Abstract
Objective
Tuberculosis (TB) treatment management services (TTMSs) are crucial for improving patient treatment adherence. Under the TB integrated control model in China, healthcare workers (HCWs) in the primary healthcare (PHC) sectors are responsible for TTMS delivery. This mixed-method study aimed to explore the status of and barriers to TTMS delivery faced by HCWs in PHC sectors from the health organisational and patient perspectives.
Design
We completed a questionnaire survey of 261 TB healthcare workers (TB HCWs) and 459 patients with TB in the PHC sector and conducted 20 semistructured interviews with health organisational leaders, TB HCWs and patients with TB. SPSS V.22.0 and the framework approach were used for data analysis.
Setting
PHC sectors in Southwest China.
Results
Our results showed that TTMS delivery rate by HCWs in PHC sectors was <90% (88.4%) on average, and the delivery rates of intensive and continuation phase directly observed therapy (DOT) were only 54.7% and 53.0%, respectively. HCWs with high work satisfaction and junior titles were more likely to deliver first-time home visits and DOT services. Our results suggest that barriers to TTMS delivery at the organisational level include limited patient-centred approaches, inadequate resources and incentives, insufficient training, poor cross-sectional coordination, and strict performance assessment. At the patient level, barriers include low socioeconomic status, poor health literacy and TB-related social stigma.
Conclusion
TTMSs in Southwest China still need further improvement, and this study highlighted specific barriers to TTMS delivery in the PHC sector. Comprehensive measures are urgently needed to address these barriers at the organisational and patient levels to promote TB control in Southwest China.
Keywords: Tuberculosis, PRIMARY CARE, HEALTH SERVICES ADMINISTRATION & MANAGEMENT
Strengths and limitations of this study.
This is a mixed-method study on accessing the status of and barriers to tuberculosis treatment management service (TTMS) delivery by healthcare workers (HCWs) in the primary healthcare sectors (PHC) of Southwest China.
This study collected perspectives from organisations and patients and used the practical robust implementation and sustainability model model to evaluate specific barriers to TTMS delivery.
We collected 720 questionnaires from HCWs and patients and conducted 20 interviews with leaders, HCWs and patients in a total of 71 PHC sectors.
Further studies are required to provide more evidence for producing more effective tuberculosis control strategies, as well-evidenced implementation strategies that can address current barriers in TTMS delivery could not be provided in this study.
Introduction
Tuberculosis (TB) is a leading cause of death worldwide.1 According to the WHO global TB report 2021, there was a large global drop in the number of newly diagnosed TB cases (fall from 7.1 million in 2019 to 5.8 million in 2020).1 However, the most immediate consequence of this large drop is an increase in the number of deaths from TB in 2020 (from an estimated 1.2 million deaths among HIV-negative people in 2019 to an estimated 1.3 million in 2020).1 The Chinese government pays great attention to addressing the TB epidemic and aims to reduce the incidence of TB to less than 55/100 000 by 2022 and maintain a low mortality rate below 3/100 000 population.2 3 Although TB case notification in China has decreased from 70.6/100 000 population in 2012 to 58/100 000 population in 2019, with a treatment success rate above 90%.1 2 China is listed as high-burden country with TB, HIV-associated TB and multidrug/rifampicin-resistant TB (MDR) for 2021–2025 in the WHO global TB report 2021.1
The goal of China’s latest Action Plan to Stop TB (2019–2022) is to reduce the incidence of TB nationwide to less than 55/100 000 population by 2022 and maintain a low mortality rate below 3/100 000 population.2 To accomplish this goal, TB prevention and control programmes have been further improved with enhanced service capacity, strengthening the prevention and control measures for key populations and key areas, advancing standardised diagnosis and treatment coverage, and increasing the public awareness level of TB prevention and control.2 Patient adherence to anti-TB treatment plays an important role in curing and avoiding DR-TB (drug-resistant TB); hence, treatment management is essential for patients with TB to ensure treatment adherence, monitor adverse side effects from treatment and avoid the development of DR-TB.4 Since the Chinese National 12th Five-Year TB Control Plan (2011–2015) came out in 2011, the TB control model in China has started using the integrated TB control model in most regions.5 Under the integrated TB control model, the Centers for Disease Control and Prevention (CDC) are responsible for TB programme governance, surveillance, training and health promotion; TB-designated hospitals are responsible for diagnosis and treatment; and primary healthcare (PHC) sectors are responsible for referrals, tracing, health education and tuberculosis treatment management services (TTMSs).5 Later, China’s National 13th Five-Year TB Control Plan (2016–2020) combined with the Action Plan to Stop TB (2019–2022) requested further strengthening of TB prevention and control, which emphasised TTMSs and strengthened the implementation of various measures to reduce the TB epidemic in China.2 6 TTMSs are one of the key BPHSs (basic public health services) programmes available to all residents in China (one of the priorities of the new health reform launched in 2009) and is delivered by TB healthcare workers (TB HCWs) in the PHC sector.6 7 The BPHS guidelines aimed to raise standard TTMS rates and treatment success rates to above 90%.6 7 The TTMSs for diagnosed patients with TB is delivered by HCWs in the PHC sector, under the supervision of the CDC, with coordination from other departments, such as assistance from the TB-designated hospital to deal with patient side effects and support from the Department of Education to conduct health education in the student population.7
A study in Jiangxi indicated that TTMS under an integrated TB control model improved treatment outcomes.8 A study in Wuhan indicated that TTMSs are crucial for monitoring treatment complications and reducing the development of DR-TB.9 10 Other studies have shown that, in more developed areas in China, TTMS coverage was highly improved and produced impressive effects.8 9 11–14 A few studies have reported the status of TTMS delivery in resource-limited and mountainous regions with a high TB/DR-TB burden in China. One study found that only 37.1% of patients with TB received TTMSs from HCWs in West China,15 and study in Chongqing found that 34.3% of patients with TB never received TTMSs from HCWs.16 However, few studies have focused on the perspective of HCWs to evaluate the current TTMS programme under the integrated TB control model. Therefore, this study not only aimed to assess the delivery status of the TTMS programme from the perspectives of both organisations and patients, but also to explore the specific barriers to TTMS delivery faced by HCWs in PHC sectors in order to provide evidence for promoting TB control and treatment outcomes.
Methods
Study design
This cross-sectional study used mixed research methods17 to collect data from June to December 2018. Questionnaire surveys and semistructured in-depth interviews were conducted to evaluate the delivery of TTMSs in the PHC sector from both health organisations (HCWs and leaders) and patients’ perspectives.
Study setting
The prevalence of TB in the western region is significantly higher than that in the central and eastern regions of China.18 Chongqing Municipality is located at the junction of the Yangtze and Jialing rivers, and it has a population of 32.09 million.19 This region has a relatively developed socioeconomic status, with a gross domestic product (GDP) of CNY2.5 trillion and a per capita GDP of CNY55.6 thousand in 2020.19 Chongqing’s growing population depends more on secondary and tertiary industries as the main economic activity.19 Its urbanisation rate and literacy rates were 69.5% and 98.4%, respectively, in 2021.19 The TB incidence in Chongqing Municipality (2019) ranks tenth (75/100 000) in China.20
Guizhou Province is a mountainous province in West China with a population of 38.6 million.21 A total of 50.9% of its population depends on tertiary industries as the main source of income.21 The employment rate and literacy rates were 49.0% and 93.3% respectively in 2020.21 The area maintains a relatively less developed socioeconomic status, with a GDP of CNY1.8 trillion and a per capita GDP of CNY46.3 thousand in 2020.21 The incidence of TB in Guizhou Province (2019) was ranked third (133.5/100 000) in China, after Xinjiang and Tibet.20
A stratified random sampling method was used to select the study sites in Chongqing Municipality and Guizhou Province. All counties/districts in Chongqing Municipality and Guizhou Province were grouped into three levels according to their socioeconomic status (GDP) in 201822: the relatively developed (GDP in the highest 30%), the medium developed (GDP in the middle 40%) and the relatively less developed (DGP in the lowest 30%). From each group of counties/districts, four counties/districts were randomly selected as study sites. Twelve districts/counties were included in this study. All of the PHC sectors (including both community health centres (CHCs) and township hospital centres (THCs)) in the 12 selected counties/districts and a total of 71 PHC sectors were included in this study.
