Abstract
Background
The Posttraumatic Stress Disorder Checklist (PCL-5) is the most widely used screening tool in assessing posttraumatic stress disorder symptoms, based on the Diagnostic and Statistical Manual of Mental disorders (DSM-5) criteria. This study aimed to evaluate the psychometric properties of the newly translated Bangla PCL-5.
Methods
A cross-sectional survey was carried out among 10,605 individuals (61.0% male; mean age: 23.6 ± 5.5 [13–71 years]) during May and June 2020, several months after the onset of the COVID-19 outbreak in Bangladesh. The survey included the Bangla PCL-5 and the PHQ-9 depression scale. We used confirmatory factor analysis to test the four-factor DSM-5 model, the six-factor Anhedonia model, and the seven-factor hybrid model.
Results
The Bangla PCL-5 displayed adequate internal consistency (Cronbach’s alpha = 0.90). The Bangla PCL-5 score was significantly correlated with scores of the PHQ-9 depression scale, confirming strong convergent validity. Confirmatory factor analyses indicated the models had a good fit to the data, including the four-factor DSM-5 model, the six-factor Anhedonia model, and the seven-factor hybrid model. Overall, the seven-factor hybrid model exhibited the best fit to the data.
Conclusions
The Bangla PCL-5 appears to be a valid and reliable psychometric screening tool that may be employed in the prospective evaluation of posttraumatic stress disorder in Bangladesh.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12888-022-03920-4.
Keywords: PTSD, PCL-5, Bangla, Depression, Confirmatory factor analysis
Introduction
Bangladesh, a low-middle-income nation with a high population density, is inordinately vulnerable to adverse ecological events due to its geographic location [1]. Indeed, Bangladesh is ranked 9th in the world among the worst affected countries in the 2017 Climate Risk Index, and has consistently ranked in the top 10 on the Long-Term Climate Risk Index for the last two decades [2]. Every year, the country will experience a variety of natural disasters, such as floods, hurricanes, and cyclones, with their attendant consequences of loss of human lives and property. These naturally occurring disasters predispose the general population to an inordinate burden of psychosocial consequences, including acute stress disorder, depression, generalized anxiety disorders, posttraumatic stress disorder (PTSD), sleep disorders, and suicidal ideation [3]. Currently, systematic detection and interventions targeting the psychosocial morbidities of such recurring disasters are not undertaken due to the lack of a robust language-appropriate instrument to assess PTSD particularly in the context of epidemiological surveillance.
PTSD is a common psychiatric condition associated with a stressful experience, and has emerged as a major burden to those affected and to society [4]. Troubles with sleeping, somatic chronic pain, depression, drug abuse, adverse interpersonal relations, and reduced overall wellness are characteristic of PTSD [5, 6]. PTSD follows traumatic events characterized by a typical intrusion symptom pattern, persistence of trauma, avoidance, physiological and emotional numbness, and hypersensitivity [7].
The Posttraumatic Stress Disorder Checklist (PCL) has long been the leading self-reported instrument for assessing PTSD symptoms [8, 9]. Since the popularization of the most recent edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), the PCL has been updated to incorporate additional symptoms and to conform with the four-factor PTSD conceptualization of the DSM (PTSD Checklist for DSM-5 [PCL-5]) and its associated symptom clusters: re-experiencing, avoidance, negative changes in cognition and mood, and increased arousal and reactivity [9, 10]. This transition from the previously outlined three-factor PTSD model in DSM-IV [11], is based on a substantial body of empirical data indicating that this four-factor model better fits the composition of PTSD symptomatology [12, 13].
The PCL-5 [14] consists of 20 items corresponding to the 20 criteria for PTSD outlined in the DSM-5, and includes 4 subscales referring to the 4 symptom clusters mentioned above. It is de facto a modified version of the PCL-4 containing 17 items and three subscales referring to the former three symptom clusters of the DSM-IV [8]. Earlier research on the psychometric properties of the PCL-5 has been promising. In a study of college students, the PCL-5 illustrated positive and significant correlation with depression (convergent validity), proper test–retest reliability, and divergent validity [15]. Such findings are comparable to the psychometric findings in previous versions of the measure [16] and suggest that the PCL-5 has the same psychometric rigor as the previous versions. A PCL-5 cut-off score of 31 to 33 points has been suggested to assess PTSD, and exhibits 88% sensitivity, and 69% specificity [17].
Earlier versions of the PCL were available in multiple languages [18]. However, as far as we know, the PCL-5 is still available in only a few, limited number of languages [9, 19–24]. The PCL-5 exhibited excellent internal consistency for each language including Chinese (α = 0.91), Dutch (α = 0.93), English (α = 0.95), French (α = 0.94), German (α = 0.95), Tagalog (α = 0.95), Turkish (α = 0.94), and Swedish (α = 0.90) [9, 19–24]. For convergent validity, earlier studies reported high correlations ranging from 0.70 to 0.77 between PTSD and depressive symptoms when using the PCL-5 and the Patient Health Questionnaire (PHQ-9) instruments [17, 23, 24]. Likewise, significant correlations (r = 0.60–0.65) were also reported using PCL-5 and other screening instruments for depression (e.g., Center for Epidemiological Studies-Depression Scale [CES-D], Beck Depression Inventory [BDI], Depression Hopkins Symptom Checklist [DHSC], and Montgomery-Asberg Depression Rating Scale [MADRS]) [9, 20, 21, 25]. Despite the fact that the DSM-5 proposed a four-factor model of PTSD (i.e., Re-experiencing [B1-B5], Avoidance [C1-C2], Negative alterations in cognitions and mood [D1-D7], and Alterations in arousal and reactivity [E1-E6]), several studies using confirmatory factor analysis (CFA) found that the DSM-5 model is not suitable for the population studied [15, 26, 27]. Current literature suggests that PTSD can be defined by inclusion of numerous factors: for example, the Anhedonia model, proposed by Liu et al., includes six factors of PTSD (i.e., Re-experiencing [B1-B5], Avoidance [C1-C2], Negative affect [D1-D4], Anhedonia [E1-E3], Dysphoric arousal [H1-H2], Anxious arousal [E1-E2], and Dysphoric arousal [H3-H4]) [26], while Armour et al. proposed a seven-factor hybrid model for PTSD (i.e., Re-experiencing [B1-B5], Avoidance [C1-C2], Negative affect [D1-D4], Anhedonia [E1-E3], Externalizing behaviors [F1-F2], Anxious arousal [G1-G2], and Dysphoric arousal [H1-H2]) [27].
COVID-19 was first reported in Bangladesh on March 8th, 2020 [28, 29], and similar to many other countries rapidly propagated, with more than 310,800 people infected and 4,248 deaths as of August 31st, 2020 [30, 31]. To reduce the spread of SARS-CoV-2, the Government of Bangladesh imposed strict social isolation, home quarantine, and restricted travel measures starting as of March 26th, 2020 [32, 33]. Pandemic-related issues such as spatial distancing, isolation and quarantine, as well as social and economic consequences, have naturally led to a multitude of psychosocial responses, including stress, anger, boredom, fear, frustration, grief, depression, and of course PTSD, [34–37], all of which are common mental health problems that many individuals will experience during and after a crisis [38]. Experiencing or witnessing the suffering imposed by COVID-19 can cause PTSD among survivors, their families, frontline workers, and even the general public [39]. It is further anticipated that the COVID-19 pandemic will result in a high prevalence of psychological problems at the population level, including PTSD [40], and previous studies involving outbreaks of SARS in 2003 [41] and influenza A H1N1 in 2009 [42] have corroborated such assumption.
In the context of COVID-19, this pandemic will likely impose major adverse effects on mental health, and yet there are few studies addressing these issues in Bangladesh, as illustrated by the use of a previously not validated tool in a study that was conducted among the survivors of Rana Plaza collapse [5]. To better address this important problem, the PCL-5 was translated to the Bangla language, and in the current study, we present the validation of this instrument as items of the PCL-5 may now be answered more consistently by participants because the items included refer to the same stressful experience. As indicated above, the PCL-5 is one of the most widely used self-report measures of PTSD [15]. In an earlier study, Islam et al. (2020) suggested the need to conduct a nationwide survey to investigate PTSD symptoms and prevalence during the COVID-19 pandemic [36]. The present study was designed to explore the presence of acute posttraumatic stress symptoms among Bangladeshi people in the several months that have followed the onset of the COVID-19 outbreak in the country, and to ascertain whether the Bangla version of the PCL-5 is suitable for the Bangladeshi cultural framework as a screening instrument.
