Traditionally, women are under-represented in leadership positions in cardiology and are less likely than men to receive grants in academic medicine.1 Despite major recent advancements in cardiovascular research, trends in research funding for cardiovascular research are unknown. Therefore, we assessed National Institutes of Health (NIH) funding trends in the allocation of R01 grants for cardiovascular research stratified by gender.
The NIH RePORTER (Research Portfolio Online Reporting Tools Expenditure) was searched using cardiovascular-related search and MeSH terms to obtain information regarding funding amount, principal investigator (PI), co-PIs, and institution name for R01 grants in cardiovascular research from 2011 to 2020. The gender of each PI was categorized using Genderize. In an instance where probability threshold for gender assignment was <95%, personal pronouns on institutional profiles were used. Consumer Price Index was used to adjust funding amount to 2020 equivalent U.S. dollars. The number of citations, publications, H-index, and seniority were obtained from Scopus and Web of Science in January 2021. Seniority was defined as years from first publication to the time of grant award. The membership roster of the American College of Cardiology was used to identify applicants who were cardiologists. Linear regression was conducted to analyze trends in funding. Multiple linear regression was used to determine the relationship between funding amount and gender after adjusting for the number of publications, citations, degrees, institution, H-index, and seniority. A P value <0.05 was considered significant.
A total of 1,534 NIH-funded R01 grants amounting to $761.4 million were awarded for cardiovascular research. Women (n = 307; 20.0% [95% CI: 18.0%–22.1%]) received fewer grants than men (n = 1,227; 80.0% [95% CI: 77.9%–82.0%]). From 2011 to 2020, the number of grants awarded increased significantly among both men (113 to 126 [12%; P = 0.02]) and women (18 to 47 [161%; P < 0.01]) (Figure 1A). Similarly, the grant amount (in millions) awarded increased significantly among men and women (50.3 to 65.0 in men [29%; P < 0.01] vs 7.7 to 26.9 in women [249%; P < 0.01]) (Figure 1B). The rate of change in total grant dollars ($1.92 million) and total number of grants (2.9) per person was higher in women compared with men (grant dollars: $1.47 million; number of grants: 1.3). Only 93 grant awardees were cardiologists, among whom 13 were women. A significant association between female gender and lower funding amount was observed (β = −0.09; P < 0.01).
FIGURE 1.
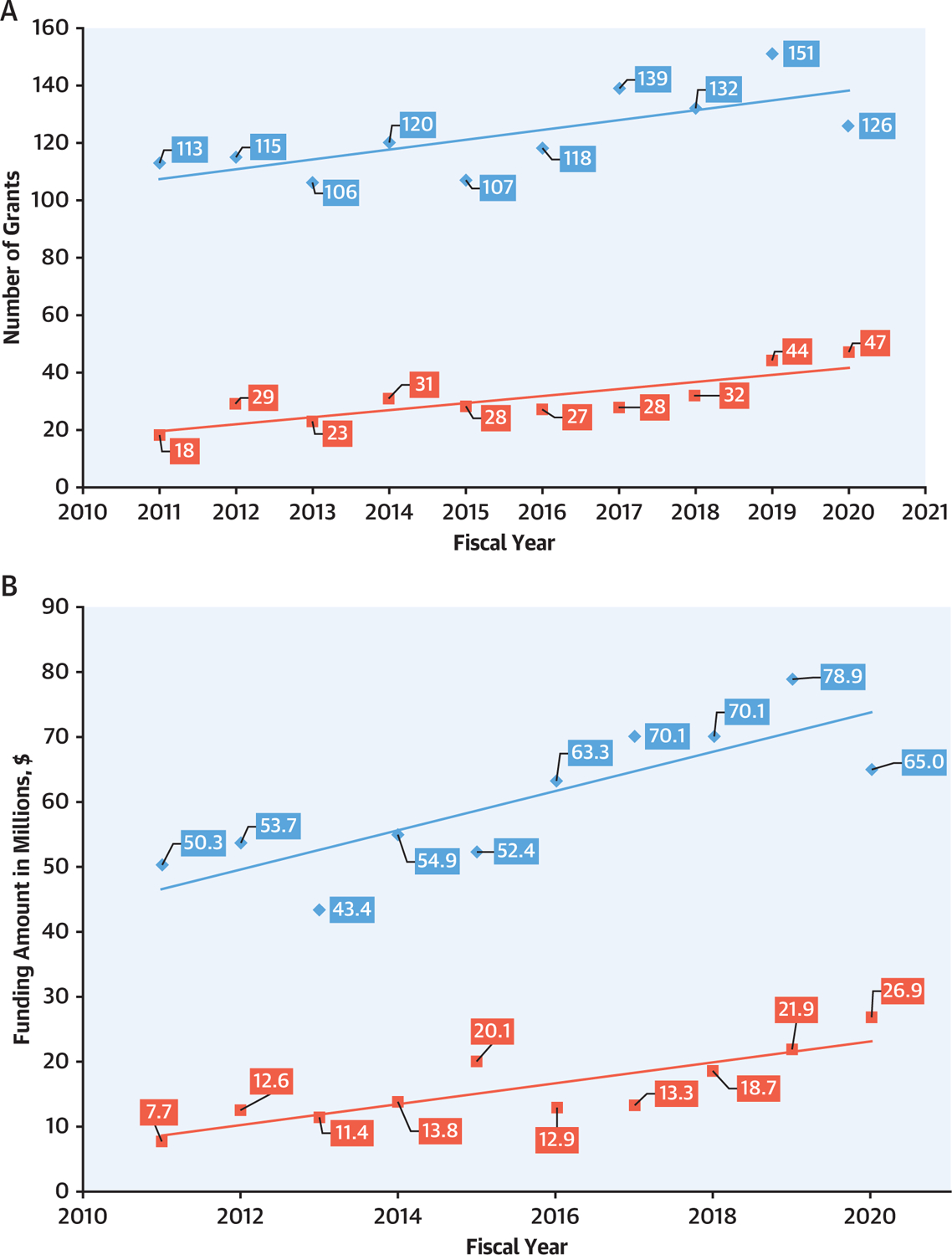
Trends in National Institutes of Health R01 Funding to Principal Investigator by Gender
(A) Total number of R01 grants and (B) total amount of R01 funding for both men (blue) and women (red).
