Abstract
Recovery from COVID-19 is not always uneventful, especially in critically ill hospitalized patients. Persistent symptoms including fatigue/ weakness, shortness of breath, anxiety, and depression have been described at one-year follow-up. Furthermore, symptoms from the musculoskeletal system like joint pain or stiffness are underreported in studies with long-term follow-up of up to one year. Infection with SARS-CoV-2 itself has been associated with endothelial damage, and together with high-dose corticosteroid treatment, it is predisposed to the dissemination of microthrombi and the development of femoral head osteonecrosis (FHOn), as it has been shown during the previous (2003–2004) coronavirus outbreaks. A resurgence of FHOn cases is anticipated but this is not reflected in the existing studies with long-term follow-up. Prompt diagnosis is critical for early treatment and possibly for the hip joint preservation. Patients with COVID-19 treated with corticosteroids should be screened for avascular necrosis early after discharge from the hospital. Every healthcare worker involved in the management of these patients should maintain a high level of suspicion and should be alert when patients report symptoms such as vague aches at the buttocks, hip area, adductors, and/or above the knee. Studies are needed to identify risk factors for FHOn including disease severity, type of steroid, cumulative dose, and duration of treatment.
Keywords: COVID-19, corticosteroids, femoral head osteonecrosis, symptoms, musculoskeletal system
The immense burden of the COVID-19 pandemic has globally challenged the healthcare delivery and the healthcare system reserves. It is important that the postacute sequelae of SARS-CoV-2 infection (PASC) and complications of the disease and the therapeutic interventions in millions of patients worldwide are intensively studied and monitored.
Few studies have reported PASC after infection with SARS-CoV-2. Darcis et al (2021) reported improvement in radiographic imaging and pulmonary functional tests but persistence of symptoms after six months. The most prevalent symptoms were shortness of breath and fatigue. Fatigue and memory impairment were unexpectedly increased over time. There was a trend for association between diffusion capacity of carbon monoxide and persistent symptoms. In another study, Huang et al reported a wide range of lesser known PASC in COVID-19 survivors one year after discharge from the hospital (Huang et al., 2021). Again, dyspnea, anxiety, and depression increased in prevalence at one year. Female sex and corticosteroid therapy at the acute phase were risk factors for fatigue or muscle weakness, with more prevalent mobility or discomfort problems than in the matched controls (Huang et al., 2021).
Reporting PASC regarding the musculoskeletal system, however, is inconsistent and variable. Fatigue and muscle weakness are some of the most common persistent long-term symptoms and are probably associated with lung diffusion capacity injury, viral myositis, or steroids myopathy (Huang et al., 2021; Tsai et al., 2004). Other symptoms such as mobility and discomfort problems, joint pain, and stiffness are not systematically investigated and reported. Huang et al reported a 12% incidence of joint pain and 4% of myalgia. In addition, 9% of the patients had mobility problems (Huang et al., 2021). Generally, the impact of SARS-CoV-2 infection and the combined therapeutic interventions on the skeletal system have not been thoroughly investigated as part of the follow-up protocol in most long-term studies. More specifically, there is no report of the incidence of femoral head osteonecrosis (FHOn) or other necrotic lesions of the skeleton.
In hundreds of thousands of patients globally, the systemic corticosteroids have been extensively used at the early stages of the disease in variable dosages and treatment durations (Agarwala et al., 2021; Mont et al., 2015; Zhao et al., 2021). Compared with usual care or placebo, they have been associated with lower 28-day all-cause mortality of critically ill patients (Huang et al., 2021). In the study by Huang et al (2021), 48% of the hospitalized COVID-19 survivors received corticosteroid therapy. By large-scale use of life-saving corticosteroids in COVID-19 cases, we anticipate that there will be a resurgence of cases in the femoral head and/or other joints of the skeleton (Mont et al., 2015) (Figs. 1 , 2 , and 3 ). It is estimated that a cumulative dose of 2000 mg of prednisolone or equivalent is associated with increased risk of FHOn (Jones, 2001). This varies with daily administered dose, type of steroid, maximum dose, and underlying disease (Powell et al., 2010). The minimum dose for FHOn development is approximately 700 mgr of prednisolone or equivalent (Anderton and Helm, 1982). A duration of at least six months to one year is needed after corticosteroid treatment before FHOn develop symptoms (McKee et al., 2001). Corticosteroids may induce osteonecrosis (ON), mainly through altering the lipid metabolism resulting in fat accumulation in the bone marrow and enlargement of fat cells with subsequently increased intramedullary pressure. Furthermore, by decreasing the blood supply at the femoral head through fat embolism and microthrombosis and by corticosteroid-induced apoptosis of the osteocytes, corticosteroids may cause ON (Wang et al., 2018).
Fig. 1.
MRI of the left hip of a 67-year-old patient. The patient had severe SARS-CoV-2 infection and received 3400 mgr of prednisolone during hospital admission. He presented with hip pain after 8 months of COVID-19. T2W MRI sequence demonstrates the pathognomonic double-line sign of FHOn.
