Abstract
The Infectious Diseases Data Observatory (IDDO, https://www.iddo.org) has launched a clinical data platform for the collation, curation, standardisation and reuse of individual participant data (IPD) on treatments for two of the most globally important neglected tropical diseases (NTDs), schistosomiasis (SCH) and soil-transmitted helminthiases (STHs). This initiative aims to harness the power of data-sharing by facilitating collaborative joint analyses of pooled datasets to generate robust evidence on the efficacy and safety of anthelminthic treatment regimens. A crucial component of this endeavour has been the development of a Research Agenda to promote engagement with the SCH and STH research and disease control communities by highlighting key questions that could be tackled using data shared through the IDDO platform. Here, we give a contextual overview of the priority research themes articulated in the Research Agenda—a ‘living’ document hosted on the IDDO website—and describe the three-stage consultation process behind its development. We also discuss the sustainability and future directions of the platform, emphasising throughout the power and promise of ethical and equitable sharing and reuse of clinical data to support the elimination of NTDs.
Keywords: schistosomiasis, soil-transmitted helminthiasis, data sharing, data reuse, treatment, anthelmintic, neglected tropical diseases
Disclaimer
The views expressed in this article are those of the authors. Publication in Wellcome Open Research does not imply endorsement by Wellcome.
Introduction
At least one billion of the world’s poorest people suffer from neglected tropical diseases (NTDs). Two of the most common NTDs are schistosomiasis (SCH) and soil-transmitted helminthiases (STHs), caused by parasitic worms (helminths, trematodes and nematodes, respectively) that are endemic throughout the tropical and sub-tropical regions and intimately associated with poverty 1– 3 . The World Health Organization (WHO), supported by global health partners, has spearheaded efforts to eliminate these diseases as a public health problem by 2030 4 , predominantly using a strategy of preventive chemotherapy (PC). This entails the distribution of anthelmintic drugs (anthelmintics) to at-risk populations on an annual or semi-annual basis, by mass drug administration (MDA), upon pre-determined infection prevalence thresholds.
The scale up of these PC programs over the past decade is unprecedented and they are among the first public health interventions to resume after recent disruptions caused by the coronavirus disease 2019 (COVID-19) pandemic. Every year, since 2017, more than a billion people have been treated for NTDs 5, 6 , including in 2019, 105 million people were given praziquantel for SCH and 613 million people were given benzimidazoles for STHs 7 . Despite this, there remain questions on the factors that shape individual responses to treatment; responses to treatment in understudied groups; anthelmintic safety and tolerability profiles, and methodological questions on how and when responses should be measured and how future studies, including clinical trials, should be best designed to address these questions. Moreover, although the spectre of emerging anthelmintic resistance is ever-present—having already arisen to all major classes of anthelmintics in the veterinary field 8– 11 —there remains little systematic monitoring of anthelmintic efficacy in human populations.
The Infectious Diseases Data Observatory (IDDO) is working with the SCH and STH research and disease control communities to develop a clinical data platform for the collation, curation, standardisation and reuse of individual participant data (IPD) on treatment responses to anthelmintics. It is becoming increasingly well-recognised that data sharing and curation to a standardised format maximises the utility of data by enabling joint analysis of pooled datasets to increase the power of analysis, uncover new information and generate new evidence 12– 14 . The goal of the IDDO initiative is to facilitate collaborative research to improve the efficacy and sustainability of treatments for SCH and STHs through ethical and equitable sharing and reuse of data for scientific outputs that produce better evidence 13, 15, 16 .
As part of the platform development phase, we have developed a Research Agenda highlighting research questions that could be tackled using data shared through the IDDO platform. This is intended to spur the SCH and STHs research communities to engage with the platform which will ultimately enhance research aimed at improving treatments for these diseases. Here, we first describe the consultative process used to develop the Research Agenda, an approach shared across the IDDO portfolio of infectious diseases. We then provide a contextual overview of the priority research areas identified by this process, highlighting areas where sufficient data exist and could be tackled within the short- to mid-term (2–3 years) as well as questions for which there are currently insufficient data, or which are out of the current scope of the platform, but which may in the long-term be important or trigger new research.
Developing the Research Agenda
By taking an inclusive, consultative approach to developing the Research Agenda we have promoted engagement with the SCH and STHs research and disease control communities and developed a document to spur new research. In Box 1, we describe briefly how the Research Agenda developed for visceral leishmaniasis (VL)—another NTD in the IDDO portfolio—has successfully galvanised the VL research community.
Box 1. Development of a Research Agenda for visceral leishmaniasis.
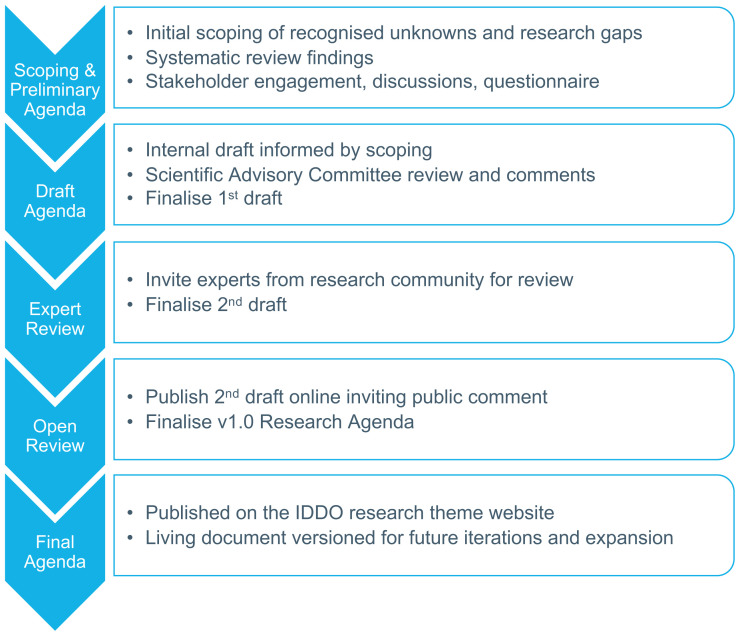
The Research Agenda for visceral leishmaniasis (VL) was completed in 2019 following the same consultative development process as used for the schistosomiasis and soil-transmitted helminthiases Research Agenda as outlined in Figure 1. The VL Research Agenda provided a clear indication of which knowledge gaps could be addressed by the research community if the individual participant data (IPD) were made available. This inspired research proposals for two collaborative Study Groups which were drafted with the VL Scientific Advisory Committee, as representatives of the global VL research community, and key partners, including non-governmental organisations, regional health agencies and funders dedicated to serving VL patients. These proposals were in turn shared with relevant investigators identified from the scoping review inviting them to contribute data and participate in the analysis for each Study Group. By presenting clear research proposals to investigators outlining the outcomes to be achieved through their data contribution, these Study Groups—which were originally inspired by the Research Agenda—have greatly enhanced data contribution, participation and engagement with the VL platform and have led to collaborative analyses of data received from across all endemic regions.
The SCH and STH Research Agenda has been developed following the same process as used for VL (and across IDDO platforms, Figure 1), reflecting topics identified by systematic scoping reviews 17, 18 , engagement with the communities, and written and revised through a three-stage consultation process:
Figure 1. The Infectious Diseases Data Observatory (IDDO) Research Agenda development process.
Schematic reproduced with permission from https://www.iddo.org/research-agenda-development-process.
-
1.
Internal process: development of the first draft by the Secretariat and the Scientific Advisory Committee (SAC) members
-
2.
External expert process: review of the first draft by key experts in the field and production of a second version of the research agenda
-
3.
Public consultation process: the second version is publicly shared with the scientific community and comments were called from April to July 2020 to produce a first ‘living document’ that can be updated as the research needs of the disease communities evolve.
Version 1.0 of the SCH and STHs Research Agenda is hosted on the IDDO website. This document reflects current consensus from the scientific community on priority research areas that could help to improve treatment (and control/elimination) of SCH and STHs. Hereafter, we provide a contextual overview of these research areas.
