Abstract
Background:
There are few studies examining the usage and utility of patient portals among seriously ill and end-of-life populations and their caregivers.
Objective:
The aim of this study was to describe portal user characteristics among patients and their caregivers (proxy login) at two time points: (1) the 12 months following an electronic medical record flag for serious illness and (2) during the last 12 months of life.
Methods:
A retrospective cohort analysis of Kaiser Permanente Colorado (KPCO) patients with serious illness, as defined by Kaiser Permanente's prognostic algorithm, and their proxy caregivers was performed for the two time periods. Use was characterized as (1) the discrete number of days the portal was used and (2) the number of days that portal features were accessed. Differences in use by user characteristics were assessed.
Results:
Patients flagged for serious illness (N = 6129) were 70.4 ± 14.2 years of age, and used the portal on average 50.4 days. Patients (N = 6517) in the last year of life were 76.7 ± 13.7 years of age and used the portal on average 43 days. Caregiver proxy use of the portal was low in both cohorts. Patients who were older, female, non-White, and healthier were less likely to use the portal.
Conclusions:
In comparison with overall KPCO portal use and recent patient portal studies examining use patterns, patient portal use was high among patients flagged with serious illness and nearing the end of life. However, because use was associated with age, gender, and race, addressing barriers to portal adoption among underserved populations and caregiver proxies is key to better leveraging patient portal systems for palliative and end-of-life care.
Keywords: digital health, electronic medical record, patient portal utilization, personal health record
Introduction
Nearly 2 million people die each year from serious chronic illness,1 a health condition with high mortality risk that negatively impacts a person's daily functioning and quality of life or excessively strains their caregivers.2 Patients with serious illness experience significant physical, spiritual, and psychological symptom burden and progressive dependence on their caregivers and family.3 Palliative care is an interprofessional and patient–family-centered approach for addressing the physical, psychological, emotional, and spiritual suffering for patients with serious illness and their families.4 Patient portals provide an opportunity to facilitate palliative care and end-of-life (PCEOL) care among populations with serious illness by improving patient–provider communication, access to health information, self-management support, and symptom monitoring.
Patient portals5 are secure websites for personal health information and tailored resources linked to a patient's electronic health record. Patient portals commonly allow patients to digitally communicate with their providers, access test results, receive health education, and manage medications. Due to portability and 24-hour access, patient portals are one of the most widely used health information technologies.6 Patient portals house tools that may improve patient and family caregiver outcomes across the trajectory of serious illness, from first diagnosis to end of life. For example, several palliative care researchers are investigating the use of patient portals for advance care planning and oncology symptom monitoring.7,8 In our previous work, we assessed the usability and user experience specifically among patients with multiple chronic conditions. Our participants indicated that patient portals save time and money and avoid unnecessary trips to the clinic.9 However, the usability, acceptability, and utility of patient portals during the early stages of serious illness or the end of life have not yet been studied.7,10
There are no studies investigating the utility and usage of patient portals among adult patients and their caregivers across the trajectory of palliative care, from onset of serious illness to end of life; these data are needed to inform patient portal strategies targeting PCEOL health outcomes such as symptom management, treatment preference, quality of life, caregiver distress, and family perceptions of care. This study uses Kaiser Permanente Colorado's (KPCO) established patient portal, My Health Manager (MHM), one of the most developed and fully integrated portal systems in the United States, to examine the utility of patient portals in the setting of PCEOL. The aims of this study are to describe MHM user characteristics among patients and their caregivers (through a proxy login option) at two time points in the setting of PCEOL: (1) the 12 months following the onset of serious illness and (2) during the last 12 months of life.
