Key Points
Question
Can the efficacy of cognitive behavioral therapy (CBT) in the treatment of major depressive disorder be enhanced by the simultaneous use of transcranial direct current stimulation (tDCS)?
Findings
In this randomized clinical trial including 148 patients, a 6-week CBT group intervention augmented by tDCS was not found to be superior to CBT plus sham-tDCS or to CBT alone. However, all patients improved significantly irrespective of group, and there were no relevant adverse effects throughout the trial.
Meaning
Results of this randomized clinical trial suggest that noninvasive brain stimulation techniques need to be thoughtfully combined with psychotherapeutic interventions and that more research is needed to optimize treatment synchronization to achieve synergies.
Abstract
Importance
Major depressive disorder (MDD) affects approximately 10% of the population globally. Approximately 20% to 30% of patients with MDD do not sufficiently respond to standard treatment. Therefore, there is a need to develop more effective treatment strategies.
Objective
To investigate whether the efficacy of cognitive behavioral therapy (CBT) for the treatment of MDD can be enhanced by concurrent transcranial direct current stimulation (tDCS).
Design, Setting, and Participants
The double-blind, placebo-controlled randomized clinical trial PsychotherapyPlus was conducted at 6 university hospitals across Germany. Enrollment took place between June 2, 2016, and March 10, 2020; follow-up was completed August 27, 2020. Adults aged 20 to 65 years with a single or recurrent depressive episode were eligible. They were either not receiving medication or were receiving a stable regimen of antidepressant medication (selective serotonin reuptake inhibitor and/or mirtazapine). A total of 148 women and men underwent randomization: 53 individuals were assigned to CBT alone (group 0), 48 to CBT plus tDCS (group 1), and 47 to CBT plus sham-tDCS (group 2).
Interventions
Participants attended a 6-week group intervention comprising 12 sessions of CBT. If assigned, tDCS was applied simultaneously. Active tDCS included stimulation with an intensity of 2 mA for 30 minutes (anode over F3, cathode over F4).
Main Outcomes and Measures
The primary outcome was the change in Montgomery-Åsberg Depression Rating Scale (MADRS) score from baseline to posttreatment in the intention-to-treat sample. Scores of 0 to 6 indicate no depression; 7 to 19, mild depression; 20 to 34, moderate depression; and 34 and higher, severe depression.
Results
A total of 148 patients (89 women, 59 men; mean [SD] age, 41.1 [13.7] years; MADRS score at baseline, 23.0 [6.4]) were randomized. Of these, 126 patients (mean [SD] age, 41.5 [14.0] years; MADRS score at baseline, 23.0 [6.3]) completed the study. In each of the intervention groups, intervention was able to reduce MADRS scores by a mean of 6.5 points (95% CI, 3.82-9.14 points). The Cohen d value was –0.90 (95% CI, –1.43 to –0.50), indicating a significant effect over time. However, there was no significant effect of group and no significant interaction of group × time, indicating the estimated additive effects were not statistically significant. There were no severe adverse events throughout the whole trial, and there were no significant differences of self-reported adverse effects during and after stimulation between groups 1 and 2.
Conclusions and Relevance
Based on MADRS score changes, this trial did not indicate superior efficacy of tDCS-enhanced CBT compared with 2 CBT control conditions. The study confirmed that concurrent group CBT and tDCS is safe and feasible. However, additional research on mechanisms of neuromodulation to complement CBT and other behavioral interventions is needed.
Trial Registration
ClinicalTrials.gov Identifier: NCT02633449
This randomized clinical trial examines the use of simultaneous cognitive behavioral therapy and transcranial direct current stimulation in the treatment of major depressive disorder in adults.
Introduction
Major depressive disorder (MDD) is a debilitating disease affecting approximately 10% of the population globally.1 Clinical management primarily comprises psychotherapy, pharmacologic treatment, and neuromodulatory interventions.2
Cognitive behavioral therapy (CBT) is effective in the treatment of MDD, with reported mean effect sizes of 0.75 and a sustainable improvement of symptoms in a 2020 systematic review and meta-analysis.3 Cognitive behavioral therapy is recommended as first-line treatment in national and international guidelines.4,5,6 However, approximately 20% to 30% of patients with MDD do not sufficiently respond to standard treatment consisting of CBT, pharmacotherapy, or the combination.7 Therefore, there is a need to develop more effective treatment strategies.8
In recent years, the concept of treatment augmentation (as previously known from pharmacologic approaches) has been transferred to psychotherapeutic interventions. The basic idea of this approach is to enhance the neuroplastic and clinical effects of the treatment by pharmacologic interventions, such as psilocybin9 or noninvasive brain stimulation techniques.10,11 Noninvasive brain stimulation comprises transcranial magnetic stimulation, which has been approved by the US Food and Drug Administration for the treatment of MDD, as well as transcranial direct current stimulation (tDCS). In tDCS, a weak direct current is applied through electrodes placed on the scalp with the aim to modify cortical excitability.12 Compared with transcranial magnetic stimulation, tDCS has the advantage of flexible usability in various settings, a better safety profile, and lower costs.
Studies in healthy populations indicate that tDCS is capable of enhancing cognitive functions involving prefrontal regions that are also relevant for CBT. Specifically, it has been shown that tDCS can improve the use of reappraisal strategies13 and cognitive control techniques14 required for emotion regulation. In addition, recent empirical findings suggest that tDCS effects are activity dependent, meaning that tDCS-induced antidepressant effects can be enhanced by concurrent cognitive activity.15 This finding implies that tDCS efficacy may be augmented by simultaneous external activation of the stimulated brain area.
We previously conducted trials in participants without depression demonstrating that tDCS can positively modulate neuronal activity in prefrontal structures central for affective and cognitive processes. These processes, such as emotion regulation,13 cognitive control,14 working memory,15 and learning,16 are centrally involved in CBT. Small pilot trials have indicated an activity-dependent, augmenting effect of tDCS for the antidepressant efficacy of cognitive control training as well as CBT-oriented online interventions in MDD.17,18 Based on these findings, we assumed that tDCS in conjunction with a CBT-activated prefrontal cortex might produce clinically relevant synergistic effects.
Thus, we conducted a multicenter, placebo-controlled randomized clinical trial (PsychotherapyPlus) comparing the efficacy of a tDCS-enhanced CBT with CBT plus sham-tDCS and CBT alone in patients with MDD. We hypothesized that tDCS-enhanced CBT would be superior to CBT plus sham-tDCS and to CBT alone.
