Abstract
Background:
Questions remain regarding the traditional protocols used in rehabilitation and clearance for return to sports after anterior cruciate ligament reconstruction (ACLR).
Purpose/Hypothesis:
To investigate the impact on injury rates after return to sports by developing and validating a Safer Return to Play Following ACL Reconstruction Checklist consisting of subjective and objective functional tests that can be quickly and easily implemented into a sports medicine practice. It was hypothesized that patients who successfully passed the checklist before returning to sports would experience lower rates of ipsilateral and contralateral knee injuries at a 2-year follow-up as compared with patients who returned to play before completing the checklist.
Study Design:
Cohort study; Level of evidence, 2.
Methods:
First, a systematic review was performed to generate a list of the most common outcome measures used to assess return to play after ACLR. To refine our checklist, we conducted a survey with an expert panel of 10 medical professionals utilizing the Delphi technique. After the creation of the checklist, validation was performed by prospectively evaluating patients who had undergone ACLR for injury of the ipsilateral or contralateral knee, with a minimum 2-year follow-up.
Results:
After our systematic review of 60 studies, 7 criteria were included in the final checklist. During the period studied, October 2014 to December 2017, a total of 222 patients met the inclusion criteria and were enrolled in the study. At a minimum 2 years of follow-up, there were 146 patients who successfully passed the checklist and 38 who did not. Overall, 24 (16.4%) patients who had passed the checklist sustained an injury to either knee, as compared with 10 (26.3%) from the group that did not pass the checklist (P = .162). Of the group that passed the checklist, 8 (5.5%) patients sustained an injury to the ipsilateral knee, as compared with 7 (18.4%) in the group that did not pass (P = .017).
Conclusion:
Prospective validation of our checklist demonstrated that patients who successfully passed the checklist before returning to play experienced a significantly lower incidence of ipsilateral anterior cruciate ligament injury as compared with patients who did not pass the checklist.
Keywords: knee, anterior cruciate ligament, return to sport, physical therapy, reinjury, injury prevention
Anterior cruciate ligament reconstruction (ACLR) is among the most common orthopaedic surgical procedures performed, with nearly 250,000 procedures annually in the United States alone. 4,17 In 2006, the annual incidence of ACLR in the United States was 43.48 per 100,000 individuals, approximately 130,000 in total. 30 Greater than 60% of these were in individuals <30 years of age. 29 Anterior cruciate ligament (ACL) injuries are commonly a result of jumping, pivoting, and decelerating movements and therefore are common among young athletes. While nonoperative management is an option, surgery is indicated in young and active patients to maximize the potential to return to competitive sport participation and reduce the risk of subsequent meniscal injury. 12,14,15,38
Many patients who undergo reconstruction are athletes who seek return to some level of competitive sport. However, rates of retear in addition to meniscal and contralateral knee injuries in the years after ACLR have been reported at approximately 30%, with an incidence of graft retear 8% to 17% and contralateral ACL tear as high as 24%. 24,25,37 Compounding the problem, reoperation after graft retear has been associated with less favorable outcomes than primary reconstruction. 39 Previous literature has shown that after revision surgery, <60% of patients were capable of returning to their preinjury levels of activity. 1,5 Many studies have sought to identify factors that influence the risk of failure after ACLR. 13,26 –28 Csintalan et al 13 reported risk factors for subsequent operations: previous meniscal repair, allograft use, female sex, and previous surgery.
Further research into the mechanics underlying knee injury after ACLR has identified several strength and movement deficiencies that can influence the risk of ipsilateral and contralateral knee injury. 21 These observed weaknesses in individuals after ACLR are similar to those in patients recorded at the time of injury. 7,22 In response, investigators have questioned the traditional protocols used in rehabilitation and clearance to return to sports. 3,20,33 Criteria used to assess readiness to return to play (RTP) after ACLR have traditionally included time from surgery and occasionally 1 or 2 objective criteria, such as isokinetic quadriceps/hamstring strength or thigh circumference. 2,3 Several studies have proposed that these historical measures are insufficient to adequately evaluate readiness for RTP. 19,31 With current protocols, individuals may be cleared for full activity despite strength and neuromuscular deficiencies that predispose them to knee injury. 2,4,33 Therefore, there is a need for more precise criteria, such as functional and dynamic testing, to better assess the complex kinematics and neuromuscular control required for return to high-level athletic competition. 4,20,35,40 The anticipation is that such a checklist consisting of subjective and objective criteria could help define which patients might be at risk of returning too soon after surgery. The ultimate goal of the checklist would be to reduce the risk of ipsilateral and contralateral knee injury after ACLR and help athletes with targeted therapy modalities to achieve better chances of successful RTP.
The purpose of this study was to develop and validate a checklist of subjective and objective functional tests that can quickly and easily be implemented into a sports medicine practice. We sought to more adequately identify individuals who may be at a greater risk for injury as a result of deficiencies in strength, mobility, balance, and other neuromuscular metrics. We hypothesized that patients who successfully passed the checklist before returning to sports would experience lower rates of ipsilateral and contralateral knee injury at a 2-year follow-up as compared with patients who returned to sports before passing the checklist.
Methods
Identification of Studies for Inclusion in the Systematic Review
We initially identified and reviewed all published objective measures used to assess RTP after ACLR. Results of the systematic review were used to generate a list of the most common outcome measures used to assess RTP. The full description of how our systematic review was performed using PRISMA methodology, as well as a list of the included articles, is outlined in Supplemental Material 1.
