Abstract
Objectives
To evaluate the frequency of abnormal progression that could ultimately affect the reliability of the skeletal maturity index (SMI) and the cervical vertebral maturation (CVM) method that are most commonly used analyses for skeletal age assessment.
Materials and Methods
A retrospective design was used to compare 299 hand-wrist radiographs with 299 lateral skull radiographs regarding the number of abnormalities in the proposed sequence of maturation in the SMI and CVM methods.
Results
A significantly greater number of abnormalities occurred in the sequence of CVM progression compared with SMI (P < .001). Sex and age did not have an effect.
Conclusions
Skeletal age assessment based on SMI is more accurate than CVM regarding the progressive sequence of stages.
Keywords: SMI, CVM
INTRODUCTION
It is important to assess skeletal age of patients accurately during dentofacial orthopedic treatment. The skeletal maturity index (SMI) and the cervical vertebral maturation (CVM) methods are the two most commonly used analyses for skeletal age assessment and growth prediction in orthodontics. In recent years, some orthodontists have favored CVM over SMI to reduce radiation to patients. The use of CVM has been supported by some investigators to be as accurate as SMI.1,2 However, Gabriel et al. found poor reproducibility of the CVM index.3 Those results were confirmed by a later study that found a low intra-assessor repeatability of 54% and an even lower inter-assessor reproducibility of 42%.4 In addition to low reproducibility, CVM has been recently criticized for not correlating with the mandibular growth spurt.5 This is in contrast to SMI, which has been shown to have a high correlation with mandibular peak growth.6 Baccetti et al. showed the CVM method to be accurate.7 However, in that study, a large number of subjects (i.e., 676) were excluded from the original sample size of 706 due to the exclusion criteria. It is conceivable that the small sample size of that study may not have been fully representative of the larger population to which CVM was subsequently applied.
In the CVM and SMI methods, the last stage attained is used to determine the growth stage. This means that the assignment of a growth stage assumes a perfect progression through the stages without any deviation from the proposed sequence of the stages. The CVM or SMI stage cannot be assigned if it is deviated from the proposed sequence. For example, when assessing a patient's SMI, capping of the third finger middle phalanx (SMI 6) may be observed before that of the distal phalanx (SMI 5): This is abnormal because SMI 6 cannot be reached before SMI 5 in the normal progression of SMI. Likewise, in the CVM method, one can encounter the formation of inferior border concavity in C4 (CVM III) while the shape of C3 is still trapezoidal (CVM I or CVM II). Such abnormalities would make the identification of skeletal age very difficult. The aim of the current study was to evaluate the frequency of abnormal progression that could ultimately affect the reliability of either method.
In the current study, it was regarded as “normal” whenever a growth stage of CVM and SMI could be assigned properly as proposed by Baccetti et al. and Fishman, respectively.6,7 However, the term “exception” or “abnormal” was defined in this study to describe the maturation sequence when deviated from the proposed CVM and SMI sequence. The term had no association with pathological bone development; it was used only in connection to the proposed sequence of bone maturation.
MATERIALS AND METHODS
This was a retrospective study using the patient data bank of Maimonides Medical Center (MMC). The current study was approved as exempt, as it was deemed to have satisfied the criteria for exempt review set forth in federal regulations by the Institutional Review Board/research chair of MMC. After preliminary statistical analysis, to achieve a minimum 85% power with alpha = 0.05, a sample size of about 300 was recommended. Radiographs of 315 patients were collected randomly from the MMC data bank. For each patient, a hand-wrist radiograph and a lateral cephalometric radiograph were collected.
Exclusion criteria were as follows: poor quality radiographs, hand-wrist radiographs that did not include key diagnostic components (such as the radial epiphysis), cervical radiographs that did not include key diagnostic components (such as C4), and patients with growth pathology that could potentially interfere with skeletal age assessment. Based on the exclusion criteria, 16 sets of radiographs were eliminated, leaving a sample size of 299 sets of radiographs, including 151 females and 148 males. The average ages of the subjects at the times of radiographic examination were 13 years and 2.4 months for the lateral cephalometric, and 13 years and 3.4 months for the hand-wrist, radiographs. All of the radiographs were taken with the Sirona Orthophos XG5 imaging system (Charlotte, NC, USA). The exposure setting was fixed at the manufacturer's recommendation of 9.1 s/64 kV/16 mA for hand-wrist and 14.9 s/73 kV/15 mA for lateral cephalometric radiographs.