My Health Manager
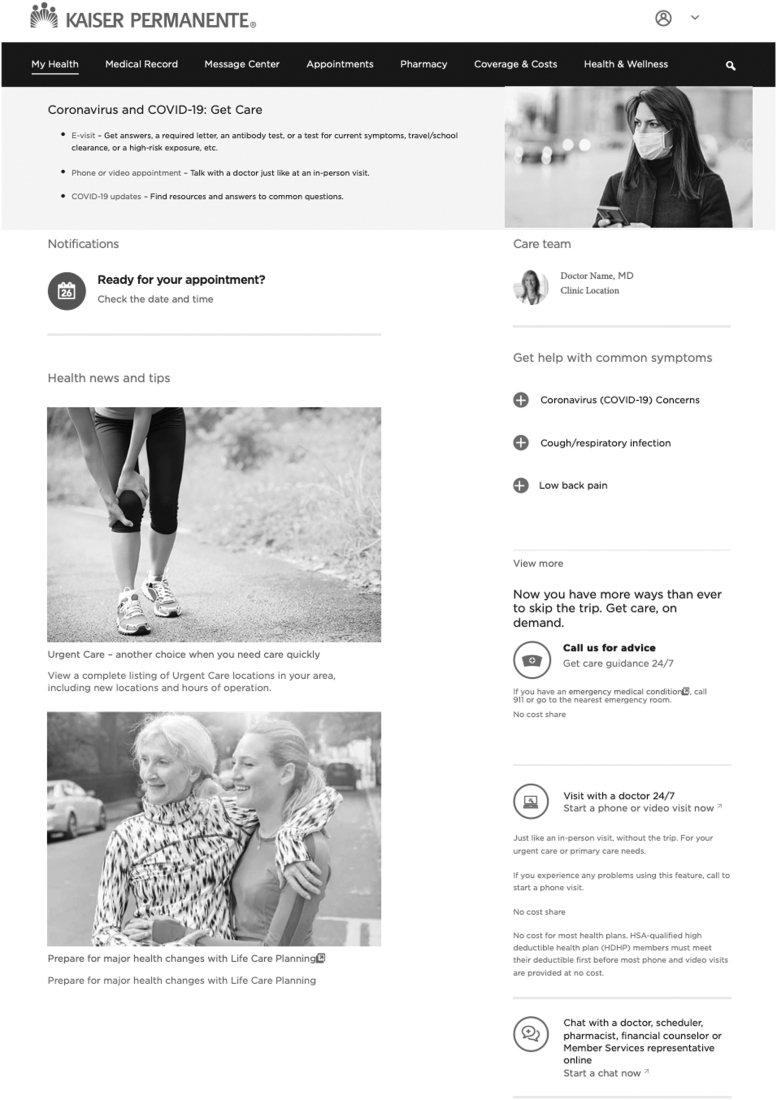
Nearly a half million people use MHM each year. Sixty-three percent of all KPCO patients and 25% of KPCO patients over the age of 65 use MHM to access portal services. MHM offers a variety of programs (Fig. 1) to facilitate services and coordinate care. MHM allows caregivers to log in to the portal on behalf of a patient through the caregiver login proxy option with patient permission. To become a caregiver proxy user, a patient can add caregivers to their portal through their profile settings and sign access authorization. Caregivers can also request authorization to add patients to their profile through profile settings.
FIG. 1.
Screenshot of MHM. Description of various MHM tools. Visits and Appointments: users can schedule or cancel appointments; My Medical Record: users can view test results, immunization records, ongoing health concerns, and care plans; Pharmacy Center: users can manage prescriptions and order medications; Health Guides and Health Management Tools: users can access health resources and self-care tools for diet, exercise, smoking cessation, and disease-specific care; Message Center: users can e-mail their provider; and Recently Added Tools: eVisits and provider chat functions for nonemergent questions and visits. MHM, My Health Manager.
| My Health Manager Tool | Functions Available |
|---|---|
| My Medical Record | Users can view test results, immunization records, ongoing health concerns, and care plans |
| Visits and Appointments | Users can schedule or cancel appointments |
| Message Center | Users can e-mail their provider |
| Pharmacy Center | Users can manage prescriptions and order medications |
| Health Guides and Health Management Tools | Users can access health resources and self-care tools for diet, exercise, smoking cessation, and disease-specific care |
| Recently Added Tools | eVisits and provider chat functions for nonemergent questions and visits |
Methods
This study included analyses of two retrospective cohorts using KPCO's MHM (Fig. 1). All study procedures were approved by KPCO's Institutional Review Board.