Expert Panel
To refine our checklist, we conducted a survey with an expert panel of 10 medical professionals using a Delphi technique. 23 Criteria for inclusion in the panel were expert level knowledge in rehabilitation after ACLR for a minimum of 10 years. For surgeons, sports medicine fellowship training and a minimum of 75 ACLRs per year were the minimum requirements, and physical therapists were required to treat at least 100 patients after ACLR per year. Our panel consisted of 8 fellowship-trained sports medicine orthopaedic surgeons and 2 physical therapists. The panelists were surveyed regarding several measures that were identified through our systematic review and about functional testing that had been used in our RTP protocols. These tests include the Functional Movement Screen, 10,11 Pro Agility, 32,41,42 and an internally generated quality-of-movement assessment that objectively scores 5 aspects of biomechanics during hop testing and a 12-inch (30.5 cm) box jump: hip stability, shock absorption, hip strategy, pelvic stability, and trunk stability.
The Functional Movement Screen analyzes 7 movement patterns based on grading from 0 to 21, with 21 representing full marks. 8 Scores <14 have been shown to be indicative of knee instability and predictive for future injury. 36
Jump analysis testing such as the Landing Error Scoring System measures the quality of an individual’s movements through a jump-landing task with a score ranging from 0 to 17. Suboptimal movement patterns are noted, such as inadequate knee flexion or valgus collapse. A score of 0 represents a perfect and symmetric landing. 6
The panel was asked at how many months it typically recommended until release to unrestricted RTP. Additionally, panelists were asked to grade the significance of 12 parameters in determining RTP on a Likert scale (1-5, with 5 indicating most important). The panel was instructed to consider importance for RTP and ease of implementation in the clinic when ranking. Parameters included clinically acceptable range of motion (ROM), isokinetic strength measurement, lack of effusion, lack of pain, lack of instability, KT-1000 arthrometer side-to-side laxity comparison, thigh circumference difference, International Knee Documentation Committee (IKDC) score, 9 and 4 dynamic functional tests used to further evaluate an athlete’s risk of reinjury: hop tests, the Functional Movement Screen, 10,11 our movement assessment, and the Pro Agility test. 32,41,42 The experts were asked to consider clinical experience, published literature, and practicality to generate their grades for each RTP parameter. Scores were aggregated for each measure and used to supplement the results of the systematic review in the generation of the checklist.
Data Synthesis and Checklist Generation
The results from our systematic review and expert panel were compared in an attempt to determine which measures were most important in determining RTP. Using our review, we looked for a clear consensus among studies. Outcome measures were ranked by frequency of evaluation and stratified by threshold for RTP. Similarly, our survey was used to identify the parameters voted most important in determining RTP by experts. Both modalities were combined to generate a list of measures deemed most important by the literature and the experts. Those included in the final checklist must have shown either frequent use in the published literature or high utility as assessed by our panel. When conflicts emerged, inclusion decisions were weighed by ease of assessment, utility of the test, and function within the context of other measures.
Prospective Evaluation
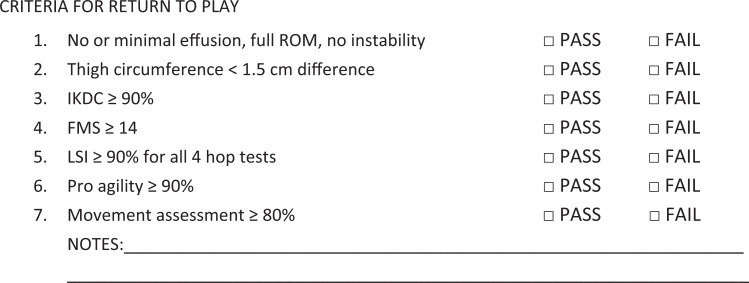
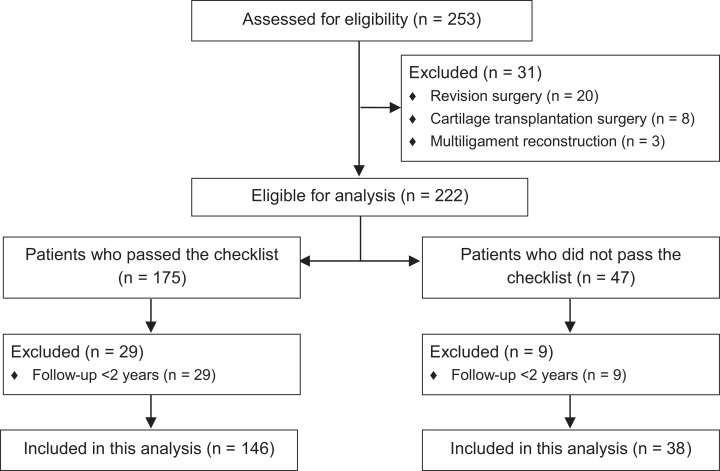
Institutional review board approval was obtained for this study. Between October 1, 2014, and December 31, 2017, patients who underwent ACLR by multiple surgeons at a single institution and who consented to participate were prospectively enrolled into this study. There were 222 patients who met the inclusion criteria and agreed to participate. All patients between the ages of 15 and 35 years who underwent primary ACLR were evaluated using the RTP checklist after their surgery (Figure 1; the full checklist is available in Supplemental Material 2). Patients were excluded from our study if they underwent multiligament reconstruction or revision ACLR or if the ACLR procedure was being performed in conjunction with a cartilage transplantation surgery (matrix-induced autologous chondrocyte implantation, osteochondral autograft transfer system, osteochondral allograft transplantation) (Figure 2).
