Abstract
Background
The assessment of human and diagnostic resources is a prerequisite to improving the management of emergency neurology.
Objective
To provide a landscape on the organization of the Lombardy Region hospitals for emergency neurological care management.
Methods
We designed an anonymized questionnaire including 6 sections with 21 questions on facilities, human and diagnostic resources, and intra- and between-hospital connections. The time needed to fill the questionnaire was estimated not to exceed 6 min.
Results
The questionnaire was returned by 33/41 (80.5%) hospitals, 22 classified as level 1 (spoke), and 11 as level 2 (hub). Five of 33 (15%) did not have a neurology unit. The mean annual rate of neurological consultations accounted for 5–6% of all admissions (range 2–8%) and did not differ between levels 1 and 2 hospitals. Neurologists were 24-h available in 21/33 (64%) hospitals, 12-h and on call at night in 6 (18%), less than 12 h without nocturnal availability in 5 (15%), and neither present nor available in 1 (3%). Brain CT and CSF examinations were 24-h universally available, whereas EEG and neurosonology were not in most hospitals. Despite angio-CT was 24-h available in more than 75% of the hospitals, only 45% of them had 24-h availability of diffusion/perfusion imaging, and 43% were not available at any time. Only 12% of the hospitals had 24-h availability of neuroradiologists and 6% of interventional neuroradiologists.
Conclusion
Our data, while emphasizing current critical issues, offer clues for identifying priorities and improving the management of emergency and time-dependent neurological diseases.
Keywords: Emergency neurology, Stroke, Healthcare management, Lombardy Region
Introduction
The burden of neurological diseases is steadily increasing worldwide, accounting for 16.5% of global deaths and 11.6% of global disability-adjusted life years (DALYs) [1], a substantial proportion of which is caused by acute illnesses including stroke, encephalitis, traumatic brain, and spinal injury.
National health systems will be facing the medical needs related to the increased life expectancy, with an expected progressively higher number of incident events, likely without a corresponding increase in resources. Therefore, the optimal allocation of available resources is important to assure the sustainability of acute care health settings organizations without decreasing the efficacy of delivered care [2].
In Italy, the health system is universal, and the organization of resources for both acute and chronic care is determined at a regional level [3]. Lombardy is the most densely populated Italian region, with approximately 10 million inhabitants. Its regional health system is articulated in hospitals with different facilities, from first-level point-of-care to hospitals endowed with an emergency service, subdivided in second and third-level structures according to the availability of multispecialty facilities [4]. The Lombardy Region has promoted the institution of a neuroscience network, coordinated by regional authorities and composed of healthcare professionals with different roles in the diagnosis and care of neurological diseases. One major objective is the definition of the diagnostic pathways for acute neurological patients in different hospital settings, with the aim to understand if any differences could influence healthcare efficacy and efficiency. A prerequisite to this is an analytical collection of data regarding the availability and organization of professional, technological, and logistic resources in the different hospitals involved in acute neurological care, as well as their interconnections.
To this aim, the Lombardy section of the Italian Association for Emergency Neurology (ANEU), endorsed by the Italian Society of Neurology and the Italian Society of Hospital Neurosciences, has promoted a data collection to quantify the impact of the neurological activities on those performed in the regional emergency departments and to provide information for the improvement of acute neurological diseases care.
Methods
We designed a questionnaire using the Google Forms application including 6 main sections (Table 1) with 21 questions on type of facilities, human and diagnostic resource availability, intra- and between-hospital collaboration. We referred to 2019 because, in 2020, the regional healthcare organization was transiently changed to face the COVID-19 pandemic. The questionnaire was anonymized, and no sensitive data was included. The time needed to fill the questionnaire was estimated not to exceed 6 min to increase the participation rate. The questionnaire was sent to 41 neurological units on April 2021 with feedback requested within 30 days. All data were included in a dedicated datasheet.
Table 1.
