Abstract
Objectives:
To analyze the frequency and rates of community respiratory virus infections detected in patients at the National Institutes of Health Clinical Center (NIHCC) between January 2015 and March 2021, comparing the trends before and during the coronavirus disease 2019 (COVID-19) pandemic.
Methods:
We conducted a retrospective study comparing frequency and rates of community respiratory viruses detected in NIHCC patients between January 2015 and March 2021. Test results from nasopharyngeal swabs and washes, bronchoalveolar lavages, and bronchial washes were included in this study. Results from viral-challenge studies and repeated positives were excluded. A quantitative data analysis was completed using cross tabulations. Comparisons were performed using mixed models, applying the Dunnett correction for multiplicity.
Results:
Frequency of all respiratory pathogens declined from an annual range of 0.88%–1.97% between January 2015 and March 2020 to 0.29% between April 2020 and March 2021. Individual viral pathogens declined sharply in frequency during the same period, with no cases of influenza A/B orparainfluenza and 1 case of respiratory syncytial virus (RSV). Rhino/enterovirusdetection continued, but with a substantially lower frequency of 4.27% between April 2020 and March 2021, compared with an annual range of 8.65%–18.28% between January 2015 and March 2020.
Conclusions:
The decrease in viral respiratory infections detected in NIHCC patients during the pandemic was likely due to the layered COVID-19 prevention and mitigation measures implemented in the community and the hospital. Hospitals should consider continuing the use of nonpharmaceutical interventions in the future to prevent nosocomial transmission of respiratory viruses during times of high community viral load.
The coronavirus disease 2019 (COVID-19) pandemic has had a profound impact on society at large and on medicine and healthcare, specifically. Although healthcare-associated bacterial infections have increased during the pandemic, 1,2 one striking pandemic-associated finding was a dramatic decrease in influenza and other respiratory virus infections around the world, both among the public 3–12 as well as in healthcare institutions. 13–16
The National Institutes of Health Clinical Center (NIHCC) is a federally funded 200-bed clinical research hospital located in Bethesda, Maryland. NIH investigators recruit patients, who often have rare, unknown, or difficult-to-treat disorders, to participate in clinical research studies. In our hospital, a substantial decrease in respiratory infections diagnosed in our clinical laboratory occurred during the early stages of the pandemic. This finding stimulated us to conduct this retrospective study of respiratory virus infections in our hospital to quantify the decrease and to assess trends in these infections in our institution before and during the pandemic.
Beginning in 2014, symptomatic patients were tested for respiratory viral infections using a newly acquired multiplex polymerase chain reaction (PCR) test. Because many NIHCC patients are immunocompromisedand stay for extended periods, they are at increased risk for healthcare-associated infections. Healthcare providers are encouraged to have a low threshold for testing all patients who have respiratory symptoms. This guidance was maintained throughout the pandemic, leading to testing for non–severe acute respiratory coronavirusvirus 2 (non–SARS-CoV-2)in parallel with SARS-CoV-2 testing, though we know some healthcare providers opted to forgo non–SARS-CoV-2 testing for symptomatic patients.
Methods
Design and population
Upon detecting a stark change in the trend of respiratory virus infections in 2020 and 2021, the NIHCC Hospital Epidemiology Service conducted a retrospective study comparing frequency and rates of community respiratory viruses detected in NIHCC patients from January 2015 through March 2021. The data reviewed included results from respiratory specimens collected from both inpatients and outpatients with respiratory symptoms seen at the NIHCC.
Data collection
Respiratory specimens from patients with respiratory symptoms are tested using the BioFire multiplex PCR respiratory pathogen panels (RPPs; Biofire Diagnostics, Salt Lake City, UT) (Table 1). The NIHCC Department of Laboratory Medicine performs RPPs on nasopharyngeal swabs and washes, oropharyngeal swabs, tracheal aspirates, bronchoalveolar lavages, and bronchial washes. Beginning January 2021, samples requiring urgent testing for SARS-CoV-2 were instead tested via the Cepheid Xpert Xpress Quadplex (Cepheid, Sunnyvale, CA), a rapid PCR test that also tests for RSV, influenza A and influenza B. All respiratory virus results from every patient tested for respiratory viruses from January 2015 through March 2021 were extracted from the electronic medical record. During the pandemic, visitors were also tested, and these data are included for completeness.