Methods
Trial Design
This double-blind, placebo-controlled randomized clinical trial was conducted at 6 German university hospitals (Berlin, Munich, Tübingen, Leipzig, Freiburg, and Mannheim) and approved by all 6 local ethics committees. An initially planned fourth control group was not approved by the institutional review board of Charité–Universitätsmedizin Berlin; the final approved trial protocol and statistical analysis plan are available in Supplement 1. There were no relevant changes to the methods after trial commencement. Further details, including sample size calculations, are included in the eMethods in Supplement 2. Written informed consent was obtained from all participants at least 24 hours before inclusion. Participants did not receive financial compensation. This study followed the Consolidated Standards of Reporting Trials (CONSORT) reporting guideline.
Randomization and Blinding
Patients were randomly assigned in a 1:1:1 ratio to receive 1 of the 3 following treatments: CBT alone (group 0), CBT plus tDCS (group 1), or CBT plus sham-tDCS (group 2). Patients receiving active or sham-tDCS attended the same CBT group to reduce group effects. For each study site, a list of numeric 5-digit codes was generated by the manufacturer of the tDCS devices. Each code indicated either active or sham stimulation, with 1 unique code per patient. Random tDCS code assignment was conducted by a study manager not involved in treatment or Montgomery-Åsberg Depression Rating Scale (MADRS) ratings. Codes were then sent to one member of the local study team (S.A., S.V.M., G.B., N.M., L.F., and A.B.) before the first CBT session (the sequence of each session is reported in eTable 1 in Supplement 2). Psychotherapists, raters, and patients were blinded for tDCS conditions until the end of the trial.
Patients
The study included women and men between the ages of 20 and 65 years with MDD (single or recurrent episode) and a Hamilton Depression Rating Scale, 21-item version19 total score of 15 or more (cutoff score of 15 or higher fulfills the diagnostic criteria of MDD). Data on educational level and employment were collected in addition to information related to MDD. Race and ethnicity were not used as covariates because of the lack of heterogeneity. Duration of the current depressive episode was limited to 5 years, thereby including patients with a severe course of illness. Patients were tDCS naive and were either not receiving medication or were being treated with a selective serotonin reuptake inhibitor and/or mirtazapine with a stable dosage for at least 4 weeks before inclusion. The full list of inclusion and exclusion criteria is presented in the trial protocol and statistical analysis section in Supplement 1.
Cognitive Behavioral Therapy
The psychotherapeutic approach included guideline-based, well-established, and empirically validated CBT-oriented strategies20,21,22 and is described in the trial protocol (Supplement 1) and a previous publication.23 Sessions were conducted in a closed group format (maximum of 6 patients and 2 psychotherapists). The program consisted of 12 sessions lasting 100 minutes within 6 weeks. Each session started with a 10-minute introductory round. After that, stimulators were turned on simultaneously and the main CBT intervention began. Stimulation was then delivered for 30 minutes while the main CBT intervention continued until minute 80. Thus, the peak of tDCS effects24 was supposed to be reached during the second half of the main intervention and during the final round (eFigure 1 in Supplement 2). The final round lasted 20 minutes and was aimed at formulating take-home messages and transferring learning content into the daily life of patients. To implement group CBT across all study sites, a manual for psychotherapists and a handbook for patients with worksheets25 was written including detailed descriptions of each session as well as a guide for the management of difficult situations. All therapists successfully completed study-specific training (provided by S.A., E.-L.B., and J.S.). Sessions were videotaped for supervision purposes; 4 sessions of supervision (after group sessions 1, 4, 7, and 11) were mandatory and provided by a trained and certified psychotherapist and experienced supervisor (E.-L.B.).
Transcranial Direct Current Stimulation
Stimulation was applied simultaneously with group CBT as assigned. Stimulators were turned on after the introductory round, synchronized with the start of the main CBT intervention of the session, and turned off automatically after 30 minutes. Technical setup was designed in parallel with previous tDCS studies and the DepressionDC multicenter trial.26 Active tDCS included stimulation with an intensity of 2 mA, with the anode placed over F3 and the cathode over F4 according to the electroencephalogram 10-20 system. Montage was guided by a cap system used for standardized electrode positioning. Small portable devices were used (neuroConn GmbH). Active tDCS sessions comprised a 15-second ramp-in phase followed by 30-minute tDCS at 2-mA intensity and a 30-second ramp-out phase (ie, total duration of 1845 seconds). Sham tDCS sessions had the same duration but did not include a constant DC phase (ie, 15-second ramp-in to 2 mA, 30-second ramp-out, a 1755-second interval, and 15-second ramp-in to 2 mA and 30-second ramp-out in the end; total duration of 1845 seconds). During the 1755-second interval, sinus 85 Hz stimuli at 50 μA intensity were applied to control impedance to prevent unblinding of patients, psychotherapists, and other study team members. Stimulation efficacy was continuously monitored by a cloud-based approach,27 with stimulation log data being controlled by technical supervisors after each session. The percentage of technically effective stimulation sessions was calculated.
Outcomes
The primary outcome was the change in MADRS28 scores (0-6 indicates no depression; 7-19, mild depression; 20-34, moderate depression; and 34 and higher, severe depression) from baseline to postintervention (week 6) as well as an 18-week and 30-week follow-up. Secondary end points included clinical responses to treatment, defined as a greater than or equal to 50% reduction of MADRS scores, and remission rates, defined as MADRS scores less than or equal to 10. Further secondary end points were changes from baseline to postintervention regarding self-rated depression severity (Beck Depression Inventory–II [0-8 indicates no depression; 9-13, minimal depression; 14-19, mild depression; 20-28, moderate depression; and 29-63, severe depression]29), anhedonia (Snaith-Hamilton Pleasure Scale–Depression30), and health-related quality of life (Short Form-36, mental health31). There were no changes to outcomes after the trial commenced.
Tolerability and Safety
Stimulation tolerability was assessed via the Comfort Rating Questionnaire32 after each session. Neuropsychological effects were measured at baseline and postintervention using the EmoCogMeter,33 a tablet-based application to assess individual performances on memory span, working memory, cognitive speed, selective and sustained attention, and executive functioning. All adverse events had to be documented and reported within 24 hours. Annual reports with all relevant safety data were provided to an external safety monitoring board.
Statistical Analysis
Primary and secondary outcome data were analyzed by one of us (T.K.) who was blinded to study group assignment during the time of analysis. Linear mixed models were calculated for intention-to-treat (ITT) and per-protocol samples. Missing values were replaced via last observation carried forward. In both samples, postintervention MADRS scores (weeks 6, 18, and 30) were estimated by the variables group and time as well as their interaction. Logistic multilevel models were calculated to investigate whether there was an increased likelihood of a clinically relevant response or remission as a function of treatment arm. To specify efficacy, the Cohen d value was calculated for ITT and per-protocol samples. Group differences in patient characteristics were detected via 1-way analysis of variance with factor group. All post hoc tests were Bonferroni corrected; and χ2 tests were used for nonparametric group comparisons. Group differences regarding tolerability and safety were analyzed using paired t test statistics. The significance threshold was P < .05, with 2-sided testing.
