Abstract
Background
The COVID-19 pandemic had its first peak in the United States between April and July of 2020, with incidence and prevalence rates of the virus the greatest in the northeastern coast of the country. At the time of study implementation, there were few studies capturing the perspectives of nurses working the frontlines of the pandemic in any setting as research output in the United States focused largely on treating the disease.
Objective
The purpose of this study was to capture the perspectives of nurses in the United States working the frontlines of the COVID-19 pandemic's first wave. We were specifically interested in examining the impact of the pandemic on nurses' roles, professional relationships, and the organizational cultures of their employers.
Design
We conducted an online qualitative study with a pragmatic design to capture the perspectives of nurses working during the first wave of the United States COVID-19 pandemic. Through social networking recruitment, frontline nurses from across the country were invited to participate. Participants provided long form, text-based responses to four questions designed to capture their experiences. A combination of Latent Dirichlet Allocation--a natural language processing technique--along with traditional summative content analysis techniques were used to analyze the data.
Setting
The United States during the COVID-19 pandemic's first wave between May and July of 2020.
Results
A total of 318 nurses participated from 29 out of 50 states, with 242 fully completing all questions. Findings suggested that the place of work mattered significantly in terms of the frontline working experience. It influenced role changes, risk assumption, interprofessional teamwork experiences, and ultimately, likelihood to leave their jobs or the profession altogether. Organizational culture and its influence on pandemic response implementation was a critical feature of their experiences.
Conclusions
Findings suggest that organizational performance during the pandemic may be reflected in nursing workforce retention as the risk for workforce attrition appears high. It was also clear from the reports that nurses appear to have assumed higher occupational risks during the pandemic when compared to other providers. The 2020 data from this study also offered a number of signals about potential threats to the stability and sustainability of the US nursing workforce that are now manifesting. The findings underscore the importance of conducting health workforce research during a crisis in order to discern the signals of future problems or for long-term crisis response.
Tweetable abstract
Healthcare leaders made the difference for nurses during the pandemic. How many nurses leave their employer in the next year will tell you who was good, who wasn't.
Keywords: Nurses, Nursing, COVID-19, Pandemic, Health care systems, Health care organizations, Health policy, Health workforce
What is already known
-
•
US nurses faced multiple challenges during the early days of the COVID-19 pandemic, including shortages of personal protective equipment and stress associated with the uncertainty of managing the effects of an unknown disease.
-
•
Working conditions varied widely during the pandemic with perspectives of pandemic working influenced by the timing of the disease's arrival to the geographic location of the country.
What this paper adds
-
•
Nurses working on the frontlines of the COVID-19 pandemic in the US experienced high levels of occupational risk to their health and were observed by them as threats to patient outcomes.
-
•
Risks were not experienced equally across health professions and contributed to stress and threatened well-being. Risks were mitigated by organizational policies centered on pandemic management, which varied widely in quality and strategy thereby affecting nurses differently.
-
•
There appears to be a very real threat of massive losses to the frontline US nursing workforce stemming from working conditions that are contributing to high rates of burnout.
1. Introduction
The United States (US) has 5 million nurses spread across 50 states (Smiley et al., 2021; Smiley et al., 2021). There are a number of frontline nursing roles in the country to deliver care across all points of the health care system. These include licensed vocational/practical nurses (equivalent to enrolled nurses in some countries); registered nurses (who may have diploma, associate, bachelors, or masters entry-level training); and advanced practice nurses that include nurse practitioners and midwives who are masters or doctorally prepared. The majority of midwives in the US are classified as “nurse-midwives” and they are occupationally grouped with nurses due to their small numbers (less than 13,000 nationally) [hereafter, the use of the word “nurse” will refer to all levels of preparation and roles unless otherwise noted]. Approximately 1% of nurses in the US have doctoral degrees (e.g. clinical, research, etc.) and those individuals largely work in research and educational roles (Smiley et al., 2021).
Like all countries, the COVID-19 pandemic has had a major effect on the US nursing workforce. The Centers for Disease Control's (CDC) October 2020 analysis reported that nurses contracted COVID-19 at work at rates six times higher than physicians (Hughes et al., 2020). A Kaiser Family Foundation report also found similar findings with different data (Artiga et al., 2020). Nursing workforce-centric studies from the US during the pandemic have focused largely on issues related to staffing (Figueroa et al., 2020; Gao et al., 2020; George et al., 2021; Gorges and Konetzka, 2020; Harrington et al., 2020; Kates et al., 2021; Li et al., 2020; McGilton et al., 2020; Xu et al., 2020), shortages of personal protective equipment and other resources for care delivery (Butler et al., 2020; Sharma et al., 2021; Wahlster et al., 2021), and the mental health consequences of working the frontlines (Baskin and Bartlett, 2021; Combe, 2020; Gray et al., 2021; Kelley et al., 2021; Kim-Godwin et al., 2021; Norman et al., 2021; Raso et al., 2021; Sharma et al., 2021). Other publications take the form of calls to action, pandemic response programs, or opinion papers (Anders and Lam, 2021; Collins, 2020; Hardt Dicuccio et al., 2020; Jones and Bowles, 2020).
Overall, the global literature that has studied the impact of the COVID-19 pandemic on frontline nurses and midwives grew exponentially from the start of the pandemic in early 2020 and through the end of 2021 with simple searches in the PubMed database yielding over 2000 publications. The majority of these studies have been published by authors from China or those from high-income, Organization of Economic Cooperation and Development (OECD), English speaking countries. Thematically, the literature groups broadly into occupational health related consequences of working during the pandemic, infection control risks experienced by health workers, and studies of manager experiences (Baskin and Bartlett, 2021; Im et al., 2021; Simonovich et al., 2021).
In both the US and international literature, what is less well understood is how the COVID-19 pandemic has affected the intersections of nurses' roles, interprofessional relationships, and the organizations where they work. Since research has long established how roles, relationships, and organizations affect nurses' work experiences, a pandemic specific gap exists. Understanding what happened in the early wave of the pandemic may become critical for understanding the present. Therefore, the purpose of this study was to capture the perspectives of US nurses working the frontlines of the COVID-19 pandemic during the first wave that happened in the Spring of 2020 (April to July). This study was initially commissioned as a working paper for the US National Academy of Medicine as part of the Future of Nursing 2020–2030 consensus study in order to provide initial evidence of the pandemic's effects on the nursing workforce.
2. Methods
2.1. Design
Pragmatic qualitative designs aim to generate findings that are rapidly actionable and translatable into real world settings (Patton, 2015). It is a useful approach for studying the experiences of individuals who work or practice bounded within organizations, like nurses (Kelly and Cordeiro, 2020). With that approach underpinning the design, we developed a national, online qualitative study to pragmatically examine our phenomenon of interest. Prior to the pandemic, online qualitative studies had solidified methodologically to the point where several books were published on the subject (Fielding et al., 2016; Salmons, 2016, Salmons, 2015). Qualitative studies that use online data collection methods (e.g. e-mail interviews, virtual interviews, virtual focus groups, etc.) should adhere to the same principles of rigor and trustworthiness as traditional qualitative methods (Fielding et al., 2016). Online data collection approaches are also recommended when the target population is considered “hard to reach” through traditional recruitment strategies and allow for a national recruitment approach (Matthews et al., 2018; Reisner et al., 2018).
Since the pandemic changed the nature of conducting all forms of research due to social distancing restrictions, including qualitative approaches (Lobe et al., 2020), an online approach to data collection would allow us to achieve the goals of the study and address multiple implementation concerns. This was reinforced after initial exploratory work led us to conclude that scheduling interviews with nurses who were potentially exhausted from working would slow the study's progress.
2.2. Ethics approval
This study was approved by the lead author's Institutional Review Board [#IRB-FY2020–4440]. Participants completed the informed consent process online prior to answering the study's questions. The system did not collect participant emails but did collect IP addresses, which were removed prior to data analysis. Collecting IP addresses did allow us to identify the state where the participant completed the questions. In the US, it is acceptable to collect IP addresses when conducting online research but when collecting data internationally, practices must adhere to the strictest regulations. No incentives were offered to participants as part of completion. No questions were “required” to be answered to progress.
2.3. Sample
To participate in the study, prospective participants had to have worked in a frontline, clinical nursing role in the US between April and July of 2020. They also had to have cared for a person infected with the SARS-CoV-2 to be included in the study. We excluded nurses in indirect care delivery roles (e.g. staff educators, managers)—unless redeployed to frontline roles--to increase sample homogeneity as we wanted to capture the perspectives of direct care providers.
