Abstract
Purpose
Studies have shown increased residential greenspace is associated with improved outcome following stroke. This study sought to determine if residential greenspace is an independent stroke risk factor.
Methods
A retrospective 1:4 matched case-control study involving 1174 stroke and 4696 control patients over a 3-year period from Milwaukee County, Wisconsin, was conducted. Greenspace was determined using normalized difference vegetation index (NDVI) for a 250-meter radius surrounding a subject’s residence. The area deprivation index (ADI) for the census block tract of a subject’s residence was obtained from the Neighborhood Atlas® (University of Wisconsin School of Medicine and Public Health). Relationship between greenspace, ADI, and stroke was determined using conditional logistic regression. Relationships among NDVI, state and national ADI, and proximity to public parks were determined using Spearman’s rank-order correlation.
Results
NDVI and stroke risk were inversely correlated (odds ratio [OR]: 0.33, 95% CI: 0.111–0.975; P=0.045), with 19% lowered odds of stroke for patients living in the highest greenspace quartile compared to the lowest quartile (OR: 0.81, 95% CI: 0.672–0.984; P=0.045). Patients living in the most deprived ADI quartile had 28% greater stroke risk than those living in the least deprived ADI quartile (OR: 1.28, 95% CI: 1.02–1.6; P=0.029). Non-Hispanic Black patients lived in residential areas with lower greenspace (P<0.001) and neighborhoods of greater state and national ADI (P<0.001 for both) than non-Hispanic White patients.
Conclusions
In Milwaukee County, living with greater surrounding greenspace or areas of lower deprivation is associated with lower odds of stroke. NDVI represents an independent risk factor for stroke, not simply a proxy for socioeconomic status.
Keywords: greenspace, stroke, area deprivation index, NDVI, socioeconomic status
Greenspace — areas covered with trees, grass, or other vegetation — is increasingly recognized for its benefits to mental and physical health.1 There is a direct correlation between greenspace and improved attention, mood, and physical activity.2 Additionally, data from multiple studies indicate that increased greenspace is linked to decreased hospitalizations for heart disease and stroke as well as reduced stroke severity and mortality.2–5 Investigators from Perth, Australia, reported that the odds of hospitalization for heart disease or stroke was lower for adults living in the highest tertile of greenspace compared to those living in the lowest (odds ratio [OR]: 0.87, 95% CI: 0.60–1.27).3 A study from Beth Israel Deaconess Medical Center (Boston, MA) found that stroke mortality was lower for patients living in the highest quartile of greenspace compared to the lowest (hazard ratio: 0.78, 95% CI: 0.63–0.97),5 and in a longitudinal study of 575,000 Canadians, investigators found that stroke mortality was lower in the highest greenspace quartile compared to the lowest (relative risk: 0.96, 95% CI: 0.93–0.95).6 Investigators from Barcelona, Spain, determined that stroke severity decreased as residential greenspace increased when comparing highest quartile to lowest (OR: 0.75, 95% CI: 0.60–0.95).7 While clearly linked to stroke outcomes, it remains unknown if greenspace is an independent risk factor for stroke incidence.
Stroke incidence worldwide is negatively correlated with socioeconomic status (SES).8 Both in low-SES countries and among low-SES populations within high-income countries, the risk of stroke was reported to be higher.9 Higher levels of deprivation also have been associated with an increased risk of adverse health and health care outcomes,10 including stroke.8–11 Although greenspace might be expected to correlate with SES, it is unclear whether greenspace functions as a proxy for SES.6
The primary purpose of this study was to determine if residential greenspace is a risk factor for stroke, independent of SES and individual stroke risk factors. We also sought to determine if neighborhood disadvantage was an independent risk factor for stroke. As the largest study to address the relationships among residential greenspace, geographic SES, and stroke risk, findings may improve our understanding of the interconnectivity between the environment in which we live and health outcomes, knowledge that could be used to inform public policy interventions.
METHODS
Study Design
This retrospective 1:4 matched case-control study was deemed exempt human subjects research by the Advocate Aurora Health institutional review board (per 45 CFR 46.104[d][4i & 4iii]). The primary outcome measures were the odds of stroke as a function of residential greenspace exposure as measured by the normalized difference vegetation index (NDVI). Secondary outcome measures include the odds of stroke as a function of neighborhood socioeconomic status as measured by the area deprivation index (ADI).
