Abstract
Background:
Orthopaedic injuries are common in ice hockey at all levels and can result in physical and psychological adverse effects on these athletes.
Purpose:
Primarily, to summarize published data on orthopaedic hockey injuries at the junior through professional level. Secondarily, to characterize the literature based on anatomic site injured, return-to-play rates, cause/mechanism of injury, time lost, and treatments used.
Study Design:
Scoping review; Level of evidence, 4.
Methods:
PubMed, EMBASE, Cochrane library, and SCOPUS were searched using the terms “hockey” and “injuries” using PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines, and 4163 studies involving orthopaedic injuries were identified. Our inclusion criteria consisted of accessible full-text articles that evaluated orthopaedic injuries in men’s ice hockey athletes of all levels. We excluded case reports and articles evaluating women’s ice hockey injuries, as well as those evaluating nonorthopaedic injuries, such as concussions; traumatic brain injuries; and facial, dental, and vascular injuries, among others. Studies were divided based on level of play and anatomic site of injury. Level of evidence, year published, country of corresponding author, method of data collection, incidence of injury per athlete-exposure, and time lost were extracted from each article.
Results:
A total of 92 articles met the inclusion criteria and were performed between 1975 and 2020, with the majority published between 2015 and 2020. These were divided into 8 anatomic sites: nonanatomic-specific (37%), intra-articular hip (20.7%), shoulder (9.8%), knee (8.7%), trunk/pelvis (7.6%), spine (7.6%), foot/ankle (6.5%), and hand/wrist (2.2%). Of these studies, 71% were level 4 evidence. Data were obtained mostly via surveillance programs and searches of publicly available information (eg, injury reports, player profiles, and press releases).
Conclusion:
This scoping review provides men’s hockey players and physicians taking care of elite ice hockey athletes of all levels with a single source of the most current literature regarding orthopaedic injuries. Most research focused on nonanatomic-specific injuries, intra-articular hip injuries, knee injuries, and shoulder injuries, with the majority having level 4 evidence.
Keywords: athletic training, epidemiology, ice hockey, injury prevention
Hockey is a popular international sport, and injuries occur commonly due to high speed of play, hard ice surface, and contact nature of the sport. Any injury has the potential to be detrimental to a player’s physical and mental health. 8 Having a succinct compilation of the most common injuries and associated games missed can help players, coaches, athletic trainers, and management (in the case of professional leagues) have a more well-rounded understanding of prognosis for an athlete’s return to play. In addition, this study stands to highlight certain anatomic areas where novel protective equipment can be researched and developed to protect players from the most common injuries, such as bony injuries in the foot and ankle. Despite the international popularity of ice hockey, orthopaedic literature regarding competitive hockey players is lacking. In the United States, there has been some examination using the National Collegiate Athletics Association (NCAA) Injury Surveillance Program to assess injury rates and anatomic location in collegiate hockey athletes, as well as the National Hockey League (NHL) Injury Surveillance System to examine similar outcomes in professional athletes. ¶ However, this study serves to broaden the population studied outside of solely collegiate and professional athletes to provide a more well-rounded summary of hockey injuries and how they vary based on level of play.
The primary goal of this scoping review was to summarize published data on orthopaedic hockey injuries at the junior through professional level, providing team physicians and clinicians with a comprehensive single source of the most current literature regarding the frequency and outcomes of orthopaedic injuries in these athletes, allowing physicians and clinicians to quickly and accurately gather the most up-to-date information regarding treatment. The secondary objective was to characterize the literature based on the anatomic site injured, return-to-play rates, mechanism of injury, time lost, and treatments used. It was hypothesized that most injuries would occur during gameplay rather than practice and those competing at the international level would be most likely to get injured.
Methods
PubMed, EMBASE, Cochrane library, and SCOPUS were searched using the search terms “hockey” and “injuries” to identify all studies of orthopaedic injuries. Three authors (P.F.S., P.T.O., and M.M.) independently conducted the search and compared findings. Disagreements among reviewers were brought to the attention of the senior author (J.P.S.) who ultimately made the final decision regarding article inclusion. Our inclusion criteria consisted of accessible full-text articles that evaluated orthopaedic injuries in men’s ice hockey athletes of all levels. We excluded case reports and articles evaluating women’s ice hockey injuries, as well as those evaluating nonorthopaedic injuries, such as concussions; traumatic brain injuries; and facial, dental, and vascular injuries. Duplicate studies were consolidated into a single article.
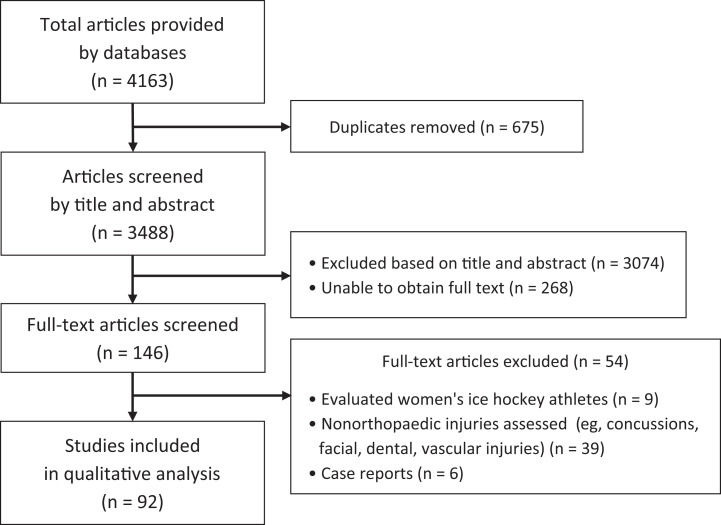
The studies were divided based on level of play and anatomic site of injury. Level of evidence, year published, country of corresponding author, method of data collection, incidence of injury per athlete-exposure (AE; a unit of susceptibility to injury defined as 1 athlete participating in 1 practice or game where the athlete is exposed to the possibility of injury, reported as a rate per 1000 AEs), and time lost were extracted from each article. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart of the search strategies is presented in Figure 1. We identified 3488 studies via a database search, of which 92 articles met inclusion criteria. Figure 2 summarizes the articles based on anatomic site.
Figure 1.
Flowchart of article screening process.
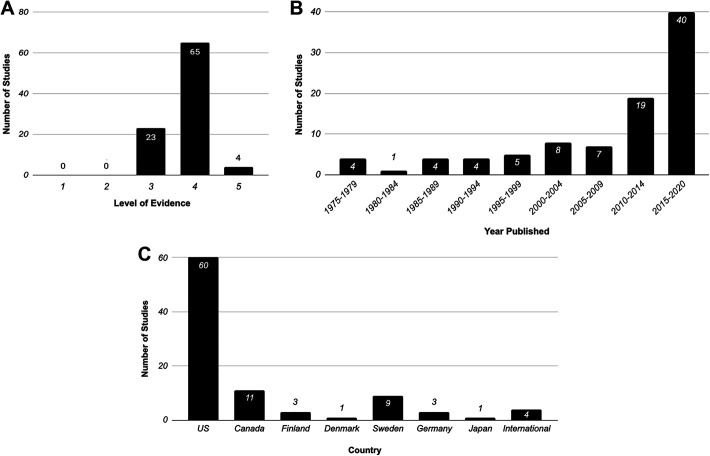
Figure 2.