Study participants and data collection
Quantitative study
All adult patients with pulmonary TB who met the following criteria were recruited from the 71 PHC sectors in the 12 selected counties/districts: (1) registered at TB dispensaries and were diagnosed with drug-sensitive pulmonary TB according to national TB diagnosis standards; (2) completed standard anti-TB drug treatment for at least 4 months, which indicated that they received TTMSs for both intensive (first 2 months) and continuation phases (following 4 months) and (3) aged 15 years and older. Patients who (1) had extrapulmonary TB, (2) could not express themselves clearly (had disturbance of consciousness or difficulties with speech or hearing) and (3) were unwilling to participate in the study were excluded. Patient recruitment was facilitated by the local PHC sectors in the study counties/districts. First, the research group members provided a detailed explanation of the study objectives to all the potential participants. Those who were willing to participate in the study were asked to read and sign the informed consent form to ensure confidentiality.
The sample size was estimated using the Kish and Leslie formula23:
Where, n is the minimum desired sample size. Zα is the standard normal deviate, usually set as 1.96, corresponding to a 5% level of significance. P is the average rate of TB treatment management, set at 37.1% based on estimates from the available literature,15 and d is the degree of accuracy (precision) set at 5% (0.05). Therefore, the calculated minimum sample size for patient participants was 359. A total of 481 patients with TB were recruited to participate in the survey, of whom 16 declined. Six patients with TB <15 years were excluded, and finally, 459 patients with TB were included in the analysis (response rate: 95.4%).
All HCWs who were TB control medical staff in the PHC sectors in the selected counties/districts and who were willing to participate in the study were recruited as participants. TB HCWs unwilling to participate in the study were excluded. There were 261 TB HCWs in the selected counties/districts. Finally, all 261 TB HCWs were recruited and willing to participate in the survey, and zero declined (response rate: 100.0%). Local CDCs in the study districts/counties facilitated HCW recruitment.
Structured questionnaires were administered to collect data from participating patients with TB and HCWs. Among patients with TB, the structured survey that was administered asked the participants about their demographic information (eg, gender, age and residence) and TTMSs received from HCWs during their treatment (eg, intensive phase directly observed therapy (DOT) and continuation phase DOT). Among HCWs, the questionnaire included demographic and work-related information (eg, gender, age, professional title and working years), work satisfaction and delivery situation of TTMSs (eg, first-time home visit). Questionnaires were designed by our research team based on existing literature reports and then we consulted with related experts.
In the reliability evaluation, Cronbach’s α was calculated to determine the reliability of the questionnaire for patients with TB and the HCWs’ questionnaire. Cronbach’s α ranges from 0 to 1; the higher the coefficient value (>0.8), the better the reliability and internal consistency. Both the patients with TB (Cronbach’s α=0.816) and HCWs (Cronbach’s α=0.910) questionnaires had good reliability and internal consistency. In the validity evaluation, the face validity coefficient was calculated through the Pearson correlation coefficient (r) to determine the validity of the questionnaire for patients with TB. The questionnaire had r>0.4 and p<0.001, indicating good face validity. The questionnaire for the HCWs, which contained 60 TTMS questions, also had good construct validity (item-centent validity index (I-CVI)=0.850–1.000; scale-centent validity index (S-CVI)=0.960).
In the reliability evaluation, Cronbach’s α was calculated to determine the reliability of the questionnaire for patients with TB and the HCWs’ questionnaire. Cronbach’s α ranges from 0 to 1; the higher the coefficient value (>0.8), the better the reliability and internal consistency. Both the patients with TB (Cronbach’s α=0.816) and HCWs (Cronbach’s α=0.910) questionnaires had good reliability and internal consistency. In the validity evaluation, the face validity coefficient was calculated through the Pearson correlation coefficient (r) to determine the validity of the questionnaire for patients with TB. The questionnaire had r>0.4 and p<0.001, indicating good face validity. The questionnaire for the HCWs, which contained 60 TTMS questions, also had good construct validity (I-CVI=0.850–1.000; S-CVI=0.960).
All questionnaires were administered by trained investigators from our research group in a meeting or clinic room in each PHC sector. Patients with TB and HCWs who volunteered to participate in the study were asked to read the informed consent form and sign it. Each completed questionnaire was checked and examined for quality control by trained investigators.
Qualitative study
In-depth interviews were conducted to explore the current status and identify the barriers of TTMS delivery from HCWs to patients with TB. Purposive sampling was used to select participants with different backgrounds, ages and experiences related to TTMS. An integrated TB control model was established, and TTMSs were provided in all included counties/districts. Therefore, in-depth interviews were conducted with: HCWs from the PHC sectors of different socioeconomic levels who had delivered TTMSs for at least 1 year during the study period; leaders from the local CDC and the Health Commission who were responsible for the TB control programme during the study period; and patients from regions of different socioeconomic levels who had received TTMSs and were about to end their TB treatment during the study, which ensured that patients had sufficient experience related to TTMS. During recruitment, all HCWs, leaders and patients were approached and provided detailed explanations of the study and its objectives. Those who expressed an interest in volunteering to participate in the in-depth interview were asked to read and sign an informed consent form to confirm their voluntary participation in the study.
The sample size of the qualitative study was determined by the point of data ‘saturation’.24 Recruitment continued until evidence of data saturation was obtained and adding further participants did not generate new findings. Each interview was conducted face to face by at least two trained interviewers to enhance the information’s trustworthiness and credibility. During each interview, one interviewer performed the interview according to the semistructured topic guides, while the other interviewer was responsible for taking notes of the key information and could supplement questions to the interview as necessary. At the end of each interview, the interviewers discussed the findings and key information obtained to confirm whether a supplementary interview was required. Information related to TTMS delivery was cross-validated between patients (service receivers) and HCWs (service providers) to increase information trustworthiness. Documentary sources such as regulations and standard service procedures have also been used to enhance information credibility. Nine purposely selected leaders, seven HCWs and four patients participated in the in-depth interviews.
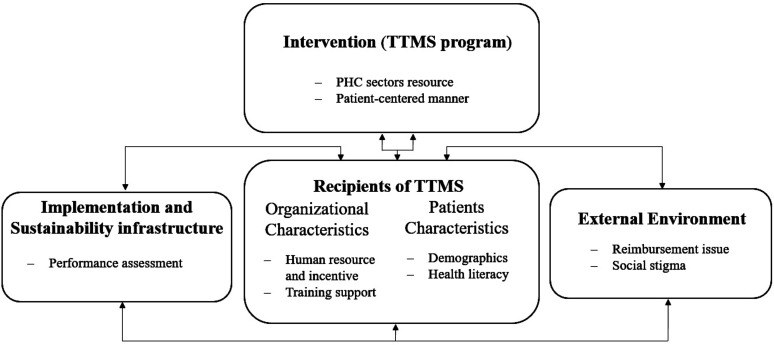
Semistructured topic guides with open-ended questions were used in all interviews. The guiding framework for topic design was the practical robust implementation and sustainability model (PRISM).25 This model considers how the intervention design, recipients, external environment, and implementation and sustainability infrastructure influence health programme implementation and success, and is widely used as a theoretical framework in implementation research.25–27 Using the PRISM guide, this study collected data on the barriers to TTMS delivery in terms of the following aspects: (1) intervention design, (2) recipients, (3) external environment and (4) implementation and sustainability infrastructure. The adaptation of PRISM in this study is illustrated in figure 1. All interviews were conducted in Mandarin or the local language in meeting rooms in the PHC sector. Only participants and interviewers were present at the interview location. Each interview lasted approximately 40–60 min and was audiorecorded with the consent of the participants.
Figure 1.
Adapted practical robust implementation and sustainability model (PRISM) for barriers on TTMS delivery in PHC sectors. This figure presents the four core domains of PRISM for barriers on TTMS delivery in PHC sectors, including: (1) TTMS programme design; (2) the recipients, (3) the external environment and (4) the implementation and sustainability infrastructure. Activated elements for each domains were presented in boxes. HCW, healthcare worker; PHC, primary healthcare; TTMS, tuberculosis treatment management service.
Data analysis
The data analysis integrated quantitative and qualitative data to assess the status of and barriers to TTMS programme delivery by HCWs in the PHC sectors. For example, patients’ demographic information from questionnaires integrated with the results from in-depth interviews allowed us to determine how patients’ social economy and healthy literacy affected TTMS delivery. In addition, qualitative results regarding patient-centred manners, training support provided to HCWs, the workload and performance evaluations of HCWs, and so on, clarified the quantitative results regarding the proportion of TTMSs received and the delivery rate of TTMSs by HWCs.