2.4. Recruitment
Consistent with the practices of the majority of U.S. nursing workforce studies related to COVID-19 (see discussion above), the overall recruitment strategy was designed to generate a convenience sample and capitalize on the potential for snowball sampling through social media. This has become a standardized sampling strategy when conducting online data collection (Bethel et al., 2021; Surdam et al., 2020). Based on recommendations from Salmons (2016), the minimum sample goal was a total of 50 participants who would fully complete the series of questions—a number that would allow us to achieve data saturation. This strategy also allowed us to compensate for the low response rates or incomplete responses expected from web-based data collections strategies and fluctuating social media site memberships that make total sample size estimation difficult (Fan and Yan, 2010).
To begin the recruitment process, we developed a digital study flyer to “brand” the study when sharing invitations to participate. This would provide a consistent visual image associated with the study.
Recruitment strategies between April and July 2020 were then multi-pronged, involving professional networks, social media (e.g. Twitter, Facebook), and the use of nursing and midwifery focused listservs that would reach a national audience. The team initially reached out via the alumni networks from their respective alma mater institutions (8 total) through the alumni offices, which did not share their lists but distributed the link. Importantly, the accuracy of these lists is usually incomplete and dependent upon individuals updating their information, so the total number of people reached were estimates at best, with 4–5000 nurses and midwives reached nationally.
The next step was to send a study invitation via social media sites. Team members already had affiliated themselves with Facebook groups associated with nurses aligned to their professional interests. The study leads also used their personal professional networks on social media to send recruitment notices to another 135 individuals who then subsequently shared the information with their social and professional networks. Posts by 2 Twitter active team members and the study leads' home institution also occurred every 2 to 3 weeks. Finally, three national listservs received one recruitment email. The team estimated that overall recruitment efforts reached between 8 and 10,000 nurses and midwives.
2.5. Data collection
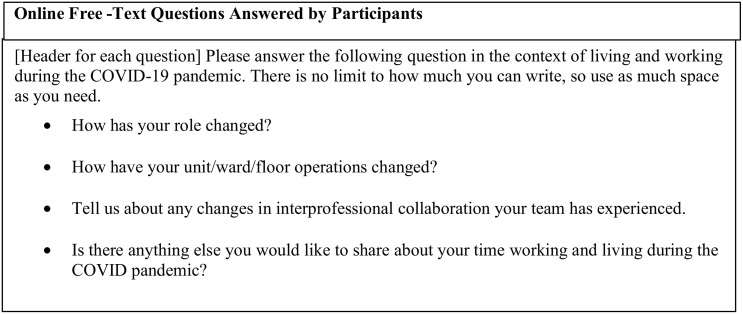
The Qualtrics XM Survey software was used to collect data. Once prospective participants confirmed their participation, they were asked to connect to an online link to complete a free-text questionnaire. After completing a demographic profile, participants were asked to provide free text responses to the questions focused on role changes, teamwork, and their place of work. These questions were developed based on the team's expertise and reviewed by the original commissioner of the work (see Fig. 1 ). Each question was given a single page on the screen to focus the response. The text box was made large enough to fill the entire screen to encourage participants to write as much as they desired. Participants could go back and review answers prior to submitting. They were not prompted nor reminded to complete the survey once it was started.
Fig. 1.
Online free-text questions answered by participants.
2.6. Data analysis
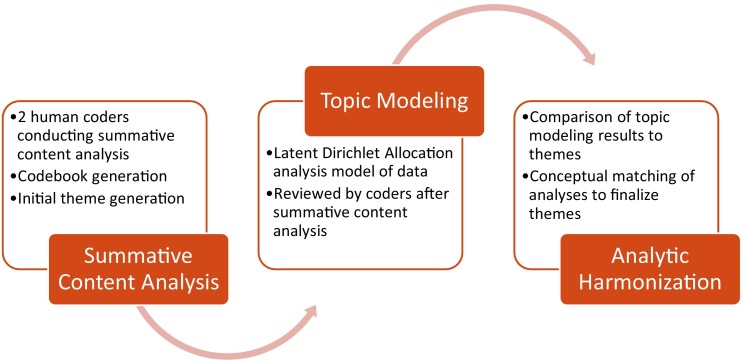
The analysis team consisted of a health services researcher, a clinician-researcher who also worked the frontlines, and a methods specialist for the natural language processing component. The team used a novel combination of summative content analysis and computational natural language processing approaches to analyze the data.
For background, traditional content analysis, as an approach to qualitative data analysis, is widely used. It can involve text-based, theoretical, intuitive, impression-based, interpretive, or systematic analyses (Cavanagh, 1997). The overall approach of content analysis emerges from a largely naturalistic paradigm where the main goal of the analysis is to enhance the knowledge and understanding of a specific phenomenon of interest (Hsieh and Shannon, 2005). Summative content analysis quantifies the contextual use of words or phrases in a dataset while integrating interpretive strategies that help to explain the frequency with which the words and phrases appear in the dataset (Hsieh and Shannon, 2005). Importantly, the lack of frequent appearance in a dataset can be interpreted as just as significant as those which appear regularly. Most important in the interpretation of word and phrase frequency is the significance of the observed patterns in relation to the context in which they appear (Morgan, 1993).
For the coding process, searches of word appearances occur by hand or through the use of computer word search functions. Speakers of the words and phrases are tracked simultaneously to see if there are links to the specific speakers' identities in terms of how frequencies are generated. This step helps to determine if, for example, a single speaker biases the results by artificially increasing the frequency of the appearances which would conflate the interpretation of the results. Confirmation of the accuracy of coding processes always involves a second coder confirming the frequencies and interpretations. Quantifiable measures of intercoder reliability are often used but not required. Overall, the process lends insights into the how and why the speakers used the words since frequencies are always considered within the context of who spoke and how often.
For machine-based text analyses, a number of valuable technological approaches to text analysis have recently been applied within the social sciences; for overviews see Benoit (2020), Grimmer and Stewart (Grimmer and Stewart, 2013), or Grimmer et al. (2022). Among those approaches, topic modeling using Latent Dirichlet Allocation (Blei et al., 2003) has emerged as a particularly useful method for automatically discovering latent categories bottom-up in collections of texts; examples in a range of disciplines include political science (Grimmer and Stewart, 2013; Isoaho et al., 2021), social and cultural studies (Mohr and Bogdanov, 2013), digital humanities (Meeks and Weingart, 2012), and bioinformatics (Liu et al., 2016). In contexts particularly relevant for nursing studies, recent examples include Guo et al. (2021), who report on the use of topic modeling for social media posts by self-reported COVID-19 positive individuals as a step toward better informed patient-centered care practices, and Fairie et al. (2021), who analyzed a large database of patient feedback and concerns. Although a number of more sophisticated variations exist, including models handling covariates that are specifically designed for application to open-ended survey responses (Card et al., 2018; Roberts et al., 2014) the simpler Latent Dirichlet Allocation method is dominant when topic models are used in practice and was applied here (Blei et al., 2003).
The core idea in a topic model is very similar to more common methods in statistics for discovering latent structures in sets of data--such as principal component analysis or factor analysis. In principal component analysis, the idea is to take a set of high-dimensional items, and reduce the way they are represented to a much smaller number of explanatory dimensions (Isoaho et al., 2021). By squeezing representations into a lower-dimensional space, each dimension captures some general aspect of the data – effectively finding dimensions of commonality among the items. In the case of a topic model, each item is a document (here, an open-ended response), and by analogy the topic model derives a smaller set of dimensions of commonality expressed in the dataset as a whole, despite the fact that each item has a very large number of dimensions, namely the size of the vocabulary. Each resulting topic, or latent category, is represented as a probability distribution of the vocabulary.
To illustrate, in analyzing the set of responses to a question about how people are coping with stress, the topics or latent categories that emerge from the analysis include one that assigns high probability score to the words family, yoga, walks, friends, exercise, outside, … . Looking at these high-probability terms that characterize the topic and also looking at the responses that are weighted most heavily for this category (analogous to items with high loadings on a particular dimension in a principal component analysis), a content expert will quickly discern that one relevant dimension in people's responses involves coping via physical activities. Another topic emerges with high probabilities for friends, family, talk, coworkers, …, which, again in tandem with inspection of associated responses, yields an interpretation of another coping strategy involving social interaction with friends, family, and coworkers. More details regarding the topic modeling can be found in the supplementary materials.