Figure 1.
Return-to-play checklist. FMS, Functional Movement Screen; IKDC, International Knee Documentation Committee; LSI, Limb Symmetry Index; ROM, range of motion.
Figure 2.
Patient flowchart.
A patient must have passed at least 6 of the 7 checklist criteria to be cleared to return to one’s preinjury level of activity. Patients who did not pass the checklist were instructed to work on their nonpassing areas for 4 to 6 weeks and then retake the test to obtain a passing grade before returning to play.
Patients were observed for 2 years after surgery to determine the primary outcome of injury to the ipsilateral and/or contralateral knee. Injury after surgery to the ipsilateral and/or contralateral knee was determined via physical examination and magnetic resonance imaging. Patients were also assessed on their ability to RTP, level of RTP, and the IKDC outcome questionnaire. The final scores were tallied by a single researcher and compared with previously reported outcomes in the literature of patients who returned to play based on clinical judgment alone. 43
Statistical Analysis
Continuous variable data were reported as means with standard deviations and categorical data as frequencies with percentages. The Shapiro-Wilk test was used to determine whether data were normally distributed. Continuous variables compared between groups were assessed with the Student t test for parametric data and the Mann-Whitney U test for nonparametric data, while categorical variables between ≥2 groups were assessed with the Fisher exact or chi-square analysis. Multivariate logistic regression was performed using any reinjury as the dependent outcome to see if any factors were potential predictors of reinjury. Statistical significance was set at P < .05. All statistical analyses were performed with SPSS Statistics Software Version 26 (IBM).
Results
Systematic Review
Initial literature searches yielded 5332 results, from which 432 articles were selected based on title for further investigation. Sixty studies specified at least 1 objective measure to allow RTP after ACLR (Supplemental Material 1). Of the 60 studies, 49 (83%) indicated only 1 or 2 objective criteria before clearance to RTP (Table 1). The greatest number of tests in any study was 6. 35 Types of criteria consistent across all studies were physical examination findings (ROM loss, effusion, positive Lachman), thigh circumference difference, isokinetic strength testing, hop testing, arthrometric testing, questionnaires, and other unspecified sport-specific or functional testing. A synopsis listing the number of criteria used to assess readiness to RTP is presented in Table 1.
Table 1.
Number of Criteria Used for Return to Play in Systematic Review of Literature
| No. of Criteria | No. of Studies |
|---|---|
| 1 | 20 |
| 2 | 29 |
| 3 | 4 |
| 4 | 5 |
| 5 | 1 |
| 6 | 1 |
Checklist Generation
Data from our systematic review and expert panel were pooled to determine the most commonly cited, practical, and important parameters to determine RTP after ACLR. Seven criteria were included in the final checklist, as shown in Supplemental Material 2. Criteria chosen for inclusion fell under 3 major categories: physical examination findings, dynamic/kinematic sport-specific testing, and the IKDC questionnaire. Physical examination items consisted of lack of effusion, full ROM, lack of instability, and thigh circumference (difference <1.5 cm). Kinematic testing consisted of 4 components: the Functional Movement Screen (score >14), all 4 hop tests (>90% of contralateral side), Pro Agility (time >90% of contralateral side), and our movement assessment (score >80% of contralateral side). Last, scoring >90% on the IKDC questionnaire was considered a passing score.
Prospective Evaluation
During the period studied, 222 patients met the inclusion criteria and consented to participate in the study. An overall 175 (78.8%) successfully passed our RTP checklist before receiving clearance to return to their preinjury levels of activity. Of the 175 patients, reinjury data were available for 146 (83.4%) at a minimum 2 years of follow-up. The remaining 47 (21.2%) patients underwent our RTP checklist at least once but never passed before returning to play. These patients were instructed to work on their nonpassing areas of the checklist for 4 to 6 weeks and then retake the test and obtain a passing grade before returning to play; however, they elected to not do so before returning to play. Of these 47 patients, injury data were available for 38 (80.9%) at a minimum 2 years of follow-up (Table 2).
Table 2.
Characteristics of Patients Who Completed the Return-to-Play Checklist a
| Patients Who Passed the Checklist (n = 146) | Patients Who Did Not Pass the Checklist (n = 38) | P | |
|---|---|---|---|
| Age, y | 18.3 (15.0-34.3) | 20.1 (15.0-30.6) | .163 |
| Sex | |||
| Male | 66 (45.2) | 22 (57.9) | |
| Female | 80 (54.8) | 16 (42.1) | |
| Follow-up, mo | 32.3 (24.0-56.9) | 28.4 (24.0-46.8) | |
| Autograft | 135 | 31 | .308 |
| Patellar tendon | 78 | 21 | |
| Hamstring tendon | 57 | 10 | |
| Allograft | 4 | 5 | .066 |
| Patellar tendon | 1 | 4 | |
| Hamstring | 3 | 0 | |
| Tibialis anterior | 0 | 1 | |
| Hamstring tendon autograft with allograft augmentation | 7 | 2 | .458 |
a Values are presented as No. (%) or mean (range).
