Abstract
Rationale.
Applying an intersectional framework to quantitative public health research among Black and Latino sexual minority men requires analysis that considers interlocking, multidimensional systems of racist and homonegative oppression that fundamentally subvert health. In this study, person-centered methods reflected the complexity of intersecting stigma and how subgroups experience that intersection differently.
Methods.
Data were from a cohort of 435 Black and Latino sexual minority young men (mean age=22.3 years) in the Healthy Young Men’s Cohort Study in Los Angeles, United States. Participants provided data semiannually on five occasions spanning 24 months from 2016 to 2019. The marginal approach to longitudinal latent class analysis was used to identify latent classes indicated by multidimensional experiences of racism (e.g., police harassment, workplace discrimination, sexual objectification) and homonegativism (e.g., violence, family rejection, identity concealment) during the transition to adulthood. Associations between sociostructural burdens (e.g., socioeconomic status, food insecurity, unstable housing) and class incidents were investigated. Prevalence of mental health care needs, chronic health conditions, and overall self- reported health were compared among classes.
Results.
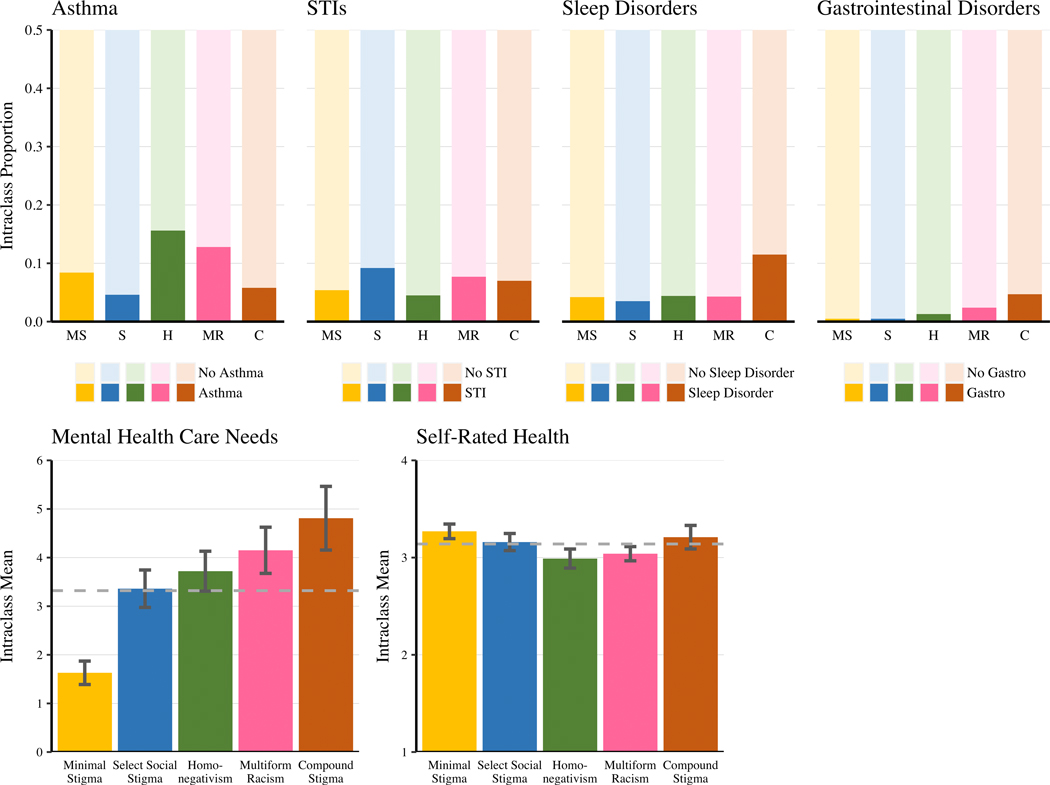
Five latent classes were identified: Minimal Stigma (26% of person records), Select Social Stigma (22%), Homonegativism (17%), Multiform Racism (24%), and Compound Stigma (11%). Sociostructural burdens were generally associated with 1.69 to 3.75 times higher odds of Select Social Stigma, Homonegativism, Multiform Racism, and Compound Stigma class incidents relative to Minimal Stigma. The Compound Stigma class had the greatest sociostructural burden, highest mental health care needs, and highest odds of sleep and gastrointestinal disorders, but classes did not differ in overall self-reported health.
Conclusion.
These results exemplify how sociostructural burdens are interconnected with intersectional stigma experiences that together erode the health of Black and Latino sexual minority young men.
Keywords: discrimination, homophobia, intersectionality, latent class analysis, mental health, physical health, racism, socioeconomic status
INTRODUCTION
For Black and Latino sexual minorities, experiences at the intersection of racism and homonegativism reflect the pervasive reach of stigma across many contexts, levels, and relationships (Bowleg, 2013; Crenshaw, 1989). Myriad studies identify stigma as a fundamental cause of health disparities and demonstrate the connection of stigma with diverse physical health outcomes (e.g., asthma, sexually transmitted infections, sleep, gastrointestinal disorders)(Blosnich et al., 2013; Dyar et al., 2019; Jeffries and Johnson, 2015; Patterson and Potter, 2019) and elevated mental health care needs (Clark et al., 1999; Cochran et al., 2017; Denton et al., 2014; Meyer, 1995; Phelan and Link, 2015). Intersectionality provides a framework for understanding and analyzing how unique intersecting stigma experiences embedded in broader contexts of inequity converge to negatively impact the health of Black and Latino sexual minority men (Bauer, 2014; Bowleg, 2013; Crenshaw, 1989). Understanding how intersectional stigma impacts health is especially important during the transition to adulthood when the association between stigma and health disparities is especially strong (Layland et al., 2020b; Rice et al., 2021).
For Black and Latino young men, racism remains a fundamental cause of health disparities impacting physical and psychological health through numerous multilevel mechanisms (Phelan and Link, 2015; Priest and Williams, 2018; Williams et al., 2019). Acute stressful events and chronic experiences of racism contribute to shifts in behavioral patterns, emotional dysregulation, and physiological responses that directly impact health (Clark et al., 1999; Priest and Williams, 2018). Racism invades diverse contexts including health care setting (Hammond, 2010), the workplace (Allen, 2019), and gay bars (Diaz et al., 2001). Likewise, perpetrators are innumerable, including police (Brunson, 2007), potential romantic and sexual partners (Hidalgo et al., 2020), and employers (Allen, 2019). Racism is a multidimensional, insidious force that permeates diverse contexts, impacting individual health through many concurrent experiences.
Minority stress theory posits homonegativism as an underlying cause of health disparities among sexual minorities (Brooks, 1981; Meyer, 2003, 1995). Because sexual minorities often live within contexts defined by dominant heterosexual norms, minority stress is considered broad and chronic (Meyer, 1995). Sexual minorities may experience violent hate crimes (Herek, 2009), family rejection (Puckett et al., 2015), police harassment (Mallory et al., 2015), and workplace discrimination (Galupo and Resnick, 2016). To avoid perpetrators and contexts where homonegative stigma is expected, sexual minorities may adopt protective strategies (Herek et al., 2009). Examples of behavioral responses driven by anticipated homonegativism include concealing sexual orientation (Pachankis, 2007) and avoiding family and friends (Diaz et al., 2001). Anticipation of homonegativism can contribute to shame, emotional dysregulation, and social isolation that in turn impact health (Meyer, 2003; Pachankis, 2007). Additionally, sexual minority individuals experience internalized homonegativism when they accept and integrate societal messages about the inferiority of sexual minorities into their personal value systems (Herek et al., 2009), which is often related to mental health (Herek et al., 2009; Meyer, 2003; Puckett et al., 2015).
From an intersectional perspective, social identities cannot be divided into mutually exclusive, unidimensional categories wherein one identity (e.g., race/ethnicity, sexual orientation) fully explains disparities without considering other intersecting identities and stigma experiences (Bowleg, 2012). Unidimensional studies consistently find links of racism or homonegativism with mental health and diverse chronic health conditions (Hammond, 2010; Lick et al., 2013; Meyer, 2003; Puckett et al., 2015), but rarely is the intersection of racism and homonegativism considered when quantitatively investigating health disparities among Black and Latino sexual minority men.
An Intersectional Perspective
Intersectionality provides a framework for understanding how multiple identities (e.g., race, sexual identity) converge in personal, individual experiences—including interpersonal experiences of stigma—that reflect multiple interlocking systems of oppression (Bowleg, 2012; Crenshaw, 1989). Systems of oppression refers to the far-reaching ways in which racism and homonegativism are normalized, legalized, and institutionalized to ensure maintenance of power and unequal distribution of resources for marginalized groups (Herek, 2004; Jones, 2000). While these systems permeate many structures related to health, it is often through interpersonal experiences of enacted stigma where people with marginalized identities experience racism and homonegativism explicitly.
Compartmentalization of identities into discrete dimensions overlooks intersections that exist for multiple identities and ignores power and oppression linked to group membership (Bowleg, 2013; Bauer, 2014). Qualitative intersectional research provides extensive evidence that experiences of racism and homonegativism for Black and Latino sexual minorities intersect to form new, unique experiences of stigma that are more than the additive summing of unidimensional identities and stigma experiences (Bowleg, 2008; Bowleg, 2013; Schmitz et al., 2020). Quantitative studies of intersecting experiences should reflect this complexity rather than reduce stigma’s impact to additive effects (Bauer, 2014; Bowleg, 2008), which posit that adding together separate effects of racial/ethnic identity and sexual identity can account for the combined effect of multiple sources of stigma. For example, in a qualitative study, Black gay and bisexual men described intertwining stereotypes portraying both Black men and gay men as hypersexual and aggressively promiscuous, thus making it difficult, if not impossible, to disentangle stigma centered at the intersection of race and sexual orientation (and gender) (Bowleg, 2013). Additionally, sexual racism (i.e., racial/ethnic sexual objectification or rejection) experienced by Black and Latino sexual minority men has been linked to mental health problems (Hidalgo et al., 2020). Intersectional studies of stigma among Black and Latino sexual minority men must consider how systems of racism and homonegativism converge to exacerbate stress and erode health in ways not captured when systems are modeled independently or additively.