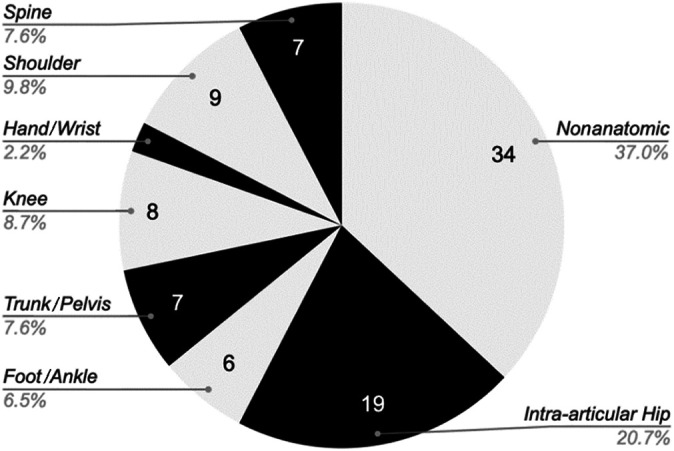
Number of studies based on anatomic site. No. of hand/wrist studies is 2.
Results
No evidence level 1 or 2 studies met our inclusion criteria (Figure 3A). The majority of studies were published between 2015 and 2020 (Figure 3B), and 62% of the studies were published in the United States (Figure 3C). Most studies obtained their data via surveillance programs (Table 1).
Figure 3.
Number of studies based on (A) level of evidence, (B) year of publication, and (C) country of publication. US, United States.
Table 1.
Number of Studies Based on Method of Data Collection a
| Method of Data Collection | No. of Studies | References |
|---|---|---|
| Surveillance programs (NHL ISS, NCAA ISP, and CAIRS) | 23 | 1, 2, 11 -13, 18 -21, 27, 32, 33, 40, 41, 46, 52, 55, 57, 59, 66, 73, 81, 93 |
| League data | 21 | 3, 4, 15, 23, 34, 38, 42, 45, 47, 54, 60 -62, 64, 67, 68, 74, 75, 82, 85, 90, 91 |
| Individual team data | 18 | 9, 22, 24, 25, 30, 35, 37, 48, 50, 51, 56, 65, 71, 79, 80, 84, 87 |
| Institutional data | 15 | 7, 10, 26, 28, 29, 31, 36, 43, 44, 53, 69, 70, 88, 89, 92 |
| Internet | 7 | 5, 14, 16, 49, 58, 78, 83 |
| Literature review | 4 | 6, 17, 63, 72 |
| Olympic data | 4 | 39, 76, 77, 86 |
a CAIRS, Canadian Athletic Injuries/Illness Reporting System; NCAA ISP, National Collegiate Athletic Association Injury Surveillance Program; NHL ISS, National Hockey League Injury Surveillance System.
Nonanatomic-Specific Injuries
The overall injury rate for all levels of play was 19.68 per 1000 AEs (range, 4.9-68.5 per 1000 AEs) (Table 2). # Professional European players had the highest overall injury rate with 68.5 per 1000 AEs, whereas collegiate athletes had the lowest at 4.9 per 1000 AEs. 25,41,56,62 Junior players were the most likely to get injured in games, while professional players outside of the United States were most likely to get injured in training. 16,30,38,42,47,67,84 Overall, players were more likely to get injured during games compared with training, and forwards were more likely to get injured compared with defenseman and goalkeepers. ** Anterior Cruciate Ligament (ACL) injuries were found to have the most game-time missed in professional ice hockey players (Table 3). 22,46,50,79,81
Table 2.
Overall Injury Rate by Anatomic Site and Level of Play a
| No. of Injuries | ||||
|---|---|---|---|---|
| Lead Author (Year) | Player Cohort | Per 1000 AEs | Per 1000 Game-Hours | Per 1000 Training-Hours |
| Nonanatomic Specific | ||||
| McKay (2014) 55 | NHL | 15.6 | 49.4 | |
| Donskov (2019) 16 | NHL | 64.5 | ||
| Mölsä (2000) 62 | Professional European | 68.5 | ||
| Jørgensen (1986) 38 | Professional European | 38 | 1.5 | |
| Tegner (1991) 85 | Professional European | 53 | ||
| Lorentzon (1988) 48 | Professional European | 78.4 | 1.4 | |
| Pettersson (1993) 67 | Professional European | 74.1 | 2.6 | |
| Kuzuhara (2009) 42 | Professional Asian | 74.3 | 11.2 | |
| Tuominem (2015) 86 | International | 52.1 | ||
| Lorentzon (1988) 47 | International | 79.2 | ||
| Donskov (2019) 16 | Collegiate (Canada and US) | 16.85 | ||
| Kerr (2015) 41 | Collegiate (Canada and US) | 9.5 | ||
| Flik (2005) 25 | Collegiate (Canada and US) | 4.9 | 13.8 | 2.2 |
| Agel (2010) 1 | Collegiate (Canada and US) | 18.7 | 2.2 | |
| McKnight (1992) 56 | Collegiate (Canada and US) | 10.2 | 14.2 | 2.52 |
| Pelletier (1993) 66 | Collegiate (Canada and US) | 19.95 | ||
| Donskov (2019) 16 | Junior | 80.4 | ||
| Stuart (1995) 84 | Junior | 9.4 | 96.1 | 3.9 |
| Tuominem (2015) 86 | Junior | 39.8 | ||
| Gröger (2001) 30 | Junior | 46.8 | ||
| Intra-articular Hip | ||||
| Epstein (2013) 21 | NHL | 1.81 | ||
| Dalton (2016) 13 | Collegiate (Canada and US) | 1.03 | ||
| Kerbel (2018) 40 | Collegiate (Canada and US) | 3.43 | ||
| Cruz (2019) 12 | Collegiate (Canada and US) | 3.43 | ||
| Trunk/Pelvis | ||||
| Tyler (2002) 88 | NHL | 3.2 | ||
| Knee | ||||
| Longstaffe (2020) 46 | NHL | 0.2 | ||
| Agel (2016) 2 | Collegiate (Canada and US) | 0.03 | ||
| Grant (2013) 28 | Collegiate (Canada and US) | 0.44 | ||
| Foot/Ankle | ||||
| Roos (2017) 73 | Collegiate (Canada and US) | 0.15 | ||
| Mauntel (2017) 52 | Collegiate (Canada and US) | 0.11 | ||
| Shoulder | ||||
| Hibberd (2016) 33 | Collegiate (Canada and US) | 0.64 | ||
| Melvin (2018) 57 | Collegiate (Canada and US) | 7.33 | 0.83 | |
| Gil (2018) 27 | Collegiate (Canada and US) | 0.06 | ||
| Spine | ||||
| Zupon (2018) 93 | Collegiate (Canada and US) | 0.56 | ||
a AEs, athlete-exposures; NHL, National Hockey League; US, United States.
Table 3.
Average Game Time Missed by Anatomic Site and Level of Play a
| Injury | Lead Author (Year) | Player Cohort | Average Game-Time Missed, wk |
|---|---|---|---|
| Intra-articular Hip | |||
| General intra-articular hip injuries | Epstein (2013) 21 | NHL | 6.17 |
| Wörner (2020) 91 | Other professional leagues (Swedish) | 2 | |
| Hip arthroscopy for FAI | Schallmo (2018) 78 | NHL | 23.4 |
| Sochacki (2019) 83 | NHL | 29.1 | |
| Philippon (2007) 69 | NHL | 23.8 | |
| Bizzini (2007) 9 | International/Olympics | 47 | |
| Knee | |||
| ACL | Longstaffe (2020) 46 | NHL | 58.1 |
| Erickson (2014) 22 | NHL | 54.6 | |
| Mai (2017) 50 | NHL | 60.2 | |
| Sikka (2016) 81 | NHL | 68.6 | |
| Arthroscopic microfracture | Schallmo (2018) 79 | NHL | 60.2 |
| Foot/Ankle | |||
| High ankle sprains | Mollon (2019) 59 | NHL | 6.4 |
| Wright (2004) 92 | NHL | 3.1 | |
| Shoulder | |||
| Clavicle fractures | Hebert-Davies (2018) 32 | NHL | 15.2 |
| Labral tears | Rangavajjula (2016) 72 | NHL | 30.1 |
| Spine | |||
| ACDF | Watkins (2018) 90 | NHL | 66.5 |
| Mai (2018) 51 | NHL | 31.7 | |
| Spondylolysis | Donaldson (2014) 15 | Juniors | 8 |
a ACDF, anterior cervical diskectomy and fusion; ACL, anterior cruciate ligament; FAI, femoroacetabular impingement; NCAA, National Collegiate Athletic Association; NHL, National Hockey League.