Sections of the questionnaire on facilities, human, and diagnostic resource availability, intra- and between-hospital collaboration. *Level 1 is the emergency department in most large and medium-sized hospitals, with surgeons and anesthesiologists on call 24 h daily, with an intensive care unit and staffed usually with emergency medicine specialists. This level can handle common surgical problems, most car accidents, and almost all illnesses including heart attacks and strokes. Level 2 is the highest level and must have immediately available surgical specialists and subspecialists (vascular surgeons, neurosurgeons, orthopedic surgeons, anesthesiologists, plastic surgeons) in order to handle the most severe and complicated injuries
| *Hospital classification | •Level 1 (spoke) •Level 2 (hub) |
|---|---|
| Hospital with neurology ward and stroke unit |
•Yes •No |
| Availability of neurologist |
•24-h daily •12-h daytime + 12-h on call •On call < 12 h •Not available |
| Laboratory and instrumental diagnostic accessibility |
•No hourly limitations (24-h daily) •Wide daytime availability (6–12 h daily) •Restricted daytime availability (< 6 h) |
|
Availability of •Neuroradiologist •Interventional neuroradiologist •Neurosurgeon |
•No hourly limitations (24-h daily) •Wide daytime availability (6–12 h) •Restricted daytime hourly availability (< 6 h) |
| Interhospital connection |
•No structured connection •Structured connection -Images system -Formal interhospital agreement |
Results
Thirty-three out of 41 (80.5%) hospitals replied to the questionnaire, 22 classified as level 1 (spoke) and 11 as level 2 (hub) hospitals. Five of 33 (15%) did not have a neurology unit. Figures 1 and 2 illustrate the number of accesses per year to the emergency departments and the percentage of neurological consultations according to the type of hospital. Level 2 hospitals showed a higher number of emergency department accesses. Conversely, there was no difference in the percentage of the neurological consultation comparing level 1 and level 2 hospitals, which ranged from 2 to 8% (mean value 5.3%). There was only one outlier level 1 hospital (15.7%) whose higher number of neurological consultations likely depended on the much wider territory which refers to it.
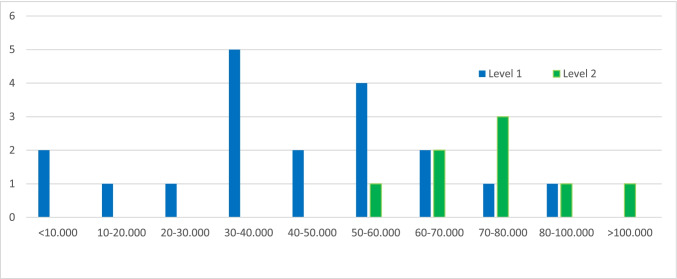
Fig. 1.
Distribution of the number of admissions/year to the emergency departments in level 1 and level 2 hospitals of the Lombardy Region in 2019
Fig. 2.
Percentage of neurological consultations compared to the total number of accesses to the emergency departments in level 1 (mean 5.2%) and level 2 (5.5%) hospitals of the Lombardy Region in 2019 (range 2.2 to 15.7%). Red squares indicate no data available
Availability of the neurologist
In 21 of 33 (64%) hospitals, the neurologist was available 24 h a day; in 6 of 33 (18%), 12 h during the day shift and on call at night; in 5 of 33 (15%), for less than 12 h without nocturnal availability; and in one (3%) hospital, the neurologist was neither present nor available.
Diagnostic accessibility
We quantified the accessibility to diagnostics, i.e., for how many hours a day they were available considering three availability bands: no hourly limitations (24 h), wide daytime availability (6–12 h), and restricted daytime availability (< 6 h). Furthermore, we recorded the functioning and efficiency of the connection networks between levels 1 and 2 hospitals. Figure 3 summarizes the availability of the main neurological and neuroradiological tests: electroencephalography (EEG), cerebrospinal fluid (CSF) examination, neurosonological study of intra- and extracranial vessels, computed tomography (CT) of the brain and cerebral vessels, cerebral and spinal magnetic resonance imaging (MRI), and diffusion/perfusion studies (CT and/or MRI) for reperfusion therapy in the hyperacute phase of stroke.
