Summary
Introduction
We assessed change in substance use from before to during the COVID-19 pandemic in young adults and identified factors associated with initiation/increase in use.
Methods
The sample comprised young adults from a longitudinal investigation of 1294 youth recruited at ages 12-13 (1999-2000) in 10 Montréal-area high schools. Pre-pandemic data on use of cannabis, alcohol, combustible cigarette, e-cigarette and binge drinking were collected at ages 20.4, 24.0 and 30.6. During COVID-19, data were collected from December 2020 to June 2021 (age 33.6). We studied the prevalence of any and weekly/daily use from age 20.4 to 33.6. Individual-level change in substance use during the pandemic was estimated as differences in the frequency of use from age 30.6 to 33.6 versus from age 24.0 to 30.6. Heterogeneity in the risk of initiated/increased substance use during COVID-19 across sociodemographic subgroups was assessed using modified Poisson regression.
Results
The prevalence of cannabis use increased from 17.5% to 23.1% from before to during the pandemic; e-cigarette use increased from 3.8% to 5.4%. In individual change analyses, the proportion of participants whose substance use did not change ranged from 48.9% (alcohol) to 84.0% (e-cigarettes). The incidence of initiated/increased cannabis use (22.4%), and quit/decreased alcohol (35.2%) and binge drinking (53.5%) were higher during the pandemic than between ages 24.0 to 30.6. Low education and living alone were associated with higher risks of initiated/increased use of most substances.
Discussion
Most participants reported stable patterns in substance use from before to during the COVID-19 pandemic.
Funding
The NDIT study was supported by the Canadian Cancer Society (grant numbers 010271, 017435, 704031) and the Canadian Institutes of Health Research (grant number 451832).
Keywords: substance use, COVID-19 pandemic, young adults, longitudinal study
Research in context.
Evidence before this study
We searched EPPI-Centre (COVID-19: a living systematic map of the evidence), PubMed and Google Scholar for studies published in English or French as of July 22nd 2021 on change in substance use during the COVID-19 pandemic, using search terms including “cannabis”, “alcohol”, “binge drinking”, “cigarettes”, “substance use”, “change” and “COVID-19”. Much of the evidence to date on COVID-19-related change in substance use is drawn from cross-sectional studies in which participants are asked to recall substance use behaviour prior to the pandemic, likely leading to recall errors that can bias estimates of change in prevalence. We identified one large representative population-based longitudinal study with pre-pandemic data on multiple substances (the UK Household Longitudinal Study), which reported declines in smoking and increases in the frequency of alcohol use and binge drinking while COVID-19 containment measures were implemented. Other longitudinal studies are challenged by small sample sizes, a focus on specific high-risk groups rather than representative population-based samples, possible selection bias due to low response proportions during COVID-19, lack of generalizability due to the use of online and/or volunteer samples, and a focus on one specific substance rather than multiple psychoactive substances. No longitudinal study to date has focused specifically on young adults, a group reported to have the highest levels of anxiety/distress during the pandemic.15,16
Added value of this study
This is the first longitudinal population-based study that measured the use of cannabis, alcohol, binge drinking, combustible cigarettes, and e-cigarettes in young adults before and during the COVID-19 pandemic. In general, substance use appears to have been stable in this sample of young adults in Canada. Although our findings do not support commonly held concerns that substance use has increased dramatically during the pandemic, they do indicate that some subgroups may warrant targeted attention. Specifically, those with lower education and adults living alone were more likely to initiate/increase substance use during COVID-19, suggestive that they may have been particularly vulnerable during the pandemic.
Implications of all the available evidence
Our conclusion that there were few notable increases in substance use during the COVID-19 pandemic, will need replication in larger population-based samples with a wider age range and better representation of vulnerable subgroups. Longitudinal studies with more frequent observations during COVID-19 and longer follow-ups are needed to investigate whether changes in substance use during COVID-19 translate into changes in health service use, morbidity, or mortality. In addition, extending existing longitudinal studies could provide an evidence base for public health practitioners and policy makers to confirm or allay concerns that substance use has attained higher than expected levels. More vulnerable groups (e.g., those with lower education levels, those living alone) may need targeted interventions to cope with the effects of the pandemic on their substance use.
Alt-text: Unlabelled box
Introduction
There is considerable concern that the use of psychoactive substances including alcohol, cannabis and nicotine increased during the COVID-19 pandemic.1 Underpinning this apprehension is the notion that containment-related social isolation and financial instability increased levels of psychological distress, especially in more vulnerable subgroups such as people with lower incomes or education, those with mental health problems, and single-parent families.2 More specifically, limited opportunities for social gatherings, boredom, loneliness, and increased stress and anxiety could all have contributed to higher levels of psychological distress increasing the need for distraction and/or the perceived need to self-medicate, which in turn may have increased substance use.3, 4, 5, 6, 7
However, despite these concerns, few longitudinal studies document changes in substance use from pre to during the COVID-10 pandemic - a critical first step toward better understanding whether worrisome pandemic-related changes in substance use did occur. Much of the evidence to date on COVID-19-related change in substance use is drawn from cross-sectional studies in which participants are asked to recall substance use behaviour before the pandemic.2,8,9 Recall in these studies could be compromised, introducing error into estimates of change in prevalence from before to during COVID-19. Longitudinal studies with empirical data collected before the onset of the COVID-19 pandemic are critical to establishing whether these concerns are warranted and if so, in which population subgroups. In one of the few longitudinal studies to date with pre-pandemic data, the UK Household Longitudinal Study collected data on binge drinking, smoking and e-cigarette use from 9748 adults in four survey waves between 2015 and 2020.10 The 25-44 age group reported increases in binge drinking, declines in smoking and no change in e-cigarette use.10 Other extant longitudinal studies are challenged by small sample sizes,7 a focus on a narrow demographic or specific high-risk group rather than representative population-based samples,7,11 possible selection bias due to low response proportions during COVID-19,12 lack of generalizability due to the use of online and/or volunteer samples,11,12 and a focus on one specific substance rather than measures of multiple psychoactive substances.11,12
In this paper, we address gaps in the longitudinal literature documenting change in substance use, drawing on data collected before and during the COVID-19 pandemic from young adults participating in the 20-year Nicotine Dependence in Teens (NDIT) study.13 Young adults constitute a group of considerable interest in terms of COVID-19-related research because they are already undergoing numerous major life transitions as they establish their social, educational and work identities,14 and because they report the highest levels of anxiety/distress during the pandemic.15,16
Our specific objectives were to describe change in substance use (i.e., cannabis, alcohol, combustible cigarettes, e-cigarettes) and related behaviours (binge drinking) from before to during the COVID-19 pandemic in young adults, and to assess whether changes in substances use were heterogeneous across subgroups based on sociodemographic characteristics and a history of mental health diagnosis. Although binge drinking is a specific subtype of alcohol use, we include it under the general rubric of ‘substance use’ in this article to ease readability.