Heterogeneity in treatment responses
Responses to anthelmintic treatments vary among individuals 19– 22 and among populations 23, 24 . Variation in treatment responses can be driven by multiple factors, including those relating to demography, spatiotemporal effects 22, 23, 25, 26 , such as potentially emerging anthelminthic resistance or the distribution of low-quality medicine 27, 28 , drug effects, such as differences in the efficacy of treatment regimens and poorly understood individual-level differences. Heterogeneity is also enhanced by methodological, study design and reporting variation that affect the apparent treatment response (i.e., the response measured through the lens of a particular diagnostic used in a particular manner and reported in a particular way). Indeed, it is because of these high levels of heterogeneity in study methodologies, analyses and reporting 17, 18 that discriminating and quantifying different sources of variation using only group/population-level responses (i.e. traditional meta-analyses) becomes difficult to impossible. Comprehensive IPD meta-analyses can overcome some of these challenges and would permit better understanding of the role of different pharmacological, (host and parasite) biological and methodological components in shaping treatment responses. In turn, such understanding will enable optimal evidence-based recommendations and guidance on how best to deploy the medicines to current and future demographic groups that are the cornerstone of global efforts to control and eliminate SCH and STHs.
Characterising spatiotemporal heterogeneity
For both SCH and STHs, there exist examples of geographical and temporal variability in responses to anthelminthics, which have sometimes been linked to the duration of MDA, a proxy of drug pressure and potential driver of anthelminthic resistance. In Uganda, the efficacy of praziquantel against intestinal SCH caused by Schistosoma mansoni, has been shown to be lower in schools with a longer duration (higher drug pressure) of MDA 29 . Elsewhere, S. mansoni populations with reduced susceptibility to praziquantel have been documented in Egypt 30 , Kenya 31 and Senegal 32 . Notwithstanding these reports—and although resistance to praziquantel can be induced in the laboratory—and can emerge in natural populations 30 , there remains no conclusive evidence for its establishment in the field and the topic remains controversial 25, 33, 34 . Moreover, a recent meta-analysis found that the efficacy of praziquantel has been maintained since its introduction as the preferred treatment for SCH in the late 1970s 35 .
Links between the duration of MDA and the efficacy of benzimidazoles have also been reported. In Pemba Island, which has a long history of MDA, poor efficacy of albendazole against Trichuris trichiura (whipworm) and hookworm has been reported 22, 23, 36 , and a population-level meta-analysis found the efficacy of benzimidazoles against whipworm had declined globally between 1995 and 2015 (although this global trend may be biased by the abundance of trials conducted in Pemba Island where the intensity of whipworm is very high and responses are consistently poor) 26 . Benzimidazole treatment is known to select for β-tubulin mutations which are associated with resistance 37, 38 (and particularly so in helminths of veterinary importance 39 ) although currently, no direct association between duration of MDA (drug pressure) and the selection of β-tubulin mutations resulting in reduced efficacy has been documented in the species infecting human populations.
Naturally, factors other than emerging resistance can shape treatment efficacy variation over time and space. An important neglected possible driver is medicine quality, which may differ between countries and regions depending on the source and distribution of the drugs. For example, a relatively high prevalence of poor quality benzimidazoles—linked to the country of origin—has been identified in Ethiopia 28 and quality has also shown to be variable among brands and could cause variable responses 27 . The paucity of published studies that explore medicine quality for SCH 40 and STHs 27, 28 means that it is unclear how quality may shape spatiotemporal heterogeneity in responses. In malaria, poor-quality medicines are recognised as a determinant of treatment failure, morbidity, mortality and drug resistance 41– 43 . The IDDO Medicine Quality Research Group is dedicated to strengthening knowledge about the scale and extent of problems associated with substandard and falsified medicines for human and veterinary diseases.
Numerous factors such as co-infections, drug-drug and host-drug interactions may also shape the response landscape. Many of these may be difficult to distinguish from the variables that typically comprise clinical data. Nevertheless, there exist some intriguing possibilities such as genetic diversity in the cytochrome P 450 enzyme across SCH-endemic regions in Africa being linked to the metabolism—and possibly the efficacy—of praziquantel 44, 45 . But ultimately, a better phenomenological understanding of treatment efficacy—irrespective of the underlying drivers—would be highly beneficial from a pragmatic perspective, particularly as this is so crucial to the effectiveness of PC programmes.
Consequently, we envisage that an important first step in better characterising spatiotemporal heterogeneity will be to map and visualise anthelminthic responses ( Table 1), inspired by the pioneering work of the Worldwide Antimalarial Resistance Network (WWARN) in tracking the emergence and spread of artemisinin-resistant Plasmodium falciparum malaria in Southeast Asia 46 . This would provide an overview of the current geographical picture of anthelmintic responses, and spur more detailed analysis of the IPD hosted by the platform to identify drivers of geographical and temporal heterogeneity, particularly with respect to PC history. This process can begin now with existing submissions to the IDDO platform and be updated as new data are contributed.
Table 1. Priority research themes, activities & timescales.
| Research theme | Activity | Timescale |
|---|---|---|
| Characterising spatiotemporal
variation in treatment responses |
• Development of an efficacy explorer to map responses in space and time
• Engagement to increase research and data collection on anthelminthic quality |
Short-term
Mid-/long-term |
| Improving evidence base for
treatment regimens |
• Individual participant data (IPD) meta-analyses on drug combinations for
treating hookworm & Trichuris trichiura (whipworm) • IPD meta-analyses on effect of dose and frequency of administration on efficacy of praziquantel (e.g. 40 mg/kg vs. 60 mg/kg in single or multiple doses) |
Short-/mid-term
Short-/mid-term |
| Evaluating new antigen-
detection & molecular diagnostics |
• Define reference range of responses to praziquantel measured using antigen
detection methods (CCA or CAA) • Comparison of assays and laboratory protocols for molecular identification of soil-transmitted helminth infection and promotion of standardised approaches |
Short-/mid-term
Short-/mid-term |
| Standardising study design and
reporting |
• Development of a case record form incorporating the data standard developed
by the Clinical Data Interchange Standards Consortium (CDISC) • Engagement to foster adoption of standardised protocols and reporting |
Short-term
Mid-/long-term |
| Medicine safety in pregnancy | • IPD meta-analyses of safety (and efficacy) of praziquantel and benzimidazoles in
pregnant and breastfeeding women |
Short-/mid-term |
| Medicine formulation for
preschool-age children |
• Collation, curation & standardisation of phase III clinical trial data on paediatric
praziquantel formulation |
Short-/mid-term |
| Analytical approaches | • Testing, comparison and recommendations on optimal statistical approaches
for IPD (meta-) analyses using ‘gold standard’ datasets |
Short-/mid-term |
Improving evidence-base for treatment regimens
Praziquantel is used exclusively for PC regimens against SCH, typically given at a dose of 40 mg/kg. Some (but not all 47 ) studies have shown 60 mg/kg (typically divided into three 20 mg/kg doses given over the course of a single day) to be more efficacious than the single 40 mg/kg dose 19, 35, 48, 49 . There also exists evidence that repeated doses of praziquantel may improve responses 50 and that co-administration of food increases bioavailability 51, 52 , which is increasingly recommended as best practice in MDA. Moreover, the efficacy of praziquantel is variable against different Schistosoma species 53 —with little yet known on the susceptibility of hybrids 54– 56 —indicating that modified regimens could be recommended where either intestinal or urogenital infections dominate.
Preventive chemotherapy programmes for STHs are based on single-dose benzimidazoles (albendazole or mebendazole). However, this regimen has poor efficacy against T. trichiura 26, 57, 58 , particularly in heavily infected individuals 59, 60 , and the efficacy of mebendazole against hookworm has also been questioned 61, 62 . There is thus growing consensus that more efficacious regimens are needed to reach control and elimination goals 22 . Combination therapies of benzimidazoles with ivermectin 63– 66 , oxantel pamoate 63, 67, 68 or moxidectin 69 , and tribendimidine with oxantel pamoate 67 have shown substantive improvement in efficacy compared to benzimidazoles alone 57 .