Within 2 years of surgery, 34 patients (18.4%) sustained an injury to either knee, and 20 (10.9%) had an injury to either the ipsilateral or contralateral ACL. On subgroup analysis, 24 (16.4%) patients in the “passed checklist” group experienced an injury to either knee, as compared with 10 (26.3%) in the did not pass group. There was no significant difference between the groups with any injury in either knee at final follow-up (P = .162). Within the passed-checklist group, 8 (5.5%) patients sustained an injury to the ipsilateral ACL, and 5 (3.4%) had an injury to the contralateral ACL. In comparison, in the did-not-pass group, 7 (18.4%) patients sustained an injury to the ipsilateral ACL while no patients had an injury to the contralateral ACL. As noted in Table 3, the ipsilateral ACL injury rate was significantly higher in the did-not-pass group as compared with the passed group (P = .017). Injury rates between the groups did not appear to be significantly influenced by graft type (Table 4).
Table 3.
Patient Injuries and Complications a
| Patients Who Passed the Checklist (n = 146) | Patients Who Did Not Pass the Checklist (n = 38) | P | |
|---|---|---|---|
| Patients requiring reoperation for injury | 24 (16.4) | 10 (26.3) | .162 |
| Ipsilateral ACL tear | 8 (5.5) | 7 (18.4) | .017 |
| Contralateral ACL tear | 5 (3.4) | 0 | .585 |
| Lateral meniscal tear | 2 (1.4) | 1 (2.6) | .503 |
| Contralateral lateral meniscal tear | 2 (1.4) | 0 | ≥.999 |
| Medial meniscal tear | 9 (6.2) | 2 (5.3) | ≥.999 |
| Contralateral medial meniscal tear | 2 (1.4) | 1 (2.6) | .503 |
| LCL injury | 0 | 1 (2.6) | .207 |
| Contralateral LCL injury | 1 (0.7) | 1 (2.6) | .371 |
| MCL injury | 0 | 3 (7.9) | .008 |
| Patients requiring reoperation for complications | 0 | 1 (2.6) | .207 |
| Manipulation under anesthesia | 0 | 1 (2.6) | .207 |
a Data are reported as No. (%). Bold P values indicate statistically significant difference between groups (P < .05). Some patients sustained multiple injuries, and each injury has been counted under the correct category. ACL, anterior cruciate ligament; LCL, lateral collateral ligament; MCL, medial collateral ligament.
Table 4.
Type of Graft Used in Patients Who Sustained an Injury
| Injured Patients Who Passed the Checklist (n = 24) | Injured Patients Who Did Not Pass the Checklist (n = 10) | P | |
|---|---|---|---|
| Autograft | 24 | 7 | .394 |
| Patellar tendon | 11 | 5 | |
| Hamstring tendon | 13 | 2 | |
| Allograft | 0 | 3 | .153 |
| Patellar tendon | 0 | 2 | |
| Hamstring | 0 | 0 | |
| Achilles tendon | 0 | 0 | |
| Tibialis anterior | 0 | 1 | |
| Posterior tibial allograft | 0 | 0 |
Patients underwent checklist testing at a mean 8.41 months (range, 5.72-18.6) after surgery. The majority of patients who passed the checklist passed on their first time taking the test (n = 119; 81.5%). Of the 27 patients who did not pass on their first checklist attempt, 25 (17.1%) passed on their second attempt, and the remaining 2 (1.4%) passed on their third. Of the 24 patients who sustained an injury, 19 (79.2%) passed the checklist on their first attempt, while the remaining 5 (20.8%) passed the checklist on their second. The 19 patients who had an injury after passing the checklist returned to play at a slightly earlier time frame, at a mean 8.79 months (range, 7.00-18.64 months).
There were 13 (8.9%) patients who passed the checklist but not the ROM criteria (within 5° of the normal side on flexion and extension). Three (23.1%) patients passed the checklist on the first attempt after passing the other 6 criteria of the checklist. None of these patients sustained a reinjury. The remaining 10 patients all passed the checklist on the second attempt, with 9 (90.0%) passing the ROM portion. One patient did sustain an ipsilateral medial meniscus injury 13.08 months after surgery, but this patient did pass the ROM criteria.
Secondary outcome measures, including RTP status and IKDC outcome scores, were available for 164 patients (Table 5). In the cohort of patients who passed the checklist, 115 (91.3%) returned to play at any level at 9.5 ± 2.8 months (mean ± SD; range, 5.0-27.0 months), and 105 (83.3%) returned at the same or higher level of competition. In comparison, for those patients who never passed the checklist, 35 (92.1%) returned to sport at any level at 9.2 ± 2.0 months (range, 6.0-15.0 months), and 32 (84.2%) returned at the same or higher level of competition. There was no detected difference with respect to RTP rates at any level between the groups. Additionally, functional outcomes scores were not significantly different between the groups (P = .763).
Table 5.
Summary of Return to Play and IKDC Outcome Measure a
| Patients Who Passed the Checklist (n = 126) | Patients Who Did Not Pass the Checklist (n = 38) | P | |
|---|---|---|---|
| Returned to play, No. (%) | .738 | ||
| Yes | 115 (91.3) | 35 (92.1) | |
| Lower level of competition | 10 | 3 | |
| Same or higher level of competition | 105 | 32 | |
| No | 11 (8.7) | 3 (7.9) | |
| IKDC score, mean ± SD (range) | 91.15 ± 8.82 (50.57-100.00) | 87.96 ± 15.90 (44.82-100.00) | .763 |
a IKDC, International Knee Documentation Committee.
Furthermore, multivariate analysis was performed to determine whether certain factors may predispose patients to be at a higher risk of reinjury after surgery. Our analysis demonstrated that passing the checklist, age, sex, and body mass index did not put patients at an increased risk for reinjury (Table 6).