Fig. 3.
Accessibility/availability of the main examinations of neurological diagnosis and neuroradiology in an emergency setting. EEG, electroencephalography; MRI, magnetic resonance imaging; CT, computed tomography
Between hospitals connections
Figure 4 indicates how many level-1 hospitals are in a network with level-2 hospitals through connections of neuroradiological images and the contextual availability of neuroradiology and neurosurgery both for diagnosis and for any surgical and/or endovascular therapeutic procedures.
Fig. 4.
Interhospital neuroradiology and neurosurgery network in the Lombardy Region
Discussion
The survey allowed at outlining some important aspects of emergency neurology management in the Lombardy Region, reflecting the organization of 80.5% of the regional hospitals and 68.3% of the neurological units. The proportion between levels 1 and 2 hospitals, 22 and 11, respectively, is numerically adequate to provide a specific image for their respective organization [5]. Level 2 hospitals, acting as hub centers, had a numerically higher number of accesses to the emergency departments, but the average percentage of neurological consultations was similar to that recorded in level 1 hospitals. The mean annual rate of neurological consultation in emergency departments accounted for about 5–6% of acute medical admissions, ranging between 2 and 8%, with a peak of about 16%. These values, and the quite wide range of recording, have been previously reported in Italy [6] and in other European and non-European countries [7–9].
In our survey, such as in others, the quite wide range of neurological consultations compared to all the accesses to the emergency departments could be related to different approaches and/or different fast-track neurological plans and/or lack of standardized clinical and diagnostic workup [10, 11]. The evidence of a similar rate of neurological consultations between levels 1 and 2 hospitals suggests that the request is not determined or influenced by the geographical area, hospital size, functional context, and/or ease of access but by an actual diagnostic need, even if we could not assess whether the number of neurological consultations did correspond to number and type of neurological complains at the admission. These regional findings reflect the Italian nationwide features as reported by de Falco and colleagues [12]. One further explanation for the similar average percentage of neurological consultations could be the wide availability of on-call neurologists and first-level diagnostic tools in most of the hospitals in our sample, irrespective of their classification as level 1 or 2.
Indeed, brain CT and CSF examinations appear available in all the participating centers without limitations, whereas EEG and neurosonology are widely available in the daytime range but not for 24 h daily. At least for the EEG, this represents a critical issue for the management of some clinical conditions, such as nonconvulsive epileptic seizures, altered mental status, and coma both in pediatric and adult patients [13, 14], even if in most cases, it would be sufficient to guarantee the availability of EEG within 24 h for an appropriate diagnostic and therapeutic approach. The limited availability of neurosonology in the hyperacute phase of ischemic stroke is currently compensated by the large availability of angio-CT 24 h daily in more than 75% of the hospitals that, together with brain CT scan, can speed the diagnostic workup in time-dependent pathology as stroke. However, if we consider the current therapeutic perspectives for ischemic stroke and the recent indications of widening the therapeutic window to 9 h for intravenous fibrinolysis and 16 or 24 h as a function of advanced imaging of diffusion/perfusion methods for mechanical thrombectomy [15], we found that only 45% of the hospitals were available 24 h a day and 43% of the hospitals were not available any time.