Other demographic (e.g. age, sex), socioeconomic, nutritional and health indicators may influence how an individual responds to treatment. For example, treatment efficacy may be affected by the intensity of both schistosome 70– 72 and soil-transmitted helminths 24, 59, 60, 73 infections, and responses may vary among age groups (e.g. 19, 24). Combined analyses of existing IPD could provide the strength of evidence required to prompt revised recommendations on optimised PC, critically in terms of optimal dosing to treat SCH and optimal combinations to treat STHs ( Table 1), but also considering other individual-level factors that may be important determinants of treatment response. A more nuanced approach to treatment recommendations may be required to take into consideration the various factors that can modify treatment responses, including the geographical distribution and local dominance of different schistosome and soil-transmitted helminth infections.
Evaluating new antigen-detection & molecular diagnostics
Traditionally, responses to anthelmintic treatment have been measured using classical microscopy-based parasitological techniques. Indeed, the WHO defines responses as either ‘satisfactory’, ‘doubtful’ or ‘reduced’ based on so-called egg reduction rates (ERRs), the percent reduction in the post-treatment parasitological egg count compared to the corresponding pre-treatment measurement in a population of treated individuals 74 . However, new antigen-detection and molecular techniques—such as the detection of schistosome circulating cathodic or anodic antigen (CCA/CAA) in urine or serum 75, 76 and the quantification of STH DNA by PCR of stool samples 23, 77, 78 —are increasingly being used as more sensitive alternatives to classical parasitological diagnostic techniques for evaluating treatment responses.
The move towards molecular approaches (particularly in research contexts) brings challenges when interpreting responses that have for decades been quantified using well-understood parasitological measures ( Table 1). More sensitive molecular and antigen-detection diagnostics may yield estimates of efficacy that are lower than those measured by traditional parasitological methods, but this may also depend on the infecting species, when after treatment assessments are undertaken, and what parasitological technique it is being compared with. For example, CCA/CAA levels drop rapidly (within 24 hours) after treatment of schistosome infection with praziquantel 79– 81 but may indicate lower efficacy than parasitology-based assessments (e.g. Kato Katz) because of their higher sensitivity for detecting low-level infections 82 . This is further complicated by the differential performance of antigen-detection diagnostics for the detection of intestinal and urogenital schistosome infections 83, 84 .
The standardisation and commercial availability of some antigen-detection diagnostics (e.g. point-of-care CCA) provide advantages in comparability of results between studies (as well as for other activities such as epidemiological mapping). However, most diagnostics are not standardised and there remain questions on the comparability of molecular diagnostics results derived from assays run in different laboratories 85– 88 and different epidemiological settings 89 . Ultimately, the sharing of data and detailed laboratory protocols and procedures will permit formal comparison of diagnostics both within the context of assessing responses to anthelmintics and more generally 87, 88 .
Standardising study design and reporting
The design of a study assessing anthelmintic responses is crucial to the interpretation of the resulting data. For example, it is known that post-treatment egg counts for both schistosome and soil-transmitted helminths infections tend to be at their lowest approximately 2–3 weeks after treatment, which is why this time window is recommended for efficacy assessment 90, 91 . Although there maybe subtleties in optimal timing for different infections (e.g. between S. mansoni 92 and S. haematobium 93 ), it is more important that a standardised and adequate follow-up time is employed consistently to facilitate comparison and interpretability of results, although the time window for assessment may be quite different for detection of antigens rather than excreted eggs 79 . Similar arguments can be made for the ubiquitous use of the Kato-Katz method for egg microscopy; any inferiority in performance compared to other diagnostics maybe outweighed by the advantages of standardisation 23 .
Notwithstanding, even widely used and relatively standardised tools have elements that can vary between studies and should be recorded (just as detailed protocols should be documented for molecular laboratory techniques). For example, even Kato-Katz test kits from different providers may sometimes yield differences in weight of stool (although this has not been found to require adjustment to the multiplication factor to convert to eggs per gram 94 ). Therefore, details of manufacturers and other specifications of diagnostics and study protocols should be recorded and reported in a standardised fashion to enhance interpretability and comparison. Similarly, there will be variation among technicians in the reading and preparing of Kato-Katz slides, and other microscopy-based approaches, which should be captured by recording individual identifiers for who processed each slide as observed in malaria 95 .
Variability in eligibility criteria among studies can also lead to systematic differences and bias in study outcomes. For example, a common inclusion criterion in an efficacy assessment is for individuals to be diagnosed with infection using a single Kato-Katz slide. But this can lead to positive bias (overestimation) of drug efficacy, particularly when infection levels and/or efficacy are/is low. This can be mitigated by re-testing individuals after the initial eligibility screen and using this re-test measure of infection in subsequent estimations of drug efficacy 96 .
The IDDO platform intends to facilitate the development of a standard case reporting form (CRF) to foster increased standardisation of protocols and reporting for clinical studies on SCH and STHs ( Table 1). This will be achieved through engagement with the respective research communities and will be informed by current and future contributions to the platform. The CRF will also integrate the principles of the Clinical Data Interchange Standards Consortium (CDISC) clinical data standards that the platform is using to curate data contributions, further enhancing data interpretability, clarity and interoperability.
Medicine safety, tolerability and side effects
The drugs used to treat SCH and STHs are considered very safe and associated predominantly with only relatively mild side effects, although the published research in this area is limited. A particular strength of aggregating IPD from multiple studies is to increase power when individual studies are comparatively scarce. Side effects of praziquantel, particularly in heavily infected individuals, can be substantial 97, 98 and may have a deleterious effect on participation with subsequent rounds of MDA 99 . Side effects of benzimidazoles are generally mild (but see 100), including in young children under 5 years old 101, 102 but it will be necessary to assess side effect and tolerability profiles of new combination therapies that improve treatment of T. trichiura and hookworm infections 63, 103 . A key component of any analysis of tolerability is the robust assessment of bias; studies actively collecting information on adverse events are likely rare and those based on passive surveillance, such as during MDA programmes, will be subject to reporting bias 104 .
Safety and responses in understudied groups
Determining safety and drug responses in understudied groups is crucial to defining appropriate inclusion/exclusion criteria for PC. This directly impacts the success of PC programmes that must strive to maximise therapeutic coverage to meet control and elimination goals. Like studies on side effects, data on understudied groups are, by definition, limited which only emphasises further the importance of data sharing to maximise the information and power of IPD. Indeed, the ‘leaving no one behind’ principle, as articulated in the Sustainable Development Goals, has gained prominence as an indicator of neglected tropical disease (NTD) programme success 105 .
Medicine safety in pregnancy
The WHO recommend inclusion of pregnant and breastfeeding women for treatment with praziquantel based on studies that have indicated that it is safe and efficacious 106– 108 . However, praziquantel is still frequently not offered during PC to pregnant or breastfeeding women, sometimes because of prioritisation of school-based rather than community-based delivery of MDA 109 . Data on the safety of other anthelmintics for use in pregnancy are limited 110, 111 and current recommendations indicate treatment only on the second and third trimesters as an important component of antenatal care 112, 113 . New updated analyses using pooled IPD could add considerable value to the evidence-base to support treatment recommendations ( Table 1).
Medicine formulations for preschool-age children
In recent years it has been recognised that treating preschool-age children (less than 5 years old) for SCH may have substantial benefits for preventing morbidity and reducing community transmission 45, 114 . It is recommended that children aged ≤5 years be given a 40 mg/kg dose of praziquantel (doses above 40 mg/kg appear to offer no improvement in response) 47, 115 as crushed tablets 45 . However, the bitter taste of praziquantel has led to operational difficulties 47, 116 and spurred the development of a paediatric formulation by the Paediatric Praziquantel Consortium. Phase III trials are currently ongoing and an important component along the pathway towards registration will be the curation and standardisation of the clinical data and, ideally, its sharing for scrutiny and comparison with existing formulations ( Table 1). More research should also be conducted on the pharmacokinetics of praziquantel in preschool-age children and its bioavailability profile 45 .