Methodology
Study design and participants
This present research study utilized a cross-sectional study design with a sample of 10,605 individuals and conducted between May and June 2020, i.e., nearly 3 months after the onset of the COVID-19 outbreak in Bangladesh. A self-reported anonymous questionnaire with informed consent was developed and administered in online. The targeted participants were the general population of Bangladesh, who could speak and understand Bangla. Individuals approached who were unwilling to participate were not included.
Study procedure and adaption of the PCL-5 into Bangla
A convenience sampling technique was implemented, but in light of the pandemic situation, the survey questionnaire was conceived and published in online. The questionnaire took roughly 10 to 15 min to complete. The PCL-5 questionnaire was translated using the widest used guideline [i.e. Beaton et al. (2000)] [43]. Firstly, the questionnaire was translated into Bangla (participants’ language) by 3 expert translators, who after reaching consensus on this final Bangla version, the latter was then back-translated into English (i.e., forward–backward translation) by 3 additional translators. All the copies of the questionnaire were then evaluated and approved by the core research team. A conceptual translation was implemented instead of a literal translation to ensure that the original meaning of an item was preserved while adapting it to the Bangladeshi cultural context.
A pilot test was initially conducted to check the reliability of the questionnaire using 150 participants. Then, using Google Survey Tool and with the help of research assistants selected from different areas of Bangladesh to ensure a high response rate, a web-based survey was carried out.
Measures
To obtain information from participants, a self-reported survey questionnaire was used containing an informed consent form, and questions concerning socio-demographic and psychometric scales (i.e., the PCL-5, and the PHQ-9) [see questionnaire – Supplementary material].
Socio-demographic measures
During the survey, socio-demographic data were collected by asking questions regarding age, sex, education, occupation, marital status, type of family (nuclear versus joint/extended), monthly family income, residence (rural versus urban), and smoking habits (yes versus no). The monthly family income was categorized into the following three classes based on their monthly total family income in Bangladeshi Taka (BDT): < 15,000 BDT, 15,000–30,000 BDT, and > 30,000 BDT [33, 44].
PTSD Checklist for DSM-5 (PCL-5)
The Bangla translated version of the PCL-5 is, exactly as the original English version, a self-reported 20-item scale, and evaluates the presence, severity, and 20 symptoms related to PTSD in the DSM-5 [14]. The scale represents the extent to which an individual is suffering from PTSD. Respondents were asked to fill up the scale in the questionnaire following their feelings in the last month (e.g., “Repeated, disturbing, and unwanted memories of the stressful experience”), on a five-point Liker scale, which ranges from 0 to 4: 0 “Not at all”, 1 “A little bit”, 2 “Moderately”, 3 “Quite a bit”, and 4 “Extremely”. The final score was obtained by summating the 20 items, such that the final score ranges from 0–80. It includes four subscales; i) Re-experience (5 symptoms), ii) Avoidance (2 symptoms), iii) Negative alterations in cognition and mood (7 symptoms), and iv) Alterations in arousal and reactivity (6 symptoms). Moreover, researchers proposed several models by the inclusion of numerous factors: for example, the Anhedonia model, proposed by Liu et al., includes six factors of PTSD (i.e., i) Re-experiencing [5 symptoms], ii) Avoidance [2 symptoms], iii) Negative affect [4 symptoms], iv) Anhedonia [3 symptoms], v) Dysphoric arousal [4 symptoms], and vi) Anxious arousal [2 symptoms]) [26], while Armour et al. proposed a seven-factor hybrid model for PTSD (i.e., i) Re-experiencing [5 symptoms], ii) Avoidance [2 symptoms], iii) Negative affect [4 symptoms], iv) Anhedonia [3 symptoms], v) Externalizing behaviors [2 symptoms], vi) Anxious arousal [2 symptoms], and vi) Dysphoric arousal [2 symptoms]) [27]. In the present study, the psychometric properties of the Bangla PCL-5 scale were evaluated and are presented.
Patient Health Questionnaire (PHQ-9)
The PHQ-9 is the most widely used self-reported screening tool for assessing the severity of depressive disorders [45]. This scale comprises nine items with a four-point Likert scale ranging from 0 (“Not at all”) to 3 (“Nearly every day”). Each item refers to problems experienced including issues with sleep, exhaustion, changes in appetite, difficulties with concentration, and suicidal thoughts are measured over the past two weeks (e.g., “Little interest or pleasure in doing things”). The level of depression varies into five groups as minimal, mild, moderate, moderately severe, and severe based on scoring 0–4, 5–9, 10–14, 15–19, and 20–27 points, respectively. The present study employed the previously validated Bangla PHQ-9 questionnaire to investigate the level of participants’ depressive disorders [46] which has been extensively used [47–50]. In the present study, the PHQ-9 scale was found to have very good reliability (Cronbach’s alpha = 0.89).
Statistical analysis
The data were analyzed using Microsoft Excel 2019, IBM SPSS Statistics version 25, and IBM SPSS Amos version 23. Descriptive statistics (e.g., frequencies, percentages, means, standard deviations, etc.) were performed using SPSS software. To investigate the validity and reliability of the Bangla PCL-5, its properties were examined and reported both at item-level and scale level.
Item-level analysis
For the item-level analysis, means, standard deviations, skewness, and kurtosis were computed. Furthermore, item-total correlations, and Cronbach’s alpha-if item deleted were reported.
Reliability
The internal consistency of the scale and its subscales were examined using reliability coefficients (i.e., Cronbach’s alpha).
Structural validity
CFA was executed to evaluate the structural validity of the Bangla PCL-5 instrument using SPSS Amos. The three most popular models were investigated for confirmatory factor analysis including the DSM-5 four-factor model, the six-factor Anhedonia model [26], and the seven-factor hybrid model [27].
In all of the CFA models, the chi-square (χ2), Root Mean Square Error of Approximation (RMSEA), Standardized Root Mean Square Residual (SRMR), Comparative Fit Index (CFI), Normed Fit Index (NFI), Tucker Lewis Fit Index (TLI), Goodness of Fit Index (GFI), and Adjusted Goodness of Fit (AGFI) were calculated using SPSS Amos. Thresholds and conventional fit indices were applied to investigate the goodness of fit of the model under statistical analysis: RMSEA (0.05;0.08), SRMR (0.05;0.08), CFI (0.90:0.95), GFI (0.90;0.95), AGFI (0.90;0.95), TLI (0.90;0.95), and NFI (0.90;0.95) [51–54].
Furthermore, the Bayesian information criterion (BIC; [55]) and the Akaike information criterion (AIC; [56]) were estimated to evaluate the model fit of these non-nested models. A BIC difference of 6–10 is considered strong support, and a difference of more than 10 is considered very strong support in favor of the model with the lower value [57]. Relatively lower AIC values are usually considered to support a better-fitting model [55].
Convergent validity
The convergent validity of the Bangla PCL-5 instrument and its subscales was evaluated by reporting its correlations with the related instrument (i.e., PHQ-9). The average variance extracted (AVE) and composite reliability (CR) were also calculated to examine convergent validity. According to Fornell and Larcker, convergent validity is supported when the values of CR and AVE fall into the following acceptable thresholds: CR > 0.6 and AVE > 0.5 [58].
Ethical considerations
All procedures of this study were carried out in keeping with the principles of Institutional Research Ethics and The Code of Ethics of the World Medical Association involving human subjects (Declaration of Helsinki). Formal ethics approval was granted by the Ethical Review Committee, Uttara Adhunik Medical College, Uttara, Dhaka-1230, Bangladesh. All data were collected anonymously, and all participants consented to the survey willingly. The consent form was clearly outlined and included i) the purpose and process of the research, ii) aims and objectives of the research, iii) data anonymity and privacy, iv) option to participate in the study, and v) right to withdraw data from studies at any time.
Results
General characteristics of participants
Initially, 10,850 respondents have submitted the survey form after obtaining informed consent. Of these, 10,664 (98.3%) respondents completed the entire survey. After eliminating surveys that were completed but had data missing, 10,605 surveys were included in the final analysis. Of which 61.0% were male with an average age of 23.6 ± 5.5 years, ranging from 13 to 71 years. A sizeable portion of respondents were students (75.2%), and unmarried (84.0%), and had a bachelor’s degree level of education (67.9%) (Table 1). Moreover, the majority of the responders came from urban areas (63.1%), lived in nuclear families (78.9%), and had monthly family income above 30,000 BDT (45.3%). A sizeable portion of respondents reported as being non-smokers (84.6%).
Table 1.
