Abstract
Background & Aims
Autoimmune hepatitis episodes have been described following SARS-CoV-2 infection and vaccination but their pathophysiology remains unclear. Herein, we report the case of a 52-year-old male, presenting with bimodal episodes of acute hepatitis, each occurring 2-3 weeks after BNT162b2 mRNA vaccination. We sought to identify the underlying immune correlates. The patient received oral budesonide, relapsed, but achieved remission under systemic steroids.
Methods
Imaging mass cytometry for spatial immune profiling was performed on liver biopsy tissue. Flow cytometry was performed to dissect CD8 T-cell phenotypes and identify SARS-CoV-2-specific and EBV-specific T cells longitudinally. Vaccine-induced antibodies were determined by ELISA. Data were correlated with clinical laboratory results.
Results
Analysis of the hepatic tissue revealed an immune infiltrate quantitatively dominated by activated cytotoxic CD8 T cells with panlobular distribution. An enrichment of CD4 T cells, B cells, plasma cells and myeloid cells was also observed compared to controls. The intrahepatic infiltrate showed enrichment for CD8 T cells with SARS-CoV-2-specificity compared to the peripheral blood. Notably, hepatitis severity correlated longitudinally with an activated cytotoxic phenotype of peripheral SARS-CoV-2-specific, but not EBV-specific, CD8+ T cells or vaccine-induced immunoglobulins.
Conclusions
COVID-19 vaccination can elicit a distinct T cell-dominant immune-mediated hepatitis with a unique pathomechanism associated with vaccination-induced antigen-specific tissue-resident immunity requiring systemic immunosuppression.
Lay summary
Liver inflammation is observed during SARS-CoV-2 infection but can also occur in some individuals after vaccination and shares some typical features with autoimmune liver disease. In this report, we show that highly activated T cells accumulate and are evenly distributed in the different areas of the liver in a patient with liver inflammation following SARS-CoV-2 vaccination. Moreover, within the population of these liver-infiltrating T cells, we observed an enrichment of T cells that are reactive to SARS-CoV-2, suggesting that these vaccine-induced cells can contribute to liver inflammation in this context.
Keywords: COVID-19, Vaccination, Autoimmune hepatitis, Virus-specific T cell, CD8+ T cell, Immunosuppression
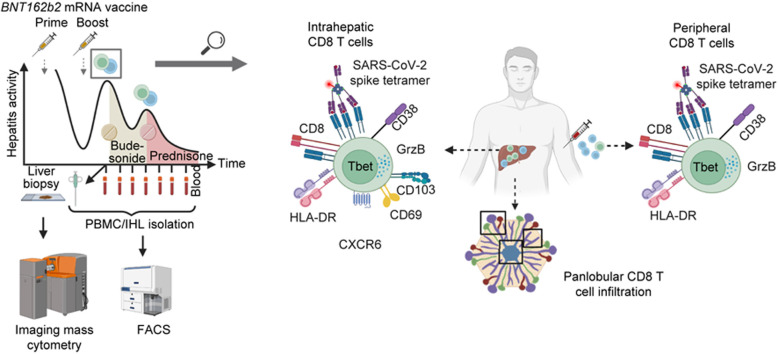
Graphical abstract
Introduction
Vaccination is the key strategy to fight the global COVID-19 pandemic. There was no hepatitis safety signal in COVID-19 vaccination trials,1 however several reports have recently associated autoimmune hepatitis (AIH)-like conditions with COVID-19 vaccines.[2], [3], [4], [5], [6], [7], [8], [9], [10], [11] To our knowledge, no severe case with liver failure requiring liver transplantation was reported. Liver injury was observed after both mRNA and vector-based vaccines, while time from vaccine administration to symptom onset ranged between 4 days after the first dose to 6 weeks after the second dose. One patient was re-exposed to the vaccine which led to a worsening of liver injury.11 It remains unclear whether the reported association of AIH with vaccination is coincidental, might reflect transient drug-induced liver injury, or could involve unique SARS-CoV-2-induced antigen-specific immune activation.12 However, the fact that AIH-like conditions also occurred after SARS-CoV-2 infection13 suggests that the latter could be a driving factor for the sporadic cases.
Herein, we describe the case of a 52-year-old male presenting with acute mixed hepatocellular/cholestatic hepatitis after the first dose of BNT162b2 mRNA vaccine and severe hepatitis after the second dose. Diagnostic evaluation was compatible with criteria for AIH. After initiation of oral budesonide therapy, liver function tests improved for a month before a relapse occurred that was successfully treated with systemic prednisolone and ursodeoxycholic acid. Comprehensive immunologic assessment of the inflammatory infiltrates in the liver revealed the presence of a highly activated cytotoxic CD8 T-cell infiltrate including a SARS-CoV-2-specific CD8 T-cell population that correlated with the peripheral activation of SARS-CoV-2-specific CD8 T cells, indicating that post-COVID-19 vaccination hepatitis involves vaccination-elicited antigen-specific immune responses with distinct histological features compared to bona fide AIH.
