economy of pandemic preparedness and effectiveness. 2021. Accessed August 15, 2021. https://www.piie.com/publications/working-papers/political-economy-pandemic-preparedness-and-effectiveness?gclid=CjwKCAjwtfqKBhBoEiwAZuesiK9A2olunmxT8bdQcoac63QZfzgQdaj9l7J8G_oCEtOhydAAuJaWVhoCa58QAvD_BwE
- 49. Hassan MS, Al Halbusi H, Razali A, et al. The Swedish Gamble and the battle to combat the COVID-19 pandemic: evidence from the Field. September 18, 2020. PREPRINT (Version 1) available at Research Square. 10.21203/rs.3.rs-78258/v1 [DOI]
- 50. Geerts JM, Kinnair D, Taheri P, et al. Guidance for health care leaders during the recovery stage of the COVID-19 pandemic: a consensus statement. JAMA Netw Open. 2021;4:e2120295. [DOI] [PubMed] [Google Scholar]
- 51. Liberman T, Roofeh R, Chin J, et al. Remote advance care planning in the emergency department during COVID-19 disaster: program development and initial evaluation. J Emerg Nurs. 2022;48:22-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Mahmood S, Hasan K, Colder Carras M, Labrique A. Global preparedness against COVID-19: we must leverage the power of digital health. JMIR Public Health Surveill. 2020;6:e18980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Resciniti NV, Fuller M, Sellner J, Lohman MC. COVID-19 incidence and mortality among long-term care facility residents and staff in South Carolina. J Am Med Dir Assoc. 2021;22:2026-2031.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Quigley DD, Dick A, Agarwal M, Jones KM, Mody L, Stone PW. COVID-19 preparedness in nursing homes in the midst of the pandemic. J Am Geriatr Soc. 2020;68:1164-1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Shang J, Chastain AM, Perera UGE, et al. Covid-19 preparedness in US home health care agencies. J Am Med Dir Assoc. 2020;21:924-927. [DOI] [PMC free article] [PubMed] [Google Scholar]