General characteristics of participants (N = 10,605)
| Categorical variables | n | (%) |
|---|---|---|
| Sex | ||
| Male | 6472 | (61.0) |
| Female | 4133 | (39.0) |
| Marital status | ||
| Unmarried | 8903 | (84.0) |
| Married | 1657 | (15.6) |
| Divorced | 45 | (0.4) |
| Educational qualification | ||
| No academic education | 84 | (0.8) |
| Primary (1–5 grades) | 51 | (0.5) |
| Secondary (6–10 grades) | 281 | (2.6) |
| Intermediate (11–12 grades) | 1562 | (14.7) |
| Bachelor | 7202 | (67.9) |
| Higher education (above bachelor) | 1425 | (13.4) |
| Occupation | ||
| Student | 7976 | (75.2) |
| Private employee | 828 | (7.8) |
| Government employee | 342 | (3.2) |
| Housewife | 303 | (2.9) |
| Businessman | 263 | (2.5) |
| Freelancer | 164 | (1.5) |
| Farmer | 59 | (0.6) |
| Day laborer | 39 | (0.4) |
| Unemployed | 478 | (4.5) |
| Retired | 22 | (0.2) |
| Doctor | 48 | (0.5) |
| Others | 83 | (0.8) |
| Family type | ||
| Nuclear | 8369 | (78.9) |
| Join | 2236 | (21.1) |
| Monthly family income | ||
| < 15,000 BDT | 1983 | (18.7) |
| 15,000–30,000 BDT | 3817 | (36.0) |
| > 30,000 BDT | 4805 | (45.3) |
| Residence | ||
| Urban area | 6696 | (63.1) |
| Rural area | 3909 | (36.9) |
| Smoking habits | ||
| Yes | 1634 | (15.4) |
| No | 8971 | (84.6) |
| Continuous variables | Mean | (SD) |
| Age | 23.77 | (5.46) |
Item-level analysis
Table 2 presents the mean, standard deviation, item-total correlation, Cronbach’s alpha of the scale if each item is omitted, as well as Skewness and Kurtosis of each translated PCL-5 item. The item-total correlation (Table 2) contained no negative values, indicating that the items were assessing the same construct. All items yielded Skewness and Kurtosis values within the ± 2.0 range, indicating that they were normally distributed [59].
Table 2.
Item-level psychometric properties of the Bangla PCL-5
| PCL-5 item | Mean (SD) | Median | Item-total correlation | Skewness | Kurtosis | Cronbach's α if Item Deleted |
|---|---|---|---|---|---|---|
| 1 | 2.13 (1.21) | 2 | 0.43 | 0.04 | -1.14 | 0.89 |
| 2 | 1.02 (1.13) | 1 | 0.54 | 1.04 | 0.18 | 0.89 |
| 3 | 1.95 (1.26) | 2 | 0.43 | 0.21 | -1.15 | 0.89 |
| 4 | 2.14 (1.3) | 2 | 0.49 | 0.02 | -1.25 | 0.89 |
| 5 | 0.9 (1.11) | 1 | 0.55 | 1.16 | 0.46 | 0.89 |
| 6 | 1.72 (1.22) | 1 | 0.40 | 0.32 | -0.92 | 0.90 |
| 7 | 1.68 (1.28) | 1 | 0.39 | 0.35 | -0.97 | 0.90 |
| 8 | 0.99 (1.13) | 1 | 0.50 | 1.01 | 0.08 | 0.89 |
| 9 | 1.22 (1.27) | 1 | 0.59 | 0.82 | -0.45 | 0.89 |
| 10 | 1.02 (1.2) | 1 | 0.53 | 1.01 | -0.03 | 0.89 |
| 11 | 1.48 (1.28) | 1 | 0.56 | 0.53 | -0.83 | 0.89 |
| 12 | 1.45 (1.26) | 1 | 0.61 | 0.61 | -0.77 | 0.89 |
| 13 | 1.62 (1.39) | 1 | 0.61 | 0.44 | -1.14 | 0.89 |
| 14 | 1.15 (1.26) | 1 | 0.59 | 0.89 | -0.36 | 0.89 |
| 15 | 1.53 (1.34) | 1 | 0.63 | 0.53 | -0.97 | 0.89 |
| 16 | 0.93 (1.19) | 0 | 0.50 | 1.12 | 0.15 | 0.89 |
| 17 | 1.57 (1.21) | 1 | 0.23 | 0.40 | -0.84 | 0.90 |
| 18 | 1.23 (1.24) | 1 | 0.63 | 0.77 | -0.52 | 0.89 |
| 19 | 1.59 (1.34) | 1 | 0.63 | 0.48 | -1.02 | 0.89 |
| 20 | 1.36 (1.36) | 1 | 0.55 | 0.65 | -0.88 | 0.89 |
Reliability
Cronbach’s alpha for the total score and each of the subscales of the Bangla PCL-5 instrument are presented in Table 3. The coefficients of Cronbach’s alpha were calculated to investigate internal consistency. Cronbach’s alpha for the total PCL-5 was 0.90, indicating excellent internal consistency, which is well beyond the accepted threshold of 0.70 [58, 60].
Table 3.
The descriptive statistics, and Cronbach’s alpha of each scale/subscale, and correlations among all scales along with subscales
| Scales/subscales | Mean (SD) | Item Range | α | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. R | 8.14 (4.26) | 5 (0–20) | 0.75 | ― | |||||||||
| 2. A | 3.40 (2.10) | 2 (0–8) | 0.58 | 0.43* | ― | ||||||||
| 3. NACM | 8.92 (6.18) | 7 (0–28) | 0.83 | 0.52* | 0.38* | ― | |||||||
| 4. AR | 8.20 (5.20) | 6 (0–24) | 0.76 | 0.54* | 0.36* | 0.73* | ― | ||||||
| 5. NA | 4.71 (3.67) | 4 (0–16) | 0.74 | 0.47* | 0.35* | 0.91* | 0.64* | ― | |||||
| 6. An | 4.21 (3.21) | 3 (0–12) | 0.76 | 0.47* | 0.32* | 0.88* | 0.67* | 0.61* | ― | ||||
| 7. DA | 5.41 (3.95) | 4 (0–16) | 0.75 | 0.50* | 0.32* | 0.73* | 0.95* | 0.63* | 0.69* | ― | |||
| 8. AA | 2.80 (1.92) | 2 (0–8) | 0.37 | 0.43* | 0.31* | 0.45* | 0.76* | 0.42* | 0.39* | 0.51* | ― | ||
| 9. EB | 2.46 (2.12) | 2 (0–8) | 0.58 | 0.41* | 0.27* | 0.68* | 0.84* | 0.59* | 0.63* | 0.88* | 0.47* | ― | |
| 10. Total PCL-5 | 28.66 (14.52) | 20 (0–80) | 0.90 | 0.77* | 0.56* | 0.89* | 0.88* | 0.80* | 0.80* | 0.84* | 0.64* | 0.75* | ― |
| 11. Total PHQ-9 | 9.02 (6.81) | 9 (0–27) | 0.89 | 0.44* | 0.26* | 0.67* | 0.67* | 0.58* | 0.64* | 0.70* | 0.36* | 0.59* | 0.69* |
SD Standard deviation, α Cronbach alpha, R Re-experiencing, A Avoidance, NACM Negative alterations in cognitions and mood, AR Alterations in arousal and reactivity, NA Negative affect, An Anhedonia, DA Dysphoric arousal, AA Anxious arousal, EB Externalizing behaviors, PCL-5 Posttraumatic Stress Disorder Checklist, PHQ-9 Patient Health Questionnaire; *p < 0.001
Construct validity
CFA was performed to appraise the structural validity of the Bangla PCL-5 instrument using the DSM-5 four-factor model, the six-factor Anhedonia model, and the seven-factor hybrid model. Each of the CFA models, the Absolute Fit (i.e., χ2, RMSEA, SRMR, GFI), and the Incremental Fit (i.e., AGFI, CFI, TLI, NFI) were observed for the model fit estimation (see Table 4). All fitness indexes were satisfactory within their conventional thresholds, which the models displaying an excellent fit to the data. Of these, the seven-factor hybrid model exhibited the best fit to the data (see Table 4). Furthermore, AIC and BIC values also support the seven-factor hybrid model, as this model also exhibited the lowest AIC and BIC values.
Table 4.