Table 6.
Multivariate Regression Analysis With Any Reinjury as the Dependent Outcome
| Variable | Estimate | P | Odds Ratio (95% CI) |
|---|---|---|---|
| Groups: passed | 0.58 | .189 | 1.78 (0.73-4.14) |
| Age | 0.03 | .636 | 1.02 (0.92-1.13) |
| Body mass index | –0.001 | .982 | 1.00 (0.89-1.10) |
| Gender | 0.15 | .724 | 1.16 (0.51-2.69) |
Discussion
There is increasing evidence, including a recent study by Mayer et al, 31 that time since surgery and clinical judgment alone are insufficient to identify patients with functional deficits within the first 6 months after surgery. Furthermore, through a systematic review of return-to-sport guidelines after ACLR in level 1 randomized controlled trials (49 studies, 4178 patients), Harris et al 19 determined that 90% of studies failed to use objective criteria before returning patients to sport and 65% failed to use any criteria before returning patients to sport. Ultimately, we used this information to generate a checklist of physical examination, strength, and coordination measures capable of assessing multiple aspects of joint function, stability, and dynamics. Since the development, our checklist has been implemented as the primary indicator for patient readiness to RTP after ACLR at our institution.
The primary objective of this study was to generate and validate a Safer Return to Play Following ACL Reconstruction Checklist, consisting of validated subjective and objective functional tests that can be quickly and easily implemented into a sports medicine practice. We hypothesized that patients who successfully passed the checklist before returning to sports would experience lower rates of ipsilateral and contralateral knee injury at the 2-year follow-up in comparison with patients who failed the checklist and returned to play without passing. Our analysis indicates that although there was no significant difference between the groups with any injury in either knee at final follow-up (P = .162), the ipsilateral ACL injury rate was significantly higher in the did-not-pass group as compared with the passed group (P = .017). The odds ratio for this was 3.9 with a 95% CI of 1.2 to 11.8.
Wiggins et al, 43 through a systematic review, investigated the risk of secondary injury in younger athletes after ACLR. There were 19 articles that met the inclusion criteria and were included in the authors’ analysis. The ipsilateral ACL injury rate was cited in 14 studies at 7% while contralateral ACL data were reported in 7 studies at 8%, for a combined ACL injury rate of 15%. In patients aged <25 years, the ipsilateral ACL injury rate increased to 10% and the contralateral ACL injury rate to 11%, for a combined ACL injury rate of 21%. 43 The results of our study demonstrate that patients who successfully passed the ACL checklist before returning to play experienced lower rates of ACL injury: ipsilateral (5.5% vs 7%), contralateral (3.4% vs 8%), and overall (8.9% vs 15%).
Other investigators have evaluated objective criteria before return from ACLR. Grindem et al 18 evaluated 106 patients who participated in pivoting sports for 2 years after ACLR. Before RTP, patients’ knee function was assessed with the Knee Outcome Survey–Activities of Daily Living Scale, Global Rating Scale of Function, and quadriceps strength and hop test symmetry. To be cleared to RTP, patients needed to achieve scores >90 on all tests. There were 74 patients who returned to IKDC level I sports (handball, football, basketball, or floorball) and 69 (93.2%) who underwent functional testing before returning to play. Of the 74 patients, 18 (24.3%) successfully passed the return-to-sport criteria. Of the 55 patients who failed RTP criteria, 21 (38.2%) experienced knee injuries, as compared with only 1 (5.6%) of the patients who successfully passed the return-to-sport criteria. These results are similar to our study, as patients who underwent and successfully passed checklist testing had a lower reinjury rate (16.4%) than the did-not-pass group (26.3%).
Several studies have investigated objective criteria before patients RTP after ACLR. 16,34 Nawasreh et al 34 investigated 108 patients who had participated in IKDC level 1 or 2 sports activities and who completed return-to-activity criteria (RTAC) at 6, 12, and 24 months after ACLR. The authors’ RTAC testing consisted of isometric quadriceps strength index, 4 single-leg hop tests, and 2 patient-reported outcome measures: the Knee Outcome Survey–Activities of Daily Living Scale and the Global Rating Scale of Function. A passing score consisted of >90% on all 4 measures, while a score <90% on any measure consisted of a failing grade. Patients in the passing RTAC group, as compared with patients in the failing RTAC group, had more normal knee function and movement symmetry at 12 and 24 months postoperatively as well a higher rate of return to their preinjury activity levels. Gokeler et al 16 retrospectively evaluated 28 patients who underwent a test battery at 6.5 ± 1.0 months after ACLR. The battery consisted of the jump-landing task (Landing Error Scoring System), single hop for distance, triple hop for distance, side hop, and isokinetic test, performed in order. The authors noted that only 2 (7.14%) patients passed all the criteria, leading to a conclusion that for the majority of patients who are 6 months after ACLR, additional rehabilitation is necessary.
Our study has several strengths. We performed a comprehensive review of the literature to summarize the objective criteria used to assess RTP after ACLR to develop our checklist. In addition, we asked an expert panel to analyze these and other criteria for importance regarding readiness to RTP. We then combined these data to form our Safer Return to Play Following ACL Reconstruction Checklist as a practical, objective assessment of our patients after ACLR. Additionally, the validation of our study demonstrated that successfully passing the checklist reduced a patient’s risk of injuring one’s ipsilateral ACL within the first 2 years after surgery.