Donaldson et al 14 reviewed all NHL players between 2009 and 2012 and found that 50.9% of players missed at least 1 game, with most sustaining a leg/foot injury with salary loss of $68.2 million. Lubbe et al 49 found the number of games played in the first season after injury by NHL players was reduced significantly after hip arthroscopy (HA), noninstability shoulder arthroscopy, knee arthroscopy, and core muscle injury repair (P = .002, P = .009, P = .03, and P = .01, respectively).
Mölsä et al, 62 studying players in the Finnish Hockey League, found the injury rate per game increased from 54 per 1000 player-hours in the 1970s to 83 per 1000 player-hours in the 1990s, with an increasing risk as players aged. In the Superisligaen, Jørgensen and Smasal 38,68 found the head to be most commonly injured, followed by the lower extremity (LE). The majority of LE injuries were ligamentous sprains seen most commonly in the ankle and muscular strains seen most commonly in the thigh. 68 In the Swedish Hockey League, most injuries occurred to the LE due to in-game trauma, with shoulder injuries being the most common upper extremity (UE) injury. 3,4,48,67,85 One study examined injuries in the Asian Ice Hockey League and found players were 6.6 times more likely to sustain serious injuries in a game compared with in practice. 42
Between 2006 and 2013 in international competitions, Tuominem et al 86 found the most commonly injured body part was the face, the knee for the LE, and the shoulder for the UE. Arenas with flexible boards and glass reduced the risk of injury by 29%. 86 In the 2008 Olympic Games in Beijing, 20.4% of hockey athletes sustained an injury, with the majority occurring during gameplay due to contact with a stick/puck. 39
When examining collegiate athletes, researchers have reported most injuries occurred with collisions resulting in concussions followed by knee injuries. 1,25,56,66 This population had a lower rate of facial injuries compared with professional hockey players, which authors have hypothesized was due to the face shields required in college. 56
For junior level hockey athletes, the most prevalent injuries were facial lacerations, acromioclavicular (AC) sprains, and knee injuries, most often due to collisions. 30,65,76,77,84,87
Intra-articular Hip Injuries
The rate of intra-articular hip injuries was 2.63 per 1000 AEs, with most occurring in a regular season game. 12,13,21,40 Goalkeepers and older players were significantly more likely to have intra-articular hip pathology (P ≤ .0001). 21 The most frequent intra-articular hip pathology was labral tearing, followed by osteoarthritis, loose body, and femoroacetabular impingement (FAI). 21
Asymptomatic Screening
Multiple studies found high rates of asymptomatic hip labral tears, acetabular retroversion, and cam-type morphology in NHL players, with cam-type morphology correlating with decreased hip range of motion and positive anterior impingement. 26,43,44 Goalkeepers had the highest prevalence of cam-type deformity and the least acetabular coverage. 44 Wörner et al 91 found that over one-half of Swedish professional hockey players reported hip and groin problems. Silvis et al 82 found that 64% of asymptomatic American Hockey League players had magnetic resonance imaging (MRI) findings of hip pathology. Dalton et al 13 analyzed NCAA hockey athletes between 2009 and 2015 and found the most common diagnosis was a muscular strain in 1 of the 24 muscles that act on the hip/groin region. Multiple studies have demonstrated that most collegiate injuries were noncontact, causing <24 hours of time lost. 12,40 Ayeni et al 6 found that junior hockey athletes were more likely to have radiographic findings of cam but not pincer impingement compared with nonathletes.
Hip Arthroscopy
Schallmo et al 78 found that NHL players returned to sport at a significantly greater rate compared with National Basketball Association, National Football League, and Major League Baseball (MLB) athletes after HA (P = .048). NHL players had a significant decrease in performance 1 season after surgery as compared with their baseline (P = .002). 78 Sochacki et al 83 studied 70 NHL players who underwent HA for FAI between 2000 and 2016 and found 90% of athletes returned to sport at an average of 6.8 months, with 1-year NHL career survival rate being 84.4%. Matched control players had significantly longer careers compared with those who had surgery (P = .00002). 83 Menge et al 58 found that, in 60 NHL players undergoing HA for FAI, 67% continued to play professionally a minimum of 5 years after HA, with career length correlating with age at time of surgery. Philippon et al 69 studied 24 professional hockey players who underwent HA for FAI and found that 23 returned to sport. The average time to return to training was 3.4 months, with the average modified Harris Hip Score improving from 70 to 95. 70 McDonald et al 53,54 reviewed 17 NHL athletes who underwent arthroscopic microfracture of the hip and found 82% of athletes returned to play with no change in performance measures.
Bizzini et al 9 followed 5 Swiss national athletes who underwent open surgery for FAI and found average return to gameplay was 9.6 months, with 2 athletes unable to return to their previous level of play.
Trunk and Pelvic Injuries
Groin and Abdominal Strains
Emery et al 20 found an increasing injury rate of groin and abdominal strains in NHL players from 12.99 per 100 players per year in the 1991 season to 19.87 per 100 players in the 1997 season. The majority of injuries were noncontact adductor strains, with a 23.5% recurrence rate. 20 The mean time lost from abdominal injuries was significantly greater compared with groin injuries, which the authors hypothesized was due to abdominal injuries requiring surgery more often compared with groin injuries (P = .0058). 20 Groin injuries were more common in those who completed <18 offseason training sessions and those with an adductor strength <80% of their abductor strength. 19,88,89 Eckard et al 18 found, via the NCAA Injury Surveillance Program, that both hip flexor and adductor strains were often from noncontact injuries, resulting in <24 hours of gametime loss, with hip flexor strains more likely to be recurrent.
Core Muscle Injuries
All NHL players who underwent repair of the external oblique aponeurosis returned to play without complications, although most had decreased assists and games played versus a control group. 10,36,37 Players with ≤6 seasons played were likely to play significantly fewer games in the following 2 seasons postoperatively compared with controls (P = .01). 37 However, players with ≥ seasons had significantly decreased games played and performance in the following 2 seasons postoperatively compared with controls (P = .03). 37
Foot and Ankle Injuries
Fractures
Baker et al 7 found 27 bony injuries in 31 NHL athletes via MRI, with 10 being occult fractures. Direct impact injury was more likely to cause a bony injury, usually occurring in the medial foot or ankle. 7
Sprains
Mollon et al 59 prospectively evaluated high ankle sprains in NHL athletes between 2006 and 2012 and found 81% of these injuries caused an average of 8 games missed. A retrospective review of MRI scans revealed that 62% had complete tears to the anterior inferior tibiofibular ligament, 24% had high-grade partial tears of the anterior inferior tibiofibular ligament, and 43% had a partially torn posterior inferior tibiofibular ligament. 59 Wright et al 92 evaluated 2 NHL teams over a 10-year period and found 14 players were diagnosed with syndesmosis sprains and 5 players were diagnosed with lateral ankle sprains with a mean time to return to games of 45 and 1.4 days, respectively. In NCAA athletes, Roos et al 73 found most lateral ligament ankle sprains occurred during gametime due to contact. Crowley et al 11 examined foot and ankle injuries in NCAA athletes and found that 87% occurred during the regular season, with the most common injury being foot contusions. High ankle sprains accounted for the most severe time loss (>14 days), while foot contusions accounted for the most moderate time lost (<14 days). 11 Mauntel et al 52 examined high ankle sprains in collegiate hockey athletes and found that 69% of injuries occurred during competition.
