Abstract
Background
Fatigue is a common symptom in adults that may cause physical and psychological problems and reduce quality of life. Aromatherapy could possibly provide relief for those suffering from fatigue. Here, we evaluated the effect of aromatherapy on fatigue in adults.
Methods
We searched the PubMed, Embase, Cochrane Library, Web of Science, China National Knowledge Infrastructure, Chinese Biomedical Literature, SinoMed, Wanfang, and Chinese Scientific Journal Database databases for randomized controlled trials of aromatherapy treatment for fatigue in adults from their inception to June 2021. Two reviewers searched independently, extracted the characteristics of the studies, and assessed the risk of bias using the Cochrane risk-of-bias tool and Stata v. 14.0.
Results
Nineteen studies were included in this systematic review. Aromatherapy had a significant effect on fatigue (standardized mean difference −0.64, 95% confidence interval−1.14, −0.15, I2 94.4%, P < 0.001). Subgroup analysis according to aromatic type, substance, frequency, treatment duration, intervention, outcomes measurement, and population type showed that aromatherapy had a significantly greater effect in the intervention group, compared to the control group. Funnel plots and Egger's test indicated no significant publication bias.
Conclusion
Our results suggest that aromatherapy ameliorates fatigue in adults who suffer from chronic diseases. A rigorous intervention program and larger randomized controlled trials are needed.
1. Background
Fatigue is a subjective feeling of tiredness, weakness, or lack of energy and motivation [1]. It is distressing and highly prevalent in adults, particularly in those diagnosed with cancer, receiving hemodialysis or suffering from chronic diseases. It has no specific mechanism and can occur at any disease stage [1]. Fatigue is related to an elevated incidence of physical and mental diseases (such as cardiovascular disease, anxiety, depression, and sleep disorders), which reduce quality of life and prolong hospitalization [2, 3]. Approximately 5–40% of patients experience fatigue from hospitalization and follow-up visits, and >50% of patients with chronic hepatitis C virus infection and 60–97% of those undergoing hemodialysis feel fatigue [4, 5].
Aromatherapy is the application of plant essential oils or herbal essences by inhalation, massage, or compression to alleviate a symptom or disease [6]. As a nonpharmacological, complementary, and alternative modality, aromatherapy is economical and has fewer adverse effects compared with Western medicine. The United States federal government funds aromatherapy research with $30.2 billion annually [7]. Aromatherapy can improve symptoms such as sleep problems, pain, chronic fatigue, anxiety, depression, stress, and postoperative nausea and vomiting [8, 9].
Most RCTs show the significant effect of aromatherapy on fatigue, but others have reported discrepant findings. Moreover, reviews have verified the efficacy of complementary and alternative therapies, such as acupuncture, moxibustion, Tai Chi, and acupressure on fatigue [10]. Hence, this meta-analysis evaluated the evidence and estimated effects of aromatherapy on fatigue in adults.
2. Methods
This systematic review and meta-analysis was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [11] and is registered at the International Prospective Register of Systematic Reviews (no. CRD42021268038).
2.1. Search Strategy
Two reviewers (Q.T. Wang and P. Hu) independently and systematically searched for relevant studies in the PubMed, Embase, Cochrane Library, Web of Science, China National Knowledge Infrastructure, Chinese Scientific Journal Database, Chinese Biomedical Literature, and Wanfang databases. A manual search was not performed in this study. The search terms comprised aromatherapy (or aroma therapy, aromatherapies, etc.) and fatigue (or lassitude). The search process had no date or language restrictions. Taking PubMed as an example, we used the following search parameters: (aromatherapy [Mesh]) OR (((((Aromatherapies [Title/Abstract])) OR (Aroma Therapy [Title/Abstract])) OR (Aroma Therapies [Title/Abstract])) OR (Therapy, Aroma [Title/Abstract])) OR (Therapies, Aroma [Title/Abstract]) AND ((fatigue [Mesh Terms])) OR (Lassitude[Title/Abstract]). Both mesh and non-mesh terms were included.
2.2. Eligibility Criteria
Inclusion and exclusion criteria were determined according to the participants, interventions, comparisons, outcomes, and study design principles. The inclusion criteria were (1) adults (≥18 years) diagnosed with fatigue regardless of race, sex, disease type, or disease duration; (2) the treatment group received aromatherapy, the details of which were described; (3) the control group received a placebo, regular care, or no treatment; (4) the degree of fatigue was regarded as the primary or secondary outcome and was estimated by a fatigue scale, such as the Fatigue Severity Scale, Multidimensional Fatigue Inventory, Brief Fatigue Inventory, or a Visual Analog Scale; and (5) the included studies were randomized controlled trials (RCTs) published in any language.
2.3. Exclusion Criteria
We excluded trials of chronic fatigue syndrome, defined as persistent fatigue over 6 months with multisystem disorders [9]. RCTs, quasi-randomized trials, and parallel trials were included. Trials that did not report outcomes or included incomplete data were excluded.
2.4. Study Selection
We searched the articles that met the inclusion criteria and created a database using EndNote v. 9.0 software. According to the PRISMA flow diagram [11], we removed duplicate studies, screened the titles and abstracts, and finally browsed the full text to identify relevant RCTs.
2.5. Data Extraction
Two reviewers (Q.T. Wang and L.J. Zhu) extracted the data, and another reviewer (Y.C. Liu) checked for accuracy. Discrepancies were resolved by discussion until a consensus was achieved. Information collected from the trials consisted of the first author, publication year, country, participants' details (e.g., age, sample size, type of disease), interventions (e.g., aromatic mode, dosage, duration and frequency), and outcome metrics [12]. If necessary, one reviewer (Q.T. Wang) contacted the author to obtain missing information.
2.6. Risk of Bias Assessment
Using the Cochrane Collaboration Risk of Bias Tool, the risk of bias was assessed as low risk, high risk, or unclear by two reviewers (Q.T. Wang and Y.C. Liu) separately [13]. We ranked risk based on the following seven domains: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other biases. Disagreements were resolved by discussion until a consensus was achieved.
2.7. Statistical Analysis
We analyzed the data using Stata v. 14.0 software. Continuous data are presented as means and standard deviations. Outcomes were synthesized as standardized mean differences and 95% confidence intervals using a random-effects model. Subgroup analyses were performed to identify sources of heterogeneity, including aromatic type, substance, frequency and treatment duration, the control intervention, outcomes assessment, and type of population. A sensitivity analysis was conducted to evaluate the stability of the results and whether the meta-analysis results were affected by any of the individual trials. If heterogeneity was significant (I 2 ≥ 50% or p < 0.10) [14], we used the random-effects model or screened the included studies one by one to identify the influential factors. A fixed-effects model was applied in the meta-analysis if there was no significant heterogeneity. p < 0.05 was considered indicative of statistical significance. Funnel plots and Egger's test were used to assess publication bias.