The large availability of neuroimaging sharing is apparently indicative of a good networking capability between levels 1 and 2 hospitals. However, if we transfer this finding to the operational level, the contextual availability of neuroradiologists for 24 h daily in only 12% of the hospitals and for 6–12 h in 45%, along with the availability of interventional neuroradiologists for 24 h daily in 6% of the hospitals and for 6–12 h in 25%, raise important questions on the differences between management priorities and availability of resources for acute stroke patients. While this imbalance indicates an incomplete ability of the healthcare system to face the neurological emergency needs, which by definition must not recognize any time limit to avoid uneven treatments, it also suggests that the distribution and number of the neuroradiology departments and interventional neuroradiologists should be reconsidered based on the territorial needs. This should include larger and better use of technologies such as telemedicine and advanced images system in emergency settings, particularly in time-dependent diseases [16]. Telestroke has been demonstrated to increase access to time-depended care [17]. The current pandemic has been showing that teleneurology applied to many other neurological disorders can increase and improve the access to care; its application in the clinical setting is a step forward for modernizing medical care [18, 19].
A second critical issue is the normative regulation of the hub-and-spoke relationship because a formal agreement with the neuroradiology department was reported to be signed in less than 30% of cases, albeit that percentage is likely underestimated considering the high percentage of active image connection between hospitals and perhaps partially correlated to an ambiguity in the questionnaire that merged the hourly availability with the presence of an agreement, without reserving a specific item for the latter. The area of neurosurgical emergencies appears more homogeneous with a wide availability both at night and during the day. Taken as a whole, this survey offers an exhaustive landscape of emergency neurology management in the Lombardy Region, and outlines some critical points related to hospital networking that identify areas worthy of further studies of interest for the public healthcare policymakers. One limitation of the study is that 85% of the hospitals included in the survey have a neurology department, while hospitals without are underrepresented. We believe that the structure of the questionnaire and its fast compilation could be taken as a template for a similar survey at a nationwide level, to identify issues relevant to improving the acute care of patients with neurological disorders.
In conclusion, our findings confirm the importance of human and technological resources in emergency neurology. One major critical issue appears to be the relative lack of efficient networking among the regional hospitals for the management of acute cerebrovascular diseases, which would require a balanced public investment to guarantee all the citizens access to the treatments following the most recent international guidelines [15].
Acknowledgements
We thank Emiliano Marzi and Maurizio Cicero for their support for data mining and analysis.
On behalf of the Lombardy section of the Italian Association for Emergency Neurology (ANEU)
Vincenzo Belcastro, Elisabetta Domina (Ospedale Maggiore di Lodi, Ospedale di Codogno)
Sandro Beretta, Massimiliano Braga (Ospedale di Vimercate)
Sara Bonato, Isabella Ghione (Fondazione IRCSS Policlinico, Milano)
Luigi Caputi, Fabio Brusaferri (Ospedale Maggiore di Crema)
Anna Cavallini, Alessandra Persico (Fondazione IRCCS "C. Mondino", Pavia)
Alfonso Ciccone, Giorgio Silvestrelli (Ospedale di Mantova)
Raffaella Clerici, Claudio De Piazza (Ospedale Valduce, Como)
Giancarlo Conti (Ospedale Bassini, Milano)
Maria Sofia Cotelli, Marinella Turla (Ospedale di Esine)
Carlo Dallocchio, Sara Mazza (Ospedale di Voghera)
Carlo Ferrarese, Maria Luisa Piatti (Ospedale San Gerardo, Monza)
Bruno Ferraro, Marinella Carpo (Ospedale di Treviglio)
Simona Fanucchi (Ospedale di Melegnano, Ospedale di Cernusco)
Fabrizio Fiacco, Paola Maggio (Ospedale di Seriate)
Fabio Frediani, Simone Tonietti (Ospedale San Carlo, Milano)
Giampiero Grampa (Ospedale S. Anna, Como)
Lorenzo Lo Russo (Ospedale di Merate)
Francesco Lo Savio (Ospedale di Saronno)
Eugenio Magni, Francesco Palmerini (Fondazione Poliambulanza, Brescia)
Mauro Magoni (Spedali Civili, Brescia)
Simona Marcheselli, Manuel Corato (IRCCS Humanitas, Rozzano, Milano)
Mauro Mattioli (Ospedale di Garbagnate; Ospedale di Rho)
Alessandro Padovani (Clinica Neurologica, Università di Brescia)
Leonardo Pantoni, Giacomo Baso (Ospedale Luigi Sacco, Milano)
Alessandro Prelle, Francesco Muscia (Ospedale di Legnano)
Alberto Priori, Lucia Tancredi (Ospedale San Paolo, Milano)
Ignazio Santilli (Ospedale di Desio)
Chiara Scaccabarozzi (Ospedale di Lecco)
Maria Sessa, Sara La Gioia (Ospedale Papa Giovanni XXIII; Ospedale San Giovanni Bianco, Bergamo)
Declarations
Ethical approval and consent to participate.