Cohort 1: Patients and their caregivers at the onset of serious illness cohort
The cohort consisted of 6129 patients with serious illness, over the age of 18, who were registered for MHM, and who became seriously ill between May 1, 2018, and June 30, 2018. To identify serious illness, we used KPCO's proprietary Care Group prognostic scoring, which is used in clinical practice for classifying patients who may benefit from a palliative care referral. The Kaiser Permanente prognostic algorithm uses a combination of diagnoses (ranging from various cancer types, cardio and respiratory disease, dementia, end-stage chronic heart failure or renal disease, and transplant to major mental health concerns), health risk scores, and care utilization factors to determine the severity of illness and categorizes patients as follows: Care Group 1—healthy; Care Group 2—chronic conditions; Care Group 3—advanced illness; and Care Group 4—end of life. For Cohort 1, only patients in Care Group 4 were included because patients in this score group have a 50% mortality rate at two years. Patients who were initially flagged for Care Group 4 between May 1, 2018, and June 30, 2018, were included to examine MHM use in the earlier stages of serious illness (i.e., 12 months postinitial onset of Care Group 4). Patients who died during the 12-month study period were excluded to ensure the complete analysis of patient portal use over a 12-month period. Patients with serious illness who died are the focus of Cohort 2 described below. The 148 proxy caregivers of patients identified in this cohort who were at least 18 years of age and used the patient portal as a proxy for the patient were also included. Patients and caregiver proxies are linked in the backend data.
Cohort 2: Patients and their caregivers at the end-of-life cohort
The cohort consisted of 6517 patients with chronic or serious illness, over the age of 18, who were registered for MHM, and who died between January 1, 2016, and June 30, 2019. Having a chronic or serious illness was defined by having a KPCO Care Group 2–4 flag in the last 12 months of life. Those who died from something other than chronic illness (e.g., accident) were excluded from analysis. The 163 proxy caregivers of the patients identified in this cohort who were at least 18 years of age and used the patient portal as a proxy for the patient were also included.
Data extraction and analyses
Data were extracted from KPCO's integrated electronic medical record, KP HealthConnect—Epic Systems (Epic Ambulatory, versions 2014 through 2018), Death Records, Research Data Warehouse, and MHM databases. Data extracted included patient and caregiver characteristics (age, gender, race, ethnicity, and Care Group flag) and MHM utilization (MHM use dates and features used). Using raw utilization data, we calculated the number of days that MHM and specific features were used over the 12-month study period: 12 months post the onset of serious illness and 12 months before patient's death. We analyzed unadjusted and adjusted effects of patient characteristics on 12-month daily usage using a negative binomial generalized linear model with a log link to account for overdispersion in the Poisson model. All analyses were conducted using SAS statistical software, version 9.4 (SAS Institute, Inc., Cary, NC, USA).
Results
MHM users
The demographic characteristics of the two cohorts are listed in Table 1. The average age of patients was 70.4 years in the onset of serious illness cohort and 76.7 years in the end-of-life cohort. Caregivers were 60 and 61 years of age, respectively, and mostly female in both cohorts.
Table 1.
Characteristics of My Health Manager Patient and Caregiver Proxy Users
| Onset of serious illness |
Near end of life |
|||
|---|---|---|---|---|
