Abstract
Background:
Disparities in outcomes of adult sepsis are well described by insurance status and race/ethnicity. There are limited data looking at disparities in sepsis outcomes in children. We investigated whether disparities in outcome of sepsis occur according to a child’s race/ethnicity or insurance type.
Methods:
We performed a population-based retrospective cohort study in the United States. Using multilevel logistic regression, clustered by hospital we tested the association of race/ethnicity and insurance status with hospital mortality adjusting for individual and hospital level characteristics. The secondary outcome of length of stay was examined through multilevel time to event (hospital discharge) regression, with death as a competing risk.
Findings:
9,816 children with sepsis were included. Black children had higher odds of death than White children (adjusted OR = 1·19, 95 % CI 1·02–1·38; p = 0·028), driven by higher Black mortality in the South (aOR 1·30, 95% CI 1·04–1·62; p = 0·019) and West (aOR 1·58, 95% CI 1·05–2·38; p = 0·027) of the country. There was evidence of longer hospital stays in Hispanic and Black children, particularly Black neonates. There was no difference in survival between publicly and privately insured children; however, other insurance status (self-pay, no charge, and other) was associated with increased mortality (aOR 1·30, 95% CI 1·04–1·61; p = 0·021).
Interpretation:
In this large representative analysis of pediatric severe sepsis in the United States, we found evidence of outcome disparity by race/ethnicity and insurance status. Our findings suggest that there may be differential sepsis recognition, approaches to treatment, access to health care service, and/or provider bias that contribute to poorer outcomes from sepsis for minority patients and those of lower socioeconomic position. Studies are warranted to investigate the mechanisms of worse outcomes in Black and Hispanic children.
Funding:
Nadir Yehya is supported by National Institutes of Health (NIH) grant number K23-HL136688.
Introduction:
Sepsis is a leading cause of morbidity and mortality in children globally.1 In the United States (US), prevalence estimates of severe sepsis and septic shock in hospitalised children range from 1–26%, with an estimated inpatient mortality ranging from 10 to 20%.1,2 National healthcare costs of pediatric sepsis were an estimated $7·31 billion in 2016.3
Despite improvements in care delivery, disparities in incidence and outcome from sepsis persist in adults, both by socioeconomic position and race/ethnicity.4 Rates of sepsis in adults are higher in high poverty areas,5 with increased risk of death in uninsured patients.6 Studies focused on race and ethnicity have shown nearly double the incidence of sepsis in Black and Hispanic patients, compared to White, with persistent difference after adjusting for chronic illness and neighborhood privation.5,7 Black and Hispanic patients tended to present with sepsis at a younger age.5,8 There is strong evidence of racial disparities in survival, with Black patients aged 18 to 65 years being twice as likely to die of sepsis than White patients.8 Black patients with severe sepsis were less likely than White patients to be cared for in the intensive care unit (ICU), however once admitted to the ICU they had higher case fatality.5 There was also evidence of longer hospital length of stay in Black patients as compared to White.7
Disparities in disease outcomes between different racial/ethnic and socioeconomic groups have been described across a range of pediatric conditions. Literature looking specifically at disparities in survival of pediatric sepsis by race/ethnicity and socioeconomic position is sparse, with little published data outside of the neonatal period.9–11 Therefore, using a large hospital discharge database, we aimed to determine whether disparities in outcome from childhood severe sepsis were associated with race/ethnicity and insurance status. We hypothesised that non-White children would have higher rates of mortality and longer length of hospital stay compared to White children and that public insurance would be associated with higher mortality.
Methods:
Design
This is a population-based retrospective cohort study, using data from the 2016 database release from the Healthcare Cost and Utilization Project (HCUP) Kids’ Inpatient Database (KID). This study analysed de-identified, publicly available data. The Children’s Hospital of Philadelphia Institutional Review Board reviewed the protocol, and determined that ethical approval and IRB oversight was not required.
Setting
The 2016 KID included 3,117,413 discharges which accounts for 80% of national pediatric discharges from 4,200 U.S. hospitals across 47 states.12
Participants
We included patients aged 0–20 years with a diagnosis of severe sepsis in 2016. Children at the upper limit of this age group are commonly managed in pediatric floors, hospitals, and ICUs, particularly if they have comorbidities; hence the decision to include patients up to 20 years old.
We used International Classification of Diseases, Tenth Revision, Clinical Modification codes to identify patients admitted with severe sepsis without septic shock (R65·20) and severe sepsis with septic shock (R65·21).13 Subjects with missing data on one of the primary exposures (race/ethnicity or insurance type) were excluded. Children transferred out to a different hospital were also excluded as they could not experience the primary outcome and to ensure they were not included twice in the analysis.
Variables
The co-primary exposures were race/ethnicity and insurance status. Race and ethnicity are reported to KID by hospitals as a single variable. If a hospital provides both race and ethnicity, ethnicity takes precedence over race as the reported variable. This variable is subdivided in KID as White, Black, Hispanic, Asian and Pacific Islander, Native American, and other. Insurance status is subdivided as Medicare, Medicaid, private insurance, self-pay, no charge, and other.
For our analysis, race/ethnicity exposures were grouped into White, Black, Hispanic and other (Asian and Pacific Islander, Native American, and other). Insurance status was grouped into public (Medicaid and Medicare), private and other (self-pay, no charge, and other). Groupings were justified based on concerns that self-pay, no charge, and other were too small a group to be analysed individually.
The primary outcome was death prior to discharge. The secondary outcome was length of hospital stay with death as a competing risk, censored at day 30.
Available patient characteristics were age, sex, presence of any of ten complex chronic conditions as defined by Feudtner,14 and median household income for patient’s zip code (subdivided by KID into quartiles with 1 being lowest and 4 being highest). Characteristics related to the admission included whether the patient was admitted on weekday or weekend, admitted through the emergency department (ED), admitted electively, or transferred in, and in what quarter of the year the admission occurred. Available hospital level characteristics were hospital size (small, medium, or large), rural or urban location, teaching hospital status, and hospital control (government or private). Geographic location was subdivided by KID into Northeast, Midwest, South, and West. All the above variables were included in the multivariate analyses.
Power analysis
Assuming a mortality of 16·9%,1 to detect 1·2 times odds of death in Black and Hispanic children compared to White children with 80% power and 0·05 significance, a sample size of 7,959 would be needed.