Despite recent uptake of intersectionality in contemporary public health research, quantitative approaches to intersectional stigma remain a challenge, and intersectionality scholars continue to call for research that reflects stigma’s multidimensionality (Agénor, 2020; Bauer, 2014; Bowleg, 2008; Turan et al., 2019). In a critical overview of quantitative approaches to intersectionality, Bauer outlined the limitations of relying on additive approaches for variable centered analysis of intersectional processes (Bauer, 2014). Additive approaches to intersectional analysis can suggest an individual’s experience is a summation of their inseparable parts, which in turn can inadvertently erase the unique lived experiences at the intersection of multiple identities and oppressions (Bowleg, 2008). The most common quantitative approach to intersectional analysis and moving beyond an additive approach is to include interaction terms in regression (Turan et al., 2019). Moderated regression models with interaction terms are especially useful for intercategorical approaches to intersectional research in which effects of social processes are compared between groups (McCall, 2005; Turan et al., 2019). For example, in a recent study on LGBT community connection and mental health, regression models included interaction terms between community connection and race/ethnicity and demonstrated a stronger protective effect of community connection for gay men of color, compared to White gay men (Petruzzella et al., 2019). This approach is flexible and especially useful for comparisons between groups; however, at times main effects may account for the majority of the variance in a model and make it difficult to detect meaningful interactions (Turan et al., 2019).
Disparity-focused, between-group research may mask heterogeneity in stigma experiences and health outcomes among sexual minority men (Diamond, 2003; Plö et al., 2015). Person-centered methods can optimally decompose this heterogeneity by identifying subgroups characterized by similar multidimensional patterns of stigma experiences in ways traditional variable-centered approaches cannot. Contrasted with traditional, variable-centered approaches to quantitative intersectional analyses, latent class analysis (LCA) applies a person-centered approach to identify subgroups characterized by similar experiences of stigma. This approach models intersecting stigma as a holistic, embodied experience without artificial division into split identities or experiences. LCA provides greatest utility when qualitatively discrete subgroups within a population are identifiable based on distinct constellations of shared characteristics (Collins and Lanza, 2010). Research conducting LCA among sexual minority People of Color has often identified subgroups along a low to high stigma continuum or subgroups contrasted by no, single, or multiple sources of stigma (Earnshaw et al., 2018; Shramko et al., 2018). These contributions set a foundation exemplifying how LCA can be used to enrich our understanding of intersecting stigma but do not model the many different ways racism and homonegativism may be concurrently experienced by Black and Latino sexual minority men. By analyzing myriad stigma experiences across contexts, perpetrators, forms, and frequency, LCA can uncover subgroups who experience stigma differently and how these unique constellations of stigma may differentially impact health.
Extensions of LCA with covariates and outcomes can situate subgroups in context and in relation to health outcomes (Collins and Lanza, 2010). Analysis that focuses on only interpersonal or internalized stigma may fail to capture the numerous ways that individual experiences with sociostructural systems also severely impact health. For example, the socioeconomic burdens (e.g., financial strain, low education, unemployment), material deprivation (food insecurity, unmet basic needs), and unstable living situation (e.g., housing instability, incarceration) together with stigma erode the health of Black and Latino sexual minority men. Though often studied between unidimensional identities (e.g., contrasting race groups or sexual orientation), extensive evidence demonstrates disparities in sociostructural burdens and resultant mental and physical health consequences (Downing and Rosenthal, 2020; Gates, 2014; LoSchiavo et al., 2020; Raifman et al., 2021; Wang and Green, 2010). By situating intersectional stigma experiences of Black and Latino sexual minority men in the context of sociostructural burden, it is possible to identify subgroups who experience intersecting stigma differently and document how unique patterns of stigma converge with sociostructural burdens to impact mental and physical health.
Study Aims
The current study aimed to identify subgroups indicated by constellations of racist and homonegative stigma experiences among Black and Latino sexual minority young men during the transition to adulthood. Next, we investigated associations between sociostructural burdens (low education, unemployment, sex exchange, unmet basic needs, food insecurity, unstable housing, incarceration history) and subgroup incidents. Finally, we tested associations of subgroups with mental health care needs, chronic health conditions (asthma, STIs, sleep disorders, and gastrointestinal disorders), and self-rated health, while simultaneously accounting for sociostructural burdens. Disparities between sexual minority men and heterosexual men, often attributed to experiences of stigma, have been demonstrated for each of these health outcomes in the past (Blosnich et al., 2013; Dyar et al., 2019; Jeffries and Johnson, 2015; Patterson and Potter, 2019) and further examination at the intersection of racism and homonegativism is needed. Subgroup constellations characterized by multidimensional stigma experiences—including greater frequency and greater diversity in stigma forms, contexts, and perpetrators—were hypothesized to be positively associated with mental health care needs and chronic health conditions and negatively associated with self-rated health, compared to subgroups characterized by constellations with lower or no stigma experiences.
METHODS
Data were from the Healthy Young Men’s Cohort Study (n=448), a 2-year longitudinal study beginning in 2016 (Kipke et al., 2019). The study utilized venue-based recruitment, social media, and participant and health clinic referrals to identify eligible individuals who (1) were aged 16 to 24 years; (2) were assigned male sex at birth; (3) self-identified as gay, bisexual, or uncertain about their sexual orientation; (4) reported sex with a man within the past year; (5) self-identified as Black or Latino; and (6) lived in the Los Angeles area. Ethical research approval was provided by Children’s Hospital Los Angeles. Participants provided written consent.
Sample
Thirteen participants were excluded who did not initially identify as cis-gender men, resulting in an analytical sample of 435 participants. The sample included Latino (58.9%), Black (21.1%), and Afro-Latino (20.0%) sexual minority men. Baseline participant age ranged from 16.2 to 25.2 years (M = 22.3, SD = 2.0). Most participants identified as gay (75.9%) and were not living with HIV (89.0%). Participants completed survey assessments at baseline and every six months for two years, yielding five data occasions for analysis. Across occasions, retention rates were high (89%−93%) versus baseline. Compared to retained participants, attriters at 24 months did not differ by race, sexual identity, or HIV status. At 24 months, attriters were, on average, younger at baseline than participants who were retained (t = 2.45; p = .01).
Measures
Stigma
Stigma measurement followed the intracategorical approach to intersectional research (McCall, 2005) and reflected in-depth exploration of diverse experiences of racist and homonegative stigma forms, perpetrators, contexts, severity, and frequency rather than limited measures of stigma compared across many different identities (i.e., intercategorical). Stigma was measured with 16 items from the Diaz et al. (Diaz et al., 2001) indices of racism and homonegativity and one shortened scale score from Ross and Rosser’s internalized homophobia measure (Ross and Rosser, 1996). Experiences of racism and homonegativism were measured across diverse contexts (e.g., work, gay bars, relationships, family), perpetrators (e.g., police, employers, romantic and sexual partners, friends), forms (e.g., violence, discrimination, prejudice, felt stigma, internalized stigma) and frequency.
Racism.
At baseline participants reported how often they experienced each of 10 racism items since childhood. Participants reported how often they experienced violence, general mistreatment, police harassment, and workplace discrimination, how often they felt uncomfortable in gay bars and clubs, and how often they had trouble finding a relationship due to their race/ethnicity. Four items assessed experiences of racism in romantic/sexual relationship contexts: how often their sexual partners were preoccupied with their race/ethnicity, how often partners and potential partners rejected, sexualized (i.e., made sexual comments), or objectified them. Responses were coded never (1), once or twice (2), and a few times/multiple times (3). All items were assessed at every data occasion.
Homonegativism.
On six items, participants reported how often since childhood they experienced any violence, police harassment, and workplace discrimination related to their sexuality (Diaz et al., 2001). Participants reported how often they experienced three types of felt stigma and related self-preservation strategies related to their sexuality: How often they felt their sexuality embarrassed their family, they avoided family and friends because of their sexuality, and they concealed their sexual identity to be accepted. Item responses were coded to never (1), once or twice (2), and a few times/multiple times (3). All items were assessed at every data occasion. The recall period was ever in adulthood at baseline through 18-month follow-up and past six months at 24-month follow-up for both racism and homonegativism items. Sensitivity analyses indicated inclusion of follow-up data at 24-months did not alter model results.
To measure internalized stigma, participants rated their agreement with four statements about their affect toward their own sexual attractions and behavior (e.g., I feel stress or conflict within myself over having sex with men) (Ross and Rosser, 1996). Response options ranged from strongly disagree (1) to strongly agree (4) (α=.87-.93). Items were averaged then discretized into a single, three-level categorical variable [low (scores <2), mixed (scores ≥2 and <3), high (scores ≥3)] to match a 3-level structure across all indicators and increase ease of interpretation in the latent class model. Higher levels indicate more internalized homonegativism. Combined with the homonegative discrimination items and a single score for internalized homonegativism, there were seven total homonegative items.
Sociostructural Burdens
Sociostructural burdens included individual low education, unemployment, sex exchange, food insecurity, unmet basic needs, unstable housing, and incarceration history. Education contrasted high school or less with any post-secondary to reflect economic benefits of any higher education (Vuolo et al., 2016). Unemployment indicated being unemployed and seeking work but unable to find work in the past six months (Nott and Vedhara, 1995). Sex exchange included any sex in exchange for money, a place to stay, clothes/jewelry, travel, a job, drugs, or a car/ride during the past six months. The six-item Household Food Security Survey (USDA, 2012) measuring past-year food insecurity was dichotomized as recommended to contrast food insecurity with food security. Unmet basic needs indicated how frequently (never, <once a month, once a month, 1–3 times a month, once a week, many times a week) participants ran out of money to meet basic needs in the past three months with scores ranging from one to six. Unstable housing indicated ever going without a place to sleep. Incarceration history included ever spending time in jail or prison. Across follow-up occasions, the recall period was past six months for sociostructural burdens.
Health Outcomes
Participants reported whether in the past six months (past year at baseline) they needed mental health care or counseling for each of 36 mental health conditions including anxiety, helplessness, lack of motivation, thoughts of suicide, eating disorders, and social withdrawal. The number of items endorsed was summed into a mental healthcare needs score representing overall need. Participants reported past 6-month (lifetime at baseline) diagnosis of 30 physical chronic health conditions. The four most common types in this sample (Kipke et al., 2020) were included as binary outcomes: asthma, sexually transmitted infections (STIs: herpes, HPV, hepatitis), sleep related disorders, and gastrointestinal disorders. Participant self-reported health compared their own health to other people their age as poor, fair, good, or excellent (1–4). Sensitivity analyses tested whether model results and interpretation changed when excluding baseline measures of lifetime chronic health outcomes; no meaningful changes in magnitude, direction, or significance of findings were observed.
Covariates
Covariates included age (continuous), race/ethnicity (Black, Afro-Latino, Latino as referent), sexual identity (gay vs. other sexualities), and HIV status.
Analytical approach
Analysis followed the recommended three-step approach to LCA with covariates and outcomes (Dziak et al., 2016). First, the latent class model was identified. Second, participant records were assigned to latent classes using modal posterior probabilities. Third, associations between latent class incidents and sociostructural burdens and health outcomes were estimated using an adjustment for error in modal assignments. These three steps achieved the study aims: identify latent subgroups indicated by racist and homonegative stigma experiences, investigate differences in sociostructural burdens among subgroups, and test associations between subgroup incidents and health outcomes.