| Patients (N = 6129) | Caregiver/proxy users (N = 148) | Patients (N = 6517) | Caregiver/proxy users (N = 163) | |
| Characteristic | ||||
| Age,a mean (SD) | 70.4 (14.2) | 59.6 (12.9) | 76.7 (13.7) | 61.0 (13.0) |
| Female, % | 56.9 | 75.0 | 49.9 | 77.9 |
| Care Group,b % | ||||
| Group 2: chronic illness | 15.3 | |||
| Group 3: advanced illness | 21.1 | |||
| Group 4: frailty and end of life | 100 | 63.6 | ||
| Race, % | ||||
| American Indian/Alaska Native | 0.9 | 0 | <1.0 | 1.2 |
| Asian | 1.9 | 4.7 | 1.4 | 2.5 |
| Black or African American | 3.4 | 4.7 | 2.5 | <1.0 |
| Native Hawaiian/Pacific Islander | 0.2 | 0 | <1.0 | <1.0 |
| White | 81.1 | 79.7 | 83.6 | 81.6 |
| Other | 3.6 | 3.4 | 3.3 | 3.7 |
| Unknown or not reported | 8.9 | 7.4 | 8.3 | 9.8 |
| Hispanic, % | 10.3 | 9.3 | 7.2 | 14.1 |
| Portal tool use, mean (SD) | ||||
| Care team information | 7.0 (8.7) | 0 (0) | 10.8 (12.0) | 0 (0) |
| Cost and coverage | 1.1 (2.6) | 0 (0.09) | 0.9 (2.4) | 0.01 (0.13) |
| Health management guides | 2.4 (4.3) | 0.04 (0.47) | 1.4 (3.0) | 0.02 (0.36) |
| Laboratory and test results | 11.7 (16.5) | 0.19 (1.94) | 11.4 (16.8) | 0.19 (2.15) |
| Medical record | 9.9 (13.4) | 0.12 (1.31) | 4.6 (8.5) | 0.08 (1.26) |
| Medications | 11.5 (17.8) | 0.16 (1.99) | 9.4 (16.2) | 0.11 (1.65) |
| Recently added (eChat/eVisit) | 25.0 (28.8) | 0.26 (2.83) | 11.2 (19.0) | 0.16 (1.89) |
| Patient–provider communication | 24.0 (25.8) | 0.50 (4.50) | 20.8 (25.6) | 0.43 (4.41) |
| Visits and appointments | 16.8 (22.4) | 0.34 (3.66) | 13.6 (19.1) | 0.29 (3.53) |
Patient age was calculated at time of Care Group flag for onset of serious illness or at date of death for the near end-of-life cohort. Caregiver age was calculated at the end of the study period.
Care Group flag in the last 12 months of life; if there are multiple flags, the Care Group closest to the time of death is reported.
SD, standard deviation.
Caregiver use of MHM was low in both cohorts. Of the 6129 patients in the onset of serious illness cohort, 6030 used MHM at least once in the study period. Patients and caregivers used MHM on average 50.4 days in the 12 months following the onset of serious illness. Patients and caregivers in this cohort most commonly used new MHM features, including eChat functions and eVisits (25 days ±29), patient–provider communication tools (24 days ±26), and visit-scheduling options (17 days ±23). For the 6517 patients in the end-of-life cohort, 6308 used the portal at least once in the last 12 months of life. Patients and caregivers used MHM for 43 days in the last 12 months of life. Users in this cohort also commonly used patient–provider communication (21 days ±26) and visit-scheduling tools (14 days ±19), but only used the new tools for 11 days ±19. Health management and cost coverage tools were the least used tools in both cohorts. As seen in Tables 2 and 3, among the onset of serious illness cohort, rates of use of MHM were lower for females than for males (48.6 vs. 52.8), for Asians (41.6) and Blacks (44.9) than for Whites (52.8), and for users as they aged (usage by age group listed in Table 2). These trends were all seen for the near end-of-life cohorts. In this cohort, rates for use of MHM were lower for females than for males (41.1 vs. 44.6), for Asians (41.1) and Blacks (32.5) than for Whites (44.5), and also for users as they aged.
Table 2.
My Health Manager Use by Patient Characteristics
| |
Onset of serious illness (N = 6129) |
Near end of life (N = 6517) |
||||
|---|---|---|---|---|---|---|
| Characteristic | Rate | 95% CI | Rate | 95% CI | ||
| Overall | 50.4 | 49.3 | 51.5 | 42.9 | 41.9 | 43.9 |
| Age, years | ||||||
| <20 | 48.3 | 17.2 | 79.4 | 0 | 0 | 0 |
| 20–29 | 49.5 | 36.4 | 62.6 | 38.1 | 24.1 | 52.2 |
| 30–39 | 63.1 | 55.3 | 71.0 | 40.1 | 30.6 | 49.6 |
| 40–49 | 55.8 | 50.7 | 60.8 | 44.4 | 37.9 | 51.0 |
| 50–59 | 55.6 | 52.1 | 59.2 | 52.6 | 47.8 | 57.4 |