Table 1.
Respiratory Pathogen Panel (RPP) Tests Collected From the NIH Clinical Center Patients Between January 2015 and March 2021
| Test | Frequency | % of All Tests |
|---|---|---|
| Parainfluenza 1 | 8,145 | 5.95 |
| Parainfluenza 2 | 8,142 | 5.95 |
| Parainfluenza 3 | 8,103 | 5.92 |
| Parainfluenza 4 | 8,144 | 5.95 |
| Influenza A | 7,699 | 5.63 |
| Influenza B | 7,720 | 5.64 |
| Adenovirus | 8,102 | 5.92 |
| Rhinovirus/Enterovirus | 7,667 | 5.60 |
| Respiratory Syncytial Virus | 8,075 | 5.90 |
| Human Metapneumovirus | 8,101 | 5.92 |
| Coronavirus HKU1 | 8,120 | 5.93 |
| Coronavirus 229E | 8,132 | 5.94 |
| Coronavirus OC43 | 8,102 | 5.92 |
| Coronavirus NL63 | 8,132 | 5.94 |
| Bordetella pertussis | 8,148 | 5.96 |
| Chlamydophila pneumoniae | 8,148 | 5.96 |
| Mycoplasma pneumoniae | 8,149 | 5.96 |
| Total | 136,823 | 100.00 |
NIHCC policy requires negative test results to remove patients from respiratory isolation for some viral infections. For this reason, patients often have multiple positive results for the same virus. We excluded duplicate test results related to such serial testing. If serial testing was not done to discontinue isolation but multiple positive results for the same virus were detected, 2 additional assessments of the results were completed to determine whether duplicate results should be included or excluded. If the duplicate positives occurred within 1 year, only the earlier result was included; if the positive samples were obtained >1 year apart, record review was used to determine whether the patient had a persistent or newly acquired infection. Finally, samples from challenge studies of influenza and RSV were also excluded from the analysis.
Statistical analysis
Data are reported as frequencies and percentages, and were analyzed using mixed models for longitudinal data, and applied the Dunnettcorrection for multiplicity. Comparisons were of warm and cool months through the study period relative to the COVID-19 period (April 2020–March 2021) as the reference. Data were analyzed using SAS version 9.4 software (SAS Institute, Cary, NC).
Study definitions
For the purposes of this study, environmental and behavioral nonpharmaceutical interventions at the NIHCC are listed in detail in Table 3. Warm months are defined as April through September of each year. Cold months are defined as October of a preceding year through March of the following year.
Table 3.
Nonpharmaceutical Factors Possibly Contributing to Decreased Detection of Respiratory Virus Infections
| Arena | Actions Taken |
|---|---|
| Public COVID-19 mitigation strategies | Masks |
| Physical distancing | |
| Hand hygiene | |
| Cough etiquette | |
| Quarantining | |
| School closures | |
| Workplace closures | |
| Community lockdowns | |
| Border closures | |
| Limited public assemblies | |
| Limitations on travel | |
| Healthcare-associated COVID-19 mitigation strategies used in the NIHCC | Syndromic screening of all entering the hospital |
| Allowing only staff essential to patient care into the hospital | |
| Universal masking | |
| Protective eyewear for providers when within 2 m (6 feet) of patients for >5 minutes | |
| Offering testing for symptomatic and asymptomatic staff (ref) | |
| Hand hygiene | |
| Isolation of symptomatic suspected or diagnoses COVID-19 patients | |
| Serial testing for patients believed to have been exposed to COVID-19 | |
| Reduced non–COVID-19 hospital census | |
| Visitor restrictions | |
| Suspension of elective procedures | |
| Admissions and pre-AGP testing |
Note. AGP, aerosol-generating procedure.