Case and Control Ascertainment
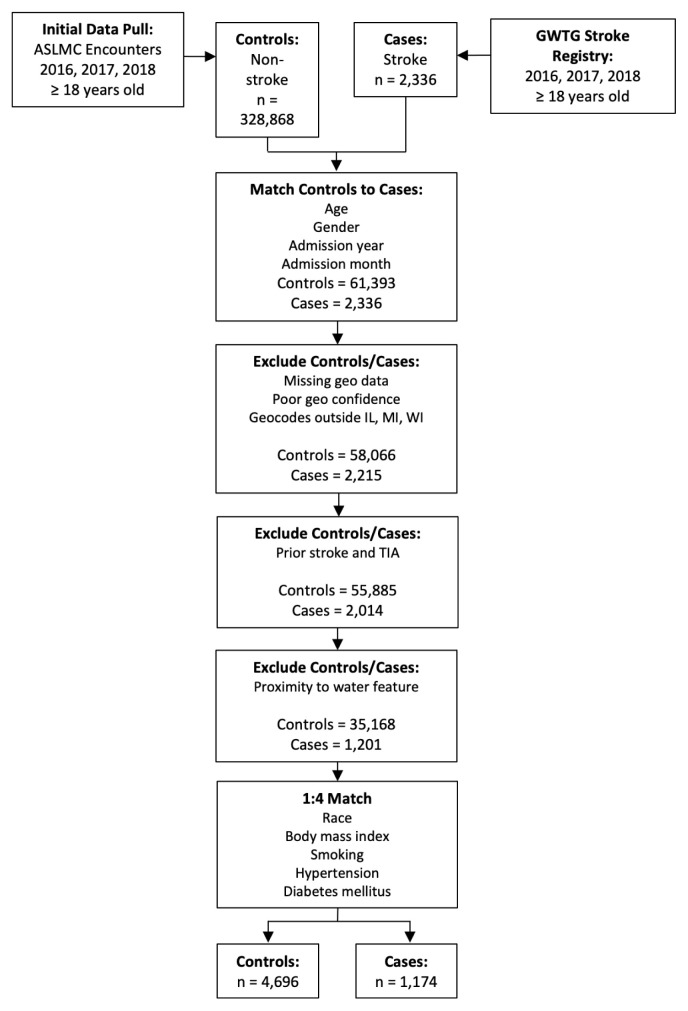
Any patient ≥18 years of age discharged from Aurora St. Luke’s Medical Center (ASLMC) in Milwaukee Wisconsin, with an International Classification of Diseases (ICD)-coded diagnosis of stroke in calendar years 2016, 2017, or 2018 was included in this study (Figure 1). Patients at ASLMC with a nonstroke diagnosis from the same years were included as potential controls. Stroke was defined as ischemic stroke, transient ischemic attack, subarachnoid hemorrhage, or intracerebral hemorrhage.
Figure 1.
Flow chart of study participants depicting how study participants were chosen and exclusion criteria. ASLMC, Aurora St. Luke’s Medical Center; GWTG, Get With The Guidelines; geo, geographic; IL, Illinois; MI, Michigan; TIA, transient ischemic attack; WI, Wisconsin.
Patients with stroke (n=2336 cases) were identified through the Get with the Guidelines database (maintained as a requirement of Comprehensive Stroke Center designation). Patients with no stroke diagnosis (n=328,868 controls) were identified via search of the hospital’s electronic health records database (Epic Systems Corporation). Using a 1:M (many) case-control design,12,13 1 case (patient with stroke diagnosis) was matched to up to 4 nonstroke controls without replacement (ie, 1 control could only match 1 case). For each case, a restricted pool of potential controls was identified based on gender, 5-year age group, and admit month and year (n=61,393). Patients with missing geocode data or poor geocode confidence were excluded, as were those with geocodes outside of Milwaukee County. Additional patient exclusions included prior stroke history or the presence of a water feature within 250 meters of their residential zone (n=1201 cases; n=35,168 controls), as living near a body of water confers health benefits distinct from those of greenspace.14–16
Controls were matched to stroke cases based on admission year, age, gender, and race. Stroke risk factors also were used as matching criteria and included hypertension, diabetes, current or past smoking history, body mass index, and cholesterol. Mahalanobis distance matching was utilized to determine the distance between the patients with stroke and patients in the control group based on a set of variables (caliper width of 0.20). This procedure minimizes the Mahalanobis distance between the stroke case and control, and the caliper specifies the chosen cutoff for the maximum distance allowed. If a control was eligible for multiple cases, it was assigned to the case with the fewest potential controls. In the event of a tie, the control was assigned at random. The final study cohort was comprised of 1174 stroke cases and 4696 nonstroke controls (Table 1).
Table 1.
Study Inclusion/Exclusion Criteria and Characteristics of Population Analyzed
| Inclusion/Exclusion criteria | Total patients identified, N=331,204 | Stroke cases identified, n=2336 | Nonstroke controls identified, n=328,868 |
|---|---|---|---|
| Matched for age, gender, admission | 63,729 | 2336 | 61,393 |
| Remaining after missing data exclusion | 60,281 | 2215 | 58,066 |
| Remaining after exclusion for prior stroke | 57,899 | 2014 | 55,885 |
| Within Milwaukee County | 36,369 | 1201 | 35,168 |
| 1:4 matched for race, body mass index, smoking, hypertension, diabetes | 5870 | 1174 | 4696 |
|
| |||
| Characteristic | Total, N=5870 (100%) | Stroke cases, n=1174 (20.0%) | Nonstroke controls, n=4696 (80.0%) |
|
| |||
| Median age | 70.0 years | 70.0 years | 70.0 years |
| Gender, n (%) | |||
| Female | 3111 (53.0) | 622 (53.0) | 2489 (53.0) |
| Male | 2759 (47.0) | 552 (47.0) | 2207 (47.0) |
| Race/Ethnicity, n (%) | |||
| Non-Hispanic White | 4071 (69.4) | 812 (69.2) | 3259 (69.4) |
| Non-Hispanic Black | 933 (15.9) | 186 (15.8) | 747 (15.9) |
| Hispanic | 674 (11.5) | 135 (11.5) | 539 (11.5) |
| Other | 192 (3.3) | 41 (3.5) | 151 (3.2) |
| Admit year, n (%) | |||
| 2016 | 2020 (34.4) | 404 (34.4) | 1616 (34.4) |
| 2017 | 1820 (31.0) | 364 (31.0) | 1456 (31.0) |
| 2018 | 2030 (34.6) | 406 (34.6) | 1624 (34.6) |
| History of smoking, n (%) | 3580 (61.0) | 716 (61.0) | 2864 (61.0) |
| Hypertension, n (%) | 1910 (32.5) | 382 (32.5) | 1528 (32.5) |
| Diabetes, n (%) | 735 (12.5) | 147 (12.5) | 588 (12.5) |
| Median body mass index | 28.0 kg/m2 | 28.1 kg/m2 | 28.0 kg/m2 |
Greenspace by NDVI and Proximity to Public Parks
Residential greenspace exposure was measured in two ways: NDVI uses satellite imagery to determine the amount of greenspace in a particular area and proximity to public parks (PPP) as walking distance on straight line.1 NDVI quantifies the density of green vegetation as a ratio of near-infrared (NIR) light reflected to red light absorbed: NDVI = (NIR – Red)/(NIR + Red). NDVI values range from −1 to +1, with greenness increasing with increased NDVI. The NIR light and red light spectral bands are included with Landsat 8 satellite imagery, available through the U.S. Geological Survey’s Global Visualization Viewer (GloVis, https://glovis.usgs.gov).