Using participant reports of racism (10 three-level indicators) and homonegativism (7 three-level indicators) frequency, the marginal-means approach to longitudinal LCA used data from all participant records at any occasion to identify subgroup constellations of racist and homonegative stigma (Diggle et al., 2002; Vermunt, 2010a). We chose this approach because (1) we observed instability in participants’ stigma experiences over time, (2) there was no developmental event or timing expected to give meaning to transitions in latent classes of stigma, and (3) we did not want to reduce the diversity of intersecting indicators representing the pervasive reach of racism and homonegativism experienced by participants. This approach is well-suited to identifying robust, sample-level patterns in a developmental period but does not estimate individual developmental change (Vermunt, 2010a). Thus, by using repeated measures data across two years, the latent classes identified represent the classes that exist across the transition to adulthood in this sample; at any given data occasion, a participant may be estimated to belong to a different class. When person records are estimated to belong to a class at a given occasion, it is labeled as an incident of belonging to a class. For example, an individual may be most likely to belong to Class 1 at baseline and 6-months and to Class 2 at 12-, 18-, and 24- months; thus, the first two records were incidents of Class 1 and later three records were incidents of Class 2. As recommended, latent class estimate standard errors were adjusted for the non-independent data structure due to repeated measures within persons (Diggle et al., 2002; Vermunt, 2010a).
To select the optimal number of classes, relative model fit criteria (AIC, BIC, adjusted-BIC), model stability, and theoretical interpretability were considered in models with one to eight classes (Collins and Lanza, 2010). Analyses were conducted using Mplus V8.4 (Muthen and Muthen, 2017). Estimation of latent class item-response probabilities and class incident prevalences used full information maximum likelihood with robust error variance, as recommended for non-normal, non-independent observed data. Maximum likelihood parameter estimate identification was confirmed for all models using 1000 initial, 500 second, and 10 final stage sets of random starting values. All person records with data on at least one stigma item were retained.
Measurement invariance of the latent class structure was tested across racial/ethnic groups, age groups, sexual identity, and HIV status by comparing more parsimonious models (i.e., item-response probabilities constrained across groups) to expanded models (i.e., probabilities free across groups). A significant likelihood ratio test, accompanied by minimized model fit criteria (AIC, BIC, adjusted-BIC), indicated a need to examine model structure for meaningful differences in class interpretations across known groups.
The standard, adjusted three-step approach (Vermunt, 2010b) to covariates estimated associations of sociostructural burdens with odds of class incidents. This describes changes in odds of class incidents (versus a reference class) given presence (versus absence) of each sociostructural burden, controlling for covariates. The recommended, adjusted three-step approach (Bakk and Vermunt, 2016; Dziak et al., 2016) to outcomes estimated associations of class incidents with mental health care needs, odds of chronic conditions, and self-reported health using linear and logistic regression and controlling for sociostructural burdens and covariates. This approach uses modal posterior probability assignment to classes and adjusts for classification error according to Bolck, Croon, and Hagenaar’s (BCH) approach (Bakk and Vermunt, 2016; Dziak et al., 2016). All model estimates were also adjusted for the non-independent repeated measures data.
Missing data on stigma indicators was handled through full information maximum likelihood and all person records providing data on at least one stigma indicator were used in latent class identification. For LCA with covariates and outcomes, complete case analysis was employed and records missing health outcome or covariate data were excluded from regression models. This resulted in fewer than 3% of person records deleted.
RESULTS
Across five occasions, 435 participants (n) provided 2,003 person records (i) comprising a 92.1% global participation rate with 90.3% of participants providing data on four or more occasions. Records with no stigma data were excluded (i=8), reducing person records to i=1,995. Across person records, 24.8% had a high school education or less, 22.4% reported unemployment, 11.7% engaged in sex exchange, 49.3% had unmet basic needs (i.e., basic needs>1), 33.7% experienced food insecurity, 10.1% experienced unstable housing, and 5.5% reported prior incarceration. Prevalences of sociostructural burdens were generally stable across follow-ups, excluding prevalence of unemployment which decreased.
Stigma
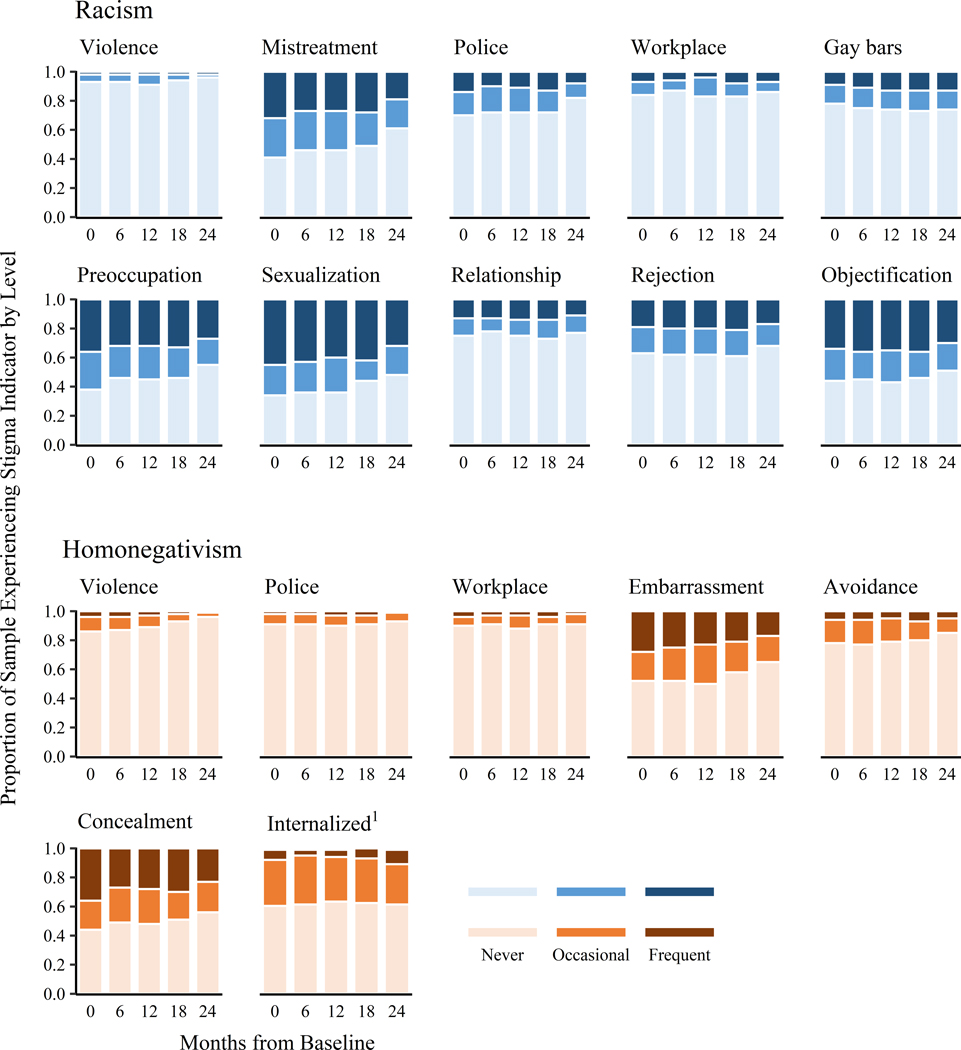
Non-violent, subtle stigma experiences in close interpersonal relationships were more common than overt, enacted discrimination. For example, all forms of sexual racism and anticipated homonegative stigma were generally more common than racist and homonegative experiences of violence, workplace discrimination, and police harassment. Frequency within types of stigma maintained relative sample-level stability across time. Proportions of person records reporting stigma items are summarized in Figure 1.
Fig. 1.
Proportion of Racism and Homonegativism Three-level Indicators across Occasions. Summary based on observed frequencies. 1Internalized homonegativism levels are low, mixed, and high.
Latent Classes Indicated by Stigma Experiences
Model Selection
Latent class models with one to eight classes were well identified (Table 1). Because most information criteria continued to decrease as classes were added and improvements to model fit diminished after six classes, models with two to six classes were considered for conceptual interpretability and stability. In the 5-class model, all classes from previous models (two to four classes) replicated and demonstrated structural stability (i.e., item response probabilities). In the 6-class model, there were two classes considered conceptually similar, each with elevated probabilities of experiencing all types of racism and homonegativism. Because these two classes were conceptually and statistically similar, the more parsimonious, 5-class model was preferred. Therefore, drawing on information criteria, model interpretability, and model stability over time, the 5-class model was selected as optimal for interpretation and further analysis following recommendations (Heron et al., 2015; Vermunt, 2010b); this model was selected as the optimal before introducing covariates. Tests of measurement invariance across known groups (age, race/ethnicity, HIV status) provided no evidence of differing latent class structure and fit criteria within groups suggested the five-class model as optimal. Sensitivity analyses comparing latent class structure in each follow-up occasion revealed no meaningful changes. Thus, the 5-class model with measurement constrained across time and groups was considered appropriate for additional analyses.
Table 1.
Longitudinal Latent Class Model Fit and Information Criteria for 1 to 8 Classes
| No. of Classes | LL | AIC | BIC | a-BIC | a-BICDifference | Entropy |
|---|---|---|---|---|---|---|
| 1 | −24964.506 | 49997.01 | 50187.35 | 50079.33 | − | 1.00 |
| 2 | −22498.37 | 45134.74 | 45521.03 | 45301.82 | −4777.52 | 0.86 |
| 3 | −21900.71 | 44009.42 | 44591.65 | 44261.24 | −1040.58 | 0.82 |
| 4 | −21643.52 | 43565.03 | 44343.21 | 43901.60 | −359.64 | 0.80 |
| 5 | −21465.11 | 43278.22 | 44252.34 | 43699.53 | −202.06 | 0.77 |
| 6 | −21314.91 | 43047.82 | 44217.89 | 43553.88 | −145.65 | 0.79 |
| 7 | −21207.74 | 42903.48 | 44269.49 | 43494.28 | −59.60 | 0.80 |
| 8 | −21110.69 | 42779.38 | 44341.33 | 43454.94 | −39.35 | 0.80 |
Note. LL=log-likelihood; AIC=Akaike information criterion; BIC=Bayesian information criterion; a-BIC=adjusted BIC. n=435; i=1,995. Bold indicates the model selected for further analyses.