Scale-level psychometric properties of the Bangla PCL-5
| Name of index | Index Abbreviation | Four-factor DSM-5 model | Six-factor Anhedonia model | Seven-factor Hybrid model | Level of acceptance |
|---|---|---|---|---|---|
| Absolute Fit | |||||
| Discrepancy chi square | χ2 (df) | 7905.8* (164) | 6243.7* (155) | 5967.0* (149) | p > 0.05 |
|
Root Mean Square Error of Approximation 90% Confidence interval |
RMSEA 90% CI | 0.08 (0.065–0.068) | 0.06 (0.060–0.062) | 0.06 (0.059–0.062) | < 0.08 |
| Standardized Root Mean Square Residual | SRMR | 0.05 | 0.05 | 0.05 | < 0.08 |
| The goodness of Fit Index | GFI | 0.92 | 0.93 | 0.94 | > 0.9 |
| Incremental Fit | |||||
| Adjusted Goodness of Fit | AGFI | 0.9 | 0.91 | 0.91 | > 0.9 |
| Comparative Fit Index | CFI | 0.9 | 0.91 | 0.92 | > 0.9 |
| Tucker-Lewis Index | TLI | 0.9 | 0.9 | 0.9 | > 0.9 |
| Normed Fit Index | NFI | 0.9 | 0.91 | 0.92 | > 0.9 |
| Information Criteria | |||||
| Akaike Information Criterion | AIC | 7997.84 | 6353.69 | 6089.01 | Lower indicating better fit |
| Bayesian Information Criterion | BIC | 8332.22 | 6753.49 | 6532.42 | Lower indicating better fit |
| Reliability | |||||
| Composite Reliability | CR | 0.93 | 0.93 | 0.94 | > 0.6 |
| Average Variance Extracted | AVE | 0.39 | 0.39 | 0.43 | > 0.5 |
*p < 0.001
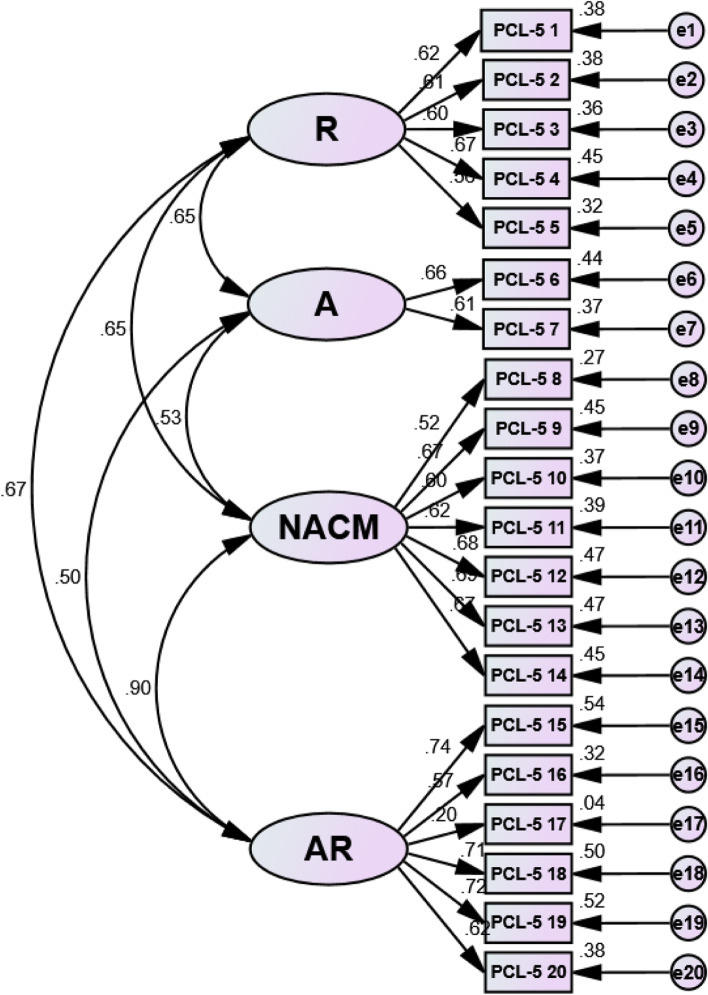
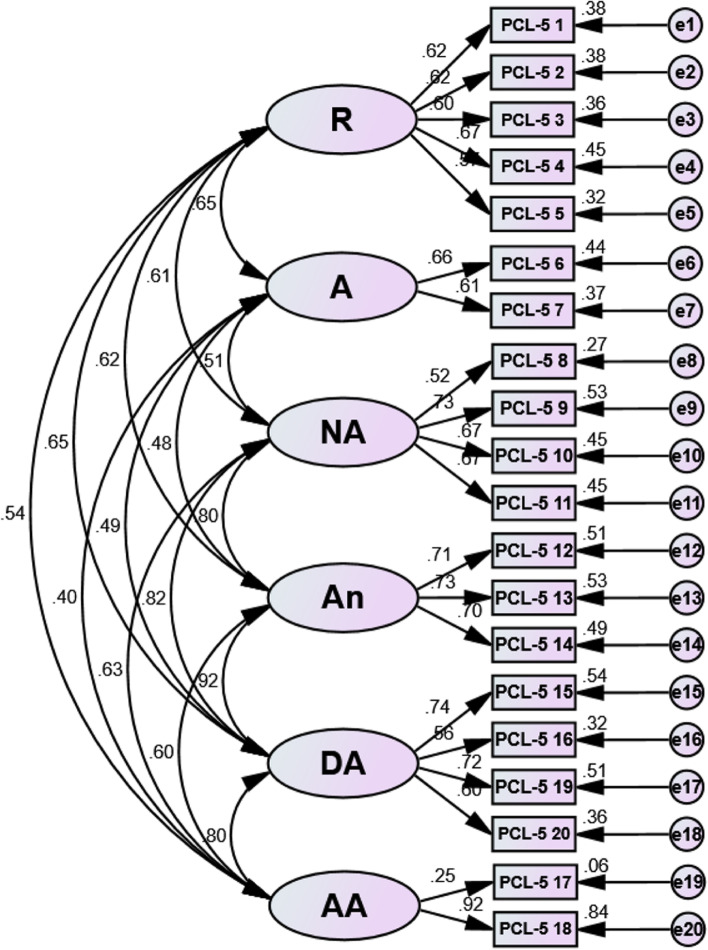
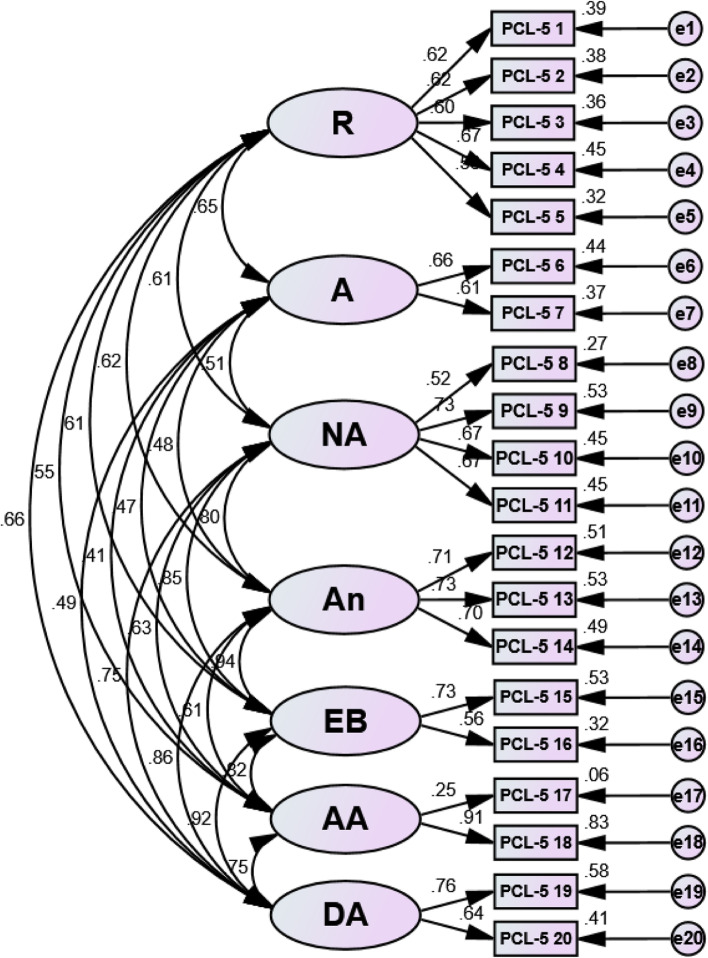
Factor loadings for each model of the Bangla PCL-5 ranged between 0.52 and 0.92 (see Table 5) except item no 17. The acceptability factor was greater than the load value of 0.32 [61]. Structural equation modeling (SEM) revealed a positive correlation between each latent variable in all examined three models – the DSM-5 four-factor model, the six-factor Anhedonia model, and the seven-factor hybrid model, respectively (see ― Figs. 1, 2 and 3), indicating that the items were assessing the same construct.
Table 5.