Analysis
All analyses were performed with hospital sampling weights, per HCUP guidance.12 Baseline characteristics of the cohort were described. Univariate association with hospital mortality was done using mixed effects logistic regression, clustered by hospital, to calculate crude odds of mortality and 95% confidence intervals for each of the available variables. Likelihood ratio tests were done to look for an overall association of each variable with mortality. For the multivariate analysis, multilevel causal mixed effects logistic regression models were constructed, clustered by hospital. Results are presented as adjusted odds ratios (aOR) interpreted as within-hospital effects (i.e., aOR for a Black patient relative to a White patient admitted to the same hospital).
For the secondary outcome of hospital length of stay, a multilevel mixed effects competing risk regression model was constructed with hospital length of stay as the outcome of interest and death as a competing event. Length of stay was censored at 30 days, making this outcome comparable to discharge alive or hospital-free days by 30 days. Results are presented as adjusted hazard ratios (aHR).
Pre-planned interaction tests were performed looking for any evidence of modification of the effect of race/ethnicity by either insurance status, median household income by zip code, or hospital region. As these were exploratory analyses, we used a threshold of p < 0·05 for interaction terms without correction of multiple comparisons.
Given the substantial evidence of neonatal disparities,15 a planned secondary analysis was repeated restricted to patients flagged by KID as neonates on admission (first 28 days after birth indicator).
Finally, to test the possibility of residual confounding of between-hospital effects of race/ethnicity, we performed an analysis to explicitly disentangle within- and between-hospital effects of race/ethnicity. A variable was created showing what proportion of patients treated at a hospital were Black. To create this variable, we started with all 3,117,413 discharges. Hospitals treating fewer than 100 patients were excluded, and the proportion of Black patients being treated at a hospital was calculated and ordered into quintiles, with 1 being hospitals treating the lowest proportion of Black patients and 5 being the highest. We then added this variable to the multilevel models for mortality and length of stay.
The dataset was examined for missing data. Overall amount of missing data for the exposure variables was judged to be small and unlikely to alter final results, so patients missing data on key exposures were excluded from the final analysis. Analyses were done using Stata version 15 (StataCorp, College Station, Texas, USA).
There was no funding source and the corresponding author had full access to all of the data and the final responsibility to submit for publication.
Results
Description of cohort
A total of 12,297 patients with sepsis were admitted to 1,253 hospitals in the 2016 KID dataset. 1,265/12,297 (10·3%) patients did not have a race/ethnicity recorded, 15/12,297 (0·1%) children were missing data on insurance and 1,324/12,297 children were transferred out of the hospital, leaving a final cohort of 9,816 (Fig 1, Tables 1 and 2).
Figure 1:
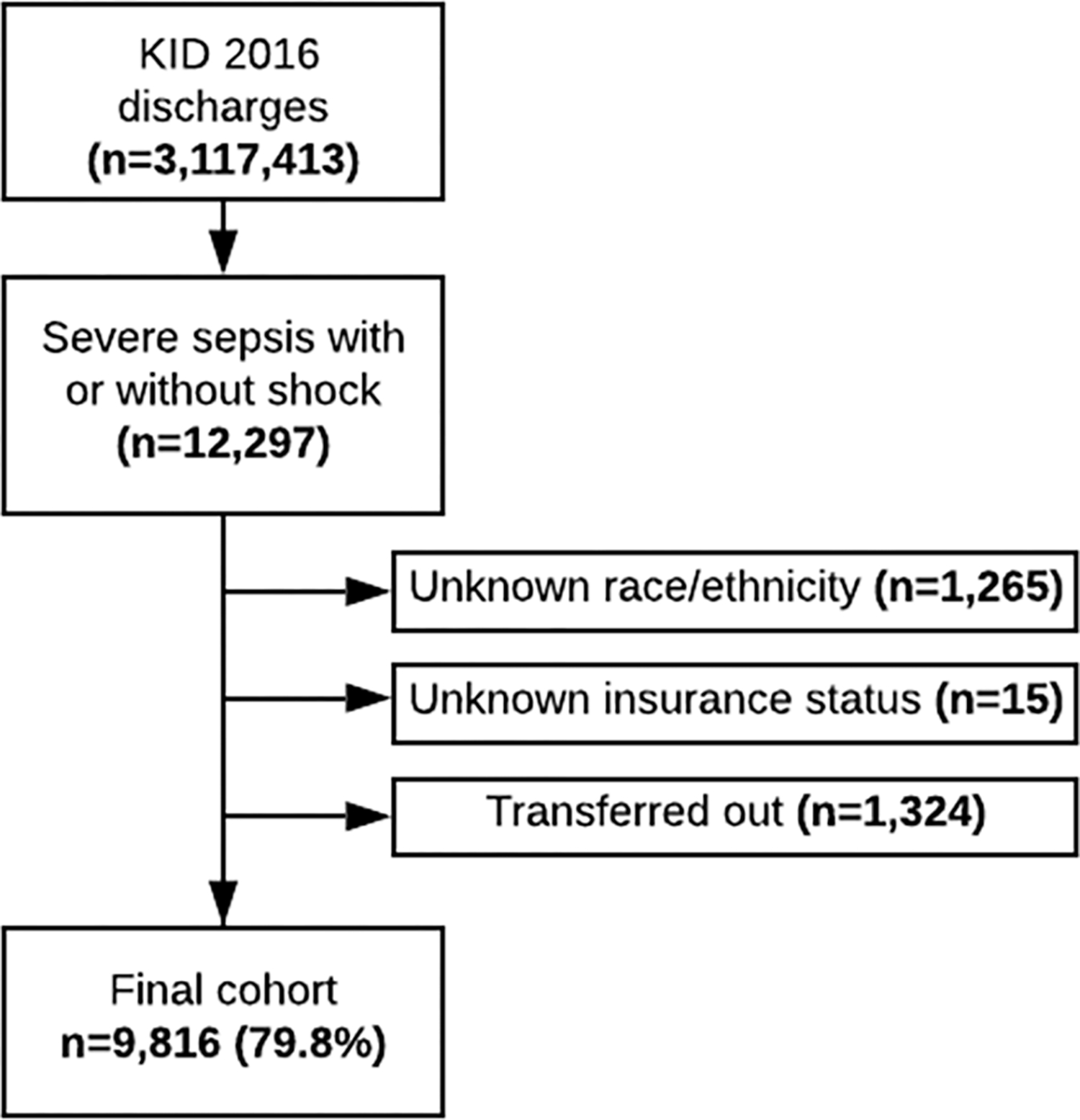
Flow chart of sample size
*numbers add to over 100% as some patients missing data for multiple variables
Table 1:
Characteristics of cohort (by race/ethnicity) n=9,816 (excluding any patients missing information on race/ethnicity, insurance status, or transferred out)
| White | Black | Hispanic | Other | Total | P value a | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| N. | % | N. | % | N. | % | N. | % | N. | % | |||
|
| ||||||||||||