Results
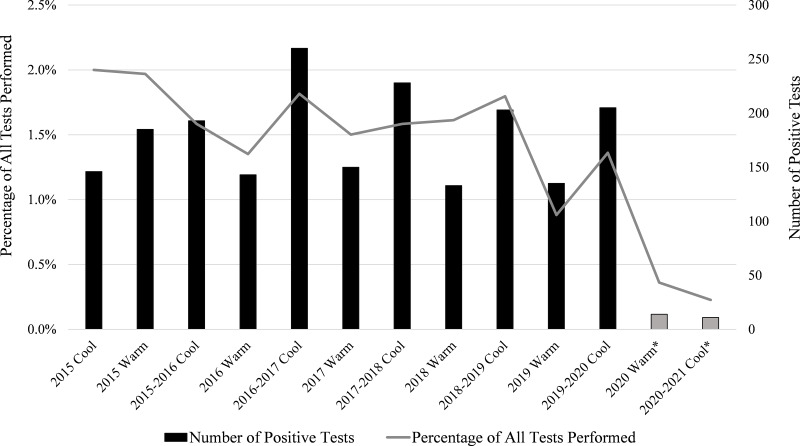
After excluding data corresponding to duplicate infections and challenge studies, 136,823 results remained from 3,329 unique patients over the study period. The frequency of tests for each virus can be found in Table 1. Figure 1 depicts the change in overall detection rate for the combined non–COVID-19 respiratory viruses during 2015–2021. The detection rate was 2% during the early cool months of 2015 and steadily dropped to 1.35% by the warm months of 2016. The rates hovered at ∼1.5%–1.8% through 2019. Beginning in the warm months of 2020, a stark drop in the data occurred: the non–COVID-19 respiratory virus detection rate dropped to 0.36%. The rate remained low during the cool months of the COVID-19 pandemic (October 2020 through March 2021) at 0.23%.
Fig. 1.
Detection of all respiratory pathogens among NIH Clinical Center patients from January 2015–March 2021.* indicates the COVID-19 period; compared to the COVID-19 reference period (2020 warm period and 2020–2021 cool period), the rates for all of the previous year and seasonal periods were substantially higher (P < .001; P = .002 for 2019 warm period).
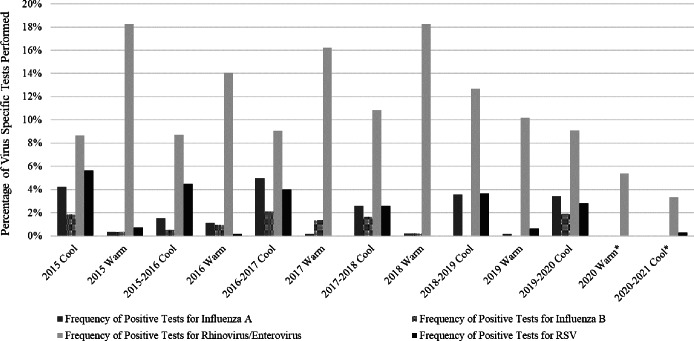
Changes in the detection rates for 4 important respiratory pathogens are portrayed in Table 2, with the frequency representing the percentage of virus specific tests with positive results. The most commonly detected viruses in NIHCC patients—influenza A, influenza B, and RSV—are seasonal in nature; their detection during the pandemic significantly decreased. Influenza A appeared mainly in cool months, with a historic frequency between 2.5% and 5%. However, during the cool months of the COVID-19 pandemic, no cases of influenza A infection were detected. Influenza B also tends to be most prevalent in cool months, but it is slightly less seasonal. For the cool months of 2016–2017 through the cool months of 2019–2020, influenza B was detected in 1.3%–2.2% of submitted samples. In the cool months of 2018–2019, we detected no cases. From April 2020 through March 2021, no cases of influenza B were detected. RSV is detected in Clinical Center patients almost exclusively during cool months. The infection frequency during cool months from 2015 through 2019–2020 was consistently between 2.6% and 5.6%. During the cool months of the COVID-19 period, October 2020 through March 2021, the RSV detection rate dropped to 0.29%.
Table 2.