Methods
Setting and source of data
Data were drawn from the ongoing Nicotine Dependence in Teens (NDIT) study, the main objectives of which are to investigate the natural course and determinants of cigarette smoking and nicotine dependence in adolescents and young adults.13 In addition to its focus on smoking, NDIT also collected data on sociodemographic factors, genetics, anthropometric measures, lifestyle behaviours, psychosocial factors and mental health.13 NDIT recruited 1294 7th grade students age 12-13 in 1999-2000, in a purposive sample of 10 Montréal-area high schools in Québec, Canada (i.e., schools located in urban, suburban, and rural neighbourhoods, schools serving advantaged and disadvantaged students, and schools serving French- and English-speaking students). Between 1999 and 2005, participants completed self-report questionnaires every 3 months during the 10-month school year from 7th to 11th grade, for a total of 20 data collection cycles during high school. At baseline in 1999-2000, NDIT participant characteristics were comparable to those reported in the 1999 provincially representative Québec Child and Adolescent Health and Social Survey.13,17
The current study uses NDIT data collected in four post-high school data collection cycles. Pre-pandemic data were collected in cycle 21 (2007-08; mean (SD) age 20.4 (0.8)), cycle 22 (2010-12; age 24.0 (0.7)), and cycle 23 (2017-20; age 30.6 (1.0). In Québec, a state of sanitary emergency was declared on March 13, 2020, which led to the closure of all daycares, schools, post-secondary institutions, and non-essential businesses, as well as bans on indoor gatherings. Some restrictions were loosened briefly in summer 2020 before most were reinstated in fall 2020. Québec returned to unrestricted openings of institutions and businesses (with masks) in summer 2021.18,19 In NDIT cycle 23, 99.3% of participants completed data collection before the COVID-19 state of sanitary emergency was declared in Québec.
Data for cycle 24 were collected online from December 2020 to June 2021 during the COVID-19 pandemic when participants were age 33.6 (0.6) years on average. Because more than 80% of participants completed cycle 24 in December 2020, their reports on past-year substance use (see Measures section below) covered from 1 to < 4 months pre-pandemic (i.e., from December 2019 to March 2020). Figure S1 in the Supplementary Material provides a timeline of data collection for cycles 23-24.
NDIT was approved by ethics committees at the Montréal Department of Public Health , McGill University and Centre hospitalier de l'Université de Montréal (2007-2384, 2017-6895, ND06.087). Parents/guardians provided written consent at baseline and participants provided consent post-high school.
Study design
We studied cannabis use, alcohol consumption, binge drinking, combustible cigarette smoking, and e-cigarette use over time in two studies including a study of trends in prevalence from cycle 21 to 24, and a study of change in individual-level substance use between cycles 23 and 24 compared to change between cycle 22 and 23. Change from cycle 22 to 23 provides an estimate of the expected change between cycle 23 to 24 under the scenario that the pandemic had not occurred. Differences in changes between cycle 22 and 23 and between cycle 23 to 24 may be partially attributable to the effects of the COVID-19 pandemic under the assumption that pre-pandemic trends in substance use would have remained stable if the pandemic had not occurred. Longitudinal studies suggest that substance use increases from adolescence to early adulthood and then declines from the mid-twenties to mid-thirties.14,20,21 Comparison of changes between cycle 22 to 23 and cycle 23 to 24 is thus valid under the assumption of a stable decline from age 24 to 34.
Measures
Participants reported past-year frequency (i.e., never, less than once a month, 1-3 times/month, 1-6 times/week, every day) of using: (i) cannabis (cycles 21-22) and cannabis with or without tobacco (cycles 23-24) defined as the highest reported frequency with or without tobacco (i.e., a conservative estimate of the frequency of cannabis use); (ii) alcohol (cycles 21-24); (iii) binge drinking (i.e., consuming ≥5 alcoholic beverages on one occasion) (cycles 21-24); (iv) combustible cigarettes (cycles 21-24); and (v) e-cigarettes with or without nicotine (cycles 23-24) defined as the highest reported frequency with or without nicotine. A sensitivity analysis restricting e-cigarette use to use with nicotine only did not change the interpretation of the results (data not shown) and therefore data for e-cigarettes with or without nicotine is reported herein. Past year any use (yes, no) was defined as using the substance at least once in the past year. Past year weekly/daily use (yes, no) was defined as reporting use 1-6 times/week or every day.
Sociodemographic characteristics included age, sex, Caucasian ancestry (yes, no), born in Canada (yes, no), lives in Canada (yes, no), lives in urban/suburban setting (yes, no), lives alone (yes, no), lives with children (no, yes as a single parent, yes with another parent), number of children at home (none, ≥1 child age ≤5 years, children all age >5 years), highest education (high school, more than high school), unemployed (yes, no), and household income (<50 000$, ≥50 000 CAN$). In cycle 24, participants also reported work-at-home status during COVID-19 (unemployed/works at home; works outside home/mixed).
Mental health diagnosis (yes, no) was defined as self-reports of having been diagnosed by a health professional with one of the two most prevalent mental disorders in Canada,22 including a mood (i.e., depression, bipolar disorder) and/or an anxiety disorder (i.e., phobia, fear of social situations, obsessive-compulsive disorder, panic disorder, generalized anxiety disorder).
All measures were updated in cycles 21-24. Supplementary Table S1 details all study variables.
Statistical analysis
For the trends in prevalence study, past-year prevalence of any use and weekly/daily use of each substance was estimated in cycles 21 to 24.
For the change in individual-level substance use study, each participant was classified into one of six categories for each substance. Those not using a substance in cycle 23 were classified as stable nonusers if they were not using in cycle 24 or initiated if they reported any use in cycle 24. Participants reporting any use in cycle 23 were classified as quit if they did not report any use in cycle 24, increased if they reported a higher frequency of use in cycle 24, decreased if they reported a lower frequency of use in cycle 24, or stable users if they reported the same frequency in cycles 23 and 24. To avoid small sample sizes, reduce the complexity of the analysis and focus on categories of most utility to public health, the six categories were collapsed into four by combining initiated with increased (i.e., labelled initiated/increased), and quit with decreased (i.e., quit/decreased). Unweighted incidences of each of initiation, increased use, cessation, and decreased use from cycles 22 to 23 and from cycles 23 to 24 are reported in Table S2 in the Supplementary Material.
We then computed six estimates describing stability/change in the frequency of substance use from cycles 23 to 24. Four estimates reflected stability including: (i) the proportion of participants overall who did not change frequency of use from cycles 23 to 24; (ii) stable nonusers (i.e., the proportion of nonusers in cycle 23 who remained nonusers in cycle 24); (iii) stable users (i.e., the proportion of participants who reported any use in cycle 23 who reported the same frequency of any use in cycle 24); and as an important subset of stable users, we also report the proportion of stable weekly/daily users. Two estimates reflected change including the cumulative incidence (hereafter referred to as incidence) of: (v) initiated/increased use estimated as the number of participants who initiated/increased use divided by the number of nonusers and less than daily users in cycle 23 (i.e., because daily use represents a “ceiling” that could not increase); and (vi) the incidence of quit/decreased was estimated as the number of participants who quit/decreased divided by the number of users in cycle 23. We also estimated these two measures from cycles 22 to 23 to enable comparing change from cycles 23 to 24 to change during a period without COVID-19.
Relative risks (RR) for sociodemographic characteristics, a mental health diagnosis, and level of adherence to public health COVID-19 measures were estimated for the contrast between initiated/increased versus quit/decreased, stable non-daily users and stable nonusers. RR were estimated using generalized linear models with a Poisson family and log link and their standard errors were computed using sandwich estimators,23 adjusting for variables generally associated with substance use (i.e., age, sex, and education (a well-accepted measure of socioeconomic status)). P-values for the comparisons between groups based on sociodemographic characteristics and a history of mental health diagnosis were modelled-based, whereas p-values for comparisons of prevalence or incidence of substance use over time were obtained using permutation tests with 10,000 iterations.
Nonresponse weights were computed to account for attrition using inverse probability weighing (see Supplementary Material Table S3 for a description of their derivation). Listwise deletion was used for missing values (≤ 3.3%) that were not due to survey non-response. Unless otherwise stated, prevalence estimates, confidence intervals (CI) and RR were weighted for nonresponse (i.e., sample-specific weights were used for the prevalence study; weights from cycles 23 and 24 were used for the individual-level difference study). See Tables S4 to S6 in the Supplementary Material for unweighted results.
