Abstract
We report a case of primary malignant melanoma of the esophagus.
Keywords: esophagus, melanoma
Primary malignant melanoma of the esophagus (PMME) is a rare primary neoplasm of the esophagus. Although it is rare, it must be borne in mind, as early and correct diagnosis could offer the patient a better prognosis.

Α 70‐year‐old female patient was admitted to our hospital with a history of dysphagia for solids and weight loss. An endoscopy was performed and revealed an ulcerated mass involving the lower third of esophagus (Figure 1). Histology revealed a diffuse proliferation of atypical epithelioid amelanotic cells with irregular nuclear borders and sometimes prominent nucleoli associated with tumor necrosis. Immunohistochemical findings included positive Melan‐A, SOX‐10, HMB‐45, focally positive S‐100 and negative CK20, CK7, Synaptophysin, TTF‐1, LCA, and CD‐117 (Figure 2). Positron emission tomography‐CT (PET‐CT) showed an increased uptake of fluorodeoxy‐glucose in the lower part of esophagus (Figure 3). After a thorough search for a primary tumor from skin, ocular and mucosal sites a diagnosis of primary malignant melanoma of esophagus (PMME) was made. A subtotal esophagectomy was done, the patient had a good clinical outcome and was discharged 10 days after surgery.
FIGURE 1.
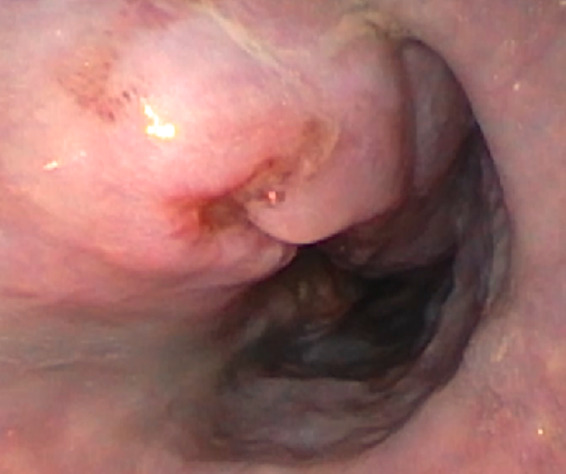
Ulcerated mass involving the lower third of esophagus
FIGURE 2.
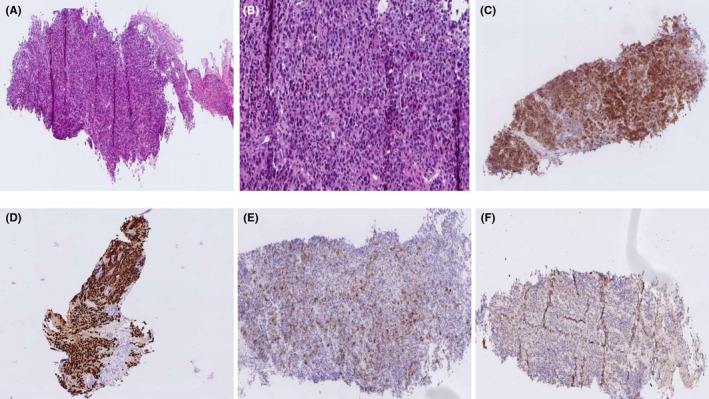
Histology examination (H&E) high‐power magnified image ×20 (A) and ×40 (B) of the tumor. Immunohistochemical findings include positive Melan‐A (C), SOX‐10 (D), HMB‐45 (E) and focally positive S‐ 100 (F)
FIGURE 3.
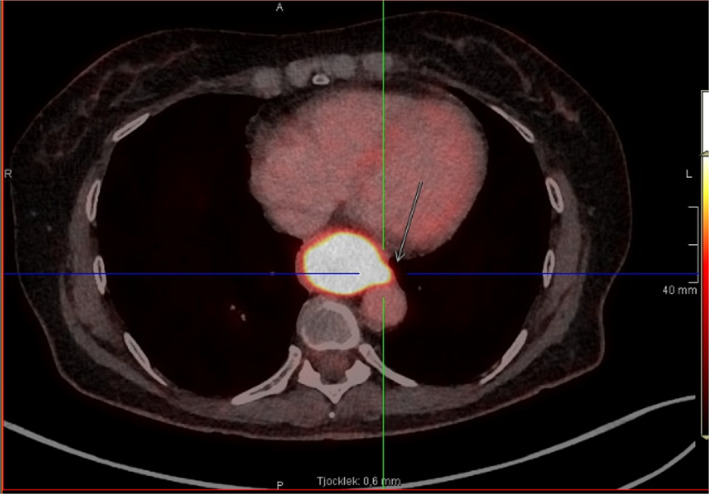
PET‐CT with an increased uptake of fluorodeoxy‐glucose in the lower part of esophagus
Primary melanoma of the gastrointestinal tract is exceedingly rare; Primary malignant melanoma of the esophagus (PMME) accounts for 0.1%–0.2% of all primary neoplasms of the esophagus. 1 Most commonly, it affects patients between the sixth and seventh decade of life, and there is a male predominance. 2 The most common symptoms are dysphagia, chest pain, and weight loss. On endoscopy, these tumors usually appear as lobulated and darkly colored masses with intact mucosa or occasional ulceration. They are occasionally misdiagnosed as poorly differentiated carcinoma. The radiological differential diagnosis of primary esophageal melanoma includes spindle cell carcinoma, leiomyosarcoma, esophageal lymphoma, and Kaposi's sarcoma. 3 PMME is usually fatal with a mean survival time of 13.4 months. 4
CONFLICT OF INTEREST
None declared.
AUTHOR CONTRIBUTIONS
DK, SV, SI, GT, and TF contributed to the writing and approval of the final manuscript.
ETHICAL APPROVAL
Written informed consent was obtained from the patient. This case report did not receive any funding. The authors have access to all source data for this case report.
CONSENT
Informed consent has been obtained from the patient for the publication of this clinical image.
ACKNOWLEDGEMENT
None.
Karapiperis D, Vrakas S, Ignatova S, Tribonias G, Franzen T. Primary malignant melanoma of the esophagus. Clin Case Rep. 2022;10:e05660. doi: 10.1002/ccr3.5660
DATA AVAILABILITY STATEMENT
Data supporting the findings of this study are available from the corresponding author on request.
REFERENCES
- 1. Cheung MC, Perez EA, Molina MA, et al. Defining the role of surgery for primary gastrointestinal tract melanoma. J Gastrointest Surg. 2008;12(4):731‐738. [DOI] [PubMed] [Google Scholar]
- 2. Fukuda S, Ito H, Ohba R, et al. A retrospective study, an initial lesion of primary malignant melanoma of the esophagus revealed by endoscopy. Intern Med. 2017;56(16):2133‐2137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Charu J, Promila J, Ritu V. Primary malignant melanoma of the esophagus. Indian J Nucl Med. 2015;30(2):162‐164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sabanathan S, Eng J, Pradhan GN. Primary malignant melanoma of the esophagus. Am J Gastroenterol. 1989;84:1475‐1481. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data supporting the findings of this study are available from the corresponding author on request.