Standardized factor loading estimates for confirmatory factor analysis models
| DSM-5 symptoms | Four-factor DSM-5 model | Six-factor Anhedonia model | Seven-factor Hybrid model |
|||
|---|---|---|---|---|---|---|
| Factor | Factor Loads | Factor | Factor Loads | Factor | Factor Loads | |
| 1. Repeated memories | R | 0.62 | R | 0.62 | R | 0.62 |
| 2. Repeated dreams | R | 0.62 | R | 0.62 | R | 0.62 |
| 3. Flashbacks | R | 0.60 | R | 0.60 | R | 0.60 |
| 4. Upset when reminded | R | 0.68 | R | 0.67 | R | 0.67 |
| 5. Physical reaction when reminded | R | 0.57 | R | 0.57 | R | 0.56 |
| 6. Avoidance of thoughts | A | 0.66 | A | 0.66 | A | 0.66 |
| 7. Avoidance of reminders | A | 0.61 | A | 0.61 | A | 0.61 |
| 8. Trouble remembering | NACM | 0.52 | NA | 0.52 | NA | 0.52 |
| 9. Negative beliefs | NACM | 0.67 | NA | 0.73 | NA | 0.73 |
| 10. Blame of self or others | NACM | 0.60 | NA | 0.67 | NA | 0.67 |
| 11. Negative feelings | NACM | 0.62 | NA | 0.67 | NA | 0.67 |
| 12. Loss of interest | NACM | 0.68 | An | 0.71 | An | 0.71 |
| 13. Feeling distant | NACM | 0.69 | An | 0.73 | An | 0.73 |
| 14. Trouble positive feelings | NACM | 0.67 | An | 0.70 | An | 0.70 |
| 15. Irritable behavior | AR | 0.74 | DA | 0.74 | EB | 0.73 |
| 16. Reckless behavior | AR | 0.57 | DA | 0.56 | EB | 0.56 |
| 17. Being super alert | AR | 0.21 | AA | 0.25 | AA | 0.25 |
| 18. Feeling jumpy | AR | 0.71 | AA | 0.92 | AA | 0.91 |
| 19. Difficulty concentrating | AR | 0.72 | DA | 0.72 | DA | 0.76 |
| 20. Trouble sleeping | AR | 0.62 | DA | 0.60 | DA | 0.64 |
R Re-experiencing, A Avoidance, NACM Negative alterations in cognitions and mood, AR Alterations in arousal and reactivity, NA Negative affect, An Anhedonia, DA Dysphoric arousal, AA Anxious arousal, EB Externalizing behaviors
Fig. 1.
Structural equation modeling (SEM) of the DSM-5 four-factor model. Note: R = Re-experiencing; A = Avoidance; NACM = Negative alterations in cognitions and mood; AR = Alterations in arousal and reactivity
Fig. 2.
Structural equation modeling (SEM) of the six-factor Anhedonia model. Note: R = Re-experiencing; A = Avoidance; NA = Negative affect; An = Anhedonia; DA = Dysphoric arousal; AA = Anxious arousal
Fig. 3.
Structural equation modeling (SEM) of the seven-factor hybrid model. Note: R = Re-experiencing; A = Avoidance; NA = Negative affect; An = Anhedonia; EB = Externalizing behaviors; AA = Anxious arousal; DA = Dysphoric arousal
Convergent validity
To evaluate the convergent validity of the Bangla PCL-5 instrument, its total, as well as its subscales correlations with the PHQ-9 instrument, are outlined in Table 3. The correlation between the Bangla PCL-5 and the PHQ-9 generated a significant and positive correlation (r = 0.69, p < 0.001), confirming strong convergent validity. Furthermore, the correlation between the PCL-5 subscales and PHQ-9 scale yielded a positive correlation in each case (i.e., Re-experiencing: r = 0.44; Avoidance: r = 0.26; Negative alterations in cognitions and mood: r = 0.67; Arousal: r = 0.67; Negative affect = 0.58; Anhedonia = 0.64; Dysphoric arousal = 0.70; Anxious arousal = 0.36; Externalizing behaviors = 0.59; p < 0.001 for all comparisons).
The values of AVE and CR of the three models ranged between 0.93–0.94, and 0.39–0.43, respectively (see Table 4). The convergent validity is supported if the CR is higher than 0.6, and the AVE is higher than 0.5 for each construct [58]. According to Fornell and Larcker, if the AVE is less than 0.5, but the CR is higher than 0.6, the convergent validity of the construct is still adequate [58].
Discussion
The present study aimed to translate and validate the Bangla PCL-5 in a large cohort in Bangladesh after at least nearly months from the beginning of the COVID-19 outbreak, and as such enable the use of the most widely used psychometric tool to assess PTSD. Several studies conducted with different cohorts including general population, university students, medical students, slum-dwellers, health workers, and COVID-19 survivors highlighted various mental health problems (e.g., anxiety, depression, panic, stress, suicidal ideation, and behavioral problems such as problematic use of smartphone, internet, social media) in Bangladesh during the pandemic [32, 34, 37, 49, 62–68]. These mental health problems can increase the prevalence of PTSD as a result of experiences related to the COVID-19 pandemic [69]. Several studies corroborated that PTSD was prevalent during the COVID-19 pandemic in other countries, including in China (2.7%-12.8%) [70–72], Saudi Arabia (19.6%-24.8%) [69], Italy (29.5%) [73], Spain (15.8%) [74], and in the USA (31.8%) [75]. Thus, a nationwide study would be desirable to investigate PTSD in Bangladesh. Considering the lack of currently available validated instruments for assessing PTSD, the study findings should contribute to future studies aimed at investigating PTSD in Bangladesh.
The Bangla PCL-5 emerged as psychometrically sound and as a robust instrument since it demonstrated (i) excellent internal consistency and reliability, (ii) construct validity, and (iii) strong convergent validity. The findings suggest that Bangla PCL-5 is a valid and potentially useful tool to assess posttraumatic stress disorder among Bangladeshi people.
The findings revealed excellent internal consistency of the Bangla version of PCL-5, which was similar to previous studies in different languages [9, 20–24]. The Cronbach’s alpha of the subscales of the Bangla PCL-5 was also very similar to the aforementioned studies examining translations into different languages. The inter-item correlation matrix yielded positive values across all items, indicating that these items were assessing the same construct. All items had Skewness and Kurtosis values within the ± 2.0 range, indicating that they were normally distributed [59]. Accordingly, the Bangla PCL-5 showed significant validity at this stage of assessment and performed similarly to previous efforts to translate the instrument in other countries.
The construct validity of the Bangla PCL-5 was also corroborated by confirmatory factor analysis using the DSM-5 four-factor model (i.e., Re-experiencing [B1-B5], Avoidance [C1-C2], Negative alterations in cognitions and mood [D1-D7], and Alterations in arousal and reactivity [E1-E6]) [14], the six-factor Anhedonia model (i.e., Re-experiencing [B1-B5], Avoidance [C1-C2], Negative affect [D1-D4], Anhedonia [E1-E3], Dysphoric arousal [H1-H2], Anxious arousal [E1-E2], and Dysphoric arousal [H3-H4]) [26], and the seven-factor hybrid model (i.e., Re-experiencing [B1-B5], Avoidance [C1-C2], Negative affect [D1-D4], Anhedonia [E1-E3], Externalizing behaviors [F1-F2], Anxious arousal [G1-G2], and Dysphoric arousal [H1-H2]) [27]. Within their conventional thresholds, all fitness indices were highly satisfactory, indicating that the models were an excellent fit to the data. Of these, the seven-factor hybrid model exhibited the best fit (see Table 4).. The findings resonate with the previous studies that reported that the seven-factor hybrid model is the best fitting model in diverse populations, including community population [76, 77], treatment-seeking population [78], university students [9], and military personnel [15, 27, 79]. A more recent study conducted among Chinese healthcare workers during the COVID-19 pandemic also found the seven-factor hybrid model as the best fitting model [19].
The correlation between the PCL-5 and depression (using PHQ-9) generated a significant and positive correlation (r = 0.69, p < 0.001), confirming strong convergent validity, a finding that has also been similarly reported in previous studies using a similar instrument (Philippines: PCL-5 vs. PHQ-9, r = 0.71; [23]; Netherlands: PCL-5 vs. PHQ-9, r = 0.72; [24]). A strong correlation obtained between the PCL-5 and depression using different instruments in different languages including English (PCL-5 vs. CES-D, r = 0.64) [9], French (PCL-5 vs. CES-D, r = 0.62) [9], Turkish (PCL-5 vs. BDI, r = 0.64) [20], Arab/Kurdish (PCL-5 vs. DHSC, r = 0.65) [25], and Swedish (PCL-5 vs. MADRS, r = 0.60) [21], further confirms the robustness of the tool across various translations including Bangla. Moreover, the CR yielded factors ranging (0.93–0.94) for each model, which is well beyond the accepted threshold of 0.60 [58] and supported convergent validity. The AVE obtained ranges of 0.39–0.43 for each model. Of note, and according to Fornell and Larcker, if AVE is less than 0.5, but CR is higher than 0.6, the convergent validity of the construct is still adequate [58].