3. Results
3.1. Literature Search
We identified 216 studies in the electronic databases, among which 19 were included in the analysis after removing 67 duplicates. One hundred forty-nine articles were excluded after screening the title and abstract. Among the remaining 66 articles, 47 were excluded due to an irrelevant title (n = 14), irrelevant abstract (n = 14), non-RCT (n = 13), no full-text (n = (2), or incomplete data (n = 4). Finally, 19 studies were eligible for the meta-analysis. The selection process is shown in Figure 1.
Figure 1.
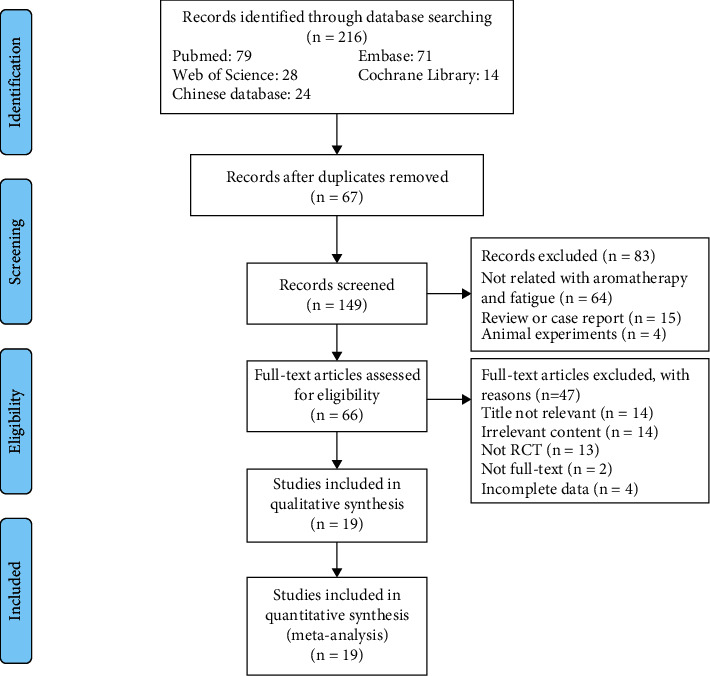
Flow diagram of trial selection.
3.2. Study Characteristics
A total of 1381 participants were included in this meta-analysis. The 19 studies were published in Iran [15–22], Turkey [23–26], Korea [27], South Korea [28, 29], Japan [30, 31], China [32], or the United States [33] from 2012 to 2021. The essential oils used as interventions were lavender, citrus, and mixed essential oils. The control groups received routine care or a placebo (distilled water or vegetable juice). The oil dose was 2/3/5/8/20 drops, and 12 and 7 comparisons used inhalation and massage, respectively. The intervention frequency was two, three, or four times per week, or one to two times per day, or every other day. The treatment duration ranged from 1 or 2 days to 8 weeks. The primary outcome was fatigue as measured by the Fatigue Severity Scale (FSS), Brief Fatigue Inventory (BFI), Multidimensional Fatigue Inventory (MFI), Numeric Rating Scale (NRS), Visual Analog Scale (VAS), and so on. The characteristics of the included trials are listed in Table 1.
Table 1.
Characteristics of the included RCTs.
| The characteristics of the included studies in the meta-analysis | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Author (Year) | Country | Population characteristics | Age (y) | Sample Size (intervention/control) | Interventions | Aromatic type | Aromatic frequency | Dosage | Treatment duration | Outcome measurement | |
| Intervention group | Control group | ||||||||||
| Karadag E 2019 | Turkey | Received hemodialysis treatment | 18–65 | 30/30 60 | 2% lavender oil | Routine care | Inhalation | 2 or 3 times a week | 2 drops | 30 days | Fatigue Severity Scale (FSS) |
| Sharare A 2019 | Iran | Received hemodialysis treatment | 18–65 | 30/30 60 | Lavender essential oil | Placebo | Inhalation | 3 or 4 times a week | 5 drops | Unknown | Fatigue Severity Scale (FSS) |
| Bagheri-Nesami M 2016 | Iran | Received hemodialysis treatment | ≥18 | 29/30 59 | 5% lavender essential oil | Routine care | Inhalation | 3 times a week | 3 drops | 4 weeks | Fatigue Severity Scale (FSS) |
| Kawabata N 2020 | Japan | Diagnosed with advanced cancer | ≥18 | 27/30 57 | Mixture oils | Routine care | Massage | Unknown | Unknown | Unknown | Brief Fatigue Inventory (BFI) |
| Hassanzadeh M 2018 | Iran | Receiving hemodialysis treatment | 20–65 | 35/35 70 | a mixture of 5% lavender essential oil and sweet almond oil | Routine care | Inhalation | Twice a day | 2 drops | 4 weeks | Brief Fatigue Inventory (BFI) |
| Genç F 2020 | Turkey | The institutionalized elderly | ≥65 | 30/29 59 | 3% lavender oil | Routine care | Inhalation | Once a day | 2 drops | a month | Fatigue Severity Scale (FSS) |
| Demirba BC 2014 | Turkey | Female patients with fibromyalgia | Unknown | 54/54 108 | Mixture oils | Routine care | Inhalation | Every other day | Unknown | 6 weeks | Fatigue Severity Scale (FSS) |
| Gok Metin Z 2016 | Turkey | Diagnosis of Rheumatoid arthritis | ≥18 | 17/17 34 | 5% mixture oils | Routine care | Massage | 3 times a week | 20 drops | 6 weeks | Fatigue Severity Scale (FSS) |
| Mohammadpourhodki R 2021 | Iran | Receiving hemodialysis treatment | 18–65 | 35/35 70 | 1.5% lavender essential oil | Massage | Massage | 3 times a week | 10 to 15 cubic centimeter | Unknown | Fatigue Severity Scale (FSS) |
| Shirzadegan R 2020 | Iran | Diagnosis of acute myocardial infarction | 18–60 | 40/40 80 | Mixture oils | Placebo | Inhalation | Twice a day | 3 drops | 2 days | Multidimensional Fatigue Inventory (MFI) |
| Fariba Kabiri 2018 | Iran | Diagnosis of knee osteoarthritis | 40–60 | 31/31 62 | Lavender oil | Routine care | Inhalation | Every other day | 2 drops | one month | Multidimensional Fatigue Inventory (MFI) |
| Jessie Hawkins 2019 | USA | Women diagnosed with hypothyroidism | 18–55 | 21/20 41 | Mixture oils | Placebo | Inhalation | Once a day | 3 drops | 2 weeks | Multidimensional Fatigue Symptom Inventory (MFSI) |