Analyses were performed using R version 4.0.4 (R Foundation for Statistical Computing, Vienna, Austria).
Role of the funding source
The funders were not involved in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript.
Results
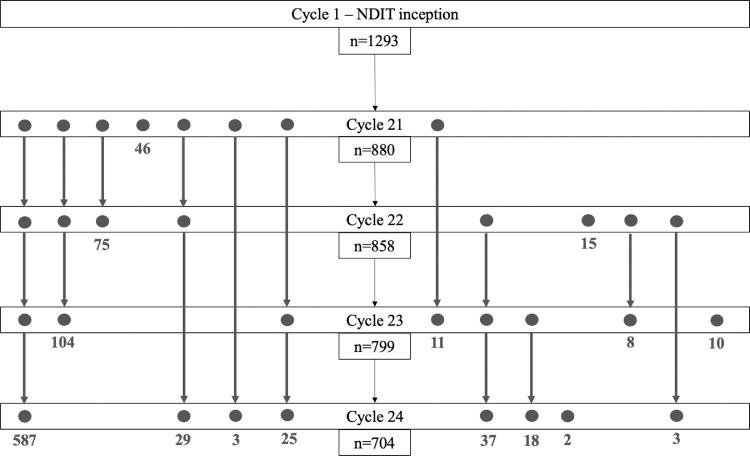
Of 1294 participants at NDIT baseline, 972 (75.1%) provided data in at least one of cycles 21-24. Sample sizes were 880, 858, 799 and 704 in cycles 21-24, respectively (Figure 1). Data on individual changes in substance use required for the calculations of incidence were computed using the subsamples of 739 and 667 participants who provided data in cycles 22-23 and cycles 23-24 respectively. RR were computed from the subsample of 667 participants. Compared to participants lost-to-follow-up, those retained in cycle 24 included a higher proportion of females, were less likely to have tried alcohol or combustible cigarettes at baseline and were more likely to have a university-educated mother (Supplementary Material Table S7).
Figure 1.
Flow chart of response from NDIT baseline (cycle 1) to cycle 24, Nicotine Dependence in Teens study, Montréal, Canada, 1999-2021.
During COVID-19, the weighted prevalence of weekly/daily alcohol and cannabis use was 44% and 23%, respectively (Table 1). Weekly/daily binge drinking and use of combustible and e-cigarettes were less prevalent (i.e., 8%, 12% and 5%, respectively). The prevalence of weekly/daily alcohol use was highest among males, those employed or living alone and those with an income ≥50,000CAN$. The prevalence of weekly/daily use of the other substances was higher among participants with low education (except for binge drinking), those with lower incomes, those with mental health diagnoses, those who lived alone and among single parents of younger children. Table S8 shows the absolute differences in prevalence across categories of the characteristics investigated and p-values for the tests of difference.
Table 1.
Prevalence of past-year weekly/daily substance use during the COVID-19 pandemic according to selected characteristics of participants, Nicotine Dependence in Teens study, Montreal, Canada 2020-2021
| Unweighted sample |
Weighted sample |
|||||||
|---|---|---|---|---|---|---|---|---|
| Weekly/daily use in the past year % (95% CI)* | ||||||||
| n† | % | %* | Cannabis | Alcohol | Binge drinking | Combustible cigarettes | E-cigarettes | |
| Total | 704 | 100 | - | 23.1 (21.1; 25.1) | 44.2 (41.9; 46.5) | 7.9 (6.7; 9.3) | 11.9 (10.5; 13.5) | 5.4 (4.4, 6.5) |
| Sex | ||||||||
| Male | 294 | 41.8 | 39.8 | 27.7 (24.5; 31.1) | 51.9 (48.2; 55.6) | 13.5 (11.2; 16.3) | 12.5 (10.3; 15.2) | 6.3 (4.7; 8.4) |
| Female | 410 | 58.2 | 60.2 | 20.0 (17.7; 22.5) | 39.1 (36.2; 42.1) | 4.2 (3.2; 5.6) | 11.6 (9.8; 13.6) | 4.8 (3.7; 6.3) |
| Ethnicity | ||||||||
| European ancestry | 518 | 77.7 | 75.4 | 25.4 (23.1; 27.9) | 47.3 (44.5; 50.1) | 9.9 (8.4; 11.7) | 11.6 (9.9; 13.5) | 2.4 (1.3; 4.4) |
| Other ancestry | 149 | 22.3 | 24.6 | 17.4 (14.0; 21.3) | 34.3 (29.9; 39.1) | 3.8 (2.3; 6.1) | 11.1 (8.4; 14.5) | 5.1 (4.0; 6.4) |
| Born in Canada | ||||||||
| No | 39 | 5.5 | 6 | 6.6 (3.1; 13.2) | 25.8 (18.3; 35.0) | 4.7 (1.9; 10.8) | 2.9 (0.9; 8.5) | 0.0 (0.0; 1.0) |
| Yes | 665 | 95.5 | 94 | 24.1 (22.1; 26.2) | 45.4 (43.0; 47.8) | 8.1 (6.9; 9.6) | 12.5 (11.0; 14.2) | 5.8 (4.7; 7.0) |
| Lives in Canada | ||||||||
| No | 29 | 4.1 | 3.4 | 3.1 (0.7; 12.3) | 33.4 (22.6; 46.2) | 10.9 (5.1; 21.7) | 0.0 (0.0, 1.0) | 3.1 (0.7; 12.3) |
| Yes | 674 | 95.9 | 96.6 | 23.8 (21.8; 25.9) | 44.5 (42.2; 46.9) | 7.8 (6.6; 9.2) | 12.4 (10.9; 14.0) | 5.5 (4.5; 6.7) |
| Lives in urban/suburban setting | ||||||||
| No | 120 | 17.1 | 17.7 | 17.3 (13.4; 21.9) | 43.8 (38.3; 49.4) | 11.0 (7.9; 15.0) | 10.4 (7.4; 14.3) | 6.2 (4.0; 9.6) |
| Yes | 581 | 82.9 | 82.3 | 24.0 (21.9; 26.3) | 44.0 (41.4; 46.5) | 7.3 (6.1; 8.8) | 12.4 (10.8; 14.2) | 5.4 (4.2; 6.6) |
| Lives alone | ||||||||
| No | 595 | 84.5 | 83.1 | 21.1 (19.1; 23.3) | 42.6 (40.1; 45.2) | 7.6 (6.4; 9.1) | 9.7 (8.3; 11.4) | 4.2 (3.3; 5.4) |
| Yes | 109 | 15.5 | 16.9 | 32.7 (27.6; 38.3) | 52.1 (46.4; 57.7) | 9.3 (6.5; 13.2) | 22.8 (18.4; 28.0) | 11.2 (8.0; 15.3) |
| Lives with children | ||||||||
| No | 396 | 56.2 | 56.1 | 26.7 (24.1; 29.6) | 49.2 (46.1; 52.4) | 9.7 (8.0; 11.8) | 12.2 (10.3; 14.4) | 5.7 (4.4; 7.3) |
| Yes, as single parent | 25 | 3.6 | 3.2 | 44.6 (32.2; 57.6) | 40.3 (28.4; 53.5) | 12.9 (6.3; 24.4) | 47.0 (34.5; 60.0) | 4.8 (1.5; 14.6) |
| Yes, with another parent | 283 | 40.2 | 40.6 | 16.3 (13.7; 19.2) | 37.6 (34.1; 41.2) | 5.0 (3.6; 6.9) | 8.8 (6.9; 11.1) | 5.1 (3.7; 7.0) |
| Number of children at home | ||||||||
| None | 383 | 56.5 | 56.4 | 26.9 (24.2; 29.8) | 49.3 (46.2; 52.4) | 9.7 (8.0; 11.7) | 12.2 (10.3; 14.4) | 5.6 (4.4; 7.3) |
| ≥ 1 child age ≤ 5 years | 266 | 38.6 | 39.1 | 14.9 (12.4; 17.8) | 37.3 (33.8; 41.0) | 5.2 (3.7; 7.1) | 7.9 (6.1; 10.2) | 4.8 (3.5; 6.7) |