Change in the Detection Rates for Four Respiratory Pathogens Among NIH Clinical Center Patients Between January 2015 and March 2021
| Year and Season | Frequency of Positive Tests | |||||||
|---|---|---|---|---|---|---|---|---|
| Influenza A, % | P Value | Influenza B, % | P Value | Rhinovirus/ Enterovirus, % |
P Value | RSV, % | P Value | |
| 2015 Cool | 4.25 | <.001 | 1.86 | .026 | 8.65 | NS | 5.63 | <.001 |
| 2015 Warm | 0.36 | NS | 0.36 | NS | 18.29 | <.001 | 0.72 | NS |
| 2015–2016 Cool | 1.53 | NS | 0.56 | NS | 8.72 | NS | 4.50 | <.001 |
| 2016 Warm | 1.13 | NS | 0.95 | NS | 14.04 | <.001 | 0.17 | NS |
| 2016–2017 Cool | 5.00 | <.001 | 2.14 | <.001 | 9.05 | NS | 4.00 | <.001 |
| 2017 Warm | 0.17 | NS | 1.36 | NS | 16.21 | <.001 | 0.00 | NS |
| 2017–2018 Cool | 2.58 | .006 | 1.64 | .017 | 10.86 | .003 | 2.61 | <.001 |
| 2018 Warm | 0.20 | NS | 0.20 | NS | 18.28 | <.001 | 0.00 | NS |
| 2018–2019 Cool | 3.60 | <.001 | 0.00 | NS | 12.70 | <.001 | 3.65 | <.001 |
| 2019 Warm | 0.17 | NS | 0.00 | NS | 10.19 | .007 | 0.66 | NS |
| 2019–2020 Cool | 3.45 | <.001 | 1.92 | .004 | 9.11 | .050 | 2.82 | .005 |
| 2020 Warm a | 0.00 | 0.00 | 5.38 | 0.00 | ||||
| 2020–2021 Coola | 0.00 | 0.00 | 3.35 | 0.29 | ||||
|
All COVID-19
(4/2020–3/2021) |
0.00
(Ref) |
0.00
(Ref) |
4.27
(Ref) |
0.17
(Ref) |
||||
Note. NS, not statistically significant.
Warm months were defined as April–September of the year, and cool months were defined as October of a preceding year through March of the following year.
Comparisons were between each seasonal period versus the reference period of the COVID-19 pandemic (April 2020–March 2021), and reportedP values corrected for multiplicity using the Dunnett test.
These seasonal periods are listed separately for information purposes as they are part of the COVID-19 reference period.
Rhinovirus/enterovirusdetection from 2015 through the cool months of 2019–2020 ranged from 8.65% up to 18.29% during the pre–COVID-19 period. However, during the warm months of 2020, infection frequency dropped to 5.38%, and it fell even lower to 3.35% during the cool months of 2020–2021.
Discussion
Our review confirmed the significant decrease of non–SARS-CoV-2 respiratory viruses, including influenza A, influenza B, RSV, and rhino/enterovirus, during the first year of the COVID-19 pandemic compared to the previous 5 years. Several factors (both community and healthcare related) may help explain the observed decrease in respiratory virus infections (Table 3). Whereas many of the factors listed in Table 3 have been suggested as contributing to the reduction in respiratory infections, quantification of the contribution of any one of these factors is difficult, if not impossible, because most were implemented simultaneously as COVID-19 mitigation strategies. Lee et al 17 analyzed Korean national data to demonstrate that implementation of nationally sponsored COVID-19 mitigation strategies was associated with diminished influenza activity and a truncated influenza season. Olsen et al 8 noted substantial decreases in detection of influenza in the United States, Australia, Chile, and South Africa. Chan et al 18 noted that, while influenza A remained suppressed, other respiratory viruses (eg, RSV, enteroviruses/rhinoviruses) returned after schools were reopened in Singapore. Nawrocki et al 19 found a clear association between physical distancing policies and community transmission of 11 non-COVID-19 respiratory viruses.
In our institution, molecularly diagnosed respiratory infections decreased dramatically, despite the personal stress of the pandemic as well as a host of additional pandemic-related factors. Intuitively, these factors might have been thought to facilitate rather than inhibit transmission of viral respiratory pathogens (Table 4). Nonetheless, even in the face of intense institutional COVID-19 activities and increased acuity of inpatients who remained hospitalized, detection of these viral respiratory pathogens dramatically decreased (Figs. 1 and 2; Table 2). Molecularly diagnosed influenza A and influenza B infections decreased to zero during the pandemic.
Table 4.