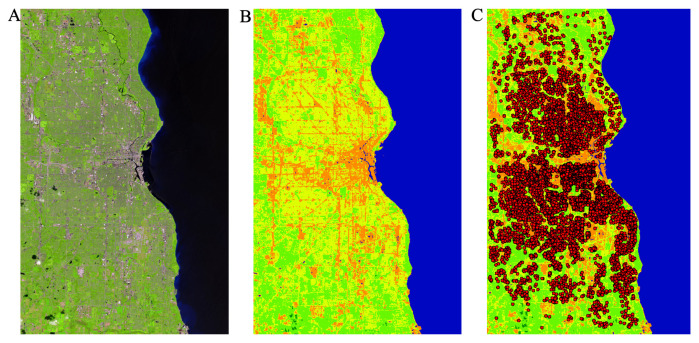
Landsat 8 images (spatial resolution 15 to 100 meters) over Milwaukee County were filtered for May, June, and July (maximal greenness) of 2016, 2017, and 2018 during 0%–20% cloud cover. Satellite images were selected for each of the 3 years based on closest matching dates, then imported into ArcGIS Pro 2.4.1 geospatial mapping software (Esri), and NDVI transformation was performed (Figure 2A, 2B). An XY coordinate layer was added to the NDVI map to permit localization of subjects’ residences. Using the zonal statistics tool, a 250-meter radius was drawn around each residence and the average NDVI within that radius calculated (Figure 2C).
Figure 2.
Determination of residential greenspace. A: Representative Landsat 8 image for Milwaukee County from the U.S. Geological Survey’s Global Visualization Viewer (GloVis). B: The normalized difference vegetation index-transformed satellite image. C: Each circle represents a 250-meter radius surrounding a residence.
Walking distance from a subject’s residence at time of admission to the nearest public park was determined using ArcGIS. In addition to the actual distance in meters, a dichotomous variable was created to identify residences ≤1 km from a public park, and those >1 km from a park.
Area Deprivation Index
The Neighborhood Atlas® is an online tool provided by the University of Wisconsin School of Medicine and Public Health (Madison, WI) that provides the ADI for a particular address, based on American Community Survey Five Year Estimates.17 For our analysis, the 2018 ADI was sourced (https://www.neighborhoodatlas.medicine.wisc.edu/). ADI measures the socioeconomic deprivation within a neighborhood; it uses 17 variables of SES and has been refined and validated to the census block level, defined as the smallest geographic unit used by the U.S. Census Bureau.11 Two ADI scores are available: national percentile rankings from 1 to 100 and rankings in deciles from 1 to 10 for each state. The national percentiles are constructed by ranking the ADI values from low to high for the United States, which are then grouped by neighborhood for each 1% change in ADI. The state deciles are constructed by ranking ADI values from low to high for each state without consideration of national ADI. Higher ADI represents higher levels of deprivation, ie, the more disadvantaged an area.
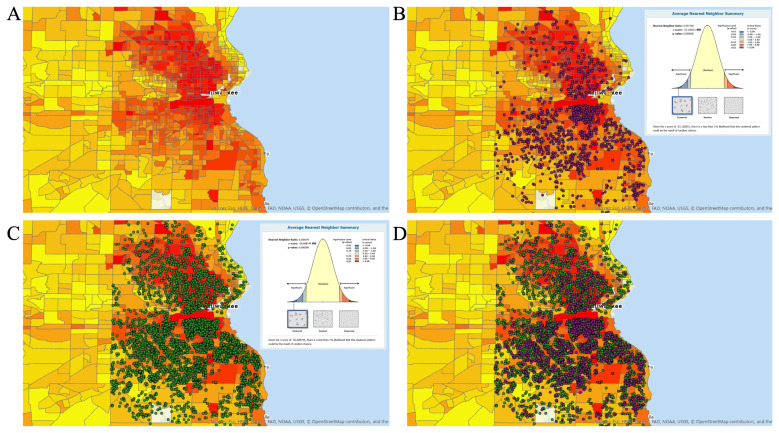
Using the Neighborhood Atlas, state decile and national percentile ADI scores were recorded for each subject and transferred to the ArcGIS map (Figure 3A).
Figure 3.
