Abstract
Introduction
The COVID-19 pandemic has placed health care workers at unprecedented risk of stress, burnout, and moral injury. This paper describes the design of an ongoing cluster randomized controlled trial to compare the effectiveness of Stress First Aid (SFA) to Usual Care (UC) in protecting the well-being of frontline health care workers.
Methods
We plan to recruit a diverse set of hospitals and health centers (eight matched pairs of hospitals and six pairs of centers), with a goal of approximately 50 HCW per health center and 170 per hospital. Participating sites in each pair are randomly assigned to SFA or UC (i.e., whatever psychosocial support is currently being received by HCW). Each site identified a leader to provide organizational support of the study; SFA sites also identified at least one champion to be trained in the intervention. Using a “train the trainer” model, champions in turn trained their peers in selected HCW teams or units to implement SFA over an eight-week period. We surveyed HCW before and after the implementation period. The primary outcomes are posttraumatic stress disorder and general psychological distress; secondary outcomes include depression and anxiety symptoms, sleep problems, social functioning problems, burnout, moral distress, and resilience. In addition, through in-depth qualitative interviews with leaders, champions, and HCW, we assessed the implementation of SFA, including acceptability, feasibility, and uptake.
Discussion
Results from this study will provide initial evidence for the application of SFA to support HCW well-being during a pandemic.
Trial registration: (Clinicaltrials.govNCT04723576).
Keywords: COVID-19, Stress, Mental health, Healthcare workers
1. Introduction
The COVID-19 pandemic is the most challenging public health crisis of our time. Health care workers (HCW) in particular are facing unprecedented stressors and are at high risk of not only COVID-19 infection but also of psychological distress during the pandemic [[1], [2], [3]]. Systematic reviews summarizing evidence across countries indicate significant and wide-ranging mental health consequences for HCW during COVID-19, including depression, anxiety, insomnia, acute stress disorder, posttraumatic stress disorder, psychological distress, and burnout [2,[4], [5], [6], [7], [8]]. About one in four HCW have reported clinically elevated anxiety and depression during the COVID-19 pandemic [8]. In a survey conducted in the United States in 2020, significant rates of psychological problems were reported, including probable major depression, anxiety, posttraumatic stress disorder (PTSD), and alcohol use problems [6]. Lower team cohesion and difficulty following the hospital policies (to limit nosocomial COVID-19 transmission) were associated with greater PTSD symptoms and major depressive symptoms, respectively [6]. Exposure to viral outbreak may have a long-lasting mental health impact on HCW years after the outbreak [[9], [10], [11], [12], [13]]. Adequate psychological support is critical for HCW well-being during and after a pandemic that place increased risk and demand on the health care system.
HCW well-being also has a significant effect on patient experiences of care. Pre-pandemic studies showed that HCW with burnout have lower productivity, more self-reported medical errors, lower quality of care, and worse relationships with their patients. Protecting and supporting HCW mental well-being will likely benefit patients for receiving higher quality care and ensuring the stability of patients' access to care given the concerns for attrition due to burnout. Additionally, the quadruple aim of healthcare now includes healthcare team well-being as a dimension for improving population health and the patient experience [14].
Despite the threat to HCW well-being and the potential cascading effects on patient care, interventions to protect HCW well-being during disease outbreaks or other disasters are scarce. Only one uncontrolled study from Taiwan reported that a SARS prevention program for nursing staff (e.g., access to mental health team, limiting shift hours, providing PPE) showed promise for reducing depression and anxiety [15]. Implementing an intervention to support HCW is an urgent public health need during COVID-19 and for the future.
Stress First Aid (SFA) is a promising evidence-informed intervention [[16], [17], [18], [19], [20], [21], [22]] to mitigate the psychological impact of the chronic stress during the COVID-19 on HCW. This cluster randomized controlled trial (cRCT) will assess the effect of SFA tailored for HCW compared to Usual Care (UC) on the mental and physical well-being of HCW during the COVID-19 pandemic through three aims. In Aim 1, we will test the comparative effectiveness of SFA versus UC on mental and physical well-being through quantitative data collection. In Aim 2, we will document the landscape of existing UC activities to support HCW well-being prior to implementing SFA across sites through qualitative data collection. In Aim 3, we will assess the experiences of HCW and in sites with SFA (acceptability, uptake, lessons learned) and impact on HCW well-being through qualitative data collection.
2. Methods
2.1. Design overview
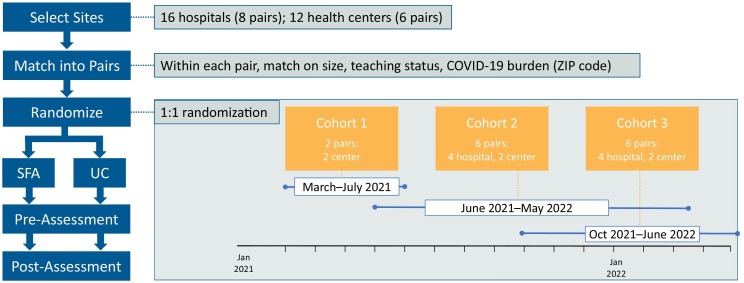
Fig. 1 shows the study sampling design and recruitment approach. The current study uses a mixed methods approach that includes a quantitative component (Aim 1) designed as a cRCT and a qualitative component (Aims 2 & 3) designed as a complementary descriptive study. The qualitative and quantitative data are being collected simultaneously and data analyses will be conducted simultaneously by separate teams [23]. The quantitative data are collected for the primary purpose of confirmation or hypothesis testing. The qualitative data will be used to corroborate the quantitative findings and to generate explanatory models for variation in the quantitative findings.
Fig. 1.
Sampling design and recruitment approach
The cRCT is comprised of three cohorts of matched pairs representing approximately 28 diverse sites (eight pairs of hospitals and six pairs of health centers) to determine whether SFA for frontline HCW improves mental and physical well-being compared to Usual Care (UC). Sequential roll-out of the SFA intervention in three cohorts allows for feedback from each cohort to be integrated into subsequent cohorts and also provides different “snapshots” over the course of the pandemic. Each recruited site involves leadership (executive level leaders to support and endorse the project) and HCW. Under a “train-the-trainer” model, intervention sites implementing SFA also have clinical champions who train their peers in the SFA model and the integration of its seven core actions into their daily routines over an eight-week period.
To collect data for this study, we will administer a web-based survey to HCW at all sites before and after the intervention period. In addition, we will conduct interviews with all site leaders before and after the intervention period; and with champions (intervention sites only) and a sub-sample of HCW (intervention and control sites) after the intervention period.