Pandemic-Associated Factors That Could Have Facilitated Respiratory Virus Transmission in Healthcare Settings
| Factor Type | Description |
|---|---|
| Personal | Pandemic emotional stresses |
| Staffing shortages | |
| Surge stress in emergency rooms and COVID-19 units | |
| Presenteeism | |
| Environmental | Supply chain shortages of personal protective equipment and standard supplies |
| Overcrowded emergency rooms and ICUs | |
| Medical | Hospitalized non–COVID-19 patients were generally sicker than typically, and likely more susceptible to respiratory virus infections. |
Note. ICU, intensive care unit.
Fig. 2.
Frequency of detection by virus among NIH Clinical Center patients between January 2015 and March 2021. Observations of substantial statistical differences between year and seasonal periods for each virus are specified in Table 2. *indicates the COVID-19 period.
Our study had several limitations. First the patient population at the NIHCC is not typical, even for most academic centers. The Clinical Center’s patient population is focused in 2 areas—patients who have rare, often heritable chronic diseases (many of whom have disseminated malignancies) and phase 1 and 2 clinical trials. Most of the patient population isimmunosuppressed, placing these patients at high risk for all types of infections, including repeatedly positive viral test results. The inclusion and exclusion criteria described earlier controls for the possibility of repeat positives for the same infection but may also exclude some reinfections incorrectly presumed to be long-term infections.
A second limitation is that milder infections that did not prompt clinicians to order testing may be underrepresented. Because of the pandemic, the threshold for ordering such tests was likely lowered, but the focus may have been on ruling out severe acute respiratory coronavirus virus 2 (SARS-CoV-2). A third limitation is that many aspects of care in our hospital changed dramatically in response to the pandemic. The hospital census declined substantially because only acutely ill patients were hospitalized, elective admissions were curtailed, and elective procedures were postponed. Furthermore, visitors were restricted; only staff essential to patient care were allowed into the hospital; and dedicated COVID-19 care units (including an intensive care unit) were created.
Finally, some investigators have explored whether direct viral–viral interactions may play a role in these findings. 20–23 The ecologic aspects of seasonal and pandemic viral infections are areas of active research, but they are currently incompletely defined.
The decrease in the incidence of molecularly diagnosed respiratory viral infections in our hospital during the first 12 months of the COVID-19 pandemic was striking. Numerous factors noted above and in Table 3 likely contributed to this reduction. Many, if not most, published manuscripts suggest the primary reason for such a decrease relates directly to the implementation of COVID-19 mitigation strategies (Table 3). 3,8,13–16,24–37 However, as noted previously, demonstrating the effect of any individual intervention is often challenging. Universal masking represented a major departure from prior infection prevention strategies in our institution that we suspect substantially affected the risk for respiratory virus transmission. A recently published meta-analysis that examined results from 72 studies conclusively demonstrated that several mitigation strategies were associated with a substantial decrease in the risk for transmission of SARS-CoV-2, including mask wearing, handwashing, and physical distancing. 38 The effectiveness of universal masking (both for personal protection and source control) has been a striking feature of this pandemic.
The colder weather in the late fall and early winter of 2021 may already be heralding the return of non-SARS-COV-2 respiratory infection. Some institutions have observed an increase in RSV and other respiratory virus infections. 39
The COVID-19 pandemic continues, with the current δ (delta) variant increasing in prevalence in the upper Midwest and the troubling discovery of the newly detected o (omicron) strain. 40 The persistence, and perhaps even escalation, of pandemic COVID-19 cases argues for the consistent application of the effective nonpharmaceutical interventions discussed above. Even when the pandemic subsequently subsides, when influenza or another respiratory virus again emerges, we will advocate for empiric universal masking in our institution.
Acknowledgments
We acknowledge the support of NIH Clinical Center leadership, our patients (NIHCC research subjects), and the staff of the NIHCC Laboratory Medicine and Nursing Departments.
Financial support
No financial support was provided relevant to this article.
Conflicts of interest
All authors report no conflicts of interest relevant to this article.