Visualization of deprivation index and stroke patients. A: The area deprivation index (ADI) for Milwaukee County obtained from the University of Wisconsin Neighborhood Atlas. The darker the color, the more disadvantaged the block group. B: Stroke cases were laid over the ADI map, where each purple dot indicates a stroke case. Inset: results of the Nearest Neighbor summary. C: Controls also were overlaid, with each control shown as a green dot. Inset: results of the Nearest Neighbor summary. D: Comparative ADI map showing both stroke (purple) and control (green) patients.
Geocoding
Sociodemographic information and geocodes for each subject were obtained from ASLMC’s geographic characteristics research database (per IRB no. 15.81) and based on their home address at the time of admission. The geocode included the decimal latitude and longitude and the Federal Information Processing Standard (FIPS) code, a 12-digit number that identifies a street address to its census block level group. ASLMC’s research analytics team created the algorithm and code to convert street addresses to FIPS and to provide a confidence score for each match. Geocodes were used to connect ADI, PPP, and NDVI to each subjects’ residence.
Statistical Methods
Descriptive statistics were applied to demographic variables. Kolmogorov-Smirnov test was used to check the normality of a variable’s distribution. Nonparametric methods were used to compare nonnormally distributed variables. A Spearman’s rank-order correlation was performed to determine the relationship between NDVI, state and national ADI, and PPP. Conditional logistic regression was used to examine relationships between a stroke event and NDVI, state and national ADI, and PPP.
Race (ie, non-Hispanic White [NHW] and non-Hispanic Black [NHB]) and gender differences were compared using a t-test or Mann-Whitney U test as appropriate for the distribution properties of NDVI, ADI state decile, and national ADI percentile. When conducting t-test on groups with unequal variance as determined by Levene’s test, the degrees of freedom were adjusted as appropriate. Ischemic stroke is the most common type of stroke, so we analyzed these patients as a separate subgroup. NDVI was considered as both a continuous and a categorical (by quartiles) variable. ADI percentiles and deciles were considered as continuous and categorical (by quartiles) variables. Multicollinearity was evaluated using the variance inflation factor.
For all statistical tests, an alpha of P<0.05 denoted significance. Statistical analyses were performed using SAS® 9.4 (SAS Institute Inc.); Stata® 15.1 (StateCorp); and R version 3.6.1 (The R Foundation) software.
RESULTS
Characteristics of the study population are summarized in Table 1. The initial matching process identified 63,729 patients (2336 cases and 61,393 potential controls; Figure 1). Following exclusion of cases or controls for missing or poor geographic confidence (n=3327), residence outside Milwaukee County (n=20,717), a prior history of stroke (n=2181), and proximity to a water feature, there were 1201 stroke cases and 35,168 controls. Upon completion of 1:4 matching, the study cohort comprised 1174 cases and 4696 controls. There were 27 unmatched cases — 18 patients with stroke were missing body mass index data, 8 were missing race data, and 1 was missing both (Table 1, Online Supplemental Figure S1, and Online Supplemental Table S1). Unmatched cases were not included in the analysis.
Following the analysis of overall stroke cases, we determined whether there was an association between greenspace and ischemic stroke. After determining geographic distribution, stroke cases (Figure 3B, purple dots) and nonstroke controls (Figure 3C, green dots) were plotted using the average nearest neighbor tool in ArcGIS. An overlay of the cases and controls (Figure 3D) found that both the nonstroke patients and patients with stroke were clustered rather than randomly distributed throughout the county (Figure 3, insets).
Relationship Between Greenspace and Sociodemographic Variables
Of the greenspace and sociodemographic variables tested, only NDVI was normally distributed. Therefore, Spearman’s rank-order correlation determined the relationship between NDVI, ADI state decile, national ADI percentile, and PPP (Online Supplemental Table S2). There was a strong positive correlation between the ADI state decile and ADI national percentile (rs(5870)=0.992; P<0.001), indicating that these two measurements were consistent with one another. There was a weakly positive correlation between PPP and both the ADI state decile (r(5870)=0.092; P<0.001) and national ADI percentile (r(5870)=0.085; P<0.001). This indicates that the further away from a public park, the greater the neighborhood disadvantage (ie, higher ADI). There were moderate negative correlations between NDVI and the ADI state decile (rs(5870)=−0.550; P<0.001) and national ADI percentile (rs(5870)=−0.548; P<0.001). This indicates that increased greenspace (ie, higher NDVI) correlates, at least modestly, with lower neighborhood deprivation.
Relationships Among NDVI, ADI, Gender, and Race
No difference was detected in NDVI values between males (mean ± standard deviation [SD]: 0.28 ± 0.06) and females (0.28 ± 0.06); t(5712)=0.16; P=0.874; d=0.004. Similarly, there was no detectable difference in either the median ADI state deciles (P=0.1450) nor the median national ADI percentiles (P=0.1535) for males and females.