Results
Patients
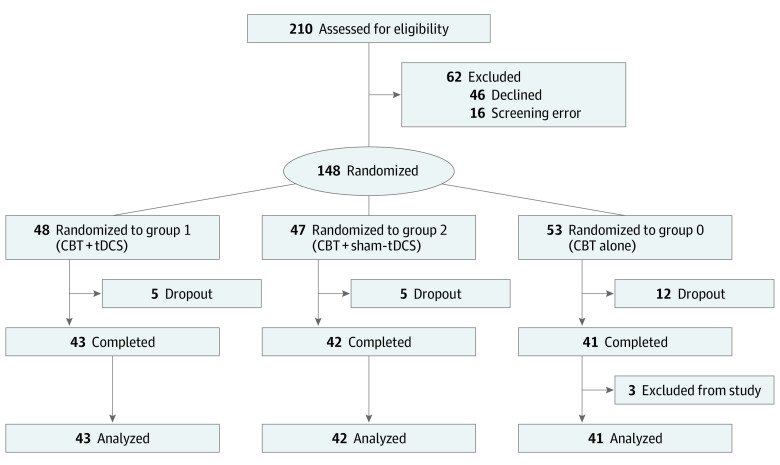
From June 2, 2016, to March 10, 2020, a total of 210 patients were assessed for eligibility at 6 university hospitals across Germany (Berlin: n = 50, Tübingen: n = 48, Munich: n = 47, Leipzig: n = 42, Freiburg: n = 15, and Mannheim: n = 8). Enrollment had to be terminated prematurely due to the start of the COVID-19 pandemic and nationwide contact restrictions affecting outpatient clinical studies. Follow-up was completed August 27, 2020. A total of 148 patients (89 women, 59 men) with a mean (SD) age of 41.1 (13.7) years and a mean (SD) baseline MADRS score of 23.0 (6.4) were randomly assigned to the 3 study arms (group 0: CBT alone, n = 53; group 1: CBT plus tDCS, n = 48; and group 2: CBT plus sham-tDCS, n = 47). A total of 126 participants (mean [SD] age, 41.5 [14.0] years; MADRS score at baseline, 23.0 [6.3]) completed the study (group 0: n = 41; group 1: n = 43; and group 2: n = 42). Three patients were excluded from the study due to a violation of study regulations (1 changed antidepressant medication during the intervention phase, 2 missed >2 CBT sessions). These patients were included in the ITT analyses (Figure 1). Patient characteristics are displayed in Table 1.
Figure 1. Study Flow Diagram.
A total of 148 patients were included in the intention-to-treat analysis. CBT indicates cognitive behavioral therapy; tDCS, transcranial direct current stimulation.
Table 1. Patient Characteristics According to Treatment Arma.
| Characteristic | Group 0: CBT alone | Group 1: CBT + tDCS | Group 2: CBT + sham-tDCS | P value |
|---|---|---|---|---|
| No. | 53 | 48 | 47 | |
| Age at inclusion, mean (SD), y | 41.5 (13.6) | 42.7 (12.7) | 39.0 (14.8) | .34 |
| Female sex, No. (%) | 36 (67.9) | 25 (52.1) | 28 (59.6) | .001 |
| Years of education, mean (SD) | 11.2 (1.3) | 11.4 (1.2) | 11.9 (1.2) | .85 |
| No. of previous episodes, mean (SD)b | 4.3 (3.9) | 3.8 (4.7) | 5.0 (6.8) | .48 |
| Duration of current episode, mean (SD), mo | 12.2 (11.9) | 21.3 (15.9) | 16.6 (15.2) | .01 |
| ATHF score, mean (SD)c | 1.5 (2.5) | 1.5 (2.7) | 2.4 (2.6) | .35 |
| SSRI and/or mirtazapine intake, No. (%) | 17 (32.1) | 16 (33.3) | 24 (51.1) | .001 |
| Baseline scores, mean (SD) | ||||
| HDRS-21d | 20.5 (4.3) | 20.3 (4.2) | 21.0 (4.3) | .16 |
| MADRSe | 23.0 (7.2) | 22.9 (6.7) | 23.1 (5.5) | .93 |
| BDI-IIf | 26.0 (10.6) | 29.0 (8.2) | 29.9 (10.9) | .22 |
| Any comorbid psychiatric disorder, No. (%)g | 26 (49.1) | 14 (29.2) | 13 (27.7) | .001 |
| Employed in the past 3 mo, No. (%) | 32 (60.4) | 31 (64.6) | 33 (70.2) | .001 |
Abbreviations: ATHF, Antidepressant Treatment History Form; BDI-II, Beck Depression Inventory–II; CBT, cognitive behavioral therapy; HDRS-21, Hamilton Depression Rating Scale, 21-items; MADRS, Montgomery-Åsberg Depression Rating Scale; SSRI, selective serotonin reuptake inhibitor; tDCS, transcranial direct current stimulation.
Total of 148 patients included in intention-to-treat analysis. Group differences were detected via 1-way analysis of variance with factor group; post hoc tests were Bonferroni corrected; and χ2 tests were used for nonparametric group comparisons. Allocation to the CBT group and study site did not influence the results (eResults 4, eFigure 3 in Supplement 2).
Previous plus current.
cThe ATHF rates each antidepressant trial during the current episode on a 5-point scale. Scores of 3 and above indicate different degrees of treatment resistance.
Cutoff score of 15 or higher fulfills the diagnostic criteria of major depressive disorder.
Scores of 0 to 6 indicate no depression; 7 to 19, mild depression; 20 to 34, moderate depression; and 34 and higher, severe depression.
Scores of 0 indicate 8 no depression; 9 to 13, minimal depression; 14 to 19, mild depression; 20 to 28, moderate depression; and 29 to 63, severe depression.
Comorbid psychiatric disorders comprised agoraphobia, specific phobia, hypochondria, and somatoform pain disorders; their distributions across groups are listed in eTable 3 in Supplement 2.