Of the 1,534 grants awarded, 728 were awarded to PhDs, 433 to MDs, and 373 to MD/PhDs. From 2011 to 2020, the proportion of grants awarded to women MDs significantly increased from 6.5% to 42.5% (P = 0.02), contrasting with nonsignificant temporal changes among women PhDs (22.4% to 33.7%; P = 0.15) and women MD/PhDs (11% to 4%; P = 0.06). Funding amount was significantly associated with the number of publications (β = 0.12; P < 0.01), H-index (β = 0.15; P < 0.01) and institution (P = 0.02). Of the 408 co-PIs identified, 330 were men (80.9% [95% CI: 76.7%–84.6%]) and 78 were women (19.1% [95% CI: 15.4%–23.3%]).
From 2011 to 2020, 1 in 5 cardiovascular R01 grants were awarded to women. Possible factors may include fewer female cardiologists, fewer female applicants, or unfair evaluation during grant application review. Upstream factors such as lack of institutional support, mentorship, and inequitable work environments could also disadvantage women applicants.1
Studies have shown that women’s scholarship is less-often cited, leading to a lower H-index.2 Our analysis demonstrates that number of publications and H-index are associated with grant amount, suggesting that high-impact publications may be an important consideration during grant application review. Therefore, including women in research and authorship networks should be considered within a comprehensive approach to support female investigators and reduce disparities in NIH-funded cardiovascular research.
Although the reported gender gap in R01 grants is extensive, we found encouraging trends. We observed a higher percentage increase in funding amounts and number of grants awarded to women than men, which is analogous to the increase in percentage of female cardiologists between 2010 and 2019 (95% CI: 10.8%–14.9%).3
Limitations of this study should be noted. First, NIH RePORTER reports only funded grants; we could not account for the number of applications and success rates in grant applications. Second, cardiovascular-related search terms may not have yielded all grants. Additionally, seniority was measured by years since first publication and not by academic rank. Although this analysis shows marginal improvement toward gender equity in R01 awards, concerted efforts to reduce the continued gender gap are warranted.
Acknowledgments
Dr Van Spall has received research support from the Canadian Institutes of Health Research and the Heart and Stroke Foundation of Canada (modest). Dr Reza is supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under award number KL2TR001879 (modest). Dr Greene has received research support from the Duke University Department of Medicine Chair’s Research Award, American Heart Association, Amgen, AstraZeneca, Bristol Myers Squibb, Cytokinetics, Merck, Novartis, Pfizer, and Sanofi; has served on advisory boards for Amgen, AstraZeneca, Bristol Myers Squibb, Cytokinetics, and Sanofi; and serves as a consultant for Amgen, Bayer, Bristol Myers Squibb, Merck, Sanofi, and Vifor. Dr Michos has received research support from the Amato Fund for Women’s Cardiovascular Health at Johns Hopkins University; and has served on advisory boards for AstraZeneca, Bayer, Boehringer Ingelheim, Novartis, Novo Nordisk, Amarin, and Esperion. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
REFERENCES
- 1.Van Spall HGC, Lala A, Deering TF, et al. Ending gender inequality in cardiovascular clinical trial leadership: JACC review topic of the week. J Am Coll Cardiol. 2021;77(23):2960–2972. [DOI] [PubMed] [Google Scholar]
- 2.Ha GL, Lehrer EJ, Wang M, et al. Sex differences in academic productivity across academic ranks and specialties in academic medicine: a systematic review and meta-analysis. JAMA Netw Open. 2021;4(6): e2112404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.2019 Physician Specialty Data Report. Association of American Medical Colleges. Accessed February 26, 2022. https://www.aamc.org/data-reports/workforce/interactive-data/active-physicians-sex-and-specialty-2019 [Google Scholar]