2.2. Recruitment, study settings, and target population
Recruitment of participating sites is being conducted through partnership with Vizient Inc. and Clinical Directors Network (CDN). Vizient is a member-owned health care performance improvement organization serving more than half of all health care organizations across the country from which we will recruit eight pairs of hospitals. Vizient will recruit members from their organization using targeted emails, existing communication channels, and telephone outreach to key site leaders, supplemented by a live webinar (which is recorded and posted for members). CDN is a practice-based research network (PBRN) and AHRQ-designated Center of Excellence (P30) for practice-based research and learning, from which we plan to recruit six pairs of Federally Qualified Health Centers (FQHCs). CDN is reaching out to centers directly, using its extensive listserv of FQHC and primary care clinical leaders and clinicians. Recruitment is purposive to ensure some geographic and academic status diversity. Each recruited site is matched on size, type (i.e., hospital or outpatient clinic/center), geography, and COVID-19 case rates at the time of intervention start; sites must have an appropriate match to participate. For hospitals and health centers, matched sites can be within the same health system if appropriately independent of each other (i.e., organizationally and geographically distinct enough to avoid contamination, including no sharing of clinicians), or from two different systems.
Once matched, each site is asked to identify at least one site leader; intervention sites also identified site champions (at least one champion per every 50 HCW planned to receive the intervention), and the HCW team(s) or unit(s) that will receive the SFA intervention (e.g., emergency department, intensive care unit, general floors, specialty services) with input from both the site leaders and champions. UC sites must include the same teams/units as their matched intervention site. The role of the site leaders is to provide the study team with a birds-eye view of operations at the site, including the typical supports and resources the organization or system provides to maintain health care worker well-being. Site leaders are likely to be executive leadership (e.g., Chief Medical Officers, Chief Quality Officers, Chief Nursing Officers), given their knowledge of operations. The role of the site champions at the intervention sites is to train HCW teams in the SFA intervention, provide support as HCW begin to use the model in their daily practice, and provide the study team with information regarding the implementation of SFA at their site, including barriers and facilitators. The champions have some flexibility in how the training will be implemented to ensure that local context and other important factors are considered.
Each hospital aims to recruit an average of 170 HCW. Each FQHC aims to recruit an average of 50 HCW. Site champions and participating HCW in the SFA sites will receive continuing education (CE) credits as an incentive to participate in the SFA training. HCW at UC sites do not receive SFA or CE, but champions at UC sites are offered early access training as soon as the study evaluation is completed and can then train their HCW locally. All HCW participants are provided a $25 gift card per completed survey. HCW in the subsample who complete a post-intervention interview are provided a $50 gift card. All gift cards are delivered electronically.
2.3. Inclusion and exclusion criteria
For participating sites, leadership at the recruited sites must commit to supporting the effort, including survey endorsement, encouragement, and protecting time for all trainings. Participating sites can either agree to cede to RAND IRB or provide their own IRB approval in a timely fashion.
For participants of the SFA intervention, among ambulatory centers, both HCW and supporting staff who are patient-facing (e.g., front desk staff) are eligible to participate; among hospitals, only HCW are eligible to participate, and can be spread across multiple teams or units.
2.4. Randomization
Before randomizing, we match sites into pairs for each of the three cohorts based on the following characteristics: 1) size (number of beds for hospitals & number of patients for health centers); 2) type (teaching vs. non-teaching); 3) COVID-19 burden (e.g., case rates using zip code or city as a proxy), and 4) region (i.e., census region) [24]. Each pair is then assigned to either SFA or UC using a simple 1:1 randomization.
For each matched pair of sites, the site randomized (see below) to the SFA intervention first selects their sample of participating HCW; the UC site is then asked to select a similar sample (e.g., to include the same types of providers, in hospitals to select the same department or clinical unit).
2.5. Assessment
We are conducting a quantitative assessment (Aim 1) via an online survey of HCW that captures the primary and secondary outcomes of the study before and after the intervention period at all sites (i.e., intervention and UC sites). We are conducting qualitative interviews (Aims 2 & 3) for HCW (all sites), site champions (intervention sites only), and site leaders (all sites)
2.6. Stress first aid (SFA)
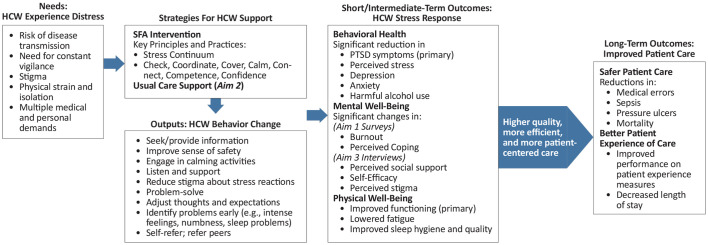
Fig. 2 shows the logic model of SFA for HCW. SFA was initially developed for the United States Navy and Marine Corps [[25], [26], [27]] as a framework of actions for peer support delivered by individuals without mental health training, with a goal of mediating and mitigating impacts in atypically stressful circumstances. It was not designed to prevent any particular disorder, but to enhance individual and system capacity to weather and withstand adversity. SFA has been adapted for use in a variety of high-risk occupations, such as firefighters and emergency medical services personnel [19]. In the current study, the adaptation of the SFA manual is based on the SFA manual developed in VA to meet the specific needs among HCW during the COVID-19 pandemic [28]
Fig. 2.