Patients and methods
Patient samples
A 52-year old male and 3 health care workers (all HLA-A∗03:01, confirmed by NGS) >26 days post boost (dpb) vaccination who received the mRNA vaccine BNT162b2 were recruited at the University Medical Center Freiburg, Germany. Written informed consent was obtained from all participants. Additionally, 5 samples from healthy liver tissue (colorectal cancer liver metastasis-distant tissue) were obtained from the Institute of surgical pathology in Freiburg. The study was conducted according to federal guidelines and local ethics committee regulations (Albert-Ludwigs-University Freiburg, Germany; vote: #21-1135 and #21-1372) and the Declaration of Helsinki (1975).
Imaging mass cytometry
Liver tissue was obtained by transcutaneous biopsy, formalin-fixed, paraffin-embedded, cut into 4 μm sections and stained as previously described.25 Briefly, after deparaffinization, rehydration, antigen-retrieval and blocking, slides were stained with metal-labeled antibodies and air-dried. Image acquisition of the biopsy (30.912 mm2) and 2.25 mm2 of the control samples was performed using a Hyperion Imaging System (Fluidigm; USA). Regions of interest were laser-ablated spot-by-spot at 200 Hz, resulting in a pixel resolution of 1 μm2. Image visualization was performed with FIJI (v1.52p, ImageJ). Segmentation of single cells was conducted using an adapted unbiased, supervised analysis pipeline using Ilastik (v 1.3.3) and CellProfiler (v 3.1.9). To analyze liver zones the distance of each pixel to GLUL, CD34 and α-SMA was calculated using CellProfiler (v 4.0.4), added to the high-dimensional information of each cell and used for gating in OMIQ (Omiq Inc). Liver zones were defined: Centrilobular (distance to GLUL ≤50 μm), periportal (distance to GLUL >50 μm and distance to CD34 and α-SMA ≤50 μm) and intermediate (distance to GLUL >50 μm and distance to CD34 and α-SMA >50 μm). Absolute cell counts were normalized to 1 mm2. Stacked barplots were created with R version 4.0.1 using ggplot2.
PBMC isolation
Peripheral blood mononuclear cells (PBMCs) were isolated from anticoagulated blood samples after density gradient centrifugation and subsequently stored at −80°C until further usage.
Single-cell suspension from liver biopsy
Remaining liver tissue was mechanically homogenized and filtered through a 70 μm cell strainer (Corning). Cells were washed and directly processed for flow cytometry analysis. Additionally, freshly isolated PBMCs were also stained and analyzed by flow cytometry.
Analysis of spike-specific CD8 T cells
SARS-CoV-2 spike peptide (S378-386: KCYGVSPTK) was synthesized with a purity of >70% (Genaxxon Bioscience), loaded on HLA-A∗03:01 easYmers® (immunAware) and subsequently conjugated with phyocerythrin (PE)-streptavidin (Agilent) according to manufacturer's instructions. Spike(A∗03/S378)-specific CD8 T cells were analyzed after magnetic bead-based enrichment as previously described.10 Briefly, PBMCs were incubated with PE-conjugated tetramerized S378-386-loaded HLA-A∗03:01 easYmers. Similarly, EBV-specific CD8 T cells were detected using PE-conjugated tetramerized LMP-1419-427-loaded HLA-A∗24:02 easYmers. Virus-specific CD8 T cells were enriched by MACS technology using anti-PE beads. Subsequently, both enriched and pre-enriched samples were analyzed by multiparametric flow cytometry. Frequencies of spike-specific CD8 T cells were calculated as described before.10 , 11 Enriched samples with less than 5 virus-specific CD8 T cells were excluded from the final analysis, resulting in a detection limit of 5∗10-6 virus-specific CD8 T cells.
Multiparametric flow cytometry
Antibodies used for flow cytometry analysis are listed in the supplementary CTAT table. FoxP3/Transcription Factor Staining Buffer Set (Thermo Fisher) and Fixation/Permeabilization Solution Kit (BD Biosciences) were used for intranuclear and cytoplasmic molecules, respectively. After fixation of cells in 2% paraformaldehyde/PBS (Sigma), acquisition was performed on LSRFortessa (BD). Data were analyzed with FlowJo, LLC (BD).
Dimensional reduction of multiparametric flow cytometry data
Dimensionality reduction was conducted with R version 4.1.1 using Bioconductor (release 3.13) CATALYST (Version 1.16.2). The analyses were performed on live non-naïve CD8+ T cells including the markers CD137, CD39, CD38, CXCR3, CD127, CXCR6, PD-1. Downsampling to 45,000 cells was performed. Marker intensities were transformed by arcsinh (inverse hyperbolic sine) with a cofactor of 150. Dimensionality reduction on the transformed data was performed by t-distributed stochastic neigbor embedding.
ELISA
Spike-binding antibodies were assessed by Anti-SARS-CoV-2-QuantiVac-ELISA (IgG) (Euroimmun) detecting S1 IgG (<25.6 BAU/ml: negative; 25.6-35.1 BAU/ml: marginally positive; ≥35.2 BAU/ml: positive) according to manufacturer’s instructions.