Neither traditional content analysis nor automatic topic modeling is a perfect process. However, comparing the results of traditional human coding with automatically discovered topics and their interpretations adds rigor to the analysis, and increases confidence that the resulting categories of response are valid. Thus, for this study two team members first conducted the summative content analysis, with one conducting the initial coding and the other completing the coding confirmation process. A common codebook was created after 15% of responses were coded. Coding saturation (Hennink et al., 2017), where no new codes emerge, occurred after 45% of responses were coded. Discrete responses--defined as a sentence or thought series comprised of multiple sentences on the same topic--were quantified. Comments with a “sentiment” were classified as positive or negative.
All coding was then compared with the automatic, bottom-up computer-based analysis using a Latent Dirichlet Allocation topic model as a further check on the consistency of the analytic process and as an exercise in reflexivity using a very conservative approach with regard to the contributions of the automated method. Rather than a topic modeling analysis plus human validation (Ying et al., 2021) our method in this paper is more appropriately viewed as a traditional summative content analysis augmented by comparison with automatically derived categories — that is, the human content analysis was primary, with the automated analysis serving as an additional component. To the extent that codes emerging from the traditional process corresponded well with automatically derived categories, that lent confidence to those codes being robustly present in the data rather than emerging from researcher biases or expectations. Figure 2 illustrates our data analysis process.
Fig. 2.
Combined data analysis process model.
3. Results
Raw data showed that 1074 persons had visited the initial study page. There were 318 initial engagements with the survey, meaning users who agreed to participate. Among those, 46 of the total participants indicated that they were not nurses with an additional 18 who indicated they had not cared for COVID patients (thus meeting exclusion requirements), 3 selected that they did not want to participate, and 9 consented but did not answer a single question.
The final sample size for the analysis comprised 242 participants meeting the inclusion criteria, with participants from 29 out of 50 states. The majority of participants came from work locations east of the Mississippi river, consistent with where the COVID-19 pandemic was having its greatest impact during April and July of 2020. The average time spent on the answering questions was 22.9 minutes and ranged from 15 to 45 minutes. Table 1 provides a summary of participant demographics. The responses notably lack the perspectives of Latinx/Hispanic and Native American nurses.
Table 1.
Participant demographics (n = 242)*.
| State | # Participants1 | % | Demographics | |||||
|---|---|---|---|---|---|---|---|---|
| Alaska | 1 | 0.4% | Item | # | % | Item | # | % |
| Arizona | 1 | 0.4% | Gender | Population served | ||||
| California | 13 | 5.4% | Female | 191 | 78.9% | Adults | 201 | 83.1% |
| Colorado | 1 | 0.4% | Male | 21 | 8.7% | Geriatric | 12 | 5.0% |
| Connecticut | 7 | 2.9% | No response | 30 | 12.4% | Pediatric | 10 | 4.1% |
| Delaware | 2 | 0.8% | No response | 19 | 7.9% | |||
| Florida | 3 | 1.2% | Sexual orientation | |||||
| Georgia | 4 | 1.7% | Straight | 194 | 80.2% | Place of work | ||
| Illinois | 1 | 0.4% | Bisexual | 9 | 3.7% | Emergency department | 25 | 10.3% |
| Kansas | 1 | 0.4% | Lesbian or Gay | 8 | 3.3% | Intensive care unit | 73 | 30.2% |
| Louisiana | 1 | 0.4% | Queer | 3 | 1.2% | Labor and delivery | 6 | 2.5% |
| Maryland | 3 | 1.2% | Prefer not to answer | 1 | 0.4% | Medical-surgical | 39 | 16.1% |
| Missouri | 2 | 0.8% | Other | 1 | 0.4% | Mental health/psychiatric | 1 | 0.4% |
| Mississippi | 1 | 0.4% | No response | 26 | 10.7% | Other | 54 | 22.3% |
| Montana | 1 | 0.4% | No response | 44 | 18.2% | |||
| North Carolina | 1 | 0.4% | Race &/or ethnicity | |||||
| Nebraska | 6 | 2.5% | Asian/Pacific Islander | 34 | 14.0% | Geographic location of place of work | ||
| New Hampshire | 1 | 0.4% | Black/African-American | 14 | 5.8% | Rural | 12 | 5.0% |
| New Jersey | 30 | 12.4% | Latinx/Hispanic | 0 | 0.0% | Suburban | 46 | 19.0% |
| New Mexico | 1 | 0.4% | Native American/Indigenous | 0 | 0.0% | Urban | 148 | 61.2% |
| New York | 96 | 39.7% | White | 151 | 62.4% | No response | 36 | 14.9% |
| Ohio | 2 | 0.8% | Biracial | 11 | 4.5% | |||
| Pennsylvania | 34 | 14.0% | Other | 5 | 2.1% | |||
| Texas | 3 | 1.2% | Prefer not to answer | 2 | 0.8% | Education level | ||
| Virginia | 7 | 2.9% | No response | 25 | 10.3% | Associates Degree | 4 | 1.7% |
| Washington | 2 | 0.8% | Bachelor's Degree | 105 | 43.4% | |||
| Washington, DC | 4 | 1.7% | Years of experience in nursing/midwifery | Master’s Degree or Higher | 51 | 21.1% | ||
| Wisconsin | 2 | 0.8% | 0–3 | 66 | 27.3% | Other | 52 | 21.5% |
| West Virginia | 1 | 0.4% | 4–6 | 48 | 19.8% | No response | 30 | 12.4% |
| No IP Identified | 10 | 4.1% | 7–10 | 24 | 9.9% | |||
| Total | 242 | 100.0% | > 11 | 75 | 31.0% | Role | ||
| No response | 29 | 12.0% | Registered Nurse | 166 | 68.6% | |||
| Advanced Practice Nurse | 34 | 14.0% | ||||||
| Type of facility | Administration/Education | 5 | 2.1% | |||||
| Teaching Hospital | 146 | 60.3% | Other | 3 | 1.2% | |||
| Non-Teaching Hospital | 50 | 20.7% | No response | 34 | 14.0% | |||
| No response | 46 | 19.0% | ||||||
No participants indicated they were transgender even though the option was provided.
From the analysis, six themes emerged. They are discussed in the succeeding sections. The original participant emphasis on specific words is maintained but abbreviations used by them are spelled out.
3.1. Place of work matters: characteristics of supportive vs. unsupportive organizational level pandemic response implementation
Where a nurse worked and the associated organizational culture strongly affected participant responses and emerged as a significant theme. Quite starkly, an employer was perceived as supportive or not of nurses during the pandemic, as reflected by their 204 comments on the subject. Comments were consistently positive or negative, with little variation, and thus allowed this kind of dichotomous categorization. For example, staff felt valued by their organizations actions or punished with actions like cuts to vacation time, raises, or retirement contributions despite the risks and extra work hours they assumed. Hospital administration was either present and conveying their awareness of staff challenges while working, or perceived as completely out of touch with the frontlines, as evidenced by a lack of physical presence. Email communications from management were too much or not enough, either conveying a sense of chaos or coordination.
Table 2 illustrates these contrasts with exemplars of descriptions provided by hospital nurse participants of the dimensions of supportive and unsupportive organizational cultures. Categories comprising this theme include: Communication; In-Person Contact Quality with Hospital Administration; the Frontline Manager; the Culture of the Response as Perceived by the Nurse/Midwife; and Staff Treatment during the first wave. Conceptual definitions of the categories are also provided in Table 2. Figure 3 provides a conceptual model of the dimensions of organizational cultures affecting pandemic response implementation based on the participants' experiences.
Table 2.