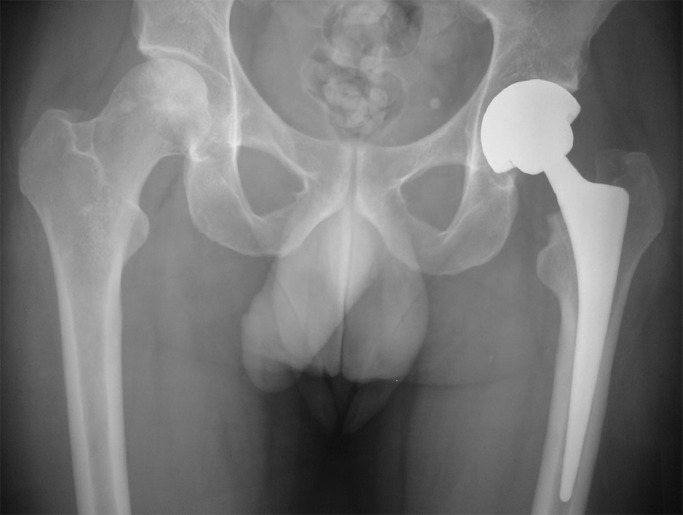
Fig. 2.
Preoperative radiograph. Collapse of the femoral head and mild arthritic changes of the hip joint are shown.
Fig. 3.
Postoperative radiograph depicting total hip arthroplasty of the left hip.
In the case of COVID-19, the “thrombo-inflammatory cascade” causes endothelial injury and predisposes to microthrombosis. The hypercoagulability state of SARS-CoV-2 infection is also considered a risk factor for ON (Mehta et al., 2020). In addition, other treatments studied during the early phase of the pandemic such as the antivirals ritonavir and lopinavir may trigger FHOn (Patel et al., 2021).
Observational studies of patients treated with corticosteroids for SARS-1 epidemic in 2003 reported FHOn and/or major joints, as early as four months from the infection, ranging from 24%–41%, when the patients were followed up to three and even to seven years (Guo et al., 2014; Hong and Du, 2004; Hui et al., 2009; Zhao et al., 2010; Zhao et al., 2013). FHOn was confirmed by MRI, which is considered the method of choice for early-stage diagnosis. The mean total steroid dose varied from 4904–4117 mg of prednisone or equivalent, and higher doses were associated with increased risk for ON (Guo et al., 2014). In some cases, bilateral FHOn was noted. Besides femoral head, other sites were also affected, including the shoulder, knee, and ankle (Guo et al., 2014; Hong and Du, 2004; Hui et al., 2009; Zhao et al., 2010; Zhao et al., 2013). The natural history of these necrotic bone lesions at the weight bearing areas of the joints involves the progression to articular surface collapse, painful and restricted range of motion, and nonreversible joint destruction (Zhao et al., 2010; Zhao et al., 2013). In a recent review, it was reported that the time interval between corticosteroid treatment and FHOn onset was shorter in patients with COVID-19 than those without COVID-19, and in some cases, FHOn develops without corticosteroid treatment (Shetty, 2021). The precise cumulative corticosteroids dose and/or duration of therapy for developing FHOn cannot be estimated in SARS-CoV-2 infection, but higher dose, longer duration, severe COVID-19 pneumonia, intensive care unit admission, elevated inflammatory serum markers, and personal history of smoking or excessive alcohol consumption have been postulated as potential risk factors (Shetty, 2021). However, no observational cohort study has been published regarding COVID-19 and FHOn incidence.
When assessing PASC, especially in patients treated with a high dose of corticosteroids, it is crucial to maintain a high index of suspicion for the development of the initially asymptomatic (which could last for several months but potentially evolving to collapse) infarcts at the femoral head, knees, shoulders, and/or talus (Krez et al., 2021; Zhang et al., 2021; Zhao et al., 2010). Close follow-up with MRI screening of the hips and all major joints should be conducted in the first 3–4 months after discharge for early detection of the lesions, before the collapse of the necrotic bone. Upon diagnosis, prompt intervention might save the native joint and avoid an undesirable total joint replacement in young patients. All specialties involved in management of patients with COVID-19 should be aware of this potential serious consequence of the disease and its treatment. In addition, mobility problems caused by fatigue or muscle weakness should be promptly managed to avoid any decline in quality of life of patients with COVID-19.
Furthermore, future studies of long-term follow-up of patients with SARS-CoV-2 infection should include in their methodology the reporting of musculoskeletal symptoms and especially, the incidence of FHOn. In addition, these studies could help determine the predisposing factors that are associated with FHOn development, including the cumulative dose of corticosteroids, type and route of corticosteroid administration, duration of therapy, disease severity, inflammatory biomarkers, and other yet unknown risk factors.
Ethical Approval
The study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of the University General Hospital of Larissa.
Declaration of Competing Interest
The authors have no competing interests to declare.
Acknowledgments
No funds were received for this perspective article.
