Abstract
Obesity is a worldwide epidemic affecting over 13% of the adult population and is defined by an excess of body fat that predisposes comorbidities. It is considered a multifactorial disease in which environmental and genetic factors interact, and it is a risk marker for cardiovascular disease. Lifestyle modifications remain the mainstay of treatment for obesity based on adequate diet and physical exercise. In addition, obesity is related to cardiovascular and skeletal muscle disorders, such as cardiac hypertrophy, microvascular rarefaction, and skeletal muscle atrophy. The discovery of obesity-involved molecular pathways is an important step to improve both the prevention and management of this disease. MicroRNAs (miRNAs) are a class of gene regulators which bind most commonly, but not exclusively, to the 3′-untranslated regions of messenger RNAs of protein-coding genes and negatively regulate their expression. Considerable effort has been made to identify miRNAs and target genes that predispose to obesity. Besides their intracellular function, recent studies have demonstrated that miRNAs can be exported or released by cells and circulate within the blood in a remarkably stable form. The discovery of circulating miRNAs opens up intriguing possibilities for the use of circulating miRNA patterns as biomarkers for obesity and cardiovascular diseases. The aim of this review is to provide an overview of the recent discoveries of the role played by miRNAs in the obese phenotype and associated comorbidities. Furthermore, we will discuss the role of exercise training on regulating miRNAs, indicating the mechanisms related to these alterations.
Keywords: Obesity, MicroRNA, Microvascular rarefaction, Cardiac hypertrophy, Biomarker, Exercise training
Introduction
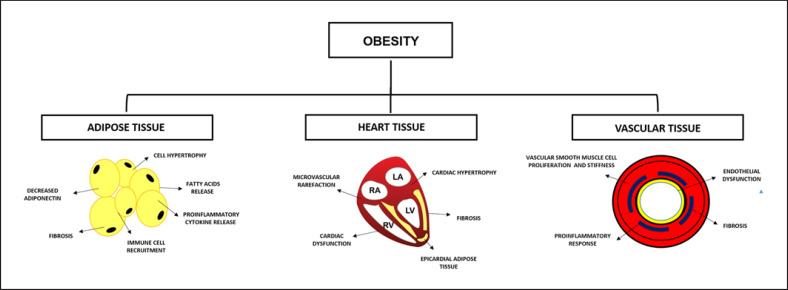
Obesity and overweight are defined as excessive fat accumulation that leads to health risks [1]. Fat cells, or adipocytes, are the main component of adipose tissue, and distinct roles have emerged for adipose tissue depots in regulating susceptibility to obesity [2]. World Health Organization (WHO) [1] data have shown that the incidence of obesity has been increasing since 1975 (quadrupled for children aged 6–11 years, tripled in adolescents aged 12–19 years, and doubled in adults), and in 2016, more than 1.9 billion adults were overweight, and 650 million were characterized with the obesity phenotype. The WHO also characterized obesity as a major risk factor for the development of chronic diseases such as diabetes, cancer, and various cardiovascular disorders, given its increasing incidence and prevalence [1]. Therefore, obesity leads to various metabolic disorders, which results in phenotypic and functional damages on adipose tissue and the cardiovascular system, as illustrated in Figure 1 [3, 4, 5, 6, 7].
Fig. 1.
Adipose tissue and cardiovascular system remodeling and dysfunction in response to obesity.
Many therapies have been proposed to decrease the prevalence and incidence of obesity, also to mitigate comorbidities caused by obesity (i.e., cardiovascular disorders). Exercise and diet are the primary treatments for the cardiovascular and skeletal muscle damages caused by obesity [8, 9, 10]. However, little is known about the molecular changes in obesity and what possible cellular functions could be used as an anti-obesity treatment.
MicroRNAs (miRNAs) have been studied as a therapy for many diseases, including obesity and metabolic disorders [11, 12]. miRNAs are a class of small noncoding RNA molecules of 18–22 nucleotides whose main function is RNA silencing and post-transcriptional regulation of gene expression [13, 14]. The miRNA recognizes a messenger RNA (mRNA) target by base-pair complementarity and negatively regulates its expression by inhibiting or degrading the mRNA by preventing its translation into a protein [13, 14]. There are numerous studies in the scientific literature that describe the role of miRNAs in many cellular processes. Therefore, many efforts have been made to modulate the expression of miRNAs to inhibit, restore, or even increase their expression to use them as a therapy.
Clinical and blood biomarkers for obesity, such as body mass index, fasting blood glucose, triglycerides, and cholesterol, are well-established predictors of the disease and its comorbidities. However, there are limited insights regarding the underlying pathophysiology. The use of miRNAs as biomarkers in circulation represents an attractive approach for early screening to identify individuals at risk of developing diseases and may reflect adipose tissue expression [11]. In addition, many studies have shown that miRNAs participate in the adipogenesis process, such as lipotoxicity in the heart, cardiac hypertrophy, atherosclerosis, microvascular rarefaction, phenotypic changes in skeletal muscle, and other comorbidities [2, 11, 15].
Exercise training is one of the main treatments for obesity. It has many well-known effects such as increasing metabolic activity, weight loss, and attenuating obesity sarcopenia, aiding in the regulation of secretion or activity of hormones that often show abnormal function in obesity (e.g., ghrelin and insulin) and in glycemic control [16, 17, 18, 19]. In addition, accumulated evidence indicates that exercise training also plays a role in controlling the expression of miRNAs [16, 17, 20, 21, 22, 23]. Therefore, the phenotypic and functional effects generated by exercise training are also related to molecular and epigenetic changes, such as changes in the expression of miRNAs [24, 25, 26]. The therapeutic effects of exercise training in obese individuals are also related to the control of the expression of several miRNAs in different tissues [27].
Therefore, the aim of this review is to describe the role of miRNAs as regulators of the obese phenotype. We will also review how miRNAs control cellular functions that determine changes in tissues and systems, such as adipose tissue and the cardiovascular system. The second objective is to describe the role of exercise training as an agent for regulating miRNAs expression and how it can be used to give insights for the development of new therapeutic tool to alleviate obesity disorders.
The Effects of Exercise Training on Obesity
Physical inactivity is the main cause of most chronic diseases [28]. On the other hand, studies show that aerobic (i.e., running, cycling, swimming, etc.) and resistance (i.e., weightlifting) exercise training are treatments for obesity and related metabolic dysfunctions.
Also, keeping an exercise routine is a predictor of long-term weight maintenance or prevention of weight regain. Da Rocha et al. [29] showed a decreased body mass index and body fat percentage in obese individuals when there was a combination of resistance and aerobic exercise training. These data are corroborated by Skrypnik et al. [30], who compared the effects of 3-month (1) aerobic exercise training and (2) aerobic exercise training combined with resistance training, both on anthropometric measures such as body mass index, and circulatory parameters in obese women. According to the study, there was a significant and similar decrease in all mentioned parameters in both conditions [30]. Also, the authors showed that both endurance and mixed endurance strength training promoted significant increases in cardiorespiratory fitness and exercise tolerance when compared to sedentary condition, counteracting the harmful impact of obesity.
Vilarreal et al. [31] tested the difference between (1) aerobic training, (2) resistance training, and (3) the combination of both in 141 obese subjects on weight management. The participants were subjected to 6-month activities, and the researchers noted that weight loss was similar and significant across all groups compared to the control group. The resistance and combined training groups developed more lean mass than the aerobic and control groups. The aerobic training group showed more oxygen consumption than the resistance and control groups. The data show that physical activities are important for weight management in obesity, but combined training is the strategy that most achieves positive results.
Aerobic exercise is capable of decreasing the adipose tissue content due to an increase in the activity of lipoprotein lipase. It leads to an increase in circulation levels of the high-density lipoprotein (HDL-cholesterol) and its subfraction HDL2. Also there was a chemical composition of low-density protein (LDL-cholesterol) modification, making them less atherogenic [32]. In addition, the fat weight loss (≥5% of the baseline body weight) is considered an effective way of reducing cardiovascular risk factors [33]. The STRRIDE study [34] has confirmed that there is a dose-response relationship between exercise volume and fat mass loss but no significant impact on fat mass loss between the moderate and vigorous intensity groups, indicating that fat mass loss is more related to exercise volume than intensity. The current guidelines recommend 250–300 min of exercise duration per week for long-term weight loss and for prevention of weight regain in obese individuals [35].
Studies have documented that the inflammatory cytokine secretion production by adipose tissue is elevated in the presence of adiposity. The higher inflammatory state in obesity contributes to several clinical diseases [36, 37]. In fact, the vascular dysfunction, recognized by microvascular rarefaction and decreased blood flow is well-established in obesity and associated disorders, leading to tissue hypoxia [38]. Hypoxia has been associated with macrophage infiltration and pro-inflammatory gene expression increases, while adiponectin expression and anti-inflammatory protein in adipose tissue decrease [39]. In contrast, weight loss is able to improve the metabolic syndrome and the chronic inflammation in obese subjects [40]. In agreement, findings from several studies also support an anti-inflammatory effect of exercise training on obesity. Exercise training promotes angiogenesis, vasodilation, and increased blood supply [16, 17, 21], thereby reducing hypoxia and pro-inflammatory cytokines in adipose tissue and other tissues like muscle and vessels, and circulation [36, 37].