| Kyoko Asazawa 2018 | Japan | Women in early postpartum period | Average 30 | 115/114 229 | 2% mixture oils | No application | Massage | Unknown | Unknown | 1 session | Self-Diagnosis Checklist for Assessment of Worker's Accumulated Fatigue |
| Hur M-H 2019 | South Korea | Prediabetic women | 40–65 | 31/31 62 | 3% mixture oils | Routine care | Massage | Once a day | 20 drops | 2 weeks | Numeric Rating Scale (NRS) |
| Xu 2020 | China | Diagnosis of certain cancer | Unknown | 49/49 98 | Mixture oils | Routine care | Massage | 2 times a week | 1–4 drops | 8 weeks | Fatigue Self-Assessment Scale (FSAS) |
| Vaziri F 2017 | South Korea. | Women after normal vaginal delivery | 18–35 | 29/27 56 | Lavender oil | Placebo | Inhalation | 6hours | 5 drops | The first 24h after delivery | Visual Analog Scale (VAS) |
| Kim JO 2012 | Korea. | Women in rural areas | Unknown | 26/26 52 | Mixture oils | Routine care | Massage | 3 times a week | Unknown | 6 weeks | Fatigue Assessment Instrument (FAI) |
| Varaei S 2020 | Iran | Receiving hemodialysis treatment | Unknown | 32/32 64 | Mixture oils of lavender and sweet orange | Routine care | Inhalation | 3 times a week | 2 drops | 8 weeks | Rhoten Fatigue Scale (RFS) |
| Abdollahi F 2020 | Iran | Type 2 diabetic patients | 30–65 | 30/30 60 | Citrus(bitter orange) | Routine care | Inhalation | Once a day | 8 drops | 3 days | Visual Analog Scale (VAS) |
3.3. Risk of Bias
Eight trials were considered low risk because they applied random sequence generation. Three trials did not mention randomization and thus were ranked as high risk. Only three studies described the process of allocation concealment. Two trials were high risk due to the use of an improper method of allocation concealment. Six studies were assessed as low risk because they had single or triple blinding; by contrast, one had incomplete blinding and thus was ranked as high risk. One trial was high risk because the blinding was broken, and six trials were low risk. Two trials were assessed as unclear risk and the others as low risk. Two trials were low risk because they explained the outcome report; the others were unclear risk. No other type of bias was detected (Figures 2 and 3).
Figure 2.
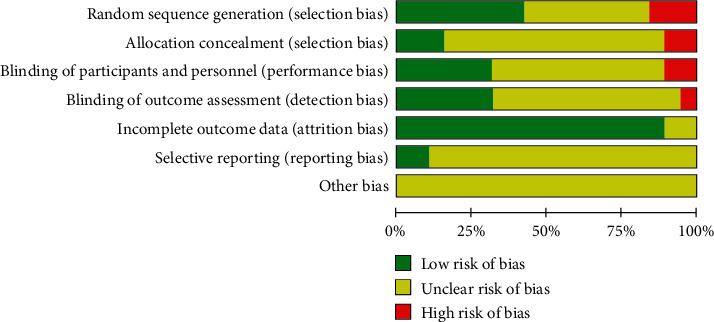
Risk of bias graph.
Figure 3.
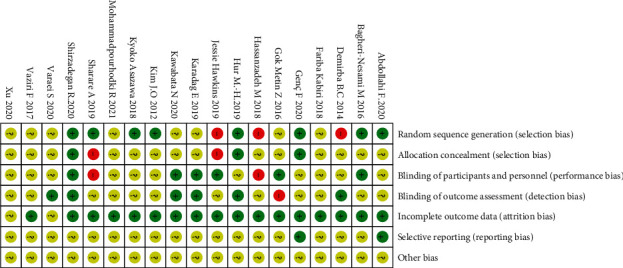
Risk of bias summary.
3.4. Overall Effect of Aromatherapy
The 1381 participants were divided into intervention (n = 691) and control (n = 690) groups. Using a random-effects model, the intervention group showed a significant effect on fatigue compared with the control group (standardized mean difference, −0.64; 95% confidence interval −1.14, −0.15). Aromatherapy significantly relieved fatigue, but the studies showed high heterogeneity (I2 94.4%, P < 0.001) (Figure 4).
Figure 4.
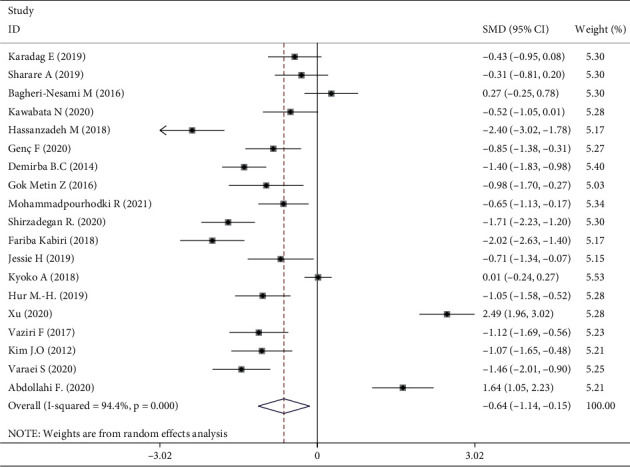
Meta-analysis of aromatherapy group versus control group on fatigue in adults.
3.5. Subgroup Analysis
Meta-analysis of three trials [16, 30, 31] showed that aromatherapy did not ameliorate fatigue in adults. Therefore, we conducted subgroup and sensitivity analyses to estimate the effect of aromatherapy on fatigue. Considering the high heterogeneity among the studies, we performed subgroup analyses according to aromatic delivery mode, substance, frequency, treatment duration, control intervention, outcome measurement, and type of population. The results suggested that aromatherapy significantly relieved fatigue compared with the control group, irrespective of the aromatic delivery mode (Figure 5). Regarding aromatic substances, lavender essential oil and mixed oils were effective for fatigue, whereas citrus oil was not (Figure 6). Regarding aromatic frequency, there were differences in efficacy between the intervention and control groups. However, when aromatherapy was administered two, three, or four times weekly, once or twice daily, for several hours, the heterogeneity was significant (Figure 7). The heterogeneity of studies with treatment durations of ≥6 weeks and ≤1 week was higher than that of the other studies (Figure 8). The effect of aromatherapy did not differ between the intervention and control groups when the treatment period lasted less than 1 day. Additionally, aromatherapy for 2–4 weeks or 4 weeks showed considerable effectiveness in the intervention group, regardless of the control intervention used (placebo control, massage, or no application) (Figure 9). For the outcome assessment and type of population, the subgroup analysis showed a significant difference between the intervention and control groups on fatigue (Figures 10, 11).