The optimal formulation of benzimidazoles for STHs, which are periodically given to preschool-age children over 12 months old 101 , also remains an open question. Both albendazole and mebendazole are available as chewable tablets 117– 119 or can be crushed 120 to minimise the likelihood of choking events 100, 120 . Collating available safety data on the administration of benzimidazole tablets to preschool-age children could provide important information on the frequency of these adverse events and, crucially, highlight safest modes of administration.
Analytical approaches
The WHO provides guidance on analysis protocols for calculating anthelmintic efficacy as ERRs on a population-level basis 90 . These approaches, however, do not extend to IPD when incorporating covariates of the treatment response. A number of new methods have been proposed in both the human 19– 22, 121 and veterinary 122, 123 domains for analysing IPD, but there remain no standardised or consensus approach and many unresolved technical questions. For example, how quantitative expressions of the distribution of drug responses among individuals (e.g., percentage of individuals with a ‘satisfactory’ or ‘reduced’ response) relate to more traditional population-level summaries (e.g., average ERR or cure rate), how accurately can individual suboptimal (or ‘reduced’) responses be identified, and importantly, be distinguished from response variation not associated with decreased efficacy? should responses measured using (multiple) molecular diagnostics be integrated into analytical frameworks? These questions will not be answered by the sharing of data per se, but the assemblage of an abundance of IPD will provide the raw material to test different analytical approaches. We envisage that the platform will play an important role in facilitating collaboration to improve the quality and consistency of methods for IPD meta-analyses in the helminth and NTD domain.
Conclusions
Here, we have given a contextual overview of the Research Agenda that has been developed as part of the process building a SCH and STHs sharing and reuse platform for clinical data. The Research Agenda is not intended to be either prescriptive or exhaustive, but rather to provide a guide to research questions—identified as priorities by the disease control and research communities—that could be tackled through the sharing and reuse of IPD identified by scoping review. Clearly, with time, priority areas will change and the online ‘living’ Research Agenda will evolve to reflect these changes. Indeed, although the scope of the platform is currently restricted to clinical IPD on SCH and STHs, IDDO is committed to responding to the future needs of disease control and research communities. This includes, where practicable, broadening its scope to capture new data and new diseases. For example, in response to strongyloidiasis being included under STHs in the WHO’s priority list of NTDs, future searches to identify studies with suitable IPD will be designed to capture data on treatment of infection by Strongyloides stercoralis 124 . Ultimately, of course, the scope and sustainability of this platform and others are limited by resources and funding. Although the principles of data sharing are widely acclaimed and highly encouraged, stable funding streams are crucial to sustain data platforms as digital resources for the research and disease control communities for future generations. Resources to keep platforms operational, active and updated will ensure that the utility of clinical data and the beneficial impact of data-sharing are fully realised.
Data availability
No data are associated with this article.
Acknowledgements
We thank the following people for providing feedback on the content of this manuscript: Professor Daniel G Colley, University of Georgia; Dr Thomas Crellen, Big Data Institute, University of Oxford; Dr Julia Dunn, Clinton Health Access Initiative; Dr Cristin Fergus, Firoz Lalji Institute for Africa, London School of Economics and Political Science; Mr Amadou Jallow, Ministry of Health, The Gambia; Dr William Lin, EJD Global Health; Mr Bakary Sanneh, Ministry of Health, The Gambia; Dr Anthony Solomon, World Health Organization.
Funding Statement
MW acknowledges funding from Research England’s Connecting Capabilities Fund (Bloomsbury SET [https://bloomsburyset.org.uk/]; BSA34). This work was supported by Wellcome (208378, <a href=https://doi.org/10.35802/208378>https://doi.org/10.35802/208378</a>; a Wellcome Biomedical Resources grant to MW, LTF, JBH, MB and PJG for the Infectious Diseases Data Observatory [https://www.iddo.org/]). MGB acknowledges funding from the Medical Research Council (MRC) Centre for Global Infectious Disease Analysis (MR/R015600/1), jointly funded by the UK MRC and the UK Foreign, Commonwealth & Development Office (FCDO), under the MRC/FCDO Concordat agreement and is also part of the European and Developing Countries Clinical Trials Partnership (EDCTP2) programme supported by the European Union.
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
[version 1; peer review: 2 approved]
References
- 1. Herricks JR, Hotez PJ, Wanga V, et al. : The global burden of disease study 2013: What does it mean for the NTDs? PLoS Negl Trop Dis. 2017;11(8):e0005424. 10.1371/journal.pntd.0005424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hotez PJ, Molyneux DH, Fenwick A, et al. : Control of neglected tropical diseases. N Engl J Med. 2007;357(10):1018–27. 10.1056/NEJMra064142 [DOI] [PubMed] [Google Scholar]
- 3. Hotez PJ, Fenwick A, Savioli L, et al. : Rescuing the bottom billion through control of neglected tropical diseases. Lancet. 2009;373(9674):1570–5. 10.1016/S0140-6736(09)60233-6 [DOI] [PubMed] [Google Scholar]
- 4. World Health Organization: Ending the neglect to attain the Sustainable Development Goals - A road map for neglected tropical diseases 2021-2030.Geneva: World Health Organization;2021. Reference Source [Google Scholar]
- 5. World Health Organization: Neglected tropical diseases: treating more than one billion people for the fifth consecutive year.Geneva: World Health Organization;2020. Reference Source [Google Scholar]
- 6. World Health Organization: Crossing the Billion. Preventive chemotherapy for neglected tropical diseases. Lymphatic filariasis, onchocerciasis, schistosomiasis, soil-transmitted helminthiases and trachoma.Geneva: World Health Organization;2017. Reference Source [Google Scholar]
- 7. World Health Organization: Schistosomiasis and soil-transmitted helminthiases: numbers of people treated in 2019. Wkly Epidemiol Rec. 2020;95:629–40. Reference Source [Google Scholar]
- 8. Traversa D, von Samson-Himmelstjerna G: Anthelmintic resistance in sheep gastro-intestinal strongyles in Europe. Small Rumin Res. 2016;135:75–80. 10.1016/j.smallrumres.2015.12.014 [DOI] [Google Scholar]
- 9. Matthews JB: Anthelmintic resistance in equine nematodes. Int J Parsitol Drugs Drug Resist. 2014;4(3):310–5. 10.1016/j.ijpddr.2014.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kaplan RM: Drug resistance in nematodes of veterinary importance: a status report. Trends Parasitol. 2004;20(10):477–81. 10.1016/j.pt.2004.08.001 [DOI] [PubMed] [Google Scholar]
- 11. Wolstenholme AJ, Fairweather I, Prichard R, et al. : Drug resistance in veterinary helminths. Trends Parasitol. 2004;20(10):469–76. 10.1016/j.pt.2004.07.010 [DOI] [PubMed] [Google Scholar]
- 12. Pisani E, Aaby P, Breugelmans JG, et al. : Beyond open data: realising the health benefits of sharing data. BMJ. 2016;355:i5295. 10.1136/bmj.i5295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Merson L, Gaye O, Guérin PJ: Avoiding data dumpsters—toward equitable and useful data sharing. N Engl J Med. 2016;374(25):2414–5. 10.1056/NEJMp1605148 [DOI] [PubMed] [Google Scholar]