Knee Injuries
Anterior Cruciate Ligament Injuries
Longstaffe et al 46 reviewed the NHL database between the 2006 and 2016 seasons and found 67 ACL tears among NHL players, with forwards being most susceptible. Compared with controls, NHL athletes with ACL tears had a significant decrease in performance, with no difference in games/seasons played after injury (P = .001). 46 Erickson et al 22 examined 36 NHL athletes undergoing ACL reconstruction (ACLR) between 1990 and 2013 and found a 97% return to the NHL at a mean of 7.8 months. Length of career after ACLR was 4.47 years, with a 2.5% revision rate. 22 There was no significant difference in performance after ACLR when compared with preinjury performance (P = .056). 22 Sikka et al 81 examined ACL injuries in 47 NHL players between 2006 and 2010 and found the average postoperative performance/career length after ACLR was significantly less compared with controls (players without ACL tears matched via those who entered the league within 2 years and were drafted within 2 rounds with similar performance, years of experience, age, height, and weight; 2.8 vs 4.4 years; P = .004); 8.5% of players had a failure of ACLR with an overall 20% reoperation rate, 10.6% of players did not return to play, and 8.5% of players were unable to return to play for a full season. 81 Mai et al 50 examined professional athletes in the NHL, National Football League, National Basketball Association, and MLB and found NHL players had higher return to play (95.8% vs 83.4%), shorter average recovery time (258 days vs 367 days), and smallest decrease in performance the season after ACLR compared with all other athletes.
Other Knee Injuries
Schallmo et al 79 examined professional athletes in multiple American sports who underwent knee microfracture and found only NHL and MLB players to have 100% return-to-play rates. Lian et al 45 evaluated the prevalence of patellar tendinitis in Norwegian professional athletes and found an overall prevalence of 13% in hockey athletes. Hockey players were least symptomatic of all athletes, owing to the lack of jumping required in hockey. 45 Grant et al 28 followed a single varsity NCAA hockey team between 2003 and 2011 and found 13 MCL injuries in 10 athletes, with an overall injury rate of 0.44 per 1000 AEs. The majority were Grade 2 sprains due to contact, and the grade of injury correlated with time lost from play. 28
Hand and Wrist Injuries
Greditzer et al 29 reported a prevalence of 81% of os styloideum in NHL players, which was significantly increased when compared with the other population (P < .001). Rovere et al 75 examined “gamekeeper’s thumb” sustained from fighting in minor league players between 1973 and 1975 and found all hockey players were treated successfully with a thumb spica cast, resulting in no residual thumb-index pinch instability or time lost secondary to injury.
Shoulder Injuries
Screening via MRI
Hacken et al 31 reported MRI findings on 25 asymptomatic hockey players and demonstrated labral tears in 25%, with 75% found in the nondominant stick hand. The authors reported 8% of AC joint abnormalities without separation, with 75% of these abnormalities in the dominant shoulders; 6% of athletes had rotator cuff tears. 31 Shoulder pathology overall was significantly more common in the dominant shoulder (P = .021). 31 In contrast, Dwyer et al 17 reported MRI findings of 24 NHL players who sustained traumatic injury with description of acute subluxation or dislocation. They found 75% of players had Bankart lesions, 54.2% had a Hill-Sachs lesion, 20.8% had a Type 2 superior labrum anterior to posterior tear, and 8.3% had isolated posterior labral tears; 12.5% of players had a glenoid bony defect, all of which were <25% of the anteroinferior glenoid. 17
Nonspecific Shoulder Injuries
Gil et al 27 reported an incidence of 0.60 per 10,000 AEs for operative UE injuries in collegiate athletes. Similarly, Melvin et al 57 found the most commonly injured positions were forward (55.1%) and defenseman (29.7%). The shoulder was the most common site injured (54.4%), followed by the hand and wrist (18.9% and 13.8%, respectively). 57 The most common injuries were sprains (40.4%), contusions (19.9%), and fractures (9.5%). 57 The most common UE injury was partial or complete AC joint sprains, most frequently from in-game contact. 57
Clavicle and AC Joint Pathology
Norfray et al 63 analyzed clavicle radiographs of 77 NHL players and found 8 ligamentous injuries, with 6 AC joint subluxations and 2 AC joint dislocations, and 2 players with distal clavicle fractures. Follow-up radiographs demonstrated coracoclavicular ligament calcifications in 2 players with dislocation, 1 player after distal clavicle surgical excision after failed nonoperative treatment of AC joint subluxation, and 1 player with posttraumatic osteoarthritis. 63 Hebert-Davies and Agel 32 reported average time from injury to return to play after clavicle fracture was 65.0 and 97.6 days for operative and nonoperative treatment, respectively, although this finding was not found to be statistically significant. Hibberd et al 33 examined AC joint sprains in collegiate athletes and found the most commonly injured positions were forwards (57.5%) and defenseman (29.1%), with 37.9% of these sprains resulting in no time lost, whereas 11.1% of these sprains were diagnosed as severe (defined as >3 weeks’ time lost or season ending).
Glenohumeral Instability
Hovelius 34 examined 63 Swedish hockey players with shoulder dislocations and found all players were <30 years of age at the first dislocation, with recurrence rates of 90% in players <20 years of age and 50% in players >25 years of age. Rangavajjula et al 72 reported on 11 NHL players who returned to play at an average of 4.3 months after arthroscopic labral repair. No significant difference was found regarding hand dominance or performance after return to play (P = .632). 72
Spine Injuries
Other Injury Characteristics
Zupon et al 93 found most spine injuries in NCAA athletes occurred in competition, and 65.9% resulted in no time lost from play. In games, 39.2% of injuries occurred in the cervical spine, and 40.0% occurred in the lumbar spine, with the majority of the injuries being classified as pain or spasms. 93 The most common injury mechanism in games was contact and in training was noncontact (33.3%) or overuse (21.9%). 93 Fett et al 24 showed a significantly higher prevalence of back pain in German hockey players compared with all other German athletes (P = .018).
Cervical Spine
Mai et al 51 reported on NHL players treated operatively for cervical disc herniation and showed no significant decrease in performance postoperatively (P = .41). For NHL players undergoing anterior cervical diskectomy and fusion (ACDF), Watkins et al 90 reported radiographic union at an average of 7.3 months.
Lumbar Spine
NHL players with lumbar disc herniations had a >80% return-to-play rate at an average of 2.9 years after diagnosis, with a significant decrease in games played and performance (P < .05). 35,80 Those treated nonoperatively returned to sport at a greater rate and played more games, but they had a significant decrease in performance compared with those treated surgically (P < .02). 80 Donaldson 15 examined junior hockey players with low back pain and found 44% of players had evidence of lumbar spondylolysis. The level of spondylolysis occurred predominantly at L5 (55%), followed by L4 (36%). 15 Spondylolysis occurred on the same side as the player’s shooting side in 73% of cases and most commonly in forwards (67%). 15 Return to play averaged 8 weeks, with 96% of athletes continuing to play at an elite level ranging from juniors to professional. 15
Discussion
To the best of the authors’ knowledge, this is the first scoping review to examine the range of hockey injuries from all levels of elite athletes, from junior through professional level. Not only were most injuries sustained during game play, but there was also an increased risk of facial or head/neck injuries in the professional leagues. Most studies focused on nonanatomic-specific injuries, followed by intra-articular hip injuries, with the majority having level 4 evidence.