Limitations
This study is limited by several factors. Several studies in the review did not describe their criteria for RTP in full detail and frequently referred to tests as “sport-specific,” “functional,” or “strength” without qualifying which were performed or at what goal. It is possible that functional assessments such as the hop test were used more frequently in the literature than what the review would suggest. Furthermore, quadriceps strength was not in our analysis. This variable was not selected by our expert panel. The initial purpose of the checklist was to have it easily utilized in physical therapy clinics or offices without excessive equipment. It was decided that isokinetic testing may not be readily available and, for this reason, was eliminated from the final checklist. Isokinetic testing is an additional criterion that can be used to assess an athlete’s readiness to RTP. However, our checklist was developed with simplicity and generalizability in mind, and isokinetic testing is something that is not available to everyone. In conducting our systematic review, initial searches were performed by title review, followed by more detailed abstract review in search of articles discussing objective RTP criteria. This may have led us to overlook potential articles that did discuss RTP criteria but did not indicate as such in the title or abstract. Additionally, our study did not include review articles, some of which advocate for increased testing before RTP, leading us to possibly underestimate the prevalence of individuals using only 1 criterion in assessing RTP. A component that was not in our checklist criteria was an athlete’s psychological readiness to RTP. We recognize this as an important component in assessing an athlete’s readiness to return; therefore, we are working on developing it as part of our checklist moving forward. For the validation component of our study, patients were not randomized between taking and not taking the checklist. As such, a direct comparison could not be performed between patients taking the checklist and passing before returning to play and those returning to play under the traditional criteria of clinical judgment. Last, a number of surgeons were in our analysis; as a result, the individual surgical technique may have influenced a patient’s reinjury as well.
Conclusion
In this study, we present a checklist of criteria for return to sports after ACLR through the implementation of a systematic review and expert panel. As compared with historical standards of 1 or 2 criteria, our list combines 4 tests of joint kinetics, strength, coordination, and control alongside traditional physical examination findings and a patient questionnaire. Validation of our checklist demonstrated that patients who successfully passed it before returning to play experienced a lower injury rate, in particular a significant reduction in ipsilateral ACL injury, as compared with patients who failed the checklist, as well as with what has been reported in the literature.
Supplemental material for this article is available at http://journals.sagepub.com/doi/suppl/10.1177/23259671221090412.
Supplemental Material
Supplemental Material, sj-pdf-1-ojs-10.1177_23259671221090412 for Safer Return to Play After Anterior Cruciate Ligament Reconstruction: Evaluation of a Return-to-Play Checklist by Christopher J. Hadley, Somnath Rao, Fotios P. Tjoumakaris, Michael G. Ciccotti, Christopher C. Dodson, Paul A. Marchetto, Sommer Hammoud, Steven B. Cohen and Kevin B. Freedman in Orthopaedic Journal of Sports Medicine
Supplemental Material, sj-pdf-2-ojs-10.1177_23259671221090412 for Safer Return to Play After Anterior Cruciate Ligament Reconstruction: Evaluation of a Return-to-Play Checklist by Christopher J. Hadley, Somnath Rao, Fotios P. Tjoumakaris, Michael G. Ciccotti, Christopher C. Dodson, Paul A. Marchetto, Sommer Hammoud, Steven B. Cohen and Kevin B. Freedman in Orthopaedic Journal of Sports Medicine
Footnotes
Final revision submitted November 10, 2021; accepted December 15, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: F.P.T. has received consulting fees from Medical Device Business Services and hospitality payments from Stryker. M.G.C. has received grants from Arthrex and DJO and education payments from Liberty Surgical. C.C.D. has received education payments from Liberty Surgical, consulting and speaking fees from Arthrex, and hospitality payments from Stryker. P.A.M. has received education payments from Liberty Surgical. S.H. has received education payments from Arthrex/Liberty Surgical and hospitality payments from Smith & Nephew. S.B.C. has received education payments from Liberty Surgical and consulting fees from Biomet. K.B.F. has received education payments from Liberty Surgical, consulting fees from DePuy/Medical Device Business Services, and speaking fees and honoraria from Vericel. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Thomas Jefferson University.