- 14. Humphreys GS, Tinto H, Barnes KI: Strength in Numbers: The WWARN case study of purpose-driven data sharing. Am J Trop Med Hyg. 2019;100(1):13–5. 10.4269/ajtmh.18-0649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Merson L, Guérin PJ, Barnes KI, et al. : Secondary analysis and participation of those at the data source. Lancet Glob Health. 2018;6(9):e965. 10.1016/S2214-109X(18)30341-3 [DOI] [PubMed] [Google Scholar]
- 16. Bull S, Cheah PY, Denny S, et al. : Best Practices for Ethical Sharing of Individual-Level Health Research data from low- and middle-income settings. J Empir Res Hum Res Ethics. 2015;10(3):302–13. 10.1177/1556264615594606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Halder JB, Benton J, Julé AM, et al. : Systematic review of studies generating individual participant data on the efficacy of drugs for treating soil-transmitted helminthiases and the case for data-sharing. PLoS Negl Trop Dis. 2017;11(10):e0006053. 10.1371/journal.pntd.0006053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Julé AM, Vaillant M, Lang TA, et al. : The schistosomiasis clinical trials landscape: a systematic review of antischistosomal treatment efficacy studies and a case for sharing individual participant-level data (IPD). PLoS Negl Trop Dis. 2016;10(6):e0004784. 10.1371/journal.pntd.0004784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Walker M, Mabud TS, Olliaro PL, et al. : New approaches to measuring anthelminthic drug efficacy: parasitological responses of childhood schistosome infections to treatment with praziquantel. Parasit Vectors. 2016;9:41. 10.1186/s13071-016-1312-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Walker M, Churcher TS, Basáñez MG: Models for measuring anthelmintic drug efficacy for parasitologists. Trends Parasitol. 2014;30(11):528–37. 10.1016/j.pt.2014.08.004 [DOI] [PubMed] [Google Scholar]
- 21. Olliaro PL, Vaillant M, Diawara A, et al. : Toward measuring Schistosoma response to praziquantel treatment with appropriate descriptors of egg excretion. PLoS Negl Trop Dis. 2015;9(6):e0003821. 10.1371/journal.pntd.0003821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Walker M, Cools P, Albonico M, et al. : Individual responses to a single oral dose of albendazole indicate reduced efficacy against soil-transmitted helminths in an area with high drug pressure. PLoS Negl Trop Dis. 2021;15(10):e0009888. 10.1371/journal.pntd.0009888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Vlaminck J, Cools P, Albonico M, et al. : Therapeutic efficacy of albendazole against soil-transmitted helminthiasis in children measured by five diagnostic methods. PLoS Negl Trop Dis. 2019;13(8):e0007471. 10.1371/journal.pntd.0007471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Vercruysse J, Behnke JM, Albonico M, et al. : Assessment of the anthelmintic efficacy of albendazole in school children in seven countries where soil-transmitted helminths are endemic. PLoS Negl Trop Dis. 2011;5(3):e948. 10.1371/journal.pntd.0000948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Levecke B, Vlaminck J, Andriamaro L, et al. : Evaluation of the therapeutic efficacy of praziquantel against schistosomes in seven countries with ongoing large-scale deworming programs. Int J Parasitol Drugs Drug Resist. 2020;14:183–7. 10.1016/j.ijpddr.2020.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Moser W, Schindler C, Keiser J: Efficacy of recommended drugs against soil transmitted helminths: systematic review and network meta-analysis. BMJ. 2017;358:j4307. 10.1136/bmj.j4307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Belew S, Getachew M, Suleman S, et al. : Assessment of efficacy and quality of two albendazole brands commonly used against soil-transmitted helminth infections in school children in Jimma Town, Ethiopia. PLoS Negl Trop Dis. 2015;9(9):e0004057. 10.1371/journal.pntd.0004057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Suleman S, Zeleke G, Deti H, et al. : Quality of medicines commonly used in the treatment of soil-transmitted helminths and Giardia in Ethiopia: a nationwide survey. PLoS Negl Trop Dis. 2014;8(12):e3345. 10.1371/journal.pntd.0003345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Crellen T, Walker M, Lamberton PH, et al. : Reduced efficacy of praziquantel against Schistosoma mansoni is associated with multiple rounds of mass drug administration. Clin Infect Dis. 2016;63(9):1151–9. 10.1093/cid/ciw506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ismail M, Botros S, Metwally A, et al. : Resistance to praziquantel: direct evidence from Schistosoma mansoni isolated from Egyptian villagers. Am J Trop Med Hyg. 1999;60(6):932–5. 10.4269/ajtmh.1999.60.932 [DOI] [PubMed] [Google Scholar]
- 31. Melman SD, Steinauer ML, Cunningham C, et al. : Reduced susceptibility to praziquantel among naturally occurring Kenyan isolates of Schistosoma mansoni. PLoS Negl Trop Dis. 2009;3(8):e504. 10.1371/journal.pntd.0000504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Stelma FF, Talla I, Sow S, et al. : Efficacy and side effects of praziquantel in an epidemic focus of Schistosoma mansoni. Am J Trop Med Hyg. 1995;53(2):167–70. 10.4269/ajtmh.1995.53.167 [DOI] [PubMed] [Google Scholar]
- 33. Vale N, Gouveia MJ, Rinaldi G, et al. : Praziquantel for schistosomiasis: single-drug metabolism revisited, mode of action, and resistance. Antimicrob Agents Chemother. 2017;61(5):e02582–16. 10.1128/AAC.02582-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. King CH, Muchiri EM, Ouma JH: Evidence against rapid emergence of praziquantel resistance in Schistosoma haematobium,. Kenya. Emerg Infect Dis. 2000;6(6):585–94. 10.3201/eid0606.000606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Fukushige M, Chase-Topping M, Woolhouse MEJ, et al. : Efficacy of praziquantel has been maintained over four decades (from 1977 to 2018): A systematic review and meta-analysis of factors influence its efficacy. PLoS Negl Trop Dis. 2021;15(3):e0009189. 10.1371/journal.pntd.0009189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Albonico M, Rinaldi L, Sciascia S, et al. : Comparison of three copromicroscopic methods to assess albendazole efficacy against soil-transmitted helminth infections in school-aged children on Pemba Island. Trans R Soc Trop Med Hyg. 2013;107(8):493–501. 10.1093/trstmh/trt051 [DOI] [PubMed] [Google Scholar]
- 37. Orr AR, Quagraine JE, Suwondo P, et al. : Genetic markers of benzimidazole resistance among human hookworms ( Necator americanus) in Kintampo North municipality, Ghana. Am J Trop Med Hyg. 2019;100(2):351–6. 10.4269/ajtmh.18-0727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Diawara A, Halpenny CM, Churcher TS, et al. : Association between response to albendazole treatment and β-tubulin genotype frequencies in soil-transmitted helminths. PLoS Negl Trop Dis. 2013;7(5):e2247. 10.1371/journal.pntd.0002247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Redman E, Whitelaw F, Tait A, et al. : The emergence of resistance to the benzimidazole anthlemintics in parasitic nematodes of livestock is characterised by multiple independent hard and soft selective sweeps. PLoS Negl Trop Dis. 2015;9(2):e0003494. 10.1371/journal.pntd.0003494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Sulaiman SM, Traoré M, Engels D, et al. : Counterfeit praziquantel. Lancet. 2001;358(9282):666–7. 10.1016/S0140-6736(01)05796-8 [DOI] [PubMed] [Google Scholar]