Logic model for role of SFA in HCW and patient well-being
SFA is designed to teach simple, supportive actions that can be seamlessly integrated into the health care environment for HCW self-care and to help HCW support patients and families (Fig. 2). SFA training focuses on seven core actions: check (assess the situation: observe or listen), coordinate (get help, refer as needed), cover (restore and support a sense of safety), calm (encourage simple strategies such as breathing), connect (engage in and promote social support), competence (improve ability to address crucial needs and concerns), and confidence (increase hope and limit self-doubt and guilt). SFA is an excellent candidate for a rapid deployment and it is actionable and generalizable to different settings and HCW types in a variety of roles during COVID-19
We are implementing SFA using a “train-the trainer” model. From intervention sites, we identify at least one champion per every 50 HCW planned to receive the SFA intervention (this number is based on general expectations regarding needs for cross-coverage and sustainability). Site champions participate in a two-hour virtual live SFA training delivered by Dr. Patricia Watson, the developer of the SFA model, which also includes time to develop their plans for implementing SFA locally. Prior to this training, they are asked to review four hours of training videos on SFA covering each principle in detail, an implementation handbook describing ways to deliver SFA to HCW teams and sustain the integration of SFA into daily practice, and all materials they would use in delivering SFA to their teams (e.g., training slide decks, handouts, and workbooks). Champions are also provided with more in-depth SFA training manuals and slides from the National Center for PTSD for reference. Once trained, the champions implement their training plan at their organizations for their HCW peers
2.7. Usual care (UC)
UC condition in this study refers to any programs already in place (or not in place) to support HCW during and beyond the COVID-19 pandemic. While the intervention sites implement SFA, the control sites simply continue whatever constitutes UC. The control sites are asked only to support the survey of HCW in analogous teams/units and timeline compared to their paired intervention site. For example, if the intervention site is implementing SFA among all nurses in their ICUs, the control sites are asked to field the survey to all nurses in their ICUs. While we cannot anticipate the specific types of programs or interventions implemented in UC sites, any existing interventions at UC sites could dampen the detection of the effect of the SFA intervention [29]. Therefore, in Aim 2, we collect qualitative data to document the types of activities being implemented before and after the SFA intervention and conduct post-hoc analyses to further examine variation across sites in comparing SFA with UC. All UC sites have the opportunity to identify champions to take the SFA training once the evaluation is complete so that they can train their HCW in turn. SFA training and materials are also provided at the end of the study
3. Quantitative assessment and measures
A brief online survey of HCW is conducted pre- and post-intervention in both SFA and UC conditions. Each survey has about 85 items and takes about 15 min to complete. A full list of primary, secondary, and other outcome measures collected through survey is shown in Table 1
Table 1.
Primary and secondary outcomes from quantitative/survey data.
| Measure | Description |
|---|---|
| Primary Outcomes (survey) | |
| Posttraumatic Stress Checklist (PCL-5) | DSM-5 measure of PTSD symptoms rated on 0–4 frequency scale |
| Kessler 6 (K-6) | General psychological distress |
| Secondary Outcomes (survey) | |
| PROMIS Sleep Related Impairment | PROMIS-SRI short form; items rated on a 1–5 scale from not at all to very much |
| Workplace stress | American Psychological Association's Stress in the Workplace survey; items rated on a 1–5 scale from strongly disagree to strongly agree |
| Burnout | Dolan single item burnout inventory; participants choose the description of burnout level that reflects their experience |
| Connor-Davidson Resilience Scale (CD-RISC-2) | Brief version the CD-RISC; items rated on a 1–5 scale from not true at all to true nearly all the time |
| Moral Distress Thermometer | Sliding scale with responses rated on a 0–10 scale from none to worst possible |
| Health Care Worker Characteristics (survey) | |
| COVID-19 Experience | Adapted from other COVID-19 surveys (e.g., American Life Panel, NIH, relevant literature) |
| Demographics | Age, gender, race, ethnicity |
| Professional Characteristics | Provider type, years working at hospital/clinic |
| SFA Evaluation (survey; SFA condition only) | |
| HCW's experience with SFA | Attendance |
| Secondary Patient Outcomes (secondary data) | |
| Patient quality and safety measures | Mortality, avoidable safety events (e.g., sepsis, pressure ulcers) |
| Patient experience of care | Patient experience: HCAHPS and length of stay for hospitals and CG-CAHPS for FQHCs, |
3.1. Primary outcomes
There are two primary outcomes: acute distress (i.e., PTSD symptoms) measured using the Posttraumatic Stress Disorder Checklist (PCL-5) [30] and chronic symptoms of psychological distress measured using Kessler 6 (K-6) [31]. The PCL-5 is a 20-item self-report measure that assesses the 20 DSM-5 symptoms of Posttraumatic Stress disorder (PTSD). Items are rated on a five-point Likert scale. The K-6 is a six-item self-report global measure of distress drawing from depressive and anxiety related symptomology. The items are rated on a five-point Likert-scale and assess distress over the past four weeks
3.2. Secondary and other outcomes
Secondary outcomes include measures of sleep disturbance, burnout, moral distress, workplace stress, and resilience. Daytime sleepiness (four items) is measured using the PROMIS-Sleep Related Impairment short form [32,33]. Burnout is measured using Dolan single item burnout inventory [34]. Moral distress is measured using the Moral Distress Thermometer (one item) [35]. Workplace stress is measured using selected items (three items; feeling valued, intend to seek employment outside, recommend my workplace) from the Stress in the Workplace survey [36]. Resilience is measured using the Connor-Davidson Resilience Scale (2 items) [[37], [38], [39]]
Other outcomes include information about COVID-19 experiences (e.g., number of patients with confirmed or presumed COVID-19, availability of COVID-19 testing at the HCW's organization, vaccination status) and demographics (e.g., age, sex, HCW subgroup/role). HCW's perceived organizational support for the past six months (nine items) will be measured using items developed for this study based on the literature [40]. Sample items include: “in the past 6 months, my organization took appropriate steps to protect me from becoming infected with COVID-19,” “my organization listened and understood my needs and concerns,” and “my organization provided support for my emotional needs.” (Sample items are described because this is a new scale). Items are rated on a five-point Likert scale from “not at all” to “very much.” Coping strategies (e.g., social support from coworkers or family/friends, physical activities; 15 items), as well as the frequency of using each strategy, used by HCW to deal with stress during COVID-19 are also assessed and the items are developed specifically for this study (co-author P.W. developed the items based on clinical experience working with HCW during the pandemic). Sample items include: “during the COVID-19 pandemic, I used this strategy to help me deal with stress…social support from coworkers; social support from family/friends; mentoring or consultation from supervisors/respected others; rewarding, meaningful or enjoyable activities; mental health counseling/treatment/telehealth; alcohol.” Items are rated on a five-point Likert scale from “not at all” to “very much.”
HCW in the SFA condition are asked to complete additional questions about their experience with SFA. These questions include the attendance of both the primary training session and booster sessions of SFA, as well as their evaluation of SFA (e.g., helpfulness of SFA)
4. Secondary data
We also obtain low-burden, routinely collected, site-level, patient-related outcomes pre- and post- intervention. Hospitals report safety and quality measures to Vizient, including mortality, length of stay, and safety events in Vizient's Clinical Database/Resource Manager. Participating hospitals must agree to have Vizient share this data back to us both pre- and post-intervention period. We will also obtain data from CDN on patient experiences at pre and post intervention
5. Qualitative assessment
The goal of the qualitative assessment is to gain insight on additional, unidentified factors that health care system leaders, intervention champions, and HCW report as important to shaping HCW well-being. We are conducting interviews with a sample that is reflective of the intervention and control groups [41]. Participants provide verbal consent at the beginning of each interview
Table 2 shows the topics and sample questions for each type of qualitative interview. Interview topics and questions are rooted in the Consolidated Framework for Implementation Research (CFIR) [42] and developed in partnership with our working group. Drawing from the existing literature and CFIR framework, we identified both workplace contextual factors (i.e., organizational-level factors such as climate, culture, practices, resources) [43]. and other contextual factors influenced by the workplace (i.e., job-level factors such as roles and requirements) that play an important role in predicting HCW well-being, including mental health and burnout outcomes. Prior work has indicated that performance and well-being of HCW is affected by external, macro-level (health care system) factors as well as internal, micro-level (units within the system, which may be clinics, emergency departments, intensive care units) factors that vary across the health care systems and across units within the health care systems [44,45]
Table 2.