| Age (years) | 0 | 880 | 18·9 | 444 | 26·8 | 499 | 19·9 | 249 | 25·3 | 2,072 | 21·1 | <0·001 |
| 1–5 | 681 | 14·6 | 234 | 14·1 | 402 | 16·1 | 180 | 18·3 | 1,497 | 15·3 | ||
| 6–12 | 757 | 16·2 | 265 | 16·0 | 515 | 20·6 | 168 | 17·0 | 1,705 | 17·4 | ||
| 13–17 | 931 | 19·9 | 275 | 16·6 | 480 | 19·2 | 143 | 14·5 | 1,829 | 18·6 | ||
| 18–20 | 1,419 | 30·4 | 440 | 26·5 | 608 | 24·3 | 246 | 25·0 | 2,713 | 27·6 | ||
|
| ||||||||||||
| Sex | Male | 2,239 | 48·0 | 768 | 46·3 | 1,214 | 48·5 | 490 | 49·7 | 4,711 | 48·0 | 0·35 |
| Female | 2,427 | 52·0 | 890 | 53·7 | 1,289 | 51·5 | 496 | 50·3 | 5,102 | 52·0 | ||
|
| ||||||||||||
| Complex chronic condition | No | 1,351 | 28·9 | 366 | 22·1 | 631 | 25·2 | 261 | 26·5 | 2,609 | 26·6 | <0·001 |
| Yes | 3,317 | 71·1 | 1,292 | 77·9 | 1,873 | 74·8 | 725 | 73·5 | 7,207 | 73·4 | ||
|
| ||||||||||||
| Payer | Medicare | 46 | 1·0 | 28 | 1·7 | 18 | 0·7 | 10 | 1·0 | 102 | 1·0 | <0·001 |
| Medicaid | 1,889 | 40·5 | 1,137 | 68·6 | 1,722 | 68·8 | 535 | 54·3 | 5,283 | 53·8 | ||
| Private insurance | 2,420 | 51·8 | 379 | 22·9 | 510 | 20·4 | 361 | 36·6 | 3,670 | 37·4 | ||
| Self-Pay | 120 | 2·6 | 48 | 2·9 | 100 | 4·0 | 30 | 3·0 | 298 | 3·0 | ||
| No Charge | 11 | 0·2 | 3 | 0·2 | 4 | 0·2 | 3 | 0·3 | 21 | 0·2 | ||
| Other | 182 | 3·9 | 63 | 3·8 | 150 | 6·0 | 47 | 4·8 | 442 | 4·5 | ||
|
| ||||||||||||
| Median Household Income for patient’s zip code | $0 - $42,999 | 1,103 | 24·1 | 863 | 52·9 | 1,025 | 41·5 | 275 | 28·7 | 3,266 | 33·9 | <0·001 |
| $43,000 - $53,999 | 1,182 | 25·8 | 336 | 20·6 | 592 | 24·0 | 183 | 19·1 | 2,293 | 23·8 | ||
| $54,000 - $70,999 | 1,204 | 26·3 | 261 | 16·0 | 544 | 22·0 | 247 | 25·8 | 2,256 | 23·4 | ||
| $71,000+ | 1,094 | 23·9 | 170 | 10·4 | 309 | 12·5 | 253 | 26·4 | 1,826 | 18·9 | ||
|
| ||||||||||||
| Hospital region | Northeast | 732 | 15·7 | 275 | 16·6 | 291 | 11·6 | 228 | 23·1 | 1,526 | 15·6 | <0·001 |
| Midwest | 1,346 | 28·8 | 387 | 23·3 | 212 | 8·5 | 139 | 14·1 | 2,084 | 21·2 | ||
| South | 1,666 | 35·7 | 825 | 49·8 | 913 | 36·5 | 249 | 25·3 | 3,653 | 37·2 | ||
| West | 924 | 19·8 | 171 | 10·3 | 1,088 | 43·5 | 370 | 37·5 | 2,553 | 26·0 | ||
|
| ||||||||||||
| Hospital location | Rural | 97 | 2·1 | 14 | 0·8 | 8 | 0·3 | 9 | 0·9 | 128 | 1·3 | <0·001 |
| Urban nonteaching | 437 | 9·4 | 100 | 6·0 | 280 | 11·2 | 74 | 7·5 | 891 | 9·1 | ||
| Urban teaching | 4,134 | 88·6 | 1,544 | 93·1 | 2,216 | 88·5 | 903 | 91·6 | 8,797 | 89·6 | ||
|
| ||||||||||||
| Hospital control | Government, nonfederal | 486 | 10·4 | 243 | 14·7 | 266 | 10·6 | 104 | 10·6 | 1,099 | 11·2 | <0·001 |
| Private, not-profit | 3,864 | 82·8 | 1,269 | 76·5 | 1,980 | 79·1 | 814 | 82·6 | 7,927 | 80·8 | ||
| Private, invest-own | 318 | 6·8 | 146 | 8·8 | 258 | 10·3 | 68 | 6·9 | 790 | 8·1 | ||
|
| ||||||||||||
| Outcome | Mortality (%) | 627 | 13·4 | 305 | 18·4 | 342 | 13·7 | 158 | 16·0 | 1,432 | 14·6 | <0·001 |
|
|
||||||||||||
| Median | (IQR) | Median | (IQR) | Median | (IQR) | Median | (IQR) | Median | (IQR) | |||
|
|
||||||||||||
| Length of stay (all) | 8 | (4–18) | 10 | (5–24) | 10 | (4–23) | 10 | (5–22) | 9 | (4–21) | ||
| Length of stay (survivors) | 8 | (4–17) | 11 | (5–22) | 9 | (5–21) | 9 | (5–21) | 9 | (4–19) | ||
Chi squared test, or ANOVA on ranks
Table 2:
Characteristics of cohort (by insurance status) n=9,816 (excluding any patients missing information on race/ethnicity, insurance status, or transferred out)
| Public | Private | Other | Total | P value a | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| N. | % | N. | % | N. | % | N. | % | |||
|
| ||||||||||
| Age (years) | 0 | 1,284 | 23·8 | 650 | 17·7 | 138 | 18·1 | 2,072 | 21·1 | <0·001 |
| 1–5 | 921 | 17·1 | 465 | 12·7 | 111 | 14·6 | 1,497 | 15·3 | ||
| 6–12 | 1,004 | 18·6 | 603 | 16·4 | 98 | 12·9 | 1,705 | 17·4 | ||
| 13–17 | 894 | 16·6 | 815 | 22·2 | 120 | 15·8 | 1,829 | 18·6 | ||