Supportive vs. unsupportive aspects of organizational culture.
| Category | Supportive | Unsupportive |
|---|---|---|
|
Communication Definition: How communication about pandemic response was handled. |
There is a lot more communication between managers and the nursing staff about how to address the COVID patients and how to protect ourselves. There are emails being sent out everyday to all hospital staff about updates of the hospital and what everyone should be doing and what to expect. (Urban medical-surgical nurse) | The epidemiologists are having to work with us and that has been a really eye opening experience for them. In my opinion, they undervalue us and what we are capable of. Their communication with us has been downright awful. Things have been so confusing that in a recent meeting, one of the nurses actually started yelling at the epidemiologist. Every minute there is a new process or a new way to input data and there has been little high quality training. The epis get frustrated when we don't do things right, but they don't explain what they want clearly. I don't think that they realize that if they just wrote out what they wanted us to do or had a brief five minute video that things would be done more correctly. There is this hesitation to delegate larger tasks which increases the burden on them. It's like they don't know how to use their nurses. Granted, we have enough going on, but still, if more needed to be done, we could make it happen. (Urban medical-surgical nurse) |
|
In-Person Contact Quality with Hospital Administration Definition: The quality of interpersonal interactions experienced by nurses with administrators or managers |
Frequent meetings and “huddles” regarding surge plans, disaster preparedness, changing of current guidelines, etc. (Suburban intensive care unit nurse) |
There is a more sound feeling of an “us vs. them” front line workers being the “us” and upper management or corporate being “them”. (Suburban medical-surgical nurse) |
|
Frontline Manager Definition: How the nurse's direct supervisor was perceived to handle pandemic response. |
My manager was amazing and was at one point taking teams on night shift to help out in as well as two assistant nurse managers from other medical surgical floors who divided shifts and spent most of the time making sure we had PPE stocked, keeping us abreast of the changing protocols, and making sure we had enough staff to function (always a challenge). (Teaching hospital pediatric nurse) |
Our manager formed a Covid prep team on our unit that was or organize equipment and supplies. They were supposed to run Covid drills and until under scrutiny these drills only started recently. The Covid prep team also quickly dismantled because they were micromanaged and poorly lead. (Teaching hospital medical-surgical nurse) |
|
Culture of Response Definition: How nurses' perceived the culture of pandemic response by their organization. |
Overall the response in my institution was a concerted effort to be patient and helpful with *everyone*, whether other disciplines or RNs redeploying from other areas. (Rural hospital nurse) |
It upsets me that [the main hospital] and [the specialty hospital] (can't speak for the others) were swimming with resources and didn't share with sister [system] sites. (Urban teaching hospital nurse) |
|
Staff Treatment Definition: How nurses reported they felt they were treated by their employer |
The support of admin and community really helped. Cheers, cards, meals etc. was so appreciated. Staff who cared directly for covid should receive hazard pay. (Urban medical-surgical nurse) |
Not being recognized or treated as an essential human that holds up a place/company but rather just expendable asset/tool is beyond infuriating. (Suburban intensive care unit nurse) |
Fig. 3.
Factors affecting nurses' experiences with organizational level pandemic response implementation.
3.2. “We are doing everything now” – role changes of frontline nurses
Seventy percent of participants noted how their roles had changed and said changes affected both registered nurses and advanced practice ones. The 30% of participants who reported no changes to their roles were usually working in states that had not yet experienced a surge in cases at the time of data collection.
Reported changes most often took the form of assuming more responsibility and becoming the focal person who was delivering care because personnel (e.g. physicians, pharmacists, etc.) with little recent hospital care experience were assigned to work on their units. Consequently, registered nurses reported that they frequently directed personnel with prescriptive privileges assigned to their units what to order to ensure their patient's needs were met—physiologically, psychologically, physically, and spiritually. A nurse from a medical-surgical unit wrote: “We went from having Physician Assistants and residents to having doctors from different services who had not done [hospital work] for years and honestly, had no idea what they were doing.”
All nurses noted that they spent more time on the phone and communicating with family members due to hospital visitation restrictions, as illustrated by this quote from a medical-surgical nurse: “I feel like I spend more time on the phone updating family members. I also need to provide my patients with emotional support that they would normally get from family members.” The added time with familial support was coupled with the complexity of working with staff that had little recent inpatient experience.
Organizational responses to the COVID-19 pandemic that involved human resources interventions also generated more role changes for nurses. As an organizationally driven nosocomial infection prevention strategy, in one academic medical center registered nurses were often asked to assume environmental services (a.k.a. “housekeeping”) and clerical duties. A medical-surgical nurse from that organization reported that she and her colleagues “…have taken on added roles of [nursing assistants], lab, housekeeping as it allows for less exposure for the rest of the Staff”. A step-down unit nurse from the same city noted she had “more responsibility (trash, cleaning, having nothing supplied in the room, ventilator changes, no [certified nursing assistants])” and that she “had to cluster care together more than ever to minimize exposure in the room.” These new additions to their roles also translated into more work, especially in the intensive care unit.
By contrast, advanced practice nurses participating in the study noted their only significant changes centered on the point of care delivery, usually a major shift to telehealth work or reduced practice restrictions that expanded their responsibilities (a number of US states lifted practice restrictions on advanced practice nurses to address personnel shortages). When previous restrictions on their scope of practice had been lifted, they uniformly reported that it helped them work more efficiently since they had fewer restrictions on what they could do.
3.3. The changed nature of workplace risk
From participant responses, risks at work changed for nurses on the frontlines during the first wave of the COVID-19 pandemic. The nature of these changes came in two forms: 1) from redeployment and 2) increased risk for occupational injury.
3.3.1. Redeployment
Redeployment was a phenomenon experienced by nurses that they perceived increased their “risks” at work. They experienced the phenomenon when they were reassigned to work on another unit that had a) higher acuity patients (e.g. medical-surgical nurse redeployed to an intensive care unit); b) a different patient population (e.g. a pediatric nurse assigned to work on an adult unit); or c) a practice area where they had no recent experience (e.g. a primary care nurse who had previously worked in intensive care more than a decade ago).
Nurses who reported they were redeployed during the pandemic were acutely aware of their risk for committing a mistake due to a lack of training or support. At most, training (if any was provided) for these redeployment roles involved a single day. None of the 73 participants who indicated they had been redeployed reported more time than that.
For nurses who were not redeployed, the complexity of their role increased as they mitigated additional patient safety threats and risks brought by the presence of “new” personnel on the unit. “New” personnel included physicians and physician assistants with no recent inpatient care experiences as well as “Travel Nurses” (a.k.a ‘Travelers’).1 For example, a nurse working on a telemetry floor who had experienced working with all three types of new personnel remarked, “I have become more of a mistake fixer than a nurse caring for her patients. I fix doctors mistakes and other nurses (mainly travelers) mistakes.” Redeployment, therefore, appears to have increased nurses' sense of threats to patient safety and thus, their perception of risks to their own practice while working.
3.3.2. Occupational risks
Participants reported different risks for occupational injury based on their nursing roles. The uniform perception among all registered nurse participants was they assumed higher levels of risk in terms of occupational exposure to COVID-19 infection compared to advanced practice nurses, physician assistants, or physicians. Eighty reports from participants noted this issue. For example, an intensive care unit nurse in a suburban hospital reported:
The nurses were constantly in the rooms. Everyone else wasn't. That was the biggest change. Doctors did their assessments from the windows, respiratory would run in to change a vent and run out, anesthesia would gown up, intubate and run out as fast as possible. Many times we were the ones stuck inside to deal with the clean-up and any emergencies that might arise from someone's negligence due to fear of being in the room for too long.
Medical-surgical nurses shared similar examples of physicians conducting daily patient assessments from outside the room.
Registered nurses often had to enforce organizational policies around protective measures designed to minimize nosocomial transmission of the virus. Enforcement of these rules added to their occupational risks for experiencing hostile behavior in the workplace. An obstetrics nurse relayed this story of a hospital employee whose wife was admitted in labor:
We had one instance where an [intensive care unit] attending was the patient's visitor. He admittedly took care of hundreds of COVID-positive patients and had a temperature of 99.9F. Our cutoff was 100.0F. We told him to walk around for an hour and come back. He was angry that we delayed his entry into the unit. But we had to make sure she was staying before we let him upstairs. He walked around outside for an hour and his temp came back as 97.3F. In these instances, doctors were unsupportive of our efforts to delay entry. But if he had brought infection to our unit, our workforce would be depleted.
In this case, the obstetric nurse had to enforce the same standards for all visitors despite the visitor being an employee of the hospital. The reaction of the employee was also a source of stress because the nurse felt like she should not have to deal with someone who should know better when it comes to infection prevention.
3.4. The dynamics of pandemic teamwork
Reports from participants in this study highlighted both the positive and negative aspects of frontline teamwork. Positive aspects of teamwork fell into three categories. “Bonding with co-workers” reflected how the nature of working the frontlines helped nurses and their interprofessional coworkers bond and form stronger workplace relationships. “More teamwork improved care” meant that when every professional contributed to patient care, no matter how small the task or if it was not in their usual duties, nurses perceived the overall quality of care as improved. Finally, “Humility and Respect” represents descriptions of interprofessional collaboration that reflected humble and respectful interactions by all team members when delivering care. Table 3 illustrates four positive examples of teamwork experiences from nurses on the frontlines, underscoring the importance of teamwork between nurses themselves, nurses and physicians, as well as any person involved in delivering care –including management.
Table 3.