Studies have been demonstrating that exercise training leads to epigenetic changes [41, 42]. Therefore, exercise training influences miRNA expression in different cellular tissues, playing an important role in the programming gene expression in pathological and physiological processes [23, 43]. The therapeutic effects of exercise training in obese individuals are related to the control of the expression of several miRNAs in different tissues [20, 21, 22, 23, 44].
Baggish et al. [45], demonstrated that runners had alterations in circulating miRNA levels that are abundant in specific tissues such as the heart (miRNA-208a), skeletal muscle (miRNA-1, −133a and −499-5p), and vessels (miRNA-126), after a marathon race (42 km). Interestingly, these miRNAs' post-run levels returned to their baseline values after 24 h, suggesting that miRNAs can be used as biomarkers both to determinate the molecular adaptations caused by exercise and to clinically assist in the identification of tissue changes [45]. Although the magnitude of tissue-specific miRNA expression and the precise mechanisms of release of cellular miRNAs to extracellular environment remain largely unknown on the exercise training scenario, recent studies suggest that the expression of these intracellular and circulating miRNAs can be associated with the beneficial effects of exercise on obesity.
Throughout this review, we have covered studies that show the role of miRNAs associated with obesity and its comorbidities, as well as the existing evidence on the regulation of physical exercise on the expression of miRNAs in the obesity phenotype.
Adipose Tissue: Obesity, miRNAs, and Exercise Training
Obesity triggers macrophage infiltration and adipokine release, which is associated with low-grade inflammation of adipose tissue [46]. The inflammatory environment within adipose tissue induces insulin resistance, oxidative stress, and endothelial damage, which leads to diabetes and cardiovascular diseases (Fig. 1) [15, 46, 47]. The involvement of miRNAs in obesity pathogenesis is well-established since many of them have been found modified in adipose tissue (white, brown, and beige) during obesity and closely associated with obesity-related metabolic disorders [2, 11, 48]. Thus, a proper understanding of the molecular events regulating adipogenesis can provide essential information in identifying new targets and effective therapeutic strategies against obesity.
Evidence that miRNA plays a significant role in adipocyte development came from a study showing that the deletion of Dicer, a key enzyme for miRNA processing, repressed adipocyte differentiation and the formation of adipose tissue during adipogenesis. It was also accompanied by reduced adipocyte markers such as peroxisome proliferator-activated receptor-gamma (PPARγ), tumor necrosis factor (TNF) receptor superfamily member 6 (also known as FAS), glucose transporter type 4, and fatty acid-binding protein 4 [49]. Another study with a specific Dicer deletion in differentiated adipocytes showed a reduced level of various adipogenic-associated transcripts and inhibited lipogenesis in white adipocytes. On the other hand, Dicer was not required for brown fat formation [50]. In the same context, Mori et al. [51] showed that fat-specific Dicer-KO mice developed a form of lipodystrophy that was characterized by a loss of intra-abdominal and subcutaneous white fat with enlargement and “whitening” of interscapular brown fat, suggesting the important role of miRNAs in the control of adipogenesis-related metabolic disorders.
Several miRNAs participate in adipocyte differentiation through a series of regulated stages, including differentiation into preadipocytes, growth arrest and clonal expansion, and terminal differentiation into adipocytes. miRNAs-141, −143, −200a-c, −204, and −429 are important in early adipocyte cell fate determination, whereas miRNA-17-92, −27a-b, −130, −378, and −378-3p have been suggested to be involved in terminal differentiation and mature white adipocyte function [52]. In the same sense, Ahn et al. [53] showed that the highest fold change was observed in miRNA-146b in mature adipocyte, suggesting it as a positive regulator of accelerated adipocyte differentiation through modulation of sirtuin 1 (SIRT1) and Kruppel-like factor 7 (KLF7). Also, miRNA-146b was increased in high-fat diet-induced obese mice and ob/ob mice, whereas the expression of its target gene SIRT1 was decreased in white adipose tissue [54]. Indeed, previous studies showed that miRNA-146b had been described as a positive regulator of adipocyte proliferation and differentiation [54].
In accordance, Xu et al. [55] showed that miRNA-26b is an obesity-related miRNA abundantly expressed in mice and mature human adipocytes and is associated with the expression of adipokines. In addition, miRNA-26a-b was also identified as a determinant for brown adipogenesis and energy dissipation activity by targeting the ADAM metallopeptidase domain 17 (ADAM17) [56]. On the other hand, transgenic mice overexpressing miRNA-196a induced increased brown adipose tissue content and energy expenditure and were resistant to obesity when fed a high-fat diet. miRNA-196a suppressed the expression of the white fat gene Hoxc8 post-transcriptionally and repressed the CCAAT enhancer-binding proteins β (C/EBPβ), a master switch for the brown fat gene program, during the brown adipogenesis of white fat progenitor cells. In fact, increased brown adipose content can help counter the adverse effects of obesity [57].
Studies that used miRNA array analyses are important to determine expression profiles. Ortega et al. [47] isolated fat cells from both lean and obese subjects for miRNA microarray and identified 5 upregulated miRNAs (-99a, −1229, −125b, −221, and −199a-5p) and 4 downregulated miRNAs (-185, −139-5p, −484, and −130b) that were different between lean and obese without type-2 diabetes mellitus subjects. Martinelli et al. [58] evaluated whether miRNA dysfunction contributed to obesity. The authors analyzed, by microarray, the expression profile of 1,458 miRNAs and 42 were differentially expressed in subcutaneous adipose tissue from nondiabetic severely obese and nonobese adults. miRNA-519d was overexpressed, whereas the protein levels of PPARα (a predicted miRNA-519d target) were lower in severely obese subjects compared with nonobese subjects, suggesting that miRNA-519d induces metabolic imbalance and adipocyte hypertrophy in obesity [58]. Also, Shi et al. [59] showed that miRNA-148 was increased in both obese human subjects and mice fed a high-fat diet. Conversely, Lozano-Bartolomé et al. [60] demonstrated that miRNA-181a-5p and −23a-3p were reduced in adipose tissue from obese subjects, and its overexpression contributed to TNF-α downregulation in visceral white adipose tissue. In this way, expression of miRNAs-143 and −103 was significantly decreased in adipocytes of obese mice [61]. Curiously, miRNA-34a appeared to be dysregulated during obesity. In fact, miRNA-34a KO mice gained more weight at baseline and in response to a high-fat diet. In addition, epididymal white adipose tissue in miRNA-34a KO had a smaller adipocyte area, which significantly increased with a high-fat diet accompanied by an increased expression of metabolic genes involved in lipid uptake (cluster of differentiation 36), de novo lipogenesis (fatty acid synthase), and cholesterol biosynthesis (3-hydroxy-3-methylglutaryl-coenzyme A reductase), which caused increases in adipocyte total and free cholesterol and is associated with adipocyte hypertrophy [62].
In addition to the adipocyte cell subtypes, other cellular constituents, such as endothelial cells, fibroblasts, stem cells, neurons, and immune cells, may contribute to obesity. High-fat feeding reduced miRNA-10a-5p levels in adipose tissue macrophages, and treatment of mice with a miRNA-10a-5p mimic suppressed pro-inflammatory responses and improved systemic glucose tolerance in obesity [63]. Ferrante et al. [64] evaluated whether adipocyte-derived exosomes from obese and lean subjects contained mediators capable of activating end-organ inflammatory and fibrotic signaling pathways. The authors found 55 differentially expressed miRNAs accompanied by growth factor beta (TGFβ) signaling and Wnt/β-catenin signaling among the top canonical pathways expected to be altered in visceral adipocytes from obese subjects compared to lean subjects [64].