Topics and sample questions for interviews with leaders, champions, and HCW
| Topic by Role | Sample Question |
|---|---|
| Pre-Intervention Leaders | |
| Sources of Support | What kinds of initiatives did you have in place to support health care workers in your facility before COVID-19? |
| Communication with Staff | Do you have a way for HCW to provide feedback to voice concerns, either in general or with respect to safety and wellbeing? |
| COVID-19-related Challenges | What have been significant disruptions to work processes during the COVID-19 pandemic in your facility? |
| Post-Intervention Leaders | |
| Facility-Level Factors (SFA Sites) | What kinds of infrastructure changes were needed to accommodate the intervention? |
| Sources of Support (UC Sites) | In the past year, has your facility adopted any additional services or support systems to help health care workers address stress? |
| General Impressions of Staff Health | What are your general impressions of how health care workers are managing their stress/stressful situations now? |
| Champions | |
| Engagement with SFA | Which strategies did you use to encourage your fellow HCW to join the intervention? |
| SFA Training | What did you find was particularly useful about the SFA training? |
| How could the training be improved? | |
| CFIR Implementation factors e.g., adaptation, patient needs, hospital/clinic culture, leadership engagement | How did you adapt SFA for your setting? |
| How much demand was there for the training? | |
| What support did you receive from [site name] to help facilitate SFA? | |
| HCW | |
| COVID-19-related Challenges | How would you describe the impact of COVID-19 on your role as a ___ at [site name]? |
| Motivation (SFA Sites) | What motivated you to participate in the SFA intervention? |
| Importance of HCW health and well-being | In general, how much do you feel [site name] emphasizes your health and wellbeing? |
| Impact of Core SFA Actions (SFA Sites) | Have you used a core SFA actions after a stressful instance? |
| Peer Support | How do you and your fellow HCW help each other out during stressful times? |
Prior to the intervention period, we conduct brief semi-structured interviews with at least one leader (e.g., Chief Quality Officer) at each of the SFA and UC sites on: [1] organizational-level characteristics; [2] interventions in place to support HCW well-being; and [3] anticipated facilitators and barriers to implementation during COVID-19 (SFA sites only). Leaders are asked to speak on behalf of their site
We also collect information on characteristics of each site using a standardized form, including number of fulltime healthcare providers, percent of HCW receiving COVID19 vaccine, number of patient encounters per week or number of hospital discharges per week, patient demographic characteristics, patient insurance, patient comorbidities, and regular staff meeting structure and frequency. These forms are pre-populated by either Vizient or CDN, then reviewed and completed by each site
After the intervention period, we conduct brief, semi-structured interviews with champions at all SFA sites for insights into factors to consider when refining and then scaling up the intervention. We include champions across all SFA sites to elicit the full range of the on-the-ground perspectives on implementation and actions taken to drive uptake and sustainment of SFA
We also conduct semi-structured interviews among a range of HCW, until thematic saturation is reached. We sample HCW from all sites to ensure a full understanding of the impact of SFA, COVID-19-related stress and trauma, sources of support, role clarity, and perspectives on the effectiveness of strategies to improve HCW well-being. Working with our health care systems partners, we purposively sample 2–3 representatives across HCW roles at all sites for a richer understanding of differential effects on HCW
6. Data analysis
6.1. Sample size and power
Assuming a 40% response rate for hospitals (20 sites with 170 HCW each) and 50% for ambulatory centers (12 sites with 50 HCW each), we expect a sample size of 1660 respondents who can complete surveys in both pre- and post-intervention waves. Using a simplified end-stage comparison setting, we calculated the effect sizes that can be detected under the regular setting of two-sided p-value <0.05 and power > 0.80 in a two-sample comparison for the PCL-5 measure of PTSD symptoms. We also calculated the overall effects pooling all samples and the subgroup effect within a health care setting using a part of the sample. We have hypothesized potentially differential treatment effects between hospitals and FQHCs. Hospitals are larger with more staff distributed across multiple departments, whereas the FQHCs are much smaller, and all staff are in a single location. HCW in FQHCs may also be at lower risk of adverse psychological effects such as PTSD and burnout given the lower acuity of illness among patients being cared for in the ambulatory setting and the use of telehealth during at least some of the pandemic. Therefore, conceptually, types of facility may moderate the treatment effect. For the PCL-5, a minimally important difference (MID) is 5–10 points and a clinically significant change is 10–20 points [30]. We assumed an intra-class correlation (ICC) of 0.01 within each site. We can detect a minimum overall effect of 0.18 times standard deviation (SD), an effect of 0.20 times SD by the hospital sample, and an effect of 0.37 times SD by the clinic sample, respectively. These standardized effect sizes translate to 0.99, 1.1, and 2.0 points for the PCL-5 score (SD ≈ 5.5), respectively, all of which are below the MID
Based on the actual study hospital and center recruitment, the final sample size is 12 healthcare centers and 16 hospitals. The projected average HCW sample size is roughly 30 per center and 100 per hospital after taking into account various levels of attritions. This gives an estimated total sample size of 1960. We use a repeated measure setting with a serial correlation of 0.8 within the same respondent to calculate the detectable effect size under two-sided p-value <0.05 and power > 0.80. We also vary the site-level correlation between 0.01 and 0.05. To be conservative, all fixed effects, including pairing of sites, are assumed to cost the error degree of freedom by 50 to 100 without explaining any proportion of error variance. We can detect a standardized effect size between 0.18 and 0.32 times SD of the outcome in an overall analysis, where the larger detectable effect sizes reflect higher site-level correlations and stronger site-paring effects. The subgroup analysis for health centers can detect 0.34 to 0.52 times SD, and the subgroup analysis for hospitals can detect 0.18 to 0.34 times SD