Based on injury rates seen per AE, most injuries occurred in games compared with training. †† Gameplay, regardless of level, lends itself to producing more injuries due to the higher speed of play and increased rates of body checking as compared with practice, where portions of play are often dedicated to skill-specific training and installation of offensive and defensive sets. The highest injury rates were seen in athletes at the international or junior level, while the lowest rates were seen in collegiate athletes. ‡‡ This low rate of injuries among collegiate athletes is likely related to the rules regarding allowable contact. In collegiate hockey, body checking, or the act of the player physically using the body first to deliberately cause collisions, is strictly forbidden. Contrarily, there are more liberal rules in professional leagues with respect to body checking and player-to-player contact, yielding higher injury rates.
The highest injury rates seen in training were in those competing in professional Asian leagues, followed by those at the junior level, likely due to the demanding and rigorous training schedules these athletes must endure to stay competitive at such a high level. 42,84 Athletes in professional European leagues were least likely to get injured during practice. 38,48,67 The majority of studies reported that the most common injuries were facial injuries, followed by LE injuries, especially in professional players. §§ Collegiate athletes had comparatively lower rates of facial injuries, likely due to the required use of face shields. 56 This disparity in facial injuries when comparing collegiate athletes with others does obviate the question of whether or not protective shields (full or half) should be required among the professional leagues. However, most facial injuries (nonconcussion injuries) sustained are minor in nature and do not account for missed games. 47 In addition, there would likely be player opposition to such a proposed change because of some athletes' perceived decrease in visibility with either a half or full shield as compared with no shield. Another significant difference in professional leagues that can result in an increase in facial injuries is fighting. Although fighting is met with subsequent penalization for both parties in professional leagues, the act of fisticuffs is neither forbidden nor immediately stopped by the referees.
The most common LE injury was the knee, whereas in the UE, it was the shoulder. 57,86 Players’ shoulders are often the first thing that is contacted by either another player or when up against the boards, resulting in a high rate of injury to this anatomic area. In addition, older players were more likely to get injured, likely due to loss of conditioning/reduced peak performance or from years of prolonged exposure to physical contact due to the nature of the sport. 19,21,61
The most commonly injured position was forwards, followed by defenseman then goalkeepers. 38,42,46,48,56,65,66,71 Forwards are injured most commonly due to the elevated speed with which they play, and they are also commonly of smaller stature as compared with the defenseman against whom they are competing. Also, forwards are more commonly the position that receives a body check to disengage them from the puck as opposed to the defensive player who typically initiates contact. Interestingly, arenas with flexible boards and glass have reduced the risk of injury by 29%. 86 This finding is not only interesting but also provides initial evidence that ice hockey rinks should be fitted with flexible boards and glass throughout all of levels of play. This is certainly an area where future research should focus to facilitate injury reduction especially at levels where checking into the boards is allowed.
For hip injuries, hockey athletes had an increased incidence of cam but not pincer deformity, and goalkeepers had the highest prevalence of intra-articular hip pathology. 6,21,43,44 The most frequent intra-articular hip pathology was a labral tear. Over 90% of athletes returned to sport after arthroscopic hip surgery at an average of 6.8 months with no decrease in postoperative performace. 21,58,70,78,83 Hip flexor/adductor strains are common injuries, frequently resulting in <24 hours of game time lost, although hip flexor strains were more likely to be recurrent. 18
Trunk/pelvic injuries are a common yet preventable injury, as athletes who performed more off-season training sessions or implemented a preseason exercise program were less likely to sustain trunk injuries. 20,88,89 Understanding this fact can play a critical role in hockey-specific training programs that focus on core/trunk training. Providing a preseason focus on strengthening this area will serve to limit the incidence of these preventable injuries and thus decrease games/practices missed. However, regardless of preseason training, these injuries will occur due to the contact nature of hockey and the rotational forces present in the trunk/core musculature. It is important to note that, for those athletes with core injuries that did require surgical repair, 80% returned to sport, although their performance overall decreased. 10,36,37
We found that ACL injuries occurred with less frequency as compared with other hockey injuries, likely owing to the lack of both jumping and hard pivoting in hockey compared with other sports. Those hockey athletes who did sustain ACL tears were likely to be forwards because of the increased speed and sudden change of direction necessitated by this position. 46 ACLR in hockey players is a more successful procedure compared with ACLR in athletes of other sports, with hockey athletes having a higher return to play and shorter recovery rate. 22,50 However, after ACLR, hockey players had decreased performance with a shorter length of career compared with healthy controls. 46,50,81 Knee microfracture was also found to be a successful procedure, with hockey athletes returning to play at a higher rate compared with athletes in other sports. 79
Our results indicated that the most common shoulder injury was an AC joint sprain secondary to direct contact, although studies were conflicted about whether hand dominance is a factor. 17,31,33,57 For clavicle fractures, hockey athletes treated operatively returned to play sooner compared with those treated nonoperatively, although this finding was not found to be significant (65 vs 97.6 days). 32
We found that lumbar disc herniations were common in hockey players and respond well to both nonoperative and operative treatment, with those treated nonoperatively returning to sport at a higher rate but with lower performance. 24,35,80,93 Lower back injuries occurred more commonly in gameplay due to contact injuries, while those sustained in practice were more likely to be due to noncontact overuse injuries. 93
Limitations
There are limitations to this scoping review. Inherent to the review design, we were reliant on previously published information. Very few studies have been published for thigh, hand, and wrist injuries in hockey athletes probably because of the scarcity of these injuries. Most included studies were of lower-quality evidence (level 3 or 4). However, this seems appropriate, as all studies included examined descriptive data pertaining to injuries in hockey athletes. There were multiple studies included that obtained their data via an internet-based search of publicly available data (eg, injury reports, player profiles, and press releases). Data collected in this manner are not standardized and may not produce reliable estimates. Also, publicly available data are limited and do not provide access to detailed medical records. In addition, we found that 20% of studies collected data from a single team, and therefore, the results of these studies may not be generalizable to all hockey athletes. Multiple studies also collected data via a survey of team physicians and/or athletic trainers and thus were subject to recall bias and nonresponse. Studies captured were performed between 1975 and 2020, and observed changes in injury types, rates, and return to play are likely subject to rule changes/enforcement, training methods, safety equipment advances, and injury treatment methods over time.
Conclusion
This scoping review provides men’s hockey players and physicians taking care of ice hockey athletes of all levels with a comprehensive single source of the most current literature regarding the frequency and outcomes of orthopaedic injuries in these athletes, allowing those taking care of these athletes to quickly and accurately gather the most up-to-date information regarding their prognosis and treatment.