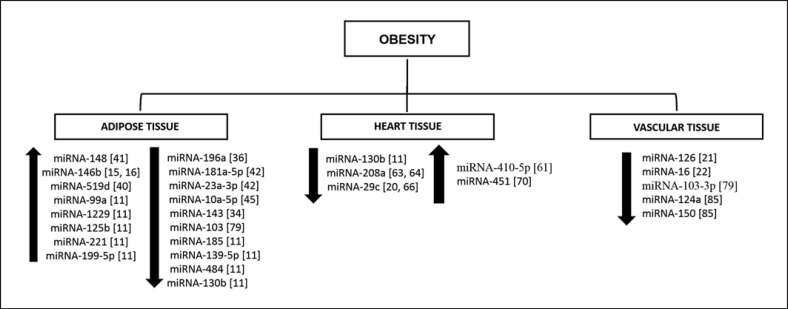
miRNA mimetics and inhibitors offer an option for the development of tissue-specific therapeutic interventions. The miRNA-33 family (miRNA-33a-b) is implicated in lipid metabolism and atherosclerotic plaque formation and rupture [65, 66]. The miRNA-33 family targets the adenosine triphosphate-binding cassette transporter A1 (ABCA1) and genes involved in fatty acid oxidation, important regulators of high-density lipoprotein synthesis and reverse cholesterol transport. Silencing of the miRNA-33 family increased hepatic expression of ABCA1 receptors and plasma high-density lipoprotein levels [65, 66]. Mice treated with anti-miRNA-33 for 4 weeks showed an increase in circulating high-density lipoprotein levels and enhanced reverse cholesterol transport to the plasma, liver, and feces. Consistent with this, anti-miRNA-33-treated mice showed reductions in plaque size and lipid content, increased markers of plaque stability, and decreased inflammatory gene expression. These studies indicate therapeutic promise for the treatment of dyslipidemias that increase cardiovascular disease risk using a miRNA-33 family inhibitor [67]. The dysregulated miRNA profile in obesity-induced adipose tissue is illustrated in Figure 2.
Fig. 2.
Dysregulated miRNA profile associated with the obesity phenotype in different tissues (e.g., adipose, heart, and vascular). miRNA, microRNA.
Studies on the role of exercise training on the expression of miRNAs in obesity are still incipient. Few studies deal with the expression of miRNAs in the fatty tissue of trained obese individuals, despite the large number of studies showing that exercise training has a direct influence on adipose tissue, including increased lipolysis, increased mitochondrial density in adipocytes, increased expression of cholinergic receptors in adipocytes, among others [68]. In this context, Tsiloulis et al. [69] conducted a study to determine the expression of miRNAs in adipocytes that are responsive to aerobic exercise and to determine the exercise-responsive miRNAs that control metabolism. The authors performed a large-scale sequencing analysis on the fat tissue of overweight men before and after 6 weeks of endurance training. Although the authors observed an increase in the subjects' adipocyte lipolysis, there was no change in the expression of miRNAs in the sequencing. There was a tendency to reduce miRNA-10b [69]. Also, Brandão et al. [70] showed that aerobic exercise training upregulates Dicer in adipose tissue of mice and humans, increasing overall miRNA expression in adipose tissue; and upregulation of miRNA-203-3p limits glycolysis in adipose under conditions of metabolic stress. However, the effects of exercise training on Dicer expression and miRNA biogenesis are unknown in the obesity context [70]. These data will provide a framework for further studies on exercise training and obesity in adipose tissue involving miRNAs.
Circulating miRNAs in Obesity and Exercise Training
While the majority of miRNAs are detected in intracellular environment, there are a great number of miRNAs, commonly known as circulating miRNAs, that have also been detected in extracellular environment, being exported or released by cells into the circulation [11, 71, 72, 73]. miRNAs are very stable in body fluids (plasma, urine, saliva), microvesicles (exosomes, microparticles, apoptotic bodies), and protein/lipoprotein complexes (high-density lipoprotein ([HDL]) and Argonaute 2. Upon uptake by target recipient cells, circulating miRNAs can regulate translation of complementary mRNAs. Thus, miRNAs can be explored for their roles in intercellular communication affecting physiological processes, and also miRNAs could be used in the development of molecular biomarkers for various diseases, including obesity and associated comorbidities [73, 74, 75]. Indeed, adipose-derived circulating miRNAs may regulate gene expression in other tissues highlighting their “endocrine-like” systemic effects [76].
There is a growing body of evidence that has demonstrated that circulating miRNAs are dysregulated in subjects with obesity or metabolic syndrome, and some of these dysregulated miRNAs are closely associated with obesity measures, markers of inflammation, and diabetes measures, suggesting a diagnostic role of these miRNAs in the detection and classification of morbid obesity [49]. Ortega et al. [11] showed that morbidly obese patients had a marked increase in miRNA-140-5p, −142-3p, and −222, and decreased levels of miRNA-532-5p, −125b, −130b, −221, −15a, −423-5p, and −520c-3p. Heneghan et al. [77] showed that circulating levels of miRNA-17-5p and −132 were decreased in obesity, and this change was also reflected in the expression of miRNAs in omental fat tissue from the same individuals. In agreement, Liu et al. [78] also showed that the circulating levels of miRNA-1934, which were decreased in obese subjects, were inversely correlated with body mass index, low-density lipoprotein cholesterol, insulin resistance, and inflammatory marker. Iacomino et al. [43] assessed the profile of circulating miRNAs expressed in plasma samples of overweight or obese and normal weight prepubertal children from a European cohort. Gene arrays were employed to differentially screen the expression of 372 miRNAs, and miRNAs-31-5p, −2355-5p, and −206 were differentially expressed and correlated with obesity [43]. It is likely that additional circulating miRNAs will be identified as biomarkers for cardiovascular disease. This type of study represents a rapidly evolving area of research [78].
Shi et al. [59] showed that miRNA-148a could be a potential biomarker of obesity. This miRNA plays a key role in adipogenesis by inhibiting Wnt1. Wnt-induced changes in gene expression result in repression of adipogenic transcription factors, such as C/EBPα and PPARγ [79]. Wang et al. [80] showed that adipocytes secreted miRNA-130b during adipogenesis, reflecting the degree of obesity, and could serve as a potential biomarker for hypertriacylglycerolemia and metabolic syndrome.
It is noteworthy that some studies have demonstrated the modulation of circulating miRNAs induced by exercise training, pointing them as possible biomarkers of the harmful effects of intense exercise training as a potential tool [81, 82]. Additionally, studies suggest dose-response relationships between aerobic exercise and circulating miRNA expression, varying under different exercise type, duration, and intensity [83, 84]. However, there are few studies about exercise-induced circulating miRNAs in the obesity phenotype [85].
Bao et al. [86] analyzed the expression of miRNAs-126, miRNA-130b, miRNA-221, and miRNA-222 in the circulation of nonobese and obese individuals after a single session of aerobic exercise. It was found that this set of miRNAs had an increased baseline state before the exercise session in obese individuals, and there was a pronounced increase in the content of this set of miRNAs in the circulation of obese subjects after exercise [86]. These miRNAs are linked to inflammation pathways, so it is observed that an acute session of aerobic exercise increased the number of miRNAs in circulation that signal inflammation in obese individuals more than in nonobese individuals. There is no evidence of a chronic effect of aerobic exercise on the expression of this set of miRNAs. Corroborating, Russo et al. [87] showed miRNA-146a-5p, but not miRNA-126, was significantly increased in obese patients as compared with controls and decreased in patients after a 3-month physical activity program characterized by aerobic training sessions of 90 min administered twice a week. Exercise-induced miRNA-146-5p levels were correlated with beneficial effects on waist circumference, the inflammatory and lipid parameters, indicating the use of miRNA-146a-5p as a biomarker and predictor of the clinical response to physical activity in obesity. Recently, de Mendonça et al. [88] demonstrated that aerobic training changed the circulating extracellular vesicles' miRNA profile of diet-induced obese mice, including decreases in miRNA-122, −192, and −22 levels. Aerobically trained obese mice also showed reduced adipocyte hypertrophy and increased numbers of smaller adipocytes and the expression of adipogenesis markers, and ATP-citrate lyase enzyme activity. Other miRNAs are possibly involved in these effects and may contribute to the overall effect of aerobic training and should be further investigated [88].
Therefore, the use of miRNAs as potential biomarkers and their potential therapeutic measures can be useful for early detection and treatment of disorders, including heart disorders caused by obesity. One of the advantages of the use of miRNAs would be its easy detection, which would be ideal as a specific biomarker.
Heart Tissue: Obesity, miRNAs, and Exercise Training
There is a consensus that obesity can be a precursor of cardiovascular disorders that could trigger a heart failure phenotype (Fig. 1). Obese individuals have double the risk of heart failure compared to individuals with a normal body mass index. In a study from Kenchaiah et al. [89], the authors analyzed 5,881 subjects (3,177 women and 2,704 men), and the results demonstrated that an increase of one unit in body mass index generated a 5% increase in the risk of heart failure in men and 7% for women.
Several factors have been involved in obesity-related cardiovascular disorders, such as inflammation, neurohormonal activation with an increased sympathetic tone, elevated leptin and insulin concentrations, obstructive sleep apnea, increased free fatty acid turnover, and intramyocardial and subepicardial fat deposition [90]. In addition, miRNAs have been described as critical regulators of cardiovascular function and play important roles in almost all aspects of cardiovascular biology, including heart disorders caused by obesity [48].