The work did not directly involve human participants and/or animals. Informed consent was not a requirement.
Conflict of interest
The authors declare no competing interests.
Footnotes
The original online version of this article was revised: The online version contains an error. In the author group, the collaborative (on behalf of the Lombardy section of the Italian Association for Emergency Neurology (ANEU)) were missing during the process, instead, all the members were mentioned in the PDF. The Acknowledgement section were also missing during processing. These are now corrected and modified accordingly.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
6/1/2022
A Correction to this paper has been published: 10.1007/s10072-022-06118-4
Contributor Information
Carla Zanferrari, Email: carla.zanferrari@asst-melegnano-martesana.it.
on behalf of the Lombardy section of the Italian Association for Emergency Neurology (ANEU):
Vincenzo Belcastro, Elisabetta Domina, Sandro Beretta, Massimiliano Braga, Sara Bonato, Isabella Ghione, Luigi Caputi, Fabio Brusaferri, Anna Cavallini, Alessandra Persico, Alfonso Ciccone, Giorgio Silvestrelli, Raffaella Clerici, Claudio De Piazza, Giancarlo Conti, Maria Sofia Cotelli, Marinella Turla, Carlo Dallocchio, Sara Mazza, Carlo Ferrarese, Maria Luisa Piatti, Bruno Ferraro, Marinella Carpo, Simona Fanucchi, Fabrizio Fiacco, Paola Maggio, Fabio Frediani, Simone Tonietti, Giampiero Grampa, Lorenzo Lo Russo, Francesco Lo Savio, Eugenio Magni, Francesco Palmerini, Mauro Magoni, Simona Marcheselli, Manuel Corato, Mauro Mattioli, Alessandro Padovani, Leonardo Pantoni, Giacomo Baso, Alessandro Prelle, Francesco Muscia, Alberto Priori, Lucia Tancredi, Ignazio Santilli, Chiara Scaccabarozzi, Maria Sessa, and Sara La Gioia
References
- 1.Sejvar JJ. Global burden of neurological disease: what’s in a name? Lancet Neurol. 2017;16(11):858–859. doi: 10.1016/S1474-4422(17)30333-2. [DOI] [PubMed] [Google Scholar]
- 2.Fiorentini G, Lippi Bruni M, Ugolini C. Healthsystems and health reforms in Europe: the case of Italy. Intereconomics. 2008;43(4):205–212. [Google Scholar]
- 3.Nuti S, Seghieri C, Vainieri M, Zett S. (2012) Assessment and improvement of the Italian healthcare system: first evidence from a pilot national performance evaluation system. J Healthc Manag.;57(3):182–98; discussion 98–9. [PubMed]
- 4.Salute Md. (2017) Annuario Statistico del Servizio Sanitario Nazionale. [Statistical Yearbook of the National Health Service.]. http://www.salutegovit/imgs/C17pubblicazioni2879allegatopdf.
- 5.Decreto Ministeriale 2 aprile 2015 n. 70 Regolamento recante definizione degli standard qualitativi s, tecnologici e quantitativi relativi all’assistenza ospedaliera.(G.U. 4 giugno 2015, n. 127). .