| 60–69 | 55.4 | 53.0 | 57.7 | 51.8 | 49.0 | 54.6 |
| 70–79 | 53.1 | 51.0 | 55.2 | 49.7 | 47.6 | 51.8 |
| 80–89 | 42.8 | 40.8 | 44.9 | 38.6 | 37.0 | 40.1 |
| 90+ | 30.5 | 27.7 | 33.3 | 29.2 | 27.4 | 31.0 |
| Gender | ||||||
| Female | 48.6 | 47.3 | 50.0 | 41.1 | 39.8 | 42.5 |
| Male | 52.8 | 51.0 | 54.5 | 44.6 | 43.2 | 46.0 |
| Race | ||||||
| American Indian/Alaska Native | 51.8 | 40.0 | 63.6 | 49.9 | 36.1 | 63.7 |
| Asian | 41.6 | 33.6 | 49.5 | 41.1 | 33.5 | 48.7 |
| Black or African American | 44.9 | 38.9 | 50.9 | 32.5 | 27.5 | 37.6 |
| Native Hawaiian or Other Pacific Islander | 45.0 | 19.1 | 70.9 | 53.0 | 25.4 | 80.6 |
| Other | 40.5 | 35.1 | 45.8 | 39.8 | 34.5 | 45.1 |
| Unknown or not reported | 37.2 | 34.0 | 40.3 | 30.7 | 27.7 | 33.6 |
| White | 52.8 | 51.5 | 54.0 | 44.5 | 43.4 | 45.6 |
| Care Group | ||||||
| Group 2: chronic illness | 29.8 | 27.8 | 31.7 | |||
| Group 3: advanced illness | 41.0 | 39.0 | 43.0 | |||
| Group 4: frailty and end of life | 46.7 | 45.4 | 48.0 | |||
CI, confidence interval.
Table 3.
(Adjusted) Rates of My Health Manager Usage
| Characteristic | Onset of serious illness (N = 6129) |
Near end of life (N = 6517) |
||
|---|---|---|---|---|
| Rate ratio (95% CI) | p | Rate ratio (95% CI) | p | |
| Age | 0.990 (0.988–0.991) | <0.0001 | 0.985 (0.983–0.987) | <0.0001 |
| Gender | <0.0001 | 0.0016 | ||
| Female | 0.905 (0.864–0.948) | <0.0001 | 0.925 (0.882–0.971) | 0.0016 |
| Male | Reference | Reference | ||
| Race | <0.0001 | <0.0001 | ||
| American Indian/Alaska Native | 0.950 (0.747–1.207) | 0.6727 | 0.984 (0.748–1.293) | 0.9051 |
| Asian | 0.759 (0.641–0.898) | 0.0014 | 0.853 (0.693–1.050) | 0.1330 |
| Black or African American | 0.803 (0.707–0.913) | 0.0008 | 0.646 (0.553–0.756) | <0.0001 |
| Native Hawaiian/Other Pacific Islander | 0.804 (0.496–1.303) | 0.3757 | 1.077 (0.641–1.809) | 0.7793 |
| Other | 0.725 (0.640–0.821) | <0.0001 | 0.869 (0.759–0.995) | 0.0424 |
| Unknown or not reported | 0.673 (0.620–0.730) | <0.0001 | 0.630 (0.577–0.689) | <0.0001 |
| White | Reference | Reference | ||
| Care Group | <0.0001 | |||
| Group 2: chronic illness | 0.576 (0.537–0.617) | <0.0001 | ||
| Group 3: advanced illness | 0.890 (0.838–0.946) | 0.0002 | ||
| Group 4: frailty and end of life | Reference | |||
Discussion
This is one of the first studies to examine the characteristics of patient portal users and use patterns in the setting of serious illness and end of life. In the KPCO system, patients and their caregivers are using their patient portal at the onset of serious illness and near the end of life. In comparison with other recent retrospective cohort studies investigating patient portal use patterns, usage rates among both cohorts are high. For example, the number of days that patients used the portal in a 12-month period among other studies in general primary care settings ranged from 18.5 days11 to 27.2 days,12 with some use estimates as low as 9.6 days.13This finding aligns with other work suggesting that once registered for a patient portal, patients with poorer health status are more likely to use the portal.14 However, in the setting of serious illness, patients may be too fragile to use the portal, and caregivers may have used the member's login to the portal rather than using a proxy login. Therefore, the patient usage may actually reflect use by the caregiver on the patient's portal account. In the context of KPCO, the three-year average use is 2.9 logins per month among all MHM users. However, this is logins per month rather than days used per month, which is likely a lower estimate since logins can occur multiple times a day; again suggesting that use in the study cohorts is high. A strength of this study is that we examined both people in the early stages of serious illness and those in the last year of life and found similar results.