Studies utilizing microarray have been important to elucidate the role of miRNAs in cardiac disorders induced by obesity. In this sense, Ortega et al. [11] conducted a study with 97 patients (40 obese patients with heart failure, 40 lean patients with heart failure, and a control group of 17 healthy lean patients), using a computational prediction, the authors identified miRNA expression alterations in these different phenotypes. The plasma sample analyses of the individuals identified a decrease in miRNA-130b expression in the obese group with the heart failure phenotype when compared to the other phenotypes (lean heart failure group and control group) [11]. This result was corroborated by a study that used microarray analysis to identify differentially regulated miRNAs in the heart of rats fed a high-fat diet. Zou et al. [91] showed that miRNA-410-5p was markedly upregulated in the cardiac tissues of obese rats. miRNA-410-5p activates the TGFβ signaling pathway by targeting Smad 7, which is associated with cardiac fibrosis and dysfunction induced by obesity. Thus, these miRNAs possibly represent a potential therapeutic target for the treatment of cardiac disorders caused by obesity; however, it is necessary to analyze the molecular mechanisms manipulated by them [80].
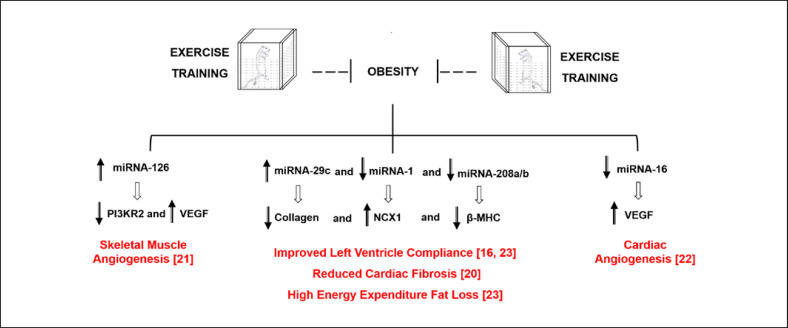
In 2000, the Olson laboratory group from Texas University published a series of studies showing the pivotal role of miRNAs in counteracting cardiac disorders [92, 93]. In 2007, the Olson group published an article showing that continuous stress in the heart caused by thoracic aortic banding led to an increase in beta myosin heavy chain (β-MHC) expression and a decrease in alpha myosin heavy chain (α-MHC) expression in the heart [93]. This gene expression change was accompanied by the dysregulated expression of miRNA-208a [93]. This miRNA is expressed in intron 27 of the α-MHC gene, and a cardiac-specific miRNA [94]. Van Rooji et al. [93] were the first to demonstrate that the inhibition of a miRNA could treat cardiac disorders. In this case, a decrease in miRNA-208a led to regulation of factors that led to decreased β-MHC expression after cardiac stress, showing that this miRNA plays a key role in cardiac homeostasis. Later, in 2012, the same group published an article showing that miRNA-208a directly targeted MED-13, a unit of the mediator complex that regulates the transcription of thyroid hormone [92]. This study used transgenic overexpressing MED13 animals and animals with anti-miR for miRNA-208a that were fed a high-fat diet. Both had a lean phenotype with increased energy expenditure and resistance to weight gain even when exposed to a high-fat diet [92]. This study concluded that there is an important association between MED13 and miRNA-208a in the heart, which is necessary for systemic homeostasis. Fernandes et al. [23] showed that obese Zucker rats had an increase of 57% in miRNA-208a levels, compared to the lean group, which was accompanied by a decrease of 39% in the MED13 levels. However, when these animals were subjected to swimming training, the miRNA-208 and MED13 levels normalized when compared to the sedentary lean group. This study demonstrated that aerobic exercise training modulated the expression of specific miRNAs and, consequently, their target, suggesting a potential therapeutic target for obesity-associated cardiac disorders [23].
miRNA-29c has also emerged as an important factor in cardiac remodeling because it has the potential to target the collagen gene directly (66). Animals that overexpressed miRNA-29c through the use of an LNA mimic showed a significant reduction in IA and IIIA collagen expression in infarcted animals [95]. Silveira et al. [20] demonstrated that the expression of miRNA was downregulated in the heart of obese Zucker rats, and this decrease was also followed by an increase in cardiac collagen content. Cardiac fibrosis was restored when these obese animals were submitted to aerobic training. Curiously, this study also demonstrated that miRNA-1 expression was upregulated and that exercise was able to normalize their expression and thus regulate the expression of proteins in the calcium signaling pathway [20]. This once again highlights the role of exercise as a strategy to modulate the expression of miRNAs and establish cardiac homeostasis in obesity [82].
Marchand et al. [96] identified miRNA-322 as protective against high-fat diet-induced cardiac dysfunction in mice by regulating the insulin signaling pathway. In Kuwabara's study, it was shown that cardiac hypertrophy induced in animals after 20 weeks of a high-fat diet exacerbated the increase in miRNA-451 in the heart, which increased cellular toxicity [97]. However, a knockout model for miRNA-451 showed protection against cardiomyopathy induced by a high-fat diet, and there was an attenuation of lipotoxicity induced by palmitate. Finally, this attenuation was associated with the regulation of the direct target of miRNA-451, calcium-binding protein 39 [97]. Curiously, this article also shows that miRNA-451 was directly regulated by GATA4, and this transcription factor has been shown in the literature to play an important role in cardiac hypertrophy process [97, 98]. In an editorial in Circulation Research, Lopaschuk and Ussher concluded that Kuwabara's findings were of high clinical relevance and that miRNAs are great candidates for the treatment of obesity and cardiovascular disorders caused by it [99]. All dysregulated miRNAs in obesity-induced heart tissue are illustrated in Figure 2. Although our knowledge of the roles of miRNAs in cardiac disorders has greatly improved, additional research is needed to identify and validate miRNAs as biomarkers for the diagnosis and prognosis of obesity-related cardiomyopathy.
Vascular Tissue: Obesity, miRNAs, and Exercise Training
miRNAs present in the vascular endothelium are also potential therapeutic targets to correct the inflammation, capillary rarefaction, defective angiogenesis, and endothelial dysfunction observed in obesity. Endothelial dysfunction is well-established in obesity and is considered an early predictor of atherosclerosis, which increases the risk for the occurrence of cardiovascular events [100]. Strong predictors for cardiovascular events are carotid intima-media thickness and fibrosis and plaque formation in the carotid segments. These predicators are highly correlated with adiposity (Fig. 1) [101, 102]. Obesity is also associated with microvascular rarefaction and a significant decrease in myocardial vascular endothelial growth factor (VEGF) and eNOS expression [103].
The understanding of the role of miRNAs in regulating specific vascular function may help with the prevention and identification of new therapeutic strategies for obesity. There is growing evidence for an important role of miRNAs in modulating crucial biological process, such as inflammation [104], vascular endothelial and smooth muscle cells [105, 106], reactive oxygen species [107], adipocyte differentiation and function [108], and insulin resistance [2].
There is evidence showing the role of aerobic exercise in controlling the expression of miRNAs in obese individuals. Fernandes et al. [22] demonstrated the role of aerobic exercise training in modulating deregulated miRNA in obesity that contributed to the microvascular rarefaction observed in cardiac tissue from obese Zucker rats. The study showed that aerobic exercise was a nonpharmacological strategy to prevent cardiac capillary rarefaction induced by obesity due to its capacity to restore the levels of cardiac miRNA-16 in obese animals. The downregulation of miRNA-16 induced by exercise training increased VEGF expression, which is critical for the angiogenesis observed in the cardiac microcirculation from obese Zucker rats [22].
In the same sense, Gomes et al. [21] investigated the role of aerobic exercise counteracting capillary rarefaction in the skeletal muscle generated by obesity. The authors investigated the effects of aerobic exercise training on the expression of miRNA-126 on skeletal muscle angiogenesis in obese Zucker rats. It was observed that obese rats showed capillary rarefaction compared to the lean controls. However, exercise training normalized the capillary density in obese rats. The authors observed that exercise training on obese rats increased the levels of VEGF, PI3K, and eNOS proteins. Also, an increased level of miRNA-126 expression and a decreased expression of its target, PI3KR2 (PI3K inhibitor, an important mediator of the VEGF signaling pathway), were observed [21].
Studies have also shown that exercise training improves vascular function by normalizing miRNA expression in obese humans. Dimassi et al. [109] conducted a study with obese women and lean controls. The aim of the study was to determine the effect of 8 weeks of exercise training on the expression of miRNAs related to inflammation and vascular function in obesity. The results showed that women with obesity had a high prevalence of cardiovascular risk factors and a higher level of circulating miRNA-carrying microparticles compared to healthy individuals, and the profile of miRNAs was significantly different in the 2 groups. The effects after the training protocol were reduced body mass index, inflammatory profile, and vascular function in both groups. In addition, physical training increased the level of miRNA-carrying microparticles in both groups. The authors performed an in silico analysis and selected 9 miRNAs related to the inflammatory profile. The training protocol increased 4 miRNAs in both groups. There was also a correlation between microparticles, increased expression of miRNA-124a and −150, and the decreased expression of inflammatory cytokines such as adiponectin, TNFα, or IL-6 [109]. The functional roles for these miRNAs in vascular tissue (Fig. 2) will require further study.