Primary Outcomes and Follow-up
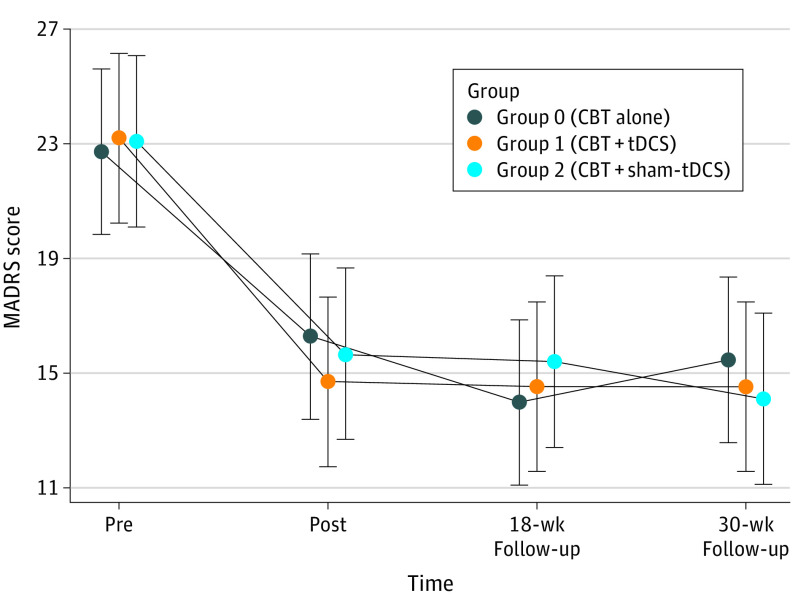
In the ITT analysis, the intervention (regardless of treatment arm) was able to reduce MADRS scores by a mean of 6.5 points (95% CI, 3.82-9.14 points) on average. The Cohen d value was –0.90 (95% CI, –1.43 to –0.50), indicating a significant effect over time. There was no significant effect of group and no significant interaction of group × time, indicating that the estimated additive effects of tDCS or sham-tDCS (groups 1 and 2) compared with CBT alone (group 0) were not statistically significant (Figure 2). In the per-protocol sample, pre-post effects were greater than those in the ITT analysis, with a MADRS score reduction of 9.0 points (95% CI, 6.28-11.62 points) and a Cohen d value of –1.37 (95% CI, –2.17 to –0.86) as expected, but neither group nor interaction effects reached statistical significance. When including follow-up MADRS scores in the analyses, effects remained unchanged (Cohen d at week 18, –1.01; week 30, –0.78).
Figure 2. Fitted Values of Montgomery-Åsberg Depression Rating Scale (MADRS).
The error bars represent 95% CIs. CBT indicates cognitive behavioral therapy; tDCS, transcranial direct current stimulation.
Secondary Outcomes
In the ITT sample, 40 patients (27.0%) achieved remission and 45 patients (30.4%, including those who achieved remission) showed a treatment response. A logistic multilevel model showed no increased likelihood of remission or response as a function of group. There were no significant effects of group and no significant interactions of group × time regarding all secondary outcomes (Beck Depression Inventory-II, Snaith-Hamilton Pleasure Scale–Depression, and Short Form-36, mental health), although patients significantly improved irrespective of group (Table 2).
Table 2. Primary, Secondary, and Exploratory Outcomes According to Treatment Arma.
| Outcome | Mean (SD) | ||
|---|---|---|---|
| Group 0: CBT alone | Group 1: CBT + tDCS | Group 2: CBT + sham-tDCS | |
| No. | 41 | 43 | 42 |
| Remission, No. (%) | 14 (34.1) | 15 (34.9) | 11 (26.2) |
| Response, including remission, No. (%) | 17 (41.5) | 15 (34.9) | 13 (31.0) |
| MADRSb | |||
| Pre | 23.0 (7.2) | 22.9 (6.7) | 23.1 (5.5) |
| Postc | 16.6 (8.8) | 14.4 (6.9) | 15.7 (7.3) |
| Week | |||
| 18c | 14.2 (8.3) | 14.2 (8.0) | 15.4 (8.6) |
| 30c | 15.9 (9.3) | 14.2 (9.4) | 14.1 (8.6) |
| BDI-IId | |||
| Pre | 6.0 (10.6) | 29.0 (8.2) | 29.9 (10.9) |
| Postc | 17.5 (9.9) | 18.3 (10.6) | 18.4 (10.4) |
| Week | |||
| 18c | 14.5 (8.0) | 15.6 (9.9) | 17.7 (12.7) |
| 30c | 15.6 (9.7) | 16.3 (13.8) | 16.2 (13.9) |
| SHAPS-De | |||
| Pre | 26.0 (7.0) | 23.9 (6.8) | 24.7 (8.3) |
| Post | 26.1 (9.1) | 25.5 (8.1) | 28.4 (8.3) |
| Week | |||
| 18c | 29.5 (7.0) | 28.8 (6.4) | 28.9 (8.2) |
| 30c | 30.2 (6.6) | 30.2 (8.2) | 29.1 (8.4) |
| SF-36 mental healthf | |||
| Pre | 15.3 (4.5) | 14.6 (3.2) | 14.3 (4.0) |
| Postc | 17.5 (4.8) | 16.6 (4.5) | 16.5 (4.1) |
| Week | |||
| 18c | 17.6 (4.1) | 17.1 (4.0) | 16.5 (4.3) |
| 30c | 19.1 (4.4) | 18.3 (6.0) | 18.6 (4.7) |
| Memory span | |||
| Pre | 7.4 (1.1) | 7.1 (1.3) | 7.2 (1.2) |
| Post | 7.4 (1.0) | 7.1 (1.5) | 7.4 (1.1) |
| Working memory accuracy | |||
| Pre | 52.8 (38.6) | 49.9 (49.6) | 53.4 (36.3) |
| Postc | 69.3 (26.7) | 69.4 (37.5) | 65.3 (41.0) |
| Cognitive speed (correct items) | |||
| Pre | 49.3 (16.2) | 51.2 (13.1) | 50.5 (17.0) |
| Postc | 54.1 (15.7) | 55.8 (14.7) | 55.1 (15.2) |
| Selective attention accuracy | |||
| Pre | 89.3 (8.8) | 85.1 (26.9) | 88.9 (13.0) |
| Post | 87.6 (23.1) | 88.0 (23.0) | 95.2 (5.5) |
| Sustained attention accuracy | |||
| Pre | 27.1 (48.5) | 22.3 (62.5) | 28.5 (17.6) |
| Post | 27.0 (59.3) | 20.0 (59.7) | 31.4 (68.5) |
| Executive function | |||
| Pre | 70.0 (21.7) | 76.6 (12.9) | 73.7 (16.0) |
| Post | 74.4 (16.2) | 71.8 (16.0) | 67.9 (18.3) |
Abbreviations: BDI-II, Beck Depression Inventory–II; CBT, cognitive behavioral therapy; MADRS, Montgomery-Åsberg Depression Rating Scale; SF-36, Short Form-36, mental health; SHAPS-D, Snaith-Hamilton Pleasure Scale–Depression; tDCS, transcranial direct current stimulation.