Results
Clinical course
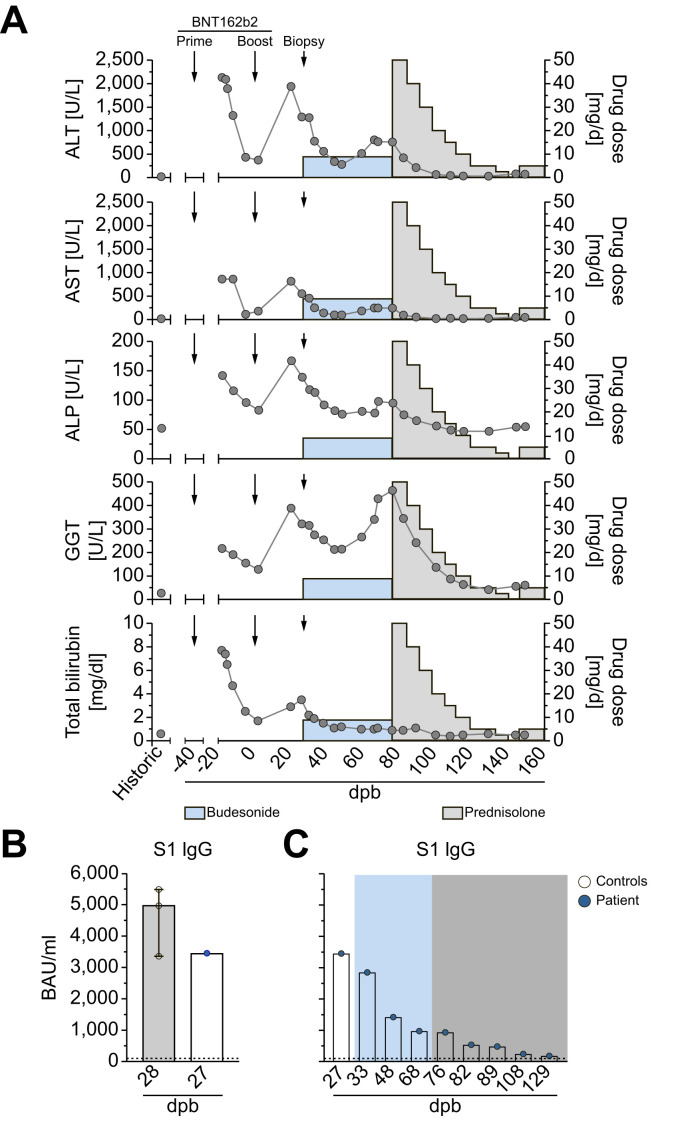
The 52-year-old male patient with no remarkable medical history other than pre-existing hypothyroidism under long-term substitution therapy with levothyroxine and normal historic liver function tests (LFTs) developed progressive nausea, fatigue, loss of appetite and pruritus with symptoms starting approximately 10 days after the first (prime) dose of the BNT162b2 mRNA vaccine. He subsequently developed jaundice and presented at his primary care physician with LFT indicative of acute mixed hepatocellular/cholestatic hepatitis (alanine aminotransferase [ALT] 2,130 U/L, alkaline phosphatase [ALP] 142 U/L, gamma-glutamyltransferase [GGT] 217 U/L, bilirubin 7.7 mg/dl) (Fig. 1 ). The patient was admitted to a primary care center 25 days post first vaccination. Viral hepatitis A, B, C and E as well as cytomegalovirus- and Epstein-Barr virus-infections were excluded by serology and/or PCR testing. HFE genotyping did not reveal hemochromatosis-associated variations. There was also no significant alcohol consumption and autoimmune serology remained inconclusive with borderline anti-mitochrondrial-M2 (AMA-M2) reactivity. The patient recovered rapidly without specific therapy and was discharged with decreasing LFTs after 3 days under the leading differential diagnosis of a toxic hepatitis. Over the next 2 weeks, liver enzymes declined further, with normalization of AST and ALP and the patient received his second (boost) dose of the BNT162b2 mRNA vaccine 41 days after the first vaccination (Fig. 1). 20 dpb vaccination, the patient re-experienced nausea and fatigue. Laboratory testing revealed a relapse of acute mixed hepatitis with (ALT 1,939 U/L, ALP 167 U/L, bilirubin 2.9 mg/dl). He was subsequently referred to our tertiary center at 26 dpb. Autoimmune serology was repeated with mild hyperglobulinemia (IgG levels 1.02-fold of the upper limit of normal, normal IgA and IgM levels), anti-nuclear antibodies (1:200) and borderline positivity for anti-smooth muscle and AMA-M2 antibodies, while tests for anti-liver-kidney-microsomal antibodies remained negative. We performed a liver biopsy that histologically showed interface hepatitis with a moderate degree of lymphoplasmacytic infiltrate and foci of lobular necrosis and apoptosis. Eosinophilic granulocytes were not present. Neither relevant perisinusoidal nor portal fibrosis were observed. Together, these findings are compatible with a probable AIH according to the revised original score for AIH14 and the patient was treated with 9 mg oral budesonide per day. Over the next weeks liver enzymes declined before a relapse occurred 39 days after initiation of therapy (66 dpb), that was controlled subsequently after escalation to systemic steroids in combination with ursodeoxycholic acid. The patient’s LFTs subsequently normalized within 8 weeks (Fig. 1). Anti-spike antibodies did not show major fluctuations with similar titers compared to healthy individuals at the time of diagnosis at 27 dpb vaccination (Fig. 1B) and an expected reduction of titers over time (Fig 1C).
Fig. 1.
Clinical course with hepatitis after BNT162b2 vaccination.