Categories and supporting quotes of positive teamwork experiences during the first pandemic peak.
| Bonding with co-workers |
| I do also feel like I am able to make a difference like no other time in my career...and the teamwork has never felt stronger. My coworkers have really bonded. (Urban hospital registered nurse) |
| More teamwork improved care |
| The doctors and nurses have, in my opinion, worked more collaborative. They really ask our opinion and respect our profession a bit more than before and vice versa. We had some amazing doctors jumping in to help with duties they have never done before and I think that really improved patient care. (Teaching hospital advanced practice nurse) I believe this pandemic showed us all the importance of working as a team. It would have not been possible without the cooperation from everyone. Everyone played an intricate part in trying to save the lives of our community. I was very proud of all my co-workers, the nurses, travelers, doctors, respiratory therapists, X-ray techs, dietary, MDD, engineering, building services, and upper management who jumped right in to do what was needed to assist and make a difference. I am honored to work for an Organization who went to every length to assist the affected community and it's employees. This truly was the year of the Nurse and the patient! (Community hospital registered nurse) |
| Humility & respect |
| It was refreshing to see attending MDs with decades of experience all eagerly learning how to care for covid patients as self-proclaimed new residents/interns. Many volunteered. Previously intimidating providers seemed more personable as everyone was outside of their own comfort zone. (Academic medical center registered nurse) |
Nonetheless, not all reports were positive. An intensive care unit nurse from the Midwest working at a small teaching hospital offered this example of a negative experience with teamwork:
Awful. I am so sad writing this right now. I knew there was a lack of maintaining [evidence-based practice] knowledge in my hospital but this pandemic has truly highlighted it. No, we are not an academic hospital but, we do have residents. And I feel bad for them because they are being shown awful ways of practicing. Respiratory therapy are running our ventilators. Not once in three months have I witnessed a physician collaborate with a [respiratory therapist] on appropriate ventilator settings. Not once have I heard a physician say, "I read recently..." I pride myself for being a nurse who cares about research and [evidence-based practice] but to work with physicians who don't is hard.
In this case, the negative teamwork experience was rooted in maintaining evidence-based practice. The nurse was anticipating the longer term effects of poor training of medical residents for future teamwork as well as working with physicians who did not value staying up to date on the latest evidence. She knew it would affect the quality of care for patients infected with COVID-19 as well as others.
Negative teamwork experiences were also about disclosing COVID symptoms to the team. About 20% of the negative comments about teamwork centered on failure to disclose symptoms of an actual or potential COVID-19 infection or frustration with organizations that were relaxed about testing and/or testing requirements. An intensive care unit nurse wrote:
One particular doctor was very ill at the beginning of the pandemic, requiring [intensive care unit] admission. He was still treating patients for a week while he was symptomatic. Some of his patients came to the hospital with COVID infections. This really sowed distrust amongst colleagues. I remain cordial with this doctor but many nurses were angered by this.
The latter two descriptions helped to identify where two sources of frustration associated with teamwork in hospital care likely occurred during the pandemic.
3.5. Should I stay or should I go? – the pandemic's impact on retention & turnover
Reflections on turnover and attrition from the participants offer some insight into the reasons why nurses at all levels may leave their positions and what some of the drivers of organizational level attrition. A nurse who left her job in Texas to work during the first surge of hospitalizations in New York City associated with pandemic infections captures one dimension of the pandemic's potential effects on nurses leaving their current positions:
I feel honored to have the knowledge and skills to care for the almost severely affected during this pandemic. I left my home to come assist in the largest hotspot in the country. I was forced to resign to do this. I have no regrets. But this experience has changed me and I am not sure what to do professionally after this experience. I will, of course, continue to be an [intensive care unit] RN, I just do not know where or when. It doesn't feel like I could just go back to finding a regular full time job. I know many RNs going through this feel the same.
Her words highlight how she and others were reflecting on the how, where, when, and why of their nursing jobs.
At the same time, the management practices of some health care organizations during the pandemic may drive many away. A highly experienced (11 + years) medical-surgical nurse recounts the following about the management response in her organization and how it drove her to think about quitting the profession for the first time in her career:
The fact that we were not given N95 masks and received push back from management when requesting [COVID] testing has made me realize that our current system does not value health care workers. This is the first time in 25 years that I've wanted to quit nursing. I am still committed to my patients but I know that my hospital does not value my well-being or my life. It is a very broken system.
The sentiments expressed in these two exemplar quotes were echoed in 43 similar comments provided by participants.
3.6. Finding value in nursing work
Valuing nursing work fell into two categories: Renewed personal value for nursing work and the public's value of nursing. First, about one quarter of the responses from participants conveyed a renewed sense of their mission and value as a nurse and why they chose the profession. A nurse whose organization expanded their deployment into the local community relayed the following example of how she felt personally renewed when working the frontlines:
We are so exhausted when we have to be out …in full PPE dying in the sun, but it is so fulfilling to feel like you're out there making a difference. Even working through our list of positives and calling all of our patients, it is really fulfilling to get to the end of the list - or set up an entire family for testing (FREE TESTING!) and help be a part of stopping this monster from running through our community. We've also found that we are reaching some of the more health disparaged parts of our community who don't know anything about what we do and we are connecting them to the overall health system…I wouldn't quit this job or trade it in for anything.
The organization reaching out to expand work in the community at no cost to the local residents was an energizing force for the nurse that sustained her through grueling work.
Finally, multiple participants also noted, with mixed feelings, that it took a pandemic for the public to really recognize the risks nurses face in their jobs and appreciate them. The following quote from a medical-surgical nurse shows the mixed-emotions many participants expressed about the public response: “While the support was amazing, it makes me angry that it took this event for people to appreciate the amazing work nurses do both during and before such a pandemic.”
4. Discussion
Our analyses provide needed insight into the working conditions experienced by nurses on the frontlines of the pandemic's first wave in the US. Importantly, this study helps to contextualize their working conditions and the role of the organization in shaping the experience. The study also offers a number of policy signals about the future of the nursing workforce in the US and supports the findings of other studies.
To begin, the findings aligned thematically with a qualitative study conducted by Kelley et al. (2021) with 78 largely Midwestern participants in the same year when the pandemic was spreading more widely. Other studies have also shown that the work environment, teamwork, and occupational risks were similar across multiple countries and settings (Bhandari et al., 2021; Firew et al., 2020; Kim-Godwin et al., 2021; Kluger et al., 2020; Rollison et al., 2021; Shinners and Cosme, 2020; Simonovich et al., 2021). Valuing nursing and career changes were more specific to the US as findings from other countries were highly specific to the context of nursing practice and care delivery.
The findings also suggest that nursing workforce indicators, like retention rates of nursing personnel, may be a good gauge of overall organizational performance when managing both patients hospitalized with COVID-19 infections as well as other standardized outcome measures. Just as where patients received care affected their hospitalization-related outcomes (Azar et al., 2020; Harrington et al., 2020; Mackey et al., 2021; Rodriguez et al., 2021), this study suggests that where nurses worked provided a similar dynamic. Future research should explore if there is such an association along with studies examining workforce sensitive predictors of patient outcomes.
The legacy of role changes nurses' experienced is likely to be an ongoing subject of future research studies. The long-term impact of role changes on registered nurses is less clear and requires further study. By contrast, advanced practice nurses may gain the most from the pandemic. For context, prior to the pandemic most advanced practice nurses in the roles of nurse practitioners or nurse midwives did not have equal scope of practice across all US states (National Academies of Sciences, Engineering, and Medicine, 2021). Some states allowed them to practice to the full extent of their license whilst others did not. Findings about advanced practice nurses in this study support other US based studies about this role during the pandemic (Feyereisen and Puro, 2020; Kleinpell et al., 2021; O'Reilly-Jacob and Perloff, 2021) as well as the United Kingdom-based findings from Wood et al. (2021). With multiple states reducing or eliminating scope of practice barriers, a natural experiment has occurred that can provide the data to determine if these policy changes should remain permanent (Feyereisen and Puro, 2020).
The perception of experiencing higher levels of occupational risk when working the first wave of the pandemic has been confirmed by other studies (Artiga et al., 2020; Bui et al., 2020; Hughes et al., 2020). Our study offers some contextualization as to why and how that occurred across multiple organizations. The higher rates of infection by frontline nurses may reflect organizational policies that protect “revenue generators” (e.g. physicians or roles that can bill for services) at the expense of other employees who are typically classified as “expenses” (e.g. nurses who can be furloughed). The current incentive structure of the US healthcare system has no economic protections or rewards for nurses as studies published since these data were collected have confirmed that nurses are furloughed or terminated at higher rates than physicians across the country (Gooch, 2020). It is one of the better illustrations of how incentive and reimbursement systems in the US may have added both economic and occupational risk to the experiences of nurses on the frontlines during the first wave of the pandemic. The call for “hazard pay” by many of the study's participants appears warranted.