Total of 148 patients included in intention-to-treat analysis; 126 patients completed the study.
Scores of 0 to 6 indicate no depression; 7 to 19, mild depression; 20 to 34, moderate depression; and 34 and higher, severe depression.
Significant difference between the score following the intervention (post) compared with the baseline (pre) score in the intention-to-treat sample irrespective of treatment arm (all differences P < .001; Bonferroni correction applied). Additional exploratory pre-post data are reported in eTable 4 in Supplement 2.
Scores of 0 to 8 indicate no depression; 9 to 13, minimal depression; 14 to 19, mild depression; 20 to 28, moderate depression; and 29 to 63, severe depression.
eThe SHAPS-D consists of 14 4-point Likert scale items measuring the ability to experience pleasure. Higher scores indicate less anhedonia (ie, more experienced pleasure). There are no validated cutoff scores.
fThe SF-36 is a 36-item self-report measure of health-related quality of life independent of psychiatric disorders. Higher scores indicate better health. There are no validated cutoff scores.
Blinding Efficacy
Patients receiving stimulation (groups 1 and 2) were not able to correctly guess their assigned treatment arm regarding active vs sham intervention. The percentage of correct assignments was below chance (39%), indicating that blinding was effective.
Quality of Stimulation
A total of 93.6% of stimulation sessions were evaluated as technically appropriate. Patients who completed the intervention phase underwent a mean (SD) of 10.7 (1.1) complete and technically appropriate tDCS sessions. Of 1052 administered stimulations, 34 (3.2%) were canceled automatically because of high voltage or high impedance, and 33 (3.1%) stimulations ended early due to technical problems or operating errors. These events usually occurred silently to ensure blinding. An acoustic signal occurred only at the end of stimulation (both in active and sham conditions) or when a stimulation was manually canceled by the user. Manual cancellation happened 32 times (3.0%), typically at the beginning when patients wanted to start the stimulation and pressed the button twice instead of once. In these cases, stimulators could be restarted to count as appropriate within the same session.
Tolerability and Safety
There were no significant differences of self-reported adverse effects during and after stimulation between groups 1 and 2 (eResults 1 in Supplement 2). There were no severe adverse events throughout the whole trial (eg, no new-onset mania or hypomania, no attempted or completed suicides, and no hospitalizations). A total of 25 adverse events affecting 16.2% of all randomized patients were reported (Table 3). Five events (20%) were considered potentially related or related (active tDCS: 3 events [local pain at stimulation site], sham-tDCS: 2 events [local pain at stimulation site and dizziness]), but all were limited to previously described adverse reactions typical for tDCS.34 Neuropsychological results showed a significant improvement with regard to working memory accuracy and cognitive speed across the whole sample (P<.001), and there were neither significant effects of group nor significant interactions of group × time in any of the tested domains (Table 2).
Table 3. Full List of 25 Reported Adverse Events According to Treatment Arm.
| Type of adverse event | No. | Group 0: CBT alone | Group 1: CBT + tDCS | Group 2: CBT + sham-tDCS |
|---|---|---|---|---|
| Influenza infection | 9 | 2 | 5 | 2 |
| Gastroenteritis | 4 | 0 | 1 | 3 |
| Functional diarrhea | 2 | 2 | 0 | 0 |
| Headache | 2 | 2 | 0 | 0 |
| Discomfort | 1 | 0 | 0 | 1 |
| Sleep problems | 1 | 0 | 1 | 0 |
| Local pain at stimulation sitea | 4 | 0 | 3 | 1 |
| Dizzinessa | 1 | 0 | 0 | 1 |
| Skin reddeningb | 0 | 0 | 0 | 0 |
| Fracture of wrist due to a bike accident | 1 | 0 | 0 | 1 |
Abbreviations: CBT, cognitive behavioral therapy; tDCS, transcranial direct current stimulation.
Five events were classified related or potentially related to the intervention because of a temporal correlation to the intervention; all others were classified as unrelated.
Skin reddening was assessed when devices were removed by members of the study team, which took place after the CBT session (ie, 60 minutes after tDCS ended). This process was done to prevent unblinding by different levels of skin reddening after active vs sham stimulation. Therefore, no cases of skin reddening could be observed.
Discussion
This double-blind, placebo-controlled randomized clinical trial compared a 6-week treatment of tDCS-augmented CBT with 2 CBT control conditions (with and without sham-tDCS) for MDD and found no significant group differences in terms of antidepressant efficacy. However, the intervention, regardless of treatment arm, was able to significantly reduce depressive symptoms with effects maintained over time. Analyses of secondary outcomes indicated that response and remission rates were similar, neuropsychological performance improved in 2 domains, and no serious adverse events occurred across all 3 trial groups.
Irrespective of group assignment, patients showed significantly lower depression scores postintervention compared with baseline. We provide evidence that the simultaneous combination of group CBT and tDCS is well tolerated and can be applied safely with no relevant neuropsychological or clinical adverse effects. Albeit no clinical differences were detected between the tDCS-augmented CBT and the 2 control conditions, the results of the present study are relevant for future studies aiming at generating synergies between neuromodulatory and psychotherapeutic interventions.
There are at least 3 plausible reasons why the tDCS-augmented CBT did not show superior efficacy. First, we had translated initial findings of tDCS-induced cognitive control enhancement into a more complex CBT setting. We expected the enhancement to be transferable to CBT settings with cognitive control being a key mechanism involved in many processes of cognitive change in a CBT-based treatment of depressive symptoms. However, in the PsychotherapyPlus trial, stimulation might have taken place in various, maybe not sufficiently standardized, learning settings underlying strong interindividual temporal dynamics. Especially, the group setting with difficult-to-control interactions between study participants and potentially imbalanced learning processes across individuals might have significantly increased variability of individual learning conditions. Thus, it seems possible that state dependency and thereby proper synchronization between stimulation and psychotherapeutic intervention could not sufficiently be achieved.35,36 In addition, group CBT sessions focused more on interpersonal than cognitive learning. Therefore, synchronizing tDCS with existing psychotherapeutic approaches that directly address cognitive control, such as techniques from metacognitive therapy,37 or with explicit cognitive control training38 could be a promising approach for future investigations. Also, augmenting psychotherapy with tDCS in 1:1 sessions might be more effective with patients’ individual cognitive processes being more present (and thus more guidable) to therapists than in group settings.