Quantitative analysis
Data were entered using Epi Data V.3.1 and then analysed using the Statistical Package for the Social Sciences (SPSS V.22.0 (IBM)). Missing data were excluded from the analysis—when analysing gender, age, medical school education, major, professional title, number of BPHS programmes undertaken, monthly income and work satisfaction of HCWs, and so on, only 259, 249, 247, 256, 240, 225, 242 and 259 HCWs responded to the questions in the survey; therefore, we removed the data from the HCWs who did not respond to these questions. A two-tailed probability level of p<0.05 was chosen as the level of statistical significance. Descriptive statistics were used to describe the participants’ demographic characteristics and TTMS delivery rates. Factors associated with lower delivery rates (<90%), as screened by the χ2 test (p<0.05) (online supplemental appendix 1), were entered into multivariate logistic regression models (delivery rate <90%=1, delivery rate >90%=0), which were used to examine the effects of these factors on TTMS delivery.
bmjopen-2021-053797supp001.pdf (211KB, pdf)
Qualitative analysis
The framework approach was used to analyse all qualitative data following a five-step process: (1) familiarisation, (2) adapting the theoretical framework, (3) indexing, (4) summarising and (5) data synthesis and interpretation.28 29 Subsequently, all interviews were carefully transcribed into Word documents, reviewed for accuracy, and coded and classified by our research team members. We identified themes of the theoretical framework on TTMS delivery barriers based on the four domains of PRISM,25 including: (1) intervention design (PHC sector resource and patient-centred mannerisms); (2) recipients (human resources and incentives, training support, socioeconomy and health literacy); (3) external environment (health insurance, cross-sectional coordination and social stigma) and (4) implementation and sustainability infrastructure (performance assessment). All the names of the participants were removed from the results to maintain anonymity. According to the 13th 5-Year TB Prevention and Control Plan, the targeted TTMS delivery rate from HCWs to patients with TB is >90%0.5 Therefore, a delivery rate below 90% was described as a lower delivery rate in this study.
Definitions
PHC sectors in China include CHCs and stations in urban areas, THCs and village health clinics in rural areas.4 TB healthcare workers (TB HCWs) include healthcare professionals in the PHC sector that are responsible for TTMS delivery. TTMSs are one of the key basic public health services available to all residents in China, and these are delivered by TB HCWs in the PHC sector, with seven themes: first-time home visits, health education, supervising drug intake, follow-up supervision, case closing evaluation, other services and services among patient’s family members.6 7 Both the Chinese National BPHS guidelines and the 13th 5-Year TB Prevention and Control Plan set a target TTMS rate of >90%.6 7 Therefore, in this study, a delivery rate <90% is described as a lower delivery rate.
Patient and public involvement
There were no patients or public involvement in the design, conduct, reporting or dissemination plans of this study.
Results
Characteristics of participants
Participants for the quantitative study
In total, 261 TB HCWs and 459 patients with TB were included in the quantitative analysis (table 1). Among the HCWs, 66.4% (n=172) were female, 71.5% (n=178) were aged 20–39 years, 72.4% (n=189) worked at THCs, and 50.0% (n=120) and 35.8% (n=86) had junior and non-professional titles, respectively. Nearly 60% (n=155) of the HCWs had junior college education, and over 80% (n=202) had a medical school education background (32.4% majored in clinical medicine and 30.5% majored in nursing). More than half (53.3%, n=139) of the HCWs undertook 2–3 BPHS programmes in PHC sectors, and only13.0% (n=34) were dedicatedly in charge of TB programmes. The majority (88.9%, n=242) had a monthly income of CNY2500–CNY4500, obtained traning 2/6 months (51.7%, n=135); and notably, 40.5% (n=105) reported low work satisfaction.
Table 1.
Characteristics of participants surveyed by questionnaires
| Demographic characteristic | No | % |
| HCWs in questionnaire survey | ||
| Gender (n=259) | ||
| female | 172 | 66.4 |
| male | 87 | 33.6 |
| Age (n=249) | ||
| 20–29 | 94 | 37.8 |
| 30–39 | 84 | 33.7 |
| 40–50 | 52 | 20.9 |
| >50 | 19 | 7.6 |
| Education (n=259) | ||
| Technical secondary school or below | 60 | 23.2 |
| Junior college | 155 | 59.8 |
| Undergraduate college or above | 44 | 17.0 |
| Medical school education (n=247) | ||
| Yes | 202 | 81.8 |
| No | 45 | 18.2 |
| Major (n=256) | ||
| Clinical Medicine | 83 | 32.4 |
| Nursing | 78 | 30.5 |
| Public health | 33 | 12.9 |
| Chinese medicine | 27 | 10.5 |
| Other | 17 | 6.6 |
| Region (n=261) | ||
| Relatively developed | 93 | 35.6 |
| Medium developed | 89 | 34.1 |
| Less developed | 79 | 30.3 |
| Working place (n=261) | ||
| Township health centre | 189 | 72.4 |
| Community health centre | 72 | 27.6 |
| Professional Title (n=240) | ||
| Non | 86 | 35.8 |
| Junior | 120 | 50.0 |
| Intermediate | 31 | 12.9 |
| Deputy senior | 3 | 1.3 |
| No of BPHS programmes undertook (n=261) | ||
| TB programme only | 34 | 13.0 |
| 2–3 | 139 | 53.3 |
| ≥4 | 88 | 33.7 |
| Monthly income (CNY) (n=242) | ||
| <2500 | 52 | 21.5 |
| 2500–3500 | 89 | 36.8 |
| 3500–4500 | 74 | 30.6 |
| >4500 | 27 | 11.2 |
| Training frequency (n=261) | ||
| 0/6 months | 13 | 5.0 |
| 1/6 months | 56 | 21.5 |
| 2/6 months | 135 | 51.7 |
| 3/6 months | 36 | 13.8 |
| >3/6 months | 21 | 8.0 |
| Work satisfaction (n=259) | ||
| High satisfaction | 58 | 22.4 |
| Middle satisfaction | 96 | 37.1 |
| Low satisfaction | 105 | 40.5 |
| Patients with TB in questionnaire survey | ||
| Gender (n=459) | ||
| Male | 324 | 70.6 |
| Female | 135 | 29.4 |
| Age (n=459) | ||
| <40 | 94 | 20.5 |
| 40–49 | 96 | 20.9 |
| 50–59 | 78 | 17.0 |
| ≥60 | 191 | 41.6 |
| Ethnicity (n=459) | ||
| Han | 359 | 78.2 |
| Ethnic minority | 100 | 21.8 |
| Marital status (n=459) | ||
| Single | 69 | 15.0 |
| Married | 320 | 69.7 |
| Divorced/widowed | 70 | 15.3 |
| Residence (n=459) | ||
| Urban | 81 | 17.6 |
| Rural | 378 | 82.4 |
| Registered information (n=459) | ||
| Permanent resident | 437 | 95.2 |
| Migrant | 22 | 4.8 |
| Education (n=459) | ||
| Primary and below | 257 | 56.0 |
| Junior middle school | 125 | 27.2 |
| High school and above | 77 | 16.8 |
| Occupation (n=459) | ||
| Staff/cadre/retiree | 50 | 10.9 |
| Self-employed | 10 | 2.2 |
| Farmer/migrant worker | 315 | 68.6 |
| Student | 20 | 4.4 |
| Others | 64 | 13.9 |
BPHS, basic public health service; HCW, healthcare worker; TB, tuberculosis.
Among the patients with TB, the majority of the patients were male (70%, n=324), married (69.7%, n=320), of Han ethnicity (78.2%, n=359) and 41.6% (n=191) were aged ≥60 years. A total of 82.4% (n=378) of the patients lived in rural residences, and 95.2% (n=437) lived in permanent residences. Almost 70% (n=315) of the patients were farmer/migrant workers, and 56.0% (n=257) had only primary education or below.
Participants for the qualitative study
Nine organisational leaders, seven HCWs and four patients with TB were interviewed. Most organisational leaders were male (7/9), with deputy senior titles (5/9) and worked for 7.6 years an average. The majority of HCWs were female (5/7), technical secondary school educated (6/7), majored in clinical medicine (4/5) and 4/5 came from CHCs with no or junior professional titles. In addition, among four interviewed patients, which included two drug-sensitive TB (DS-TB) and two DR-TB patients, respectively, and all patients completed anti-TB therapy (6–8 months therapy for DS-TB, and 24 months therapy for DR-TB).