6.2. Missing data
We will conduct two types of analysis to address missing data: a complete-case analysis and an imputation analysis. In the complete-case analysis, we will run all statistical models for complete respondents only. In the imputation analysis, we will fit an imputation model by complete respondents, using the baseline characteristics and the observed pre-intervention data to predict the post-intervention data. We will impute the missing values of the partial respondents by the fitted imputation model [46]. We plan to run 20 rounds of imputations and aggregate the results by standard multiple imputation process. We will report results from both the imputation and complete-case analyses and acknowledge the specific limitations in each type of analysis
6.3. Statistical analysis
We will test the hypothesis that HCW in the sites that receive SFA training will have better mental and physical well-being compared with HCW in UC sites as captured by the primary and secondary outcomes. We will apply a difference-in-differences (DID) model, which is robust to unobserved differences at the baseline and temporal trends unrelated to treatment. Let t = 0,1 represent the baseline and follow-up waves, and D represent the treatment status (D = 1 for SFA and D = 0 for UC). Let Yijt be the observed outcome for HCW i in site j at time t. The DID model is Yijt = α + β × I(t = 1) + γD + λ × D × I(t = 1) + Xijθ + εijt. In this model, α is the intercept, β is the temporal trend not related to the intervention, γ is the mean difference in the outcome at baseline adjusted for individual-level covariate effects Xijθ, and ρs(i) represents a fixed effect for site pairing where the subscript s(i) indicates a pair The random error εijt is correlated within a respondent and possibly within the same clinic. The hypothesized treatment effect is represented by the interaction effect λ, which is tested by the regular Wald's z-test using robust sandwich standard error to adjust for intra-class correlation. We will fit the model by the generalized estimating equation (GEE) method to account for serial correlations within the same respondent. Depending on the goodness of fit to real data, we may choose the linear regression or a multiplicative scale, e.g., the odds ratio, estimated by logistic regression to implement the DID analysis. We will use the quasilikelihood under the independence model (QIC) goodness of fit criterion to select a suitable working correlation matrix, as well as to determine whether a site level clustering is needed. Depending on the goodness of fit to real data judged by cross validation and model selection information criteria, we may choose the linear regression or a generalized linear model to implement the DID analysis, select necessary individual-level fixed effects, and decide if the site-pair fixed effect is needed
We will conduct two subgroup analyses (for the hospital and health center subgroups). The two subgroup analyses are completely non-overlapping and share the same approach and outcome measures. The overall effect assessment and the two subgroup analyses will follow the same DID modeling method. We will also fit a three-way interaction among facility type, treatment status, and time, to combine the two subgroup models into a single model, i.e., a difference-in-differences-in-differences (DDD) model to partially improve statistical power, if the two subgroup DID analyses exhibit a similar level of measurement errors
6.4. Qualitative data analysis
All interviews are audio recorded and transcribed; transcripts are analyzed using Dedoose [47], an encrypted qualitative data analysis software program, which facilitates inductive and deductive analysis [[48], [49], [50]]. Draft preliminary codebooks map to interview protocols which will incorporate key aspects of the CFIR, and then a small sample (~6–10) of each set of interviews is reviewed to identify any additional relevant codes. A select number of transcripts within Dedoose are independently reviewed to test the structure of the coding scheme (e.g., identification of themes and exemplars). To ensure rigor, transparency, credibility, reliability, inter-rater reliability (IRR) of the coding across the qualitative data analysis team will be evaluated with a Cohen's Kappa statistic. When inter-rater reliability falls below 0.8, raters will review discrepancies and come to consensus. Cohen suggested the Kappa result be interpreted as follows: values ≤0 as indicating no agreement and 0.01–0.20 as none to slight, 0.21–0.40 as fair, 0.41–0.60 as moderate, 0.61–0.80 as substantial, and 0.81–1.00 as almost perfect agreement [51]
The coding team will use the Butler-Kisber's approach [52] with two core phases of analysis. In the coarse-grained phase, coders will read the transcripts and write reflective memos to broadly classify emerging themes. In the fine-grained phase, coders will examine the pieces of data more closely and re-assemble chunks of data into refined categories (i.e., assigned, and reassigned names or code) [52]. The fine-grained phase of analysis isolates specific words, phrases, and ideas that represent larger themes. These more specific, discreet units of data generate support for identified abstract concepts or ideas
After completing the coding process, both qualitative and quantitative results will be generated to describe the data. Expected outputs include: code frequency counts; code co-occurrence (i.e., overlap between codes); descriptors (e.g., size of a site; burden of COVID-19) by codes; deviant case analysis to document instances of atypical workplace environmental factors and perspectives; and summarized, qualitative overviews of key themes (including exemplar direct quotations) that map to each set of interviews. We will stratify themes by sub-sample to examine the distribution of themes across types of HCW, site type, size, region, as well as the identification of cross-cutting themes to refine the intervention tools and guide implementation. To enhance credibility, we will cross-check these findings with key representatives among our partners. Ultimately, the qualitative data will provide rich insights on how to account for workplace environmental factors when evaluating the patient-centered effectiveness of SFA and issues to consider for scale-up
7. Discussion