| Children all age > 5 years | 33 | 4.8 | 4.5 | 45.6 (35.0; 56.7) | 39.8 (29.7; 51.0) | 9.7 (4.8; 18.4) | 44.1 (33.6; 55.2) | 7.5 (3.4; 15.8) |
| Highest education | ||||||||
| More than high school | 660 | 96.9 | 96.5 | 22.0 (20.1; 24.1) | 44.0 (41.6; 46.4) | 7.9 (6.7; 9.3) | 11.3 (9.9; 13.0) | 5.4 (4.4; 6.6) |
| High school | 21 | 3.1 | 3.4 | 61.4 (48.5; 72.9) | 42.2 (30.3; 55.1) | 15.2 (8.1; 26.8) | 39.2 (27.6; 52.1) | 6.4 (2.4; 16.3) |
| Unemployed | ||||||||
| No | 567 | 83.1 | 83.1 | 23.0 (20.9; 25.2) | 47.6 (45.1; 50.2) | 8.1 (6.8; 9.7) | 11.3 (9.8; 13.1) | 4.7 (3.7; 5.9) |
| Yes | 115 | 6.9 | 6.9 | 23.3 (18.8; 28.5) | 26.9 (22.2; 32.3) | 6.9 (4.5; 10.4) | 14.9 (11.3; 19.5) | 9.1 (6.3; 13.0) |
| Household income | ||||||||
| < CAN$50,000 | 149 | 21.2 | 22.8 | 35.3 (30.8; 40.1) | 32.8 (28.4; 37.6) | 7.5 (5.3; 10.6) | 28.3 (24.1; 32.9) | 8.1 (5.8; 11.2) |
| ≥ CAN$50,000 | 554 | 78.8 | 77.2 | 19.5 (17.4; 21.7) | 47.6 (45.0; 50.3) | 8.0 (6.7; 9.6) | 7.1 (5.9; 8.6) | 4.6 (3.6; 5.9) |
| Work-at-home status during COVID-19 | ||||||||
| Unemployed/works at home | 332 | 47.4 | 47.7 | 23.1 (20.4; 26.1) | 39.2 (35.9; 42.6) | 7.4 (5.8; 9.4) | 9.9 (8.0; 11.1) | 6.6 (5.1; 8.5) |
| Works outside home/mixed | 363 | 52.6 | 52.3 | 22.3 (19.7; 25.1) | 49.1 (45.9; 52.4) | 8.2 (6.5; 10.1) | 12.7 (10.7; 15.1) | 4.5 (3.3; 6.1) |
| Mental health diagnosis | ||||||||
| No | 533 | 75.7 | 76.0 | 20.7 (18.6; 22.9) | 46.2 (43.6; 48.8) | 7.2 (5.9; 8.6) | 10.0 (8.5; 11.6) | 5.3 (4.2; 6.6) |
| Yes | 171 | 24.3 | 24.0 | 32.5 (28.3; 37.0) | 40.1 (35.7; 44.7) | 9.6 (7.2; 12.8) | 16.5 (13.4; 20.3) | 5.9 (4.0; 8.5) |
Prevalence and 95% CI are weighted for non-response.
Cell specific frequencies do not add up to the total sample size due to missing values.
Trends in prevalence
The weighted prevalence of any use of all five substances was relatively stable in cycles 21 and 22, and then declined in cycles 23 and 24 (Table 2). Similar patterns were observed for weekly/daily binge drinking and use of combustible cigarettes. The prevalence of alcohol use increased from cycles 21 to 23 before decreasing moderately in cycle 24. Table S9 provides the absolute difference in prevalence between consecutive cycles with p-values for the tests of difference. Weekly/daily cannabis and e-cigarette use were the only indicators that increased during COVID-19. The prevalence of cannabis use declined from 19.3% to 17.5% in cycles 21 to 23 and then increased to 23.1% in cycle 24. The prevalence of e-cigarette use rose slightly from 3.8% in cycle 23 to 5.4% in cycle 24.
Table 2.
Prevalence of any use and weekly/daily substance use in the past-year according to data collection cycle, Nicotine Dependence in Teens study, Montréal, Canada, 2007-21
|
Any use in past-year % (95% CI)* |
Weekly/daily use in past-year % (95% CI)* |
|||||||
|---|---|---|---|---|---|---|---|---|
| Cycle 21 | Cycle 22 | Cycle 23 | Cycle 24 | Cycle 21 | Cycle 22 | Cycle 23 | Cycle 24 | |
| (n=880) | (n=858) | (n=799) | (n=704) | (n=880) | (n=858) | (n=799) | (n=704) | |
| Cannabis | 44.3 | 43.8 | 40.3 | 40.9 | 19.4 | 18.3 | 17.5 | 23.1 |
| (41.8; 46.8) | (41.4; 46.3) | (37.9; 42.7) | (38.6; 43.2) | (17.5; 21.5) | (16.5; 20.3) | (15.7; 19.4) | (21.1; 25.1) | |
| Alcohol | 90.6 | 90.7 | 86.7 | 82.0 | 36.7 | 42.8 | 49.1 | 44.2 |
| (89.1; 92.0) | (89.2; 92.1) | (85.0; 88.3) | (80.2; 83.8) | (34.2; 39.1) | (40.4; 45.3) | (46.7; 51.6) | (41.9; 46.5) | |
| Binge drinking | 76.0 | 75.1 | 64.6 | 46.1 | 14.5 | 14.1 | 9.1 | 7.9 |
| (73.8; 78.1) | (72.9; 77.2) | (62.3; 67.0) | (43.8; 48.4) | (12.8; 16.3) | (12.4; 15.8) | (7.8; 10.6) | (6.7; 9.3) | |
| Combustible cigarettes | 47.1 | 45.0 | 35.6 | 26.1 | 27.3 | 25.4 | 18.0 | 11.9 |
| (44.6; 49.7) | (42.5; 47.4) | (33.3; 38.0) | (24.1; 28.2) | (25.1; 29.6) | (23.3; 27.6) | (16.2; 19.9) | (10.5; 13.5) | |
| E-cigarettes | NA | NA | 13.4 | 9.6 | NA | NA | 3.8 | 5.4 |
| (11.8; 15.2) | (8.2; 11.0) | (2.9; 4.8) | (4.4; 6.5) | |||||
Prevalence and 95% CI are weighted for non-response.
Note: Mean age of participants was 20.4, 24.0, 30.6 and 33.6 years in cycle 21, 22, 23 and 24, respectively.
NA: Not Applicable.
Change in individual-level use
The proportion of participants with no change in the frequency of substance use from before to during COVID-19 ranged from 48.9% (alcohol) to 84.0% (e-cigarettes) (see Table 3 for prevalence and incidence with 95% CI, and Table S10 for absolute differences and p-values for the tests of difference in prevalence and incidence). Except for alcohol use (i.e., only 50.6% of alcohol nonusers in cycle 23 reported abstaining during the pandemic), more than 80% of nonusers in cycle 23 remained nonusers in cycle 24. Thirty-five to 48.2% of substance users in cycle 23 reported the same frequency of use in cycle 24, except for e-cigarette use (8.7%).
