Abstract
Background
Mechanical debridement of periodontal pockets remains the mainstay of therapy in all forms of periodontitis. There is 47% greater reduction in plaque amount when sodium hypochlorite (NaOCl) is used as an adjunct when compared with water rinsing. The aim of this study was to evaluate the effects of 0.05% NaOCl and 0.12% chlorhexidine gluconate twice daily rinse on periodontal parameters and gingival crevicular fluid (GCF) HSV1 and CMV levels in chronic periodontitis.
Methods
Patients assigned to group A were prescribed 0.05% NaOCl mouthwash for twice daily rinse. Patients in group B were prescribed 0.12% chlorhexidine gluconate mouthwash to be used twice daily. Evaluation of periodontal parameters was done at baseline and after six months following therapy. GCF HSV1 and CMV levels were evaluated using a polymerase chain reaction.
Results
A statistically significant difference was noted in the improvement in periodontal parameters between both groups, when evaluated six months following therapy with greater reduction in group A vis-a-vis group B.
Conclusion
NaOCl when prescribed as a twice daily mouthwash can be recommended as a part of the home care regime in patients with chronic periodontitis. It is more cost-effective, easily available and can be beneficial to the troops in difficult terrains and extremes of climates, where oral healthcare facilities are not easily accessible.
Keywords: Gingival crevicular fluid (GCF), Herpes simplex virus-1 (HSV-1), Cytomegalovirus, Periodontitis, Sodium hypochlorite, Chlorhexidine gluconate
Introduction
The lesions in periodontal disease are complex with periodontal pathogens residing in inaccessible areas, suggesting that a mechanical approach alone may lead to incomplete elimination of the disease in most of the cases. A 30-year Swedish epidemiologic study had concluded that there was a 8%–44% increase in periodontally healthy individuals with regular periodontal treatment and maintenance care, with concomitant reduction in the percentage of gingivitis and moderate periodontitis.1 The most important goal of periodontal treatment is to eliminate pathogenic microorganisms to achieve a state of good dental health. Mechanical debridement and adjunctive antimicrobial therapy form important components of a comprehensive treatment plan. Mechanotherapy alone may not eliminate a significant portion of periodontal microorganisms, especially in periodontal sites with advanced destruction.2 Mechanical plaque control performed in absence of antimicrobials or root planning or periodontal surgery can lead to failure to arrest advanced periodontal disease.3 The global increase in organisms with antibiotic resistance and the rising costs of newer antibiotics have generated interest in using more economic antiseptics to eliminate infections involving areas such as the periodontium. In accordance with J Slots, cases of advanced periodontitis probably have a viral aetiology, which fails to respond to conventional periodontal therapy and maintenance care. Herpesviruses, including Epstein-Barr virus and cytomegalovirus, are associated with aggressive periodontitis, probably causing advanced destruction in presence of periodontopathic bacteria. Herpesvirus have the potential to enhance the destructive potential of resident pathogens, which, may lead to increase in the virulence of herpesviruses. The ample amount of herpesviruses detected in periodontitis leads us to the possibility of redefinition of paradigm of periodontal disease.4,5 In this study, we have evaluated the effect of 0.05% sodium hypochlorite (NaOCl) twice/day rinse and compared it with the gold standard 0.12% Chlorhexidine gluconate twice/daily rinse in terms of improvement in periodontal parameters and reduction in gingival crevicular fluid (GCF) HSV-1 and CMV levels, if detected, in patients with chronic periodontitis.
Materials and methods
The patients selected from two different dental centres, were screened by means of a comprehensive periodontal examination, which consisted of plaque index (PI), gingival bleeding index (GBI), probing pocket depth (PD) and clinical attachment level (CAL). GCF samples were collected using paper strip method. After phase one therapy, the patients were grouped into two groups using block randomisation method. Patients in group A were prescribed 0.05% NaOCl mouthwash twice daily rinse for 4 weeks. The mouthwash had to be diluted, and the patients were instructed to dilute it by mixing household bleach with water (5 ml: 250 ml). Patients in group B were prescribed 0.12% chlorhexidine gluconate mouthwash to be used twice daily for 4 weeks. GCF HSV1 and CMV levels were evaluated using a polymerase chain reaction. The parameters were recorded at baseline and at six months following initiation of therapy in both the groups. All the patients received oral hygiene instructions. The results were analysed using appropriate statistical evaluation. Institutional ethical clearance and patient consent was also obtained before entry into study.
GCF sample
GCF samples were collected from the gingival sulcus for each subject, in all the three groups, before clinical examination. The selected sites were isolated with cotton rolls, supragingival plaque was removed, tooth was air dried and filter paper strips (periotron paper strips) were left in the sulcus at the depth of 1–2 mm for 30s. Eppendorf tubes containing 150 μl of elution buffer phosphate buffered saline with low concentration detergent such as 0.1% Tween (PBST) (0.05% in phosphate buffered saline) were used to store the strips at −80 °C until assayed [Fig. 1].
Fig. 1.