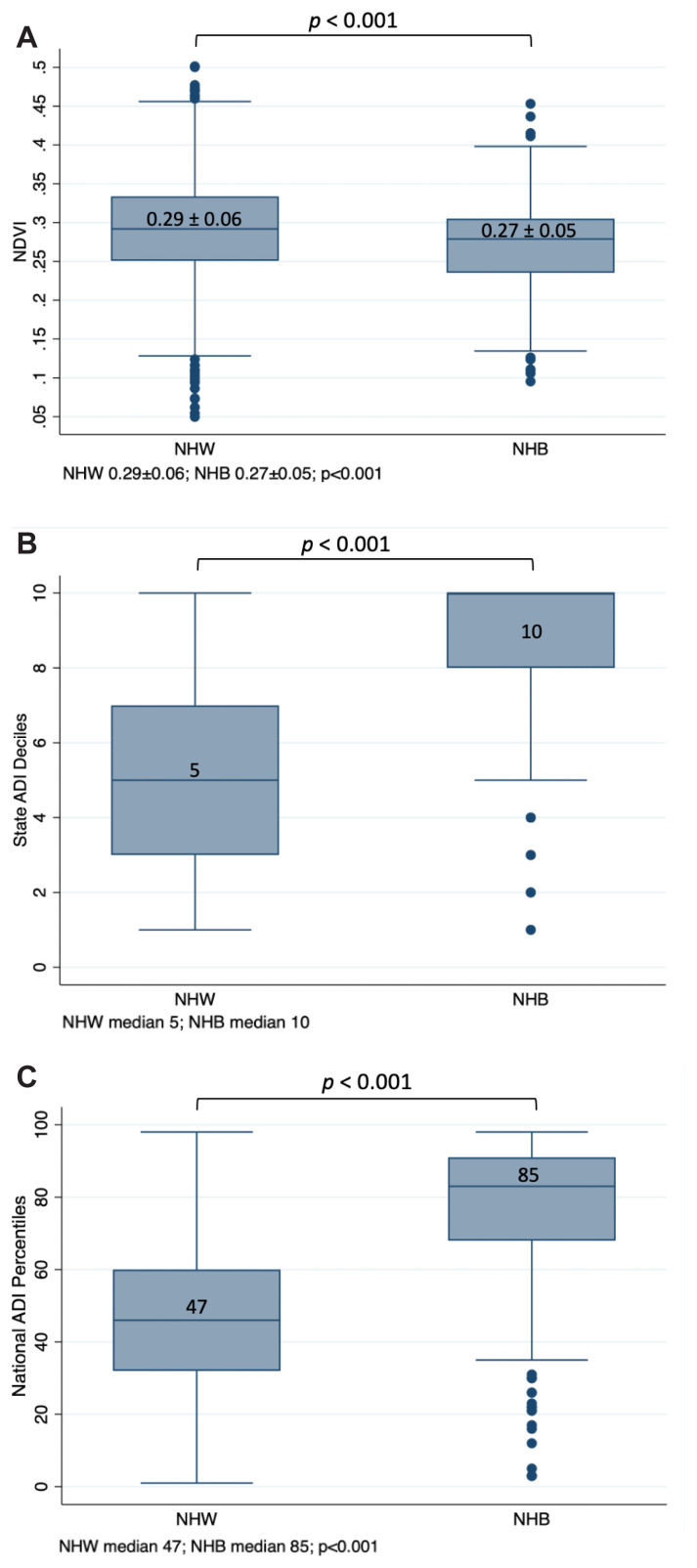
The relationship between greenspace and race was analyzed. Mean residential NDVI values were significantly lower for NHB patients (0.27 ± 0.05) than for NHW patients (0.29 ± 0.06), indicating NHB patients lived in less green areas than NHW patients (t[1569]=10.07; P<0.001; d=0.37) (Figure 4A). As Levene’s test indicated unequal variances (F=29.80; P<0.001), the degrees of freedom were adjusted from 5002 to 1569.
Figure 4.
Racial disparity and greenspace. A: Analysis of the relationship between race and greenspace (as NDVI). State ADI (B) and national ADI (C) stratified by race. P-values are shown below each graph. ADI, area deprivation index; NDVI, normalized difference vegetation index; NHB, non-Hispanic Black; NHW, non-Hispanic White.
Deprivation scores (both state and national) also were compared by race. ADI state decile scores were higher for NHB patients (median: 10, interquartile range [IQR]: 1) than for NHW patients (median: 5, IQR: 5), indicating that NHB patients lived in neighborhoods with higher levels of disadvantage (U=514,124; z=−35.03; P<0.001; r=0.50) (Figure 4B). The national ADI percentile scores also were higher for NHB patients (median: 85, IQR: 21) than for NHW patients (median: 47, IQR: 23), confirming the observation of disadvantage seen at the state level (U=488,654; z=−35.44; P<0.001, r=0.50) (Figure 4C). Thus, in Milwaukee County, NHB patients were more likely to live in areas of greater deprivation and lower greenspace than NHW patients.
NDVI and All Stroke Cases
Mean NDVI was higher for nonstroke controls (0.283 ± 0.062) than for stroke cases (0.279 ± 0.062; P=0.057). On conditional logistic regression, there was an inverse relationship between NDVI and stroke: as NDVI increased, the odds of stroke decreased (OR: 0.33, 95% CI: 0.111–0.975; P=0.045) (Table 2). For analysis of the relationship with a stroke event, NDVI values were grouped into categorical quartiles, then evaluated using conditional logistic regression. The odds of stroke were 19% lower for patients living in areas with the highest level of greenspace (highest NDVI quartile) compared to those patients living in the areas with the least amount of greenspace (lowest NDVI quartile) (OR: 0.81, 95% CI: 0.672–0.984; P=0.034).
Table 2.