Final revision submitted December 14, 2021; accepted December 31, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: P.T.O. has received education payments from Liberty Surgical, Summit Surgical, and Smith & Nephew. P.D. has received education payments from Liberty Surgical. J.P.S. has received education payments from Liberty Surgical and consulting fees from Stryker. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Agel J, Harvey EJ. A 7-year review of men’s and women’s ice hockey injuries in the NCAA. Can J Surg. 2010;53(5):319–323. [PMC free article] [PubMed] [Google Scholar]
- 2. Agel J, Rockwood T, Klossner D. Collegiate ACL injury rates across 15 Sports: National Collegiate Athletic Association injury surveillance system data update (2004-2005 through 2012-2013). Clin J Sport Med. 2016;26(6):518–523. [DOI] [PubMed] [Google Scholar]
- 3. Åman M, Forssblad M, Larsén K. Incidence and body location of reported acute sport injuries in seven sports using a national insurance database. Scand J Med Sci Sports. 2018;28(3):1147–1158. [DOI] [PubMed] [Google Scholar]
- 4. Åman M, Forssblad M, Larsén K. National injury prevention measures in team sports should focus on knee, head, and severe upper limb injuries. Knee Surg Sports Traumatol Arthrosc. 2019;27(3):1000–1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Anderson GR, Melugin HP, Stuart MJ. Epidemiology of injuries in ice hockey. Sports Health. 2019;11(6):514–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ayeni OR, Banga K, Bhandari M. Femoroacetabular impingement in elite ice hockey players. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):920–925. [DOI] [PubMed] [Google Scholar]
- 7. Baker JC, Hoover EG, Hillen TJ, Smith MV, Wright RW, Rubin DA. Subradiographic foot and ankle fractures and bone contusions detected by MRI in elite ice hockey players. Am J Sports Med. 2016;44(5):1317–1323. [DOI] [PubMed] [Google Scholar]
- 8. Biasca N, Simmen HP, Bartolozzi AR, Trentz O. Review of typical ice hockey injuries: survey of the North American NHL and Hockey Canada versus European leagues. Unfallchirurg. 1995;98(5):283–288. [PubMed] [Google Scholar]
- 9. Bizzini M, Notzli HP, Maffiuletti NA. Femoroacetabular impingement in professional ice hockey players: a case series of 5 athletes after open surgical decompression of the hip. Am J Sports Med. 2007;35(11):1955–1959. [DOI] [PubMed] [Google Scholar]
- 10. Brown RA, Mascia A, Kinnear DG, Lacroix V, Feldman L, Mulder DS. An 18-year review of sports groin injuries in the elite hockey player: clinical presentation, new diagnostic imaging, treatment, and results. Clin J Sport Med. 2008;18(3):221–226. doi:10.1097/jsm.0b013e318172831a [DOI] [PubMed] [Google Scholar]
- 11. Crowley SG, Trofa DP, Turner Vosseller J. Epidemiology of foot and ankle injuries in National Collegiate Athletic Association men’s and women’s ice hockey. Orthop J Sports Med. 2019;7(8):232596711986590. doi:10.1177/2325967119865908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cruz CA, Kerbel Y, Smith CM, Prodromo J, Trojan JD, Mulcahey MK. A sport-specific analysis of the epidemiology of hip injuries in National Collegiate Athletic Association athletes from 2009 to 2014. Arthroscopy. 2019;35(9):2724–2732. [DOI] [PubMed] [Google Scholar]
- 13. Dalton SL, Zupon AB, Gardner EC, Djoko A, Dompier TP, Kerr ZY. The epidemiology of hip/groin injuries in National Collegiate Athletic Association men’s and women’s ice hockey. Orthop J Sports Med. 2016;4(3):232596711663269. doi:10.1177/2325967116632692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Donaldson L, Li B, Cusimano MD. Economic burden of time lost due to injury in NHL hockey players. Inj Prev. 2014;20(5):347–349. [DOI] [PubMed] [Google Scholar]
- 15. Donaldson LD. Spondylolysis in elite junior-level ice hockey players. Sports Health. 2014;6(4):356–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Donskov AS, Humphreys D, Dickey JP. What is injury in ice hockey: an integrative literature review on injury rates, injury definition, and athlete exposure in men’s elite ice hockey. Sports (Basel). 2019;7(11):227. doi:10.3390/sports7110227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Dwyer T, Petrera M, Bleakney R, Theodoropoulos JS. Shoulder instability in ice hockey players: incidence, mechanism, and MRI findings. Clin J Sport Med. 2013;32(4):803–813. [DOI] [PubMed] [Google Scholar]
- 18. Eckard TG, Padua DA, Dompier TP, Dalton SL, Thorborg K, Kerr ZY. Epidemiology of hip flexor and hip adductor strains in National Collegiate Athletic Association athletes, 2009/2010-2014/2015. Am J Sports Med. 2017;45(12):2713–2722. [DOI] [PubMed] [Google Scholar]
- 19. Emery CA, Meeuwisse WH. Risk factors for groin injuries in hockey. Med Sci Sports Exerc. 2001;33(9):1423–1433. [DOI] [PubMed] [Google Scholar]
- 20. Emery CA, Meeuwisse WH, Powell JW. Groin and abdominal strain injuries in the National Hockey League. Clin J Sport Med. 1999;9(3):151–156. [DOI] [PubMed] [Google Scholar]
- 21. Epstein DM, McHugh M, Yorio M, Neri B. Intra-articular hip injuries in National Hockey League players. Am J Sports Med. 2013;41(2):343–348. doi:10.1177/0363546512467612 [DOI] [PubMed] [Google Scholar]
- 22. Erickson BJ, Harris JD, Cole BJ. Performance and return to sport after anterior cruciate ligament reconstruction in National Hockey League players. Orthop J Sports Med. 2014;2(9):2325967114548831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ferrara MS, Schurr KT. Intercollegiate ice hockey injuries: a causal analysis. Clin J Sport Med. 1999;9(1):30–33. [PubMed] [Google Scholar]
- 24. Fett D, Trompeter K, Platen P. Back pain in elite sports: a cross-sectional study on 1114 athletes. PLoS One. 2017;12(6):e0180130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Flik K, Lyman S, Marx RG. American collegiate men’s ice hockey: an analysis of injuries. Am J Sports Med. 2005;33(2):183–187. [DOI] [PubMed] [Google Scholar]
- 26. Gallo RA, Silvis ML, Smetana B. Asymptomatic hip/groin pathology identified on magnetic resonance imaging of professional hockey players: outcomes and playing status at 4 years’ follow-up. Arthroscopy. 2014;30(10):1222–1228. doi:10.1016/j.arthro.2014.04.100 [DOI] [PubMed] [Google Scholar]
- 27. Gil JA, Goodman AD, DeFroda SF, Owens BD. Characteristics of operative shoulder injuries in the National Collegiate Athletic Association, 2009-2010 through 2013-2014. Orthop J Sports Med. 2018;6(8):2325967118790764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Grant JA, Bedi A, Kurz J, Bancroft R, Miller BS. Incidence and injury characteristics of medial collateral ligament injuries in male collegiate ice hockey players. Sports Health. 2013;5(3):270–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Greditzer HG IV, Hutchinson ID, Geannette CS, Hotchkiss RN, Kelly BT, Potter HG. Prevalence of os styloideum in National Hockey League players. Sports Health. 2017;9(5):469–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Gröger A. Ten years of ice hockey-related-injuries in the German Ice Hockey Federation - a ten year prospective study/523 international games. Sportverletz Sportschaden. 2001;15(4):82–86. doi:10.1055/s-2001-19047 [DOI] [PubMed] [Google Scholar]