Table 3.
Proportion of participants who did and did not change past-year substance use from cycles 22 to 23 compared to cycles 23 to 24, Nicotine Dependence in Teens study, Montreal, Canada, 2017-21
| Cannabis % (95% CI) |
Alcohol % (95% CI) |
Binge drinking % (95% CI) |
Combustible cigarettes % (95% CI) |
E- cigarettes† % (95% CI) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Cycle 22-23 | Cycle 23-24 | Cycle 22-23 | Cycle 23-24 | Cycle 22-23 | Cycle 23-24 | Cycle 22-23 | Cycle 23-24 | Cycle 23-24 | |
| Proportion of participants who did not change substance use* | |||||||||
| Overall (proportion of total sample) | 60.0 (57.5; 62.5) |
67.1 (64.9; 69.4) |
50.0 (47.4; 52.6) |
48.9 (46.5; 51.3) |
47.1 (44.6; 49.7) |
51.3 (48.8; 53.7) |
67.2 (64.8; 69.5) |
76.5 (74.4; 78.5) |
84.0 (82.2; 85.7) |
| Stable nonusers¥ (proportion of non- users) | 81.7 (78.9; 84.2) |
82.8 (80.4; 85.1) |
60.9 (51.6; 69.7) |
50.6 (43.7; 57.4) |
70.6 (65.7; 75.1) |
84.0 (80.8; 86.9) |
90.7 (88.6; 92.6) |
94.5 (93.07; 95.8) |
93.9 (92.6; 95.1) |
| Stable users‡ (proportion of users) | 33.5 (29.9; 37.2) |
39.2 (35.5; 43.0) |
51.3 (48.6; 53.9) |
48.2 (45.6; 50.8 |
39.4 (36.6; 42.4) |
35.9 (33.1; 38.8) |
36.9 (33.3; 40.7) |
38.7 (34.6; 42.9) |
8.7 (18.8; 18.5) |
| Stable weekly/daily users§ (proportion of users) | 18.6 (15.7; 21.7) |
25.1 (21.9; 28.6) |
31.6 (29.2; 34.2 |
34.4 (32.0; 36.9) |
6.2 (4.9;7.7) |
6.2 (4.9; 7.8) |
27.6 (24.3; 31.1) |
28.4 (24.7; 32.3) |
9.6 (5.9; 14.4) |
| Proportion of participants who changed substance use* | |||||||||
| Overall (proportion of total sample) | 40.0 (37.5; 42.5) |
32.9 (30.6; 35.1) |
50.0 (47.4; 52.5) |
51.1 (48.7; 53.5) |
52.9 (50.3; 55.4) |
48.7 (46.3; 51.2) |
32.8 (30.5; 35.2) |
23.5 (21.5; 35.6) |
16.0 (14.3; 17.8) |
| Initiated/increased£ (incidence among non- users and less than daily users) | 18.5 (16.4; 20.6) |
22.4 (20.4; 24.6) | 26.3 (24.1; 28.6) |
21.5 (19.5; 23.6) |
15.9 (14.1; 17.8) |
12.5 (10.9; 14.2) |
10.1 (8.4; 11.8) |
7.3 (6.0; 8.8) |
7.1 (5.9; 8.4) |
| Quit/decreased use¤ (incidence among users) | 49.6 (45.7; 53.5) |
35.4 (31.8; 39.1) |
23.0 (20.9; 25.3) |
35.2 (32.8; 37.7) |
47.5 (44.6; 50.4) |
53.5 (50.5; 56.5) |
54.7 (50.9; 58.5) |
53.2 (49.0; 57.4) |
72.5 (65.7; 78.6) |
Prevalence, incidence and 95% CI are weighted for non-response.
Note: Mean age of participants was 24.0, 30.6 and 33.6 years in cycle 22, 23 and 24, respectively.
Data on e-cigarette use are not available at cycle 22.
Proportion of nonusers in cycle t who remained non-user in cycle t+1.
Proportion of users in cycle t who reported the same frequency of use in cycle t+1.
Proportion of users in cycle t who reported daily/weekly use in cycles t and t+1.
Cumulative incidence of increased use in cycle t+1. The denominator corresponds to non-daily users in cycle t.
Cumulative incidence of decreased use in cycle t+1. The denominator corresponds to users in cycle t.
The incidence of initiated/increased use from cycles 23 to 24 ranged from 7.1% for e-cigarettes to 22.4% for cannabis. The highest incidences of weekly/daily use between cycles 23 and 24 were 6.6% for cannabis and 3.0% for e-cigarettes. Seventy-eight percent of initiators/increasers increased use of one substance; 20.2% increased use of two substances. The incidence of quit/decreased in cycle 24 varied from 35.4% and 35.2% for cannabis and alcohol to more than 50% for the other substances.
Cycle 23 to 24 change compared to cycle 22 to 23 change
The proportion of alcohol abstainers in cycle 22 who remained abstinent in cycle 23 was 60.9%; this compares to 50.6% between cycles 23 and 24. Also notable, the proportion of weekly/daily cannabis users who remained stable users between cycle 23 and 24 was 25.1%, compared to 18.9% between cycles 22 and 23.
In regard to the incidence indicators, initiated/increased cannabis use was higher between cycles 23 and 24 (22.4%) than between cycle 22 and 23 (18.5%) and the quit/decreased indicator was much lower (35.% vs. 49.6%). Quit/decreased alcohol use was significantly higher during the pandemic than between cycle 22 and 23. Interestingly initiated/increased alcohol use was lower during the pandemic (21.5% vs. 26.3%).
Factors associated with initiated/increased use
Table 4 shows RR and 95% CI for factors associated with initiated/increased substance use from cycle 23 to 24 (see Table S11 for p-values for testing differences in RR from the null). Among the more notable findings, high school education (relative to more than high school education) was generally associated with a higher risk of initiated/increased use of all substances with two exceptions - RRs were imprecise for binge drinking and e-cigarettes due to a low number of events. Living alone was associated with higher risks of initiated/increased cannabis, combustible cigarette, and e-cigarette use. Compared to not living with children, living with children age < 5 years was positively associated with initiated/increased alcohol use, but protective of initiated/increased use of cannabis, combustible cigarettes, and e-cigarettes. Mental health diagnosis was associated with a lower risk of initiated/increased alcohol use and a higher risk of initiated/increased cannabis use.
Table 4.