Analysis of Associations Between a Stroke Event, Greenspace, and Area Deprivation
| Total, N=5870 | Stroke cases, n=1174 (20.0%) | Nonstroke controls, n=4696 (80.0%) | Univariate odds ratio (95% CI) | P | |
|---|---|---|---|---|---|
| Mean NDVI (SD) | 0.282 (0.06) | 0.279 (0.06) | 0.282 (0.06) | 0.33 (0.111–0.975) | 0.045 |
| NDVI quartiles,* n | |||||
| 2 | 1467 | 295 | 1172 | 0.92 (0.76–1.10) | 0.344 |
| 3 | 1468 | 295 | 1173 | 0.91 (0.76–1.10) | 0.321 |
| 4 (highest) | 1467 | 270 | 1197 | 0.81 (0.67–0.98) | 0.034 |
| Mean ADI National percentile (SD) | 54.0 (36.0) | 54.0 (34.0) | 53.0 (37.0) | 1.00 (0.998–1.005) | 0.274 |
| ADI National quartiles,* n | |||||
| 2 | 1502 | 323 | 1179 | 1.23 (1.03–1.47) | 0.023 |
| 3 | 1424 | 286 | 1138 | 1.14 (0.95–1.38) | 0.165 |
| 4 (highest) | 1410 | 284 | 1126 | 1.16 (0.93–1.44) | 0.187 |
| Mean ADI State decile (SD) | 6.0 (5.0) | 6.0 (5.0) | 6.0 (6.0) | 1.01 (0.985–1.038) | 0.392 |
| ADI State quartiles,* n | |||||
| 2 | 1375 | 292 | 1083 | 1.18 (0.98–1.41) | 0.075 |
| 3 | 1688 | 321 | 1367 | 1.05 (0.88–1.26) | 0.576 |
| 4 (highest) | 1146 | 249 | 897 | 1.28 (1.02–1.60) | 0.029 |
| Median proximity to public parks (IQR) | 606.3 (593.5) | 583.4 (606.8) | 613.1 (590.0) | 1.00 (1.00–1.00) | 0.456 |
| Resides within 1 km of a park, n (%) | 4580 (78.0) | 911 (77.6) | 3669 (78.1) | 1.03 (0.885–1.202) | 0.694 |
Compared to lowest quartile.
ADI, area deprivation index; IQR, interquartile range; NDVI, normalized difference vegetation index; SD, standard deviation.
NDVI values were rescaled using IQR for a more intuitive interpretation, and the IQR-rescaled predictor was achieved by dividing NDVI by its IQR (0.08). Conditional logistic regression was used to examine the relationship between a stroke event and NDVI scaled by IQR while taking matching into account. For 1 IQR increase in NDVI, there was an 8% decrease in the odds of stroke (OR: 0.92, 95% CI: 0.839–0.998; P=0.045).
ADI, PPP, and Stroke
Neither the ADI state decile nor national ADI percentile for stroke cases versus controls were significantly different (Table 2) as analyzed by Mann-Whitney (6 vs 6 [P=0.501] and 53 vs 54 [P=0.360], respectively). Additional analysis indicated that odds of stroke also did not significantly differ (OR: 1.01, 95% CI: 0.985–1.038 [P=0.392] and OR: 1.00, 95% CI: 0.998–1.005 [P=0.274], respectively). The national ADI percentiles and ADI state deciles were categorized into quartiles for direct comparison. Conditional logistic regression determined that patients living in the second highest national ADI quartile had odds of stroke that were 23% higher than those living in the lowest national ADI percentile (OR: 1.23, 95% CI: 1.029–1.474; P=0.023). Also, patients living in the highest quartile of state ADI (most disadvantage) had 28% higher odds of stroke compared to those living in the lowest quartile (ie, least disadvantaged) neighborhoods (OR: 1.28, 95% CI: 1.02–1.6; P=0.029).
No difference was found in the odds of stroke associated with the distance (in meters) from a patient’s residence to a public park (OR: 1.00, 95% CI: 1.000–1.000; P=0.456) (Table 2). In addition, residing within 1 km walking distance of a park (yes/no) was not associated with the odds of a stroke event (OR: 1.03, 95% CI: 0.885–1.202; P=0.694). Therefore, although residential greenspace was associated with stroke, distance to a public park was not.
Ischemic Stroke Subgroup
To exam the interplay between greenspace, deprivation, and ischemic stroke, a subgroup of patients with ischemic stroke were identified within the original stroke case population. This subgroup included 830 ischemic stroke cases and 3320 matched controls (for a total of 4150 patients). Conditional logistic regression determined relationships between and ischemic stroke event and NDVI, national ADI, or state ADI. All conditional analyses were stratified on the matching criteria, and each predictor was analyzed individually. No statistical differences were detected in NDVI (OR: 0.32, 95% CI: 0.088–1.178; P=0.087;), national ADI percentile (OR: 1.0, 95% CI: 0.999–1.007; P=0.177), or ADI state decile (OR: 1.02, 95% CI: 0.988–1.052; P=0.238).
Interaction Between NDVI and ADI
To determine if NDVI was simply a proxy for ADI, univariate and multivariate conditional logistic regression models were compared. The similarity of the regression coefficients for NDVI when used in a multivariate model with state or national ADI and when used in a univariate model were well within each other’s confidence intervals, suggesting that NDVI was not simply a proxy for ADI. No significant interaction between NDVI and state or national ADI was detectable (Online Supplemental Tables S3 and S4). Variance inflation was used to estimate the extent of multicollinearity. The variance inflation factor was 3.44 for NDVI and state ADI and 4.30 for NDVI and national ADI. These values indicate moderate collinearity and no adverse effect on the regression model.