At last, the utility of PCL-5 in self-report questionnaires that can be administered widely is obviously preferable over other clinical measures such as Clinician-Administered PTSD Scale for DSM-5 (CAPS-5; [80]) that needs to be administered in person and therefore requires different settings and higher resources. CAPS-5, is however, the gold standard for PTSD assessment and is obviously more applicable in clinical studies [80]. Thus, head to head comparisons between PCL-5 and CAPS-5 may be examined in future studies.
Limitations
Although the psychometric properties of the Bangla PCL-5 were overall satisfactory, there are some potential limitations worthy of commentary. First, compared with face-to-face interviews, self-reporting has limitations including potential multiple biases (e.g., memory recall, social desirability biases). Secondly, the study executed a cross-sectional study design. Longitudinal observation is important, particularly given the potential for posttraumatic experiences and temporal evolution characteristics of this process. Thirdly, this was an online-based survey, so this study was not representative, for example, of those who have limited internet access or may be unwilling to respond via this methodology. Randomized prospective studies could provide potential insights into causation, although these may be complicated to conduct during a pandemic such as COVID-19. Moreover, the study investigated somewhat constrained measures, and did not evaluate other aspects of reliability and validity, such as test–retest reliability, convergent validity (using another PTSD instrument), divergent validity and criterion validity, due to the limited number of test scales available. Likewise, the study did not use other scales to measure PTSD and other psychological symptoms in order to determine the PCL-5's divergent validity. Further investigations are warranted with the inclusion of incremental measures along with their application to clinical settings. Moreover, the exposure to and the number of experienced traumatic events have not been assessed. The study didn’t investigate the sensitivity and specificity of the PCL-5. Further studies should be designed focusing on its sensitivity and specificity (e.g., including traumatized PTSD patients, traumatized non-PTSD patients, clinical controls, and healthy controls).
Conclusions
To our knowledge, this is the first translation and validation of the PCL-5 into Bangla. We evaluated the comprehensive psychometric properties of this instrument in a large sample while ascertaining the contextual Bangladeshi cultural background setting. Our findings indicate that the Bangla PCL-5 appears to be a robust instrument to screen for the presence of posttraumatic stress disorders among Bangladeshi individuals. In light of the protracted course of the COVID-19 pandemic and the restrictive measures being implemented as well as the economic devastation imposed by this virus, the Bangla PCL-5 instrument will aid in the assessments of posttraumatic stress disorders in Bangladesh and potentially serve as the primary screening tool for further evaluation and treatment of affected individuals. Moreover, due to the lack of divergent validity measures or evaluations of specificity and sensitivity, this study will contribute to the future research on PTSD in Bangladesh.
Supplementary Information
Acknowledgements
Firstly, the authors would like to express the most profound gratitude to all of the respondents who participated in this study. Secondly, the authors wish to express their sincere appreciation to all the Research Assistants of the Centre for Advanced Research Excellence in Public Health (formerly: Youth Research Association), and Quest Bangladesh Biomedical Research Center, who took part in this research (see responsible individuals: click here - http://tiny.cc/acknowledgements).
Abbreviations
- PCL-5
Posttraumatic Stress Disorder Checklist
- DSM-5
Diagnostic and Statistical Manual of Mental disorders
- PTSD
Posttraumatic stress disorder
- COVID-19
Coronavirus disease-2019
- SARS-CoV-2
Severe acute respiratory syndrome coronavirus 2
- BDT
Bangladeshi Taka
- PHQ-9
Patient Health Questionnaire
- ANOVA
Analysis of variance
- SPSS
Statistical Package for the Social Sciences
- CR
Composite reliability
- CFA
Confirmatory factor analysis
- SEM
Structural equation modeling
- AVE
Average variance extracted
- AIC
Akaike Information Criterion
- BIC
Bayesian Information Criterion
- CAPS-5
Clinician-Administered PTSD Scale for DSM-5
Authors’ contribution
Conceptualization: MSI, MZF, MSHS, RT. Data collection: MSI, MZF, MSHS, RT. Analysis and interpretation of data: MSI. Drafting of the manuscript: MSI, MZF, MSHS, RT. Editing: MZF, JHBM, SK, ASMM, MSKC, IAK, DG. Critical revision of the manuscript: IAK, DG. All authors have read and approved the manuscript.
Funding
The authors did not receive any grants or remunerations from either public or private organizations or other funding agencies.
Availability of data and materials
The datasets/ questionnaire generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study was conducted in accordance with the Institutional Research Ethics guidelines and ethical guidelines involving human participation (i.e., Helsinki Declaration). Formal ethics approval was granted by Ethical Review Committee, Uttara Adhunik Medical College (Ref. No.: UAMC/ERC/ 16/2020). Informed consent was obtained from all participants or, if participants are under 18, from a parent and/or legal guardian.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no potential conflict of interest in the publication of this research output.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Md. Saiful Islam, Email: islam.msaiful@outlook.com.
Most. Zannatul Ferdous, Email: m.zannatul.ferdous@juniv.edu.
Md. Safaet Hossain Sujan, Email: sujanmahmuddphi@gmail.com.
Rafia Tasnim, Email: tasnimrifa97@gmail.com.
Jakir Hossain Bhuiyan Masud, Email: jakirmsd@gmail.com.
Sourav Kundu, Email: sourav@kundu.org.
Abu Syed Md. Mosaddek, Email: drmosaddek1968@gmail.com
M. Shahabuddin K. Choudhuri, Email: mskchoudhuri@juniv.edu
Ibrahim A. Kira, Email: kiraaref@aol.com
David Gozal, Email: gozald@health.missouri.edu.
References
- 1.Dasgupta S, Kamal FA, Khan ZH, Choudhury S, Nishat A. River salinity and climate change: evidence from Coastal Bangladesh. 2014. http://documents1.worldbank.org/curated/en/522091468209055387/pdf/WPS6817.pdf.
- 2.Eckstein D, Hutfils M-L, Winges M. Global Climate Risk Index 2019—who suffers most from extreme weather events? Weather-related loss events in 2017 and 1998 to 2017. https://www.germanwatch.org/sites/germanwatch.org/files/GlobalClimateRiskIndex2019_2.pdf.
- 3.Tasdik Hasan M, Adhikary G, Mahmood S, Papri N, Shihab HM, Kasujja R, et al. Exploring mental health needs and services among affected population in a cyclone affected area in costal Bangladesh: a qualitative case study. Int J Ment Health Syst. 2020;14:12. doi: 10.1186/s13033-020-00351-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kessler RC. Posttraumatic stress disorder: the burden to the individual and to society. J Clin Psychiatry. 2000;61(Suppl 5):4. [PubMed] [Google Scholar]
- 5.Fitch T, Villanueva G, Quadir MM, Sagiraju HKR, Alamgir H. The prevalence and risk factors of post-traumatic stress disorder among workers injured in rana plaza building collapse in Bangladesh. Am J Ind Med. 2015;58:756–763. doi: 10.1002/ajim.22471. [DOI] [PubMed] [Google Scholar]
- 6.Cloitre M, Cohen LR, Edelman RE, Han H. Posttraumatic stress disorder and extent of trauma exposure as correlates of medical problems and perceived health among women with childhood abuse. Women Health. 2001;34:1–17. doi: 10.1300/J013v34n03_01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Deja M, Denke C, Weber-Carstens S, Schröder J, Pille CE, Hokema F, et al. Social support during intensive care unit stay might improve mental impairment and consequently health-related quality of life in survivors of severe acute respiratory distress syndrome. Crit Care. 2006;10:R147. doi: 10.1186/cc5070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weathers F, Litz B, Herman D, Huska JA, Keane T. The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. Paper presented at the Annual Convention of the International Society for Traumatic Stress Studies, San Antonio, TX. 1993.