| 18–20 | 1,282 | 23·8 | 1,137 | 31·0 | 294 | 38·6 | 2,713 | 27·6 | ||
|
| ||||||||||
| Sex | Male | 2,634 | 48·9 | 1,744 | 47·5 | 333 | 43·8 | 4,711 | 48·0 | 0·022 |
| Female | 2,749 | 51·1 | 1,925 | 52·5 | 428 | 56·2 | 5,102 | 52·0 | ||
|
| ||||||||||
| Complex chronic condition | No | 1,355 | 25·2 | 1,043 | 28·4 | 211 | 27·7 | 2,609 | 26·6 | 0·002 |
| Yes | 4,030 | 74·8 | 2,627 | 71·6 | 550 | 72·3 | 7,207 | 73·4 | ||
|
| ||||||||||
| Race | White | 1,935 | 35·9 | 2,420 | 65·9 | 313 | 41·1 | 4,668 | 47·6 | <0·001 |
| Black | 1,165 | 21·6 | 379 | 10·3 | 114 | 15·0 | 1,658 | 16·9 | ||
| Hispanic | 1,740 | 32·3 | 510 | 13·9 | 254 | 33·4 | 2,504 | 25·5 | ||
| Asian/Pacific Islander | 173 | 3·2 | 176 | 4·8 | 32 | 4·2 | 381 | 3·9 | ||
| Native American | 88 | 1·6 | 18 | 0·5 | 4 | 0·5 | 110 | 1·1 | ||
| Other | 284 | 5·3 | 167 | 4·6 | 44 | 5·8 | 495 | 5·0 | ||
|
| ||||||||||
| Median Household Income for zip code | $0 - $42,999 | 2,339 | 44·1 | 712 | 19·7 | 215 | 29·5 | 3,266 | 33·9 | <0·001 |
| $43,000 - $53,999 | 1,341 | 25·3 | 758 | 21·0 | 194 | 26·7 | 2,293 | 23·8 | ||
| $54,000 - $70,999 | 1,053 | 19·9 | 1,007 | 27·9 | 196 | 26·9 | 2,256 | 23·4 | ||
| $71,000+ | 571 | 10·8 | 1,132 | 31·4 | 123 | 16·9 | 1,826 | 18·9 | ||
|
| ||||||||||
| Hospital region | Northeast | 825 | 15·3 | 638 | 17·4 | 63 | 8·3 | 1,526 | 15·6 | <0·001 |
| Midwest | 1,091 | 20·3 | 874 | 23·8 | 119 | 15·6 | 2,084 | 21·2 | ||
| South | 2,075 | 38·5 | 1,263 | 34·4 | 315 | 41·4 | 3,653 | 37·2 | ||
| West | 1,394 | 25·9 | 895 | 24·4 | 264 | 34·7 | 2,553 | 26·0 | ||
|
| ||||||||||
| Hospital location | Rural | 72 | 1·3 | 45 | 1·2 | 11 | 1·5 | 128 | 1·3 | <0·001 |
| Urban nonteaching | 432 | 8·0 | 354 | 9·7 | 105 | 13·8 | 891 | 9·1 | ||
| Urban teaching | 4,881 | 90·6 | 3,271 | 89·1 | 645 | 84·8 | 8,797 | 89·6 | ||
|
| ||||||||||
| Hospital control | Government, nonfederal | 680 | 12·6 | 321 | 8·8 | 98 | 12·9 | 1,099 | 11·2 | <0·001 |
| Private, not-profit | 4,259 | 79·1 | 3,083 | 84·0 | 585 | 76·9 | 7,927 | 80·8 | ||
| Private, invest-own | 446 | 8·3 | 266 | 7·3 | 78 | 10·3 | 790 | 8·1 | ||
|
| ||||||||||
| Outcome | Mortality (%) | 806 | 15·0 | 506 | 13·8 | 120 | 15·8 | 1,432 | 14·6 | 0·19 |
|
|
||||||||||
| Median | (IQR) | Median | (IQR) | Median | (IQR) | Median | (IQR) | |||
|
|
||||||||||
| Length of stay (all) | 10 | (5–22) | 8 | (4–18) | 8 | (4–19) | 9 | (4–21) | ||
| Length of stay (survivors) | 10 | (5–21) | 8 | (4–17) | 8 | (4–17) | 9 | (4–19) | ||
Chi squared test or ANOVA on ranks
Most patients (54·8%) were publicly insured. The most common race/ethnicity was White (47·6%), followed by Hispanic (25·5%), and then Black (16·9%). There was a strong association between race/ethnicity and socioeconomic position. More White children were privately insured than Black or Hispanic (51·8% vs 22·9% and 20·4%, respectively; p < 0·001). Fewer White children lived in zip codes with the lowest quartile median income compared to Black and Hispanic children (24·1% vs 52·9% and 41·5%, respectively; p < 0·001).
Overall prevalence of chronic complex conditions in the cohort was high (73·4%), however a higher proportion of Black and Hispanic children had a complex chronic condition compared to White children (p < 0·001) (Tables 1 and 2; Supplementary Table 1).
Univariate analysis
Overall mortality was 14·6%. Black children experienced significantly higher mortality than White or Hispanic children (p < 0·001; Supplementary Table 1). In univariate analysis Black race/ethnicity was associated with increased mortality compared to White (OR 1·37, 95% CI 1·19–1·58; p < 0·0001; Table 3). Hispanic children had similar odds of death to White children. There was no association between insurance status and mortality in univariate analysis (p = 0·26; Table 4).