- 41. Evans DR, Higgins CR, Laing SK, et al. : Poor-quality antimalarials further health inequities in Uganda. Health Policy Plan. 2019;34(Supplement 3):iii36–iii47. 10.1093/heapol/czz012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Newton PN, Caillet C, Guerin PJ: A link between poor quality antimalarials and malaria drug resistance? Expert Rev Anti Infect Ther. 2016;14(6):531–3. 10.1080/14787210.2016.1187560 [DOI] [PubMed] [Google Scholar]
- 43. World Health Organization: Guidlines for the treatment of malaria. 3rd edition. Geneva: World Health Organization;2015. Reference Source [Google Scholar]
- 44. Rajman I, Knapp L, Morgan T, et al. : African Genetic Diversity: Implications for cytochrome P450-mediated drug metabolism and drug development. EBioMedicine. 2017;17:67–74. 10.1016/j.ebiom.2017.02.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Osakunor DNM, Woolhouse MEJ, Mutapi F: Paediatric schistosomiasis: What we know and what we need to know. PLoS Negl Trop Dis. 2018;12(2):e0006144. 10.1371/journal.pntd.0006144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Ashley EA, Dhorda M, Fairhurst RM, et al. : Spread of artemisinin resistance in Plasmodium falciparum. malaria. N Eng J Med. 2014;371:411–423. 10.1056/NEJMoa1314981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Coulibaly JT, Panic G, Silue KD, et al. : Efficacy and safety of praziquantel in preschool-aged and school-aged children infected with Schistosoma mansoni: a randomised controlled, parallel-group, dose-ranging, phase 2 trial. Lancet Glob Health. 2017;5(7):e688–e98. 10.1016/S2214-109X(17)30187-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Bustinduy AL, Waterhouse D, de Sousa-Figueiredo JC, et al. : Population pharmacokinetics and pharmacodynamics of praziquantel in Ugandan children with intestinal schistosomiasis: higher dosages are required for maximal efficacy. mBio. 2016;7(4):e00227–16. 10.1128/mBio.00227-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Kabuyaya M, Chimbari MJ, Mukaratirwa S: Efficacy of praziquantel treatment regimens in pre-school and school aged children infected with schistosomiasis in sub-Saharan Africa: a systematic review. Infect Dis Poverty. 2018;7(1):73. 10.1186/s40249-018-0448-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. King CH, Olbrych SK, Soon M, et al. : Utility of repeated praziquantel dosing in the treatment of schistosomiasis in high-risk communities in Africa: a systematic review. PLoS Negl Trop Dis. 2011;5(9):e1321. 10.1371/journal.pntd.0001321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Castro N, Medina R, Sotelo J, et al. : Bioavailability of praziquantel increases with concomitant administration of food. Antimicrob Agents Chemother. 2000;44(10):2903–4. 10.1128/AAC.44.10.2903-2904.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Mandour ME, el Turabi H, Homeida MM, et al. : Pharmacokinetics of praziquantel in healthy volunteers and patients with schistosomiasis. Trans R Soc Trop Med Hyg. 1990;84(3):389–93. 10.1016/0035-9203(90)90333-a [DOI] [PubMed] [Google Scholar]
- 53. Zwang J, Olliaro PL: Clinical efficacy and tolerability of praziquantel for intestinal and urinary schistosomiasis-a meta-analysis of comparative and non-comparative clinical trials. PLoS Negl Trop Dis. 2014;8(11):e3286. 10.1371/journal.pntd.0003286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Fall CB, Lambert S, Léger E, et al. : Hybridized zoonotic Schistosoma. infections result in hybridized morbidity profiles: a clinical morbidity study amongst co-infected human populations of Senegal. Microorganisms. 2021;9(8):1776. 10.3390/microorganisms9081776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Leger E, Webster JP: Hybridizations within the Genus Schistosoma: implications for evolution, epidemiology and control. Parasitology. 2017;144(1):65–80. 10.1017/S0031182016001190 [DOI] [PubMed] [Google Scholar]
- 56. Gower CM, Vince L, Webster JP: Should we be treating animal schistosomiasis in Africa? The need for a One Health economic evaluation of schistosomiasis control in people and their livestock. Trans R Soc Trop Med Hyg. 2017;111(6):244–7. 10.1093/trstmh/trx047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Namwanje H, Kabatereine NB, Olsen A: Efficacy of single and double doses of albendazole and mebendazole alone and in combination in the treatment of Trichuris trichiura. in school-age children in Uganda. Trans R Soc Trop Med Hyg. 2011;105(10):586–90. 10.1016/j.trstmh.2011.07.009 [DOI] [PubMed] [Google Scholar]
- 58. Olsen A, Namwanje H, Nejsum P, et al. : Albendazole and mebendazole have low efficacy against Trichuristrichiura in school-age children in Kabale District, Uganda. Trans R Soc Trop Med Hyg. 2009;103(5):443–6. 10.1016/j.trstmh.2008.12.010 [DOI] [PubMed] [Google Scholar]
- 59. Mekonnen Z, Levecke B, Boulet G, et al. : Efficacy of different albendazole and mebendazole regimens against heavy-intensity Trichuris trichiura. infections in school children, Jimma Town, Ethiopia. Pathog Glob Health. 2013;107(4):207–9. 10.1179/2047773213Y.0000000092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Levecke B, Mekonnen Z, Albonico M, et al. : The impact of baseline faecal egg counts on the efficacy of single-dose albendazole against Trichuris trichiura. Trans R Soc Trop Med Hyg. 2012;106(2):128–30. 10.1016/j.trstmh.2011.09.007 [DOI] [PubMed] [Google Scholar]
- 61. Palmeirim MS, Ame SM, Ali SM, et al. : Efficacy and safety of a single dose versus a multiple dose regimen of mebendazole against hookworm infections in children: a randomised, double-blind trial. EClinicalMedicine. 2018;1:7–13. 10.1016/j.eclinm.2018.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Flohr C, Tuyen LN, Lewis S, et al. : Low efficacy of mebendazole against hookworm in Vietnam: two randomized controlled trials. Am J Trop Med Hyg. 2007;76(4):732–6. [PubMed] [Google Scholar]
- 63. Speich B, Ali SM, Ame SM, et al. : Efficacy and safety of albendazole plus ivermectin, albendazole plus mebendazole, albendazole plus oxantel pamoate, and mebendazole alone against Trichuris trichiura and concomitant soil-transmitted helminth infections: a four-arm, randomised controlled trial. Lancet Infect Dis. 2015;15(3):277–84. 10.1016/S1473-3099(14)71050-3 [DOI] [PubMed] [Google Scholar]
- 64. Knopp S, Mohammed KA, Speich B, et al. : Albendazole and mebendazole administered alone or in combination with ivermectin against Trichuris trichiura: a randomized controlled trial. Clin Infect Dis. 2010;51(12):1420–8. 10.1086/657310 [DOI] [PubMed] [Google Scholar]
- 65. Olsen A: Efficacy and safety of drug combinations in the treatment of schistosomiasis, soil-transmitted helminthiasis, lymphatic filariasis and onchocerciasis. Trans R Soc Trop Med Hyg. 2007;101(8):747–58. 10.1016/j.trstmh.2007.03.006 [DOI] [PubMed] [Google Scholar]
- 66. Belizario VY, Amarillo ME, de Leon WU, et al. : A comparison of the efficacy of single doses of albendazole, ivermectin, and diethylcarbamazine alone or in combinations against Ascaris and Trichuris spp. Bull World Health Organ. 2003;81(1):35–42. [PMC free article] [PubMed] [Google Scholar]
- 67. Moser W, Coulibaly JT, Ali SM, et al. : Efficacy and safety of tribendimidine, tribendimidine plus ivermectin, tribendimidine plus oxantel pamoate, and albendazole plus oxantel pamoate against hookworm and concomitant soil-transmitted helminth infections in Tanzania and Cote d'Ivoire: a randomised, controlled, single-blinded, non-inferiority trial. Lancet Infect Dis. 2017;17(11):1162–71. 10.1016/S1473-3099(17)30487-5 [DOI] [PubMed] [Google Scholar]
- 68. Speich B, Ame SM, Ali SM, et al. : Oxantel pamoate-albendazole for Trichuris trichiura infection. N Engl J Med. 2014;370(7):610–20. 10.1056/NEJMoa1301956 [DOI] [PubMed] [Google Scholar]