Some of the early warning signals from this study about nurses contemplating leaving their jobs have now come true in the US. Staffing shortages are resulting from a) how nurses were treated by their organizations during the pandemic and b) a lack of financial incentives to keep experienced nurses in the organization. Some organizations are offering sign on bonuses to registered nurses yet not increasing the base pay of existing staff. These same organizations are also hiring travel nurses at higher rates instead of increasing staff's base pay (Bernstein, 2021). For many nurses, the financial incentives and opportunity to work in a potentially better environment is driving attrition rates across the country. Nurses are now changing employers because of their work experiences during the pandemic, and this study offers insights as to why.
Finally, the descriptions of participants reflecting on their career paths support that there is an opportunity to capitalize on those seeking career transitions to strengthen the overall public health infrastructure in the country and recruit nurses into public and community health-based positions. Recruitment of nurses into these positions should be part of broader policy strategies for rebuilding public health infrastructure across the country so that it is better prepared for future pandemics and emergencies.
4.1. Methods reflection
Traditional content analysis methods and computational topic modeling have contrasting advantages and disadvantages. Latent Dirichlet analysis and related techniques have the advantage of being highly scalable, and because they are fully automatic method and driven entirely by the data, the categories they infer are not influenced by researcher preconceptions or bias. At the same time, no automatic method can be guaranteed to produce results that are fully trustworthy and relevant: that requires human subject matter expertise and insight. Therefore validation of topic models is essential, and procedures for doing so are an active subject of research (Hoyle et al., 2021; Ying et al., 2021).
One surprise in this study was Latent Dirichlet analysis' success in identifying meaningful categories (known as such by their correspondence with human content analysis categories) despite the small size of the dataset. In general, topic models can be hit-or-miss when the number of text units being analyzed numbers only in the hundreds. The fact that sensible human-interpretable topics emerged suggests a fair degree of consistency and high signal-to-noise ratio in responses.
The value-add of topic modeling in this study, over and above the human content analysis, is a motivation for further methological research on ways to integrate human subject matter expertise and automated methods, particularly in larger-data scenarios where traditional content analysis methods run up against issues of speed. Scalability, or both. One area where this may be useful is for systematically analyzing text-based responses in survey research for the “comment” sections, which often contain rich data yet go unanalyzed or fail to get integrated into the quantifiable results.
4.2. Limitations
Even though this was a national study, it relied on convenience and snowball sampling for recruitment and thus, some groups are underrepresented in the findings. Methodologically, the study has many of the same limitations as any qualitative study around the limits of the generalizability of the findings yet other studies highlighted in the discussion support the translatability of these findings to other contexts. We were also unable to follow-up with participants due to the anonymized responses. The natural language processing analysis did, however, help to mitigate human bias in the analysis and added rigor to the process. Further, the timing of the study may also have biased participants toward those who had experienced the pandemic in its initial worst stages when treatment protocols were largely experimental. A study conducted now may produce different results since evidence generated since then has improved treatments and outcomes.
5. Conclusion
Differences in health system structures, financing, and nursing roles will shape the experiences of nurses and midwives working on the frontlines of health care delivery during a pandemic or other disaster. Research about the experiences of nurses and midwives working during different waves of the pandemic is critical for ensuring that there is documented evidence about how the pandemic has affected these cadres of the health workforce around the world. Research will also form the evidence base that will inform future policies around pandemic and disaster response.
To ensure that nurses and midwives are not left out of current and future policymaking, there needs to be evidence specific to every country in the world. We also need a sufficient evidence-base to understand where commonalities and differences in the frontline experiences of nurses and midwives exist. Common experiences can aid in the development of universal, evidence-based strategies to support the nursing and midwifery workforce throughout the world; the differences will highlight what needs to be tailored to a country's specific needs. A strong evidence-base, therefore, is critical to sustaining a pandemic workforce as well as facilitating its recovery (Fraher et al., 2020).
Funding
Parts of this study were funded by a US National Science Foundation grant (NSF Grant #2031736).
CRediT authorship contribution statement
Allison Squires: Conceptualization, Data curation, Formal analysis, Methodology, Resources, Software, Supervision, Validation, Writing - original draft, Writing - review & editing. Maya Clark-Cutaia: Conceptualization, Data curation, Formal analysis, Project administration, Resources, Validation, Writing - original draft, Writing - review & editing. Marcus Henderson: Data curation, Investigation, Project administration, Software, Writing - original draft, Writing - review & editing. Gavin Arneson: Data curation, Investigation, Project administration, Software, Writing - original draft. Phil Resnik: Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Resources, Software, Supervision, Validation, Writing - original draft, Writing - review & editing.
Declaration of Competing Interest
The authors report no conflicts of interest.
Footnotes
“Travelers” is the term used by participants to describe nurses contracted by US hospitals from an outside agency to temporarily fill staffing shortages. With only a few days of orientation, they are expected to immediately work in a functional capacity as a nurse and delivery safe care.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnurstu.2022.104256.
Appendix A. Supplementary data
Supplementary material
References
- Anders R.L., Lam S.C. COVID-19 experience in mainland China: nursing lessons for the United States of America. Nurs. Forum. 2021;56:439–443. doi: 10.1111/nuf.12546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Artiga S., Rae M., Pham O., Hamel L., Muñana C. 2020. COVID-19 Risks and Impacts among Health Care Workers by Race/Ethnicity | KFF. [Google Scholar]
- Azar K.M.J., Shen Z., Romanelli R.J., Lockhart S.H., Smits K., Robinson S., Brown S., Pressman A.R. Disparities in outcomes among COVID-19 patients in a large health care system in California. Health Aff. 2020;39:1253–1262. doi: 10.1377/HLTHAFF.2020.00598. [DOI] [PubMed] [Google Scholar]
- Baskin R.G., Bartlett R. Healthcare worker resilience during the COVID-19 pandemic: an integrative review. J. Nurs. Manag. 2021;29:2329–2342. doi: 10.1111/jonm.13395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benoit K. SAGE Handbook of Research Methods in Political Science and International Relations. Sage; London: 2020. Text as data: An overview; pp. 461–497. [Google Scholar]
- Bernstein L. Nurses are leaving staff jobs during covid and tripling salaries to travel - the Washington Post. 2021. https://www.washingtonpost.com/health/covid-travel-nurses/2021/12/05/550b15fc-4c71-11ec-a1b9-9f12bd39487a_story.html [WWW Document]. The Wash. Post URL. (accessed 12.21.21)
- Bethel C., Rainbow J.G., Dudding K.M. Recruiting nurses via social media for survey studies. Nurs. Res. 2021;70:231–235. doi: 10.1097/NNR.0000000000000482. [DOI] [PubMed] [Google Scholar]
- Bhandari N., Batra K., Upadhyay S., Cochran C. Impact of covid-19 on healthcare labor market in the United States: lower paid workers experienced higher vulnerability and slower recovery. Int. J. Environ. Res. Public Health. 2021;18 doi: 10.3390/ijerph18083894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blei D.M., Ng A.Y., Jordan M.I. Latent Dirichlet Allocation. J. Mach. Learn. Res. 2003:993–1022. https://www.jmlr.org/papers/volume3/blei03a/blei03a.pdf [Google Scholar]