Conclusion
Given the high prevalence of obesity worldwide and the risk that it represents in the development of comorbidities, in recent years, the search field for treatment strategies has expanded. We note in this review that obesity results in an abnormal expression of miRNAs, which are influential factors for the function of adipose tissue, vessels, and the heart [18, 21, 81, 97].
Exercise training is frequently prescribed as a treatment for obesity. It is known to have positive effects on adipocytes, vessels, and heart function, and morphology (Fig. 3). The expression of miRNAs is also controlled by physical exercise. The benefits from physical activity in these tissues are primarily generated by better control of the expression of many miRNAs [20, 21, 22, 23]. Therefore, the modulation of miRNAs is a promising therapeutic strategy for obesity. Understanding how the miRNAs are controlled by exercise training is a possible strategy for the development of new treatments that can prevent injuries in specific tissues and improve their function in individuals unable to do exercise.
Fig. 3.
Chronic aerobic exercise-induced miRNA expression counteracting diseases and associated risk factors leading to obesity in different tissues. PI3KR2, phosphoinositide-3-kinase regulatory subunit 2; VEGF, vascular endothelial growth factor; NCX1, Na+/Ca2+-exchange protein 1; β-MHC, beta-myosin heavy chain; miRNA, microRNA.
As shown throughout this literature review, within these strategies, exercise training has shown great promise as a therapy for obesity. Exercise can modulate miRNA expression, and it could be an advantage because of its easy detection, which would be ideal as a specific biomarker for the regulatory control of disorders induced by obesity. The miRNAs described thus far as being involved in obesity and metabolic syndrome may be important targets for the treatment of these diseases. In this way, it opens a window for the use of miRNA-based therapies, once miRNAs occur naturally in the bloodstream, target multiple mRNAs, have low toxicity, and patients show a good tolerance for them [11, 62, 98].
In conclusion, this review reinforces the importance of exercise training as a well-known strategy to combat obesity and also provides evidence that exercise training could control the expression of miRNAs that are related to tissue injuries generated by obesity. Additional studies are required to help identify new exercise-derived tissue-specific and circulating miRNAs in obesity, and their potential role as a therapeutic target of obesity-associated disorders in response to exercise.
Conflict of Interest Statement
The authors declare that they have no conflict of interest.
Funding Sources
This study was supported by the São Paulo Research Foundation (FAPESP) (grant Nos. 2015/17275-8, 2015/22814-5, and 2017/22069-3) and Coordination of Superior Level Staff Improvement (CAPES). Edilamar M. Oliveira was supported by CNPQ (grant No. 313479/2017-8).
Author Contributions
All authors contributed to the writing and editing of the manuscript. All authors have read and approved the final version of the manuscript and agreed with the order of presentation of the authors.
References
- 1.World Health Organization . Obesity and overweight: fact sheets. WHO; 2020. Obesity and overweight. [Google Scholar]
- 2.Arner P, Kulyté A. MicroRNA regulatory networks in human adipose tissue and obesity. Nat Rev Endocrinol. 2015 May;11((5)):276–288. doi: 10.1038/nrendo.2015.25. [DOI] [PubMed] [Google Scholar]
- 3.Cauley JA. An overview of sarcopenic obesity. J Clin Densitom. 2015;18((4)):499–505. doi: 10.1016/j.jocd.2015.04.013. [DOI] [PubMed] [Google Scholar]
- 4.Lee J, Hong YP, Shin HJ, Lee W. Associations of sarcopenia and sarcopenic obesity with metabolic syndrome considering both muscle mass and muscle strength. J Prev Med Public Health. 2016;49((1)):35–44. doi: 10.3961/jpmph.15.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lima-Leopoldo AP, Leopoldo AS, Da Silva DC, Do Nascimento AF, De Campos DH, Luvizotto RA, et al. Long-term obesity promotes alterations in diastolic function induced by reduction of phospholamban phosphorylation at serine-16 without affecting calcium handling. J Appl Physiol (1985) 2014;117((6)):669–678. doi: 10.1152/japplphysiol.00088.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alexander JK. Obesity and the heart. Curr Probl Cardiol. 1980;5((3)):1–41. doi: 10.1016/0146-2806(80)90013-4. [DOI] [PubMed] [Google Scholar]
- 7.Mandviwala T, Khalid U, Deswal A. Obesity and cardiovascular disease: a risk factor or a riskmMarker? Curr Atheroscler Rep. 2016;18((5)):21. doi: 10.1007/s11883-016-0575-4. [DOI] [PubMed] [Google Scholar]
- 8.Oliveira-Junior SA, Martinez PF, Guizoni DM, Campos DH, Fernandes T, Oliveira EM, et al. AT1 receptor blockade attenuates insulin resistance and myocardial remodeling in rats with diet-induced obesity. PLoS One. 2014;9((1)):e86447. doi: 10.1371/journal.pone.0086447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pieri BL, Souza DR, Luciano TF, Marques SO, Pauli JR, Silva AS, et al. Effects of physical exercise on the P38MAPK/REDD1/14-3-3 pathways in the myocardium of diet-induced obesity rats. Horm Metab Res. 2014;46((9)):621–7. doi: 10.1055/s-0034-1371824. [DOI] [PubMed] [Google Scholar]
- 10.Touyz RM. Protecting the heart in obesity: role of ACE2 and its partners. Diabetes. 2016;65:19–21. doi: 10.2337/dbi15-0014. [DOI] [PubMed] [Google Scholar]
- 11.Ortega FJ, Mercader JM, Catalán V, Moreno-Navarrete JM, Pueyo N, Sabater M, et al. Targeting the circulating microRNA signature of obesity. Clin Chem. 2013 May;59((5)):781–792. doi: 10.1373/clinchem.2012.195776. [DOI] [PubMed] [Google Scholar]
- 12.Ferland-McCollough D, Ozanne SE, Siddle K, Willis AE, Bushell M. The involvement of microRNAs in type 2 diabetes. Biochem Soc Trans. 2010;38((6)):1565–1570. doi: 10.1042/BST0381565. [DOI] [PubMed] [Google Scholar]
- 13.Bartel DP. MicroRNAs: genomics, biogenesis, mechanism, and function. Cell. 2004;116((2)):281–297. doi: 10.1016/s0092-8674(04)00045-5. [DOI] [PubMed] [Google Scholar]
- 14.Ambros V. MicroRNAs: tiny regulators with great potential. Cell. 2001;107((7)):823–6. doi: 10.1016/s0092-8674(01)00616-x. [DOI] [PubMed] [Google Scholar]
- 15.Klöting N, Berthold S, Kovacs P, Schön MR, Fasshauer M, Ruschke K, et al. MicroRNA expression in human omental and subcutaneous adipose tissue. PLoS One. 2009;4((3)):e4699. doi: 10.1371/journal.pone.0004699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barretti DL, Magalhães Fde C, Fernandes T, do Carmo EC, Rosa KT, Irigoyen MC, et al. Effects of aerobic exercise training on cardiac renin-angiotensin system in an obese zucker rat strain. PLoS One. 2012;7((10)):e46114–10. doi: 10.1371/journal.pone.0046114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roque FR, Hernanz R, Salaices M, Briones AM. Exercise training and cardiometabolic diseases: focus on the vascular system. Curr Hypertens Rep. 2013 Jun;15((3)):204–214. doi: 10.1007/s11906-013-0336-5. [DOI] [PubMed] [Google Scholar]
- 18.Safdar A, Saleem A, Tarnopolsky MA. The potential of endurance exercise-derived exosomes to treat metabolic diseases. Nat Rev Endocrinol. 2016 May;12((9)):504–517. doi: 10.1038/nrendo.2016.76. [DOI] [PubMed] [Google Scholar]