- 31. Hacken B, Onks C, Flemming D. Prevalence of MRI shoulder abnormalities in asymptomatic professional and collegiate ice hockey athletes. Orthop J Sports Med. 2019;7(10):2325967119876865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hebert-Davies J, Agel J. Return to elite-level sport after clavicle fractures. BMJ Open Sport Exerc Med. 2018;4(1):e000371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hibberd EE, Kerr ZY, Roos KG, Djoko A, Dompier TP. Epidemiology of acromioclavicular joint sprains in 25 National Collegiate Athletic Association sports: 2009-2010 to 2014-2015 academic years. Am J Sports Med. 2016;44(10):2667–2674. [DOI] [PubMed] [Google Scholar]
- 34. Hovelius L. Shoulder dislocation in Swedish ice hockey players. Am J Sports Med. 1978;6(6):373–377. [DOI] [PubMed] [Google Scholar]
- 35. Hsu WK, McCarthy KJ, Savage JW. The professional athlete spine initiative: outcomes after lumbar disc herniation in 342 elite professional athletes. Spine J. 2011;11(3):180–186. [DOI] [PubMed] [Google Scholar]
- 36. Irshad K, Feldman LS, Lavoie C, Lacroix VJ, Mulder DS, Brown RA. Operative management of “hockey groin syndrome”: 12 years of experience in National Hockey League players. Surgery. 2001;130(4):759–766. [DOI] [PubMed] [Google Scholar]
- 37. Jakoi A, O’Neill C, Damsgaard C, Fehring K, Tom J. Sports hernia in National Hockey League players: does surgery affect performance? Am J Sports Med. 2013;41(1):107–110. [DOI] [PubMed] [Google Scholar]
- 38. Jørgensen U, Schmidt-Olsen S. The epidemiology of ice hockey injuries. Br J Sports Med. 1986;20(1):7–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Junge A, Engebretsen L, Mountjoy ML. Sports injuries during the summer Olympic Games 2008. Am J Sports Med. 2009;37(11):2165–2172. [DOI] [PubMed] [Google Scholar]
- 40. Kerbel YE, Smith CM, Prodromo JP, Nzeogu MI, Mulcahey MK. Epidemiology of hip and groin injuries in collegiate athletes in the United States. Orthop J Sports Med. 2018;6(5):2325967118771676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kerr ZY, Marshall SW, Dompier TP, Corlette J, Klossner DA, Gilchrist J. College sports-related injuries - United States, 2009-10 through 2013-14 academic years. MMWR Morb Mortal Wkly Rep. 2015;64(48):1330–1336. doi:10.15585/mmwr.mm6448a2 [DOI] [PubMed] [Google Scholar]
- 42. Kuzuhara K, Shimamoto H, Mase Y. Ice hockey injuries in a Japanese elite team: a 3- year prospective study. J Athl Train. 2009;44(2):208–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Larson CM, Ross JR, Kuhn AW. Radiographic hip anatomy correlates with range of motion and symptoms in National Hockey League players. Am J Sports Med. 2017;45(7):1633–1639. doi:10.1177/0363546517692542 [DOI] [PubMed] [Google Scholar]
- 44. Lerebours F, Robertson W, Neri B, Schulz B, Youm T, Limpisvasti O. Prevalence of cam- type morphology in elite ice hockey players. Am J Sports Med. 2016;44(4):1024–1030. doi:10.1177/0363546515624671 [DOI] [PubMed] [Google Scholar]
- 45. Lian ØB, Engebretsen L, Bahr R. Prevalence of jumper’s knee among elite athletes from different sports: a cross-sectional study. Am J Sports Med. 2005;33(4):561–567. doi:10.1177/0363546504270454 [DOI] [PubMed] [Google Scholar]
- 46. Longstaffe R, Leiter J, MacDonald P. Anterior cruciate ligament injuries in the National Hockey League: epidemiology and performance impact. Clin J Sport Med. 2020;30(3):224–230. [DOI] [PubMed] [Google Scholar]
- 47. Lorentzon R, Wedrèn H, Pietilä T. Incidence, nature, and causes of ice hockey injuries. Am J Sports Med. 1988;16(4):392–396. doi:10.1177/036354658801600415 [DOI] [PubMed] [Google Scholar]
- 48. Lorentzon R, Wedren H, Pietilä T, Gustavsson B. Injuries in international ice hockey: a prospective, comparative study of injury incidence and injury types in international and Swedish elite ice hockey. Am J Sports Med. 1988;16(4):389–391. [DOI] [PubMed] [Google Scholar]
- 49. Lubbe RJ, Freshman RD, Singh G, et al. Performance outcomes and return-to-sport rate of National Hockey League athletes vary after common orthopedic surgical procedures. Clin J Sport Med. 2021;31(1):57–62. doi:10.1097/JSM.0000000000000696 [DOI] [PubMed] [Google Scholar]
- 50. Mai HT, Chun DS, Schneider AD. Performance-based outcomes after anterior cruciate ligament reconstruction in professional athletes differ between sports. Am J Sports Med. 2017;45(10):2226–2232. [DOI] [PubMed] [Google Scholar]
- 51. Mai HT, Chun DS, Schneider AD, Hecht AC, Maroon JC, Hsu WK. The difference in clinical outcomes after anterior cervical fusion, disk replacement, and foraminotomy in professional athletes. Clin Spine Surg. 2018;31(1):E80–E84. [DOI] [PubMed] [Google Scholar]
- 52. Mauntel TC, Wikstrom EA, Roos KG, Djoko A, Dompier TP, Kerr ZY. The epidemiology of high ankle sprains in National Collegiate Athletic Association sports. Am J Sports Med. 2017;45(9):2156–2163. [DOI] [PubMed] [Google Scholar]
- 53. McDonald JE, Herzog MM, Philippon MJ. Performance outcomes in professional hockey players following arthroscopic treatment of femoroacetabular impingement and microfracture of the hip. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):915–919. [DOI] [PubMed] [Google Scholar]
- 54. McDonald JE, Herzog MM, Philippon MJ. Return to play after hip arthroscopy with microfracture in elite athletes. Arthroscopy. 2013;29(2):330–335. [DOI] [PubMed] [Google Scholar]
- 55. McKay CD, Tufts RJ, Shaffer B, Meeuwisse WH. The epidemiology of professional ice hockey injuries: a prospective report of six NHL seasons. Br J Sports Med. 2014;48(1):57–62. doi:10.1136/bjsports-2013-092860 [DOI] [PubMed] [Google Scholar]
- 56. McKnight CM, Ferrara MS, Czerwinska JM. Intercollegiate ice hockey injuries: a three- year analysis. J Athl Train. 1992;27(4):338–343. [PMC free article] [PubMed] [Google Scholar]
- 57. Melvin PR, Souza S, Nelson Mead R, Smith C, Mulcahey MK. Epidemiology of upper extremity injuries in NCAA men’s and women’s ice hockey. Am J Sports Med. 2018;46(10):2521–2529. doi:10.1177/0363546518781338 [DOI] [PubMed] [Google Scholar]
- 58. Menge TJ, Briggs KK, Philippon MJ. Predictors of length of career after hip arthroscopy for femoroacetabular impingement in professional hockey players. Am J Sports Med. 2016;44(9):2286–2291. [DOI] [PubMed] [Google Scholar]
- 59. Mollon B, Wasserstein D, Murphy GM, White LM, Theodoropoulos J. High ankle sprains in professional ice hockey players: prognosis and correlation between magnetic resonance imaging patterns of injury and return to play. Orthop J Sports Med. 2019;7(9):2325967119871578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Mölsä J, Airaksinen O, Näsman O, Torstila I. Ice hockey injuries in Finland: a prospective epidemiologic study. Am J Sports Med. 1997;25(4):495–499. [DOI] [PubMed] [Google Scholar]
- 61. Mölsä J, Kujala U, Myllynen P, Torstila I, Airaksinen O. Injuries to the upper extremity in ice hockey: analysis of a series of 760 injuries. Am J Sports Med. 2003;31(5):751–757. [DOI] [PubMed] [Google Scholar]