Figure 5.
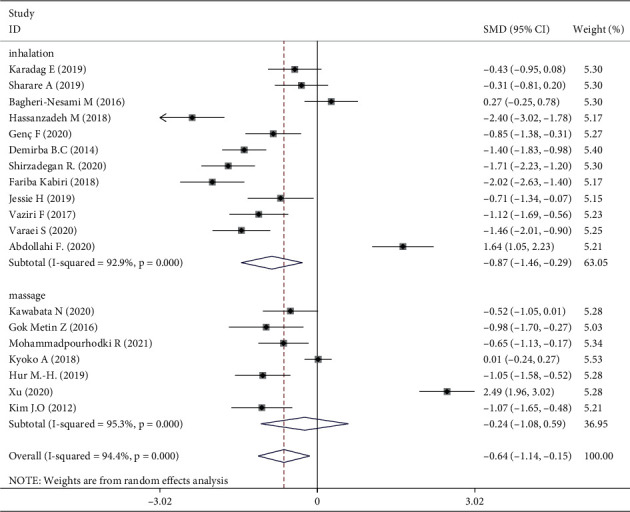
Subgroup analysis of aromatic delivery mode.
Figure 6.
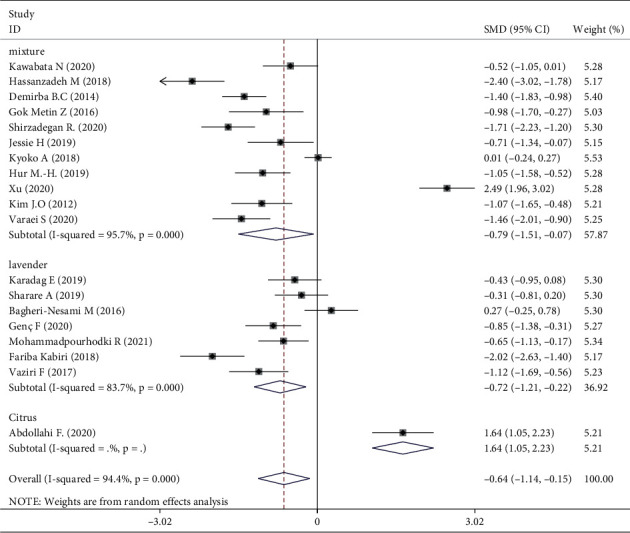
Subgroup analysis of substance.
Figure 7.
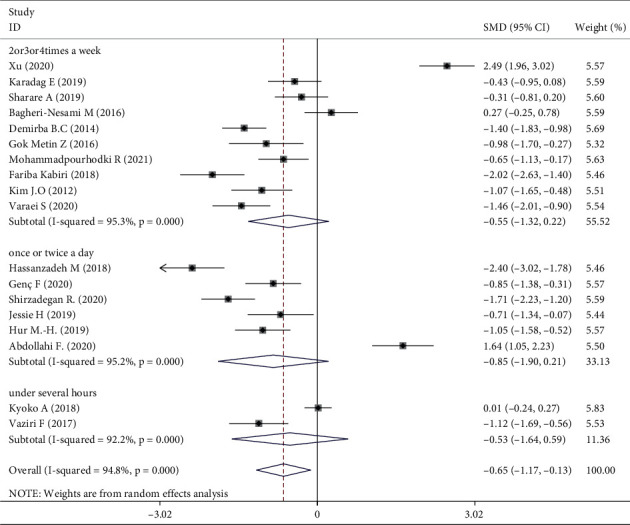
Subgroup analysis of frequency.
Figure 8.
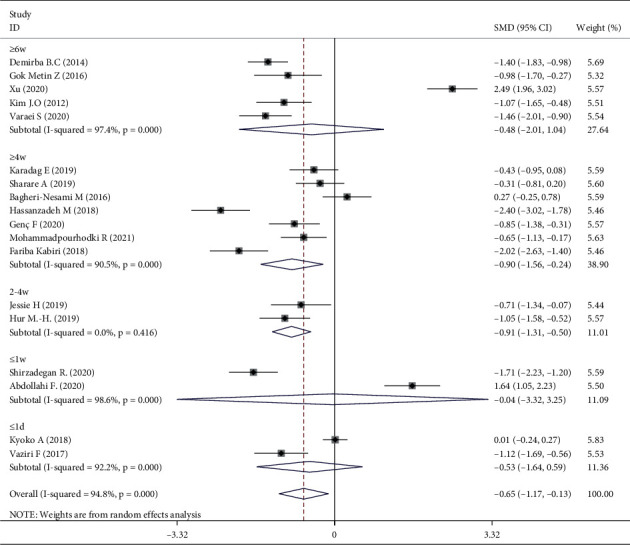
Subgroup analysis of treatment duration.
Figure 9.
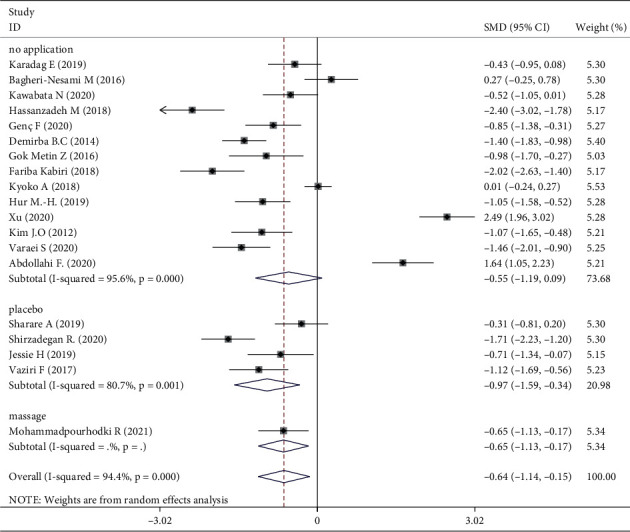
Subgroup analysis of control intervention.
Figure 10.