- 19.Yang X, Bi P, Kuang S. Fighting obesity: when muscle meets fat. Adipocyte. 2014;3((4)):280–9. doi: 10.4161/21623945.2014.964075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Silveira AC, Fernandes T, Soci ÚPR, Gomes JLP, Barretti DL, Mota GGF, et al. Exercise training restores cardiac microRNA-1 and microRNA-29c to nonpathological levels in obese rats. Oxid Med Cell Longev. 2017;2017:1549014. doi: 10.1155/2017/1549014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gomes JL, Fernandes T, Soci UP, Silveira AC, Barretti DL, Negrão CE, et al. Obesity downregulates microRNA-126 inducing capillary rarefaction in skeletal muscle: effects of aerobic exercise training. Oxid Med Cell Longev. 2017;2017((2415246)):2415246. doi: 10.1155/2017/2415246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fernandes T, Casaes L, Soci Ú, Silveira A, Gomes J, Barretti D, et al. Exercise training restores the cardiac microrna-16 levels preventing microvascular rarefaction in obese zucker rats. Obes Facts. 2018;11((1)):15–24. doi: 10.1159/000454835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fernandes T, Barretti DL, Phillips MI, Menezes Oliveira E. Exercise training prevents obesity-associated disorders: role of miRNA-208a and MED13. Mol Cell Endocrinol. 2018;476:148–154. doi: 10.1016/j.mce.2018.05.004. [DOI] [PubMed] [Google Scholar]
- 24.Fernandes T, Baraúna VG, Negrão CE, Phillips MI, Oliveira EM. Aerobic exercise training promotes physiological cardiac remodeling involving a set of microRNAs. Am J Physiol Heart Circ Physiol. 2015 Aug 15;309((4)):H543–52. doi: 10.1152/ajpheart.00899.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Flowers E, Won GY, Fukuoka Y. Micrornas associated with exercise and diet: a systematic review. Physiol Genomics. 2015;47((1)):1–11. doi: 10.1152/physiolgenomics.00095.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wahl P, Wehmeier UF, Jansen FJ, Kilian Y, Bloch W, Werner N, et al. Acute effects of different exercise protocols on the circulating vascular microRNAs −16, −21, and −126 in trained subjects. Front Physiol. 2016;7:643. doi: 10.3389/fphys.2016.00643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Caria ACI, Nonaka CKV, Pereira CS, Soares MBP, Macambira SG, Souza BSF. Exercise training-induced changes in microRNAs: beneficial regulatory effects in hypertension, type 2 diabetes, and obesity. Int J Mol Sci. 2018;19((11)):3608. doi: 10.3390/ijms19113608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Booth FW, Roberts CK, Laye MJ. Lack of exercise is a major cause of chronic diseases. Compr Physiol. 2012;2((2)):1143–211. doi: 10.1002/cphy.c110025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Da Rocha PECP, Da Silva VS, Camacho LAB, Vasconcelos AGG. Efeitos de longo prazo do treinamento resistido nos indicadores de obesidade: uma revisão sistemática. Rev Bras Cineantropometria e Desempenho Hum. 2015;17((5)):621–634. [Google Scholar]
- 30.Skrypnik D, Bogdański P, Mądry E, Karolkiewicz J, Ratajczak M, Kryściak J, et al. Effects of endurance and endurance strength training on body composition and physical capacity in women with abdominal obesity. Obes Facts. 2015;8((3)):175–187. doi: 10.1159/000431002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Villareal DT, Aguirre L, Gurney AB, Waters DL, Sinacore DR, Colombo E, et al. Aerobic or resistance exercise, or both, in dieting obese older adults. N Engl J Med. 2017;376((20)):1943–1955. doi: 10.1056/NEJMoa1616338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Walberg JL, Greenwood MR, Stern JS. Lipoprotein lipase activity and lipolysis after swim training in obese zucker rats. Am J Physiol. 1983;245((5 Pt 1)):R706–12. doi: 10.1152/ajpregu.1983.245.5.R706. [DOI] [PubMed] [Google Scholar]
- 33.Borel AL, Nazare JA, Smith J, Alméras N, Tremblay A, Bergeron J, et al. Visceral and not subcutaneous abdominal adiposity reduction drives the benefits of a 1-year lifestyle modification program. Obesity. 2012;20((6)):1223–1233. doi: 10.1038/oby.2011.396. [DOI] [PubMed] [Google Scholar]
- 34.Slentz CA, Aiken LB, Houmard JA, Bales CW, Johnson JL, Tanner CJ, et al. Inactivity, exercise, and visceral fat. STRRIDE: a randomized, controlled study of exercise intensity and amount. J Appl Physiol (1985) 2005 Oct;99((4)):1613–1618. doi: 10.1152/japplphysiol.00124.2005. [DOI] [PubMed] [Google Scholar]
- 35.Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK, et al. American college of sports medicine position stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009;41((2)):459–471. doi: 10.1249/MSS.0b013e3181949333. [DOI] [PubMed] [Google Scholar]
- 36.Lee IM, Sesso HD, Ridker PM, Mouton CP, Stefanick ML, Manson JE. Physical activity and inflammation in a multiethnic cohort of women. Med Sci Sports Exerc. 2012 Jun;44((6)):1088–1096. doi: 10.1249/MSS.0b013e318242b11a. [DOI] [PubMed] [Google Scholar]
- 37.You T, Arsenis NC, Disanzo BL, Lamonte MJ. Effects of exercise training on chronic inflammation in obesity: current evidence and potential mechanisms. Sports Med. 2013;43((4)):243–256. doi: 10.1007/s40279-013-0023-3. [DOI] [PubMed] [Google Scholar]
- 38.Spencer M, Unal R, Zhu B, Rasouli N, McGehee RE, Peterson CA, et al. Adipose tissue extracellular matrix and vascular abnormalities in obesity and insulin resistance. J Clin Endocrinol Metab. 2011;96((12)):E1990–8. doi: 10.1210/jc.2011-1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hosogai N, Fukuhara A, Oshima K, Miyata Y, Tanaka S, Segawa K, et al. Adipose tissue hypoxia in obesity and its impact on adipocytokine dysregulation. Diabetes. 2007 Apr;56((4)):901–911. doi: 10.2337/db06-0911. [DOI] [PubMed] [Google Scholar]
- 40.Christiansen T, Paulsen SK, Bruun JM, Pedersen SB, Richelsen B. Exercise training versus diet-induced weight-loss on metabolic risk factors and inflammatory markers in obese subjects: a 12-week randomized intervention study. Am J Physiol Endocrinol Metab. 2010 Apr;298((4)):E824–31. doi: 10.1152/ajpendo.00574.2009. [DOI] [PubMed] [Google Scholar]
- 41.Fabre O, Ingerslev LR, Garde C, Donkin I, Simar D, Barrès R. Exercise training alters the genomic response to acute exercise in human adipose tissue. Epigenomics. 2018;10((8)):1033–1050. doi: 10.2217/epi-2018-0039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Landen S, Voisin S, Craig JM, McGee SL, Lamon S, Eynon N. Genetic and epigenetic sex-specific adaptations to endurance exercise. Epigenetics. 2019;14((6)):523–535. doi: 10.1080/15592294.2019.1603961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Iacomino G, Russo P, Stillitano I, Lauria F, Marena P, Ahrens W, et al. Circulating microRNAs are deregulated in overweight/obese children: preliminary results of the I. Family study. Genes Nutr. 2016;11:7. doi: 10.1186/s12263-016-0525-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Soci UP, Fernandes T, Hashimoto NY, Mota GF, Amadeu MA, Rosa KT, et al. MicroRNAs 29 are involved in the improvement of ventricular compliance promoted by aerobic exercise training in rats. Physiol Genomics. 2011;43((11)):665–673. doi: 10.1152/physiolgenomics.00145.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Baggish AL, Park J, Min PK, Isaacs S, Parker BA, Thompson PD, et al. Rapid upregulation and clearance of distinct circulating microRNAs after prolonged aerobic exercise. J Appl Physiol (1985) 2018;116((21)):522–531. doi: 10.1152/japplphysiol.01141.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Maury E, Brichard SM. Adipokine dysregulation, adipose tissue inflammation and metabolic syndrome. Mol Cell Endocrinol. 2010;314:1–16. doi: 10.1016/j.mce.2009.07.031. [DOI] [PubMed] [Google Scholar]
- 47.Ortega FJ, Moreno-Navarrete JM, Pardo G, Sabater M, Hummel M, Ferrer A, et al. MiRNA expression profile of human subcutaneous adipose and during adipocyte differentiation. PLoS One. 2010 Feb;5((2)):e9022. doi: 10.1371/journal.pone.0009022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Abente EJ, Subramanian M, Ramachandran V, Najafi-Shoushtari SH. MicroRNAs in obesity-associated disorders. Arch Biochem Biophys. 2016 Jan;589:108–119. doi: 10.1016/j.abb.2015.09.018. [DOI] [PubMed] [Google Scholar]