Although use of the portal was high, there were few caregiver proxy users. This may be due to caregivers logging in as the patient rather than setting up a separate account15. An estimated 50–65% of caregivers are interested in using technologies to support and monitor the health of their loved ones,15,16 yet patient portals are rarely designed to specifically support caregivers17 or PCEOL services. Barriers to proxy adoption include difficult and time-consuming processes to gain access and privacy concerns.17–19 However, proxies who use the portal find the systems convenient and timely, and the portal is seen as important tool for engaging family in care and health communication.20,21 In the setting of serious illness, patients will increasingly rely on the support of their family, friends, and love ones to manage their care. Therefore, it is particularly important to address identified proxy adoption barriers. Facilitating proxy portal adoption may allow for easier use, improved exchange of health information, and the inclusion of tools and resources specifically for caregivers.
While the majority of patient portal research is among populations in the United States, patient portals are rolling out across Western countries.22 For example, the United Kingdom has provided patient portal access through the National Health Service since 2015.23 However, adoption and use rates in many non-US countries were found to be low and the functionality available across portals is not well described.24 To increase general adoption globally, particularly among individuals with chronic and serious illness, researchers have called for increased attention to describing characteristics of current users, contextual factors of the portal systems, and features available to patients and proxies.22 Our study contributes to this broader description of portal adoption and use in the specific context of serious illness; however, findings are unlikely to be generalizable to users beyond the KPCO system.
Patient-to-provider messaging was popular among both cohorts. Prior studies have affirmed that users value being able to communicate with providers and ask questions about nonemergent concerns.9,25,26 However, qualitative oncology patient portal research indicates that patient portal communication may have unintended negative consequences for patients with serious illness.10,27 For example, while receiving access to a simple blood test in primary care may be helpful to a patient, receiving a laboratory result related to a serious illness may indicate a treatment is no longer working. Patient portals may be a harmful method for delivering difficult news.
The new portal features, including eChat and eVisits, were the most commonly used tools among patients at the onset of serious illness. This is an unexpected finding, considering the older average age of the cohort. These tools are not commonly identified by older adults as preferred or highly valued features.14 With the onset of serious illness, there may be increased visits and interaction with the health system. Patients with serious illness may greatly benefit from the opportunity to meet with a provider using synchronous text and virtual telehealth.
Both cohorts were primarily White and female, and White users were more likely to use the portal versus non-White users. These findings support research indicating that Black and Latino patients are less likely to register for a patient portal.28,29 Low portal registration and use are attributed to lack of access to hardware (computer, tablet, and phone), English proficiency, lack of technical support, and stigmas/fears about privacy and relationship building through digital communication.30 Because Black and Latino patients and their family caregivers are less likely to receive specialized palliative care,31 if these technical barriers are addressed, patient portals may be tools for increasing awareness and access to palliative care services.
Similar to prior patient portal research,32 MHM use significantly decreased with age. Use was lowest among the oldest age groups; however, the rate of MHM use was similar, 50–55 days per year, among 40–80-year-old users in both cohorts. In these cohorts, use remained high even among older adults. Previous research recommends patient portal training sessions for older adults and caregivers and publicizing portal information (i.e., the availability and benefits of use) in public and community spaces for reducing portal adoption disparities.33 Integrating patient portal registration into clinical workflows and assigning helpers to facilitate adoption may lead to increased use.
There are several limitations to our work. First, the study was conducted in a single health system, in which patients frequently use the portal system and all were insured. The results reflect elective use rather than compulsory use and do not capture the patient portal interests of those not registered for MHM. While capturing use from the onset of serious illness until the time of death would better gauge longitudinal portal use, the cohorts were conceptualized and defined separately based on the separate questions about end-of-life and serious illness portal use. Our sample was primarily White and non-Latino, which is neither representative of Colorado's nor KPCO's racial distribution, limiting our ability to generalize these findings to a broader population. Few proxy caregivers used the portal; therefore, we were unable to test the likelihood of accessing the portal by caregiver characteristics. We were also unable to capture caregiver use if they were using the portal with patient username and password credentials. While a prognostic score is valuable in identifying seriously ill patients, we were unable to differentiate between diagnosis types; users for cancer care may have different patient portal needs and preferences than those with end-stage renal disease. Using days used, rather than logins, results in the loss of granularity in use, particularly days when patients and caregivers used the portal several times in one day. We broadly captured use in tool categories rather than specific clicks or time spent on each tool. Use may also be better captured by active (messaging and refills) versus passive use (reviewing information), which is a growing use metric for portals. The cohorts examined were before the coronavirus disease (COVID-19) pandemic, and with the uptake of telehealth, the use patterns of portals may have changed.