Quantitative results regarding TTMS delivery status
The survey of patient with TB showed that 76.0% (n=349) of the patients received TTMSs from HCWs in CHCs at some point during their entire course of treatment (83.7% and 76.7% during their intensive and continuation phases, respectively). Just around 40.0% (n=189) received TTMSs from HCWs in THCs/village clinics during their whole course of treatment (45.1% and 42.3% during their intensive and continuation phases, respectively). Only 17.0% (n=78) received standard TTMSs from HCWs during their entire course of treatment (18.1% and 55.8% for their intensive and continuation phases, respectively). A total of 2.8% (n=13) did not receive TTMSs from HCWs (3.9% and 7.2% during their intensive and continuation phases, respectively; table 2).
Table 2.
TTMS TB patient received from HCWs during treatment (n=459)
| Variable | No | % |
| Ever received TTMS from HCWs in CHCs | ||
| Intensive phase | 384 | 83.7 |
| Continuation phase | 352 | 76.7 |
| Whole course of treatment | 349 | 76.0 |
| Ever received TTMS from HCWs in THCs/village clinics | ||
| Intensive phase | 207 | 45.1 |
| Continuation phase | 194 | 42.3 |
| Whole course of treatment | 189 | 41.2 |
| Received standard TTMS from HCWs | ||
| Intensive phase | 83 | 18.1 |
| Continuation phase | 256 | 55.8 |
| Whole course of treatment | 78 | 17.0 |
| Never received TTMS from HCWs | ||
| Intensive phase | 18 | 3.9 |
| Continuation phase | 33 | 7.2 |
| Whole course of treatment | 13 | 2.8 |
CHC, community health centre; HCW, healthcare worker; TB, tuberculosis; THC, township health centre; TTMS, tuberculosis treatment management services.
The HCWs survey showed that the average delivery rate of TTMSs (involving 60 service items in total) in the PHC sector was 88.4%, and 13 TTMS items had a lower delivery rate (<90%). Notably, the delivery rates of DOT in the intensive phase and continuation phases were low, with proportions of 54.7% and 53.0%, respectively. In addition, less than half (44.9%) of HCWs in PHC sectors provided services related to collecting patient sputum samples during the follow-up supervision phase. Less than half of the HCWs provided food or transport assistance for poor patients with TB (45.2%), provided subsistence allowance or psychological support for migrant patients (49.6%), and provided injection treatment for patients with MDR-TB (41.0%). Moreover, less than 60% provided supervision for newly released prison patients (58.9%) and established platforms for TB patient communication (57.8%) (table 3).
Table 3.
TTMS with lower delivery rate provided by HCWs in PHC sectors (n=239)
| Services | Delivery rate N (%) |
| First time home visit | |
| Patients’ peer supervision establish (n=235) | 185 (78.7) |
| DOT | |
| Intensive phase DOT (n=236) | 129 (54.7) |
| Continuation phase DOT (n=236) | 125 (53.0) |
| Regular medicine delivery (n=234) | 160 (68.4) |
| Follow-up supervision | |
| Sputum sample collection (n=236) | 106 (44.9) |
| Others | |
| Providing food or transport assistances for poor patient with TB (n=230) | 104 (45.2) |
| Providing subsistence allowance or psychological support for migrant patient (n=236) | 117 (49.6) |
| Providing DOT for migrant patient with TB at their convenient time (n=235) | 203 (86.4) |
| Providing injection treatment for patient with MDR-TB (n=234) | 96 (41.0) |
| Providing supervision for newly released prison patient (n=236) | 139 (58.9) |
| Training cured patients with TB to provide peer education (n=237) | 208 (87.8) |
| Establishing platform for TB patients communication (n=237) | 137 (57.8) |
| Referring patient with TB with mental/psychological problems or alcohol/drug addiction to receive professional therapy (n=235) |
182 (77.4) |
Note: Lower delivery rate refers to a rate below 90%.
DOT, directly observed therapy; MDR-TB, multidrug-resistant tuberculosis; TB, tuberculosis; TTMS, tuberculosis treatment management service.
Factors associated with TTMSs with lower delivery rates
Multivariate logistic regression analysis showed that HCWs with high work satisfaction were less likely to have a lower delivery rate to establish patient peer supervision as needed (OR 0.182, 95% CI 0.059 to 0.562). Among both intensive and continuation phase DOT, HCWs with junior titles (OR 0.424, 95% CI 0.215 to 0.835) and high work satisfaction (OR 0.326, 95% CI 0.140 to 0.766) were less likely to have lower delivery rates. Similarly, HCWs with junior titles (OR 0.458, 95% CI 0.242 to 0.865) and high work satisfaction (OR 0.395, 95% CI 0.160 to 0.826) were more likely to deliver sputum sample collection services (table 4).
Table 4.
Multivariate logistic regression analysis of factors associated with lower delivery rate of TTMS by HCWs
| Variable | Patients’ peer supervision establish (n=235) |
Intensive phase DOT (n=236) |
Continuation phase DOT (n=236) |
Regular medicine delivery (n=234) |
Sputum sample collection (n=236) |
Injection treatment for MDR-TB patient (n=234) | Providing supervision for newly released prison patient (n=236) |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Gender | |||||||
| Female | Reference | Reference | |||||
| Male | 0.577 (0.258 to 1.270) | 0.605 (0.320 to 1.147) | |||||
| Age | |||||||
| >50 | Reference | ||||||
| 40–50 | 2.053 (0.985 to 4.279) | ||||||
| 30–39 | 2.230 (0.947 to 5.248) | ||||||
| <30 | Default | ||||||
| Professional Title | |||||||
| Non | Reference | Reference | Reference | Reference | Reference | ||
| Junior | 0.424 (0.215 to 0.835)* | 0.419 (0.228 to 0.771)* | 0.458 (0.242 to 0.865)* | 0.307 (0.159 to 0.594) | 0.681 (0.364 to 1.273) | ||
| Intermediate | 0.625 (0.233 to 1.787) | 0.860 (0.355 to 2.804) | 1.137 (0.432 to 2.995) | 0.686 (0.258 to 1.827) | 2.107 (0.829 to 5.353) | ||
| Deputy senior | 0.276 (0.021 to 3.605) | 0.415 (0.024 to 5.020) | 1.644 (0.131 to 20.581) | 0.809 (0.054 to 12.031) | 2.534 (0.179 to 35.887) | ||
| Training frequency | |||||||
| 0/6 months | Reference | Reference | Reference | ||||
| 1/6 months | 2.474 (0.566 to 10.822) | 3.533 (0.767 to 16.277) | 4.752 (0.858 to 26.335) | ||||
| 2/6 months | 2.890 (0.729 to 11.465) | 2.217 (0.534 to 9.199) | 2.568 (0.500 to 13.182) | ||||
| 3/6 months | 0.776 (0.165 to 3.660) | 0.607 (0.126 to 2.923) | 0.990 (0.162 to 6.048) | ||||
| >3/6 months | 2.307 (0.432 to 12.327) | 2.841 (0.503 to 16.-54) | 3.346 (0.508 to 22.044) | ||||
| Work satisfaction | |||||||
| Low satisfaction | Reference | Reference | Reference | Reference | Reference | ||
| Middle satisfaction | 0.354 (0.168 to 0.745)* | 0.449 (0.219 to 0.903)* | 0.584 (0.312 to 1.095) | 0.582 (0.309 to 1.094) | 0.661 (0.304 to 1.533) | ||
| High satisfaction | 0.182 (0.059 to 0.562)* | 0.326 (0.140 to 0.766)* | 0.347 (0.163 to 0.741)* | 0.375 (0.165 to 0.853) | 0.395 (0.160 to 0.826)* |
*P<0.05.
DOT, directly observed therapy; MDR-TB, multidrug-resistance tuberculosis; TTMS, tuberculosis treatment management service.
Qualitative results regarding barriers to TTMS delivery
The in-depth interviews revealed numerous barriers to TTMS delivery from the four core PRISM domains (table 5).
Table 5.