- 49.Mudhasani R, Imbalzano AN, Jones SN. An essential role for dicer in adipocyte differentiation. J Cell Biochem. 2010 Apr;110((4)):812–6. doi: 10.1002/jcb.22625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mudhasani R, Puri V, Hoover K, Czech MP, Imbalzano AN, Jones SN. Dicer is required for the formation of white but not brown adipose tissue. J Cell Physiol. 2011 May;226((5)):1399–406. doi: 10.1002/jcp.22475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mori MA, Thomou T, Boucher J, Lee KY, Lallukka S, Kim JK, et al. Altered miRNA processing disrupts brown/white adipocyte determination and associates with lipodystrophy. J Clin Invest. 2014 Aug;124((8)):3339–3351. doi: 10.1172/JCI73468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Romao JM, Jin W, Dodson MV, Hausman GJ, Moore SS, Guan LL. MicroRNA regulation in mammalian adipogenesis. Exp Biol Med. 2011;236:997–1004. doi: 10.1258/ebm.2011.011101. [DOI] [PubMed] [Google Scholar]
- 53.Ahn J, Lee H, Jung CH, Jeon TI, Ha TY. MicroRNA-146b promotes adipogenesis by suppressing the SIRT1-FOXO1 cascade. EMBO Mol Med. 2013 Oct;5((10)):1602–1612. doi: 10.1002/emmm.201302647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chen L, Dai YM, Ji CB, Yang L, Shi CM, Xu GF, et al. MiR-146b is a regulator of human visceral preadipocyte proliferation and differentiation and its expression is altered in human obesity. Mol Cell Endocrinol. 2014;393((1-2)):65–74. doi: 10.1016/j.mce.2014.05.022. [DOI] [PubMed] [Google Scholar]
- 55.Xu G, Shi C, Ji C, Song G, Chen L, Yang L, et al. Expression of microRNA-26b, an obesity-related microRNA, is regulated by free fatty acids, glucose, dexamethasone and growth hormone in human adipocytes. Mol Med Rep. 2014 May;10((1)):223–8. doi: 10.3892/mmr.2014.2204. [DOI] [PubMed] [Google Scholar]
- 56.Karbiener M, Pisani DF, Frontini A, Oberreiter LM, Lang E, Vegiopoulos A, et al. MicroRNA-26 family is required for human adipogenesis and drives characteristics of brown adipocytes. Stem Cells. 2014 Jun;32((6)):1578–1590. doi: 10.1002/stem.1603. [DOI] [PubMed] [Google Scholar]
- 57.Mori M, Nakagami H, Rodriguez-Araujo G, Nimura K, Kaneda Y. Essential role for miR-196a in brown adipogenesis of white fat progenitor cells. PLoS Biol. 2012 Apr;10((4)):e1001314. doi: 10.1371/journal.pbio.1001314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Martinelli R, Nardelli C, Pilone V, Buonomo T, Liguori R, Castanò I, et al. MiR-519d overexpression is associated with human obesity. Obesity. 2010 Nov;18((11)):2170–2176. doi: 10.1038/oby.2009.474. [DOI] [PubMed] [Google Scholar]
- 59.Shi C, Zhang M, Tong M, Yang L, Pang L, Chen L, et al. MiR-148a is associated with obesity and modulates adipocyte differentiation of mesenchymal stem cells through wnt signaling. Sci Rep. 2015 May;5:9930. doi: 10.1038/srep09930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lozano-Bartolomé J, Llauradó G, Portero-Otin M, Altuna-Coy A, Rojo-Martínez G, Vendrell J, et al. Altered expression of miR-181a-5p and miR-23a-3p is associated with obesity and TNFα-induced insulin resistance. J Clin Endocrinol Metab. 2018;103((4)):1447–1458. doi: 10.1210/jc.2017-01909. [DOI] [PubMed] [Google Scholar]
- 61.Xie H, Lim B, Lodish HF. MicroRNAs induced during adipogenesis that accelerate fat cell development are downregulated in obesity. Diabetes. 2009;58((5)):1050–1057. doi: 10.2337/db08-1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lavery CA, Kurowska-Stolarska M, Holmes WM, Donnelly I, Caslake M, Collier A, et al. miR-34a(-/-) mice are susceptible to diet-induced obesity. Obesity. 2016;24((8)):1741–1751. doi: 10.1002/oby.21561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Cho YK, Son Y, Kim SN, Song HD, Kim M, Park JH, et al. MicroRNA-10a-5p regulates macrophage polarization and promotes therapeutic adipose tissue remodeling. Mol Metab. 2019;29:86–98. doi: 10.1016/j.molmet.2019.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ferrante SC, Nadler EP, Pillai DK, Hubal MJ, Wang Z, Wang JM, et al. Adipocyte-derived exosomal miRNAs: a novel mechanism for obesity-related disease. Pediatr Res. 2015 Mar;77((3)):447–454. doi: 10.1038/pr.2014.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Najafi-Shoushtari SH, Kristo F, Li Y, Shioda T, Cohen DE, Gerszten RE, et al. MicroRNA-33 and the SREBP host genes cooperate to control cholesterol homeostasis. Science. 2010 Jun;328((5985)):1566–1569. doi: 10.1126/science.1189123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rayner KJ, Esau CC, Hussain FN, McDaniel AL, Marshall SM, van Gils JM, et al. Inhibition of miR-33a/b in non-human primates raises plasma HDL and lowers VLDL triglycerides. Nature. 2011 Oct;478((7369)):404–7. doi: 10.1038/nature10486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rayner KJ, Sheedy FJ, Esau CC, Hussain FN, Temel RE, Parathath S, et al. Antagonism of miR-33 in mice promotes reverse cholesterol transport and regression of atherosclerosis. J Clin Invest. 2011 Jul;121((7)):2921–2931. doi: 10.1172/JCI57275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tsiloulis T, Watt MJ. Exercise and the regulation of adipose tissue metabolism. Prog Mol Biol Transl Sci. 2015;135:175–201. doi: 10.1016/bs.pmbts.2015.06.016. [DOI] [PubMed] [Google Scholar]
- 69.Tsiloulis T, Pike J, Powell D, Rossello FJ, Canny BJ, Meex RC, et al. Impact of endurance exercise training on adipocyte microRNA expression in overweight men. FASEB J. 2017;31((1)):161–171. doi: 10.1096/fj.201600678R. [DOI] [PubMed] [Google Scholar]
- 70.Brandão BB, Madsen S, Rabiee A, Oliverio M, Ruiz GP, Ferrucci DL, et al. Dynamic changes in DICER levels in adipose tissue control metabolic adaptations to exercise. Proc Natl Acad Sci U S A. 2020;117((38)):23932–41. doi: 10.1073/pnas.2011243117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Navickas R, Gal D, Laucevičius A, Taparauskaitė A, Zdanytė M, Holvoet P. Identifying circulating microRNAs as biomarkers of cardiovascular disease: a systematic review. Cardiovasc Res. 2016 Sep;111((4)):322–337. doi: 10.1093/cvr/cvw174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Khalyfa A, Kheirandish-Gozal L, Bhattacharjee R, Khalyfa AA, Gozal D. Circulating microRNAs as potential biomarkers of endothelial dysfunction in obese children. Chest. 2016 Mar;149((3)):786–800. doi: 10.1378/chest.15-0799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Creemers EE, Tijsen AJ, Pinto YM. Circulating microRNAs: novel biomarkers and extracellular communicators in cardiovascular disease? Circ Res. 2012;110((3)):483–495. doi: 10.1161/CIRCRESAHA.111.247452. [DOI] [PubMed] [Google Scholar]
- 74.Khalyfa A, Gozal D. Exosomal miRNAs as potential biomarkers of cardiovascular risk in children. J Transl Med. 2014;12((1)):162. doi: 10.1186/1479-5876-12-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ogawa R, Tanaka C, Sato M, Nagasaki H, Sugimura K, Okumura K, et al. Adipocyte-derived microvesicles contain RNA that is transported into macrophages and might be secreted into blood circulation. Biochem Biophys Res Commun. 2010;398((4)):723–9. doi: 10.1016/j.bbrc.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 76.Icli B, Feinberg MW. MicroRNAs in dysfunctional adipose tissue: cardiovascular implications. Cardiovasc Res. 2017;113((9)):1024–1034. doi: 10.1093/cvr/cvx098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Heneghan HM, Miller N, Kerin MJ. Role of microRNAs in obesity and the metabolic syndrome. Obes Rev. 2010;11((5)):354–361. doi: 10.1111/j.1467-789X.2009.00659.x. [DOI] [PubMed] [Google Scholar]
- 78.Liu L, Li Q, Xiao X, Wu C, Gao R, Peng C, et al. miR-1934, downregulated in obesity, protects against low-grade inflammation in adipocytes. Mol Cell Endocrinol. 2016 Jun;428:109–117. doi: 10.1016/j.mce.2016.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ross SE, Hemati N, Longo KA, Bennett CN, Lucas PC, Erickson RL, et al. Inhibition of adipogenesis by Wnt signaling. Science. 2000;289((5481)):950–3. doi: 10.1126/science.289.5481.950. [DOI] [PubMed] [Google Scholar]