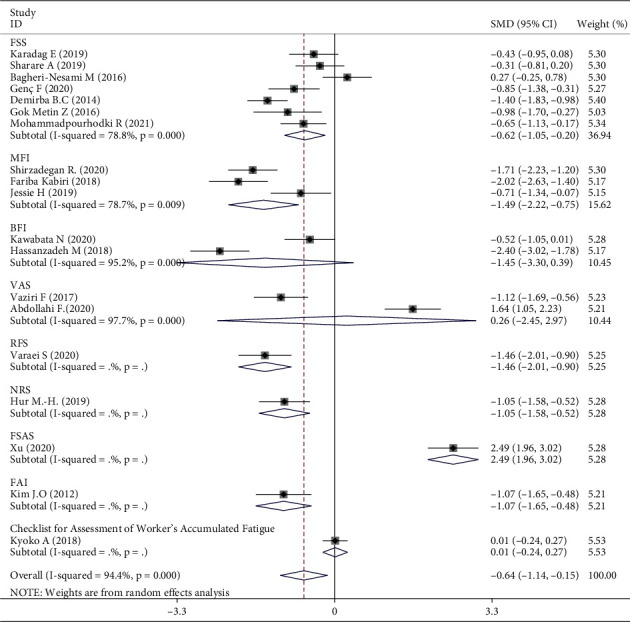
Subgroup analysis of outcomes measurement.
Figure 11.
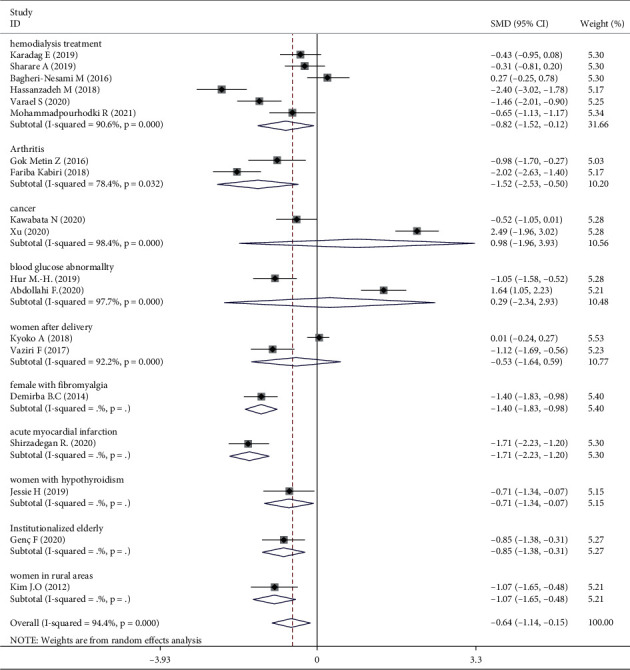
Subgroup analysis of type of population.
3.6. Publication Bias and Sensitivity Analysis
The funnel plot was symmetrical, so deviation was associated with trial methodology (Figure 12). Egger's test (P=0.621) showed no significant publication bias in terms of the effectiveness of aromatherapy on fatigue. A sensitivity analysis in which trials were excluded one by one [16, 18, 21, 23, 30–32] did not significantly alter the meta-analysis results (I2 69.5%, P < 0.001) (Figure 13).
Figure 12.
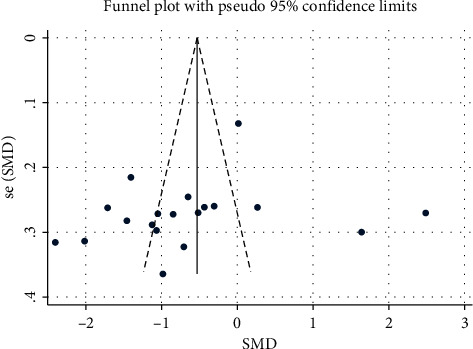
Funnel plot.
Figure 13.
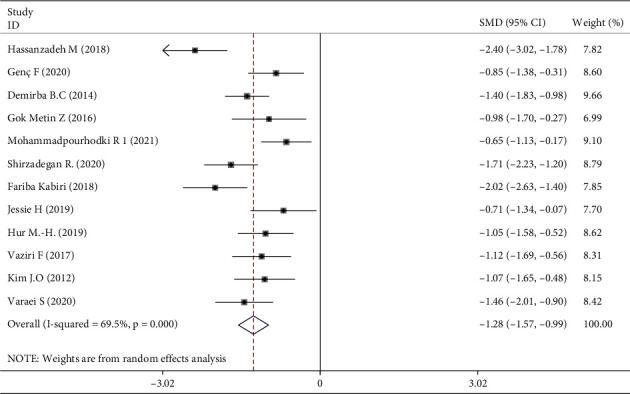
Sensitivity analysis.
4. Discussion
Aromatherapy is reportedly effective for sleep disorders, anxiety, stress, labor pain, and postoperative nausea and vomiting [34–38]. It is an inexpensive, nonpharmacological treatment, with few side effects and is convenient to administer in the home or clinic [38, 39]. Adverse effects are rare, although infrequent occurrences of allergy and drowsiness were reported by a small RCT (N = 7) [40]. Essential oils are derived from the petals, flowers, stems, leaves, needles, rinds, fruits, roots, and rhizomes of lavender, rose, orange, lemon, citrus, almond, peppermint, ginger, and so on. The oil comprises multiple natural volatile organic compounds because it is produced through distillation, extraction, or concentration from the plants by steam or a mechanical cold press [7, 41]. Its therapeutic effects are based on the systemic functions of the body (working like a drug or enzyme), which is used to trigger reflexive effects to generate a positive emotion [41].Although the mechanism by which aromatherapy relieves fatigue is unclear, it is said that aromatherapy activates the limbic system, interacting with the cerebral cortex to regulate the individual's emotion and visceral functions, such as the heart rate, respiration, blood pressure, blood flow, muscle tension, body temperature, pupil dilation, and hormonal levels [7, 23]. Aromatherapy can be delivered by inhalation, massage, compression, or foot baths [42]. Research indicates that aromatic inhalation stimulates the olfactory nerve cells and the integumentary and lymphatic systems, triggering the release of neurotransmitters, such as endorphins, peptides, enkephalin, serotonin, and noradrenaline, which can enhance wellbeing and relaxation, thus reducing chronic stress [7, 20, 34, 39]. Smell is mainly governed by the brain's limbic system, which is also associated with emotions, feeling, and behavior. Massage is thought to play a role in the skin, blood, and lymphatic systems. Moreover, aromatic massage promotes the absorption of essential oils and activates mental and physiological responses, including an immune system response [7, 19]. Additionally, aromatic massage not only facilitates the absorption of essential oil through the skin but also keeps the skin warm and relaxes the body [19].