DISCUSSION
In this study, we asked if residential greenspace (as measured by NDVI) and neighborhood disadvantage (as measured by ADI) were related to stroke risk in Milwaukee County, Wisconsin. We found that there was an inverse relationship between NDVI and stroke. Specifically, the odds of stroke decreased with increasing greenness: people living in the greenest quartile had 19% lower odds of stroke than people living in the least green quartile. Additionally, patients living in the most disadvantaged ADI state quartile had 28% higher odds of stroke compared to patients living in the least disadvantaged state quartile, consistent with previous reports on the association between neighborhood SES and stroke incidence.9 Interestingly, a study out of the University of Miami presented at the 2021 International Stroke Conference analyzed Medicare records and found a reduction in ischemic stroke with increased greenness.18
The mechanism(s) by which residential greenspace exposure contributes to positive health outcomes is unsettled but may include its modifying the microclimate by absorbing solar radiation and air pollutants, enhancing air quality,19 buffering wind and noise,4 and reducing heat.20 Greenspaces can also promote physical activity and social contact.21 The former mitigates the effects of a sedentary lifestyle such as obesity and hypertension; the latter contributes to wellness through decreased mental stress.17,22 Whatever the mechanism(s) of action, positive health benefits of greenspace exposure are myriad. A study on the relationship between residential greenspace, PPP, and pregnancy outcomes in Lithuania found that subjects who lived in areas with low surrounding greenness and those who were further from a park were at increased risk for term low birth weight and preterm birth.23 In Hong Kong, a 10% increase in greenspace was significantly associated with a reduction in all-cause mortality, circulatory system-caused mortality, and stroke-caused mortality, independent of variables age, sex, marital status, education level, SES, smoking, and alcohol intake.4 In a cross-sectional study from the University of Louisville, residential greenness was associated with lower levels of sympathetic activation, reduced oxidative stress, and higher angiogenic capacity, again, independent of age, sex, race, ADI, and statin use.22 A multicase-control study from Spain found that the risk of breast cancer was reduced among participants who had urban green areas within 300 meters of their residence compared to those with no urban green areas within that distance.7
With the novel findings from our study, stroke risk can now be added to the growing list of health issues impacted by residential greenspace. Our data also confirmed neighborhood disadvantage as a risk factor for stroke, further suggesting the environment in which we live is an independent risk factor for stroke after controlling for individual characteristics. This is important from a public health perspective. Greenspace is a readily modifiable environmental factor that should be protected and expanded in the face of relentless urbanization. Modifying neighborhood disadvantage, though more challenging, also should be considered as a means to improve health in general and decrease stroke risk in particular.
Limitations
The mechanism of action establishing greenspace as a mitigating factor for stroke risk is not known. Proposed causal pathways such as improved air quality, increased physical activity, improved social contact, and stress reduction were not evaluated in this study. Dose and duration of greenspace exposure needed to impact health outcomes are not known. The research team did not have a mechanism to quantify length of time a patient has lived at a particular address. We also could not measure the extent of greenspace exposure outside the home — at work or school, for example. Lastly, Milwaukee’s extreme segregation may be associated with independent health risks; segregation has been shown to be associated with poor birth outcomes, health behaviors, and chronic diseases,24,25 and its relationship to stroke risk warrants further study.
CONCLUSIONS
Residential greenspace correlates to stroke risk, with patients who live amidst the most greenspace significantly less likely to have a stroke event than those surrounded by the least greenspace. Similarly to, but independently of, greenspace, patients from Milwaukee County’s most socioeconomically disadvantaged neighborhoods were significantly more likely to have stroke than those residing in its least deprived neighborhoods. These findings stress the influence of environment as a risk factor for stroke.
Patient-Friendly Recap.
Residing in an area with ample greenspace has been associated with more favorable patient outcomes following stroke.
Using a study design that controlled for other variables by matching cases (patients with stroke) to controls (nonstroke patients) from a high-volume hospital, authors investigated if lack of residential greenspace within urban Milwaukee County was associated with likelihood of having a stroke.
Both lack of greenspace and low socioeconomic status pertaining to a patient’s residential surroundings correlated to higher risk of stroke.
The environment in which we live can be viewed as an independent risk factor for stroke.
Supplementary Information
Acknowledgments
The authors thank Gary Dennison for his expert guidance through the regulatory process; Andrew Marek, Jonathon Cook, and David Triscari for IT support; and Dr. Jennifer Jacob for editorial assistance and manuscript preparation. The authors also thank Dr. Clyde Schechter for insights into the interaction between normalized difference vegetation index and area deprivation index.
Footnotes
Author Contributions
Study design: Cheruvalath, Vilar, Kassam, Rovin. Data acquisition or analysis: Cheruvalath, Homa, Singh, Rovin. Manuscript drafting: Homa, Rovin. Critical revision: Rovin.
Conflicts of Interest
None.