(A) Time course of ALT, AST, ALP, GGT and bilirubin levels after BNT162b2 vaccination in the patient. Arrows indicate the timepoint of BNT162b2 prime and boost vaccination. Arrowheads indicate timepoint of liver biopsy. Duration and dose of budesonide (9 mg/d) and prednisolone therapy (initially 50 mg/d) is shown in light blue and grey colorization. (B) Comparison of anti-spike S1 IgG antibody titers between patients and timepoint-matched vaccines who did not develop hepatitis. (C) Longitudinal analysis of anti-spike S1 IgG antibodies before and after the initiation of therapy. ALP, alanine phosphatase; ALT, alanine aminotransferase; AST, aspartate aminotransferase; dpb, days post boost; GGT, gamma-glutamyltransferase.
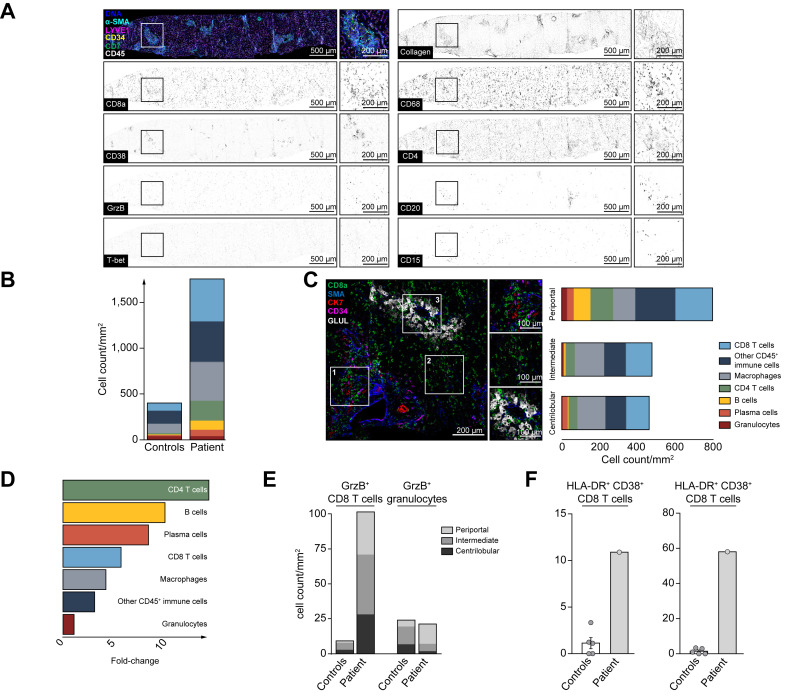
Deep spatial immune analysis of liver tissue
To understand the immune infiltrate in the liver in more detail, in addition to conventional histochemistry, we performed highly multiplexed imaging mass cytometry with a broad panel covering relevant immune populations (supplementary CTAT table). As shown in Fig. 2 A, this revealed infiltrates consisting of T cells, macrophages, B cells, plasma cells and granulocytes in the liver. The absolute number of immune cells was 5.3-fold increased compared to non-diseased control liver tissue obtained from liver resections (Fig. 2B). Interestingly, among the immune infiltrate, CD8 T cells represented the most abundant immune cell subset (465 per mm2), which was unexpected for AIH. In contrast, B cells and plasma cells that are typically enriched in AIH, were found at relatively low numbers (102 per mm2 and 66 per mm2, respectively), even though these populations were also enriched in the immune infiltrate compared to controls (Fig. 2E). These findings suggested a different immune cell contribution compared to typical spontaneous AIH. We next assessed the spatial localization of the different immune cell subsets within the liver parenchyma. The strongest immune infiltration was observed in periportal areas (Fig. 2C). Notably, while B cells and plasma cells were also enriched but predominantly present in periportal areas, CD8 T-cell distribution was panlobular (Fig. 2C, D). To test for immune correlates of hepatic damage, we assessed the cytotoxic granule marker Granzyme B. Interestingly, we observed a strong accumulation of cytotoxic (Granzyme B-positive) CD8 T cells while other Granzyme B-expressing immune cell subsets, such as granulocytes, were not increased (Fig. 2E). These data are also in line with our observation of increased intrahepatic expression of CD38, HLA-DR and transcription factor T-bet as markers of activated effector T cells (Fig. 2A,F). Based on their strong enrichment, widely scattered distribution and activated cytotoxic phenotype within the liver parenchyma, we speculated that CD8 T cells could be drivers of the hepatic inflammation.
Fig. 2.
Deep spatial analysis of the hepatic immune environment reveals immune infiltration dominated by cytotoxic CD8 T cells.
The liver biopsy was analyzed by highly multiplexed IMC. (A) Pseudocolored IMC images of the liver biopsy. Top left: Composite visualization of CD45, CK7, CD34, LYVE1, a-SMA and DNA are indicated by colors. Single marker visualization is shown for markers depicted on the left border of the visualizations. A region of interest is indicated by the box and detailed at higher resolution. Scale bars indicate 500 μm and 200 μm in the inserts, respectively. (B) Cell counts of immune cell subsets in the liver are shown as stacked barplots compared to controls. (C) Composite IMC image visualizing examples of liver zones defined by structural markers: Periportal (top), intermediate (middle) and centrilobular zones (bottom). Immune cell counts within the defined regions visualized as stacked barplots next to the respective inserts. Scale bars indicate 200 μm and 100 μm in the inserts, respectively. (D) Enrichment of indicated immune populations was calculated by dividing cell density in the patient sample by the mean of control samples. (E) Distribution of GrzB-positive CD8 T-cell and granulocyte cell counts within the liver zones. (F) Frequency (left) and cell density (right) of HLA-DR+ CD38+ CD8 T cells are shown for the patient with hepatitis and controls. GrzB, granzyme B; IMC, imaging mass cytometry.