Table 3:
Crude and adjusted odds ratios of death and length of stay (hazard ratios for discharge alive by 30 days)a in children (aged 0–20) with severe sepsis in 2016 by race/ethnicity, clustered by hospital
| Odds of death | Hazard for discharge alive by 30 days | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| (n=9,816) | (n=9,594) | (n=9,581) | ||||||||
| OR | 95% CI | P value b | aORc | 95% CI | P value d | aHR | 95% CI | P value d | ||
| Race | White | 1 | ref | 1 | 1 | |||||
| Black | 1·37 | (1·19–1·58) | 1·19 | (1·02–1·38) | 0·028 | 0·88 | (0·82–0·94) | <0·001 | ||
| Hispanic | 0·97 | (0·85–1·12) | 0·96 | (0·82–1·11) | 0·55 | 0·94 | (0·88–1·00) | 0·049 | ||
| Other | 1·17 | (0·98–1·40) | <0·0001 | 1·03 | (0·86–1·25) | 0·72 | 0·97 | (0·89–1·04) | 0·38 | |
A hazard ratio less than one is indicative of a lower probability of discharge by 30 days i.e. a longer length of stay.
LR test p-value
Adjusted for other variables in the table and sex, age, median household income for patient’s zip code, elective admission, admitted from emergency department, transferred in, admitted at weekend, admission quarter, hospital bed size, hospital region, hospital control, hospital teaching status, presence of complex chronic condition·
Wald test-p-value
intra-class correlation: 0.076 variance of the random effects
Table 4:
Crude and adjusted odds ratios of death and length of stay (hazard ratios for discharge alive by 30 days)a in children (aged 0–20) with severe sepsis in 2016 by insurance status, clustered by hospital
| Odds of death | Hazard for discharge alive by 30 days | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| (n=9,816) | (n=9,594) | (n=9,581) | ||||||||
| OR | 95% CI | P value b | aOR c | 95% CI | P value d | aHR cb | 95% CI | P value d | ||
| Payer | Public insurance | 1 | ref | 1 | 1 | |||||
| Private insurance | 0·94 | (0·84–1·05) | 1·09 | (0·96–1·23) | 0·19 | 1·03 | (0·98–1·08) | 0·24 | ||
| Other | 1·10 | (0·90–1·34) | 0·26 | 1·30 | (1·04–1·61) | 0·021 | 1·00 | (0·92–1·10) | 0·92 | |
A hazard ratio less than one is indicative of a lower probability of discharge by 30 days ie a longer length of stay.
LR test p-value
Adjusted for other variables in the table and sex, age, median household income for patient’s zip code, elective admission, admitted from emergency department, transferred in, admitted at weekend, admission quarter, hospital bed size, hospital region, hospital control, hospital teaching status, presence of complex chronic condition.
Wald test-p-value
intra-class correlation: 0.076
Children with a chronic complex condition had seven-fold increased odds of death compared to children without a chronic complex condition (p < 0·0001; Supplementary Table 1). Males had increased odds of death compared to females (OR 1·28, 95% CI 1·16–1·42; p = 0·0001). Mortality decreased with increasing age, with highest mortality observed in children less than 1 year of age (p < 0·0001; Supplementary Table 2).
Multivariate analysis
In the multivariable analysis Black race remained associated with higher mortality (aOR 1·19, 95% CI 1·02–1·38; p = 0·028; Table 3), relative to White. Hispanic children continued to have similar mortality to White (p = 0·55; Table 3). The variables that most attenuated the association between Black race and mortality were presence of chronic complex condition, age, and hospital region. Other insurance was associated with increased mortality in multivariable analysis (aOR 1·30, 95% CI 1·04–1·61; p = 0·021; Table 4).
Black and Hispanic children had evidence of longer hospital stays than White children. With death accounted for as a competing risk, both Black and Hispanic children were less likely to be discharged alive from hospital by 30 days (aHR for discharge alive for Black children 0·88, 95% CI 0·82–0·94; p = 0·001; aHR for Hispanic children 0·94, 95% CI 0·88–1·00; p = 0·049; Table 3). There was no difference in length of hospital stay by insurance status (Table 4).
Stratified analysis
There was no evidence of interaction between race/ethnicity and insurance status (p = 0·32) or between race/ethnicity and median household income by zip code (p = 0·16). There was strong evidence of interaction between race/ethnicity and hospital region (p < 0·001). Therefore, results were stratified by geographic region and re-analysed (Table 5). Highest odds of mortality in Black children were observed in the West of the country, where Black children had nearly 60% higher odds of mortality compared to White children; odds were 30% higher in the South. There was also evidence of longer hospital stays for both Black and Hispanic children in the South and West of the US (Table 5).
Table 5:
Crude and adjusted odds ratios of death and length of stay (hazard ratios for discharge alive by 30 days)a in children (aged 0–20) with severe sepsis in 2016 by race/ethnicity, clustered by hospital stratified by geographic area
| Odds of death | Hazard for discharge alive by 30 days | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P value b | aOR c | 95% CI | P value d | aHRc | 95% CI | P value d | ||
| Northeast (n=1,526) | White | 1 | 1 | 1 | ||||||
| Black | 1·02 | (0·72–1·46) | 0·75 | (0·49–1·15) | 0·18 | 1·08 | (0·91–1·29) | 0·36 | ||
| Hispanic | 0·74 | (0·50–1·08) | 0·65 | (0·42–1·02) | 0·058 | 1·12 | (0·95–1·33) | 0·17 | ||
| Other | 1·05 | (0·71–1·55) | 0·37 | 0·76 | (0·48–1·20) | 0·23 | 1·24 | (1·04–1·48) | 0·014 | |
|
| ||||||||||
| Midwest (n=2,084) | White | 1 | 1 | 1 | ||||||
| Black | 1·01 | (0·74–1·39) | 0·97 | (0·68–1·38) | 0·85 | 0·91 | (0·79–1·05) | 0·19 | ||
| Hispanic | 1·33 | (0·90–1·97) | 1·26 | (0·84–1·91) | 0·27 | 1·04 | (0·87–1·23) | 0·67 | ||
| Other | 2·25 | (1·52–3·33) | 0·0005 | 1·79 | (1·15–2·77) | 0·010 | 0·80 | (0·65–0·97) | 0·026 | |
|
| ||||||||||
| South (n=3,653) | White | 1 | 1 | 1 | ||||||
| Black | 1·51 | (1·24–1·83) | 1·30 | (1·04–1·62) | 0·019 | 0·84 | (0·76–0·93) | 0·001 | ||
| Hispanic | 0·90 | (0·72–1·13) | 0·91 | (0·71–1·17) | 0·48 | 0·90 | (0·82–1·00) | 0·044 | ||
| Other | 0·98 | (0·70–1·36) | <0·0001 | 0·87 | (0·60–1·25) | 0·44 | 1·00 | (0·86–1·16) | 0·99 | |
|
| ||||||||||
| West (n=2,553) | White | 1 | 1 | 1 | ||||||
| Black | 1·78 | (1·23–2·60) | 1·58 | (1·05–2·38) | 0·027 | 0·83 | (0·69–0·99) | 0·044 | ||
| Hispanic | 1·08 | (0·85–1·38) | 1·03 | (0·79–1·35) | 0·80 | 0·88 | (0·79–0·98) | 0·022 | ||
| Other | 1·10 | (0·79–1·52) | 0·024 | 1·08 | (0·76–1·52) | 0·67 | 0·90 | (0·78–1·03) | 0·13 | |
A hazard ratio less than one is indicative of a lower probability of discharge by 30 days ie a longer length of stay.