Each radiograph received a subject number rather than being labeled with patient names. Also, all age information and dates of radiographs were not included until after the assessment was finished. One author assessed all radiographs and abnormalities were verified and confirmed by a second author. Lateral cephalometric radiographs were cropped to show only the cervical vertebrae for assessment; the removal of all other areas, including the dentition, reduced identification bias. For assessment of hand-wrist radiographs, the current study used Fishman's SMI (Figure 1). For assessment of the lateral cephalometric radiographs, the Baccetti et al. improved method of CVM was used. Baccetti et al. described their new method by using two sets of morphological variables of the cervical vertebrae 2, 3, and 4.7 The first variable was the shape of the vertebrae: trapezoidal, rectangular horizontal, square, or rectangular vertical. The second variable was the presence or absence of an inferior border concavity (Table 1).
Figure 1.
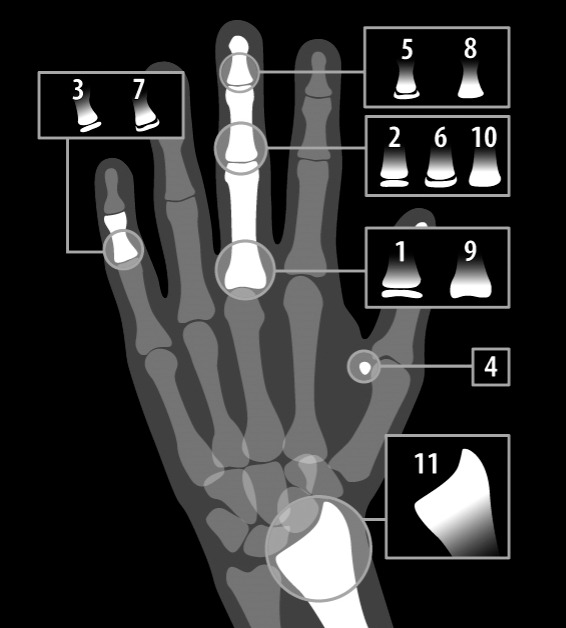
Dr. Fishman's skeletal maturity index (SMI).
Table 1.
CVM Sequence of Stages Based on Both Variablesa
| CVM Stage |
CVM 1 |
CVM2 |
CVM3 |
CVM4 |
CVM5 |
| Presence of Concavity | Odontoid can be: flat or concave | Odontoid concave | Odontoid concave | Odontoid concave | Odontoid concave |
| C3 flat | C3 concave | C3 concave | C3 concave | C3 concave | |
| C4 flat | C4 flat | C4 concave | C4 concave | C4 concave | |
| Geometric Shape | C3 trapezoidal | C3 trapezoidal or horizontal rectangle | C3 horizontal rectangle | C3 square | C3 vertical rectangle |
| C4 trapezoidal | C4 trapezoidal | C4 horizontal rectangle | C4 square or horizontal rectangle | C4 vertical rectangle or square |
CVM indicates cervical vertebral maturation.
Data were analyzed first to show overall agreement between SMI and CVM using the Cohen's Kappa statistic; this agreement analysis showed whether there was either association or lack of association between CVM and SMI regarding the exceptions of normal progression of skeletal stages. The agreement analysis was then stratified by gender to determine whether gender played a role since some previous studies indicated sexual dimorphism existed in skeletal maturation.8 Because it appeared that CVM had a higher rate of exceptions detected, the McNemar's test was used to compare the proportions of abnormalities between the groups SMI and CVM.9 Chi-square analysis was also used to determine whether the rate of exceptions detected by either SMI or CVM was different for males and females. Finally, logistic regression was used to detect whether age and the stage of skeletal maturation had any correlation with the lack of association between CVM and SMI. Logistic regression analysis was used to control the effect of age difference between SMI and CVM groups, using age as a covariate. All analyses were performed using SAS Version 9.4 (SAS Institute Inc., Cary, NC, USA) and SPSS version 23 (IBM Corporation, Armonk, NY, USA).
RESULTS
Out of the 299 individuals, 15 exhibited abnormalities in their SMI assessments while 56 individuals showed abnormalities in their CVM (Table 2). Regarding agreement between CVM and SMI on the abnormal progression, Cohen's Kappa statistic was 0.036 (P = .419). This measure indicated very poor agreement between the CVM and SMI; the abnormal CVM progression of an individual was not necessarily followed by that of SMI. When the agreement analysis was stratified by gender, the Kappa for male was 0.031 (P = .660) and for female was 0.044 (P = .428). Gender showed no significant correlation between CVM and SMI on the abnormal progression. The McNemar paired analysis showed that the rate of such abnormalities was significantly higher for the CVM group than the SMI group (P = .001). Chi-square analysis did not show any statistically significant difference between the sexes on the abnormal progression for either SMI (P = .404) or CVM (P = .420), as seen in Table 3. Also, age (P = .626) and the stage of SMI (P = .422) were determined by logistic regression analysis to not be significant factors in the lack of association between CVM and SMI.