- 9.Ashbaugh AR, Houle-Johnson S, Herbert C, El-Hage W, Brunet A. Psychometric validation of the english and french versions of the posttraumatic stress disorder checklist for DSM-5 (PCL-5) PLoS One. 2016;11:e0161645. doi: 10.1371/journal.pone.0161645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 5. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 11.American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 12.King DW, Leskin GA, King LA, Weathers FW. Confirmatory factor analysis of the clinician-administered PTSD scale: evidence for the dimensionality of posttraumatic stress disorder. Psychol Assess. 1998;10:90–96. doi: 10.1037/1040-3590.10.2.90. [DOI] [Google Scholar]
- 13.Palmieri PA, Weathers FW, Difede J, King DW. Confirmatory factor analysis of the PTSD Checklist and the Clinician-Administered PTSD Scale in disaster workers exposed to the World Trade Center Ground Zero. J Abnorm Psychol. 2007;116:329–341. doi: 10.1037/0021-843X.116.2.329. [DOI] [PubMed] [Google Scholar]
- 14.Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The ptsd checklist for dsm-5 (PCL-5). Scale available from Natl Cent PTSD www.ptsd.va.gov. 2013;10.
- 15.Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress. 2015;28:489–498. doi: 10.1002/jts.22059. [DOI] [PubMed] [Google Scholar]
- 16.Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behav Res Ther. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- 17.Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, et al. Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (PCL-5) in veterans. Psychol Assess. 2016;28:1379–1391. doi: 10.1037/pas0000254. [DOI] [PubMed] [Google Scholar]
- 18.Ventureyra VAG, Yao S-N, Cottraux J, Note I, De Mey-Guillard C. The validation of the Posttraumatic Stress Disorder Checklist Scale in posttraumatic stress disorder and nonclinical subjects. Psychother Psychosom. 2002;71:47–53. doi: 10.1159/000049343. [DOI] [PubMed] [Google Scholar]
- 19.Cheng P, Xu L-Z, Zheng W-H, Ng RMK, Zhang L, Li L-J, et al. Psychometric property study of the posttraumatic stress disorder checklist for DSM-5 (PCL-5) in Chinese healthcare workers during the outbreak of corona virus disease 2019. J Affect Disord. 2020;277:368–374. doi: 10.1016/j.jad.2020.08.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Boysan M, Guzel Ozdemir P, Ozdemir O, Selvi Y, Yilmaz E, Kaya N. Psychometric properties of the Turkish version of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (PCL-5). Psychiatry Clin Psychopharmacol. 2017;27:300–10. 10.1080/24750573.2017.1342769.
- 21.Sveen J, Bondjers K, Willebrand M. Psychometric properties of the PTSD Checklist for DSM-5: a pilot study. Eur J Psychotraumatol. 2016;7:30165. doi: 10.3402/ejpt.v7.30165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Krüger-Gottschalk A, Knaevelsrud C, Rau H, Dyer A, Schäfer I, Schellong J, et al. The German version of the posttraumatic stress disorder checklist for DSM-5 (PCL-5): psychometric properties and diagnostic utility. BMC Psychiatry. 2017;17:379. doi: 10.1186/s12888-017-1541-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hall BJ, Yip PSY, Garabiles MR, Lao CK, Chan EWW, Marx BP. Psychometric validation of the PTSD Checklist-5 among female Filipino migrant workers. Eur J Psychotraumatol. 2019;10:1571378. doi: 10.1080/20008198.2019.1571378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Van Praag DLG, Fardzadeh HE, Covic A, Maas AIR, von Steinbüchel N. Preliminary validation of the Dutch version of the Posttraumatic stress disorder checklist for DSM-5 (PCL-5) after traumatic brain injury in a civilian population. PLoS ONE. 2020;15:e0231857. doi: 10.1371/journal.pone.0231857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ibrahim H, Ertl V, Catani C, Ismail AA, Neuner F. The validity of Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5) as screening instrument with Kurdish and Arab displaced populations living in the Kurdistan region of Iraq. BMC Psychiatry. 2018;18:259. doi: 10.1186/s12888-018-1839-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liu P, Wang L, Cao C, Wang R, Zhang J, Zhang B, et al. The underlying dimensions of DSM-5 posttraumatic stress disorder symptoms in an epidemiological sample of Chinese earthquake survivors. J Anxiety Disord. 2014;28:345–351. doi: 10.1016/j.janxdis.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 27.Armour C, Tsai J, Durham TA, Charak R, Biehn TL, Elhai JD, et al. Dimensional structure of DSM-5 posttraumatic stress symptoms: Support for a hybrid Anhedonia and Externalizing Behaviors model. J Psychiatr Res. 2015;61:106–113. doi: 10.1016/j.jpsychires.2014.10.012. [DOI] [PubMed] [Google Scholar]
- 28.Ferdous MZ, Islam MS, Sikder MT, Mosaddek ASM, Zegarra-Valdivia JA, Gozal D. Knowledge, attitude, and practice regarding COVID-19 outbreak in Bangladesh: an online-based cross-sectional study. PLoS One. 2020;15:e0239254. doi: 10.1371/journal.pone.0239254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Islam MS, Emran GI, Rahman E, Banik R, Sikder T, Smith L, et al. Knowledge, attitudes and practices associated with the COVID-19 among slum dwellers resided in Dhaka City: a Bangladeshi interview-based survey. J Public Health (Bangkok) 2021;43:13–25. doi: 10.1093/pubmed/fdaa182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Institute of Epidemiology Disease Control and Research. Covid-19 status for Bangladesh. 2020. http://old.iedcr.gov.bd/. Accessed 31 Aug 2020.
- 31.Worldometer. COVID-19 coronavius pandemic. 2020. https://www.worldometers.info/coronavirus/. Accessed 31 Aug 2020.
- 32.Islam MS, Ferdous MZ, Potenza MN. Panic and generalized anxiety during the COVID-19 pandemic among Bangladeshi people: an online pilot survey early in the outbreak. J Affect Disord. 2020;276:30–37. doi: 10.1016/j.jad.2020.06.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rahman ME, Islam MS, Bishwas MS, Moonajilin MS, Gozal D. Physical inactivity and sedentary behaviors in the Bangladeshi population during the COVID-19 pandemic: an online cross-sectional survey. Heliyon. 2020;6:e05392. doi: 10.1016/j.heliyon.2020.e05392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Islam MS, Sujan MSH, Tasnim R, Sikder MT, Potenza MN, van Os J. Psychological responses during the COVID-19 outbreak among university students in Bangladesh. PLoS One. 2020;15:e0245083. doi: 10.1371/journal.pone.0245083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ahorsu DK, Lin C-Y, Imani V, Saffari M, Griffiths MD, Pakpour AH. The Fear of COVID-19 Scale: Development and Initial Validation. Int J Ment Health Addict. 2020;1-9. 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed]
- 36.Islam MS, Potenza MN, Van Os J. Posttraumatic stress disorder during the COVID-19 pandemic: upcoming challenges in Bangladesh and preventive strategies. Int J Soc Psychiatry. 2021;67:205-6. [DOI] [PubMed]
- 37.Tasnim R, Sujan MSH, Islam MS, Ritu AH, Siddique MA Bin, Toma TY, et al. Prevalence and correlates of anxiety and depression in frontline healthcare workers treating people with COVID-19 in Bangladesh. BMC Psychiatry. 2021;21:271. [DOI] [PMC free article] [PubMed]
- 38.Banerjee D. The COVID-19 outbreak: crucial role the psychiatrists can play. Asian J Psychiatr. 2020;50:102014. doi: 10.1016/j.ajp.2020.102014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Xiao S, Luo D, Xiao Y. Survivors of COVID-19 are at high risk of posttraumatic stress disorder. Glob Heal Res Policy. 2020;5:29. doi: 10.1186/s41256-020-00155-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shultz JM, Baingana F, Neria Y. The 2014 Ebola outbreak and mental health: current status and recommended response. JAMA. 2015;313:567–568. doi: 10.1001/jama.2014.17934. [DOI] [PubMed] [Google Scholar]
- 41.Peng EY-C, Lee M-B, Tsai S-T, Yang C-C, Morisky DE, Tsai L-T, et al. Population-based post-crisis psychological distress: an example from the SARS outbreak in Taiwan. J Formos Med Assoc. 2010;109:524–32. 10.1016/S0929-6646(10)60087-3. [DOI] [PMC free article] [PubMed]
- 42.Yeung NCY, Lau JTF, Choi KC, Griffiths S. Population Responses during the Pandemic Phase of the Influenza A(H1N1)pdm09 Epidemic, Hong Kong. China Emerg Infect Dis. 2017;23:813–815. doi: 10.3201/eid2305.160768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Beaton DE, Bombardier C, Guillemin F, Ferraz MB. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine (Phila Pa 1976) 2000;25:3186–91. doi: 10.1097/00007632-200012150-00014. [DOI] [PubMed] [Google Scholar]
- 44.Rahman ME, Islam MS, Mamun MA, Moonajilin MS, Yi S. Prevalence and factors associated with suicidal ideation among university students in Bangladesh. Arch Suicide Res. 2020;1-10. 10.1080/13811118.2020.1833800. [DOI] [PubMed]
- 45.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. primary care evaluation of mental disorders patient. health questionnaire. JAMA. 1999;282:1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 46.Chowdhury A, Ghosh S, Sanyal D. Bengali adaptation of brief patient health questionnaire for screening depression at primary care. J Indian Med Assoc. 2004;102:544–547. [PubMed] [Google Scholar]
- 47.Islam MS, Rahman ME, Moonajilin MS, van Os J. Prevalence of depression, anxiety and associated factors among school going adolescents in Bangladesh: findings from a cross-sectional study. PLoS One. 2021;16:e0247898. doi: 10.1371/journal.pone.0247898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Moonajilin MS, Rahman ME, Islam MS. Relationship between overweight/obesity and mental health disorders among Bangladeshi adolescents: a cross-sectional survey. Obes Med. 2020;18:100216. doi: 10.1016/j.obmed.2020.100216. [DOI] [Google Scholar]
- 49.Islam MS, Akter R, Sikder T, Griffiths MD. Prevalence and factors associated with depression and anxiety among first-year university students in Bangladesh: a cross-sectional study. Int J Ment Health Addict. 2020. 10.1007/s11469-020-00242-y.