LR test p-value
Adjusted for other variables in the table and sex, age, median household income for patient’s zip code, elective admission, admitted from emergency department, transferred in, admitted at weekend, admission quarter, hospital bed size, hospital region, hospital teaching status, presence of complex chronic condition.
Wald test-p-value
Additional analyses
When analysing neonates and non-neonates separately (Supplementary Table 4), the effect size for the association between Black race and mortality was similar to the primary analysis (aOR for neonates 1·21; aOR for non-neonates 1·15; compared to aOR 1·19 for entire cohort). However, these estimates did not reach statistical significance. Black neonates demonstrated dramatically reduced probability of discharge (i.e. longer length of stay) by day 30 (aHR 0·53, 95% CI 0·36–0·77; p = 0·001; Supplementary Table 4).
To separate the between- and within-hospital effects of race/ethnicity, we assessed the effect of the proportion of Black patients treated at a hospital as an additional between-hospital variable (Supplementary Table 5). In the univariate analysis, higher mortality was observed in hospitals with a larger percentage of Black patients, odds of mortality increased as the percentage of Black patients increased. In the multivariable analyses, this between-hospital variable was not significant, and inclusion of the between-hospital variable did not attenuate the within-hospital increased mortality observed in Black children (aOR 1·18, 95% CI 1·01–1·38; p = 0·037).
Discussion:
We present a large cohort of children with severe sepsis admitted to a range of hospitals across the United States to assess the influence of race/ethnicity and socioeconomic position on survival of childhood sepsis. There was a clear relationship between race/ethnicity and socioeconomic position, with a higher proportion of Black and Hispanic children residing in lower income areas compared to White children. More White children had private insurance compared to Hispanic and Black children. There was evidence of increased mortality in Black children, driven by higher mortality in the South and West of the country. There was evidence of higher mortality in hospitals which treated a higher proportion of Black patients in univariate analysis; however, this was not observed in the multivariate analysis. We found evidence of longer hospital stays in Black and Hispanic children with Black neonates having nearly half the probability of being discharged alive by day 30 relative to White neonates.
We used insurance status as an additional proxy for socioeconomic position,16 with evidence of inferior survival in the “other” insurance group. Due to heterogeneity of insurance categories grouped into “other,” we cannot make inferences on the mechanism of the association between “other” insurance status and increased mortality. No difference was observed in mortality between publicly and privately insured children. A possible explanation for this is that insurance functions as an invisible variable, insofar as treating providers are often not aware of individual insurance status and so may be less likely to treat patients differentially by insurance status. While insurance status and median income by zip code are plausibly proxies for socioeconomic status, and are used pragmatically given their availability, neither perfectly capture the child or their caretaker’s true socioeconomic position.17,18 We cannot exclude that more marked disparities exist by socioeconomic position, and potentially mediate the differential outcomes we observed in Black and Hispanic children. Better markers of socioeconomic position are needed in research to elucidate the role of socioeconomic position in health outcomes and understand mechanisms of disparities.19
In addition to being a proxy for socioeconomic position, insurance can also function as a financial instrument which equalises access to care without burdening families financially. Thus, the presence of any insurance, including public insurance, sufficiently improves access to care and reduces disparities. No difference was observed in mortality between publicly and privately insured children, suggesting that being covered by public insurance improves health outcomes. This finding is consistent with data on Medicaid expansion after 2010.20
In our study we found clear regional differences in outcomes for sepsis. Mortality was overall higher in children residing in the South of the country and racial disparities were most pronounced in this region. Worse health outcome for children in the South have been previously described.21 There is rising evidence that racism functions as important upstream social determinants of health and health disparities in children. As such, our findings indicate a need to examine the contribution of racism either at the structural, interpersonal or individualised level, to sepsis-related decision making and associated outcomes. Understanding the mechanisms underlying regional disparity in pediatric sepsis outcome by race/ethnicity is a crucial next step.
It is plausible that some of the differential outcomes seen could be related to differences in access to healthcare and quality of care received in different parts of the country. In a study of adult patients hospitalised with sepsis, hospital characteristics drove much of the difference in mortality, with evidence of systematic differences in hospitals used by different racial/ethnic groups.4 The racial disparities described in prior studies of neonates are driven, in part, by differences in neonatal-specific outcomes and process of care quality.22 In our study, an analysis explicitly modeling between-hospital differences in racial composition did not suggest that this was a significant contributor to disparate outcomes, although these conclusions may be sensitive to how we defined between-hospital effects. Additional work identifying characteristics of hospitals that treat disproportionate numbers of Black and Hispanic children with sepsis is indicated based on the findings of our study.