Barriers of TTMS delivery by HCWs in PHC sectors
| Core PRISM domains | Results | Quotations |
| Intervention: TTMS programme |
Patient-centred manner: Both DS-TB and MDR-TB patients stated they received TTMS from HCWs in PHC sectors by telephone. Some HCWs reported that some patients expressed antipathy to DOT and the current approach to deliver TTMS, maybe new e-health approach should be considered. |
Got telephone calls during the first 2 months, very few afterwards…I didn’t like (DOT). (DS-TB patient) Only received telephone calls from HCW in town, once per month. (MDR-TB patient) There is one MDR-TB patient…say it is annoying to call him every day (by us to deliver TTMS program). (HCW) I think that we can remind patients to take medicine via digital technologies. Although, the elders may not use phone adroitly, we find that they missed drug taking less frequently than the young patients. So, we can remind young patients through APP in mobile phone. (HCW) |
| Recipients |
Resources and incentive in PHC sectors: Majority HCWs and leaders stated that PHC sectors, particularly THCs faced insufficient human resource HCWs to deliver TTMS programme. HCWs often undertook more than 2 BPHS programmes which led to hardship to deliver standard TTMS to TB patients. And inadequate professional capability, particularly village doctors, led to patients’ distrusts and therefore hindered TTMS delivery. Many HCWs claimed that PHC sectors lacked transportation tools to facilitate home-visits especially for remote rural patients Moreover, majority HCWs and leaders reported that lack of incentive for HCWs in TTMS programme, and almost all HCWs unsatisfied with low subsidy, allowance, and salary regarding their heavy workload and infection risk. Out-of-pocket expenditure for transportations and telephone charges for TTMS delivery was also reported by HCWs. |
Too many works, it is hard to communicated well with patients…I have 2–3 days a week to give phone calls to TB patients, too tired…we often take two works by one person, the workloads are huge. (HCW) Insufficient and unstable HCWs …one HCW leave, then we need to train a new one…(CDC leader) HCWs, especially at TCHs, low quality, patients don’t trust them. (CDC leader) Lacking transportation tools for home-visit, some (patients) live in rural area, far away…need to take a long distance to visit one patient. (HCW) We face high risks of infection. There are no subsidies for us to provide manage. Funding for TTMS delivery is not separated from subsidies for the whole BPHS program. Actually, those subsidies from BPHS is not even enough for my telephone and transportation costs. (HCW) Without subsidies, the HCWs motivation and working satisfaction is low…they just to complete tasks and will not really care about the quality of TTMS. (CDC leader) |
|
Training support to HCWs in PHC sectors: Many HCWs stated that TB trainings lack of adequate professional knowledge and communication skill for TTMS delivery. Both HCWs and leaders mentioned lack of TB-specific training for HCWs. |
2–3 TB trainings each year, from CDC…combined with other (BPHS) trainings…and I think this training is not effective. (HCW) It is harder to communicate with MDR-TB patients. Sometimes they seem know more about treatment than me. Prolonged illness makes a doctor of a patient. (HCW) |
|
|
Patient’s socioeconomy: Most HCWs and leaders consistently agreed that most TB patients were old age and living with low socioeconomic status, have high risk to reject TTMS. Due to the long treatment period, the financial burden on MDR-TB patients is particularly heavy, resulting in poor adherence and TTMS difficulty. Some HCWs also stated the hardship to deliver TTMS among migrant patients since hard to reach them. |
During treatment in later period, I didn’t (take sputum test), no money, no money for transportation. (DS-TB patient) Cannot bear the financial burden… costs of follow-up examinations, CT, and medicines. (MDR-TB patient) Because TB itself is a “disease of the poor”, most TB patients have financial difficulties with bad lifestyles and poor literacy. (HC leader) Migrant patients are hard to reach…some have no stable work and often change their phone numbers…don’t like TTMS. (HCW) I told him/her the dangerousness and seriousness of MDR-TB, he/she still didn’t keep treatment, only told me: ‘no money’. (HCW) |
|
|
Patient’s health literacy: Vast majorities of HCWs stated that some patients refused to receive TTMS to manage their nonadherence behaviours due to poor health literacy and weak TB-related awareness. |
I stopped treatment because I felt good about myself. (MDR-TB patient) Some (patients) don’t prioritize their health and dislike our TTMS…they are aged and less educated…Some have very poor adherence to TB treatment. (HCW) |
|
| External environment |
Health insurance: All patients stated they still faced financial hardship even with health insurance. Most HCWs and leaders stated that the current health insurance for DS-TB patients cannot cover all medicines and examinations related to side effect, and it is more inadequate for MDR-TB patients with longer treatment, which added financial burden among poor TB patients and led to hardship for TTMS delivery. |
(After reimbursement,) medicines would cost hundreds, and the costs of CT scans can’t be reimbursed. (MDR-TB patient) The health insurance of reimbursement of TB treatment is very strict, anti-TB drugs are free, and other liver protection medicines and tests are not. (HC leader) |
|
Cross-sectional coordination: Majority HCWs and leaders reported the difficulties to conduct cross-sectional coordination for TTMS delivery, especially coordination from TB designated hospitals. One leader also stated a poor cross-sectional coordination between PHC sectors with the departments of education, public security, civil affair and finance for TTMS delivery. |
It is hard to connect with TB designated hospitals’ doctors, they are very busy. One patient stopped treatment and said it is doctors’ advice…but I cannot confirm. (HCW) The department of finance, education, civil affairs, public security, and others, … they are not highly motivated (to give us support in TTMS program). (CDC leader) |
|
|
Social stigma: TB-related social stigma was mentioned by many HCWs. Urban and young patients with more concerns of privacy issue were more likely to refuse home-visit from HCWs. |
There is one patient, it’s impossible to go to his/her home… due to privacy, he/she doesn’t like people around know they have TB. (HCW) Some TB patients, especially urban and youth patients, don’t like us to go to their home for home-visit… (They are) worried about how people around would think of them. (HCW) |
|
| Implementation and Sustainability infrastructure |
Performance assessment: All HCWs and some of the leaders stated that the performance assessment for TTMS may exist irrationality considering heavy workload. And leaders pointed out that this could lead to substandard TTMS, and hinder HCW’s working enthusiastic. |
(Performance) assessment is unreasonable, more works you do, more mistakes you make, and this is unfair. There are no rewards when you perform well…while, any negative feedbacks (such as patients’ dissatisfactions with treatment costs) would affect our performance assessment. (HCW) The indexes are quite high (considering HCW’s workload). Sometimes, the purpose becomes to complete indexes but not to really care about patients. (CDC leader) |
BPHS, basic primary health service; DOT, directly observed therapy; DS-TB, drug-sensitive tuberculosis; HCWs, healthcare workers; MDR-TB, multidrug-resistant TB; PHC, primary healthcare; TB, tuberculosis; TTMS, tuberculosis treatment management service.
Interventions
The current TTMS programme was mainly delivered via telephone calls and lacked a sufficient patient-centred approach, which led to patient antipathy to DOT. HCWs suggested that e-health approaches, including APP, would be good methods for delivering TTMSs.
Recipients
Most PHC sectors faced insufficient human resources with which to deliver TTMS programmes. Every HCWs often undertook more than two BPHS programmes. HCWs with this heavy BPHS workload had difficulty delivering standard TTMSs. On the other hand, the PHC sectors also lacked transportation tools with which to facilitate home visits, especially for remote rural patients with TB.
HCWs in the PHC sectors also faced inadequate professional capabilities, especially village doctors, which led to patient distrust and therefore hindered TTMS delivery by HCWs. On the other hand, the PHC sector also lacked sufficient incentives for HCWs in the TTMS programme, and almost all HCWs were unsatisfied with their low salaries and subsidies due to their heavy workloads and infection risk of TB. In addition, out-of-pocket expenditures for transportation and telephone charges related to TTMS delivery could further influence HCW’s working motivation, performance and attrition. Moreover, inadequate qualified training (lacked of communication skills and professional knowledge related to TTMS delivery, the training approach of TB training mixed with other BPHS programmes, and lacked of high-quality TB-specific training for HCWs) support for TB HCWs was also reported by interviewees. Therefore, the current training methods do not provide much support for HCWs’ capabilities and performance.
In terms of patient characteristics, the majority of interviewers claimed that TB is a disease of the poor and that most patients with TB were disadvantaged (of older ages, with low education, migrant workers or with financial difficulties), particularly MDR-TB patients with longer treatment periods, who had poor TB-related health literacy, and had a high risk of rejecting TTMSs. HCWs also mentioned the difficulty of delivering TTMSs to migrant patients because it was difficult to reach them.