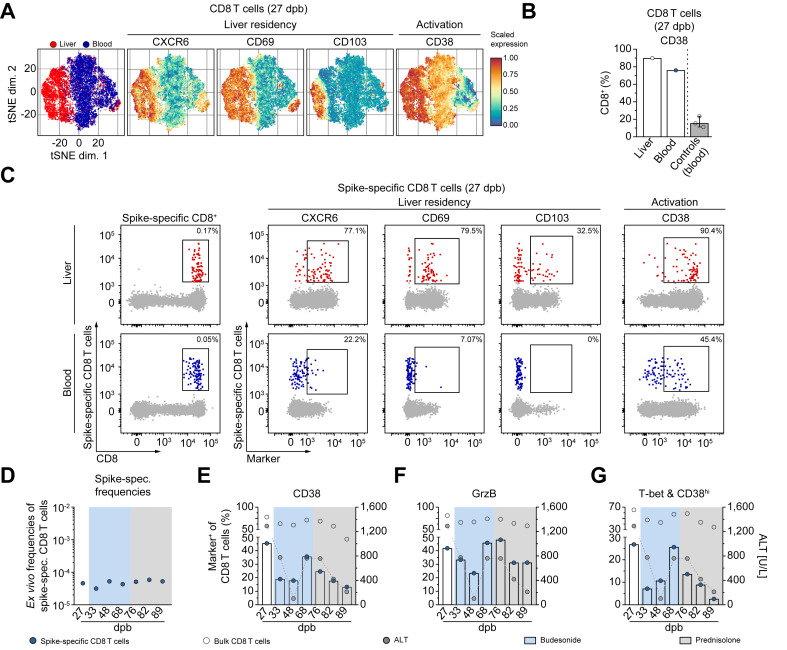
Intrahepatic and longitudinal peripheral immunophenotyping of vaccination-associated CD8 T-cell responses
We next performed a detailed analysis of the intrahepatic and peripheral CD8 T-cell populations using flow cytometry. The patient’s intrahepatic CD8 T-cell population was enriched for markers of tissue residency (CXCR6, CD69 and CD103) and activation (CD38) (Fig. 3 A). Expression of CD38 on CD8 T cells was also observed in the peripheral blood. Interestingly, CD38 expression levels were markedly elevated in the patient compared to post-vaccination timepoint matched control vaccinees who did not develop hepatitis (75.9% vs. 15.4%, respectively) (Fig. 3B). The unusual expansion of activated cytotoxic T cells observed in our spatial analysis led us to hypothesize that vaccination-induced SARS-CoV-2 spike-specific CD8 T cells might contribute to liver disease as we have recently observed rapid induction of SARS-CoV-2 spike-specific CD8 T cells by the BNT162b2 mRNA vaccine.15 Indeed, using a patient-matched HLA-A∗03 tetramer loaded with a SARS-CoV-2-spike epitope (S378-386) we identified spike-specific CD8 T cells. In the peripheral blood, spike-specific CD8 T cells were 10.2-fold more abundant than T cells specific for an EBV-specific CD8 T-cell control epitope (Fig. S1). We also identified spike-specific CD8 T cells in the liver. Compared to the peripheral blood, the intrahepatic CD8 T-cell pool was ∼3.4-fold enriched for spike-specific CD8 T cells (Fig. 3C) and displayed tissue-resident characteristics (CXCR6, CD103, CD69) and strong activation as indicated by CD38 expression (Fig. 3C). Spike protein was not identified in the liver at the time of analysis by immunohistochemistry (data not shown). We next asked whether frequency and activated phenotype of circulating spike-specific CD8 T cells was maintained during therapy. Interestingly, longitudinal analyses showed stable frequencies of circulating spike-specific CD8 T cells (Fig. 3D) with decreasing CD38 expression levels after the initiation of budesonide therapy and coinciding with declining transaminase levels. However, CD38 expression on spike-specific CD8 T cells and other cytotoxicity-associated markers such as GrzB and T-bet increased when the patient relapsed under budesonide therapy, then normalized after introduction of systemic immunosuppressive therapy (Fig. 3E-G). This pattern was not observed for LMP-1419-427-loaded HLA-A∗24:02-restricted EBV-specific CD8 T cells (Fig. S1). It was also not observed for bulk CD8 T-cell analyses, which showed a high abundance of activated cytototoxic CD8 T-cell populations in the periphery (Fig. 3E-G). In sum, these data indicate broad activation of cytotoxic CD8 T cells with the peripheral phenotype of spike-specific CD8 T cells reflecting the clinical response pattern to immunosuppressive therapy.
Fig. 3.
Immunophenotype of peripheral and vaccine-elicited CD8 T cells correlates with hepatitis severity.