The COVID-19 pandemic has created unprecedented challenges to HCW over an extended period of time, and with several waves of disruption, which may have caused significant mental health consequences among frontline HCW. Accumulating evidence clearly demonstrates the adverse mental health impact of the COVID-19 pandemic on HCW, including increased psychological distress and PTSD symptoms [6,8]. Evidence from prior viral outbreaks (e.g., SARS) suggests that this negative impact on well-being is sustained, leading to clinically significant distress and psychiatric morbidity years after the exposure (e.g., caring for patients with SARS) [11,[53], [54], [55]]. Therefore, establishing evidence-based interventions to support HCW's mental well-being is urgently needed during the current COVID-19 crisis and for future public health emergencies
To the best of our knowledge, with only a few exceptions (including an ongoing study in Spain) [15,56], there has been no large-scale study formally evaluating the effectiveness of mental health interventions tailored to HCW during viral outbreaks. The COVER-HCW study will fill the gap by evaluating the comparative effectiveness of SFA intervention, which is now adapted for HCW during the COVID-19 pandemic. We expect our results will establish the initial evidence base for SFA in a real-world setting
SFA is an ideal candidate to support HCW's mental well-being during the pandemic. It is a variant of psychological first aid (PFA), which is an evidence-informed intervention [[57], [58], [59]], delivered by individuals without mental health training to reduce the initial posttraumatic distress and to improve short- and long-term adaptive function. The COVID-19 pandemic has proven to be long-lasting and presents as a chronic stressor to HCW; therefore, SFA is better suited than PFA, which was designed to be used in more acute settings, such as disaster and emergency responses. The current study takes a unique opportunity to further tailor SFA to meet the needs of HCW across the U.S. and examine whether the SFA intervention and toolkit can reduce and mitigate distress faced by HCW during the pandemic
HCW's well-being in general, and especially during a public health crisis like COVID-19, is crucial in and of itself, and to patients to ensure the provision of uninterrupted, high-quality, patient-centered care. Building and strengthening HCW's well-being is also needed to ensure the long-term occupational capacity of the health care workforce. Therefore, protecting HCW's mental and physical well-being is essential not only for the health and resilience of health care workers as individuals, but also for ensuring their abilities to provide the best care for their patients as a high functioning team, which is a critical component of the quadruple aim, which adds attention to provider satisfaction, work/life balance and workflow optimization. With significant reductions in the healthcare workforce due to high levels of staff turnover at hospitals and FQHCs, interventions that support and enhance the fourth aim will be critical to supporting and retaining the existing health care workforce [60]. Our research will advance science by testing the comparative effectiveness of SFA on HCW during the pandemic and this knowledge will inform future pandemic preparedness and responses
Funding
This research was supported by a contract to Drs. Gidengel and Meredith from the Patient-Centered Outcomes Research Institute (PCORI #COVID-2020C2-10721)
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper
Acknowledgements
The COVER-HCW team includes the PIs (Drs. Gidengil and Meredith) and Co-Investigators at the RAND Corporation, as well as our partners at Vizient Inc., Clinical Directors Network (CDN), and Stanford University School of Medicine, and the study's Working Group. The authors are grateful to our partners at Vizient and CDN for their efforts with recruitment during the pandemic. The study team also deeply appreciates the hard work of all participating sites, site leaders, site champions, and healthcare workers, particularly during a period of many other challenges. We also thank Dr. William Nash for his contributions to study design and the SFA intervention. Finally, we thank our colleagues in the RAND Survey Research Group staff, including Chao Pham and Rosa Elena Garcia
References
- 1.Ahluwalia S.C., Farmer C.M., Abir M. RAND Corporation; Santa Monica, CA: 2020. The RAND [Internet]https://www.rand.org/blog/2020/04/amidst-a-pandemic-a-mental-health-crisis-may-be-looming.html [cited 2020]. Available from: [Google Scholar]
- 2.Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.U.S. Department of Veterans Affairs Managing Healthcare Workers' Stress Associated with the COVID-19 Virus Outbreak Washington, DC2020. https://www.ptsd.va.gov/covid/COVID_healthcare_workers.asp [cited 2020 5/21/2020]Printable Handout]. Available from:
- 4.Cabarkapa S., Nadjidai S.E., Murgier J., Ng C.H. The psychological impact of COVID-19 and other viral epidemics on frontline healthcare workers and ways to address it: A rapid systematic review. Brain Behav. Immun. Health. 2020;8:100144. doi: 10.1016/j.bbih.2020.100144. Epub 2020/09/23. PubMed PMID: 32959031; PMCID: PMC7494453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chigwedere O.C., Sadath A., Kabir Z., Arensman E. The impact of epidemics and pandemics on the mental health of healthcare workers: a systematic review. Int. J. Environ. Res. Public Health. 2021;18(13) doi: 10.3390/ijerph18136695. Epub 2021/07/03. PubMed PMID: 34206264; PMCID: PMC8296866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hennein R., Mew E.J., Lowe S.R. Socio-ecological predictors of mental health outcomes among healthcare workers during the COVID-19 pandemic in the United States. PLoS One. 2021;16(2) doi: 10.1371/journal.pone.0246602. e0246602. Epub 2021/02/06. PubMed PMID: 33544761; PMCID: PMC7864435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li Y., Scherer N., Felix L., Kuper H. Prevalence of depression, anxiety and post-traumatic stress disorder in health care workers during the COVID-19 pandemic: A systematic review and meta-analysis. PLoS One. 2021;16(3) doi: 10.1371/journal.pone.0246454. e0246454. Epub 2021/03/11. PubMed PMID: 33690641; PMCID: PMC7946321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sahebi A., Nejati-Zarnaqi B., Moayedi S., Yousefi K., Torres M., Golitaleb M. The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: An umbrella review of meta-analyses. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2021;107:110247. doi: 10.1016/j.pnpbp.2021.110247. Epub 2021/01/22. PubMed PMID: 33476692; PMCID: PMC7817526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chong M.Y., Wang W.C., Hsieh W.C., Lee C.Y., Chiu N.M., Yeh W.C., Huang O.L., Wen J.K., Chen C.L. Psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br. J. Psychiatry. 2004;185:127–133. doi: 10.1192/bjp.185.2.127. Epub 2004/08/03. [DOI] [PubMed] [Google Scholar]