Relative risk (RR) of initiated/increased substance use from cycle 23 to 24, Nicotine Dependence in Teens study, Montréal, Canada, 2017-2021
| Cannabis | Alcohol | Binge drinking | Combustible cigarettes | E-cigarettes | |
|---|---|---|---|---|---|
| RR*† (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | |
| Sex | |||||
| Female | ref | ref | ref | ref | ref |
| Male | 1.3 (0.8; 2.2) | 0.8 (0.6; 1.3) | 1.1 (0.7; 1.9) | 1.0 (0.5; 2.1) | 1.3 (0.8; 2.1) |
| Ethnicity | |||||
| Other ancestry | ref | ref | ref | ref | ref |
| European ancestry | 1.4 (0.8; 2.3) | 0.8 (0.5; 1.3) | 1.5 (0.8; 2.9) | 0.6 (0.3; 1.4) | 1.0 (0.6; 1.9) |
| Lives in urban/suburban setting | |||||
| No | ref | ref | ref | ref | ref |
| Yes | 1.0 (0.6; 1.7) | 0.6 (0.4; 1.0) | 0.7 (0.4; 1.3) | 1.9 (0.7; 5.4) | 1.6 (0.7; 3.7) |
| Lives alone | |||||
| No | ref | ref | ref | ref | ref |
| Yes | 2.4 (1.6; 3.5) | 0.6 (0.3; 1.1) | 1.0 (0.5; 2.1) | 5.7 (2.9; 11.3) | 2.1 (1.2; 3.7) |
| Lives with children | |||||
| No | ref | ref | ref | ref | ref |
| Yes, single parent | 1.5 (0.7; 3.4) | 0.9 (0.3; 2.2) | 1.2 (0.3; 3.9) | 1.8 (0.5; 7.3) | 1.6 (0.7; 3.5) |
| Yes, with another parent | 0.7 (0.5; 1.0) | 1.6 (1.1; 2.3) | 1.1 (0.7; 1.9) | 0.5 (0.2; 1.5) | 0.6 (0.3; 1.0) |
| Number of children at home | |||||
| None | ref | ref | ref | ref | ref |
| ≥ 1 child age ≤ 5 | 0.6 (0.4; 0.9) | 1.6 (1.1; 2.3) | 1.0 (0.6; 1.7) | 0.4 (0.2; 1.0) | 0.5 (0.3; 0.9) |
| All children age > 5 | 1.7 (0.8; 3.4) | 1.0 (0.5; 2.0) | 2.0 (0.9; 4.3) | 2.3 (0.9; 6.2) | 2.1 (1.0; 4.2) |
| Highest level of education attained | |||||
| More than high school | ref | ref | ref | ref | ref |
| High school | 2.1 (1.0; 4.6) | 2.6 (1.4; 5.1) | 1.1 (0.4; 3.3) | 3.5 (1.1; 11.2) | 2.2 (0.8; 6.0) |
| Unemployed | |||||
| No | ref | ref | ref | ref | ref |
| Yes | 1.3 (0.8; 2.0) | 1.4 (0.9; 2.2) | 1.4 (0.7; 2.7) | 1.4 (0.6; 3.5) | 1.3 (0.7; 2.6) |
| Work-at-home status during COVID-19 | |||||
| Works outside home | ref | ref | ref | ref | ref |
| Unemployed/works at home | 1.0 (0.7; 1.5) | 1.4 (0.9; 2.0) | 0.6 (0.3; 1.0) | 1.0 (0.5; 2.0) | 1.3 (0.8; 2.2) |
| Household income | |||||
| ≥CAN$50,000 | ref | ref | ref | qref | ref |
| < CAN$50,000 | 1.6 (1.1; 2.4) | 0.8 (0.5; 1.3) | 1.1 (0.6; 1.9) | 0.9 (0.4; 2.1) | 1.3 (0.8; 2.2) |
| Mental health diagnosis | |||||
| No | ref | ref | ref | ref | ref |
| Yes | 1.7 (1.2; 2.5) | 0.6 (0.4; 0.9) | 1.2 (0.7; 2.0) | 1.8 (0.8; 4.0) | 1.3 (0.8; 2.3) |
Relative risks (RR) and 95% CI are weighted for non-response.
Adjusted RRs estimated using a generalized linear model with a Poisson family and log link, adjusted for age, sex and education as measured in cycle 24. 95% confidence are calculated from standard errors obtained with a sandwich estimator.
Bold indicates confidence intervals that exclude the null value of 1 for RR.
Discussion
Most participants report stable substance use
Cross-sectional studies on perceived changes in substance use,1, 2, 3,24 as well as possible hyperbole in the media (i.e. media reports suggesting a doubling of cannabis sales5 and a 38% increase in alcohol sales25 early in the pandemic) have fuelled concerns that problematic substance use might be rising to “epidemic levels” during the COVID-19 pandemic. Findings in our longitudinal study of young adults in Canada offer a less striking portrait, with most participants reporting stable substance use patterns from before to 9-15 months into the pandemic. Our results align with two online surveys of a representative probability panel in Canada (Canadian Perspectives Survey series 1 and 6 (CPSS1 and CPSS6)) conducted in March-April 2020 and January 2021 in which ≥75% and ≥49% of panellists, respectively reported that their weekly consumption of alcohol and cannabis had not changed.3,5
Weekly/daily substance use generally remained relatively stable except for cannabis
In NDIT, the prevalence of any and weekly/daily alcohol use, binge drinking, and combustible cigarette use all decreased during the pandemic. In contrast, weekly/daily use of cannabis and e-cigarettes increased by 5.6% and 1.6%, respectively. In addition, cannabis was the only substance for which the proportion of participants that initiated/increased use was higher between cycle 23 and 24 than between cycle 22 to 23. Two other longitudinal studies reported similar findings. Romm et al. reported an increase of 0.82 days in cannabis use in the past 30 days among 18-24 year-olds in six US metropolitan areas,26 and Leatherdale et al. reported increases in monthly, weekly, and daily cannabis use among 12-16 year-olds in Canada, although the increases were less than those expected based on trends observed in 2018 and 2019.12 However, caution is needed in comparing results because of differences in legal access to cannabis, and because the response proportions for the COVID-19 data collections in the other two studies was low.12,26
Decreases in alcohol use and binge drinking
In NDIT, we observed decreases in both alcohol use and binge drinking, and the incidence of initiated/increased and quit/decreased during the COVID-19 pandemic was larger than expected compared to incidence data from 2010 to 2020. Results on change in alcohol use in population-based samples thus far are not consistent. Two large UK studies (UK Household Longitudinal study for the 25-44 age group; the Daly and al. study in older adults10,27) suggested increases in overall alcohol consumption, including heavy alcohol use (≥ 4 drinks per occasion). Data on 13-18 year-olds in Iceland and 19-23 year-olds in Canada, however, suggested declines in alcohol intoxication28 and heavy drinking.11 Age, differences in access to alcohol, and country-specific norms may explain these differences. Our data support the premise offered in CPSS1 reports that decreases in social gatherings due to COVID-19 containment measures might underpin declines in alcohol use in Canada during the pandemic.5.
Modest declines in combustible cigarettes
We observed modest declines in combustible cigarette use during COVID-19. This aligns with other longitudinal studies,10,28,29 which also reported that declines were greater in younger age groups10 and among smokers with lower levels of nicotine dependence.29 We posit that changes in cigarette smoking during COVID-19 were not notable in NDIT because by age 30, nicotine dependence is well-established (such that current addicted smokers likely need more intense intervention than the pandemic to decrease consumption or quit) and further, the likelihood of initiation is low since most smoking initiation occurs during adolescence. Our data on e-cigarette use suggest a slight increase in prevalence, but this observation needs corroboration in other studies.
Change in substance use are heterogeneous across sociodemographic subgroups
We identified several factors associated with initiated/increased substance use during the pandemic. First, participants with only high school education had twice the risk of initiated/increased use of four of the five substances investigated (the exception was binge drinking). In juxtaposition, findings from the UK Household Longitudinal Study suggest that highly educated subgroups reported larger increases in alcohol and binge drinking.10 Other studies investigating socioeconomic factors did not report significant associations between education27 or income loss11 and change in substance use. More research is needed to better understand age-specific effects of social position and economic hardship on substance use during the COVID-19 pandemic.