References
- 1. Weiner-Lastinger LM, Pattabiraman V, Konnor RY, et al. The impact of coronavirus disease 2019 (COVID-19) on healthcare-associated infections in 2020: a summary of data reported to the National Healthcare Safety Network. Infect Control Hosp Epidemiol 2021:1–14. [DOI] [PubMed] [Google Scholar]
- 2. Palmore TN, Henderson DK. Healthcare-associated infections during the coronavirus disease 2019 (COVID-19) pandemic. Infect Control Hosp Epidemiol 2021;42:1372–1373. [DOI] [PubMed] [Google Scholar]
- 3. Groves HE, Piche-Renaud PP, Peci A, et al. The impact of the COVID-19 pandemic on influenza, respiratory syncytial virus, and other seasonal respiratory virus circulation in Canada: a population-based study. Lancet Reg Health Am 2021;1:100015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kim J, Gomez Gomez RE, Hong K, Yum S, Jang J, Chun BC. Changing influenza activity in the Southern Hemisphere countries during the COVID-19 pandemic. Int J Infect Dis 2021;108:109–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kim JH, Roh YH, Ahn JG, et al. Respiratory syncytialvirus and influenza epidemics disappearance in Korea during the 2020–2021 season of COVID-19. Int J Infect Dis 2021;110:29–35. [DOI] [PubMed] [Google Scholar]
- 6. Kuitunen I. Influenza season 2020–2021 did not begin in Finland despite the looser social restrictions during the second wave of COVID-19: a nationwide register study. J Med Virol 2021;93:5626–5629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lee L, Butt K, Buckrell S, Nwosu A, Sevenhuysen C, Bancej C. National influenza mid-season report, 2020–2021. Can Commun Dis Rep 2021;47:1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Olsen SJ, Azziz-Baumgartner E, Budd AP, et al. Decreased influenza activity during the COVID-19 pandemic—United States, Australia, Chile, and South Africa, 2020. Morb Mortal Wkly Rep 2020;69:1305–1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rizzo KR, Hoover C, Jain S, et al. Influenza and SARS-CoV-2 coinfectionsin California, USA, September 2020–April 2021. Emerg Infect Dis 2021;27:2923–2926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sullivan SG, Carlson S, Cheng AC, et al. Where has all the influenza gone? The impact of COVID-19 on the circulation of influenza and other respiratory viruses, Australia, March to September 2020. Euro Surveill 2020;25(47). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Uyeki TM, Wentworth DE, Jernigan DB. Influenza activity in the US during the 2020–2021season. JAMA 2021;325:2247–2248. [DOI] [PubMed] [Google Scholar]
- 12. Zipfel CM, Colizza V, Bansal S. The missing season: the impacts of the COVID-19 pandemic on influenza. Vaccine 2021;39:3645–3648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. de Souza Luna LK, Perosa DAH, Conte DD, et al. Different patterns of influenza A and B detected during early stages of COVID-19 in a university hospital in Sao Paulo, Brazil. J Infect 2020;81:e104–e105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Osorio-Lopez EA, Rivera-Buendia F, Nevarez-Lujan J, Rivas-Pichon E, Vilar-Compte D. Nosocomial influenza in patients with cancer before the coronavirus disease 2019 (COVID-19) era and one year after the pandemic: can we do any better in hospitals? Infect Control Hosp Epidemiol 2021. doi: 10.1017/ice.2021.337. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Stamm P, Sagoschen I, Weise K, et al. Influenza and RSV incidence during COVID-19 pandemic-an observational study from in-hospital point-of-care testing. Med Microbiol Immunol 2021;210:277–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wong SC, Lam GK, AuYeung CH, et al. Absence of nosocomial influenza and respiratory syncytial virus infection in the coronavirus disease 2019 (COVID-19) era: implication of universal masking in hospitals. Infect Control Hosp Epidemiol 2021;42:218–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lee H, Lee H, Song KH, et al. Impact of public health interventions on seasonal influenza activity during the COVID-19 outbreak in Korea. Clin Infect Dis 2021;73:e132–e140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chan HC, Tambyah PA, Tee NWS, Somani J. Return of other respiratory viruses despite the disappearance of influenza during COVID-19 control measures in Singapore. J Clin Virol 2021;144:104992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Nawrocki J, Olin K, Holdrege MC, et al. The effects of social distancing policies on non–SARS-CoV-2 respiratory pathogens. Open Forum Infect Dis 2021;8(7):ofab133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chan KF, Carolan LA, Korenkov D, et al. Investigating viral interference between influenza a virus and human respiratory syncytial virus in a ferret model of infection. J Infect Dis 2018;218:406–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Linde A, Rotzen-Ostlund M, Zweygberg-Wirgart B, Rubinova S, Brytting M. Does viral interference affect spread of influenza? Euro Surveill 2009;14:19354. [PubMed] [Google Scholar]