- 10.Wu P., Fang Y., Guan Z., Fan B., Kong J., Yao Z., Liu X., Fuller C.J., Susser E., Lu J., Hoven C.W. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can. J. Psychiatr. 2009;54(5):302–311. doi: 10.1177/070674370905400504. Epub 2009/06/06. PubMed PMID: 19497162; PMCID: PMC3780353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maunder R.G., Lancee W.J., Balderson K.E., Bennett J.P., Borgundvaag B., Evans S., Fernandes C.M., Goldbloom D.S., Gupta M., Hunter J.J., McGillis Hall L., Nagle L.M., Pain C., Peczeniuk S.S., Raymond G., Read N., Rourke S.B., Steinberg R.J., Stewart T.E., Van De Velde-Coke S., Veldhorst G.G., Wasylenki D.A. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg. Infect. Dis. 2006;12(12):1924–1932. doi: 10.3201/eid1212.060584. Epub 2007/03/01. PubMed PMID: 17326946; PMCID: PMC3291360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Noseworthy J., Madara J., Cosgrove D., Edgeworth M., Ellison E., Krevans S., Rothman P., Sowers K., Strongwater S., Torchiana D., Harrison D. Health Affairs Blog [Internet]. Weil A, editor: Health Affairs. 2017 28 March 2017. [cited 2020] Available from: [DOI]
- 13.Shanafelt T.D., Mungo M., Schmitgen J., Storz K.A., Reeves D., Hayes S.N., Sloan J.A., Swensen S.J., Buskirk S.J. Longitudinal study evaluating the association between physician burnout and changes in professional work effort. Mayo Clin. Proc. 2016;91(4):422–431. doi: 10.1016/j.mayocp.2016.02.001. Epub 2016/04/06. [DOI] [PubMed] [Google Scholar]
- 14.Bodenheimer T., Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann. Fam. Med. 2014;12(6):573–576. doi: 10.1370/afm.1713. Epub 2014/11/12. PubMed PMID: 25384822; PMCID: PMC4226781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen R., Chou K.R., Huang Y.J., Wang T.S., Liu S.Y., Ho L.Y. Effects of a SARS prevention programme in Taiwan on nursing staff’s anxiety, depression and sleep quality: a longitudinal survey. Int. J. Nurs. Stud. 2006;43(2):215–225. doi: 10.1016/j.ijnurstu.2005.03.006. Epub 2005/06/02. PubMed PMID: 15927185; PMCID: PMC7094227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Watson P., Alexander M., et al. Office USP, editor: Federal Law Center; 2020. Stress First Aid for Pretrial and Probation Settings. [Google Scholar]
- 17.Watson P., Gist R., Taylor V., Nash W., Litz B. 2012. Stress First Aid for Wildland Firefighters and Emergency Services Personnel. (NAFRI) NAFRI, editor: Department of Forestry. [Google Scholar]
- 18.Watson P., Taylor V., Alexander M., et al. 2020. Stress First Aid for Health Care Workers. PTSD NCf, editor: U.S. Department of Veterans Affairs. [Google Scholar]
- 19.Watson P., Taylor V., R G, Elvander, F L, B M, J a, D V, W N, RJ W, al e. National Center for PTSD: US Department of Veterans Affairs; 2013. Stress First Aid for Firefighters and Emergency Medical Services Personnel Student Manual. Foundation NFF, editor. [Google Scholar]
- 20.Watson P., Taylor V., Gist R., Alexander M., et al. 2020. Stress First Aid for Patients and Familes. PTSD NCf, editor: U.S. Department of Veterans Affairs. [Google Scholar]
- 21.Watson P., Taylor V., Gist R., Elvander E., Leto F., Martin B., Tanner J., Vaught D., Nash W., Westphal R., Litz B. 2015. Stress First Aid for Firefighters and Emergency Medical Services Personnel. [Google Scholar]
- 22.Westphal R., Watson P., Gist R., Taylor V., Evlander E., Leto F., Martin R., Vaught D., Nash W., Litz B. 2014. Stress First Aid for Law Enforcement Personnel Instructor’s Manual: Oregon Department of Public Safety Standards & Training. [Google Scholar]
- 23.Palinkas L.A., Aarons G.A., Horwitz S., Chamberlain P., Hurlburt M., Landsverk J. Mixed method designs in implementation research. Admin. Pol. Ment. Health. 2011;38(1):44–53. doi: 10.1007/s10488-010-0314-z. Epub 2010/10/23. PubMed PMID: 20967495; PMCID: PMC3025112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.United States Census Bureau Census Regions and Divisions of the United States. April 9, 2022. https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf Available from:
- 25.Farmer C.M., Whipkey K., Chamberlin M. RAND Corporation; Santa Monica, CA: 2019. Programs Addressing Psychological Health and Resilience in the U.S. Department of Homeland Security. Contract No.: RR-1952. [PMC free article] [PubMed] [Google Scholar]
- 26.Nash W., Westphal R., Watson P., Litz B. In: Combat and Operational Stress First Aid: Responder Training Manual. BoMa Surgery., editor. US Navy; Washington, DC: 2011. [Google Scholar]
- 27.Nash W.P., Watson P.J. Development. Review of VA/DOD Clinical Practice Guideline on management of acute stress and interventions to prevent posttraumatic stress disorder. J. Rehab. Res. 2012;49(5) doi: 10.1682/jrrd.2011.10.0194. [DOI] [PubMed] [Google Scholar]
- 28.Watson P., Taylor V., Alexander M. National Center for PTSD; 2020. Stress First Aid for Health Care Workers. [Google Scholar]
- 29.Macklin R., Natanson C. Misrepresenting “usual care” in research: an ethical and scientific error. Am. J. Bioeth. 2020;20(1):31–39. doi: 10.1080/15265161.2019.1687777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weathers F., Litz B., Keane T., Palmieri P., Marx B., Schnurr P. National Center for PTSD: US Department of Veterans Affairs; 2013. The PTSD Checklist for DSM-5 (PCL-5) [Google Scholar]
- 31.K6+ Self Report Measure [Internet] Whitaker Institute for Innovation and Societal Change. 2011 [cited 08/01/2020] https://www.midss.org/sites/default/files/k6_self_admin_updated_08-08-11.pdf Available from:
- 32.Buysse D.J., Yu L., Moul D.E., Germain A., Stover A., Dodds N.E., Johnston K.L., Shablesky-Cade M.A., Pilkonis P.A. Development and validation of patient-reported outcome measures for sleep disturbance and sleep-related impairments. Sleep. 2010;33:781–792. doi: 10.1093/sleep/33.6.781. PMCID: PMC2880437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yu L., Buysse D.J., Germain A., Moul D. Development of short forms from the PROMIS sleep disturbance and sleep-related impairment item banks. Behav. Sleep Med. 2012;10:6–24. doi: 10.1080/15402002.2012.636266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dolan E.D., Mohr D., Lempa M., Joos S., Fihn S.D., Nelson K.M., Helfrich C.D. Using a single item to measure burnout in primary care staff: a psychometric evaluation. J. Gen. Intern. Med. 2015;30(5):582–587. doi: 10.1007/s11606-014-3112-6. Epub 2014/12/03. PubMed PMID: 25451989; PMCID: PMC4395610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wocial L.D., Weaver M.T. Development and psychometric testing of a new tool for detecting moral distress: the Moral Distress Thermometer. J. Adv. Nurs. 2013;69(1):167–174. doi: 10.1111/j.1365-2648.2012.06036.x. [DOI] [PubMed] [Google Scholar]