- Bui D.P., McCaffrey K., Friedrichs M., LaCross N., Lewis N.M., Sage K., Barbeau B., Vilven D., Rose C., Braby S., Willardson S., Carter A., Smoot C., Winquist A., Dunn A. Racial and ethnic disparities among covid-19 cases in workplace outbreaks by industry sector — Utah, March 6–June 5, 2020. MMWR Morb. Mortal. Wkly Rep. 2020;69:1133–1138. doi: 10.15585/MMWR.MM6933E3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler C.R., Wong S.P.Y., Wightman A.G., O'Hare A.M. US clinicians' experiences and perspectives on resource limitation and patient care during the COVID-19 pandemic. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.27315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Card D., Tan C., Smith N.A. Proceedings of the 56th Annual Meeting of the Association for Computational Linguistics. 2018. Volume 1: long papers. [Google Scholar]
- Cavanagh S. Content analysis: concepts, methods and applications. Nurs. Res. 1997;4:5–16. doi: 10.7748/nr.4.3.5.s2. [DOI] [PubMed] [Google Scholar]
- Collins R. COVID-19: nurses have responded, now it is time to support them as we move forward. Healthc. Manag. Forum. 2020;33:190–194. doi: 10.1177/0840470420953297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Combe L.G. Reopening schools during COVID-19: school nurse ethical conflicts and moral dilemmas. NASN Sch. Nurs. (Print) 2020;35:308–312. doi: 10.1177/1942602X20963522. [DOI] [PubMed] [Google Scholar]
- Fairie P., Zhang Z., D'souza A.G., Walsh T., Quan H., Santana M.J. Categorising patient concerns using natural language processing techniques. BMJ Health Care Inform. 2021;28 doi: 10.1136/bmjhci-2020-100274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan W., Yan Z. Factors affecting response rates of the web survey: a systematic review. Comput. Hum. Behav. 2010;26:132–139. doi: 10.1016/J.CHB.2009.10.015. [DOI] [Google Scholar]
- Feyereisen S., Puro N. Seventeen states enacted executive orders expanding advanced practice nurses' scopes of practice during the first 21 days of the COVID-19 pandemic. Rural Remote Health. 2020;20:1–4. doi: 10.22605/RRH6068. [DOI] [PubMed] [Google Scholar]
- Fielding N.G., Lee R.M., Blank G. 2016. SAGE Handb. Online Res. Methods the SAGE Handbook of Online Research Methods. [DOI] [Google Scholar]
- Figueroa J.F., Wadhera R.K., Papanicolas I., Riley K., Zheng J., Orav E.J., Jha A.K. Association of nursing home ratings on health inspections, quality of care, and nurse staffing with COVID-19 cases. J. Am. Med. Assoc. 2020;324:1103–1105. doi: 10.1001/jama.2020.14709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Firew T., Sano E.D., Lee J.W., Flores S., Lang K., Salman K., Greene M.C., Chang B.P. Protecting the front line: a cross-sectional survey analysis of the occupational factors contributing to healthcare workers' infection and psychological distress during the COVID-19 pandemic in the USA. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2020-042752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fraher E.P., Pittman P., Frogner B.K., Spetz J., Moore J., Beck A.J., Armstrong D., Buerhaus P.I. Ensuring and sustaining a pandemic workforce. N. Engl. J. Med. 2020;382:2181–2183. doi: 10.1056/NEJMP2006376. [DOI] [PubMed] [Google Scholar]
- Gao X., Jiang L., Hu Y., Li L., Hou L. Nurses' experiences regarding shift patterns in isolation wards during the COVID-19 pandemic in China: a qualitative study. J. Clin. Nurs. 2020;29:4270–4280. doi: 10.1111/JOCN.15464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George E.K., Weiseth A., Edmonds J.K. Roles and experiences of registered nurses on labor and delivery units in the United States during the COVID-19 pandemic. J. Obstet. Gynecol. Neonatal. Nurs. 2021;50:742–752. doi: 10.1016/j.jogn.2021.08.096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gooch K. Record Number of Healthcare Workers Laid off, Furloughed during Pandemic [WWW Docu. Becker's Hospital Review URLment] 2020. https://www.beckershospitalreview.com/workforce/record-number-of-healthcare-workers-laid-off-furloughed-during-pandemic.html (accessed 1.13.21)
- Gorges R.J., Konetzka R.T. Staffing levels and COVID-19 cases and outbreaks in U.S. nursing homes. J. Am. Geriatr. Soc. 2020;68:2462–2466. doi: 10.1111/jgs.16787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray K., Dorney P., Hoffman L., Crawford A. Nurses' pandemic lives: a mixed-methods study of experiences during COVID-19. Appl. Nurs. Res. 2021;60 doi: 10.1016/j.apnr.2021.151437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimmer J., Stewart B.M. Text as data: the promise and pitfalls of automatic content analysis methods for political texts. Polit. Anal. 2013;21:267–297. doi: 10.1093/pan/mps028. [DOI] [Google Scholar]
- Grimmer J., Roberts M.E., Stewart B.M. 1st ed. Princeton University Press; Princeton: 2022. Text as Data: A New Framework for Machine Learning and the Social Sciences. [Google Scholar]
- Guo J.W., Sisler S.M., Wang C.Y., Wallace A.S. Exploring experiences of COVID-19-positive individuals from social media posts. Int. J. Nurs. Pract. 2021;27 doi: 10.1111/IJN.12986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardt Dicuccio M., Reynolds C., Snyder A., Cianci N. COVID-19: the nursing administration response. Crit. Care Nurs. Q. 2020;43:468–479. doi: 10.1097/CNQ.0000000000000330. [DOI] [PubMed] [Google Scholar]
- Harrington C., Ross L., Chapman S., Halifax E., Spurlock B., Bakerjian D. Nurse staffing and coronavirus infections in California nursing homes. Policy Politics Nurs. Pract. 2020;21:174–186. doi: 10.1177/1527154420938707. [DOI] [PubMed] [Google Scholar]
- Hennink M.M., Kaiser B.N., Marconi V.C. Code saturation versus meaning saturation: how many interviews are enough? Qual. Health Res. 2017;27:591–608. doi: 10.1177/1049732316665344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyle A., Goel P., Peskov D., Hian-Cheong A., Boyd-Graber J., Resnik P. 2021. Is Automated Topic Model Evaluation Broken?: The Incoherence of Coherence; pp. 1–16. (35th Conference on Neural Information Processing Systems). [Google Scholar]
- Hsieh H.-F., Shannon S.E. Three approaches to qualitative content analysis. Qual. Health Res. 2005;15:1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- Hughes M.M., Groenewold M.R., Lessem S.E., Xu K., Ussery E.N., Wiegand R.E., Qin X., Do T., Thomas D., Tsai S., Davidson A., Latash J., Eckel S., Collins J., Ojo M., McHugh L., Li W., Chen J., Chan J., Wortham J.M., Reagan-Steiner S., Lee J.T., Reddy S.C., Kuhar D.T., Burrer S.L., Stuckey M.J. Update: characteristics of health care personnel with COVID-19 — United States, February 12–July 16, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020;69:1364–1368. doi: 10.15585/mmwr.mm6938a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Im E.O., Sakashita R., Oh E.G., Tsai H.M., Chen C.M., Lin C.C., McCauley L. COVID-19 and nursing research across five countries/regions: commonalities and recommendations. Res. Nurs. Health. 2021;44:758–766. doi: 10.1002/nur.22171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isoaho K., Gritsenko D., Mäkelä E. Topic modeling and text analysis for qualitative policy research. Policy Stud. J. 2021;49:300–324. doi: 10.1111/PSJ.12343. [DOI] [Google Scholar]
- Jones C.D., Bowles K.H. Emerging challenges and opportunities for home health care in the time of COVID-19. J. Am. Med. Dir. Assoc. 2020;21:1517–1518. doi: 10.1016/j.jamda.2020.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kates J., Gerolamo A., Pogorzelska-Maziarz M. The impact of COVID-19 on the hospice and palliative care workforce. Public Health Nurs. 2021;38:459–463. doi: 10.1111/phn.12827. [DOI] [PubMed] [Google Scholar]
- Kelley M.M., Zadvinskis I.M., Miller P.S., Monturo C., Norful A.A., O'Mathúna D., Roberts H., Smith J., Tucker S., Zellefrow C., Chipps E. United States nurses' experiences during the COVID-19 pandemic: a grounded theory. J. Clin. Nurs. 2021 doi: 10.1111/jocn.16032. [DOI] [PubMed] [Google Scholar]
- Kelly L.M., Cordeiro M. 2020. Three Principles of Pragmatism for Research on Organizational Processes; p. 13. [DOI] [Google Scholar]