A meta-analysis of the effects of aromatherapy on insomnia concluded that inhalation is more effective than massage. However, a systematic review showed that aromatic massage is more beneficial than aromatic inhalation for depressive symptoms [43]. One RCT showed that the effect of aromatherapy massage is stronger than that of inhalation on fatigue in hemodialysis patients [17]. Our subgroup analysis of aromatic delivery showed no significant difference between inhalation and massage. A single essential oil is more beneficial for sleep than mixed oils [34]. Conversely, a meta-analysis concluded that multiple aromatic oils were more effective for fatigue in patients receiving hemodialysis [43]. Indeed, our subgroup analysis showed that both lavender and mixed oils relieve fatigue. Citrus, sweet almond, and orange oils showed no significant effect, possibly due to the low quality of the studies [18, 21]. In an RCT of lavender and orange essential oils for fatigue in hemodialysis patients [18], the outcome showed no significant difference between the lavender and orange groups. Another study observed no significant difference between lavender and citrus aurantium essential oils used in massage to relieve fatigue [19].
Aromatherapy duration for 2–4 weeks or >4 weeks was effective, as demonstrated in one of the included studies [18]. However, the RCTs used different treatment durations. One study suggested that aromatherapy administrated for <2, 2–4, or >4 weeks had similar levels of efficacy [14]. There were differences in efficacy between the intervention and control groups for aromatherapy administered two, three, or four times weekly, whereas application once or twice daily showed no significant difference in efficacy between the intervention and control groups. The frequency of aromatherapy influenced efficacy with regard to fatigue from the subgroup analysis. The results showed no obvious effect on fatigue for whole treatments lasting several hours [28, 31].
For the subgroup analysis of outcome assessment and type of population, the effect of aromatherapy on fatigue was significant in a comparison between the intervention groups and the controls. There are various scales to measure people's fatigue, according to different diseases. Typically, the outcome assessment tools are chosen to fit the specific purpose of the fatigue measurement in the group participants. The scales in this study had been assessed in accordance with their content, constructive validity, and reliability and were used to measure fatigue in response to aromatherapy, as well as detect changes in disease progression over time. However, it is unclear as to the specific assessment scale/s used for fatigue level, thus making comparison between studies difficult [44]. Similarly, different types of population experience varying degrees of fatigue, and each has its own scale. The participants were female in six RCTs [26, 28, 29, 31–33] included in our analysis, and many of the clinical trials focused on women's health in using aromatherapy, for example, for menopausal symptoms, delivery, and dysmenorrhea [45]. However, there was no evidence that supported the prevalence or effects of aromatherapy use with respect to gender. We can only speculate as to why many of the studies included female participants; there was no clear reason for this in relation to the proportion suffering from chronic disease or having a stronger response to aromatherapy.
Three RCTs indicated that aromatherapy had no effect on fatigue. Subgroup analyses suggested significant heterogeneity in eight groups (Figures 5–11). A sensitivity analysis showed that seven trials were likely sources of high heterogeneity, due to being of low quality or having design deficiencies. Overall, there was no clear explanation for the high heterogeneity; thus, more hard evidence of the effects of aromatherapy on fatigue is needed.
4.1. Strengths and Limitations
We used rigorous inclusion criteria to generate reliable and objective outcomes, resulting in analysis of 19 trials. Furthermore, most previous studies focused on inhalation aromatherapy [34], but we considered both inhalation and massage aromatherapy. Finally, we used several scales to evaluate fatigue, resulting in robust results.
This study had several limitations. First, the included trials had methodological deficiencies. Only three trials performed both random sequence generation and allocation concealment. Six trials implemented blinding of participants and personnel (single or triple), six applied blinding of outcome assessments, and two trials had unclear bias and incomplete outcome data. Second, the high heterogeneity may be related to the diversity of medical conditions (which may affect fatigue scores) evaluated in the included RCTs. However, most of the trials used similar methodologies. Third, we did not evaluate the optimal treatment duration, which could influence effectiveness.
5. Conclusion
Our results showed that aromatherapy is effective for relieving fatigue in adults who suffer from chronic diseases, such as cancer, arthritis, hypothyroidism, diabetes, renal disease, and so on. However, several trials showed that aromatherapy did not ameliorate fatigue; this could be the result of treatment duration or study quality. Additionally, a scientific aromatherapy program and further high-quality RCTs are necessary to assess the effect of aromatherapy on fatigue.
Acknowledgments
The research was supported by the grant from the Program of the Guangdong Provincial Bureau of Traditional Chinese Medicine (Grant no. 20204006).
Abbreviations
- RCTs:
Randomized controlled trials
- RCT:
Randomized controlled trial
- CNKI:
China National Knowledge Infrastructure
- VIP:
Chinese Science and Technology Periodical Database
- CBM:
Chinese Biomedical Literature Database
- CFS:
Chronic Fatigue Syndrome
- CCRBT:
The Cochrane Collaboration Risk of Bias Tool
- CI:
Confidence interval
- M:
Mean
- SD:
Standard deviation
- SMD:
Standard mean difference.
Contributor Information
Yangchen Liu, Email: morning924@126.com.
Meizhen Lin, Email: lmzmay@163.com.
Disclosure
Lin Wei is the co-first author.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors' Contributions
Wei Lin and Yueming Luo designed and conceptualized the review; Qiuting Wang and Ping Hu searched and screened the literature; Qiuting Wang and Lijia Zhu analyzed and extracted the data; Qiuting Wang and Yangchen Liu assessed the risk of bias for included trials; Qiuting Wang and Wei Lin finished the manuscript and wrote the review; and Meizhen Lin, Yueming Luo, Chong Deng, and Lijun Lin revised and edited the article and provided resources. All authors improved and approved the final review.
Supplementary Materials
Data Table 1: meta-analysis of aromatherapy group versus control group on fatigue in adults. Data Table 2: subgroup analysis of aromatic delivery mode. Data Table 3: subgroup analysis of substance. Data Table 4: subgroup analysis of frequency. Data Table 5: subgroup analysis of treatment duration. Data Table 6: subgroup analysis of control intervention. Data Table 7: subgroup analysis of outcomes measurement. Data Table 8: subgroup analysis of type of population. Data Table 9: sensitivity analysis.