Gingival crevicular fluid (GCF) samples collected and stored.
HSV-1 and CMV assay
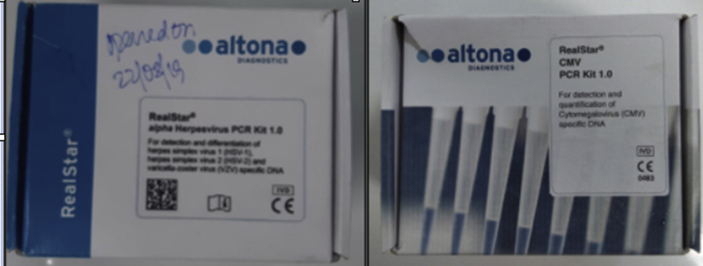
The GCF samples were thawed, and DNA was extracted for the assay using an automated nucleic acid extraction system (EasyMag instrument, bioMerieux, USA) following the protocols developed by the manufacturers. Real-time polymerase chain reaction (PCR) kits with primers and probes directed towards HSV-1 and CMV were used for molecular detection (Real Star HSV and CMV kits, Altona GmBH, Germany) [Fig. 2]. Each specimen was run in duplicate using the manufacturer's instructions on a Roche 480 II Real Time Thermal Cycler, (Roche Diagnostics USA) [Fig. 4]. We reported as positive only those samples in which >10 copies of HSV or CMV DNA/reaction were detected [Fig. 3].
Fig. 2.
HSV kit and CMV kit.
Fig. 4.
Real-time PCR.
Fig. 3.
PCR set-up.
Results
All clinical data was tabulated along with data obtained through assay. The data were statistically analysed [Table 1, Table 2, Table 3, Table 4]. The statistical software SPSS, version 24.0 was used for the analysis. Within the limitations of this study, significant statistical differences were found in two clinical parameters (probing depth and CALs) among the patients on 0.05% NaOCl mouthwash as compared to patients on 0.12% chlorhexidine mouthwash.
Table 1.
Comparison of mean between group A and group B.
| Periodontal parameters | Group | N | Mean | Std. deviation | Std. error mean | t-value | p-value |
|---|---|---|---|---|---|---|---|
| PI-0 | Group A | 30 | 2.47 | 0.51 | 0.09 | 0.766 | 0.447 |
| Group B | 30 | 2.57 | 0.50 | 0.09 | |||
| PI-1 | Group A | 30 | 1.10 | 0.48 | 0.09 | 0 | 1 |
| Group B | 30 | 1.10 | 0.55 | 0.10 | |||
| PI-2 | Group A | 30 | 0.87 | 0.43 | 0.08 | 0.288 | 0.774 |
| Group B | 30 | 0.83 | 0.46 | 0.08 | |||
| GBI-0 | Group A | 30 | 2.43 | 0.50 | 0.09 | 0.255 | 0.799 |
| Group B | 30 | 2.47 | 0.51 | 0.09 | |||
| GBI-1 | Group A | 30 | 0.83 | 0.46 | 0.08 | 0.479 | 0.634 |
| Group B | 30 | 0.90 | 0.61 | 0.11 | |||
| GBI-2 | Group A | 30 | 0.30 | 0.47 | 0.09 | 1.733 | 0.088 |
| Group B | 30 | 0.53 | 0.57 | 0.10 | |||
| PD-0 | Group A | 30 | 5.67 | 0.84 | 0.15 | 0.444 | 0.658 |
| Group B | 30 | 5.57 | 0.90 | 0.16 | |||
| PD-1 | Group A | 30 | 3.30 | 0.84 | 0.15 | 0.437 | 0.664 |
| Group B | 30 | 3.40 | 0.93 | 0.17 | |||
| PD-2 | Group A | 30 | 2.17 | 0.38 | 0.07 | 2.339 | 0.023 |
| Group B | 30 | 2.50 | 0.68 | 0.12 | |||
| CAL-0 | Group A | 30 | 3.63 | 0.85 | 0.16 | 0.953 | 0.345 |
| Group B | 30 | 3.40 | 1.04 | 0.19 | |||
| CAL-1 | Group A | 30 | 1.33 | 0.80 | 0.15 | 0.29 | 0.773 |
| Group B | 30 | 1.40 | 0.97 | 0.18 | |||
| CAL-2 | Group A | 30 | 0.23 | 0.43 | 0.08 | 2.039 | 0.046 |
| Group B | 30 | 0.53 | 0.68 | 0.12 |
Significant difference can be seen in group A and B with higher value in group B in PD-2 and CAL-2 as p-value is less than 0.05. But nonsignificant difference in other variables at all time points with p-value greater than 0.05. Bold signifies P < 0.05.
PI, plaque index, GI, gingival index, GBI, gingival bleeding index, PD, probing depth, CAL, clinical attachment level 0: Baseline, 1: at 1 month post therapy, 2: at 6 months post therapy.
Table 2.