Table 2.
Normal vs. Abnormal Progression of SMI and CVM for the Total Samplea
|
|
Normal CVM Progression |
Abnormal CVM Progression |
Total |
| Normal SMI progression | |||
| Count | 232 | 52 | 284 |
| % | 77.6% | 17.4% | 95.0% |
| Abnormal SMI progression | |||
| Count | 11 | 4 | 15 |
| % | 3.7% | 1.3% | 5.0% |
| Total | |||
| Count | 243 | 56 | 299 |
| % | 81.3% | 18.7% | 100% |
CVM indicates cervical vertebral maturation; SMI, skeletal maturity index.
Table 3.
Normal vs Abnormal Progression of SMI and CVM in Females and Malesa
|
|
SMI |
CVM |
Total |
||
| Normal |
Abnormal |
Normal |
Abnormal |
||
| Female | |||||
| Count | 145 | 6 | 120 | 31 | 151 |
| % | 96.0% | 4.0% | 79.5% | 20.5% | (100.0%) |
| Male | |||||
| Count | 139 | 9 | 123 | 25 | 148 |
| % | 93.9% | 6.1% | 83.1% | 16.9% | (100.0%) |
| Total | |||||
| Count | 284 | 15 | 243 | 56 | 299 |
| % | 95.0% | 5.0% | 81.3% | 18.7% | (100.0%) |
CVM indicates cervical vertebral maturation; SMI, skeletal maturity index.
DISCUSSION
The results of the current study showed a significantly higher rate of exceptions in the proposed sequence of CVM by almost four times. Given the findings of previous studies showing low reproducibility of CVM, the current findings may explain why CVM assessment did not have a high inter-observer agreement. Since CVM stages do not always follow the proposed sequence as Lamparski or Baccetti et al. suggested,7,10 clinicians would have difficulty assessing the stages when they encountered an abnormality. For instance, in the example shown in Figure 2, though the C4 vertebra has progressed into either a horizontal rectangle or a square, C2 to C4 vertebrae do not yet possess inferior border concavity. This example, being an exception in the normal progression of CVM, can be interpreted as either CVM 1 or CVM 4, depending on which set of variables (ie, inferior border concavity or geometric shape) the clinician used on which to base their assessment. Another aspect in assessing CVM is the subjectivity in determining the stages. It was mentioned in a study by Zhao et al.11 that “the transition in the shape of cervical vertebral bodies is a consecutive and gradual process” and this may blur the judgment of what constitutes a flat or concave inferior border. Additionally, even the size and geometric shape is also a matter of the “researcher's arbitrary decision.” Consequently, the study found a wide range of intra-assessor agreement, leading the authors to suggest that CVM alone should not be used to assess skeletal age.
Figure 2.

CVM exception: C4 appears as either horizontal rectangle or a square but no inferior concavity is noted at C2–C4.
The current study found that a significant number of CVM abnormalities occurred during CVM III (49 individuals). This was mainly due to the presence of an inferior border concavity in C3 and C4, despite C3 still being trapezoidal in shape. This common occurrence in CVM obscures the reading of CVM at stage III, which is problematic because CVM III is a critical stage for growth assessment and orthopedic intervention. Zhao et al. had similar findings regarding CVM III.11 Interestingly, most of the abnormalities in SMI (13 individuals) also occurred during stages that were critical for growth modification (ie, SMI 4–6). The apparently high frequency of abnormalities in SMI during this period may have been due to the difficulty in identifying the exact time capping first appeared on the hand wrist x-ray. Fishman described capping as “the stage in which the rounded lateral margins of the epiphysis begin to flatten and point toward the diaphysis with an acute angle on the side facing the diaphysis. The time of first appearance of this capping is applicable as an SMI.”6 The morphological change of the epiphysis is also a gradual process and the transition point is subject to identification bias, though to a much lesser extent than in the CVM method. It seems, in the CVM and SMI methods, the attempt to separate growth stages during a continuous change of morphology makes the assignment of a growth stage difficult. However, SMI exhibited only 15 abnormalities and that was significantly lower than those of CVM. The reasons for high prevalence of exception in the proposed sequence during accelerated growth need to be investigated further in the future study.