- Kim-Godwin Y., Lee M., Logan J.G., Liu X. Factors influencing sleep quality among female staff nurses during the early covid-19 pandemic in the United States. Int. J. Environ. Res. Public Health. 2021;18 doi: 10.3390/ijerph18094827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleinpell R., Myers C.R., Schorn M.N., Likes W. Impact of COVID-19 pandemic on APRN practice: results from a national survey. Nurs. Outlook. 2021;69:783–792. doi: 10.1016/J.OUTLOOK.2021.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kluger D.M., Aizenbud Y., Jaffe A., Parisi F., Aizenbud L., Minsky-Fenick E., Kluger J.M., Farhadian S., Kluger H.M., Kluger Y. Impact of healthcare worker shift scheduling on workforce preservation during the COVID-19 pandemic. Infect. Control Hosp. Epidemiol. 2020;41:1443–1445. doi: 10.1017/ice.2020.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Temkin-Greener H., Shan G., Cai X. COVID-19 infections and deaths among Connecticut nursing home residents: facility correlates. J. Am. Geriatr. Soc. 2020;68:1899–1906. doi: 10.1111/jgs.16689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu L., Tang L., Dong W., Yao S., Zhou W. An overview of topic modeling and its current applications in bioinformatics. SpringerPlus. 2016;5:1–22. doi: 10.1186/S40064-016-3252-8/TABLES/4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lobe B., Morgan D., Hoffman K.A. Qualitative data collection in an era of social distancing. Int. J Qual. Methods. 2020;19 doi: 10.1177/1609406920937875. [DOI] [Google Scholar]
- Mackey K., Ayers C.K., Kondo K.K., Saha S., Advani S.M., Young S., Spencer H., Rusek M., Anderson J., Veazie S., Smith M., Kansagara D. Racial and ethnic disparities in covid-19-related infections, hospitalizations, and deaths a systematic review. Ann. Intern. Med. 2021;174:362–373. doi: 10.7326/M20-6306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews K.L., Baird M., Duchesne G. Using online meeting software to facilitate geographically dispersed focus groups for health workforce research. Qual. Health Res. 2018;28:1621–1628. doi: 10.1177/1049732318782167. [DOI] [PubMed] [Google Scholar]
- McGilton K.S., Escrig-Pinol A., Gordon A., Chu C.H., Zúñiga F., Sanchez M.G., Boscart V., Meyer J., Corazzini K.N., Jacinto A.F., Spilsbury K., Backman A., Scales K., Fagertun A., Wu B., Edvardsson D., Lepore M.J., Leung A.Y.M., Siegel E.O., Noguchi-Watanabe M., Wang J., Bowers B. Uncovering the devaluation of nursing home staff during COVID-19: are we fuelling the next health care crisis? J. Am. Med. Dir. Assoc. 2020;21:962–965. doi: 10.1016/j.jamda.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meeks E., Weingart S.B. The digital humanities contribution to topic modeling journal of digital humanities. J. Digit. Humanit. 2012;2 [Google Scholar]
- Mohr J.W., Bogdanov P. Introduction—topic models: what they are and why they matter. Poetics. 2013;41:545–569. doi: 10.1016/J.POETIC.2013.10.001. [DOI] [Google Scholar]
- Morgan D.L. Qualitative content analysis: a guide to paths not taken. Qual. Health Res. 1993;3:112–121. doi: 10.1177/104973239300300107. [DOI] [PubMed] [Google Scholar]
- National Academy of Medicine . National Academies Press; Washington, D.C.: 2021. The Future of Nursing 2020–2030: Charting a Path to Achieve Health Equity, the Future of Nursing 2020–2030. [DOI] [PubMed] [Google Scholar]
- Norman S.B., Feingold J.H., Kaye-Kauderer H., Kaplan C.A., Hurtado A., Kachadourian L., Feder A., Murrough J.W., Charney D., Southwick S.M., Ripp J., Peccoralo L., Pietrzak R.H. Moral distress in frontline healthcare workers in the initial epicenter of the COVID-19 pandemic in the United States: relationship to PTSD symptoms, burnout, and psychosocial functioning. Depress. Anxiety. 2021;38:1007–1017. doi: 10.1002/da.23205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Reilly-Jacob M., Perloff J. The effect of supervision waivers on practice: a survey of Massachusetts nurse practitioners during the COVID-19 pandemic. Med. Care. 2021;59:283–287. doi: 10.1097/MLR.0000000000001486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton M.Q. SAGE Publications, Inc.; 2015. Qualitative Research and Evaluation Methods: Theory and Practice; p. 832. [Google Scholar]
- Raso R., Fitzpatrick J.J., Masick K. Nurses' intent to leave their position and the profession during the COVID-19 pandemic. J. Nurs. Admin. 2021;51:488–494. doi: 10.1097/NNA.0000000000001052. [DOI] [PubMed] [Google Scholar]
- Reisner S.L., Randazzo R.K., White Hughto J.M., Peitzmeier S., DuBois L.Z., Pardee D.J., Marrow E., McLean S., Potter J. Sensitive health topics with underserved patient populations: methodological considerations for online focus group discussions. Qual. Health Res. 2018;28:1658–1673. doi: 10.1177/1049732317705355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts M.E., Stewart B.M., Tingley D., Lucas C., Leder-Luis J., Kushner Gadarian S., Albertson B., Rand D.G. Structural topic models for open-ended survey responses. Am. J. Polit. Sci. 2014;58:1064–1082. [Google Scholar]
- Rodriguez F., Solomon N., de Lemos J.A., Das S.R., Morrow D.A., Bradley S.M., Elkind M.S.V., Williams J.H., Holmes D.J., Matsouaka R.A., Gupta D., Gluckman T.J., Abdalla M., Albert M.A., Yancy C.W., Wang T.Y. Racial and ethnic differences in presentation and outcomes for patients hospitalized with COVID-19: findings from the american heart association's COVID-19 cardiovascular disease registry. Circulation. 2021:2332–2342. doi: 10.1161/CIRCULATIONAHA.120.052278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rollison S., Horvath C., Gardner B., McAuliffe M., Benson A. Redeployment of certified registered nurse anesthetists during the coronavirus disease 2019 pandemic. AANA J. 2021;89:133–139. [PubMed] [Google Scholar]
- Salmons J. Cases in online interview research. Cases Online Interview Res. 2015 doi: 10.4135/9781506335155. [DOI] [Google Scholar]
- Salmons J. Doing Qualitative Research Online. 1st ed. SAGE Publications Ltd; London: 2016. Doing qualitative research online. [DOI] [Google Scholar]
- Sharma M., Creutzfeldt C.J., Lewis A., Patel P.V., Hartog C., Jannotta G.E., Blissitt P., Kross E.K., Kassebaum N., Greer D.M., Curtis J.R., Wahlster S. Health-care professionals' perceptions of critical care resource availability and factors associated with mental well-being during coronavirus disease 2019 (COVID-19): results from a US survey. Clin. Infect. Dis.: an official publication of the Infectious Diseases Society of America. 2021;72:e566–e576. doi: 10.1093/cid/ciaa1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shinners J., Cosme S. COVID-19: perspectives from nurses across the country. J. Contin. Educ. Nurs. 2020;51:304–308. doi: 10.3928/00220124-20200611-05. [DOI] [PubMed] [Google Scholar]
- Simonovich S.D., Spurlark R.S., Badowski D., Krawczyk S., Soco C., Ponder T.N., Rhyner D., Waid R., Aquino E., Lattner C., Wiesemann L.M., Webber-Ritchey K., Li S., Tariman J.D. Examining effective communication in nursing practice during COVID-19: a large-scale qualitative study. Int. Nurs. Rev. 2021;68:512–523. doi: 10.1111/inr.12690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smiley R.A., Ruttinger C., Oliveira C.M., Hudson L.R., Allgeyer R., Reneau K.A., Silvestre J.H., Alexander M. The 2020 National Nursing Workforce Survey. J. Nurs. Reg. 2021;12:S1–S96. doi: 10.1016/S2155-8256(21)00027-2. [DOI] [Google Scholar]
- Surdam J., Daly B., Fulton S., Margevicius S., Schluchter M., Flocke S., Manne S., Meropol N.J. Recruitment strategies for nurse enrollment in an online study. Nurs. Res. 2020;69:69–73. doi: 10.1097/NNR.0000000000000393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahlster S., Sharma M., Lewis A.K., Patel P.V., Hartog C.S., Jannotta G., Blissitt P., Kross E.K., Kassebaum N.J., Greer D.M., Curtis J.R., Creutzfeldt C.J. The coronavirus disease 2019 pandemic's effect on critical care resources and health-care providers: a global survey. Chest. 2021;159:619–633. doi: 10.1016/j.chest.2020.09.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood E., King R., Senek M., Robertson S., Taylor B., Tod A., Ryan A. UK advanced practice nurses' experiences of the COVID-19 pandemic: a mixed-methods cross-sectional study. BMJ Open. 2021;11 doi: 10.1136/BMJOPEN-2020-044139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu H., Intrator O., Bowblis J.R. Shortages of staff in nursing homes during the COVID-19 pandemic: what are the driving factors? J. Am. Med. Dir. Assoc. 2020;21:1371–1377. doi: 10.1016/j.jamda.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ying L., Montgomery J.M., Stewart B.M. Topics, concepts, and measurement: a crowdsourced procedure for validating topics as measures. Polit. Anal. 2021:1–20. doi: 10.1017/PAN.2021.33. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material