Latent Class Identification
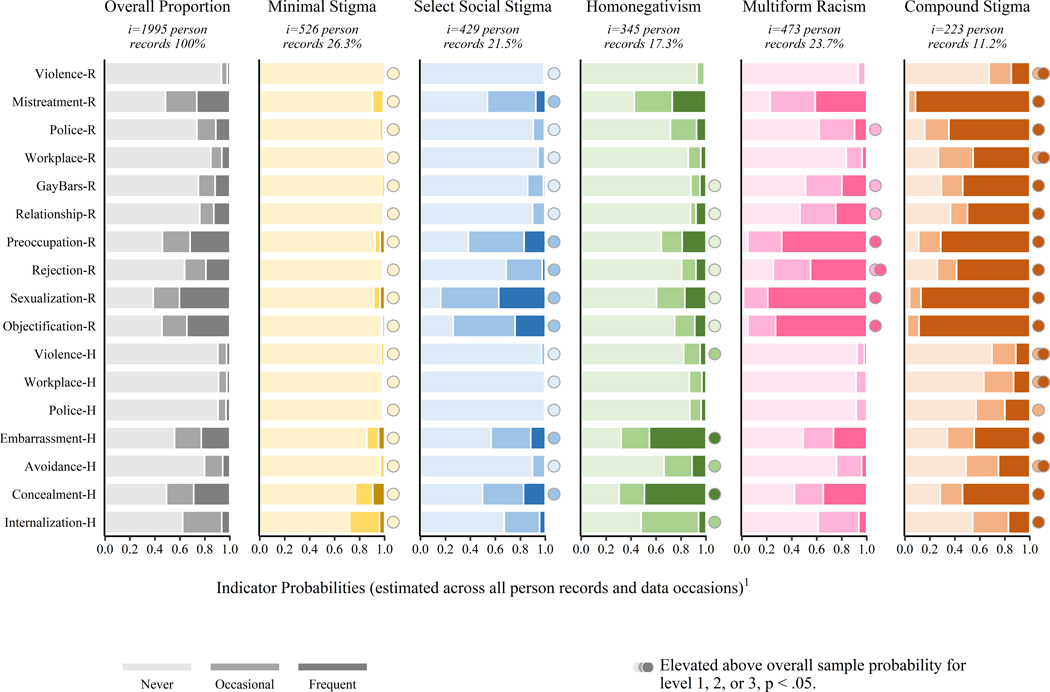
Latent class incident prevalence estimates and item-response probabilities are visualized in Figure 2. To interpret this figure, consider an example: 11.2% of participant records (i=223) were estimated to belong to the Compound Stigma class. For these Compound Stigma class incidents, represented by the top bar in the far right side of the figure, the probabilities of reporting never, occasionally (1–2 times), and frequently (multiple times) experiencing violent racism were 0.674, 0.178, and 0.148. Class prevalence sizes demonstrated rank-order stability across follow-up occasions (Figure 3).
Fig. 2.
Longitudinal Latent Class Item-Response Probabilities and Class Incident Prevalences. n=435; i =1,995. R=racism, H=homonegativism. The first column, Overall Proportion, shows the marginal probabilities for all three levels of racism and homonegativism indicators across all person records at all occasions. Values represent the grand mean proportions of all participant records at each response level given the stigma indicator. 1Columns for each class represent estimated probabilities for each indicator based on all available data from all persons and all occasions and incident prevalence may include multiple records per person.
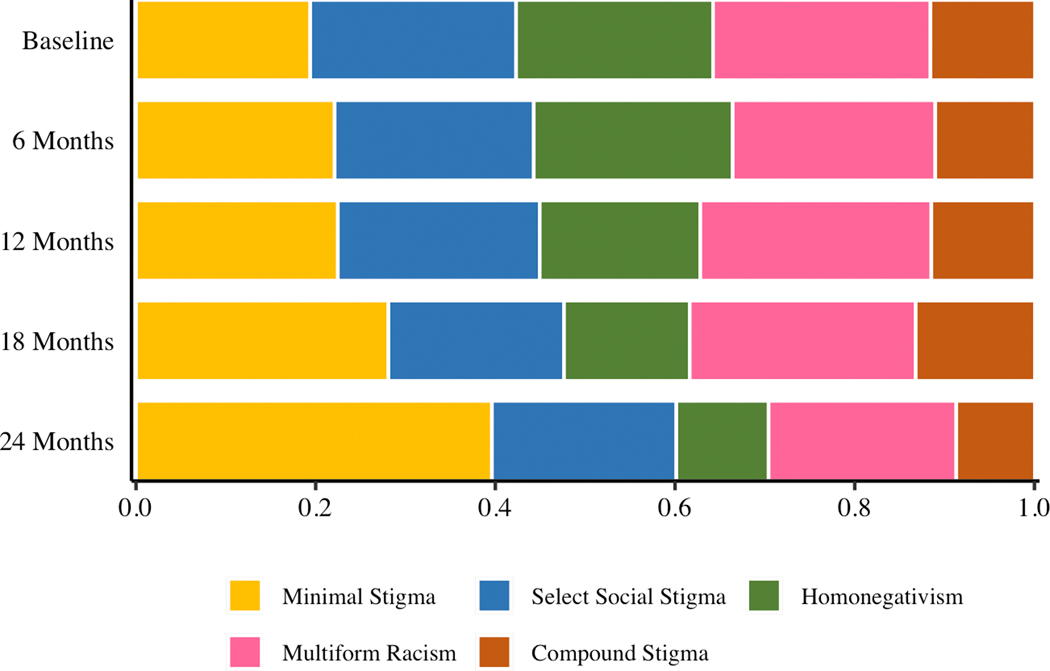
Fig. 3.
Baseline and Follow-Up Class Prevalences. Prevalences are measurement-error weighted based on the BCH approach in Mplus v8.4; i=1,995 person records.
As illustrated in Figure 2, the first class was named the Minimal Stigma class (26.3% of person records), and incidents of this class were characterized by elevated probabilities of never experiencing all types of stigma. Indeed, for Minimal Stigma class incidents, probabilities of experiencing many types of stigma, especially frequently, were very close to zero.
Select Social Stigma class incidents (21.5%) were unique from other classes in that stigma indicators with elevated probabilities were elevated only at the occasional level. On occasions when participants belonged to this class, they were likely to experience occasional racism and homonegativism on a select few stigma indicators related to close interpersonal relationships. As shown in Figure 2, Select Social Stigma class incidents had elevated probabilities of experiencing occasional (but not frequent) racist mistreatment, all four types of sexual racism, homonegative family embarrassment, and concealment. This class was also distinguished by what participants were unlikely to experience. Probabilities were elevated for never experiencing all other types of racist and homonegative stigma except homonegative internalized stigma, which was average. On occasions when participants belonged to this class, their experiences of stigma centered on sexual relationships, embarrassment from family, and their own concealment.
Homonegativism class incidents (17.3%) were characterized by elevated probabilities of some but not all types of homonegative stigma. On occasions when participants belonged to this class, they were likely to experience elevated felt homonegative stigma in close relationships (family embarrassment, avoidance of family and friends, concealment), presumably in response to actual or anticipated homonegative rejection. Further, class incidents had elevated probability of experiencing homonegative violence and mixed levels of internalized homonegativism. Although Homonegativism class incidents were marked by elevated probabilities of some homonegative stigma, the class was also distinguished by high probabilities of never experiencing racist stigma in gay bars, in relationship seeking, or objectification and rejection sexual stigma. Together, experiences of homonegativism in this group were diverse in type (violence, interpersonal, internalized) and heavily centered on close relationships (embarrassment and avoidance linked to family and friends) whereas experiences of racism in LGBT spaces, relationships, and sex were less common than average.
Multiform Racism class incidents (23.7%) were characterized by elevated probabilities of experiencing racism across many different contexts, perpetrators, and levels: police harassment, general racist mistreatment, discomfort in gay bars, difficulty with romantic relationships, and all indicators of sexual racism. On occasions when participants belonged to this class, they were likely to experience racism in many forms and pervasively across many settings. Probabilities of all homonegativism indicators were comparable to the overall averages.
Compound Stigma class incidents (11.2%) were characterized by above average probabilities of frequent racism and homonegativism on every indicator. Figure 2 illustrates the nearly ubiquitous likelihood of experiencing many types of stigma for this class, much more than in the overall sample and most other classes. This sole class exhibited elevated and frequent racist and homonegative violence, police harassment, and workplace discrimination, making it the only class with elevated probabilities of frequent stigma experiences in both close interpersonal relationships and broader contexts including employer and police interactions. Further, the Compound Stigma class was the only class with elevated probability of high internalized homonegativism.
Sociostructural Burdens
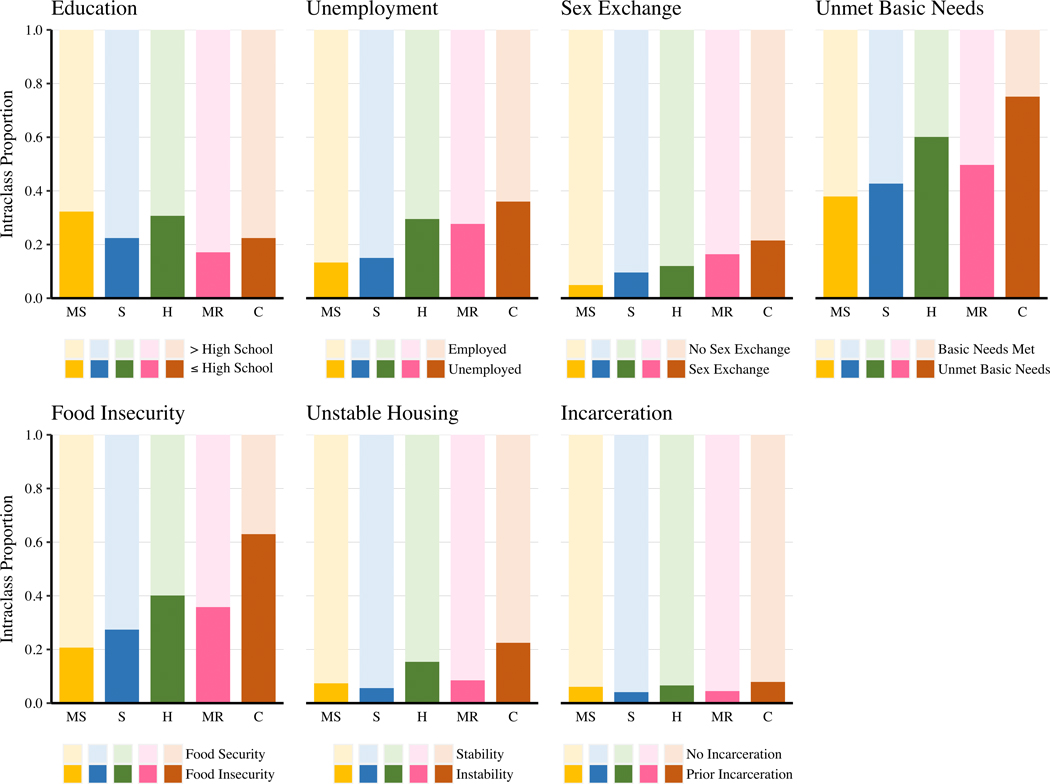
Figure 4 shows prevalences of sociostructural burdens across all occasions within the five latent classes. Generally, the Compound Stigma class incidents had the highest prevalences of sociostructural burdens (36% unemployment, 22% sex exchange, 75% unmet basic needs, 63% food insecurity, 23% unstable housing, 8% formerly incarcerated) with the Homonegativism and Multiform Racism class incidents showing less severe elevation. In contrast, Minimal Stigma class incidents had the lowest prevalence for the majority of sociostructural burdens (13% unemployment, 5% sex exchange, 38% unmet basic needs, 21% food insecurity). As shown in Table 2, sociostructural burdens were generally associated with higher odds of Select Social Stigma, Homonegativism, Multiform Racism, and Compound Stigma class incidents compared to Minimal Stigma incidents. In particular, unemployment (excluding Select Social Stigma), sex exchange, and food insecurity were associated with increased odds of class incidents for all classes compared to the Minimal stigma class. The magnitude of these effects was greatest for the Compound Stigma class. Additionally, odds of a Compound Stigma class incident were uniquely associated with unstable housing. In contrast, having high school education or less was associated with lower odds of Select Social Stigma, Multiform Racism, and Compound Stigma class incidents compared to the Minimal Stigma class.