Although the CVM and SMI methods are influenced by the subjective bias of an assessor, another possible explanation for the higher number of observed abnormalities in CVM may be because CVM is based on two sets of variables (ie, body shapes and inferior border concavity). Since any single CVM stage is based on the presence of both variables, it is feasible that the error of staging may increase because a clinician must consider both of them for staging. This is in contrast to SMI where each stage has only one criterion to fulfill. In other words, each SMI stage is an all-or-nothing decision for assessment.
The current study showed that the existence of supporting evidence for CVM requires further validation. A systematic review published in the year 2012 provides insight into this concern.12 In that review, Santiago et al. found that all studies in support of CVM had inherent biases. For example, some studies assessed the CVM stages after the vertebrae were traced, thereby influencing the decision of the assessor which should have been arrived at independently. The authors stated that most of the supporting CVM studies suffered from “serious methodological failures.”
CONCLUSIONS
A higher rate of abnormalities was found in the progression of stages in the CVM method than that of SMI.
This may be explanatory of the low rate of reproducibility of CVM, which has already been investigated in previous studies.
Based on these findings, clinicians should be more cautious in using CVM and use alternative methods when they encounter stages that are more difficult to determine.
ACKNOWLEDGMENT
We thank James Bloom for the art work of Figure 1. We also thank the late Peter Homel with his statistical analysis.
REFERENCES
- 1.Soegiharto BM, Moles DR, Cunningham SJ. Discriminatory ability of the skeletal maturation index and the cervical vertebrae maturation index in detecting peak pubertal growth in Indonesian and white subjects with receiver operating characteristics analysis. Am J Orthod Dentofacial Orthop . 2008;134(2):227–237. doi: 10.1016/j.ajodo.2006.09.062. [DOI] [PubMed] [Google Scholar]
- 2.Cericato GO, Bittencourt MA, Paranhos LR. Validity of the assessment method of skeletal maturation by cervical vertebrae: a systematic review and meta-analysis. Dentomaxillofac Radiol . 2015;44(4):20140270. doi: 10.1259/dmfr.20140270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gabriel DB, Southard KA, Qian F, Marshall SD, Franciscus RG, Southard TE. Cervical vertebrae maturation method: poor reproducibility. Am J Orthod Dentofacial Orthop . 2009;136(4):478.e1–7. doi: 10.1016/j.ajodo.2007.08.028. discussion 478–480. [DOI] [PubMed] [Google Scholar]
- 4.Predko-Engel A, Kaminek M, Langova K, Kowalski P, Fudalej PS. Reliability of the cervical vertebrae maturation (CVM) method. Bratisl Lek Listy . 2015;116(4):222–226. doi: 10.4149/bll_2015_043. [DOI] [PubMed] [Google Scholar]
- 5.Gray S, Bennani H, Kieser JA, Farella M. Morphometric analysis of cervical vertebrae in relation to mandibular growth. Am J Orthod Dentofacial Orthop . 2016;149(1):92–98. doi: 10.1016/j.ajodo.2015.06.028. [DOI] [PubMed] [Google Scholar]
- 6.Fishman LS. Radiographic evaluation of skeletal maturation: a clinically oriented method based on hand-wrist films. Angle Orthod . 1982;52:88–112. doi: 10.1043/0003-3219(1982)052<0088:REOSM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Baccetti T, Franchi L, McNamara JA., Jr An improved version of the cervical vertebral maturation (CVM) method for the assessment of mandibular growth. Angle Orthod . 2002;72(4):316–323. doi: 10.1043/0003-3219(2002)072<0316:AIVOTC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 8.Smith RJ. Misuse of hand-wrist radiographs. Am J Ortho . 1980;77:75–78. doi: 10.1016/0002-9416(80)90225-0. [DOI] [PubMed] [Google Scholar]
- 9.Despina K, Nikolasos P. Matched analysis for paired binary data (McNemar test) Am J Orthod Dentofacial Orthop . 2017;151:222–223. doi: 10.1016/j.ajodo.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 10.Lamparski DG. Skeletal Age Assessment Utilizing Cervical Vertebrae [master's thesis] Pittsburgh, PA: Department of Orthodontics, The University of Pittsburgh; 1972. [Google Scholar]
- 11.Zhao XG, Lin J, Jiang JH, Wang Q, Ng SH. Validity and reliability of a method for assessment of cervical vertebral maturation. Angle Orthod . 2012;82:229–234. doi: 10.2319/051511-333.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Santiago RC, de Miranda Costa LF, Vitral RW, Fraga MR, Bolognese AM, Maia LC. Cervical vertebral maturation as a biologic indicator of skeletal maturity. Angle Orthod . 2012;82(6):1123–1131. doi: 10.2319/103111-673.1. [DOI] [PMC free article] [PubMed] [Google Scholar]