Second, the present study indicates that outcome parameters need to be selected more carefully in future investigations. If tDCS-augmented CBT affects cognitive control mechanisms, clinically relevant effects might be overseen if rather standard depression measurements, such as the MADRS total score, are chosen. Looking at the improvement of symptom clusters (eg, core depressive, sleep, or anxiety) in networks rather than the change of total scores might allow for a more differential view.39 It might also be beneficial to select primary outcomes closer to the targeted neurobiological mechanisms of cognitive control. This narrowing of the outcomes would at the same time allow for more sophisticated study designs in transdiagnostic approaches.
Third, the chosen stimulation parameter might not have been optimal. Stimulating after the introduction phase at the beginning of the main CBT intervention might already have had a difficult-to-control effect on the outcome. In addition, recent data suggest that a stimulation duration longer than 25 minutes might lead to a reversal of tDCS effects.40 Besides stimulation point and duration, intensity might also not have been optimal. However, stimulation intensities are still a matter of debate. First, comprehensive findings for tDCS with heterogeneous effects for 1- vs 2-mA intensity on motor cortex excitability as measured with motor-evoked potential amplitudes39,40,41 suggest nonlinear intensity response relationships. In contrast, functional magnetic resonance imaging findings show maximum poststimulation effects of 2-mA intensity for anodal primary motor cortex tDCS on cerebral blood flow in the primary motor cortex.42 Second, approaches combining tDCS and cognitive training on nonmotor functions may follow their own associations between the intervention and response, and optimal stimulation intensities have not yet been established.13,43,44 Third, recent evidence from some authors of the present study applying computational modeling of electric fields support the notion that clinical groups (eg, patients with MDD) show lower tDCS-induced electric field intensities compared with healthy controls.45 This finding means that patients with MDD may need a higher stimulation intensity to reach a comparable dosage at cortex level. However, when the stimulation protocol for the study was developed, our selection was primarily guided by the findings of Brunoni and colleagues,46 who observed antidepressant effects associated with a 2-mA intensity in a large clinical sample, which were later confirmed in what was, to our knowledge, the largest randomized clinical trial investigating tDCS efficacy in MDD to date.
Strengths and Limitations
There are strengths of this study. The inclusion of 2 active control groups allowed a more precise estimation of augmenting effects of tDCS with detection of placebo effects being often reported in neuromodulation trials.47 The lacking difference between CBT plus sham-tDCS and CBT alone suggests that sham-tDCS as such did not enhance the effect on the psychotherapeutic intervention. Another strength is the demonstration of feasibility of a cloud-based monitoring of technical stimulation parameters,27 ensuring a centralized, continuous, and remote control of stimulation quality.
The trial has limitations. First is the lack of a real placebo group (ie, a control group for CBT as initially planned), limiting conclusions about the effect of the behavioral intervention. Also, we cannot fully rule out that sham tDCS has had biological effects.47 This limitation has been discussed in the context of negative findings from a multicenter trial48 in which sham-tDCS was applied with a steady low current of 0.034 mA—current that may have actually induced biological effects. In our sham condition, however, there was no direct current between the brief ramp-in and ramp-out phases that were required for mimicking the somatosensory artifacts of active tDCS. Only steady, single low-voltage pulses were used to measure impedance to ensure blinding. Still, we cannot fully exclude biological effects of this minimal stimulation. Another shortcoming is that blinding for tDCS conditions could be performed only in groups 1 and 2. Also, endophenotypes potentially influencing tDCS efficacy (eg, prefrontal anatomy and reactivity characteristics or differences in physiologic processing49) as well as dosing effects (eg, differences between 1 vs 2 mA and different frequencies of CBT) could not be considered. In addition, the group setting might not have been ideal for investigating augmentative effects of tDCS. A higher degree of standardizability, such as with a digitally delivered intervention focusing on cognitive functions in an individual setting, might have been superior. Furthermore, the study might be underpowered since the planned sample size could not be reached because of contact restrictions during the first phase of the COVID-19 pandemic (groups comprising 53, 48, and 47 individuals instead of 64, 64, and 6423). This reduced sample size also limits statistical options of analyzing potential interactions of patient characteristics, baseline group differences, and treatment efficacy. However, a post hoc simulation showed that an additional reduction of at least 6 points on the MADRS scale resulting from tDCS stimulation could have been detected in our sample (eResults 2, eFigure 2 in Supplement 2). Differences in allocation of patients receiving antidepressant medication or experiencing comorbid somatoform pain disorder (eResults 3, eTable 2 in Supplement 2) could affect treatment outcomes. Future studies should consider these variables as prognostic factors and examine their potential interaction with tDCS stimulation.
Conclusions
This trial demonstrated that a 6-week regimen of tDCS-augmented CBT was effective and sustainable, well tolerated, and feasible in group settings with stimulation quality being monitored remotely, paving the way for future resource-preserving treatment scenarios outside classical inpatient and outpatient settings (eg, digitally delivered interventions). However, the combined treatment was not superior to CBT alone.