Fig. 4.
Sociostructural Burdens Proportions Across All Latent Class Incidents and Occasions. MS=minimal stigma; S=select social stigma; H=homonegativism; MR=multiform racism; C=compound stigma. Basic Needs dichotomized for visualization to contrast past 6-month all basic needs met versus basic needs ever unmet. Based on recommended classification-error corrected estimates using the R3STEP procedure in Mplus v8.4.
Table 2.
Associations of Covariates and Sociostructural Burdens with Odds of Latent Classes Incidents Compared to Minimal Stigma Class Incidents
| Minimal Stigma |
Select Social Stigma |
Homonegativism |
Multiform Racism |
Compound Stigma |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Covariates | ||||||||||
| Age | - | - | 0.92 | [0.83, 1.02] | 0.90 | [0.80, 1.02] | 1.08 | [0.97, 1.21] | 1.11 | [0.96, 1.28] |
| Black | - | - | 0.69 | [0.37, 1.30] | 1.32 | [0.66, 2.61] | 2.59 | [1.43, 4.70] | 6.19 | [2.73, 14.03] |
| Afro-Latino | - | - | 0.73 | [0.37, 1.45] | 0.96 | [0.49, 1.90] | 1.76 | [0.96, 3.22] | 3.64 | [1.58, 8.39] |
| Gay | - | - | 2.01 | [1.19, 3.41] | 1.28 | [0.74, 2.21] | 1.28 | [0.77, 2.14] | 0.73 | [0.38, 1.40] |
| People living with HIV | - | - | 0.74 | [0.41, 1.36] | 0.71 | [0.34, 1.50] | 0.70 | [0.37, 1.32] | 0.68 | [0.30, 1.54] |
| Sociostructural Burden | ||||||||||
| ≤High School Education | - | - | 0.53 | [0.33, 0.85] | 0.66 | [0.39, 1.12] | 0.43 | [0.26, 0.69] | 0.43 | [0.22, 0.86] |
| Unemployment | - | - | 1.04 | [0.61, 1.78] | 2.01 | [1.17, 3.47] | 2.13 | [1.37, 3.32] | 2.25 | [1.27, 3.99] |
| Sex Exchange | - | - | 2.06 | [1.01, 4.18] | 2.17 | [1.01, 4.65] | 3.79 | [1.92, 7.46] | 3.61 | [1.59, 8.21] |
| Unmet Basic Needs | - | - | 1.00 | [0.83, 1.20] | 1.07 | [0.88, 1.30] | 1.01 | [0.85, 1.19] | 1.08 | [0.89, 1.30] |
| Food Insecurity | - | - | 1.71 | [1.03, 2.85] | 2.14 | [1.22, 3.76] | 1.98 | [1.23, 3.19] | 4.53 | [2.50, 8.21] |
| Unstable Housing | - | - | 0.81 | [0.35, 1.88] | 1.83 | [0.92, 3.61] | 0.92 | [0.48, 1.75] | 2.05 | [1.10, 3.84] |
| History of Incarceration | - | - | 0.79 | [0.34, 1.82] | 0.69 | [0.32, 1.53] | 0.62 | [0.28, 1.38] | 0.45 | [0.18, 1.17] |
Note. n=435, i=1949. OR=odds ratio; CI=confidence interval. Bold indicates a significant effect at p<.05. All variables are binary, excluding continuous age and unmet basic needs. All estimates are classification-error corrected using the R3STEP approach in Mplus v 8.4.
Associations between covariates (age, race/ethnicity, sexual identity, and HIV status) and class incidents are included in Table 2. Compared to the Minimal Stigma class, odds of Compound Stigma and Multiform Racism class incidents were elevated for person records from Black and Afro-Latino participants relative to Latino participants. Although the sample was 59% Latino, only 26% of Compound Stigma records and 49% of Multiform Racism records were from Latino person records, indicating imbalanced class prevalences by race/ethnicity.
Health Outcomes
Across all 1995 person records, 9.6% person records reported asthma, 6.8% reported STIs, 5.2% reported sleep disorders, and 1.6% reported gastrointestinal disorders. The average number of mental health care needs was 3.32 (SD=5.27) and average self-rated health was 3.14 (SD=1.06). Figure 5 shows the unadjusted proportions of class incidents endorsing each chronic health outcome and unadjusted class means for mental healthcare needs and self-reported health.
Fig. 5.
Unadjusted Chronic Health Proportions, Mental Health Care Needs Mean, and Self-Rated Health Mean Across All Latent Class Incidents and Occasions. Dashed line indicates overall mean across all person records. All estimates are measurement-error weighted based on the BCH approach in Mplus v8.4.
Table 3 shows unadjusted and adjusted associations of class incidents with odds of chronic conditions, mental health care needs, and self-rated health. Most associations were fairly robust to the adjustment for covariates and sociostructural burdens. Generally, Compound Stigma class incidents were most consistently and severely related to elevated negative health outcomes, compared to Minimal Stigma class incidents. For example, compared to Minimal Stigma class incidents, person records belonging to the Compound Stigma class were 2.79 times more likely to report sleep disorders, were 4.24 times more likely to report gastrointestinal disorders (marginally), and had 2.64 more mental health care needs, when accounting for diverse sociostructural burdens. Notably, Select Social Stigma, Homonegativism, Multiform Racism, and Compound stigma class incidents were all associated with greater total mental health care needs compared to Minimal Stigma class incidents even when controlling for covariates and sociostructural burdens. Self-rated health was lower for Multiform Racism class incidents compared to the Minimal Stigma class.
Table 3.
Associations of Class Incidents and Sociostructural Burdens with Health Outcomes
| Asthma1 | STIs1 | Sleep Disorders1 | Gastrointestinal Disorders1 | Mental Health Care Needs2 | Self-Rated Health2 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | β | 95% CI | β | 95% CI | |
| Unadjusted Models | ||||||||||||
| Intercept | 0.09 | [0.06, 0.14] | 0.06 | [0.03, 0.10] | 0.04 | [0.03, 0.07] | 0.01 | [0.00, 0.02] | 1.63 | [1.16, 2.10] | 3.27 | [3.13, 3.42] |
| Classes | ||||||||||||
| Minimal Stigma | ||||||||||||
| Select Social Stigma | 0.52 | [0.23, 1.22] | 1.78 | [0.91, 3.47] | 0.83 | [0.34, 2.05] | 0.98 | [0.11, 8.52] | 1.73 | [0.82, 2.64] | −0.12 | [−0.33, 0.10] |
| Homonegativism | 2.02 | [1.20, 3.40] | 0.82 | [0.32, 2.09] | 1.05 | [0.46, 2.38] | 2.62 | [0.42, 16.44] | 2.09 | [1.20, 2.98] | −0.28 | [−0.52, −0.05] |
| Multiform Racism | 1.60 | [0.91, 2.85] | 1.47 | [0.75, 2.90] | 1.01 | [0.50, 2.04] | 4.79 | [1.16, 19.85] | 2.52 | [1.49, 3.55] | −0.23 | [−0.43, −0.04] |
| Compound Stigma | 0.67 | [0.30, 1.48] | 1.34 | [0.56, 3.17] | 3.53 | [1.70, 7.35] | 9.82 | [1.99, 48.47] | 3.18 | [1.81, 4.55] | −0.06 | [−0.34, 0.22] |
| Adjusted Models 3 | ||||||||||||
| Intercept | 0.09 | [0.05, 0.16] | 0.09 | [0.04, 0.18] | 0.02 | [0.01, 0.06] | 0.00 | [0.00, 0.02] | 1.72 | [0.72, 2.72] | 3.24 | [3.03, 3.45] |
| Classes | ||||||||||||
| Minimal Stigma | ||||||||||||
| Select Social Stigma | 0.78 | [0.39, 1.54] | 1.69 | [0.82, 3.47] | 0.96 | [0.40, 2.30] | 0.94 | [0.20, 4.48] | 1.51 | [0.64, 2.38] | −0.05 | [−0.26, 0.16] |
| Homonegativism | 1.61 | [0.88, 2.95] | 0.96 | [0.39, 2.39] | 0.98 | [0.43, 2.23] | 1.57 | [0.29, 8.36] | 1.41 | [0.51, 2.32] | -0.22 | [−0.44, 0.01] |
| Multiform Racism | 1.19 | [0.62, 2.27] | 1.59 | [0.80, 3.16] | 1.15 | [0.56, 2.33] | 3.32 | [0.90, 12.27] | 2.41 | [1.37, 3.46] | −0.26 | [−0.46, −0.06] |
| Compound Stigma | 0.51 | [0.23, 1.13] | 1.30 | [0.54, 3.15] | 2.79 | [1.26, 6.18] | 4.24 | [0.93, 19.41] | 2.64 | [1.27, 4.01] | −0.07 | [−0.35, 0.21] |
| Sociostructural Burdens | ||||||||||||
| ≤High School Education | 0.96 | [0.49, 1.47] | 0.77 | [0.39, 1.19] | 1.66 | [0.87, 2.51] | 0.23 | [0.07, 0.76] | 0.02 | [−0.69, 0.74] | −0.03 | [−0.18, 0.13] |
| Unemployment | 1.07 | [0.63, 1.50] | 0.90 | [0.48, 1.35] | 1.33 | [0.79, 1.86] | 0.91 | [0.47, 1.77] | 0.76 | [−0.01, 1.54] | 0.03 | [−0.10, 0.16] |
| Sex Exchange | 1.08 | [0.57, 1.61] | 1.44 | [0.72, 2.23] | 1.19 | [0.64, 1.76] | 1.93 | [0.79, 4.70] | 0.54 | [−0.44, 1.53] | -0.15 | [−0.32, 0.03] |
| Unmet Basic Needs | 1.11 | [0.94, 1.24] | 0.91 | [0.73, 1.05] | 1.29 | [1.07, 1.45] | 1.11 | [0.79, 1.54] | 0.51 | [0.23, 0.79] | -0.05 | [−0.10, 0.00] |
| Food Insecurity | 1.01 | [0.61, 1.39] | 0.89 | [0.53, 1.24] | 0.81 | [0.45, 1.18] | 2.58 | [1.04, 6.45] | 0.86 | [0.20, 1.52] | −0.24 | [−0.39, −0.09] |
| Unstable Housing | 1.42 | [0.85, 1.97] | 1.27 | [0.55, 2.17] | 2.13 | [1.10, 3.25] | 1.02 | [0.51, 2.04] | 0.56 | [−0.35, 1.46] | −0.05 | [−0.24, 0.15] |
| History of Incarceration | 1.00 | [0.47, 1.61] | 1.66 | [0.75, 2.78] | 1.40 | [0.54, 2.57] | 2.99 | [1.13, 7.88] | −0.80 | [−1.96, 0.36] | 0.04 | [−0.29, 0.37] |
Note. OR=odds ratio. CI=confidence interval. Bold indicates significant at p<.05 and italics at p<.10. All independent variables are binary, excluding continuous unmet basic needs.