With growing interest in patient portal use patterns in oncology27,34 and PCEOL, there is need for deeper understanding of how people at the onset of serious illness and end of life can be helped using patient portals. Future research should include eliciting patient and caregiver feedback about specific use patterns to identify the benefits of particular tools, challenges in registration and use, and the potential for new helpful features. While the association between patient portal use and improved health outcomes is mixed, patient portal use is shown to improve patient satisfaction.24,35 Future research should explore the impact of patient portal use on PCEOL-specific outcomes, such as advance directive documentation, quality-of-life measures, and hospice referral.
Conclusions
Among KPCO MHM users, portal use was high among patients at the onset of serious illness and nearing the end of life. Addressing barriers to portal adoption and use for caregiver proxies and underserved populations is key to better leveraging patient portal systems for PCEOL.
Authors' Contributions
This study was led by J.D. Portz. Data management was conducted and overseen by J.D. Powers and M.B., with design operationalized by J.D. Portz, A.C., D.B.B., T.E.P., S.B., J.S.K., and E.B. Analysis was completed by J.D. Powers. Manuscript sections were drafted and extensively reviewed by all authors.
Funding Information
This project is being supported by the Palliative Care Research Cooperative Group funded by the National Institute of Nursing Research, U2CNR014637. Dr. Portz is supported by a career development award from the National Institute on Aging, K76AG059934.
Author Disclosure Statement
No competing financial interests exist.
References
- 1. Centers for Disease Control and Prevention. Chronic Diseases: The leading causes of death and disability in the United States. 2015. www.cdc.gov/chronicdisease/overview/index.htm (Last accessed May 16, 2016).
- 2. Block S: Measurment and quality: Moving towards universal access to high-quality serious illness care. Center to Advance Palliative Care. 2019. https://www.capc.org/blog/palliative-pulse-palliative-pulse-september-2017-moving-towards-universal-access-high-quality-serious-illness-care (Last accessed August 13, 2020).
- 3. Morrison RS: Research priorities in geriatric palliative Care: An introduction to a new series. J Palliat Med 2013;16:726–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Block S: In: Quill TE, Miller FG (eds.) Palliative Care and Ethics. New York, NY: Oxford University Press, 2016. [Google Scholar]
- 5. Most practices offer a patient portal. Medical Group Management Association. 2018. https://www.mgma.com/data/data-stories/are-portals-a-means-to-patient-activation (Last accessed April 29, 2019).
- 6. Ford EW, Hesse BW, Huerta TR: Personal health record use in the United States: Forecasting future adoption levels. J Med Internet Res 2016;18:e73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Siegel CS, Spies V, Rodin MB, Tu Y: Use of an EMR online portal for communication with cancer patients. J Clin Oncol 2016;34(26_suppl):147. [Google Scholar]
- 8. Jordan SR, Brungardt A, Phimphasone-Brady P, Lum HD: Patient perspectives on advance care planning via a patient portal. Am J Hosp Palliat Med 2019;36:682–687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Portz JD, Bayliss EA, Bull S, et al. : Intent to use and use-experience of a patient portal among older adults with multiple chronic conditions: A qualitative study. J Med Internet Res 2019;21:e11604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Siegel C, Gill A, Esteghamat N, et al. : Barriers to online patient portal adoption among adult oncology patients. J Clin Oncol 2017;35(31_suppl):44. [Google Scholar]
- 11. Jones JB, Weiner JP, Shah NR, Stewart WF. The wired patient: Patterns of electronic patient portal use among patients with cardiac disease or diabetes. J Med Internet Res 2015;17:e42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Riippa I, Linna M, Rönkkö I, Kröger V: Use of an electronic patient portal among the chronically ill: An observational study. J Med Internet Res 2014;16:e275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ancker JS, Barrón Y, Rockoff ML, et al. : Use of an electronic patient portal among disadvantaged populations. J Gen Intern Med 2011;26:1117–1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sakaguchi-Tang DK, Bosold AL, Choi YK, Turner AM: Patient portal use and experience among older adults: Systematic review. JMIR Med Inform 2017;5:e38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Caregiving in the U.S. AARP and National Alliance for Caregiving. 2020. https://www.caregiving.org/wp-content/uploads/2020/06/AARP1316_RPT_CaregivingintheUS_WEB.pdf (Last accessed June 17, 2020).