References
- 1.Dean A. The holistic management of fatigue within palliative care. International Journal of Palliative Nursing . 2019;25(8):368–376. doi: 10.12968/ijpn.2019.25.8.368. [DOI] [PubMed] [Google Scholar]
- 2.Lumpkin S. T., Button J., Stratton L., Strassle P. D., Kim L. T. Chronic fatigue after thyroidectomy: a patient-centered survey. The American Surgeon . 2021;88(2):260–266. doi: 10.1177/0003134821989054. [DOI] [PubMed] [Google Scholar]
- 3.Lee G., Lee J.-S., Kim J. H., Hwang D. Y., Lee Y.-S. Impact of patient’s pain and fatigue on decision of discharge after laparoscopic surgery for colorectal cancer. Annals of Coloproctology . 2019;35(4):209–215. doi: 10.3393/ac.2018.11.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ju A., Teixeira-Pinto A., Tong A., et al. Validation of a core patient-reported outcome measure for fatigue in patients receiving hemodialysis. Clinical Journal of the American Society of Nephrology . 2020;15(11):1614–1621. doi: 10.2215/CJN.05880420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Golabi P., Sayiner M., Bush H., Gerber L. H., Younossi Z. M. Patient-reported outcomes and fatigue in patients with chronic hepatitis C infection. Clinics in Liver Disease . 2017;21(3):565–578. doi: 10.1016/j.cld.2017.03.011. [DOI] [PubMed] [Google Scholar]
- 6.Song X., Peng J., Jiang W., Ye M., Jiang L. Effects of aromatherapy on sleep disorders. Medicine (Baltimore) . 2021;100(17) doi: 10.1097/MD.0000000000025727.e25727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Farrar A. J., Farrar F. C. Clinical aromatherapy. Nursing Clinics of North America . 2020;55(4):489–504. doi: 10.1016/j.cnur.2020.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bach H. V., Kim J., Myung S.-K., Cho Y. A. Efficacy of ginseng supplements on fatigue and physical performance: a meta-analysis. Journal of Korean Medical Science . 2016;31(12):1879–1886. doi: 10.3346/jkms.2016.31.12.1879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang Q., Gong J., Dong H., Xu S., Wang W., Huang G. Acupuncture for chronic fatigue syndrome: a systematic review and meta-analysis. Acupuncture in Medicine . 2019;37(4):211–222. doi: 10.1136/acupmed-2017-011582. [DOI] [PubMed] [Google Scholar]
- 10.Zeng Y. S, Wang C, Ward K. E, et al. Complementary and alternative medicine in hospice and palliative care: a systematic review. Journal of Pain and Symptom Management . 2018;56(5):781–794. doi: 10.1016/j.jpainsymman.2018.07.016. e4. [DOI] [PubMed] [Google Scholar]
- 11.Page M. J., McKenzie J. E., Bossuyt P. M., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ . 2021;372:p. n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vu-Ngoc H., Elawady S. S., Mehyar G. M., et al. Quality of flow diagram in systematic review and/or meta-analysis. PLoS One . 2018;13(6) doi: 10.1371/journal.pone.0195955.e0195955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Armijo-Olivo S., Stiles C. R., Hagen N. A., Biondo P. D., Cummings G. G. Assessment of study quality for systematic reviews: a comparison of the Cochrane collaboration risk of bias tool and the effective public health practice project quality assessment tool: methodological research. Journal of Evaluation in Clinical Practice . 2012;18(1):12–18. doi: 10.1111/j.1365-2753.2010.01516.x. [DOI] [PubMed] [Google Scholar]
- 14.Tang Y., Gong M., Qin X., Su H., Wang Z., Dong H. The therapeutic effect of aromatherapy on insomnia: a meta-analysis. Journal of Affective Disorders . 2021;288:1–9. doi: 10.1016/j.jad.2021.03.066. [DOI] [PubMed] [Google Scholar]
- 15.Hassanzadeh M., Kiani F., Bouya S., Zarei M. Comparing the effects of relaxation technique and inhalation aromatherapy on fatigue in patients undergoing hemodialysis. Complementary Therapies in Clinical Practice . 2018;31:210–214. doi: 10.1016/j.ctcp.2018.02.019. [DOI] [PubMed] [Google Scholar]
- 16.Bagheri-Nesami M., Shorofi S. A., Nikkhah A., Espahbodi F., Ghaderi Koolaee F.-S. The effects of aromatherapy with lavender essential oil on fatigue levels in haemodialysis patients: a randomized clinical trial. Complementary Therapies in Clinical Practice . 2016;22:33–37. doi: 10.1016/j.ctcp.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 17.Varaei S., Jalalian Z., Yekani Nejad M. S., Shamsizadeh M. Comparison the effects of inhalation and massage aromatherapy with lavender and sweet orange on fatigue in hemodialysis patients: a randomized clinical trial. Journal of Complementary and Integrative Medicine . 2020;18(1):193–200. doi: 10.1515/jcim-2018-0137. [DOI] [PubMed] [Google Scholar]
- 18.Ahmady S., Rezaei M., Khatony A. Comparing effects of aromatherapy with lavender essential oil and orange essential oil on fatigue of hemodialysis patients: a randomized trial. Complementary Therapies in Clinical Practice . 2019;36:64–68. doi: 10.1016/j.ctcp.2019.05.005. [DOI] [PubMed] [Google Scholar]
- 19.Mohammadpourhodki R., Sadeghnezhad H., Ebrahimi H., Basirinezhad M. H., Maleki M., Bossola M. The effect of aromatherapy massage with lavender and citrus aurantium essential oil on quality of life of patients on chronic hemodialysis: a parallel randomized clinical trial study. Journal of Pain and Symptom Management . 2021;61(3):456–463. doi: 10.1016/j.jpainsymman.2020.08.032. [DOI] [PubMed] [Google Scholar]
- 20.Shirzadegan R., Gholami M., Hasanvand S., Beiranvand A. The effects of Citrus aurantium aroma on anxiety and fatigue in patients with Acute Myocardial Infarction: a Two-center, randomized, controlled trial. Journal of Herbal Medicine . 2020;21 doi: 10.1016/j.hermed.2019.100326.100326 [DOI] [Google Scholar]
- 21.Abdollahi F., Mobadery T. The effect of aromatherapy with bitter orange (Citrus aurantium) extract on anxiety and fatigue in type 2 diabetic patients. Advances in Integrative Medicine . 2020;7(1):3–7. doi: 10.1016/J.AIMED.2019.01.002. [DOI] [Google Scholar]
- 22.Kabiri f., Hassanpour A., Dreis F. Effects of massage therapy and aromatherapy on fatigue in patients with knee osteoarthritis. Journal of Herbmed Pharmacology . 2018;7(3):141–147. doi: 10.15171/jhp.2018.24. [DOI] [Google Scholar]
- 23.Karadag E., Samancioglu Baglama S. The effect of aromatherapy on fatigue and anxiety in patients undergoing hemodialysis treatment. Holistic Nursing Practice . 2019;33(4):222–229. doi: 10.1097/HNP.0000000000000334. [DOI] [PubMed] [Google Scholar]