(A) t-SNE representation of flow cytometry data comparing non-naïve CD8+ T cells 27 dpb in the patient’s liver (red) and blood (blue). Expression levels of CXCR6, CD69, CD103 and CD38 are indicated (blue: low expression; red: high expression). (B) Quantified expression levels of CD38, 27 dpb on non-naïve CD8+ T cells within the patient’s liver (red) and blood (blue) compared to timepoint matched vaccinees without development of hepatitis. (C) Original bivariate plots showing frequencies of spike-specific (A∗03/S378) CD8+ T cells within the CD8+ T-cell population at 27 dpb, liver (red) and blood (blue). Expression levels of CXCR6, CD69, CD103 and CD38 of spike-specific CD8+ T cells are indicated. (D) Longitudinal analysis of calculated ex vivo spike-specific CD8+ T-cell frequencies. (E) Longitudinal analysis of CD38, (F) GrzB, (G) Tbet+CD38hi CD8+ T cells are shown with time-matched ALT (U/L) levels depicted in grey with connected dots, circulating non-naïve spike-specific CD8+ T cells (blue circle) and non-naïve bulk CD8+ T cells (grey open circle). Colored background indicates the patient’s therapy regime (light blue: budesonide, grey: prednisolone). ALT, alanine aminotransferase; dpb, days post boost; GrzB, granzyme B.
Discussion
AIH-like disease after vaccination against SARS-CoV-2 is now recognized as a rare adverse event not identified in early trials. The widespread use of the vaccine with administration of hundreds of million doses worldwide also raises questions of causality vs. coincidence. In particular, AIH-like disease after vaccination was reported in patients with age and sex characteristics typical for spontaneous AIH.6 , 7 , 10 While some of these cases thus may represent coincidence, a causal relationship to the vaccine is also possible, such as bystander hepatitis driven by elevation of systemic cytokines or chemokines after vaccination, similar to cases occurring in association with natural SARS-CoV-2 infection.13 The varying patterns of clinical manifestation and the wide range of time elapsed between vaccine administration and symptom onset clearly suggest that different mechanisms may contribute to these reported cases. Here, our analysis highlights that activated cytotoxic CD8 T cells, including vaccine-induced spike-specific CD8 T cells, could contribute to disease pathogenesis.
Importantly, AIH is a condition that requires lifelong immunosuppressive therapy in many affected patients.16 It is therefore important to differentiate AIH from possibly transient immune-mediated hepatitis post vaccination. Diagnosis of AIH is typically established using AIH scoring tools informed by LFTs, auto-antibody serology and typical histological features such as interface hepatitis and enrichment of plasma cells.14 In our case, prior to therapy, AIH diagnosis was deemed “probable” based on the modified original AIH score. It is important to note in this context that the first episode of acute hepatitis after the first vaccine dose was self-limiting without therapy, which also guided our choice to initiate therapy with budesonide in an attempt to minimize systemic side effects and to maintain systemic anti-SARS-Cov2 immunity if possible. However, our patient experienced a relapse 3-4 weeks after budesonide therapy and then required systemic steroid therapy, that was empirically combined with ursodeoxycholic acid, a combination used in the treatment of AIH-overlap syndrome that was chosen due to the presence of AMA-M2 antibodies typically found in primary biliary cholangitis.17 The patient subsequently recovered quickly, with gingivitis being the only possible immunosuppression-related adverse event. Due to relapse hepatitis after steroid tapering, the patient was put under long-term maintenance immunosuppressive therapy under which he achieved complete biochemical remission.
Mechanistically, the disease manifestation in our patient was distinct from classical spontaneous AIH, which is typically associated with elevated peripheral immunoglobulins, a plasma cell dominated infiltrate and prominent interface hepatitis. Here, while there was a slight elevation of peripheral immunoglobulins and intrahepatic enrichment of intrahepatic B cells and plasma cells, a more striking correlate was observed at the level of cytotoxic CD8 T cells. Activated cytotoxic CD8 T cells were strongly enriched in the patient liver to an extent that they represented the most abundant intrahepatic immune cell population and included vaccine-elicited SARS-CoV-2-specific responses. Notably, the peripheral activation state of these spike-specific CD8 T cells correlated with hepatitis severity and the clinical course after introduction of immunosuppressive therapy. These results implicate T cells as a pathogenic immune cell type of this vaccine-associated immune hepatitis. The early increase in ALT values after the first and second dose of BNT162b2 and the observation that CD8 T cells including spike-specific CD8 T cells dominate the immune infiltrate also fits with recent observations of an early mobilization of spike-specific CD8 T cells after the first dose of the vaccine.15 Of note, our tetramer reagent likely stains only a fraction of vaccination-induced antigen-specific T cells, fitting to the broad expression of T-cell activation and cytotoxicity markers observed in the analysis of the bulk CD8 T-cell population. However, it is also possible that the broad activation pattern observed involves other, non-SARS-CoV-2-specific “bystander” CD8 T-cell populations. Moreover, the precise mechanism that causes infiltration of spike-specific CD8 T cells into the liver, wherein they adopt features of tissue-resident memory T cells remains unclear. Virus-specific CD8 T cells can accumulate in the liver even if the primary site of infection is distant, such as during influenza infection, and it is possible that the liver can act as a “graveyard” for activated T cells.18 , 19 However, activated cytotoxic CD8 T cells can mediate hepatitis even in the absence of antigen.20 In addition, T-cell receptor-independent, innate-like cytotoxicity of bystander T cells has been described in acute infections.21 , 22 Of note, CXCR6+ CD8+ tissue-resident memory T cells, such as those found in this patient, may mediate auto-aggression in metabolic liver diseases, in response to local inflammatory cues .23 , 24 Whilst these reports raise the possibility of an antigen-independent T cell-mediated hepatitis, another possible explanation could be the presence of their cognate antigen, i.e. the spike protein. While we could not detect spike protein by immunohistochemistry in the liver, it has to be noted that biopsy was performed 27 days after the second vaccine dose and transient expression after vaccination, which could have caused CXCR6-expressing spike-specific CD8 T cells to home to the liver and target antigen-presenting cells, cannot be excluded. However, additional mechanisms, such as antigen cross-recognition may also contribute to the immunopathology. In sum, BNTb163b2 vaccine may trigger immune-mediated hepatitis by mechanisms linked to vaccine-induced cellular immunity. This case illustrates the induction of an unusual CD8 T cell-dominant AIH after BNT162b2 mRNA vaccination, with enrichment of vaccine-induced SARS-Cov2-specific CD8 T cells. In patients with hepatitis manifesting after the first vaccine dose, additional doses may trigger significant hepatic autoimmunity that requires long-term immunosuppression.