- 36.Interactive Harris. American Psychological Association; March 2011. Stress in the Workplace: Survey Summary. [Google Scholar]
- 37.West C.P., Dyrbye L.N., Sloan J.A., Shanafelt T.D. Single item measures of emotional exhaustion and depersonalization are useful for assessing burnout in medical professionals. J. Gen. Intern. Med. 2009;24(12):1318–1321. doi: 10.1007/s11606-009-1129-z. Epub 10/6. PubMed PMID: 19802645; PMCID: PMC2787943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.West C.P., Shanafelt T.D., Kolars J.C. Quality of life, burnout, educational debt, and medical knowledge among internal medicine residents. JAMA. 2011;306(9):952–960. doi: 10.1001/jama.2011.1247. [DOI] [PubMed] [Google Scholar]
- 39.Vaishnavi S., Connor K., Davidson J.R. An abbreviated version of the Connor-Davidson Resilience Scale (CD-RISC), the CD-RISC2: psychometric properties and applications in psychopharmacological trials. Psychiatry Res. 2007;152(2–3):293–297. doi: 10.1016/j.psychres.2007.01.006. Epub 2007/04/27. PubMed PMID: 17459488; PMCID: PMC2041449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shanafelt T., Ripp J., Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. 2020;323(21):2133–2134. doi: 10.1001/jama.2020.5893. Epub 2020/04/08. PubMed PMID: 32259193. [DOI] [PubMed] [Google Scholar]
- 41.Lowe A., Norris A.C., Farris A.J., Babbage D.R. Quantifying thematic saturation in qualitative data analysis. Field Methods. 2018;30(3):191–207. doi: 10.1177/1525822x17749386. [DOI] [Google Scholar]
- 42.Damschroder L.J., Aron D.C., Keith R.E., Kirsh S.R., Alexander J.A., Lowery J.C. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement. Sci. 2009;4(1):50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shannon H.S., Robson L.S., Sale J.E. Creating safer and healthier workplaces: role of organizational factors and job characteristics. Am. J. Ind. Med. 2001;40(3):319–334. doi: 10.1002/ajim.1106. Epub 2001/10/13. PubMed PMID: 11598981. [DOI] [PubMed] [Google Scholar]
- 44.Dieleman M., Harnmeijer J.W. Switzerland World Health Organization; Geneva: 2006. Improving Health Worker Performance: in Search of Promising Practices. [Google Scholar]
- 45.Dieleman M., Harnmeijer J.W. World Health Organization; Geneva: 2006. Improving health worker performance: in search of promising practices; pp. 5–34. [Google Scholar]
- 46.Allison P.D. Missing data techniques for structural equation modeling. J. Abnorm. Psychol. 2003;112(4):545–557. doi: 10.1037/0021-843X.112.4.545. Epub 2003/12/17. PubMed PMID: 14674868. [DOI] [PubMed] [Google Scholar]
- 47.Dedoose Version 8.3.35 . SocioCultural Research Consultants, LLC; Los Angeles, CA: 2020. Web Application for Managing, Analyzing, and Presenting Qualitative and Mixed Method Research Data; p. 2020. [Google Scholar]
- 48.Bernard H., Ryan G. Sage Publications; Thousand Oaks, CA: 2016. Analyzing Qualitative Data: Systematic Approaches. [Google Scholar]
- 49.Guest G., MacQueen K., Namey E. Sage Publications; Thousand Oaks, CA: 2011. Applied Thematic Analysis. [Google Scholar]
- 50.Miles M., Huberman A., Saldana J. Sage Publications; Thousand Oaks, CA: 2013. Qualitative Data Analysis. [Google Scholar]
- 51.McHugh M.L. Interrater reliability: the kappa statistic. Biochem. Med. (Zagreb) 2012;22(3):276–282. Epub 2012/10/25. PubMed PMID: 23092060; PMCID: PMC3900052. [PMC free article] [PubMed] [Google Scholar]
- 52.Butler-Kisber L. Sage Publications; 2010. Qualitative Inquiry: Thematic, Narrative and Arts-Informed Perspectives. [Google Scholar]
- 53.Maunder R. The experience of the 2003 SARS outbreak as a traumatic stress among frontline healthcare workers in Toronto: lessons learned. Philos. Trans. R. Soc. Lond. Ser. B Biol. Sci. 2004;359(1447):1117–1125. doi: 10.1098/rstb.2004.1483. Epub 2004/08/13. PubMed PMID: 15306398; PMCID: PMC1693388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Maunder R.G., Hunter J., Vincent L., Bennett J., Peladeau N., Leszcz M., Sadavoy J., Verhaeghe L.M., Steinberg R., Mazzulli T. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ. 2003;168(10):1245–1251. Epub 2003/05/14. PubMed PMID: 12743065; PMCID: PMC154178. [PMC free article] [PubMed] [Google Scholar]
- 55.McAlonan G.M., Lee A.M., Cheung V., Cheung C., Tsang K.W., Sham P.C., Chua S.E., Wong J.G. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can. J. Psychiatr. 2007;52(4):241–247. doi: 10.1177/070674370705200406. Epub 2007/05/16. PubMed PMID: 17500305. [DOI] [PubMed] [Google Scholar]
- 56.Serrano-Ripoll M.J., Ricci-Cabello I., Jimenez R., Zamanillo-Campos R., Yanez-Juan A.M., Bennasar-Veny M., Sitges C., Gervilla E., Leiva A., Garcia-Campayo J., Garcia-Buades M.E., Garcia-Toro M., Pastor-Moreno G., Ruiz-Perez I., Alonso-Coello P., Llobera J., MA Fiol-deRoque. Effect of a mobile-based intervention on mental health in frontline healthcare workers against COVID-19: Protocol for a randomized controlled trial. J. Adv. Nurs. 2021;77(6):2898–2907. doi: 10.1111/jan.14813. Epub 2021/03/07. PubMed PMID: 33675247; PMCID: PMC8250879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fox J.H., Burkle F.M., Jr., Bass J., Pia F.A., Epstein J.L., Markenson D. The effectiveness of psychological first aid as a disaster intervention tool: research analysis of peer-reviewed literature from 1990-2010. Disaster Med. Public Health Prep. 2012;6(3):247–252. doi: 10.1001/dmp.2012.39. Epub 2012/10/19. PubMed PMID: 23077267. [DOI] [PubMed] [Google Scholar]
- 58.Allen B., Brymer M.J., Steinberg A.M., Vernberg E.M., Jacobs A., Speier A.H., Pynoos R.S. Perceptions of psychological first aid among providers responding to Hurricanes Gustav and Ike. J. Trauma. Stress. 2010;23(4):509–513. doi: 10.1002/jts.20539. Epub 2010/07/14. PubMed PMID: 20623598. [DOI] [PubMed] [Google Scholar]
- 59.Dieltjens T., Moonens I., Van Praet K., De Buck E., Vandekerckhove P. A systematic literature search on psychological first aid: lack of evidence to develop guidelines. PLoS One. 2014;9(12):e114714. doi: 10.1371/journal.pone.0114714. Epub 2014/12/17. PubMed PMID: 25503520; PMCID: PMC4264843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sinsky C., Linzer M. Practice and policy reset Post-COVID-19: reversion, transition, or transformation? Health Aff (Millwood). 2020;39(8):1405–1411. doi: 10.1377/hlthaff.2020.00612. Epub 2020/08/04. PubMed PMID: 32744939. [DOI] [PubMed] [Google Scholar]