- 6.Micieli G, Cavallini A, Cortelli P, Rea F, Italian Ng. Did the role of the neurologist in the emergency department change during the COVID-19 pandemic? Evidence from an Italian nationwide survey. Neurol Sci. 2022. [DOI] [PMC free article] [PubMed]
- 7.Rodriguez Cruz PM, Perez Sanchez JR, Cuello JP, Sobrino Garcia P, Vicente Peracho G, Garcia Arratibel A, et al. Workload of on-call emergency room neurologists in a Spanish tertiary care centre. A one-year prospective study Neurologia. 2014;29(4):193–199. doi: 10.1016/j.nrl.2013.04.009. [DOI] [PubMed] [Google Scholar]
- 8.Moulin T, Sablot D, Vidry E, Belahsen F, Berger E, Lemounaud P, et al. Impact of emergency room neurologists on patient management and outcome. Eur Neurol. 2003;50(4):207–214. doi: 10.1159/000073861. [DOI] [PubMed] [Google Scholar]
- 9.Pitts SR, Niska RW, Xu J, Burt CW. National Hospital Ambulatory Medical Care Survey: 2006 emergency department summary. Natl Health Stat Report. 2008;7:1–38. [PubMed] [Google Scholar]
- 10.Chapman FA, Pope AE, Sorensen D, Knight RS, Al-Shahi SR. Acute neurological problems: frequency, consultation patterns and the uses of a rapid access neurology clinic. J R Coll Physicians Edinb. 2009;39(4):296–300. doi: 10.4997/JRCPE.2009.402. [DOI] [PubMed] [Google Scholar]
- 11.Hoang V, Nuwer MR. Changes in emergency department coverage for the neurologist. Neurol Clin Pract. 2013;3(4):334–340. doi: 10.1212/CPJ.0b013e3182a1b898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de Falco FA, Sterzi R, Toso V, Consoli D, Guidetti D, Provinciali L, et al. The neurologist in the emergency department. An Italian nationwide epidemiological survey. Neurol Sci. 2008;29(2):67–75. [DOI] [PubMed]
- 13.Raucci U, Pro S, Di Capua M, Di Nardo G, Villa MP, Striano P, et al. A reappraisal of the value of video-EEG recording in the emergency department. Expert Rev Neurother. 2020;20(5):459–475. doi: 10.1080/14737175.2020.1747435. [DOI] [PubMed] [Google Scholar]
- 14.Nuwer MR. EEG in the emergency department: speeding the patients toward the right treatment plans. Clin Neurophysiol. 2012;123(5):855. doi: 10.1016/j.clinph.2011.09.004. [DOI] [PubMed] [Google Scholar]
- 15.Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344–e418. doi: 10.1161/STR.0000000000000211. [DOI] [PubMed] [Google Scholar]
- 16.Langhorne P, Audebert HJ, Cadilhac DA, Kim J, Lindsay P. Stroke systems of care in high-income countries: what is optimal? Lancet. 2020;396(10260):1433–1442. doi: 10.1016/S0140-6736(20)31363-5. [DOI] [PubMed] [Google Scholar]
- 17.Adeoye O, Nystrom KV, Yavagal DR, Luciano J, Nogueira RG, Zorowitz RD, et al. Recommendations for the establishment of stroke systems of care: a 2019 update. Stroke. 2019;50(7):e187–e210. doi: 10.1161/STR.0000000000000173. [DOI] [PubMed] [Google Scholar]
- 18.Guzik AK, Switzer JA. Teleneurology is neurology. Neurology. 2020;94(1):16–17. doi: 10.1212/WNL.0000000000008693. [DOI] [PubMed] [Google Scholar]
- 19.Roy B, Nowak RJ, Roda R, Khokhar B, Patwa HS, Lloyd T, et al. Teleneurology during the COVID-19 pandemic: a step forward in modernizing medical care. Journal of the neurological sciences. 2020;414:116930. [DOI] [PMC free article] [PubMed]