- 69. Keller L, Palmeirim MS, Ame SM, et al. : Efficacy and safety of ascending dosages of moxidectin and moxidectin-albendazole against Trichuris trichiura in adolescents: a randomized controlled trial. Clin Infect Dis. 2020;70(6):1193–201. 10.1093/cid/ciz326 [DOI] [PubMed] [Google Scholar]
- 70. Danso-Appiah A, De Vlas SJ: Interpreting low praziquantel cure rates of Schistosoma mansoni infections in Senegal. Trends Parasitol. 2002;18(3):125–9. 10.1016/s1471-4922(01)02209-7 [DOI] [PubMed] [Google Scholar]
- 71. Gryseels B, Mbaye A, De Vlas SJ, et al. : Are poor responses to praziquantel for the treatment of Schistosoma mansoni infections in Senegal due to resistance? An overview of the evidence. Trop Med Int Health. 2001;6(11):864–73. 10.1046/j.1365-3156.2001.00811.x [DOI] [PubMed] [Google Scholar]
- 72. Coulibaly JT, Furst T, Silue KD, et al. : Intestinal parasitic infections in schoolchildren in different settings of Cote d'Ivoire: effect of diagnostic approach and implications for control. Parasit Vectors. 2012;5:135. 10.1186/1756-3305-5-135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Albonico M, Bickle Q, Ramsan M, et al. : Efficacy of mebendazole and levamisole alone or in combination against intestinal nematode infections after repeated targeted mebendazole treatment in Zanzibar. Bull World Health Organ. 2003;81(5):343–52. [PMC free article] [PubMed] [Google Scholar]
- 74. World Health Organization: Ninth meeting of Working Group on Monitoring of Neglected Tropical Diseases Drug Efficacy. Geneva: World Health Organization;2020. Reference Source [Google Scholar]
- 75. Prada JM, Touloupou P, Adriko M, et al. : Understanding the relationship between egg- and antigen-based diagnostics of Schistosoma mansoni infection pre- and post-treatment in Uganda. Parasit Vectors. 2018;11(1):21. 10.1186/s13071-017-2580-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Knopp S, Corstjens PL, Koukounari A, et al. : Sensitivity and specificity of a urine circulating anodic antigen test for the diagnosis of Schistosoma haematobium in low endemic settings. PLoS Negl Trop Dis. 2015;9(5):e0003752. 10.1371/journal.pntd.0003752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Vaz Nery S, Qi J, Llewellyn S, et al. : Use of quantitative PCR to assess the efficacy of albendazole against Necator americanusand Ascarisspp. in Manufahi District, Timor-Leste. Parasit Vectors. 2018;11(1):373. 10.1186/s13071-018-2838-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Easton AV, Oliveira RG, O'Connell EM, et al. : Multi-parallel qPCR provides increased sensitivity and diagnostic breadth for gastrointestinal parasites of humans: field-based inferences on the impact of mass deworming. Parasit Vectors. 2016;9:38. 10.1186/s13071-016-1314-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Kildemoes AO, Vennervald BJ, Tukahebwa EM, et al. : Rapid clearance of Schistosoma mansonicirculating cathodic antigen after treatment shown by urine strip tests in a Ugandan fishing community - Relevance for monitoring treatment efficacy and re-infection. PLoS Negl Trop Dis. 2017;11(11):e0006054. 10.1371/journal.pntd.0006054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. van Lieshout L, De Jonge N, Mansour MM, et al. : Circulating cathodic antigen levels in serum and urine of schistosomiasis patients before and after chemotherapy with praziquantel. Trans R Soc Trop Med Hyg. 1993;87(3):311–2. 10.1016/0035-9203(93)90142-d [DOI] [PubMed] [Google Scholar]
- 81. van Lieshout L, de Jonge N, Bassily S, et al. : Assessment of cure in schistosomiasis patients after chemotherapy with praziquantel by quantitation of circulating anodic antigen (CAA) in urine. Am J Trop Med Hyg. 1991;44(3):323–8. 10.4269/ajtmh.1991.44.323 [DOI] [PubMed] [Google Scholar]
- 82. Hoekstra PT, Casacuberta-Partal M, van Lieshout L, et al. : Efficacy of single versus four repeated doses of praziquantel against Schistosoma mansoni infection in school-aged children from Cote d'Ivoire based on Kato-Katz and POC-CCA: An open-label, randomised controlled trial (RePST). PLoS Negl Trop Dis. 2020;14(3):e0008189. 10.1371/journal.pntd.0008189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Midzi N, Butterworth AE, Mduluza T, et al. : Use of circulating cathodic antigen strips for the diagnosis of urinary schistosomiasis. Trans R Soc Trop Med Hyg. 2009;103(1):45–51. 10.1016/j.trstmh.2008.08.018 [DOI] [PubMed] [Google Scholar]
- 84. de Dood CJ, Hoekstra PT, Mngara J, et al. : Refining Diagnosis of Schistosoma haematobium Infections: Antigen and Antibody Detection in Urine. Front Immunol. 2018;9:2635. 10.3389/fimmu.2018.02635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Papaiakovou M, Pilotte N, Baumer B, et al. : A comparative analysis of preservation techniques for the optimal molecular detection of hookworm DNA in a human fecal specimen. PLoS Negl Trop Dis. 2018;12(1):e0006130. 10.1371/journal.pntd.0006130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Cools P, van Lieshout L, Koelewijn R, et al. : First international external quality assessment scheme of nucleic acid amplification tests for the detection of Schistosoma and soil-transmitted helminths, including Strongyloides: a pilot study. PLoS Negl Trop Dis. 2020;14(6):e0008231. 10.1371/journal.pntd.0008231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Cools P, Vlaminck J, Verweij JJ, et al. : Quantitative PCR in soil-transmitted helminth epidemiology and control programs: Toward a universal standard. PLoS Negl Trop Dis. 2021;15(3):e0009134. 10.1371/journal.pntd.0009134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Papaiakovou M, Littlewood DTJ, Gasser RB, et al. : How qPCR complements the WHO roadmap (2021-2030) for soil-transmitted helminths. Trends Parasitol. 2021;37(8):698–708. 10.1016/j.pt.2021.04.005 [DOI] [PubMed] [Google Scholar]
- 89. Graeff-Teixeira C, Favero V, Pascoal VF, et al. : Low specificity of point-of-care circulating cathodic antigen (POCCCA) diagnostic test in a non-endemic area for schistosomiasis mansoni in Brazil. Acta Trop. 2021;217:105863. 10.1016/j.actatropica.2021.105863 [DOI] [PubMed] [Google Scholar]
- 90. World Health Organization: Assessing the efficacy of anthelmintic drugs against schistosomiasis and soil-transmitted helminthiases. Geneva: World Health Organization;2013. Reference Source [Google Scholar]
- 91. Levecke B, Easton AV, Cools P, et al. : The optimal timing of post-treatment sampling for the assessment of anthelminthic drug efficacy against Ascaris infections in humans. Int J Parasitol Drugs Drug Resist. 2018;8(1):67–9. 10.1016/j.ijpddr.2017.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Scherrer AU, Sjoberg MK, Allangba A, et al. : Sequential analysis of helminth egg output in human stool samples following albendazole and praziquantel administration. Acta Trop. 2009;109(3):226–31. 10.1016/j.actatropica.2008.11.015 [DOI] [PubMed] [Google Scholar]
- 93. Stete K, Krauth SJ, Coulibaly JT, et al. : Dynamics of Schistosoma haematobium egg output and associated infection parameters following treatment with praziquantel in school-aged children. Parasit Vectors. 2012;5:298. 10.1186/1756-3305-5-298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Leuenberger A, Nassoro T, Said K, et al. : Assessing stool quantities generated by three specific Kato-Katz thick smear templates employed in different settings. Infect Dis Poverty. 2016;5(1):58. 10.1186/s40249-016-0150-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Das D, Dahal P, Dhorda M, et al. : A systematic literature review of microscopy methods reported in malaria clinical trials. Am J Trop Med Hyg. 2020;104(3):836–841. 10.4269/ajtmh.20-1219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Coffeng LE, Levecke B, Hattendorf J, et al. : Survey design to monitor drug efficacy for the control of soil-transmitted helminthiasis and schistosomiasis. Clin Infect Dis. 2021;72(Suppl 3):S195–S202. 10.1093/cid/ciab196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Jaoko WG, Muchemi G, Oguya FO: Praziquantel side effects during treatment of Schistosoma mansoni infected pupils in Kibwezi, Kenya. East Afr Med J. 1996;73(8):499–501. [PubMed] [Google Scholar]