References
- 1. Ardern CL, Taylor NF, Feller JA, Webster KE. Return-to-sport outcomes at 2 to 7 years after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2012;40(1):41–48. doi:10.1177/0363546511422999 [DOI] [PubMed] [Google Scholar]
- 2. Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45(7):596–606. doi:10.1136/bjsm.2010.076364 [DOI] [PubMed] [Google Scholar]
- 3. Barber-Westin SD, Noyes FR. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy. 2011;27(12):1697–1705. doi:10.1016/j.arthro.2011.09.009 [DOI] [PubMed] [Google Scholar]
- 4. Barber-Westin SD, Noyes FR. Objective criteria for return to athletics after anterior cruciate ligament reconstruction and subsequent reinjury rates: a systematic review. Phys Sportsmed. 2011;39(3):100–110. doi:10.3810/psm.2011.09.1926 [DOI] [PubMed] [Google Scholar]
- 5. Battaglia MJ, Cordasco FA, Hannafin JA, et al. Results of revision anterior cruciate ligament surgery. Am J Sports Med. 2007;35(12):2057–2066. doi:10.1177/0363546507307391 [DOI] [PubMed] [Google Scholar]
- 6. Bell DR, Smith MD, Pennuto AP, Stiffler MR, Olson ME. Jump-landing mechanics after anterior cruciate ligament reconstruction: a landing error scoring system study. J Athl Train. 2014;49(4):435–441. doi:10.4085/1062-6050-49.3.21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Boden BP, Torg JS, Knowles SB, Hewett TE. Video analysis of anterior cruciate ligament injury: abnormalities in hip and ankle kinematics. Am J Sports Med. 2009;37(2):252–259. doi:10.1177/0363546508328107 [DOI] [PubMed] [Google Scholar]
- 8. Bushman TT, Grier TL, Canham-Chervak M, Anderson MK, North WJ, Jones BH. The functional movement screen and injury risk: association and predictive value in active men. Am J Sports Med. 2016;44(2):297–304. doi:10.1177/0363546515614815 [DOI] [PubMed] [Google Scholar]
- 9. Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM. Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care Res. 2011;63(suppl 11):S208–S228. doi:10.1002/acr.20632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cook G, Burton L, Hoogenboom BJ, Voight M. Functional movement screening: the use of fundamental movements as an assessment of function—part 1. Int J Sports Phys Ther. 2014;9(3):396–409. [PMC free article] [PubMed] [Google Scholar]
- 11. Cook G, Burton L, Hoogenboom BJ, Voight M. Functional movement screening: the use of fundamental movements as an assessment of function—part 2. Int J Sports Phys Ther. 2014;9(4):549–563. [PMC free article] [PubMed] [Google Scholar]
- 12. Cristiani R, Janarv PM, EngstrÖm B, Edman G, Forssblad M, Stålman A. Delayed anterior cruciate ligament reconstruction increases the risk of abnormal pre-reconstruction laxity, cartilage and medial meniscus injuries. Arthroscopy. Published online November 23, 2020. doi:10.1016/j.arthro.2020.11.030 [DOI] [PubMed] [Google Scholar]
- 13. Csintalan RP, Inacio MCS, Funahashi TT, Maletis GB. Risk factors of subsequent operations after primary anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42(3):619–625. doi:10.1177/0363546513511416 [DOI] [PubMed] [Google Scholar]
- 14. Daniel DM, Fithian DC. Indications for ACL surgery. Arthroscopy. 1994;10(4):434–441. doi:10.1016/s0749-8063(05)80196-3 [DOI] [PubMed] [Google Scholar]
- 15. Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR. Fate of the ACL-injured patient: a prospective outcome study. Am J Sports Med. 1994;22(5):632–644. doi:10.1177/036354659402200511 [DOI] [PubMed] [Google Scholar]
- 16. Gokeler A, Welling W, Zaffagnini S, Seil R, Padua D. Development of a test battery to enhance safe return to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017;25(1):192–199. doi:10.1007/s00167-016-4246-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Griffin LY, Albohm MJ, Arendt EA, et al. Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt Valley II meeting, January 2005. Am J Sports Med. 2006;34(9):1512–1532. doi:10.1177/0363546506286866 [DOI] [PubMed] [Google Scholar]
- 18. Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. Br J Sports Med. 2016;50(13):804–808. doi:10.1136/bjsports-2016-096031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Harris JD, Abrams GD, Bach BR, et al. Return to sport after ACL reconstruction. Orthopedics. 2014;37(2):e103–e108. doi:10.3928/01477447-20140124-10 [DOI] [PubMed] [Google Scholar]
- 20. Herrington L, Myer G, Horsley I. Task based rehabilitation protocol for elite athletes following Anterior Cruciate ligament reconstruction: a clinical commentary. Phys Ther Sport. 2013;14(4):188–198. doi:10.1016/j.ptsp.2013.08.001 [DOI] [PubMed] [Google Scholar]
- 21. Hewett TE, Di Stasi SL, Myer GD. Current concepts for injury prevention in athletes after anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41(1):216–224. doi:10.1177/0363546512459638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hewett TE, Torg JS, Boden BP. Video analysis of trunk and knee motion during non-contact anterior cruciate ligament injury in female athletes: lateral trunk and knee abduction motion are combined components of the injury mechanism. Br J Sports Med. 2009;43(6):417–422. doi:10.1136/bjsm.2009.059162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hsu CC, Sandford BA. The Delphi technique: making sense of consensus. Practical Assessment, Research, and Evaluation. 2007;12(10):1–8. [Google Scholar]
- 24. Hui C, Salmon LJ, Kok A, Maeno S, Linklater J, Pinczewski LA. Fifteen-year outcome of endoscopic anterior cruciate ligament reconstruction with patellar tendon autograft for “isolated” anterior cruciate ligament tear. Am J Sports Med. 2011;39(1):89–98. doi:10.1177/0363546510379975 [DOI] [PubMed] [Google Scholar]