Trial Protocol and Statistical Analysis Plan
eMethods. Sample Size Calculations and Effect Sizes
eTable 1. Sequence of a Treatment Session
eFigure 1. Synchronization of CBT and tDCS
eResults 1. Self-reported Tolerability of Stimulation
eResults 2. Post Hoc Power Simulation Results
eFigure 2. Results of the Post Hoc Simulation Study
eResults 3. Results of Exploratory Sensitivity Analyses
eTable 2. Results of Sensitivity Analyses
eTable 3. Comorbid Disorders in the ITT Sample
eResults 4. Exploratory Model (Group CBT Effects Versus Individual tDCS Effects)
eFigure 3. Random Effects of CBT Group on Baseline MADRS Scores (Intercept) and Symptom Reduction (Time)
eTable 4. Descriptive Analysis of Further Variables Assessed
eReferences
Data Sharing Statement
References
- 1.Malhi GS, Mann JJ. Depression. Lancet. 2018;392(10161):2299-2312. doi: 10.1016/S0140-6736(18)31948-2 [DOI] [PubMed] [Google Scholar]
- 2.Otte C, Gold SM, Penninx BW, et al. Major depressive disorder. Nat Rev Dis Primers. 2016;2:16065. doi: 10.1038/nrdp.2016.65 [DOI] [PubMed] [Google Scholar]
- 3.Cuijpers P, Karyotaki E, Eckshtain D, et al. Psychotherapy for depression across different age groups: a systematic review and meta-analysis. JAMA Psychiatry. 2020;77(7):694-702. doi: 10.1001/jamapsychiatry.2020.0164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Psychological Association . Clinical practice guideline for the treatment of depression across three age cohorts. 2022. Accessed March 14, 2022. https://www.apa.org/depression-guideline
- 5.National Institute for Health and Care Excellence . Depression. Accessed March 14, 2022. https://www.nice.org.uk/guidance/conditions-and-diseases/mental-health-and-behavioural-conditions/depression
- 6.Nationale Versorgungs Leitlinien . Grundlagen. Accessed March 14, 2022. https://www.leitlinien.de/themen/depression/2-auflage
- 7.Rush AJ, Trivedi MH, Wisniewski SR, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry. 2006;163(11):1905-1917. doi: 10.1176/ajp.2006.163.11.1905 [DOI] [PubMed] [Google Scholar]
- 8.Cuijpers P, Karyotaki E, Ciharova M, Miguel C, Noma H, Furukawa TA. The effects of psychotherapies for depression on response, remission, reliable change, and deterioration: a meta-analysis. Acta Psychiatr Scand. 2021;144(3):288-299. doi: 10.1111/acps.13335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carhart-Harris RL, Bolstridge M, Rucker J, et al. Psilocybin with psychological support for treatment-resistant depression: an open-label feasibility study. Lancet Psychiatry. 2016;3(7):619-627. doi: 10.1016/S2215-0366(16)30065-7 [DOI] [PubMed] [Google Scholar]
- 10.Bajbouj M, Padberg F. A perfect match: noninvasive brain stimulation and psychotherapy. Eur Arch Psychiatry Clin Neurosci. 2014;264(suppl 1):S27-S33. doi: 10.1007/s00406-014-0540-6 [DOI] [PubMed] [Google Scholar]
- 11.Sathappan AV, Luber BM, Lisanby SH. The dynamic duo: combining noninvasive brain stimulation with cognitive interventions. Prog Neuropsychopharmacol Biol Psychiatry. 2019;89:347-360. doi: 10.1016/j.pnpbp.2018.10.006 [DOI] [PubMed] [Google Scholar]
- 12.Nitsche MA, Boggio PS, Fregni F, Pascual-Leone A. Treatment of depression with transcranial direct current stimulation (tDCS): a review. Exp Neurol. 2009;219(1):14-19. doi: 10.1016/j.expneurol.2009.03.038 [DOI] [PubMed] [Google Scholar]
- 13.Feeser M, Prehn K, Kazzer P, Mungee A, Bajbouj M. Transcranial direct current stimulation enhances cognitive control during emotion regulation. Brain Stimul. 2014;7(1):105-112. doi: 10.1016/j.brs.2013.08.006 [DOI] [PubMed] [Google Scholar]
- 14.Wolkenstein L, Plewnia C. Amelioration of cognitive control in depression by transcranial direct current stimulation. Biol Psychiatry. 2013;73(7):646-651. doi: 10.1016/j.biopsych.2012.10.010 [DOI] [PubMed] [Google Scholar]
- 15.Wischnewski M, Mantell KE, Opitz A. Identifying regions in prefrontal cortex related to working memory improvement: a novel meta-analytic method using electric field modeling. Neurosci Biobehav Rev. 2021;130:147-161. doi: 10.1016/j.neubiorev.2021.08.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Begemann MJ, Brand BA, Ćurčić-Blake B, Aleman A, Sommer IE. Efficacy of non-invasive brain stimulation on cognitive functioning in brain disorders: a meta-analysis. Psychol Med. 2020;50(15):2465-2486. doi: 10.1017/S0033291720003670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Segrave RA, Arnold S, Hoy K, Fitzgerald PB. Concurrent cognitive control training augments the antidepressant efficacy of tDCS: a pilot study. Brain Stimul. 2014;7(2):325-331. doi: 10.1016/j.brs.2013.12.008 [DOI] [PubMed] [Google Scholar]
- 18.Welch ES, Weigand A, Hooker JE, et al. Feasibility of computerized cognitive-behavioral therapy combined with bifrontal transcranial direct current stimulation for treatment of major depression. Neuromodulation. 2019;22(8):898-903. doi: 10.1111/ner.12807 [DOI] [PubMed] [Google Scholar]
- 19.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56-62. doi: 10.1136/jnnp.23.1.56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Beck AT, Rush J, Shaw B, Emery G. Cognitive Therapy of Depression. Guilford Press; 1979. [Google Scholar]
- 21.Hautzinger M. Kognitive Verhaltenstherapie bei Depression. Beltz; 2013. [Google Scholar]
- 22.McCullough JP Jr. Treatment for chronic depression using Cognitive Behavioral Analysis System of Psychotherapy (CBASP). J Clin Psychol. 2003;59(8):833-846. doi: 10.1002/jclp.10176 [DOI] [PubMed] [Google Scholar]
- 23.Bajbouj M, Aust S, Spies J, et al. PsychotherapyPlus: augmentation of cognitive behavioral therapy (CBT) with prefrontal transcranial direct current stimulation (tDCS) in major depressive disorder-study design and methodology of a multicenter double-blind randomized placebo-controlled trial. Eur Arch Psychiatry Clin Neurosci. 2018;268(8):797-808. doi: 10.1007/s00406-017-0859-x [DOI] [PubMed] [Google Scholar]
- 24.Nitsche MA, Seeber A, Frommann K, et al. Modulating parameters of excitability during and after transcranial direct current stimulation of the human motor cortex. J Physiol. 2005;568(pt 1):291-303. doi: 10.1113/jphysiol.2005.092429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Spies J, Bollmann S, Aust S, et al. KVTplus Gruppentherapie: Manual für Studientherapeut:innen der Studie PsychotherapiePlus. Accessed March 7, 2022. https://refubium.fu-berlin.de/handle/fub188/33912
- 26.Padberg F, Kumpf U, Mansmann U, et al. Prefrontal transcranial direct current stimulation (tDCS) as treatment for major depression: study design and methodology of a multicenter triple blind randomized placebo controlled trial (DepressionDC). Eur Arch Psychiatry Clin Neurosci. 2017;267(8):751-766. doi: 10.1007/s00406-017-0769-y [DOI] [PubMed] [Google Scholar]