- 50.Islam MS, Rahman ME, Moonajilin MS, Griffiths MD. Validation and evaluation of the psychometric properties of bangla nine-item internet disorder scale-short form. J Addict Dis. 2020;38:540–549. doi: 10.1080/10550887.2020.1799134. [DOI] [PubMed] [Google Scholar]
- 51.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model a Multidiscip J. 1999;6:1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- 52.Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychol Bull. 1980;88:588. doi: 10.1037/0033-2909.88.3.588. [DOI] [Google Scholar]
- 53.Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;107:238. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- 54.Hooper D, Coughlan J, Mullen MR. Structural equation modelling: Guidelines for determining model fit. Electron J Bus Res methods. 2008;6:53–60. [Google Scholar]
- 55.Schwarz G. Estimating the Dimension of a Model. Ann Stat. 1978;6:461–464. doi: 10.1214/aos/1176344136. [DOI] [Google Scholar]
- 56.Akaike H. Factor analysis and AIC. Psychometrika. 1987;52:317–332. doi: 10.1007/BF02294359. [DOI] [Google Scholar]
- 57.Raftery AE. Bayesian Model Selection in Social Research. Sociol Methodol. 1995;25:111–163. doi: 10.2307/271063. [DOI] [Google Scholar]
- 58.Fornell C, Larcker DF. Evaluating structural equation models with unobservable variables and measurement error. J Mark Res. 1981;18:39–50. doi: 10.1177/002224378101800104. [DOI] [Google Scholar]
- 59.George D. SPSS for windows step by step: A simple study guide and reference, 17.0 update, 10/e. Pearson Education India; 2011.
- 60.Hair JF, Black WC, Babin BJ, Anderson RE, Tatham RL. Multivariate data analysis. Prentice hall Upper Saddle River, NJ; 1998.
- 61.Tabachnick BG, Fidell LS. Using multivariate statistics. Boston: Allyn & Bacon/Pearson Education; 2001. [Google Scholar]
- 62.Banna MH Al, Sayeed A, Kundu S, Christopher E, Hasan MT, Begum MR, et al. The impact of the COVID-19 pandemic on the mental health of the adult population in Bangladesh: a nationwide cross-sectional study. Int J Environ Health Res. 2020;:1–12. 10.1080/09603123.2020.1802409. [DOI] [PubMed]
- 63.Islam MS, Sujan MSH, Tasnim R, Mohona RA, Ferdous MZ, Kamruzzaman S, et al. Problematic smartphone and social media use among Bangladeshi college and university students amid COVID-19: The role of psychological wellbeing and pandemic related factors. Front psychiatry. 2021;12:647386. doi: 10.3389/fpsyt.2021.647386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tasnim R, Islam MS, Sujan MSH, Sikder MT, Potenza MN. Suicidal ideation among Bangladeshi university students early during the COVID-19 pandemic: prevalence estimates and correlates. Child Youth Serv Rev. 2020;119:105703. doi: 10.1016/j.childyouth.2020.105703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Islam MS, Ferdous MZ, Islam US, Mosaddek ASM, Potenza MN, Pardhan S. Treatment, persistent symptoms, and depression in people infected with COVID-19 in Bangladesh. Int J Environ Res Public Health. 2021;18:1453. doi: 10.3390/ijerph18041453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Islam MS, Sujan MSH, Tasnim R, Ferdous MZ, Masud JHB, Kundu S, et al. Problematic internet use among young and adult population in Bangladesh: Correlates with lifestyle and online activities during the COVID-19 pandemic. Addict Behav Reports. 2020;12:100311. [DOI] [PMC free article] [PubMed]
- 67.Islam MS, Rahman ME, Banik R, Emran MGI, Noshin S, Hossain S, et al. Financial and Mental Health Concerns of Impoverished Urban-Dwelling Bangladeshi People During COVID-19. Front Psychol. 2021;12:663687. [DOI] [PMC free article] [PubMed]
- 68.Safa F, Anjum A, Hossain S, Trisa TI, Alam SF, Abdur Rafi M, et al. Immediate psychological responses during the initial period of the COVID-19 pandemic among Bangladeshi medical students. Child Youth Serv Rev. 2021;122:105912. doi: 10.1016/j.childyouth.2020.105912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Alshehri FS, Alatawi Y, Alghamdi BS, Alhifany AA, Alharbi A. Prevalence of post-traumatic stress disorder during the COVID-19 pandemic in Saudi Arabia. Saudi Pharm J. 2020;28:1666–1673. doi: 10.1016/j.jsps.2020.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Liang L, Gao T, Ren H, Cao R, Qin Z, Hu Y, et al. Post-traumatic stress disorder and psychological distress in Chinese youths following the COVID-19 emergency. J Health Psychol. 2020;25:1164–1175. doi: 10.1177/1359105320937057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Liu N, Zhang F, Wei C, Jia Y, Shang Z, Sun L, et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatry Res. 2020;287:112921. doi: 10.1016/j.psychres.2020.112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Tang W, Hu T, Hu B, Jin C, Wang G, Xie C, et al. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J Affect Disord. 2020;274:1–7. doi: 10.1016/j.jad.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Forte G, Favieri F, Tambelli R, Casagrande M. COVID-19 pandemic in the Italian population: Validation of a post-traumatic stress disorder questionnaire and prevalence of PTSD symptomatology. Int J Environ Res Public Health. 2020;17:4151. [DOI] [PMC free article] [PubMed]
- 74.González-Sanguino C, Ausín B, Castellanos MÁ, Saiz J, López-Gómez A, Ugidos C, et al. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun. 2020. 10.1016/j.bbi.2020.05.040. [DOI] [PMC free article] [PubMed]
- 75.Liu CH, Zhang E, Wong GTF, Hyun S, Hahm HC. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Res. 2020;290:113172. doi: 10.1016/j.psychres.2020.113172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Seligowski AV, Orcutt HK. Support for the 7-factor hybrid model of PTSD in a community sample. Psychol Trauma. 2016;8:218–221. doi: 10.1037/tra0000104. [DOI] [PubMed] [Google Scholar]
- 77.Ito M, Takebayashi Y, Suzuki Y, Horikoshi M. Posttraumatic stress disorder checklist for DSM-5: Psychometric properties in a Japanese population. J Affect Disord. 2019;247:11–19. doi: 10.1016/j.jad.2018.12.086. [DOI] [PubMed] [Google Scholar]
- 78.Zelazny K, Simms LJ. Confirmatory factor analyses of DSM-5 posttraumatic stress disorder symptoms in psychiatric samples differing in Criterion A status. J Anxiety Disord. 2015;34:15–23. doi: 10.1016/j.janxdis.2015.05.009. [DOI] [PubMed] [Google Scholar]
- 79.Wortmann JH, Jordan AH, Weathers FW, Resick PA, Dondanville KA, Hall-Clark B, et al. Psychometric analysis of the PTSD Checklist-5 (PCL-5) among treatment-seeking military service members. Psychol Assess. 2016;28:1392–1403. doi: 10.1037/pas0000260. [DOI] [PubMed] [Google Scholar]
- 80.Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, Keane TM. The clinician-administered PTSD scale for DSM-5 (CAPS-5). Interview available from Natl Cent PTSD www.ptsd.va.gov. 2013;6.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets/ questionnaire generated and/or analyzed during the current study are available from the corresponding author on reasonable request.