External environment
On the one hand, inadequate health insurance coverage for medications and tests related to side effects accentuated the financial burden among poor DS-TB patients, and the health coverage was more inadequate for MDR-TB patients with longer treatment periods, which reduced their willingness to receive TTMSs. On the other hand, difficulties in cross-sectional coordination to assist TTMS delivery have been reported, especially support from TB-designated hospitals and other departments, such as departments of public security and education. Furthermore, TB-related social stigma has been reported as one of the main barriers to conducting home visits among urban and young patients who cared about privacy, and these patients were therefore more likely to refuse home visits from HCWs.
Implementation and sustainability infrastructure
The performance assessment of TB HCWs might be irrational, considering their heavy workload. One leader pointed out that the purpose of TTMS delivery could be to complete the target indicators, and therefore, lead to substandard TTMSs in patients. Moreover, inappropriate performance assessments also hinder working motivation and increase working attrition among HCWs when delivering TTMSs.
Discussion
In China, HCWs in the PHC sector are considered an important part of the integrated TB model, and these workers are responsible for TTMS delivery. This study assessed the delivery of the TTMS programme by HCWs in the PHC sector in West China. Although we found that the TTMS delivery rates in the intensive and continuation phases were higher than in a previous study in West China,15 the standard TTMS (at least 24 times TTMS during their treatment course) delivery rate was far below the required rate of >90%, according to the National TB Control Plan.6 In addition, our study showed that the number of patients with TB receiving DOT from HCW in CHCs (in urban regions) was higher than that from HCW in THCs (in rural regions). This difference might be explained by our qualitative results, as interviewed HCWs reported challenges in delivering TTMSs to remote rural patients due to patients’ poor health literacy, which has also been reported in other studies.18 30 Our study also indicated that far distances with insufficient transportation tools for HCWs were preventing TTMS delivery. In addition, our study revealed that less than half of HCWs provided services related to collecting patient sputum samples during follow-up supervision, which is much lower than the results reported in a study in Guizhou (96.56%).30 Furthermore, we found a low level of work satisfaction (22.4%) among TB HCWs, although it was higher than in a previous study (12.2%).31 Our study results indicated that HCWs with low work satisfaction were more likely to have a low delivery rate of first-time home visits, DOT and sputum sample collection services. Efforts should be made to maintain and promote HCWs’ work satisfaction to enhance TTMS delivery.
Our study revealed that the current TTMS delivery was confronted with various barriers, despite the fact that TB HCWs in PHC sectors who carried out TTMS programmes had made many achievements in West China. At the organisational level, we found that the TTMS programmes themselves had several barriers affecting the delivery of services from HCWs. On the one hand, the national TB Action Plan and nationwide TB survey in China2 9 32 mentioned cross-sectional coordination of TTMS delivery; however, we found that HCWs in the PHC sectors still lacked good coordination with other departments, such as coordination from the Department of Education to support students’ treatment management and help from the Department of Public Security to trace migrant patients’ information. In particular, HCWs from some PHC sectors faced barriers to accessing timely connections with TB HCWs from TB-designated hospitals when addressing TB patients’ side effects and treatment adherence. It is difficult to realise the participation of the whole society in terms of TB control in China so far.33 According to the Action Plan to Stop TB (2019 to 2022) in China,2 in order to coordinate cross-sectional efforts to support TB prevention and control programmes, there is an urgent need to build a multi-sectorial collaboration mechanism led by the National Health Commission.29
The second barrier that emerges at the health organisational level is the approach to TTMS delivery. We found that TTMSs were mainly delivered via telephone calls, results that are consistent with previous studies in West China,15 33 and insufficient patient-centred mannerisms could result in patient rejection of DOT and TTMSs by HCWs. A previous study in Indonesia also reported that insufficient patient-centred care was the main treatment barrier for patients with TB in high-burden settings.34 Although research has shown that home visits and DOT led to positive treatment outcomes,35 36 our study pointed out the need to provide TTMSs through an e-health approach, which was consistent with previous studies that demonstrated the effectiveness of e-health technology for promoting patient treatment adherence.37–42 It is necessary to explore internet-based case management models, including digitally supported self-management, deliver TTMSs to patients with TB living in remote mountainous areas with the help of HCWs in PHC sectors, or provide face-to-face DOT.
The third barrier at the organisational level is the human health resources for TTMSs in the PHC sectors. Other studies reported that PHC sectors, especially those in rural areas, had a limited number of HCWs with which to conduct BPHS programmes, which led to heavy workloads and a ‘shortage of hands’, as HCWs often carried out multiple assigned services.43–45 We consistently found that PHC sectors, particularly THCs, faced human resource barriers in terms of insufficient and inadequate professional capabilities to deliver the TTMS programme. On the one hand, our study showed that a heavy workload with multiple BPHS programmes could lead to difficulties in delivering standard TTMSs to patients with TB. On the other hand, we found that inadequate professional capabilities, especially village doctors, could lead to patient distrust and hence impede TTMS delivery. Simultaneously, our study revealed that PHC sectors lack adequate TB training for HCWs, particularly training related to communication and professional knowledge related to TTMS delivery, resulting in substandard TTMSs. Other studies have proved that on-the-job training is important to improve professional skills among HCWs,33 44 46 47 especially training emphasising both knowledge and practice.48 Furthermore, we found that the performance assessment of HCWs in the TTMS programme may be irrational considering their heavy workload, and this led to difficulties in delivering standard TTMSs and hindered their enthusiasm.
Our results showed that the PHC sectors lack sufficient funding for the TTMS programme, and most HCWs are unsatisfied with their low salaries, allowances or subsidies, which is consistent with other studies.30 Many studies have also indicated that the diverse issues of financial incentives combined with heavy workloads could influence HCW’s motivation and performance.44 49–52 The appropriate use of incentives for HCWs is a means of promoting health outcomes with a direct impact on the effectiveness and sustainability of a health programme, and this can also improve service delivery rates by enhancing motivation and reducing attrition.48 Notably, we found that HCWs faced out-of-pocket expenditures related to transportation and telephone charges when delivering TTMSs, which could further impact their work enthusiasm.
Our results also identified barriers at the patient level regarding TTMS delivery, including their susceptible socioeconomic characteristics (older ages, with low education, migrant status or poor financial status) and lower literacy regarding TB control. A previous nationwide TB epidemiology survey in China revealed that nearly half (48.8%) of patients with TB were aged ≥60, less educated and over 80% of patients with TB had household incomes below local levels.18 Our results indicate that poor socioeconomic characteristics and low TB-related health literacy together impede TTMS delivery. As patients with low socioeconomic features were often found to have a lower educational background, poor health literacy, and were more likely to be non-adherent, they were more likely to refuse HCWs’ supervision, which is consistent with other studies.18 53 54 In addition, we found that TTMS delivery among migrant patients was challenging for HCWs because it was difficult to reach them. Other studies also reported that migrant patients that frequently moved residences and had low socioeconomic status had relatively poorer TB-related awareness,55–57 which could hinder their TB case management. Previous studies revealed that West China had a higher proportion of rural mountain areas as well as domestic migrants than other regions in China, and TB-related awareness among rural, less educated and migrants was particularly serious.18 55 57–59
Our study also discovered that health insurance could not cover all medicines and tests related to side effects, which accentuates the financial burden among poor patients with TB and leads to barriers to TTMS delivery. To relieve barriers to TB treatment, it is crucial to address the financial burden of TB treatment among poor patients. Notwithstanding, a previous national TB epidemiology survey in China reported that although over 90% of patients with TB had medical insurance, in combination with the policy of free TB diagnosis and treatment, the proportion of patients paying out-of-pocket was still around 75.0%–84.2%.18 Several studies and reports mentioned the need to increase the reimbursement ratio and amount provided for TB treatment, to expand the scope of the currently free TB treatment policy, and to strengthen the care and assistance provided to patients with TB.2 6 36 60 In particular, there is a need to target DR-TB and impoverished patients with transportation, accommodation and nutrition allowances during TTMS delivery in order to promote TB control outcomes.