Abbreviations
AIH, autoimmune hepatitis; ALP, alanine phosphatase; ALT, alanine aminotransferase; AMA-M2, anti-mitochondrial-M2; AST, aspartate aminotransferase; dpb, days post boost; GGT, gamma-glutamyltransferase; LFTs, liver function tests; PBMCs, peripheral blood mononuclear cells.
Financial support
The work was supported by grants from the German Federal Ministry of Education and Research (01KI2077 to MH and RT) and the German Research Foundation (272983813 to BB, TB, RT, MH, and CNH; 256073931 to BB, RT, MH and CNH; 413517907 to HL, 378189018 to BB). HL and MS are supported by the IMM-PACT-Programme for Clinician Scientists, Department of Medicine II, Medical Center – University of Freiburg and Faculty of Medicine, University of Freiburg, funded by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation) – 413517907. TB and MS are supported by the Berta-Ottenstein-Programme for Clinician Scientists, Faculty of Medicine, University of Freiburg. MH’s work is further supported by the Margarete von Wrangell fellowship (State of Baden-Wuerttemberg).
Authors’ contributions
Study concept and design (TB, MH, BB); experiments and procedures (BC, HS, HL, LW, ESA, KZ, LK, MS); patient sample recruitment (TB, BB), histology assessment (CM, PB), bioinformatics and statistical analysis (BC, HS, HL, ESA); interpretation of data and drafting of the manuscript (TB, MH, BB); revision of the manuscript for important intellectual content (MP, CNH, RT).
Data availability statement
The generated flow cytometry and imaging mass cytometry datasets will be made available in accordance with legal regulations upon reasonable request.
Conflict of interest
The authors declare no conflicts of interest that pertain to this work.
Please refer to the accompanying ICMJE disclosure forms for further details.
Acknowledgments
We thank the patient for donating samples and Saskia Killmer and Marilyn Salvat Lago from the Freiburg mass cytometry facility for excellent technical service.
Footnotes
Author names in bold designate shared co-first authorship
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jhep.2022.03.040.
Supplementary data
The following are the supplementary data to this article:
References
- 1.Polack F.P., Thomas S.J., Kitchin N., Absalon J., Gurtman A., Lockhart S., et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. New Engl J Med. 2020;383:2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Palla P., Vergadis C., Sakellariou S., Androutsakos T. Letter to the editor: autoimmune hepatitis after COVID-19 vaccination. A rare adverse effect? Hepatology. 2022;75:489–490. doi: 10.1002/hep.32156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bril F., Al Diffalha S., Dean M., Fettig D.M. Autoimmune hepatitis developing after coronavirus disease 2019 (COVID-19) vaccine: causality or casualty? J Hepatol. 2021;75:222–224. doi: 10.1016/j.jhep.2021.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clayton-Chubb D., Schneider D., Freeman E., Kemp W., Roberts S.K. Comment to the letter of Bril F et al. “Autoimmune hepatitis developing after coronavirus disease 2019 (COVID-19) vaccine: causality or casualty?”. J Hepatol. 2021 [Google Scholar]
- 5.Lodato F., Larocca A., D’Errico A., Cennamo V. An anusual case of acute cholestatic hepatitis after m-RNA BNT162b2 (Comirnaty) SARS-CoV-2 vaccine: coincidence, autoimmunity or drug related liver injury? J Hepatol. 2021 doi: 10.1016/j.jhep.2021.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Londoño M.-C., Gratacós-Ginès J., Sáez-Peñataro J. Another case of autoimmune hepatitis after SARS-CoV-2 vaccination. Still casualty? J Hepatol. 2021 doi: 10.1016/j.jhep.2021.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McShane C., Kiat C., Rigby J., Crosbie Ó. The mRNA COVID-19 vaccine - a rare trigger of autoimmune hepatitis? J Hepatol. 2021 doi: 10.1016/j.jhep.2021.06.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rocco A., Sgamato C., Compare D., Nardone G. Autoimmune hepatitis following SARS-CoV-2 vaccine: may not be a casuality. J Hepatol. 2021 doi: 10.1016/j.jhep.2021.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shroff H., Satapathy S.K., Crawford J.M., Todd N.J., VanWagner L.B. Liver injury following SARS-CoV-2 vaccination: a multicenter case series. J Hepatol. 