- 27.Kumpf U, Stadler M, Plewnia C, et al. Transcranial direct current stimulation (tDCS) for major depression—interim analysis of cloud supervised technical data from the DepressionDC trial. Brain Stimul. 2021;14(5):1234-1237. doi: 10.1016/j.brs.2021.08.005 [DOI] [PubMed] [Google Scholar]
- 28.Montgomery SA, Åsberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382-389. doi: 10.1192/bjp.134.4.382 [DOI] [PubMed] [Google Scholar]
- 29.Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory–II. Psychological Corporation; 1996. [Google Scholar]
- 30.Snaith P. Anhedonia: a neglected symptom of psychopathology. Psychol Med. 1993;23(4):957-966. doi: 10.1017/S0033291700026428 [DOI] [PubMed] [Google Scholar]
- 31.Hooker SA. SF-36. In: Gellman MD, Turner JR, eds. Encyclopedia of Behavioral Medicine. Springer; 2013. doi: 10.1007/978-1-4419-1005-9_1597 [DOI] [Google Scholar]
- 32.Palm U, Feichtner KB, Hasan A, et al. The role of contact media at the skin-electrode interface during transcranial direct current stimulation (tDCS). Brain Stimul. 2014;7(5):762-764. doi: 10.1016/j.brs.2014.06.006 [DOI] [PubMed] [Google Scholar]
- 33.Fuge P, Grimm S, Weigand A, et al. Assessment of age-related changes in cognitive functions using EmoCogMeter, a novel tablet-computer based approach. J Vis Exp. 2014;84(84):e50942. doi: 10.3791/50942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brunoni AR, Amadera J, Berbel B, Volz MS, Rizzerio BG, Fregni F. A systematic review on reporting and assessment of adverse effects associated with transcranial direct current stimulation. Int J Neuropsychopharmacol. 2011;14(8):1133-1145. doi: 10.1017/S1461145710001690 [DOI] [PubMed] [Google Scholar]
- 35.Weigand A, Richtermeier A, Feeser M, et al. State-dependent effects of prefrontal repetitive transcranial magnetic stimulation on emotional working memory. Brain Stimul. 2013;6(6):905-912. doi: 10.1016/j.brs.2013.06.004 [DOI] [PubMed] [Google Scholar]
- 36.Bortoletto M, Pellicciari MC, Rodella C, Miniussi C. The interaction with task-induced activity is more important than polarization: a tDCS study. Brain Stimul. 2015;8(2):269-276. doi: 10.1016/j.brs.2014.11.006 [DOI] [PubMed] [Google Scholar]
- 37.Callesen P, Reeves D, Heal C, Wells A. Metacognitive therapy versus cognitive behaviour therapy in adults with major depression: a parallel single-blind randomised trial. Sci Rep. 2020;10(1):7878. doi: 10.1038/s41598-020-64577-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sommer A, Plewnia C. Depression treatment by tDCS-enhanced cognitive control training: a test of two stimulation intensities. Brain Stimul. 2021;14(4):987-989. doi: 10.1016/j.brs.2021.06.004 [DOI] [PubMed] [Google Scholar]
- 39.Siddiqi SH, Taylor SF, Cooke D, Pascual-Leone A, George MS, Fox MD. Distinct symptom-specific treatment targets for circuit-based neuromodulation. Am J Psychiatry. 2020;177(5):435-446. doi: 10.1176/appi.ajp.2019.19090915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hassanzahraee M, Nitsche MA, Zoghi M, Jaberzadeh S. Determination of anodal tDCS duration threshold for reversal of corticospinal excitability: an investigation for induction of counter-regulatory mechanisms. Brain Stimul. 2020;13(3):832-839. doi: 10.1016/j.brs.2020.02.027 [DOI] [PubMed] [Google Scholar]
- 41.Batsikadze G, Moliadze V, Paulus W, Kuo MF, Nitsche MA. Partially non-linear stimulation intensity-dependent effects of direct current stimulation on motor cortex excitability in humans. J Physiol. 2013;591(7):1987-2000. doi: 10.1113/jphysiol.2012.249730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jamil A, Batsikadze G, Kuo HI, et al. Current intensity- and polarity-specific online and aftereffects of transcranial direct current stimulation: an fMRI study. Hum Brain Mapp. 2020;41(6):1644-1666. doi: 10.1002/hbm.24901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vanderhasselt MA, De Raedt R, Namur V, et al. Transcranial electric stimulation and neurocognitive training in clinically depressed patients: a pilot study of the effects on rumination. Prog Neuropsychopharmacol Biol Psychiatry. 2015;57:93-99. doi: 10.1016/j.pnpbp.2014.09.015 [DOI] [PubMed] [Google Scholar]
- 44.Weller S, Nitsche MA, Plewnia C. Enhancing cognitive control training with transcranial direct current stimulation: a systematic parameter study. Brain Stimul. 2020;13(5):1358-1369. doi: 10.1016/j.brs.2020.07.006 [DOI] [PubMed] [Google Scholar]
- 45.Mizutani-Tiebel YS, Takahashi T, Karali E, et al. Reduced fields show up in schizophrenia and major depression—a prefrontal tDCS simulation study. Clin Neurophysiol. 2020;131(3):e121-e122. doi: 10.1016/j.clinph.2019.12.300 [DOI] [Google Scholar]
- 46.Brunoni AR, Valiengo L, Baccaro A, et al. The sertraline vs electrical current therapy for treating depression clinical study: results from a factorial, randomized, controlled trial. JAMA Psychiatry. 2013;70(4):383-391. doi: 10.1001/2013.jamapsychiatry.32 [DOI] [PubMed] [Google Scholar]
- 47.Fonteneau C, Mondino M, Arns M, et al. Sham tDCS: a hidden source of variability? reflections for further blinded, controlled trials. Brain Stimul. 2019;12(3):668-673. doi: 10.1016/j.brs.2018.12.977 [DOI] [PubMed] [Google Scholar]
- 48.Loo CK, Husain MM, McDonald WM, et al. ; International Consortium of Research in tDCS (ICRT) . International randomized-controlled trial of transcranial direct current stimulation in depression. Brain Stimul. 2018;11(1):125-133. doi: 10.1016/j.brs.2017.10.011 [DOI] [PubMed] [Google Scholar]
- 49.Dedoncker J, Baeken C, De Raedt R, Vanderhasselt MA. Combined transcranial direct current stimulation and psychological interventions: state of the art and promising perspectives for clinical psychology. Biol Psychol. 2021;158:107991. doi: 10.1016/j.biopsycho.2020.107991 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol and Statistical Analysis Plan
eMethods. Sample Size Calculations and Effect Sizes
eTable 1. Sequence of a Treatment Session
eFigure 1. Synchronization of CBT and tDCS
eResults 1. Self-reported Tolerability of Stimulation
eResults 2. Post Hoc Power Simulation Results
eFigure 2. Results of the Post Hoc Simulation Study
eResults 3. Results of Exploratory Sensitivity Analyses
eTable 2. Results of Sensitivity Analyses
eTable 3. Comorbid Disorders in the ITT Sample
eResults 4. Exploratory Model (Group CBT Effects Versus Individual tDCS Effects)
eFigure 3. Random Effects of CBT Group on Baseline MADRS Scores (Intercept) and Symptom Reduction (Time)
eTable 4. Descriptive Analysis of Further Variables Assessed
eReferences
Data Sharing Statement