- 25. Leys T, Salmon L, Waller A, Linklater J, Pinczewski L. Clinical results and risk factors for reinjury 15 years after anterior cruciate ligament reconstruction: a prospective study of hamstring and patellar tendon grafts. Am J Sports Med. 2012;40(3):595–605. doi:10.1177/0363546511430375 [DOI] [PubMed] [Google Scholar]
- 26. Magnussen RA, Lawrence JTR, West RL, Toth AP, Taylor DC, Garrett WE. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012;28(4):526–531. doi:10.1016/j.arthro.2011.11.024 [DOI] [PubMed] [Google Scholar]
- 27. Maletis GB, Chen J, Inacio MCS, Funahashi TT. Age-related risk factors for revision anterior cruciate ligament reconstruction: a cohort study of 21,304 patients from the Kaiser Permanente Anterior Cruciate Ligament Registry. Am J Sports Med. 2016;44(2):331–336. doi:10.1177/0363546515614813 [DOI] [PubMed] [Google Scholar]
- 28. Maletis GB, Inacio MCS, Desmond JL, Funahashi TT. Reconstruction of the anterior cruciate ligament: association of graft choice with increased risk of early revision. Bone Jt J. 2013;95B(5):623–628. doi:10.1302/0301-620X.95B5.30872 [DOI] [PubMed] [Google Scholar]
- 29. Mall NA, Abrams GD, Azar FM, et al. Trends in primary and revision anterior cruciate ligament reconstruction among National Basketball Association team physicians. Am J Orthop (Belle Mead NJ). 2014;43(6):267–271. [PubMed] [Google Scholar]
- 30. Mall NA, Chalmers PN, Moric M, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med. 2014;42(10):2363–2370. doi:10.1177/0363546514542796 [DOI] [PubMed] [Google Scholar]
- 31. Mayer SW, Queen RM, Taylor D, et al. Functional testing differences in anterior cruciate ligament reconstruction patients released versus not released to return to sport. Am J Sports Med. 2015;43(7):1648–1655. doi:10.1177/0363546515578249 [DOI] [PubMed] [Google Scholar]
- 32. Myer GD, Schmitt LC, Brent JL, et al. Utilization of modified NFL combine testing to identify functional deficits in athletes following ACL reconstruction. J Orthop Sports Phys Ther. 2011;41(6):377–387. doi:10.2519/jospt.2011.3547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Narducci E, Waltz A, Gorski K, Leppla L, Donaldson M. The clinical utility of functional performance tests within one-year post-ACL reconstruction: a systematic review. Int J Sports Phys Ther. 2011;6(4):333–342. [PMC free article] [PubMed] [Google Scholar]
- 34. Nawasreh Z, Logerstedt D, Cummerm K, Axe MJ, Risberg MA, Snyder-Mackler L. Do patients failing return-to-activity criteria at 6 months after anterior cruciate ligament reconstruction continue demonstrating deficits at 2 years? Am J Sports Med. 2017;45(5):1037–1048. doi:10.1177/0363546516680619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Noyes FR, Barber-Westin SD. Neuromuscular retraining intervention programs: do they reduce noncontact anterior cruciate ligament injury rates in adolescent female athletes? Arthroscopy. 2014;30(2):245–255. doi:10.1016/j.arthro.2013.10.009 [DOI] [PubMed] [Google Scholar]
- 36. O’Connor FG, Deuster PA, Davis J, Pappas CG, Knapik JJ. Functional movement screening: predicting injuries in officer candidates. Med Sci Sports Exerc. 2011;43(12):2224–2230. doi:10.1249/MSS.0b013e318223522d [DOI] [PubMed] [Google Scholar]
- 37. Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968–1978. doi:10.1177/0363546510376053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Roos H, Ornell M, Gärdsell P, Lohmander LS, Lindstrand A. Soccer after anterior cruciate ligament injury—an incompatible combination? A national survey of incidence and risk factors and a 7-year follow-up of 310 players. Acta Orthop Scand. 1995;66(2):107–112. doi:10.3109/17453679508995501 [DOI] [PubMed] [Google Scholar]
- 39. Salmon LJ, Russell VJ, Refshauge K, et al. Long-term outcome of endoscopic anterior cruciate ligament reconstruction with patellar tendon autograft: minimum 13-year review. Am J Sports Med. 2006;34(5):721–732. doi:10.1177/0363546505282626 [DOI] [PubMed] [Google Scholar]
- 40. Smith FW, Rosenlund EA, Aune AK, MacLean JA, Hillis SW. Subjective functional assessments and the return to competitive sport after anterior cruciate ligament reconstruction. Br J Sports Med. 2004;38(3):279–284. doi:10.1136/bjsm.2002.001982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Stewart PF, Turner AN, Miller SC. Reliability, factorial validity, and interrelationships of five commonly used change of direction speed tests. Scand J Med Sci Sports. 2014;24(3):500–506. doi:10.1111/sms.12019 [DOI] [PubMed] [Google Scholar]
- 42. Wallace BJ, Kernozek TW, Bothwell EC. Lower extremity kinematics and kinetics of Division III collegiate baseball and softball players while performing a modified pro-agility task. J Sports Med Phys Fitness. 2007;47(4):377–384. [PubMed] [Google Scholar]
- 43. Wiggins AJ, Grandhi RK, Schneider DK, Stanfield D, Webster KE, Myer GD. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2016;44(7):1861–1876. doi:10.1177/0363546515621554 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-pdf-1-ojs-10.1177_23259671221090412 for Safer Return to Play After Anterior Cruciate Ligament Reconstruction: Evaluation of a Return-to-Play Checklist by Christopher J. Hadley, Somnath Rao, Fotios P. Tjoumakaris, Michael G. Ciccotti, Christopher C. Dodson, Paul A. Marchetto, Sommer Hammoud, Steven B. Cohen and Kevin B. Freedman in Orthopaedic Journal of Sports Medicine
Supplemental Material, sj-pdf-2-ojs-10.1177_23259671221090412 for Safer Return to Play After Anterior Cruciate Ligament Reconstruction: Evaluation of a Return-to-Play Checklist by Christopher J. Hadley, Somnath Rao, Fotios P. Tjoumakaris, Michael G. Ciccotti, Christopher C. Dodson, Paul A. Marchetto, Sommer Hammoud, Steven B. Cohen and Kevin B. Freedman in Orthopaedic Journal of Sports Medicine