Unadjusted i=1995, adjusted i=1949.
Unadjsuted i=1985, adjusted i=1943.
Models are adjusted for age, race/ethnicity, sexual identity, and HIV status. All estimates are measurement-error weighted based on the BCH approach in Mplus v8.4.
DISCUSSION
Adopting a person-centered methodological approach (Collins and Lanza, 2010) for modeling stigma, this study is grounded in an intersectional framework reflecting pervasive, myriad forms of racism and homonegativism experienced in diverse patterns associated with mental and physical health. Consideration of sociostructural burdens together with classification of racist and homonegative experiences quantified how intersectional stigma experiences converge with individuals’ experiences of social, economic, and structural inequities to sustain health disparities (Bauer, 2014). Study results exemplify the multilevel, multidimensional patterns of racism and homonegativism driving health disparities and within-group heterogeneity in mental health care needs and chronic physical health (sleep disorders, gastrointestinal disorders) among Black and Latino sexual minority young men. Five constellations of stigma experiences were identified with four classes exhibiting elevated frequency of some stigma experiences in diverse patterns and greater sociostructural burden, relative to the Minimal Stigma class. It was clear that incidents of the Compound Stigma class—characterized by the most severe, frequent, and diverse racist and homonegative experiences—were accompanied by the most extreme sociostructural burdens and greatest adverse health outcomes.
This study makes three primary contributions to understanding health and stigma among Black and Latino sexual minority young men. First, the five latent classes demonstrate how quantitative analysis of health data can be situated within an intersectional framework and represent complex lived experiences of Black and Latino sexual minority men that span multiple co-occurring identity statuses interlocked with systems of power and oppression. Stigma experiences were not uniformly experienced by Black and Latino sexual minority men in this sample, and identifying distinct stigma subgroups characterized by unique patterns of stigma experiences allowed further exploration of co-occurring sociostructural burden and downstream health consequences. Second, results revealed how different constellations of stigma experiences converge with sociostructural factors to create an inordinate, compounded burden among young men experiencing both the most ubiquitous, frequent discrimination and sociostructural hardship. These results reinforce evidence that attempts to disrupt effects of stigma must consider not only interpersonal stigma but pervasive, systemic inequities in economic and material needs. Third, by examining differences in health outcomes among classes, we identified constellations of stigma, together with sociostructural burdens, that are most consistently and strongly related to negative physical health outcomes and mental health care needs. Some health consequences (i.e., mental health care needs) were variably exacerbated across all latent classes with any elevated odds of stigma, demonstrating a nearly universal negative impact of stigma. However, on occasions when young men belonged to Compound Stigma class and experienced diverse, frequent, and severe intersecting stigma, they uniquely exhibited elevated odds of sleep disorders and gastrointestinal disorders.
Using Latent Classes to Advance Quantitative Intersectionality Research
We uncovered five classes characterized by distinct configurations of racist and homonegative stigma experiences. This strategy employed an intracategorical approach (McCall, 2005) to intersectional research by focusing in depth on stigma experiences that are salient to the entire sample. In so doing, we captured the intersection of their identities and stigma experiences rather than comparing to reference peer groups who may not occupy the same social and cultural contexts. The latent classes identified illustrate how the intersection of racism and homonegativism differs within a single, geographically homogenous sample, and the importance of accounting for racism and homonegativism together rather than as separate, additive experiences.
Results of the current study build on prior LCA of intersectional stigma among sexual minority people of color (Earnshaw et al., 2018; Shramko et al., 2018) in three majors ways. First, classes demonstrated the utility of an intracategorical (McCall, 2005), within-population approach for identifying unique configurations indicated by many forms of racism and homonegativism rather than single measures for each dimension. Second, the current LCA situated subgroups in sociostructural contexts wherein both configurations of stigma experiences and convergence with sociosoctructural burdens were meaningful for understanding health. Third, much of prior research is descriptive in nature and identifies classes without investigating covariates and associations with health. The modeling approach and results of this study are guided by an intersectional framework and integrate both person-centered and variable-centered methods not only to identify subgroups based on multidimensional experiences of stigma but also to investigate how mental and physical health differed among these groups. As a result of these innovations, we identified five unique classes with nuanced, multidimensional configurations of stigma, investigated differences across classes in individual and sociostructural factors, and identified subgroups with elevated odds or levels of adverse health outcomes while accounting for covariates.
The Minimal Stigma class represents young men unlikely to report frequent experiences of racism or homonegativism, however, this class is not a no stigma group. The numerous stigma indicators measured were multidimensional but not exhaustive; additional stigma measures (e.g., healthcare discrimination, microaggressions) could further diversify subgroups detected. The remaining four classes were characterized by unique constellations of racism and homonegativism. For the Select Social Stigma class, stigma experiences were concentrated in occasional (1–2 times) experiences of stigma in a limited number of social relationships (e.g., sexual partners, family and friends). This class shows that for Black and Latino sexual minority young men, stigma experiences may be concentrated to specific contexts and may occur rarely, highlighting the benefit of considering repeated measures of stigma with shorter recall periods rather than lifetime or past-year recollection of very broad measures of stigma. Even in the Select Social Stigma class where elevated probability of stigma was limited to a select few stigma experiences, convergence with greater sociostructural burden (sex exchange, food insecurity) relative to the Minimal Stigma class was apparent and need for mental health care was elevated.
Across all person records, half belonged to the Homonegativism, Multiform Racism, and Compound Stigma classes. The Homonegativism class was characterized by frequent and occasional homonegativism in close personal relationships (family, friends) and internalized homonegativism. For this group, stigma was limited in context and perpetrators; the intimate nature of stigma in close relationships can be especially damaging for health during the transition to adulthood (McConnell et al., 2016). Nearly one in four person records belonged to the Multiform Racism class, a subgroup characterized by average levels of homonegativism and elevated racism across diverse contexts, perpetrators, and severity. Describing latent classes necessitates parsimonious naming that can oversimplify class complexity. Though these two classes were given names highlighting the prominent dimensions of stigma in these subgroups, both classes account for experiences of racism and homonegativism and reflect unique ways that different forms of racism and homonegativism co-occurred together for incidents of these classes.
Associations of Homonegativism and Multiform Racism classes with lower self-reported health indicates need to explore additional health outcomes not explicitly captured in this study. Some sociostructural burdens and health outcomes differed between the Homonegativism and Multiform racism classes in subtle ways. For example, the Homonegativism class, in unadjusted models, was the only class associated with higher odds of asthma and had the greatest level of unstable housing (which was marginally associated with odds of asthma). It is possible that convergence of belonging to the homonegativism class and experiencing unstable housing creates a social and physical environment that increases the risk of asthma, and this association warrants further investigation.
The Compound Stigma class uniquely experienced both racism and homonegativism frequently, across contexts, and at the hands of many perpetrators. In addition to diverse experiences of stigma, this subgroup was uniquely characterized by intersecting experiences of violence. Reducing the diverse array of stigma items into a limited number of scales or factors could have prevented the identification of this class for whom frequent, diverse, and severe experiences of stigma were elevated. Of note, compared to Latino participants, Black and Afro- Latino participants were more likely to belong to the Compound Stigma class. This racial/ethnic difference in class membership highlights the way in which intersectional stigma experiences among sexual minority men of color are experienced in unique ways, likely predicated by the manner in which individuals are racialized and stigmatized.
In this sample, sociostructural burdens converged with complex patterns of stigma to harm health. Indeed, when participants belonged to subgroups experiencing the greatest stigma burden, they were also laden with unemployment, unmet financial needs, food insecurity, and unstable housing. Although some sociostructural burdens (sex exchange, food insecurity) increased the odds of all other class incidents compared to the Minimal Stigma class, it was the Compound Stigma class, followed by Homonegativism and Multiform Racism classes, that emerged as the most severely impacted by sociostructural burdens. For the Compound Stigma class, the proportion of incidents experiencing sociostructural burden were frequently higher than for any other class: unemployment (65%), unmet basic needs (75%), food insecurity (63%), and unstable housing (23%). More investment in structural interventions in tandem with individual interventions are necessary to shift policy and achieve health equity for Black and Latino sexual minority men, especially those experiencing Compound Stigma and severe sociostructural burdens.
Sexual minorities tend to seek mental health services more often than their heterosexual peers (Cochran et al., 2017). Similarly, Black and Latino sexual minority young men experiencing four different constellations of stigma in this sample reported greater mental health care needs on average than those experiencing low or no stigma. This is consistent with typical approaches to studying stigma as a fundamental cause of health disparities (Hatzenbuehler et al., 2013). Young men experiencing particular complex constellations of diverse stigma types (e.g., Multiform Racism, Compound Stigma) were most different from the Minimal Stigma class in terms of mental health care needs. Incidents of the Compound Stigma class alone were associated with chronic sleep and gastrointestinal disorders. This subgroup is burdened by extensive, frequent, and severe experiences of stigma and inordinate sociostructural burdens, and was the only subgroup associated with differences in chronic physical health outcomes. Results suggest the need for mental health care intervention is far reaching among Black and Latino sexual minority men experiencing stigma as evidenced by elevated levels of mental health care needs in all classes compared to the Minimal Stigma class. This finding extends existing literature showing sexual orientation disparities in mental healthcare needs (Cochran et al., 2017) and shows stigma drives mental healthcare needs not only between sexual minorities and heterosexual but also among Black and Latino sexual minority men specifically. Few of handful of evidence-based interventions targeting mental health by addressing stigma take an intersectional approach (Layland et al., 2020a), and further development of interventions are needed to address the confluence of intersectional stigma and sociostructural burdens.