References
- Agarwala SR, Vijayvargiya M, Pandey P. Avascular necrosis as a part of “long COVID-19. BMJ Case Rep. 2021;14 doi: 10.1136/bcr-2021-242101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderton JM, Helm R. Multiple joint osteonecrosis following short-term steroid therapy. Case report. J Bone Joint Surg Am. 1982;64:139–141. [PubMed] [Google Scholar]
- Darcis G, Bouquegneau A, Maes N, Thys M, Henket M, Labye F, et al. Long-term clinical follow-up of patients suffering from moderate-to-severe COVID-19 infection: a monocentric prospective observational cohort study. Int J Infect Dis. 2021;109:209–216. doi: 10.1016/j.ijid.2021.07.016. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo KJ, Zhao FC, Guo Y, Li FL, Zhu L, Zheng W. The influence of age, gender and treatment with steroids on the incidence of osteonecrosis of the femoral head during the management of severe acute respiratory syndrome: a retrospective study. Bone Joint J. 2014 doi: 10.1302/0301-620X.96B2.31935. 96–B:259–62. [DOI] [PubMed] [Google Scholar]
- Hong N, Du XK. Avascular necrosis of bone in severe acute respiratory syndrome. Clin Radiol. 2004;59:602–608. doi: 10.1016/j.crad.2003.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang L, Yao Q, Gu X, Wang Q, Ren L, Wang Y, et al. 1-year outcomes in hospital survivors with COVID-19: a longitudinal cohort study. Lancet. 2021;398:747–758. doi: 10.1016/S0140-6736(21)01755-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hui L, de Vlas SJ, Liu W, et al. Avascular osteonecrosis after treatment of SARS: a 3-year longitudinal study. 2009;14(Suppl. 1):79–84. doi: 10.1111/j.1365-3156.2008.02187.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones JP. In: Arthritis and allied conditions: a textbook of rheumatology. 14th ed. Koopman WJ, editor. Lippincott Williams & Wilkins; Philadelphia: 2001. Osteonecrosis; pp. 2143–2164. editor. p. [Google Scholar]
- Krez A, Lane J, Heilbronner A, Park-Min KH, Kaneko K, Pannellini T, et al. Risk factors for multi-joint disease in patients with glucocorticoid-induced osteonecrosis. Osteoporos Int. 2021;32:2095–2103. doi: 10.1007/s00198-021-05947-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKee MD, Waddell JP, Kudo PA, Schemitsch EH, Richards RR. Osteonecrosis of the femoral head in men following short-course corticosteroid therapy: a report of 15 cases. CMAJ. 2001;164:205–206. [PMC free article] [PubMed] [Google Scholar]
- Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ, et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mont MA, Pivec R, Banerjee S, Issa K, Elmallah RK, Jones LC. High-dose corticosteroid use and risk of hip osteonecrosis: meta-analysis and systematic literature review. J Arthroplasty. 2015;30 doi: 10.1016/j.arth.2015.03.036. 1506–1512.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel TK, Patel PB, Barvaliya M, Saurabh MK, Bhalla HL, Khosla PP. Efficacy and safety of lopinavir-ritonavir in COVID-19: A systematic review of randomized controlled trials. J Infect Public Health. 2021;14:740–748. doi: 10.1016/j.jiph.2021.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell C, Chang C, Naguwa SM, Cheema G, Gershwin ME. Steroid induced osteonecrosis: an analysis of steroid dosing risk. Autoimmun Rev. 2010;9:721–743. doi: 10.1016/j.autrev.2010.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shetty GM. Double trouble-COVID-19 and the widespread use of corticosteroids: are we staring at an osteonecrosis epidemic? Indian J Orthop. 2021;56:1–11. doi: 10.1007/s43465-021-00546-8. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai LK, Hsieh ST, Chao CC, Chen YC, Lin YH, Chang SC, et al. Neuromuscular disorders in severe acute respiratory syndrome. Arch Neurol. 2004;61:1669–1673. doi: 10.1001/archneur.61.11.1669. [DOI] [PubMed] [Google Scholar]
- Wang A, Ren M, Wang J. The pathogenesis of steroid-induced osteonecrosis of the femoral head: A systematic review of the literature. Gene. 2018;671:103–109. doi: 10.1016/j.gene.2018.05.091. [DOI] [PubMed] [Google Scholar]
- Zhang S, Wang C, Shi L, Xue Q. Beware of steroid-induced avascular necrosis of the femoral head in the treatment of COVID-19-Experience and lessons from the SARS epidemic. Drug Des Devel Ther. 2021;15:983–995. doi: 10.2147/DDDT.S298691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao FC, Guo KJ, Li ZR. Osteonecrosis of the femoral head in SARS patients: seven years later. Eur J Orthop Surg Traumatol. 2013;23:671–677. doi: 10.1007/s00590-012-1054-4. [DOI] [PubMed] [Google Scholar]
- Zhao FC, Li ZR, Zhang NF, Wang BL, Sun W, Cheng LM, et al. Lesion size changes in osteonecrosis of the femoral head: a long-term prospective study using MRI. Int Orthop. 2010;34:799–804. doi: 10.1007/s00264-009-0829-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Y, Yang C, An X, Xiong Y, Shang Y, He J, et al. Follow-up study on the COVID-19 survivors after one year discharged from hospital. Int J Infect Dis. 2021;112:173–182. doi: 10.1016/j.ijid.2021.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]