Living alone was associated with initiated/increased cannabis, cigarette, and e-cigarette use. Living alone during a time when containment measures restricted social gatherings, could increase feelings of isolation and loneliness, both of which could increase psychological distress.2 Two exploratory studies during COVID-19, both with small sample sizes and low response proportions, identified self-isolation and coping with depression as motives for cannabis use during the pandemic.6,7 In Canada, reports from the two CPSS surveys cited stress, boredom and loneliness as the most frequently reported motives for cannabis and alcohol use during the pandemic.3,5
Compared to participants not living with children, both living with children under age 5 and living in a two-parent family were associated with lower risks of initiated/increased cannabis, combustible cigarette, and e-cigarette use. The literature on parental substance use during the pandemic is limited to two cross-sectional studies reporting perceived change in substance use.30,31 In contrast to NDIT in which findings were inconclusive due to low precision, 27.7% of Canadian parents living with children under age 18 reported increased alcohol consumption to cope with stressors and deteriorations in mental health during the pandemic, compared to 16.1% in adults with no children at home. Disruptions caused by school closures could underpin changes in parental substance use. Data from NORC's AmerikaSpeak representative probability-based panel suggest that US parents of children age 5-12 who received in-person teaching were at lower risk of reporting increasing substance use to cope with stress during the early months of the COVID-19 pandemic, compared to parents of children who received some virtual teaching (i.e., virtual teaching only or a combination of virtual and in-person teaching).30
Finally, history of a mental health diagnosis was associated with a lower risk of initiated/increased alcohol use, but a higher risk of initiated/increased cannabis use during the COVID-19 pandemic. The results for alcohol use contrasts reports from the CPSS1 indicating that Canadians with worse self-reported mental health were more likely to report increased frequency of cannabis, alcohol and tobacco use.3 However, mental health diagnoses are frequently underreported32 and may not even relate to mental health status during the pandemic.
Limitations of the study include lack of data on opioid use.33 Although past-year frequency is a standard indicator of substance use, it does not capture short-term changes in use or distinguish frequent and problematic use. While 99% of participants had already completed questionnaires for cycle 23 before Québec declared the COVID-19 state of sanitary emergency, reports of substance use in cycle 24 covered from 1 to < 4 months of the pre-pandemic period. However, evidence on past-year recall34, 35 suggests that reports are driven by more recent months, which likely limited contamination of measurements taken during the COVID-19 pandemic by pre-pandemic behaviours. Cycle 24 participants were less likely to report alcohol or combustible cigarette use at baseline and more likely to have university-educated mothers, which could limit generalizability of the findings. Attrition may have caused selection bias, but the use of non-response weights likely attenuated its effect on the results. The validity of nonresponse weights depends on the missing-at-random assumption, which is not testable in the data. While NDIT recruited a population-based sample similar to a same-year representative population-based sample,17 it is not representative of the Québec population so that the reported prevalences of substance use may not be generalizable. However, pre-pandemic prevalence of substance use in NDIT aligned with North American estimates.36 The changes in substance use observed from cycles 23 to 24 may not be entirely attributable to COVID-19 but could also relate to secular trends associated with transitioning from young to mid-adulthood,14,20,21,36 or by societal changes (e.g., legalization of cannabis use in 2018 in Canada).
Longitudinal studies are critical to quantifying change in substance use from before to during the COVID-19 pandemic. However, representative population-based data are needed so that findings are generalizable. Further research (including qualitative studies) is needed to disentangle the intra-individual vulnerabilities (e.g., personality, mental health) and environmental factors (e.g., financial instability, stress, lack of socialization) exacerbated by COVID-19 which underpin increases in substance use. The current global crisis has been linked to higher levels of psychological distress and substance use in vulnerable populations. We must therefore address the need for a cohesive integrated approach to improve resilience to prevent substance abuse and to avoid possible long-lasting effects of the pandemic on mental health and substance use. As we aim to recover and rebuild from COVID-19, we need more in-depth and longitudinal research to better understand the impact of major societal events such as this pandemic in the general population and perhaps more importantly, in marginalized and vulnerable subgroups.
Contributors
MPS and JOL conceptualized the current study. MN reviewed the literature. MPS designed the statistical analysis and GDTD performed the statistical analysis under her supervision. MPS, TR, and JOL verified the data and take responsibility for the integrity of the data. JOL acquired the funding for the NDIT study, and JOL, MPS and MB acquired the funding for the COVID-19 data collection. JOL, MPS and MN drafted the manuscript. TR, AP and GDTD prepared the Figures and Tables for the manuscript and Supplementary Material. TR is the NDIT project coordinator. All authors reviewed and edited the manuscript.
Data sharing agreement
NDIT data are available upon request. Access to NDIT data is open to any university-appointed or affiliated investigator upon successful completion of the application process. Masters, doctoral and postdoctoral students may apply through their primary supervisor. To gain access, applicants must complete a data access form available on our NDIT website (www.CELPHIE.ca) and return it to the principal investigator (jennifer.oloughlin@umontreal.ca). The procedure to obtain access to NDIT data is described in O'Loughlin, J., Dugas, E. N., Brunet, J., DiFranza, J., Engert, J. C., Gervais, A., Gray-Donald, K., Karp, I., Low, N. C., Sabiston, C., Sylvestre, M. P., Tyndale, R. F., Auger, N., Belanger, M., Barnett, T., Chaiton, M., Chenoweth, M. J., Constantin, E., Contreras, G., Kakinami, L., Labbe, A., Maximova, K., McMillan, E., O'Loughlin, E. K., Pabayo, R., Roy-Gagnon, M. H., Tremblay, M., Wellman, R. J., Hulst, A., Paradis, G., 2015. Cohort Profile: The Nicotine Dependence in Teens (NDIT) Study. Int J Epidemiol. 44(5), 1537-1546. doi: 10.1093/ije/dyu135.
Declaration of interests
We declare no competing interests.
Acknowledgments
The NDIT study was supported by the Canadian Cancer Society (grant numbers 010271, 017435, 704031) and the Canadian Institutes of Health Research (grant number 451832). The funders were not involved in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript. MPS holds a J2 Salary award from the FRQ-S. KM holds the Murphy Family Foundation Chair in Early Life Interventions. JOL held a Canada Research Chair in the Early Determinants of Adult Chronic Diseases 2006-21. We thank the NDIT participants.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lana.2021.100168.
Appendix. Supplementary materials
Reference
- 1.Pollard MS, Tucker JS, Green HD., Jr. Changes in Adult Alcohol Use and Consequences During the COVID-19 Pandemic in the US. JAMA Network Open. 2020;3(9) doi: 10.1001/jamanetworkopen.2020.22942. e2022942-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lorant V, Smith P, Van den Broeck K, Nicaise P. Psychological distress associated with the COVID-19 pandemic and suppression measures during the first wave in Belgium. BMC Psychiatry. 2021;21(1):112. doi: 10.1186/s12888-021-03109-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rotermann M. Canadians who report lower self-perceived mental health during the COVID-19 pandemic more likely to report increased use of cannabis, alcohol and tobacco. 2020 https://www150.statcan.gc.ca/n1/en/catalogue/45280001202000100008 (accessed 2021-08-18) [Google Scholar]
- 4.Pierce M, Hope H, Ford T, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. The Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Statistics Canada. Alcohol and cannabis use during the pandemic: Canadian Perspectives Survey Series 6. 2021. https://www150.statcan.gc.ca/n1/daily-quotidien/210304/dq210304a-eng.htm (accessed 2021-08-04).