- 98. Berhe N, Gundersen SG, Abebe F, et al. : Praziquantel side effects and efficacy related to Schistosoma mansoni egg loads and morbidity in primary school children in north-east Ethiopia. Acta Trop. 1999;72(1):53–63. 10.1016/s0001-706x(98)00084-9 [DOI] [PubMed] [Google Scholar]
- 99. Muhumuza S, Olsen A, Katahoire A, et al. : Reduced uptake of mass treatment for schistosomiasis control in absence of food: beyond a randomized trial. BMC Infect Dis. 2015;15:423. 10.1186/s12879-015-1158-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Kernell JW, DePaola RV, Maglione AM, et al. : Risk of adverse swallowing events and choking during deworming for preschool-aged children. PLoS Negl Trop Dis. 2018;12(6):e0006578. 10.1371/journal.pntd.0006578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Montresor A, Awasthi S, Crompton DWT: Use of benzimidazoles in children younger than 24 months for the treatment of soil-transmitted helminthiasis. Acta Trop. 2003;86(2–3):223–32. 10.1016/s0001-706x(03)00042-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Albonico M, Allen H, Chitsulo L, et al. : Controlling soil-transmitted helminthiasis in pre-school-age children through preventive chemotherapy. PLoS Negl Trop Dis. 2008;2(3):e126. 10.1371/journal.pntd.0000126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Palmeirim MS, Hurlimann E, Knopp S, et al. : Efficacy and safety of co-administered ivermectin plus albendazole for treating soil-transmitted helminths: a systematic review, meta-analysis and individual patient data analysis. PLoS Negl Trop Dis. 2018;12(4):e0006458. 10.1371/journal.pntd.0006458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Jittamala P, Monteiro W, Smit MR, et al. : A systematic review and an individual patient data meta-analysis of ivermectin use in children weighing less than fifteen kilograms: is it time to reconsider the current contraindication? PLoS Negl Trop Dis. 2021;15(3):e0009144. 10.1371/journal.pntd.0009144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Fitzpatrick C, Engels D: Leaving no one behind: a neglected tropical disease indicator and tracers for the Sustainable Development Goals. Int Health. 2016;8 Suppl 1(Suppl 1):i15–8. 10.1093/inthealth/ihw002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Adam I, Elwasila ET, Homeida M: Is praziquantel therapy safe during pregnancy? Trans R Soc Trop Med Hyg. 2004;98(9):540–3. 10.1016/j.trstmh.2004.01.001 [DOI] [PubMed] [Google Scholar]
- 107. Olveda RM, Acosta LP, Tallo V, et al. : Efficacy and safety of praziquantel for the treatment of human schistosomiasis during pregnancy: a phase 2, randomised, double-blind, placebo-controlled trial. Lancet Infect Dis. 2016;16(2):199–208. 10.1016/S1473-3099(15)00345-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Qian C, Gong F: Praziquantel for schistosomiasis in pregnancy. Lancet Infect Dis. 2016;16(5):525–6. 10.1016/S1473-3099(16)30009-3 [DOI] [PubMed] [Google Scholar]
- 109. Friedman JF, Olveda RM, Mirochnick MH, et al. : Praziquantel for the treatment of schistosomiasis during human pregnancy. Bull World Health Organ. 2018;96(1):59–65. 10.2471/BLT.17.198879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Haider BA, Humayun Q, Bhutta ZA: Effect of administration of antihelminthics for soil transmitted helminths during pregnancy. Cochrane Database Syst Rev. 2009; (2):CD005547. 10.1002/14651858.CD005547.pub2 [DOI] [PubMed] [Google Scholar]
- 111. Ndibazza J, Muhangi L, Akishule D, et al. : Effects of deworming during pregnancy on maternal and perinatal outcomes in Entebbe, Uganda: a randomized controlled trial. Clin Infect Dis. 2010;50(4):531–40. 10.1086/649924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. St-Denis K, Blouin B, Rahme E, et al. : Ruling out early trimester pregnancy when implementing community-based deworming programs. PLoS Negl Trop Dis. 2020;14(1):e0007901. 10.1371/journal.pntd.0007901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Bangert M, Bancalari P, Mupfasoni D, et al. : Provision of deworming intervention to pregnant women by antenatal services in countries endemic for soil-transmitted helminthiasis. PLoS Negl Trop Dis. 2019;13(5):e0007406. 10.1371/journal.pntd.0007406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Faust CL, Osakunor DNM, Downs JA, et al. : Schistosomiasis control: leave no age group behind. Trends Parasitol. 2020;36(7):582–91. 10.1016/j.pt.2020.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Montresor A, Garba A: Treatment of preschool children for schistosomiasis. Lancet Glob Health. 2017;5(7):e640–e1. 10.1016/S2214-109X(17)30202-4 [DOI] [PubMed] [Google Scholar]
- 116. Sousa-Figueiredo JC, Pleasant J, Day M, et al. : Treatment of intestinal schistosomiasis in Ugandan preschool children: best diagnosis, treatment efficacy and side-effects, and an extended praziquantel dosing pole. Int Health. 2010;2(2):103–13. 10.1016/j.inhe.2010.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. World Health Organization: Pharmacopoeial standards: ensuring the efficacy of a deworming medicine: albendazole chewable tablets. WHO Drug Information. 2015;29(4):440–445. Reference Source [Google Scholar]
- 118. Palmeirim MS, Bosch F, Ame SM, et al. : Efficacy, safety and acceptability of a new chewable formulation versus the solid tablet of mebendazole against hookworm infections in children: an open-label, randomized controlled trial. EClinicalMedicine. 2020;27:100556. 10.1016/j.eclinm.2020.100556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Silber SA, Diro E, Workneh N, et al. : Efficacy and safety of a single-dose mebendazole 500 mg chewable, rapidly-disintegrating tablet for Ascaris lumbricoides and Trichuris trichiura infection treatment in pediatric patients: a double-blind, randomized, placebo-controlled, phase 3 study. Am J Trop Med Hyg. 2017;97(6):1851–1856. 10.4269/ajtmh.17-0108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. World Health Organization: Promoting safety of medicines for children.Geneva: World Health Organization;2007. Reference Source [Google Scholar]
- 121. Denwood MJ, Innocent GT, Prentice JC, et al. : A hypothesis testing framework for the ratio of means of two negative binomial distributions: classifying the efficacy of anthelmintic treatment against intestinal parasites.2019. Reference Source [Google Scholar]
- 122. Denwood MJ, Reid SWJ, Love S, et al. : Comparison of three alternative methods for analysis of equine Faecal Egg Count Reduction Test data. Prev Vet Med. 2010;93(4):316–23. 10.1016/j.prevetmed.2009.11.009 [DOI] [PubMed] [Google Scholar]
- 123. Torgerson PR, Paul M, Furrer R: Evaluating faecal egg count reduction using a specifically designed package "eggCounts" in R and a user friendly web interface. Int J Parasitol. 2014;44(5):299–303. 10.1016/j.ijpara.2014.01.005 [DOI] [PubMed] [Google Scholar]
- 124. Hofmann D, Sayasone S, Sengngam K, et al. : Efficacy and safety of ascending doses of moxidectin against Strongyloides stercoralis infections in adults: a randomised, parallel-group, single-blinded, placebo-controlled, dose-ranging, phase 2a trial. Lancet Infect Dis. 2021;21(8):1151–60. 10.1016/S1473-3099(20)30691-5 [DOI] [PubMed] [Google Scholar]