- 62. Mölsä J, Kujala U, Näsman O, Lehtipuu TP, Airaksinen O. Injury profile in ice hockey from the 1970s through the 1990s in Finland. Am J Sports Med. 2000;28(3):322–327. [DOI] [PubMed] [Google Scholar]
- 63. Norfray JF, Tremaine MJ, Groves HC, Bachman DC. The clavicle in hockey. Am J Sports Med. 1977;5(6):275–280. doi:10.1177/036354657700500616 [DOI] [PubMed] [Google Scholar]
- 64. Osborn ZH, Blanton PD, Schwebel DC. Personality and injury risk among professional hockey players. J Inj Violence Res. 2009;1(1):15–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Park RD, Castaldi CR. Injuries in junior ice hockey. Phys Sportsmed. 1980;8(2):81–90. doi:10.1080/00913847.1980.11948563 [DOI] [PubMed] [Google Scholar]
- 66. Pelletier RL, Montelpare WJ, Stark RM. Intercollegiate ice hockey injuries: a case for uniform definitions and reports. Am J Sports Med. 1993;21(1):78–81. [DOI] [PubMed] [Google Scholar]
- 67. Pettersson M, Lorentzon R. Ice hockey injuries: a 4-year prospective study of a Swedish elite ice hockey team. Br J Sports Med. 1993;27(4):251–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Pförringer W, Smasal V. Aspects of traumatology in ice hockey. J Sports Sci. 1987;5(3):327–336. [DOI] [PubMed] [Google Scholar]
- 69. Philippon M, Schenker M, Briggs K, Kuppersmith D. Femoroacetabular impingement in 45 professional athletes: associated pathologies and return to sport following arthroscopic decompression. Knee Surg Sports Traumatol Arthrosc. 2007;15(7):908–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Philippon MJ, Weiss DR, Kuppersmith DA, Briggs KK, Hay CJ. Arthroscopic labral repair and treatment of femoroacetabular impingement in professional hockey players. Am J Sports Med. 2010;38(1):99–104. [DOI] [PubMed] [Google Scholar]
- 71. Pinto M, Kuhn JE, Greenfield ML, Hawkins RJ. Prospective analysis of ice hockey injuries at the junior a level over the course of one season. Clin J Sport Med. 1999;9(2):70–74. [DOI] [PubMed] [Google Scholar]
- 72. Rangavajjula A, Hyatt A, Raneses E, McCrossin J, Cohen S, DeLuca P. Return to play after treatment of shoulder labral tears in professional hockey players. Phys Sportsmed. 2016;44(2):119–125. [DOI] [PubMed] [Google Scholar]
- 73. Roos KG, Kerr ZY, Mauntel TC, Djoko A, Dompier TP, Wikstrom EA. The epidemiology of lateral ligament complex ankle sprains in National Collegiate Athletic Association sports. Am J Sports Med. 2017;45(1):201–209. [DOI] [PubMed] [Google Scholar]
- 74. Rovere GD, Gristina AG, Nicastro JF. Medical problems of a professional hockey team: a three-season experience. Phys Sportsmed. 1978;6(1):58–63. [DOI] [PubMed] [Google Scholar]
- 75. Rovere GD, Gristina AG, Stolzer WA, Garver EM. Treatment of “gamekeeper’s thumb” in hockey players. Am J Sports Med. 1975;3(4):147–151. [DOI] [PubMed] [Google Scholar]
- 76. Ruedl G, Schnitzer M, Kirschner W. Sports injuries and illnesses during the 2015 Winter European Youth Olympic Festival. Br J Sports Med. 2016;50(10):631–636. [DOI] [PubMed] [Google Scholar]
- 77. Ruedl G, Schobersberger W, Pocecco E. Sport injuries and illnesses during the First Winter Youth Olympic Games 2012 in Innsbruck, Austria. Br J Sports Med. 2012;46(15):1030–1037. [DOI] [PubMed] [Google Scholar]
- 78. Schallmo M, Fitzpatrick T, Yancey H, Marquez-Lara A, David Luo T, Stubbs AJ. Return- to-play and performance-based outcomes following hip arthroscopy for American professional athletes in different sports. Arthroscopy. 2018;34(12):e15. doi:10.1016/j.arthro.2018.10.051 [DOI] [PubMed] [Google Scholar]
- 79. Schallmo MS, Singh SK, Barth KA, Freshman RD, Mai HT, Hsu WK. A cross-sport comparison of performance-based outcomes of professional athletes following primary microfracture of the knee. Knee. 2018;25(4):692–698. [DOI] [PubMed] [Google Scholar]
- 80. Schroeder GD, McCarthy KJ, Micev AJ, Terry MA, Hsu WK. Performance-based outcomes after nonoperative treatment, discectomy, and/or fusion for a lumbar disc herniation in National Hockey League Athletes. Am J Sports Med. 2013;41(11):2604–2608. [DOI] [PubMed] [Google Scholar]
- 81. Sikka R, Kurtenbach C, Steubs JT, Boyd JL, Nelson BJ. Anterior cruciate ligament injuries in professional hockey players. Am J Sports Med. 2016;44(2):378–383. [DOI] [PubMed] [Google Scholar]
- 82. Silvis ML, Mosher TJ, Smetana BS. High prevalence of pelvic and hip magnetic resonance imaging findings in asymptomatic collegiate and professional hockey players. Am J Sports Med. 2011;39(4):715–721. [DOI] [PubMed] [Google Scholar]
- 83. Sochacki KR, Jack RA, Hirase T, Vickery J, Harris JD. Performance and return to sport after hip arthroscopy for femoracetabular impingement syndrome in National Hockey League players. J Hip Preserv Surg. 2019;6(3):234–240. doi:10.1093/jhps/hnz030 [Google Scholar]
- 84. Stuart MJ, Smith A. Injuries in Junior A ice hockey: a three-year prospective study. Am J Sports Med. 1995;23(4):458–461. [DOI] [PubMed] [Google Scholar]
- 85. Tegner Y, Lorentzon R. Ice hockey injuries: incidence, nature and causes. Br J Sports Med. 1991;25(2):87–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Tuominen M, Stuart MJ, Aubry M, Kannus P, Parkkari J. Injuries in men’s international ice hockey: a 7-year study of the International Ice Hockey Federation Adult World Championship Tournaments and Olympic Winter Games. Br J Sports Med. 2015;49(1):30–36. doi:10.1136/bjsports-2014-093688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Tuominen M, Stuart MJ, Aubry M, Kannus P, Parkkari J. Injuries in World Junior Ice Hockey Championships between 2006 and 2015. Br J Sports Med. 2017;51(1):36–43. [DOI] [PubMed] [Google Scholar]
- 88. Tyler TF, Nicholas SJ, Campbell RJ, Donellan S, McHugh MP. The effectiveness of a preseason exercise program to prevent adductor muscle strains in professional ice hockey players. Am J Sports Med. 2002;30(5):680–683. [DOI] [PubMed] [Google Scholar]
- 89. Tyler TF, Nicholas SJ, Campbell RJ, McHugh MP. The association of hip strength and flexibility with the incidence of adductor muscle strains in professional ice hockey players. Am J Sports Med. 2001;29(2):124–128. [DOI] [PubMed] [Google Scholar]
- 90. Watkins RG IV, Chang D, Watkins RG III. Return to play after anterior cervical discectomy and fusion in professional athletes. Orthop J Sports Med. 2018;6(6):2325967118779672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Wörner T, Thorborg K, Eek F. High prevalence of hip and groin problems in professional ice hockey players, regardless of playing position. Knee Surg Sports Traumatol Arthrosc. 2020;28(7):2302–2308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Wright RW, Barile RJ, Surprenant DA, Matava MJ. Ankle syndesmosis sprains in National Hockey League players. Am J Sports Med. 2004;32(8):1941–1945. [DOI] [PubMed] [Google Scholar]
- 93. Zupon AB, Kerr ZY, Dalton SL, Dompier TP, Gardner EC. The epidemiology of back/neck/spine injuries in National Collegiate Athletic Association men’s and women’s ice hockey, 2009/2010 to 2014/2015. Res Sports Med. 2018;26(1):13–26. doi:10.1080/15438627.2017.1365295 [DOI] [PubMed] [Google Scholar]