References
- 1.Lee AC, Maheswaran R. The health benefits of urban green spaces: a review of the evidence. J Public Health (Oxf) 2011;33:212–22. doi: 10.1093/pubmed/fdq068. [DOI] [PubMed] [Google Scholar]
- 2.Kondo MC, Fluehr JM, McKeon T, Branas CC. Urban green space and its impact on human health. Int J Environ Res Public Health. 2018;15(3):445. doi: 10.3390/ijerph15030445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pereira G, Foster S, Martin K, et al. The association between neighborhood greenness and cardiovascular disease: an observational study. BMC Public Health. 2012;12:466. doi: 10.1186/1471-2458-12-466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang D, Lau KK, Yu R, Wong SY, Kwok TT, Woo J. Neighbouring green space and mortality in community-dwelling elderly Hong Kong Chinese: a cohort study. BMJ Open. 2017;7(7):e015794. doi: 10.1136/bmjopen-2016-015794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wilker EH, Wu CD, McNeely E, et al. Green space and mortality following ischemic stroke. Environ Res. 2014;133:42–8. doi: 10.1016/j.envres.2014.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Villeneuve PJ, Jerrett M, Su JG, et al. A cohort study relating urban green space with mortality in Ontario, Canada. Environ Res. 2012;115:51–8. doi: 10.1016/j.envres.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 7.O’Callaghan-Gordo C, Kogevinas M, Cirach M, et al. Residential proximity to green spaces and breast cancer risk: the multicase-control study in Spain (MCC-Spain) Int J Hyg Environ Health. 2018;221:1097–106. doi: 10.1016/j.ijheh.2018.07.014. [DOI] [PubMed] [Google Scholar]
- 8.Kim Y, Twardzik E, Judd SE, Colabianchi N. Neighborhood socioeconomic status and stroke incidence: a systematic review. Neurology. 2021;96:897–907. doi: 10.1212/wnl.0000000000011892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marshall IJ, Wang Y, Crichton S, McKevitt C, Rudd AG, Wolfe CD. The effects of socioeconomic status on stroke risk and outcomes. Lancet Neurol. 2015;14:1206–18. doi: 10.1016/s1474-4422(15)00200-8. [DOI] [PubMed] [Google Scholar]
- 10.Vivanco-Hidalgo RM, Avellaneda-Gomez C, Dadvand P, et al. Association of residential air pollution, noise, and greenspace with initial ischemic stroke severity. Environ Res. 2019;179(Pt A):108725. doi: 10.1016/j.envres.2019.108725. [DOI] [PubMed] [Google Scholar]
- 11.Kind AJH, Buckingham WR. Making neighborhood-disadvantage metrics accessible - the Neighborhood Atlas. N Engl J Med. 2018;378(26):2456–2458. doi: 10.1056/nejmp1802313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Linden A, Samuels SJ. Using balance statistics to determine the optimal number of controls in matching studies. J Eval Clin Pract. 2013;19:968–75. doi: 10.1111/jep.12072. [DOI] [PubMed] [Google Scholar]
- 13.Tenny S, Kerndt CC, Hoffman MR. StatPearls [Internet] StatPearls Publishing; 2021. Jul 9, Case control studies. [Google Scholar]
- 14.Bray BD, Paley L, Hoffman A, et al. Socioeconomic disparities in first stroke incidence, quality of care, and survival: a nationwide registry-based cohort study of 44 million adults in England. Lancet Public Health. 2018;3:e185–93. doi: 10.1016/s2468-2667(18)30030-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Howard VJ, McClure LA, Kleindorfer DO, et al. Neighborhood socioeconomic index and stroke incidence in a national cohort of blacks and whites. Neurology. 2016;87:2340–7. doi: 10.1212/wnl.0000000000003299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.White MP, Alcock I, Wheeler BW, Depledge MH. Coastal proximity, health and well-being: results from a longitudinal panel survey. Health Place. 2013;23:97–103. doi: 10.1016/j.healthplace.2013.05.006. [DOI] [PubMed] [Google Scholar]
- 17.Klinenberg E. Palaces for the People: How Social Infrastructure Can Help Fight Inequality, Polarization, and the Decline of Civic Life. Crown. 2018 [Google Scholar]
- 18.Brown SC, Aitken W, Lombard J, et al. The relationship of neighborhood greenness to stroke/transient ischemic attack in 249,405 US Medicare beneficiaries. (abstr.) Stroke. 2021;52(Suppl_1):AP631. doi: 10.1161/str.52.suppl_1.P631. [DOI] [Google Scholar]
- 19.Kim D, Ahn Y. The contribution of neighborhood tree and greenspace to asthma emergency room visits: an application of advanced spatial data in Los Angeles County. Int J Environ Res Public Health. 2021;18(7):3487. doi: 10.3390/ijerph18073487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Heo S, Chen C, Kim H, et al. Temporal changes in associations between high temperature and hospitalizations by greenspace: analysis in the Medicare population in 40 U.S. northeast counties. Environ Int. 2021;156:106737. doi: 10.1016/j.envint.2021.106737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhou Y, von Lengerke T, Dreier M. Comparing different data sources by examining the associations between surrounding greenspace and children’s weight status. Int J Health Geogr. 2021;20(1):24. doi: 10.1186/s12942-021-00278-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yeager R, Riggs DW, DeJarnett N, et al. Association between residential greenness and cardiovascular disease risk. J Am Heart Assoc. 2018;7(24):e009117. doi: 10.1161/jaha.118.009117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grazuleviciene R, Danileviciute A, Dedele A, et al. Surrounding greenness, proximity to city parks and pregnancy outcomes in Kaunas cohort study. Int J Hyg Environ Health. 2015;218:358–65. doi: 10.1016/j.ijheh.2015.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Landrine H, Corral I. Separate and unequal: residential segregation and black health disparities. Ethn Dis. 2009;19:179–84. [PubMed] [Google Scholar]
- 25.Baxter SL, Chung R, Frerichs L, Thorpe RJ, Jr, Skinner AC, Weinberger M. Racial residential segregation and race differences in ideal cardiovascular health among young men. Int J Environ Res Public Health. 2021;18(15):7755. doi: 10.3390/ijerph18157755. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.