- 22. Nickbakhsh S, Mair C, Matthews L, et al. Virus-virus interactions impact the population dynamics of influenza and the common cold. Proc Natl Acad Sci USA 2019. ;116:27142–27150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Peng JY, Shin DL, Li G, Wu NH, Herrler G. Time-dependent viral interference between influenza virus and coronavirus in the infection of differentiated porcine airway epithelial cells. Virulence 2021;12:1111–1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cheng W, Yu Z, Liu S, et al. Successful interruption of seasonal influenza transmission under the COVID-19 rapid response in Zhejiang Province, China. Public Health 2020;189:123–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Chiu NC, Chi H, Tai YL, et al. Impact of wearing masks, hand hygiene, and social distancing on influenza, enterovirus, and all-cause pneumonia during the coronavirus pandemic: retrospective national epidemiological surveillance study. J Med Internet Res 2020;22(8):e21257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Chow A, Hein AA, Kyaw WM. Unintended Consequence: influenza plunges with public health response to COVID-19 in Singapore. J Infect 2020;81:e68–e69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cowling BJ, Ali ST, Ng TWY, et al. Impact assessment of nonpharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Health 2020;5(5):e279–e288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Eisen AKA, Gularte JS, Demoliner M, et al. Low circulation of influenza A and coinfection with SARS-CoV-2 among other respiratory viruses during the COVID-19 pandemic in a region of southern Brazil. J Med Virol 2021;93:4392–4398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lagace-Wiens P, Sevenhuysen C, Lee L, Nwosu A, Smith T. Impact of nonpharmaceutical interventions on laboratory detections of influenza A and B in Canada. Can Commun Dis Rep 2021;47:142–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Li Y, Wang X, Msosa T, de Wit F, Murdock J, Nair H. The impact of the 2009 influenza pandemic on the seasonality of human respiratory syncytial virus: a systematic analysis. Influenza Other Respir Viruses 2021;15:804–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Pierce A, Haworth-Brockman M, Marin D, Rueda ZV, Keynan Y. Changes in the incidence of seasonal influenza in response to COVID-19 social distancing measures: an observational study based on Canada’s national influenza surveillance system. Can J Public Health 2021;112:620–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Qi Y, Shaman J, Pei S. Quantifying the impact of COVID-19 nonpharmaceutical interventions on influenza transmission in the United States. J Infect Dis 2021;224(9):1500–1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Soo RJJ, Chiew CJ, Ma S, Pung R, Lee V. Decreased influenza incidence under COVID-19 Control Measures, Singapore. Emerg Infect Dis 2020;26:1933–1935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Tempia S, Walaza S, Bhiman JN, et al. Decline of influenza and respiratory syncytial virus detection in facility-based surveillance during the COVID-19 pandemic, South Africa, January to October 2020. Euro Surveill 2021;26(29). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Wiese AD, Everson J, Grijalva CG. Social distancing measures: evidence of interruption of seasonal influenza activity and early lessons of the SARS-CoV-2 pandemic. Clin Infect Dis 2021;73(1):e141–e143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Williams TC, Sinha I, Barr IG, Zambon M. Transmission of paediatric respiratory syncytial virus and influenza in the wake of the COVID-19 pandemic. Euro Surveill 2021;26(29). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Yeoh DK, Foley DA, Minney-Smith CA, et al. Impact of coronavirus disease 2019 public health measures on detections of influenza and respiratory syncytial virus in children during the 2020 Australian winter. Clin Infect Dis 2021;72:2199–2202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Talic S, Shah S, Wild H, et al. Effectiveness of public health measures in reducing the incidence of COVID-19, SARS-CoV-2 transmission, and COVID-19 mortality: systematic review and meta-analysis. BMJ 2021;375:e068302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Li ZJ, Yu LJ, Zhang HY, et al. Broad impacts of COVID-19 pandemic on acute respiratory infections in China: an observational study. Clin Infect Dis 2021. doi: 10.1093/cid/ciab942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Update on omicron. World Health Organization website. https://www.who.int/news/item/28-11-2021-update-on-omicron. Updated November 28, 2021. Accessed November 28, 2021.