- 80.Wang YC, Li Y, Wang XY, Zhang D, Zhang H, Wu Q, et al. Circulating miR-130b mediates metabolic crosstalk between fat and muscle in overweight/obesity. Diabetologia. 2013;56((10)):2275–2285. doi: 10.1007/s00125-013-2996-8. [DOI] [PubMed] [Google Scholar]
- 81.Baggish AL, Park J, Min PK, Isaacs S, Parker BA, Thompson PD, et al. Rapid upregulation and clearance of distinct circulating microRNAs after prolonged aerobic exercise. J Appl Physiol (1985) 2014 Mar;116((5)):522–531. doi: 10.1152/japplphysiol.01141.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Polakovičová M, Musil P, Laczo E, Hamar D, Kyselovič J. Circulating MicroRNAs as potential biomarkers of exercise response. Int J Mol Sci. 2016;17:1553. doi: 10.3390/ijms17101553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ramos AE, Lo C, Estephan LE, Tai YY, Tang Y, Zhao J, et al. Specific circulating microRNAs display dose-dependent responses to variable intensity and duration of endurance exercise. Am J Physiol Heart Circ Physiol. 2018;315:H273–83. doi: 10.1152/ajpheart.00741.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Horak M, Zlamal F, Iliev R, Kucera J, Cacek J, Svobodova L, et al. Exercise-induced circulating microRNA changes in athletes in various training scenarios. PLoS One. 2018;13((1)):e0191060. doi: 10.1371/journal.pone.0191060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Whyte LJ, Ferguson C, Wilson J, Scott RA, Gill JM. Effects of single bout of very high-intensity exercise on metabolic health biomarkers in overweight/obese sedentary men. Metabolism. 2013;62((2)):212–9. doi: 10.1016/j.metabol.2012.07.019. [DOI] [PubMed] [Google Scholar]
- 86.Bao F, Slusher AL, Whitehurst M, Huang CJ. Circulating microRNAs are upregulated following acute aerobic exercise in obese individuals. Physiol Behav. 2018;197:15–21. doi: 10.1016/j.physbeh.2018.09.011. [DOI] [PubMed] [Google Scholar]
- 87.Russo A, Bartolini D, Mensà E, Torquato P, Albertini MC, Olivieri F, et al. Physical activity modulates the overexpression of the inflammatory miR-146a-5p in obese patients. IUBMB Life. 2018;70((10)):1012–1022. doi: 10.1002/iub.1926. [DOI] [PubMed] [Google Scholar]
- 88.de Mendonça M, Rocha KC, de Sousa É, Pereira BMV, Oyama LM, Rodrigues AC. Aerobic exercise training regulates serum extracellular vesicle miRNAs linked to obesity to promote their beneficial effects in mice. Am J Physiol Endocrinol Metab. 2020;319((3)):E579–91. doi: 10.1152/ajpendo.00172.2020. [DOI] [PubMed] [Google Scholar]
- 89.Kenchaiah S, Sesso HD, Gaziano JM. Body mass index and vigorous physical activity and the risk of heart failure among men. Circulation. 2009;119((11)):44–52. doi: 10.1161/CIRCULATIONAHA.108.807289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lavie CJ, Milani RV, Ventura HO. Obesity and cardiovascular disease. Risk factor, paradox, and impact of weight loss. J Am Coll Cardiol. 2009;53((21)):1925–1932. doi: 10.1016/j.jacc.2008.12.068. [DOI] [PubMed] [Google Scholar]
- 91.Zou T, Zhu M, Ma YC, Xiao F, Yu X, Xu L, et al. MicroRNA-410-5p exacerbates high-fat diet-induced cardiac remodeling in mice in an endocrine fashion. Sci Rep. 2018;8((1)):8780. doi: 10.1038/s41598-018-26646-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Grueter CE, Van Rooij E, Johnson BA, Deleon SM, Sutherland LB, Qi X, et al. A cardiac MicroRNA governs systemic energy homeostasis by regulation of MED13. Cell. 2012;149((3)):671–683. doi: 10.1016/j.cell.2012.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Van Rooij E, Sutherland LB, Qi X, Richardson JA, Hill J, Olson EN. Control of stress-dependent cardiac growth and gene expression by a microRNA. Science. 2007;316((5824)):575–9. doi: 10.1126/science.1139089. [DOI] [PubMed] [Google Scholar]
- 94.Callis TE, Pandya K, Seok HY, Tang RH, Tatsuguchi M, Huang ZP, et al. MicroRNA-208a is a regulator of cardiac hypertrophy and conduction in mice. J Clin Invest. 2009;119((9)):2772–2786. doi: 10.1172/JCI36154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.van Rooij E, Sutherland LB, Thatcher JE, DiMaio JM, Naseem RH, Marshall WS, et al. Dysregulation of microRNAs after myocardial infarction reveals a role of miR-29 in cardiac fibrosis. Proc Natl Acad Sci U S A. 2008;105((35)):13027–32. doi: 10.1073/pnas.0805038105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Marchand A, Atassi F, Mougenot N, Clergue M, Codoni V, Berthuin J, et al. miR-322 regulates insulin signaling pathway and protects against metabolic syndrome-induced cardiac dysfunction in mice. Biochim Biophys Acta. 2016;1862:611–621. doi: 10.1016/j.bbadis.2016.01.010. [DOI] [PubMed] [Google Scholar]
- 97.Kuwabara Y, Horie T, Baba O, Watanabe S, Nishiga M, Usami S, et al. MicroRNA-451 exacerbates lipotoxicity in cardiac myocytes and high-fat diet-induced cardiac hypertrophy in mice through suppression of the LKB1/AMPK pathway. Circ Res. 2015;116((2)):279–288. doi: 10.1161/CIRCRESAHA.116.304707. [DOI] [PubMed] [Google Scholar]
- 98.Chen L, Wang Y, Pan Y, Zhang L, Shen C, Qin G, et al. Cardiac progenitor-derived exosomes protect ischemic myocardium from acute ischemia/reperfusion injury. Biochem Biophys Res Commun. 2013;431((3)):566–571. doi: 10.1016/j.bbrc.2013.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lopaschuk GD, Ussher JR. Targeting MicroRNAs to limit myocardial lipid accumulation. Circ Res. 2015;116((2)):229–231. doi: 10.1161/CIRCRESAHA.114.305675. [DOI] [PubMed] [Google Scholar]
- 100.Daiber A, Steven S, Weber A, Shuvaev VV, Muzykantov VR, Laher I, et al. Targeting vascular (endothelial) dysfunction. Br J Pharmacol. 2017 May;174((12)):1591–619. doi: 10.1111/bph.13517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Nezu T, Hosomi N, Aoki S, Matsumoto M. Carotid Intima-media thickness for atherosclerosis. J Atheroscler Thromb. 2016;23((1)):18–31. doi: 10.5551/jat.31989. [DOI] [PubMed] [Google Scholar]
- 102.Naqvi TZ, Lee MS. Carotid intima-media thickness and plaque in cardiovascular risk assessment. JACC Cardiovasc Imaging. 2014 Oct;7((10)):1025–1038. doi: 10.1016/j.jcmg.2013.11.014. [DOI] [PubMed] [Google Scholar]
- 103.Bagi Z. Mechanisms of coronary microvascular adaptation to obesity. Am J Physiol Regul Integr Comp Physiol. 2009;297((3)):R556–67. doi: 10.1152/ajpregu.90817.2008. [DOI] [PubMed] [Google Scholar]
- 104.Hulsmans M, De Keyzer D, Holvoet P. MicroRNAs regulating oxidative stress and inflammation in relation to obesity and atherosclerosis. FASEB J. 2011 Aug;25((8)):2515–2527. doi: 10.1096/fj.11-181149. [DOI] [PubMed] [Google Scholar]
- 105.Araldi E, Suárez Y. MicroRNAs as regulators of endothelial cell functions in cardiometabolic diseases. Biochim Biophys Acta. 2016 Jan;1861((12 Pt B)):2094–103. doi: 10.1016/j.bbalip.2016.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Xiao L, Liu Y, Wang N. New paradigms in inflammatory signaling in vascular endothelial cells. Am J Physiol Heart Circ Physiol. 2014 Feb;306((3)):H317–25. doi: 10.1152/ajpheart.00182.2013. [DOI] [PubMed] [Google Scholar]
- 107.Magenta A, Greco S, Gaetano C, Martelli F. Oxidative stress and microRNAs in vascular diseases. Int J Mol Sci. 2013;14((9)):17319–46. doi: 10.3390/ijms140917319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Ling H, Li X, Yao CH, Hu B, Liao D, Feng S, et al. The physiological and pathophysiological roles of adipocyte miRNAs. Biochem Cell Biol. 2013 Aug;91((4)):195–202. doi: 10.1139/bcb-2012-0053. [DOI] [PubMed] [Google Scholar]
- 109.Dimassi S, Karkeni E, Laurant P, Tabka Z, Landrier JF, Riva C. Microparticle miRNAs as biomarkers of vascular function and inflammation response to aerobic exercise in obesity? Obesity. 2018;26((10)):1584–1593. doi: 10.1002/oby.22298. [DOI] [PubMed] [Google Scholar]