2021 doi: 10.1016/j.jhep.2021.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tan C.K., Wong Y.J., Wang L.M., Ang T.L., Kumar R. Autoimmune hepatitis following COVID-19 Vaccination: true causality or mere association? J Hepatol. 2021 doi: 10.1016/j.jhep.2021.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tun G.S.Z., Gleeson D., Dube A., Al-Joudeh A. Immune-mediated hepatitis with the Moderna vaccine, no longer a coincidence but confirmed. J Hepatol. 2021 doi: 10.1016/j.jhep.2021.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fernando B. Autoimmune hepatitis developing after coronavirus disease 2019 (COVID-19) vaccine: one or even several swallows do not make a summer. J Hepatol. 2021 doi: 10.1016/j.jhep.2021.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kabaçam G., Wahlin S., Efe C. Autoimmune hepatitis triggered by COVID-19: a report of two cases. Liver Int. 2021;41:2527–2528. doi: 10.1111/liv.15044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alvarez F., Berg P.A., Bianchi F.B., Bianchi L., Burroughs A.K., Cancado E.L., et al. International Autoimmune Hepatitis Group Report: review of criteria for diagnosis of autoimmune hepatitis. J Hepatol. 1999;31:929–938. doi: 10.1016/s0168-8278(99)80297-9. [DOI] [PubMed] [Google Scholar]
- 15.Oberhardt V., Luxenburger H., Kemming J., Schulien I., Ciminski K., Giese S., et al. Rapid and stable mobilization of CD8+ T cells by SARS-CoV-2 mRNA vaccine. Nature. 2021 doi: 10.1038/s41586-021-03841-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.EASL clinical practice guidelines: autoimmune hepatitis. J Hepatol. 2015;63:971–1004. doi: 10.1016/j.jhep.2015.06.030. [DOI] [PubMed] [Google Scholar]
- 17.Younossi Z.M., Bernstein D., Shiffman M.L., Kwo P., Kim W.R., Kowdley K.V., et al. Diagnosis and management of primary biliary cholangitis. Am J Gastroenterol. 2019;114:48–63. doi: 10.1038/s41395-018-0390-3. [DOI] [PubMed] [Google Scholar]
- 18.Mehal W.Z., Juedes A.E., Crispe I.N. Selective retention of activated CD8+ T cells by the normal liver. J Immunol. 1999;163:3202–3210. [PubMed] [Google Scholar]
- 19.Belz G.T., Altman J.D., Doherty P.C. Characteristics of virus-specific CD8(+) T cells in the liver during the control and resolution phases of influenza pneumonia. Proc Natl Acad Sci U S A. 1998;95:13812–13817. doi: 10.1073/pnas.95.23.13812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bowen D.G., Warren A., Davis T., Hoffmann M.W., McCaughan G.W., Fazekas de St Groth B., et al. Cytokine-dependent bystander hepatitis due to intrahepatic murine CD8 T-cell activation by bone marrow-derived cells. Gastroenterology. 2002;123:1252–1264. doi: 10.1053/gast.2002.36058. [DOI] [PubMed] [Google Scholar]
- 21.Kim J., Chang D.Y., Lee H.W., Lee H., Kim J.H., Sung P.S., et al. Innate-like cytotoxic function of bystander-activated CD8(+) T Cells is associated with liver injury in acute hepatitis A. Immunity. 2018;48:161–173 e165. doi: 10.1016/j.immuni.2017.11.025. [DOI] [PubMed] [Google Scholar]
- 22.Sandalova E., Laccabue D., Boni C., Tan A.T., Fink K., Ooi E.E., et al. Contribution of herpesvirus specific CD8 T cells to anti-viral T cell response in humans. PLoS Pathog. 2010;6 doi: 10.1371/journal.ppat.1001051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dudek M., Pfister D., Donakonda S., Filpe P., Schneider A., Laschinger M., et al. Auto-aggressive CXCR6(+) CD8 T cells cause liver immune pathology in NASH. Nature. 2021;592:444–449. doi: 10.1038/s41586-021-03233-8. [DOI] [PubMed] [Google Scholar]
- 24.Pfister D., Nunez N.G., Pinyol R., Govaere O., Pinter M., Szydlowska M., et al. NASH limits anti-tumour surveillance in immunotherapy-treated HCC. Nature. 2021;592:450–456. doi: 10.1038/s41586-021-03362-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schwabenland M., Salié H., Tanevski J., Killmer S., Lago M.S., Schlaak A.E., et al. Deep spatial profiling of human COVID-19 brains reveals neuroinflammation with distinct microanatomical microglia-T-cell interactions. Immunity. 2021;54:1594–1610.e1511. doi: 10.1016/j.immuni.2021.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The generated flow cytometry and imaging mass cytometry datasets will be made available in accordance with legal regulations upon reasonable request.