- 24.Gok Metin Z., Ozdemir L. The effects of aromatherapy massage and reflexology on pain and fatigue in patients with rheumatoid arthritis: a randomized controlled trial. Pain Management Nursing . 2016;17(2):140–149. doi: 10.1016/j.pmn.2016.01.004. [DOI] [PubMed] [Google Scholar]
- 25.Genç F., Karadağ S., Kılıç Akça N., Tan M., Cerit D. The effect of aromatherapy on sleep quality and fatigue level of the elderly. Holistic Nursing Practice . 2020;34(3):155–162. doi: 10.1097/HNP.0000000000000385. [DOI] [PubMed] [Google Scholar]
- 26.Demirbağ B. C., Erci B. The effects of sleep and touch therapy accompanied by music and aromatherapy on the impact level of fibromyalgia, fatigue and sleep quality in fibromyalgia patients. TAF Preventive Medicine Bulletin . 2014;13(1) [Google Scholar]
- 27.Kim J. O., Kim I. S. Effects of aroma self-foot reflexology massage on stress and immune responses and fatigue in middle-aged women in rural areas. Journal of Korean Academy of Nursing . 2012;42(5):709–718. doi: 10.4040/jkan.2012.42.5.709. [DOI] [PubMed] [Google Scholar]
- 28.Vaziri F., Shiravani M., Najib F., Pourahmad S., Salehi A., Yazdanpanahi Z. Effect of lavender oil aroma in the early hours of postpartum period on maternal pains, fatigue, and mood: a randomized clinical trial. International Journal of Preventive Medicine . 2017;8(1):p. 29. doi: 10.4103/ijpvm.IJPVM_137_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hur M.-H., Hong J. H., Yeo S. Effects of aromatherapy on stress, fructosamine, fatigue, and sleep quality in prediabetic middle-aged women: a randomised controlled trial. European Journal of Integrative Medicine . 2019;31 doi: 10.1016/j.eujim.2019.100978.100978 [DOI] [Google Scholar]
- 30.Kawabata N., Hata A., Aoki T. Effect of aromatherapy massage on quality of sleep in the palliative care ward: a randomized controlled trial. Journal of Pain and Symptom Management . 2020;59(6):1165–1171. doi: 10.1016/j.jpainsymman.2020.01.003. [DOI] [PubMed] [Google Scholar]
- 31.Asazawa K., Kato Y., Koinuma R., Takemoto N., Tsutsui S. Effectiveness of aromatherapy treatment in alleviating fatigue and promoting relaxation of mothers during the early postpartum period. Open Journal of Nursing . 2018;08(03):196–209. doi: 10.4236/ojn.2018.83017. [DOI] [Google Scholar]
- 32.Xu H., Fang X. Value of aromatherapy and massage in relieving peripheral nerve pain and fatigue in patients treated with oxaliplatin. International medical and health Herald . 2020;26(11):1617–1620. doi: 10.3760/cma.j.issn.1007-1245.2020.11.042. [DOI] [Google Scholar]
- 33.Hawkins J., Hires C. Y., Dunne E. W., Keenan L. A. Aromatherapy reduces fatigue among women with hypothyroidism: a randomized placebo-controlled clinical trial. Journal of Complementary and Integrative Medicine . 2019;17(1) doi: 10.1515/jcim-2018-0229. [DOI] [PubMed] [Google Scholar]
- 34.Cheong M. J., Kim S., Kim J. S., et al. A systematic literature review and meta-analysis of the clinical effects of aroma inhalation therapy on sleep problems. Medicine (Baltimore) . 2021;100(9) doi: 10.1097/MD.0000000000024652.e24652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hines S., Steels E., Chang A., Gibbons K. Aromatherapy for treatment of postoperative nausea and vomiting. Cochrane Database of Systematic Reviews . 2018;2018(3) doi: 10.1002/14651858.CD007598.pub3.CD007598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gong M., Dong H., Tang Y., Huang W., Lu F. Effects of aromatherapy on anxiety: a meta-analysis of randomized controlled trials. Journal of Affective Disorders . 2020;274:1028–1040. doi: 10.1016/j.jad.2020.05.118. [DOI] [PubMed] [Google Scholar]
- 37.Chen S.-F., Wang C.-H., Chan P.-T., et al. Labour pain control by aromatherapy: a meta-analysis of randomised controlled trials. Women and Birth . 2019;32(4):327–335. doi: 10.1016/j.wombi.2018.09.010. [DOI] [PubMed] [Google Scholar]
- 38.Lakhan S. E., Sheafer H., Tepper D. The effectiveness of aromatherapy in reducing pain: a systematic review and meta-analysis. Pain Research and Treatment . 2016;2016:1–13. doi: 10.1155/2016/8158693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. National Association Holistic Aromatherapy. Exploring aromatherapy. Available at: https://naha.org/explore-aromatherapy/about-aromatherapy/what-is-aromatherapy/
- 40.Freeman M., Ayers C., Peterson C. Aromatherapy and Essential Oils: A Map of the Evidence . Washington, DC, USA: Department of Veterans Affairs (US); 2019. [PubMed] [Google Scholar]
- 41.Winkelman W. J. Aromatherapy, botanicals, and essential oils in acne. Clinics in Dermatology . 2018;36(3):299–305. doi: 10.1016/j.clindermatol.2018.03.004. [DOI] [PubMed] [Google Scholar]
- 42.Guo P., Li P., Zhang X., et al. The effectiveness of aromatherapy on preoperative anxiety in adults: a systematic review and meta-analysis of randomized controlled trials. International Journal of Nursing Studies . 2020;111 doi: 10.1016/j.ijnurstu.2020.103747.103747 [DOI] [PubMed] [Google Scholar]
- 43.Yangöz Ş. T., Turan Kavradım S., Özer Z. The effect of aromatherapy on fatigue in adults receiving haemodialysis treatment: a systematic review and meta-analysis of randomised controlled trials [published online ahead of print, 2021 Jun 18] Journal of Advanced Nursing . 2021 doi: 10.1111/jan.14922. [DOI] [PubMed] [Google Scholar]
- 44.Machado M. O., Kang N. Y. C., Tai F., et al. Measuring fatigue: a meta‐review. International Journal of Dermatology . 2021;60(9):1053–1069. doi: 10.1111/ijd.15341. [DOI] [PubMed] [Google Scholar]
- 45.Tillett J., Ames D. The uses of aromatherapy in women’s health. Journal of Perinatal and Neonatal Nursing . 2010;24(3):238–245. doi: 10.1097/JPN.0b013e3181ece75d. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Table 1: meta-analysis of aromatherapy group versus control group on fatigue in adults. Data Table 2: subgroup analysis of aromatic delivery mode. Data Table 3: subgroup analysis of substance. Data Table 4: subgroup analysis of frequency. Data Table 5: subgroup analysis of treatment duration. Data Table 6: subgroup analysis of control intervention. Data Table 7: subgroup analysis of outcomes measurement. Data Table 8: subgroup analysis of type of population. Data Table 9: sensitivity analysis.