Promoting TB-related health literacy among patients and enhancing TB-related awareness among the public is urgently necessary. As revealed in our study, not only was poor TB health literacy a barrier to patients, TB-related social stigma also impeded TTMS delivery, especially in urban areas. Previous studies have suggested providing easily understandable TB health education to a particular target population (older ages, less educated, close contacts and others) with certain modes of health education.18 58 Another study indicated that a combination of mass media approaches and interpersonal communication between patients and HCWs could lead to more effective TB control.59 Similarly, the Chinese Action Plan to Stop TB called for various publicity activities with which to raise awareness of TB, including through traditional media such as television broadcasts and newspapers, as well as through the use of new media such as the WeChat app, to promote the dissemination of scientific TB knowledge and eliminate social discrimination.2
Strengths and limitations
Our study used a mixed research method combining quantitative research (questionnaire surveys) with qualitative research (semistructured, open-ended in-depth interviews) to assess TTMS programme delivery by HCWs in the PHC sectors. Perspectives from organisations and patients were included using the PRISM model to evaluate specific barriers to TTMS delivery. Three levels of the local health organisation were involved in our study, which included HCWs as front-line staff, CDC leaders as managers and health commission leaders as policy-makers. However, the current study had several limitations. First, the sample size of both the questionnaire survey and the in-depth interviews could be further expanded to enhance the representativeness of the study. Second, as we only explored the status of and barriers to TTMS delivery by HCWs in PHC sectors, well-evidenced implementation strategies that can solve the current problems successfully were not provided in this study. Further studies are required to provide evidence for the development of more comprehensive and effective TB control strategies.
Conclusion
The HCWs in the TTMS programme suggested that the government realised the importance of HCWs in the PHC sectors in promoting TB patient treatment adherence and outcomes and underscored their integration into the TB control model. We identified barriers operating at the organisational level (cross-sectional coordination, patient-centred approaches, resources and incentives, training support, reimbursement issues and performance assessments) and patient level (socioeconomic characteristics, health literacy and social stigma) to TTMS delivery by HCWs in the PHC sector. There is an urgent need to identify comprehensive measures to effectively overcome barriers to TTMS delivery and further promote TB control in southwest China.
Supplementary Material
Acknowledgments
We would like to thank the participants who responded our questionnaires. We also thank all leaders and healthcare workers in the PHCs in study places who supported this study by facilitating implementation of the field questionnaire survey and participated in our interviews. We would like to thank Editage (www.editage.cn) for English language editing.
Footnotes
Contributors: JZ, JP and YL have designed this survey, JZ, JP, GW, WX, TZ, SL and QW have collected data, JZ, JP, RZ, YC and JL have managed and analysed data, YL and DH have controlled the quality of data collection and analysis, JZ has drafted the manuscript. YL has edited the manuscript and acts as guarantor. All authors have interpreted the results, revised the report and completed the final version. The author(s) read and approved the final manuscript.
Funding: The study was funded by the National Natural Science Foundation of China (No.81773489), the Chongqing outstanding youth project (No.cstc2020jcyj-jq0035), Social Science and Technology Innovation Subject in Chongqing (No.cstc2015shmszx120070).
Disclaimer: The funders had no role in study design, data collection and analysis, interpretation of the data, writing the paper and the decision to submit the paper for publication.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Ethics approval was obtained from the Institutional Review Board of Army Medical University (Third Military Medical University), Chongqing, China (No.AF/SC-08/1.0) before starting the study.
References
- 1.World Health Organization . Global tuberculosis report 2021. Geneva: World Health Organization, 2021. [Google Scholar]
- 2.National Health Commission . Stop TB action plan (2019-2022), 2019. Available: http://www.nhc.gov.cn/jkj/s3589/201906/b30ae2842c5e4c9ea2f9d5557ad4b95f.shtml
- 3.Li T, Du X, Liu X, et al. Implementation performance of tuberculosis control in China: 2011-2020. China CDC Wkly 2021;3:252–5. 10.46234/ccdcw2021.073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization . Treatment of tuberculosis: guidelines for national programmes. 4th edn, 2010. https://www.ncbi.nlm.nih.gov/books/NBK138748/pdf/Bookshelf_NBK138748.pdf [Google Scholar]
- 5.Ministry of Health of the People’s Republic of China . National tuberculosis control programme (2011-2015). 2011. National health Commission. stop TB action plan (2019-2022), 2019. Available: http://www.gov.cn/gongbao/content/2011/content_2020914.htm
- 6.General Office of the State Council of the People’s Republic of China . The 13th five-year plan for the prevention and control of tuberculosis, 2017. Available: http://www.gov.cn/zhengce/content/2017-02/16/content_5168491.htm
- 7.National Health Commission of the People’s Republic of China . National basic public health service standard. 3rd edn, 2017. http://www.nhc.gov.cn/jws/s3578/201703/d20c37e23e1f4c7db7b8e25f34473e1b.shtml [Google Scholar]
- 8.Chen YF. Discussion on the effect of the integrated tuberculosis prevention and control model in Dongxiang County. Foreign Medical science section of medgeograpgy 2014;35. [Google Scholar]
- 9.Chen XJ, Feng ZC. Analysis of the implementation effect of the integrated tuberculosis prevention and control model in Wuhan. Medicine and society 2014;27:62–4. [Google Scholar]
- 10.XD W. The impact of community supervisors’ supervision and management visits on the rate and curative effect of non-hospital pulmonary tuberculosis patients. World Latest Medicine Information 2018;18:210. [Google Scholar]
- 11.Zhang SN, Yuan ZA, Mei J. The effectiveness of the new TB control network in Shanghai. Chin J Antituberc 2007;29:74–7. [Google Scholar]
- 12.Wang XY. Evaluation on effectiveness of the new trinity TB control network in Wujin district of Changzhou. Jiangsu J Prev Med 2013;24:18–20. [Google Scholar]
- 13.Jing GQ, Qian QW, Ding TD. The effects of tuberculosis prevention and control using the integrated mode in Bengbu. Anhui J Prev Med 2012;18:425–6. [Google Scholar]
- 14.Xie MF, Lai SF, Lian ST. Analysis on the effect of integrated tuberculosis control mode, Wuping County. Prev Med Trib 2018;24:76–8. [Google Scholar]
- 15.Pu J, Chen W, Jiang W-X, et al. Is tuberculosis patients management improved in the integrated TB control model in West China? A survey in Guizhou Province, China. Infect Dis Poverty 2019;8:55. 10.1186/s40249-019-0563-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li Y, Ehiri J, Oren E, et al. Are we doing enough to stem the tide of acquired MDR-TB in countries with high TB burden? Results of a mixed method study in Chongqing, China. PLoS One 2014;9:e88330. 10.1371/journal.pone.0088330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fetters MD, Curry LA, Creswell JW. Achieving integration in mixed methods designs-principles and practices. Health Serv Res 2013;48:2134–56. 10.1111/1475-6773.12117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang Y. The fifth national tuberculosis epidemiological sampling survey. Beijing: Military Medical Science Press, 2011. [Google Scholar]
- 19.Chongqing Statistics Bureau . Chongqing statistical yearbook 2021, 2021. Available: http://tjj.cq.gov.cn/cqtjj2021/indexch.htm
- 20.Wang Q, Li T, Du X. Analysis in the incidence of national tuberculosis reports from 2015-2019. Chinese Journal of Antituberculosis 2021;43:107–12. [Google Scholar]
- 21.Guizhou Statistics Bureau . Guizhou statistical yearbook 2021, 2021. Available: http://hgk.guizhou.gov.cn/publish/tj/2021/zk/indexch.ht
- 22.National Bureau of Statistics . China statistical year book. China Statistics Press, 2018. http://www.stats.gov.cn/tjsj/ndsj/2018/indexch.htm [Google Scholar]
- 23.Bolarinwa OA. Sample size estimation for health and social science researchers: the principles and considerations for different study designs. Niger Postgrad Med J 2020;27:67–75. 10.4103/npmj.npmj_19_20 [DOI] [PubMed] [Google Scholar]