- 6.Cousijn J, Kuhns L, Larsen H, Kroon E. For better or for worse? A pre-post exploration of the impact of the COVID-19 lockdown on cannabis users. Addiction. 2021;116(8):2104–2115. doi: 10.1111/add.15387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bartel SJ, Sherry SB, Stewart SH. Self-isolation: A significant contributor to cannabis use during the COVID-19 pandemic. Subst Abus. 2020;41(4):409–412. doi: 10.1080/08897077.2020.1823550. [DOI] [PubMed] [Google Scholar]
- 8.Zajacova A, Jehn A, Stackhouse M, Denice P, Ramos H. Changes in health behaviours during early COVID-19 and socio-demographic disparities: a cross-sectional analysis. Canadian Journal of Public Health. 2020;111(6):953–962. doi: 10.17269/s41997-020-00434-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guignard R, Andler R, Quatremère G, et al. Changes in smoking and alcohol consumption during COVID-19-related lockdown: a cross-sectional study in France. Eur J Public Health. 2021 doi: 10.1093/eurpub/ckab054. (accessed 2021-07-21) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Niedzwiedz CL, Green MJ, Benzeval M, et al. Mental health and health behaviours before and during the initial phase of the COVID-19 lockdown: longitudinal analyses of the UK Household Longitudinal Study. J Epidemiol Community Health. 2021;75(3):224–231. doi: 10.1136/jech-2020-215060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Minhas M, Belisario K, González-Roz A, Halladay J, Murphy JG, MacKillop J. COVID-19 impacts on drinking and mental health in emerging adults: Longitudinal changes and moderation by economic disruption and sex. Alcohol Clin Exp Res. 2021;45(7):1448–1457. doi: 10.1111/acer.14624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leatherdale ST, Bélanger RE, Gansaonré RJ, et al. Examining the impact of the early stages of the COVID-19 pandemic period on youth cannabis use: adjusted annual changes between the pre-COVID and initial COVID-lockdown waves of the COMPASS study. BMC Public Health. 2021;21(1):1181. doi: 10.1186/s12889-021-11241-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O'Loughlin J, Dugas EN, Brunet J, et al. Cohort Profile: The Nicotine Dependence in Teens (NDIT) Study. Int J Epidemiol. 2015;44(5):1537–1546. doi: 10.1093/ije/dyu135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen P, Jacobson KC. Developmental trajectories of substance use from early adolescence to young adulthood: Gender and racial/ethnic differences. J Adolesc Health. 2012;50(2):154–163. doi: 10.1016/j.jadohealth.2011.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McGinty EE, Presskreischer R, Han H, Barry CL. Psychological Distress and Loneliness Reported by US Adults in 2018 and April 2020. JAMA. 2020 doi: 10.1001/jama.2020.9740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pierce M, Hope H, Ford T, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. The Lancet Psychiatry. 2020;7(10):883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Paradis G, Lambert M, O'Loughlin J, et al. The Quebec Child and Adolescent Health and Social Survey: design and methods of a cardiovascular risk factor survey for youth. Can J Cardiol. 2003;19(5) [PubMed] [Google Scholar]
- 18.Gouvernement du Québec. La maladie à coronavirus (COVID-19) au Québec 2021. https://www.quebec.ca/sante/problemes-de-sante/a-z/coronavirus-2019 (accessed October 7 2021).
- 19.Institut national de santé publique du Québec. Ligne du temps COVID-19 au Québec. 2021. https://www.inspq.qc.ca/covid-19/donnees/ligne-du-temps (accessed October 7th 2021).
- 20.Windle M. Sex differences in substance use from adolescence to young adulthood: Tests of increases in emergent adulthood and maturing out in later young adulthood. Drug Alcohol Depend. 2020;207 doi: 10.1016/j.drugalcdep.2019.107813. [DOI] [PubMed] [Google Scholar]
- 21.Evans-Polce RJ, Vasilenko SA, Lanza ST. Changes in gender and racial/ethnic disparities in rates of cigarette use, regular heavy episodic drinking, and marijuana use: Ages 14 to 32. Addict Behav. 2015;41:218–222. doi: 10.1016/j.addbeh.2014.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McRae L, O'Donnell S, Loukine L, Rancourt N, Pelletier C. Mood and Anxiety Disorders in Canada, 2016. Health Promotion and Chronic Disease Prevention in Canada. 2016;36(12) doi: 10.24095/hpcdp.36.12.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zou G. A Modified Poisson Regression Approach to Prospective Studies with Binary Data. Am J Epidemiol. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 24.Taylor S, Paluszek MM, Rachor GS, McKay D, Asmundson GJG. Substance use and abuse, COVID-19-related distress, and disregard for social distancing: A network analysis. Addict Behav. 2021;114 doi: 10.1016/j.addbeh.2020.106754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zipursky JS, Stall NM, Silverstein WK, et al. Alcohol Sales and Alcohol-Related Emergencies During the COVID-19 Pandemic. Ann Intern Med. 2021;174(7):1029–1032. doi: 10.7326/M20-7466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Romm KF, Patterson B, Crawford ND, et al. Changes in young adult substance use during COVID-19 as a function of ACEs, depression, prior substance use and resilience. Subst Abus. 2021 doi: 10.1080/08897077.2021.1930629. (accessed 2021-08-02) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Daly M, Robinson E. High-Risk Drinking in Midlife Before Versus During the COVID-19 Crisis: Longitudinal Evidence From the United Kingdom. Am J Prev Med. 2021;60(2):294–297. doi: 10.1016/j.amepre.2020.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thorisdottir IE, Asgeirsdottir BB, Kristjansson AL, et al. Depressive symptoms, mental wellbeing, and substance use among adolescents before and during the COVID-19 pandemic in Iceland: a longitudinal, population-based study. The Lancet Psychiatry. 2021;8(8):663–672. doi: 10.1016/S2215-0366(21)00156-5. [DOI] [PubMed] [Google Scholar]
- 29.Siddiqi K, Siddiqui F, Khan A, et al. The Impact of COVID-19 on Smoking Patterns in Pakistan: Findings From a Longitudinal Survey of Smokers. Nicotine Tob Res. 2021;23(4):765–769. doi: 10.1093/ntr/ntaa207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jorge V, Verlenden SP, Catherine N, Rasberry Nicole Liddon, Marci Hertz Greta Kilmer, Viox Melissa Heim, Lee Sarah, Cramer Neha K., Barrios Lisa C., Ethier Kathleen A. Association of Children's Mode of School Instruction with Child and Parent Experiences and Well-Being During the COVID-19 Pandemic — COVID Experiences Survey, United States, October 8–November 13, 2020. MMWR Morb Mortal Wkly Rep. 2021;70:369–376. doi: 10.15585/mmwr.mm7011a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gadermann AC, Thomson KC, Richardson CG, et al. Examining the impacts of the COVID-19 pandemic on family mental health in Canada: findings from a national cross-sectional study. BMJ Open. 2021;11(1) doi: 10.1136/bmjopen-2020-042871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Takayanagi Y, Spira AP, Roth KB, Gallo JJ, Eaton WW, Mojtabai R. Accuracy of Reports of Lifetime Mental and Physical Disorders. JAMA Psychiatry. 2014;71(3):273. doi: 10.1001/jamapsychiatry.2013.3579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gomes T, Kitchen SA, Murray R. Measuring the Burden of Opioid-Related Mortality in Ontario, Canada, During the COVID-19 Pandemic. JAMA Network Open. 2021;4(5) doi: 10.1001/jamanetworkopen.2021.12865. e2112865-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Harrison LD, Hughes A. The validity of self-reported drug use: Improving the accuracy of survey estimates: US Department of Health and Human Services. National Institutes of Health. 1997 [Google Scholar]
- 35.Khalili P, Nadimi AE, Baradaran HR, et al. Validity of self-reported substance use: research setting versus primary health care setting. Subst Abuse Treat Prev Policy. 2021;16(1):66. doi: 10.1186/s13011-021-00398-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wellman RJ, Dugas EN, O'Loughlin EK, Sylvestre MP, Pelekanakis A, O'Loughlin J. Natural course of co-use of alcohol and cannabis in adolescents and young adults in Montréal, Canada. Psychol Addict Behav. 2021 doi: 10.1037/adb0000766. (accessed 2021-7-29) [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.