Consistent with adult literature, we found evidence of increased mortality in Black children and increased length of stay in Black and Hispanic children.7 Some of the disparity in adult sepsis is driven by the presence of comorbidities (e.g. diabetes and chronic kidney disease) which increase susceptibility to sepsis.7,8 In our cohort, increased prevalence of complex chronic condition was found in Black and Hispanic children, and adjustment for this partially attenuated the increased mortality. Increasing age and presence of a complex chronic condition were the main non-geographic drivers of mortality risk. While beyond the scope of this paper, addressing early life comorbidities, related to chronic conditions or prematurity, is likely to be central to efforts to reduce disparities.23
There are known racial disparities in neonatal outcomes, with higher rates of prematurity and low birth weight in Black infants.15 Consistent with some prior literature,9 we found strong evidence of increased length of stay in Black neonates, which we speculate could carry forward and propagate worse outcomes later in childhood, potentially via increased frequency of complex chronic conditions. In the univariate analysis Black neonates had signficantly higher odds of mortality; however, this did not reach statistical significance in the multivariable analysis, similar to the existing literature.9 While some prior literature has shown higher case fatality in Black preterm infants with early-onset sepsis, and lowest case fatality in White term infants,10 this has not been consistently demonstrated.9 It should be noted that our sample size was reduced when restricted to neonates, and as such our estimates are inprecise. Further research looking at larger samples of neonates is warranted using more recent datasets.
The higher mortality and longer length of stay in Black children may have also been related to Black patients being more sick on arrival to the hospital, presenting at later stages of illness (either due to healthcare access barriers or mistrust due to ongoing discrimination24). Due to limitations of the KID database, namely the absence of severity of illness data, it is unclear whether Black children were sicker on presentation.
Delayed recognition and treatment of sepsis are known to be associated with poor outcomes and it is plausible that differential recognition and treatment by race/ethnicity contributes to the disparities seen.2 Evidence of differential recognition of sepsis in children by race is evident in the literature.25 Provider bias in medicine is well described, with documented bias among resident physicians against both Black adult and paediatric patients.26 Evidence also exists of differential antibiotic prescribing according to patients’ race, with Black and Hispanic children being less likely to receive antibiotics than White children for viral infections.27 In an adult ER population, Black patients were triaged differently than White patients with lower acuity and longer wait times for equivalent conditions.28 The use of standardised sepsis triggers and clinical pathways for complaints such as head injury have been associated with less differential care, leaving less room for provider biases to affect timing and type of care.25,29 Standardised care pathways may counter provider-driven discrimination, and thus represent a health disparities-oriented intervention which should be explored. Additionally, while interventions to mitigate potential provider-based disparities in care are important, our data also suggests continued work on systematic changes are likely needed to combat the disparate outcomes seen.
There are important limitations of our study. KID provides race/ethnicity as an aggregate variable, so we were unable to examine the separate effects of Hispanic ethnicity from race. The data collected was primarily for administrative purposes, meaning that severe sepsis could be coded incorrectly or over/under-reported. However, the degree to which this potential coding inaccuracy is affected by race/ethnicity is unknown, and we used a validated administrative definition for sepsis used in other large database studies.13 Additionally, because KID doesn’t contain identifiable information, we were unable to ascertain which patients were readmissions and how many unique children were captured by our study. Re-admission could be a contributor to outcome differences if there was an association seen between re-admission and race/ethnicity.30 Children admitted to emergency departments who died before admission are not captured by this study. It is unclear if the race/ethnicity of those children who died prior to admission would contribute to or attenuate the disparities found in this study. Importantly, we did not have definitive data on which patients were uninsured and assumed they were included in other, self-pay, or no charge; the increased mortality seen with other insurance status suggests they may be captured by this designation. Finally, we did not have data on language preference and thus could not explore disparities among patients with limited English proficiency. Given the longer lengths of stays we documented in Hispanic children, this represents another area for future study.
Strengths of our work include use of a large, modern, representative cohort of paediatric severe sepsis. While the mortality rate was slightly lower than we powered for, the sample size was large enough to overcome this difference. The cohort includes children from a variety of hospitals and a wide range of geographic areas in the United States, improving generalisability. Length of stay was analysed in a competing risk framework, mitigating biased effect sizes by ignoring death. Overall, we had a small amount of missing data. We were also able to identify and adjust for the presence of multiple individual and hospital level confounders including complex chronic condition, which is a particularly significant variable.14
Conclusion:
Disparate outcomes exist in childhood sepsis based on race/ethnicity and insurance status, with evidence of significantly worse outcomes in the Southern and Western United States for non-White children. There are a number of plausible mechanisms underpinning these disparities. Future research should look for further disparities in sepsis care and outcome, as well as explore the mechanisms behind their existence. A clearer understanding of the reason these disparities exist will enable health care systems to develop interventions to combat them.
Supplementary Material
Research in context:
Evidence before this study
Disparities in outcome of adult sepsis have been described by socioeconomic position and race/ethnicity, and there is a large body of evidence showing substantially higher mortality from sepsis in Black adult patients. Higher rates of sepsis are seen in patients residing in high poverty areas with higher mortality seen in uninsured patients. There are very limited data looking at racial/ethnic and socioeconomic disparities in outcome of sepsis in children. Two studies investigating racial disparities in outcome from neonatal sepsis showed higher incidence and case fatality of sepsis in Black preterm neonates and higher mortality in neonates without insurance and from lower income households. There are currently no published studies looking at pediatric sepsis outcome disparities by race/ethnicity and socioeconomic position outside of the neonatal period.
Added Value of this study
This is one of the first papers to explore racial/ethnic and socioeconomic disparities in survival from pediatric sepsis outside the neonatal period in detail. Black children and children without public or private insurance experience higher mortality from sepsis. Black and Hispanic children had longer lengths of hospital stay.
Implications of all the available evidence
This initial study shows clear evidence of racial disparities in childhood sepsis outcomes. Our findings suggest that there may be differential sepsis recognition, approaches to treatment, access to health care service, and/or provider bias that contribute to poorer outcomes from sepsis for minority patients and those of lower socioeconomic position. Future research should explore the mechanisms behind these disparities. A clearer understanding of the reason these disparities exist will enable health care systems to develop interventions to combat them.
Footnotes
The authors declared no conflicts of interest.
All authors who qualify for authorship for this manuscript (in adherence with ICMJE guidelines) are included in the authorship.
Data sharing statement:
This paper uses publicly accessible data from Healthcare Cost and Utilization Project (HCUP) Kids’ Inpatient Database (KID).