This study was intentionally grounded in the experiences of Black and Latino sexual minorities without comparison to white sexual minorities or Black and Latino heterosexuals. Between group comparisons often substitute identity statuses for underlying mechanisms of stigma, systemic oppression, and cultural differences (Ford and Airhihenbuwa, 2010; Volpe et al., 2019). By focusing on Black and Latino sexual minority young men, stigma measures captured the breadth and depth of stigma targeting race/ethnicity and sexual orientation. LCA provided a way to quantitatively model intersecting stigma experiences holistically by centering the individual, thus avoiding inadvertent compartmentalization of Black and Latino sexual minority men to one-part Black or Latino and one-part sexual minority. Multiple data records from participants across data occasions with high retention (>88%) across data occasions provided a rich data set for modeling experiences during the transition to adulthood, a period of elevated mental health risk in sexual minorities (Layland et al., 2020b).
Strengths and Limitations
A major strength is the strong match between study design and guiding meta-theories of minority stress and intersectionality. The effects of racism are often rendered invisible by focusing on other theories (e.g., minority stress), shifting the focus away from racism as a fundamental cause of health inequity (Volpe et al., 2019). The current study incorporates racism and homonegativism together into latent subgroups that capture both and then situates the subgroups in the context of structural risk factors. These subgroups embody a participant’s measured experiences of racism and homonegativism holistically to adopt an intersectional approach to understanding drivers of health among Black and Latino sexual minority men. Further, indicators of racism in this study were framed in contemporary race relations (Ford and Airhihenbuwa, 2010) including racism perpetuated by romantic and sexual partners in person, online, or through dating and sexual networking apps. Likewise, indicators of police harassment reflect the ongoing public discourse around police brutality and murder targeting Black Americans.
Results are limited to Black and Latino sexual minority men in Los Angeles and generalizability to other regions and ethnic groups may be limited. The classes identified here were complex and distinct but were limited by the stigma indicators included. Stigma indicators were assessed by frequency and, although important, frequency is not equivalent to stress severity. Because baseline assessment measured lifetime chronic illness diagnoses, it may be that some baseline diagnoses occurred before reported stigma experiences in adulthood. Sensitivity analyses demonstrated no meaningful changes in magnitude, direction, or significance of findings when including baseline measures. Finally, strengths-based approaches to intersectionality could be useful for identifying not only subgroups experiencing the greatest health burdens but also resilience and resistance to oppression.
Conclusions
Ultimately, this study demonstrates how sociostructural burdens interlock with intersecting experiences of stigma to together erode the health of Black and Latino sexual minority young men during the transition to adulthood. On occasions when young men belonged to the Compound Stigma class—characterized by diverse racist and homonegative stigma—sociostructural burden (unemployment, food insecurity, unmet basic needs, unstable housing) was most severe, odds of sleep and gastrointestinal disorders were elevated, and mental health care needs were highest. In addition to the Compound Stigma class, incidents of Select Social Stigma, Homonegativism, and Multiform Racism classes were also associated with greater mental healthcare needs. Interventions and research designed to support this population should reflect this understanding of within-group differences in stigma and health.
Highlights.
Stigma experiences among Black and Latino sexual minority men are multidimensional and complex.
Latent class analysis uncovered subgroups experiencing unique patterns of intersecting stigma.
Mental and physical health differed by stigma subgroup for Black and Latino sexual minority men.
The most severe intersecting stigma pattern co-occurred with inordinate sociostructural burden.
Acknowledgements
The authors acknowledge the contributions of the many staff members who contributed to collection, management, analysis, and review of this data: James Aboagye, Alex Aldana, Stacy Alford, Ali Johnson, Nicole Pereira, Aracely Rodriguez, and Su Wu. The authors would also like to acknowledge the insightful and practical commentary of the members of the Community Advisory Board - Daniel Nguyen: Asian Pacific AIDS Intervention Team; Ivan Daniels III: Los Angeles Black Pride; Steven Campa: Los Angeles LGBT Center; Davon Crenshaw: AIDS Project Los Angeles; Andre Molette: Essential Access Health; Miguel Martinez, Joaquin Gutierrez, and Jesse Medina: Division of Adolescent and Young Adult Medicine, Children’s Hospital Los Angeles; Greg Wilson: Reach LA; and The LGBTQ Center Long Beach.
Funding This research was supported by the National Institute on Drug Abuse (U01 DA036926; P50 DA039838; T32 DA017629) and the National Institute on Mental Health (T32 MH020031) of the National Institutes of Health. The views expressed are solely those of the authors and do not necessarily reflect the views of the National Institutes of Health. The National Institutes of Health had no involvement in the collection, analysis and interpretation of data, the writing of this article, or the decision to submit for publication.
Footnotes
Declarations of Interest None.
CRediT Author Statement
Eric K. Layland: Conceptualization, Methodology, Formal Analysis, Data Curation, Writing – Original Draft Preparation, Visualization
Jennifer L. Maggs: Conceptualization, Writing – Review and Editing, Supervision
Michele D. Kipke: Investigation, Writing – Review and Editing, Project Administration, Funding Acquisition
Bethany C. Bray: Conceptualization, Methodology, Software, Validation, Writing – Review and Editing, Supervision
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Agénor M, 2020. Future directions for incorporating intersectionality into quantitative population health research. Am. J. Public Health 110, 803–806. 10.2105/AJPH.2020.305610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen E, 2019. Perceived discrimination and health: Paradigms and prospects. Sociol. Compass 13, 1–16. 10.1111/soc4.12720 [DOI] [Google Scholar]
- Bakk Z, Vermunt JK, 2016. Robustness of stepwise latent class modeling with continuous distal outcomes. Struct. Equ. Model. 23, 20–31. 10.1080/10705511.2014.955104 [DOI] [Google Scholar]
- Bauer GR, 2014. Incorporating intersectionality theory into population health research methodology: Challenges and the potential to advance health equity. Soc. Sci. Med. 110, 10–17. 10.1016/j.socscimed.2014.03.022 [DOI] [PubMed] [Google Scholar]
- Blosnich JR, Lee JGL, Bossarte R, Silenzio VMB, 2013. Asthma disparities and within-group differences in a national, probability sample of same-sex partnered adults. Am. J. Public Health 103, 83–87. 10.2105/AJPH.2013.301217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowleg L, 2013. “Once you’ve blended the cake, you can’t take the parts back to the main ingredients”: Black gay and bisexual men’s descriptions and experiences of intersectionality. Sex Roles 68, 754–767. 10.1007/s11199-012-0152-4 [DOI] [Google Scholar]
- Bowleg L, 2012. The problem with the phrase women and minorities: Intersectionality-an important theoretical framework for public health. Am. J. Public Health 102, 1267–73. 10.2105/AJPH.2012.300750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowleg L, 2008. When Black + lesbian + woman ≠ Black lesbian woman: The methodological challenges of qualitative and quantitative intersectionality research. Sex Roles 59, 312–325. 10.1007/s11199-008-9400-z [DOI] [Google Scholar]
- Brooks VR, 1981. Minority stress and lesbian women. Lexington Books, Lexington, MA. [Google Scholar]
- Brunson RK, 2007. “Police don’t like Black people”: African-American young men’s accumulated police experiences. Criminol. Public Policy 6, 71–101. 10.1111/j.1745-9133.2007.00423.x [DOI] [Google Scholar]
- Clark R, Anderson NB, Clark VR, Williams DR, 1999. Racism as a stressor for African Americans. Am. Psychol. 54, 805–816. [DOI] [PubMed] [Google Scholar]
- Cochran SD, Björkenstam C, Mays VM, 2017. Sexual Orientation Differences in Functional Limitations, Disability, and Mental Health Services Use: Results from the 2013– 2014 National Health Interview Survey. J. Consult. Clin. Psychol. 85, 1111–1121. 10.1037/ccp0000243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins LM, Lanza ST, 2010. Latent Class and Latent Transition Analysis: With Applications in the Social, Behavioral, and Health Sciences. Wiley, Hoboken, New Jersey. [Google Scholar]
- Crenshaw K, 1989. Demarginalizing the intersection of race and sex: A Black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. Univ. Chic. Leg. Forum; 139–167. 10.3868/s050-004-015-0003-8 [DOI] [Google Scholar]
- Denton FN, Rostosky SS, Danner F, 2014. Stigma-related stressors, coping self-efficacy, and physical health in lesbian, gay, and bisexual individuals. J. Couns. Psychol. 61, 383–391. 10.1037/a0036707 [DOI] [PubMed] [Google Scholar]
- Diamond LM, 2003. New paradigms for research on heterosexual and sexual-minority development. J. Clin. Child Adolesc. Psychol. 32, 490–498. 10.1207/S15374424JCCP3204 [DOI] [PubMed] [Google Scholar]
- Diaz RM, Ayala G, Bein E, Henne J, Marin BV, 2001. The impact of homophobia, poverty, and racism on mental health of gay and bisexual Latino men: Findings from 3 US cities. Am. J. Public Health 91, 927–932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diggle PJ, Heagerty P, Liang K-Y, Zeger SL, 2002. Analysis of longitudinal aata, 2nd ed. Oxford University Press, Oxford, UK. [Google Scholar]
- Downing JM, Rosenthal E, 2020. Prevalence of Social Determinants of Health Among Sexual Minority Women and Men in 2017. Am. J. Prev. Med. 59, 118–122. 10.1016/j.amepre.2020.01.007 [DOI] [PubMed] [Google Scholar]