- 16. Fox S, Duggan M, Purcell K: Family caregivers are wired for health. Pew Research Center. http://www.pewinternet.org/2013/06/20/family-caregivers-are-wired-for-health. 2013. (Last accessed August 15, 2017).
- 17. Sarkar U, Bates DW: Care partners and online patient portals. JAMA 2014;311:357. [DOI] [PubMed] [Google Scholar]
- 18. Latulipe C, Quandt SA, Melius KA, et al. : Insights into older adult patient concerns around the caregiver proxy portal use: Qualitative interview study. J Med Internet Res 2018;20:e10524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. DesRoches CM, Walker J, Delbanco T: Care partners and patient portals—Faulty access, threats to privacy, and ample opportunity. JAMA Intern Med 2020;180:850. [DOI] [PubMed] [Google Scholar]
- 20. Reed ME, Huang J, Brand R, et al. : Communicating through a patient portal to engage family care partners. JAMA Intern Med 2018;178:142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Casillas A, Cemballi A, Abhat A, et al. : An untapped potential for an invisible economy in primary care? Making patient portals work for caregivers in the safety-net. J Med Internet Res 2020;22:e18466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Alturkistani A, Greenfield G, Greaves F, et al. : Patient portal functionalities and uptake: Systematic review protocol. JMIR Res Protoc 2020;9:e14975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. About GP Online Services. National Health Service. https://www.england.nhs.uk/gp-online-services/about-the-prog. (Last accessed February 27, 2021).
- 24. Ammenwerth E, Schnell-Inderst P, Hoerbst A: The impact of electronic patient portals on patient care: A systematic review of controlled trials. J Med Internet Res 2012;14:e162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Zide M, Caswell K, Peterson E, et al. : Consumers' patient portal preferences and health literacy: A survey using crowdsourcing. JMIR Res Protoc 2016;5:e104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Reed ME, Huang J, Millman A, et al. : Portal use among patients with chronic conditions: Patient-reported care experiences. Med Care 2019;57:809–814. [DOI] [PubMed] [Google Scholar]
- 27. Alpert JM, Morris BB, Thomson MD, et al. : Implications of patient portal transparency in oncology: Qualitative interview study on the Experiences of Patients, Oncologists, and Medical Informaticists. JMIR Cancer 2018;4:e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Goel MS, Brown TL, Williams A, et al. : Disparities in enrollment and use of an electronic patient portal. J Gen Intern Med 2011;26:1112–1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gordon NP, Hornbrook MC: Differences in access to and preferences for using patient portals and other eHealth Technologies based on race, ethnicity, and age: A database and survey study of seniors in a Large Health Plan. J Med Internet Res 2016;18:e50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lyles CR, Allen JY, Poole D, et al. : “I Want to Keep the Personal Relationship With My Doctor”: Understanding barriers to portal use among African Americans and Latinos. J Med Internet Res 2016;18:e263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Johnson KS: Racial and ethnic disparities in palliative care. J Palliat Med 2013;16:1329–1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wildenbos GA, Peute L, Jaspers M: Facilitators and barriers of electronic health record patient portal adoption by older adults: A literature study. Stud Health Technol Inform 2017;235:308–312. [PubMed] [Google Scholar]
- 33. Arcury TA, Quandt SA, Sandberg JC, et al. : Patient portal utilization among ethnically diverse low income older adults: Observational study. JMIR Med Inf 2017;5:e47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Alpert JM, Morris BB, Thomson MD, et al. : Identifying how patient portals impact communication in oncology. Health Commun 2019;34:1395–1403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Palen TE, Ross C, Powers JD, Xu S: Association of online patient access to clinicians and medical records with use of clinical services. JAMA 2012;308:2012. [DOI] [PubMed] [Google Scholar]