References:
- 1.Balamuth F, Weiss SL, Neuman MI, et al. Pediatric severe sepsis in U.S. children’s hospitals. Pediatr Crit Care Med 2014; 15: 798–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Souza DC de Machado FR. Advances in Pediatric Septic Shock: Epidemiology of Pediatric Septic Shock. J Pediatr Intensive Care 2019; 8: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carlton EF, Barbaro RP, Iwashyna T, Prescott HC. Cost of Pediatric Severe Sepsis Hospitalizations. JAMA Pediatr. 2019; 173: 986–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jones JM, Fingar KR, Miller MA, et al. Racial disparities in sepsis-related in-hospital mortality: Using a broad case capture method and multivariate controls for clinical and hospital variables, 2004–2013. Crit Care Med 2017; 45: e1209–17. [DOI] [PubMed] [Google Scholar]
- 5.Barnato AE, Alexander SL, Linde-Zwirble WT, Angus DC. Racial variation in the incidence, care, and outcomes of severe sepsis: analysis of population, patient, and hospital characteristics. Am J Respir Crit Care Med 2008; 177: 279–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kumar G, Taneja A, Majumdar T, Jacobs ER, Whittle J, Nanchal R. The association of lacking insurance with outcomes of severe sepsis: Retrospective analysis of an administrative database. Crit Care Med 2014; 42: 583–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dombrovskiy VY, Martin AA, Sunderram J, Paz HL. Occurrence and outcomes of sepsis: Influence of race. Crit Care Med 2007; 35: 763–8. [DOI] [PubMed] [Google Scholar]
- 8.Mayr FB, Yende S, Linde-Zwirble WT, et al. Infection rate and acute organ dysfunction risk as explanations for racial differences in severe sepsis. JAMA - J Am Med Assoc 2010; 303: 2495–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bohanon FJ, Nunez Lopez O, Adhikari D, et al. Race, Income and Insurance Status Affect Neonatal Sepsis Mortality and Healthcare Resource Utilization. Pediatr Infect Dis J 2018; 37: e178–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weston EJ, Pondo T, Lewis MM, et al. The burden of invasive early-onset neonatal sepsis in the united states, 2005–2008. Pediatr Infect Dis J 2011; 30: 937–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thavamani A, Umapathi KK, Dhanpalreddy H, et al. Epidemiology, Clinical and Microbiologic Profile and Risk Factors for Inpatient Mortality in Pediatric Severe Sepsis in the United States From 2003 to 2014: A Large Population Analysis. Pediatr Infect Dis J 2020; published online March. DOI: 10.1097/INF.0000000000002669. [DOI] [PubMed] [Google Scholar]
- 12.HCUP : Overview of the Kids’ Inpatient Database, Kids’ Inpatient Database, 2009. Available at: http://www.hcup-us.ahrq.gov/kidoverview.jsp (accessed 31 December 2019). .
- 13.Lindell RB, Nishisaki A, Weiss SL, et al. Comparison of Methods for Identification of Pediatric Severe Sepsis and Septic Shock in the Virtual Pediatric Systems Database. Crit Care Med 2019; 47: e129–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: Updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr 2014; 14: 199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beck AF, Edwards EM, Horbar JD, Howell EA, McCormick MC, Pursley DWM. The color of health: how racism, segregation, and inequality affect the health and well-being of preterm infants and their families. Pediatr. Res. 2020; 87: 227–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Adler NE, Newman K. Socioeconomic disparities in health: Pathways and policies. Health Aff 2002; 21: 60–76. [DOI] [PubMed] [Google Scholar]
- 17.Krieger N Overcoming the absence of socioeconomic data in medical records: validation and application of a census-based methodology. Am J Public Health 1992; 82: 703–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krieger N, Chen JT, Waterman PD, Rehkopf DH, Subramanian SV. Race/ethnicity, gender, and monitoring socioeconomic gradients in health: a comparison of area-based socioeconomic measures--the public health disparities geocoding project. Am J Public Health 2003; 93: 1655–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cardel MI, Tong S, Pavela G, et al. Youth Subjective Social Status (SSS) is Associated with Parent SSS, Income, and Food Insecurity but not Weight Loss Among Low-Income Hispanic Youth. Obesity 2018; 26: 1923–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Swaminathan S, Sommers BD, Thorsness R, Mehrotra R, Lee Y, Trivedi AN. Association of Medicaid Expansion with 1-Year Mortality among Patients with End-Stage Renal Disease. In: JAMA - Journal of the American Medical Association. American Medical Association, 2018: 2242–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goldhagen J, Remo R, Bryant T, et al. The health status of southern children: A neglected regional disparity. Pediatrics 2005; 116. DOI: 10.1542/peds.2005-0366. [DOI] [PubMed] [Google Scholar]
- 22.Horbar JD, Edwards EM, Greenberg LT, et al. Racial Segregation and Inequality in the Neonatal Intensive Care Unit for Very Low-Birth-Weight and Very Preterm Infants. JAMA Pediatr 2019; 173: 455–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Flores G, Tomany-Korman SC. Racial and ethnic disparities in medical and dental health, access to care, and use of services in US children. Pediatrics 2008; 121: e286–98. [DOI] [PubMed] [Google Scholar]
- 24.Jaiswal J Whose Responsibility Is It to Dismantle Medical Mistrust? Future Directions for Researchers and Health Care Providers. Behav Med 2019; 45: 188–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Raman J, Johnson TJ, Hayes K, Balamuth F. Racial differences in sepsis recognition in the emergency department. Pediatrics 2019; 144. DOI: 10.1542/peds.2019-0348. [DOI] [PubMed] [Google Scholar]
- 26.Johnson TJ, Winger DG, Hickey RW, et al. Comparison of Physician Implicit Racial Bias Toward Adults Versus Children. Acad Pediatr 2017; 17: 120–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goyal MK, Johnson TJ, Chamberlain JM, et al. Racial and ethnic differences in antibiotic use for viral illness in emergency departments. Pediatrics 2017; 140. DOI: 10.1542/peds.2017-0203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schrader CD, Lewis LM. Racial disparity in Emergency Department triage. J Emerg Med 2013; 44: 511–8. [DOI] [PubMed] [Google Scholar]
- 29.Payne NR, Puumala SE. Racial disparities in ordering laboratory and radiology tests for pediatric patients in the emergency department. Pediatr Emerg Care 2013; 29: 598–606. [DOI] [PubMed] [Google Scholar]
- 30.Parikh K, Berry J, Hall M, et al. Racial and Ethnic Differences in Pediatric Readmissions for Common Chronic Conditions. J Pediatr 2017; 186: 158–164.e1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
This paper uses publicly accessible data from Healthcare Cost and Utilization Project (HCUP) Kids’ Inpatient Database (KID).