- 24.Saunders B, Sim J, Kingstone T, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant 2018;52:1893–907. 10.1007/s11135-017-0574-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Feldstein AC, Glasgow RE. A practical, robust implementation and sustainability model (PRISM) for integrating research findings into practice. Jt Comm J Qual Patient Saf 2008;34:228–43. 10.1016/S1553-7250(08)34030-6 [DOI] [PubMed] [Google Scholar]
- 26.Liles EG, Schneider JL, Feldstein AC, et al. Implementation challenges and successes of a population-based colorectal cancer screening program: a qualitative study of stakeholder perspectives. Implement Sci 2015;10:41. 10.1186/s13012-015-0227-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schneider JL, Davis J, Kauffman TL, et al. Stakeholder perspectives on implementing a universal Lynch syndrome screening program: a qualitative study of early barriers and facilitators. Genet Med 2016;18:152–61. 10.1038/gim.2015.43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Smith J, Firth J. Qualitative data analysis: the framework approach. Nurse Res 2011;18:52–62. 10.7748/nr2011.01.18.2.52.c8284 [DOI] [PubMed] [Google Scholar]
- 29.Ward DJ, Furber C, Tierney S, et al. Using framework analysis in nursing research: a worked example. J Adv Nurs 2013;69:2423–31. 10.1111/jan.12127 [DOI] [PubMed] [Google Scholar]
- 30.He YY, Li JL, Chen W, et al. Analysis on the implementation of basic public health tuberculosis service items in Guizhou Province. Studies of Trace Elements and Health 2020;37:54–7. [Google Scholar]
- 31.Gaspar LMdaS, Braga C, Albuquerque GDMde, et al. Knowledge, attitudes and practices of community health agents regarding pulmonary tuberculosis in a capital City in northeastern Brazil. Cien Saude Colet 2019;24:3815–24. 10.1590/1413-812320182410.01722018 [DOI] [PubMed] [Google Scholar]
- 32.Zhang H, Liu X, Xu C, et al. Guiding tuberculosis control through the healthy China initiative 2019-2030. China CDC Wkly 2020;2:948–50. 10.46234/ccdcw2020.236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu GH, Deng J, Chen W. Investigation on the status of needs on community doctors for tuberculosis management in Guizhou Province. China Health Industry 2019;16:11–13. [Google Scholar]
- 34.Pradipta IS, Idrus LR, Probandari A, et al. Barriers and strategies to successful tuberculosis treatment in a high-burden tuberculosis setting: a qualitative study from the patient's perspective. BMC Public Health 2021;21:1903. 10.1186/s12889-021-12005-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xu L, Gai R, Wang X, et al. Socio-economic factors affecting the success of tuberculosis treatment in six counties of Shandong Province, China. Int J Tuberc Lung Dis 2010;14:440–6. [PubMed] [Google Scholar]
- 36.Noé A, Ribeiro RM, Anselmo R, et al. Knowledge, attitudes and practices regarding tuberculosis care among health workers in Southern Mozambique. BMC Pulm Med 2017;17:2. 10.1186/s12890-016-0344-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chongqing tuberculosis dispensary . Implementation plan of the Chongqing stop tuberculosis action (2019-2022), 2020. Available: http://www.cqtb.org/html/zcfg/20/01/1121.html [Accessed 11 Feb 2022].
- 38.Zhang H, Liu JJ. The overview and prospect of tuberculosis control in China since the founding of the peoples Republic of China. Chin J Antituberc 2019;41:913–6. [Google Scholar]
- 39.Liu X, Lewis JJ, Zhang H, et al. Effectiveness of electronic reminders to improve medication adherence in tuberculosis patients: a cluster-randomised trial. PLoS Med 2015;12:e1001876. 10.1371/journal.pmed.1001876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Alipanah N, Jarlsberg L, Miller C, et al. Adherence interventions and outcomes of tuberculosis treatment: a systematic review and meta-analysis of trials and observational studies. PLoS Med 2018;15:e1002595. 10.1371/journal.pmed.1002595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nhavoto JA, Grönlund Åke, Klein GO. Mobile health treatment support intervention for HIV and tuberculosis in Mozambique: perspectives of patients and healthcare workers. PLoS One 2017;12:e0176051. 10.1371/journal.pone.0176051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wang N, Zhang H, Zhou Y, et al. Using electronic medication monitoring to guide differential management of tuberculosis patients at the community level in China. BMC Infect Dis 2019;19:844. 10.1186/s12879-019-4521-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Huang W, Long H, Li J, et al. Delivery of public health services by community health workers (CHWs) in primary health care settings in China: a systematic review (1996–2016). Glob Health Res Policy 2018;3. 10.1186/s41256-018-0072-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tao T, Zhao Q, Jiang S, et al. Motivating health workers for the provision of directly observed treatment to TB patients in rural China: does cash incentive work? A qualitative study. Int J Health Plann Manage 2013;28:e310–24. 10.1002/hpm.2175 [DOI] [PubMed] [Google Scholar]
- 45.Liang S, Deng H, Liu S, et al. Competency building for lay health workers is an intangible force driving basic public health services in Southwest China. BMC Health Serv Res 2019;19:596. 10.1186/s12913-019-4433-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Edwards NC, Roelofs SM. Sustainability: the elusive dimension of international health projects. Can J Public Health 2006;97:45–9. 10.1007/BF03405214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Li N, Yan LL, Niu W, et al. The Effects of a Community-Based Sodium Reduction Program in Rural China - A Cluster-Randomized Trial. PLoS One 2016;11:e0166620. 10.1371/journal.pone.0166620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Organization WH. WHO guideline on health policy and system support to optimize healyhcare worker programmes. Geneva: World Health Organization, 2018. [PubMed] [Google Scholar]
- 49.Campbell C, Scott K. Retreat from Alma Ata? the who's report on task shifting to community health workers for AIDS care in poor countries. Glob Public Health 2011;6:125–38. 10.1080/17441690903334232 [DOI] [PubMed] [Google Scholar]
- 50.Jaskiewicz W, Tulenko K. Increasing community health worker productivity and effectiveness: a review of the influence of the work environment. Hum Resour Health 2012;10:1. 10.1186/1478-4491-10-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hemminki E, Long Q, Zhang W-H, et al. Impact of financial and educational interventions on maternity care: results of cluster randomized trials in rural China, CHIMACA. Matern Child Health J 2013;17:208–21. 10.1007/s10995-012-0962-6 [DOI] [PubMed] [Google Scholar]
- 52.Meng Q, Li R, Cheng G, et al. Provision and financial burden of TB services in a financially decentralized system: a case study from Shandong, China. Int J Health Plann Manage 2004;19:S45–62. 10.1002/hpm.774 [DOI] [PubMed] [Google Scholar]
- 53.Hutchison C, Khan MS, Yoong J, et al. Financial barriers and coping strategies: a qualitative study of accessing multidrug-resistant tuberculosis and tuberculosis care in Yunnan, China. BMC Public Health 2017;17:221. 10.1186/s12889-017-4089-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Onah CK, Azuogu BN, Ossai EN, et al. Addressing constraints to informal providers' involvement in tuberculosis control: a qualitative study of patent medicine dealers and tuberculosis programme managers. Glob Health Res Policy 2021;6:43. 10.1186/s41256-021-00227-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wang SN, Deng YH, Shi YY. Investigation on knowledge of tuberculosis prevention and treatment among floating population tuberculosis patients in Putuo district, Shanghai. Health Education and Promotion 2020;15:636–8. [Google Scholar]
- 56.Ma Y, Liu YH, Du J. Survey on awareness of core information of tuberculosis prevention and control knowledge in pulmonary tuberculosis patients. Chinese Anti-tuberculosis Journal 2015. [Google Scholar]
- 57.Zou X, Zhou L, Wu H, et al. The role of tuberculosis control institutes in delivering tuberculosis information to domestic migrants in China: a multi-level analysis of a nationwide cross-sectional survey. Int J Infect Dis 2019;86:94–101. 10.1016/j.ijid.2019.06.021 [DOI] [PubMed] [Google Scholar]
- 58.Chen W, Li Y, Yang H, et al. Is tuberculosis health education reaching the public in China? A cross-sectional survey in Guizhou Province. BMJ Open 2016;6:e013534. 10.1136/bmjopen-2016-013534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Arulchelvan S, Elangovan R. Effective communication approaches in tuberculosis control: health workers' perceptions and experiences. Indian J Tuberc 2017;64:318–22. 10.1016/j.ijtb.2016.11.017 [DOI] [PubMed] [Google Scholar]
- 60.Rawal LB, Kanda K, Biswas T, et al. Health problems and utilization of health services among Forcibly displaced Myanmar Nationals in Bangladesh. Glob Health Res Policy 2021;6:39. 10.1186/s41256-021-00223-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-053797supp001.pdf (211KB, pdf)
Data Availability Statement
Data are available on reasonable request.