- Dyar C, Taggart TC, Rodriguez-Seijas C, Thompson RG, Elliott JC, Hasin DS, Eaton NR, 2019. Physical Health Disparities Across Dimensions of Sexual Orientation, Race/Ethnicity, and Sex: Evidence for Increased Risk Among Bisexual Adults. Arch. Sex. Behav. 48, 225–242. 10.1007/s10508-018-1169-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dziak JJ, Bray BC, Zhang J, Zhang M, Lanza ST, 2016. Comparing the performance of improved classify-analyze approaches for distal outcomes in latent profile analysis. Methodology 12, 107–116. 10.1027/1614-2241/a000114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Rosenthal L, Gilstad-Hayden K, Carroll-Scott A, Kershaw TS, Santilli A, Ickovics JR, 2018. Intersectional experiences of discrimination in a low-resource urban community: An exploratory latent class analysis. J. Community Appl. Soc. Psychol. 28, 80–93. 10.1002/casp.2342 [DOI] [Google Scholar]
- Ford CL, Airhihenbuwa CO, 2010. Critical race theory, race equity, and public health: Toward antiracism praxis. Am. J. Public Health 100, 693–698. 10.2105/AJPH.2009.171058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galupo MP, Resnick CA, 2016. Experiences of LGBT microaggressions in the workplace: Implications for policy, in: Kollen T (Ed.), Sexual Orientation and Transgender Issues in Organizations. Springer, New York, pp. 271–287. [Google Scholar]
- Gates GJ, 2014. Food Insecurity and SNAP ( Food Stamps ) Participation in LGBT Communities 12. [Google Scholar]
- Hammond WP, 2010. Psychosocial correlates of medical mistrust among African American men. Am. J. Community Psychol. 45, 87–106. 10.1007/s10464-009-9280-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Phelan JC, Link BG, 2013. Stigma as a fundamental cause of population health inequalities. Am. J. Public Health 103, 813–821. 10.2105/AJPH.2012.301069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herek GM, 2004. Beyond “homophobia”: Thinking about sexual prejudice and stigma in the twenty-first century. Sexuality Res Soc Policy, 1, 6–24. 10.1525/srsp.2004.1.2.6 [DOI] [Google Scholar]
- Herek GM, 2009. Hate crimes and stigma-related experiences among sexual minority adults in the United States: Prevalence estimates from a national probability sample. J. Interpers. Violence 24, 54–74. 10.1177/0886260508316477 [DOI] [PubMed] [Google Scholar]
- Herek GM, Gillis JR, Cogan JC, 2009. Internalized stigma among sexual minority adults: Insights from a social psychological perspective. J. Couns. Psychol. 56, 32–43. 10.1037/a0014672 [DOI] [Google Scholar]
- Heron J, Croudace TJ, Barker ED, Tilling K, 2015. A comparison of approaches for assessing covariate effects in latent class analysis. Longit. Life Course Stud. 6, 420–434. 10.14301/llcs.v6i4.322 [DOI] [Google Scholar]
- Hidalgo MA, Layland EK, Kubicek K, Kipke MD, 2020. Sexual racism, psychological symptoms, and mindfulness among ethnically/racially-diverse young men who have sex with men: A moderation analysis. Mindfulness (N. Y). 11, 452–461. 10.1007/s12671-019-01278-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeffries WL, Johnson OD, 2015. Homonegative attitudes and risk behaviors for HIV and other sexually transmitted infections among sexually active men in the United States. Am. J. Public Health 105, 2466–2472. 10.2105/AJPH.2015.302780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CP, 2000. Levels of racism: A theoretic framework and gardener’s tale. Am. J. Public Health 90, 1212–1215. 10.7748/phc.1.4.26.s20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kipke MD, Kubicek K, Akinyemi IC, Hawkins W, Belzer M, Bhandari S, Bray B, 2020. The Healthy Young Men’s Cohort: Health, Stress, and Risk Profile of Black and Latino Young Men Who Have Sex with Men (YMSM). J. Urban Heal. 97, 653–667. 10.1007/s11524-019-00398-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kipke MD, Kubicek K, Wong CF, Robinson YA, Akinyemi IC, Beyer WJ, Hawkins W, Rice CE, Layland E, Bray BC, Belzer M, 2019. A focus on the HIV care continuum through the Healthy Young Men’s Cohort Study: Protocol for a mixed-methods study. JMIR Res. Protoc. 8, e10738. 10.2196/10738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Layland EK, Carter JA, Perry NS, Cienfuegos-szalay J, Nelson KM, Bonner CP, Rendina HJ, 2020a. A systematic review of stigma in sexual and gender minority health interventions. Transl. Behav. Med. 10, 1200–1210. 10.1093/tbm/ibz200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Layland EK, Exten C, Mallory AB, Williams ND, Fish JN, 2020b. Suicide attempt rates and associations with discrimination are greatest in early adulthood for sexual minority adults across diverse racial and ethnic groups. LGBT Heal. 7, 439–447. 10.1089/lgbt.2020.0142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lick DJ, Durso LE, Johnson KL, 2013. Minority stress and physical health among sexual minorities. Perspect. Psychol. Sci. 8, 521–548. 10.1177/1745691613497965 [DOI] [PubMed] [Google Scholar]
- LoSchiavo C, Krause KD, Singer SN, Halikitis PN, 2020. The confluence of housing instability and psychosocial, mental, and physical health in sexual minority young adults: The P18 Cohort Study. J. Health Care Poor Underserved 31, 1693–1711. 10.1353/hpu.2020.0127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallory C, Hasenbush A, Sears B, 2015. Discrimination and harassment by law enforcement officers in the LGBT community. The Williams Institute. [Google Scholar]
- McCall L, 2005. The complexity of intersectionality. Signs J. Women Cult. Soc. 30, 1771–1800. [Google Scholar]
- McConnell EA, Birkett M, Mustanski B, 2016. Families Matter: Social Support and Mental Health Trajectories Among Lesbian, Gay, Bisexual, and Transgender Youth. J. Adolesc. Heal. 59, 674–680. 10.1016/j.jadohealth.2016.07.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH, 2003. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol. Bull. 129, 674–697. 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH, 1995. Minority stress and mental health in gay men. J. Health Soc. Behav. 36, 38–56. [PubMed] [Google Scholar]
- Muthen L Muthen inda K., B. engt O, 2017. Mplus user’s guide: Statistical analysis with latent variables, 8th ed. Muthen & Muthen, Los Angeles, CA. [Google Scholar]
- Nott KH, Vedhara K, 1995. The measurement and significance of stressful life events in a cohort of homosexual HIV positive men. AIDS Care 7, 55–70. 10.1080/09540129550126966 [DOI] [PubMed] [Google Scholar]
- Pachankis JE, 2007. The psychological implications of concealing a stigma: A cognitive-affective-behavioral model. Psychol. Bull. 133, 328–345. 10.1037/0033-2909.133.2.328 [DOI] [PubMed] [Google Scholar]
- Patterson CJ, Potter EC, 2019. Sexual orientation and sleep difficulties: a review of research. Sleep Heal. 5, 227–235. 10.1016/j.sleh.2019.02.004 [DOI] [PubMed] [Google Scholar]
- Petruzzella A, Feinstein BA, Davila J, Lavner JA, 2019. Moderators of the Association Between Community Connectedness and Internalizing Symptoms Among Gay Men. Arch. Sex. Behav. 48, 1519–1528. 10.1007/s10508-018-1355-8 [DOI] [PubMed] [Google Scholar]
- Phelan JC, Link BG, 2015. Is racism a fundamental cause of inequalities in health? Annu. Rev. Sociol. 41, 311–330. 10.1146/annurev-soc-073014-112305 [DOI] [Google Scholar]
- Plöderl M, Tremblay P, 2015. Mental health of sexual minorities. A systematic review. Int. Rev. Psychiatry 27, 367–385. 10.3109/09540261.2015.1083949 [DOI] [PubMed] [Google Scholar]
- Priest N, Williams DR, 2018. Racial discrimination and racial disparities in health, in: Major B, Dovidio JF, Link BG (Eds.), The Oxford Handbook of Stigma, Discrimination, and Health. Oxford University Press, New York, pp. 1–35. [Google Scholar]
- Puckett JA, Woodward EN, Mereish EH, Pantalone DW, 2015. Parental rejection following sexual orientation disclosure: Impact on internalized homophobia, social support, and mental health. LGBT Heal. 2, 265–269. 10.1089/lgbt.2013.0024 [DOI] [PubMed] [Google Scholar]
- Raifman J, Bor J, Venkataramani A, 2021. Association Between Receipt of Unemployment Insurance and Food Insecurity Among People Who Lost Employment During the COVID-19 Pandemic in the United States. JAMA Netw. Open 4, e2035884. 10.1001/jamanetworkopen.2020.35884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice CE, Fish JN, Russell ST, Lanza ST, 2021. Sexual Minority-related Discrimination across the Life Course: Findings from a National Sample of Adults in the United States. J. Homosex. 68, 252–268. 10.1080/00918369.2019.1648083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross MW, Rosser BRS, 1996. Measurement and correlates of internalized homophobia: A factor analytic study. J. Clin. Psychol. 52, 15–21. [DOI] [PubMed] [Google Scholar]
- Schmitz RM, Robinson BA, Tabler J, Welch B, Rafaqut S, 2020. LGBTQ+ Latino/a young people’s interpretations of stigma and mental health: An intersectional minority stress perspective. Soc Ment Health, 10, 163–179. 10.1177/2156869319847248 [DOI] [Google Scholar]
- Shramko M, Toomey RB, Anhalt K, 2018. Profiles of minority stressors and identity centrality among sexual minority Latinx youth. Am. J. Orthopsychiatry, Bullying and Peer Victimization of Vulnerable, Marginalized, and Oppressed Youth 88, 471–482. 10.1037/ort0000298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turan JM, Elafros MA, Logie CH, Banik S, Turan B, Crockett KB, Pescosolido B, Murray SM, 2019. Challenges and opportunities in examining and addressing intersectional stigma and health. BMC Med. 17, 1–15. 10.1186/s12916-018-1246-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- USDA, 2012. US Adult Food Security Survey Module: Three-Stage design, with screeners [WWW Document]. URL https://www.ers.usda.gov/media/8279/ad2012.pdf (accessed 6.8.20).
- Vermunt JK, 2010a. Longitudinal research using mixture models, in: van Montfort K, Oud J, Satorra A (Eds.), Longitudinal Research with Latent Variables. Springer, Heidelberg, Germany, pp. 119–152. [Google Scholar]
- Vermunt JK, 2010b. Latent class modeling with covariates: Two improved three-step approaches. Polit. Anal. 18, 450–469. 10.1093/pan/mpq025 [DOI] [Google Scholar]
- Volpe VV, Dawson DN, Rahal D, Wiley KC, Vesslee S, 2019. Bringing psychological science to bear on racial health disparities: The promise of centering Black health through a critical race framework. Transl. Issues Psychol. Sci. 5, 302–314. 10.1037/tps0000205 [DOI] [Google Scholar]
- Vuolo M, Mortimer JT, Staff J, 2016. The value of educational degrees in turbulent economic times: Evidence from the Youth Development Study. Soc. Sci. Res. 57, 233–252. 10.1016/j.ssresearch.2015.12.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang EA, Green J, 2010. Incarceration as a key variable in racial disparities of asthma prevalence. BMC Public Health 10. 10.1186/1471-2458-10-290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Lawrence JA, Davis BA, 2019. Racism and Health: Evidence and Needed Research. Annu. Rev. Public Health 40, 105–125. 10.1146/annurev-publhealth-040218-043750 [DOI] [PMC free article] [PubMed] [Google Scholar]