Paired T-test (overall data).
| Groups | Periodontal parameters | N | Mean | Std. deviation | Std. error mean | Mean difference | t-value | p-value |
|---|---|---|---|---|---|---|---|---|
| Pair 1 | PI-0 | 60 | 2.52 | 0.50 | 0.07 | 1.42 | 16.348 | <0.001 |
| PI-1 | 60 | 1.10 | 0.51 | 0.07 | ||||
| Pair 2 | PI-1 | 60 | 1.10 | 0.51 | 0.07 | 0.25 | 3.085 | 0.003 |
| PI-2 | 60 | 0.85 | 0.44 | 0.06 | ||||
| Pair 3 | PI-0 | 60 | 2.52 | 0.50 | 0.07 | 1.67 | 22.553 | <0.001 |
| PI-2 | 60 | 0.85 | 0.44 | 0.06 | ||||
| Pair 4 | GBI-0 | 60 | 2.45 | 0.50 | 0.06 | 1.58 | 16.504 | <0.001 |
| GBI-1 | 60 | 0.87 | 0.54 | 0.07 | ||||
| Pair 5 | GBI-1 | 60 | 0.87 | 0.54 | 0.07 | 0.45 | 6.523 | <0.001 |
| GBI-2 | 60 | 0.42 | 0.53 | 0.07 | ||||
| Pair 6 | GBI-0 | 60 | 2.45 | 0.50 | 0.06 | 2.03 | 19.643 | <0.001 |
| GBI-2 | 60 | 0.42 | 0.53 | 0.07 | ||||
| Pair 7 | PD-0 | 60 | 5.62 | 0.87 | 0.11 | 2.27 | 22.561 | <0.001 |
| PD-1 | 60 | 3.35 | 0.88 | 0.11 | ||||
| Pair 8 | PD-1 | 60 | 3.35 | 0.88 | 0.11 | 1.02 | 10.533 | <0.001 |
| PD-2 | 60 | 2.33 | 0.57 | 0.07 | ||||
| Pair 9 | PD-0 | 60 | 5.62 | 0.87 | 0.11 | 3.28 | 34.435 | <0.001 |
| PD-2 | 60 | 2.33 | 0.57 | 0.07 | ||||
| Pair 10 | CAL-0 | 60 | 3.52 | 0.95 | 0.12 | 2.15 | 20.315 | <0.001 |
| CAL-1 | 60 | 1.37 | 0.88 | 0.11 | ||||
| Pair 11 | CAL-1 | 60 | 1.37 | 0.88 | 0.11 | 0.98 | 9.892 | <0.001 |
| CAL-2 | 60 | 0.38 | 0.58 | 0.08 | ||||
| Pair 12 | CAL-0 | 60 | 3.52 | 0.95 | 0.12 | 3.13 | 29.139 | <0.001 |
| CAL-2 | 60 | 0.38 | 0.58 | 0.08 |
There is significant change in all the four variables viz. PI, GBI, PD and CAL at all the time points with p-value less than 0.01. Bold signifies P< 0.05.
PI, plaque index; GBI, GBI, gingival bleeding index; PD, pocket depth; CAL, clinical attachment level.
Table 3.
Paired T-test (group A).
| Groups | Periodontal parameters | N | Mean | Std. deviation | Std. error mean | Mean difference | t-value | p-value |
|---|---|---|---|---|---|---|---|---|
| Pair 1 | PI-0 | 30 | 2.47 | 0.51 | 0.09 | 1.37 | 12.17 | <0.001 |
| PI-1 | 30 | 1.10 | 0.48 | 0.09 | ||||
| Pair 2 | PI-1 | 30 | 1.10 | 0.48 | 0.09 | 0.23 | 2.04 | 0.05 |
| PI-2 | 30 | 0.87 | 0.43 | 0.08 | ||||
| Pair 3 | PI-0 | 30 | 2.47 | 0.51 | 0.09 | 1.60 | 15.56 | <0.001 |
| PI-2 | 30 | 0.87 | 0.43 | 0.08 | ||||
| Pair 4 | GBI-0 | 30 | 2.43 | 0.50 | 0.09 | 1.60 | 12.11 | <0.001 |
| GBI-1 | 30 | 0.83 | 0.46 | 0.08 | ||||
| Pair 5 | GBI-1 | 30 | 0.83 | 0.46 | 0.08 | 0.53 | 5.76 | <0.001 |
| GBI-2 | 30 | 0.30 | 0.47 | 0.09 | ||||
| Pair 6 | GBI-0 | 30 | 2.43 | 0.50 | 0.09 | 2.13 | 16.00 | <0.001 |
| GBI-2 | 30 | 0.30 | 0.47 | 0.09 | ||||
| Pair 7 | PD-0 | 30 | 5.67 | 0.84 | 0.15 | 2.37 | 16.95 | <0.001 |
| PD-1 | 30 | 3.30 | 0.84 | 0.15 | ||||
| Pair 8 | PD-1 | 30 | 3.30 | 0.84 | 0.15 | 1.13 | 8.00 | <0.001 |
| PD-2 | 30 | 2.17 | 0.38 | 0.07 | ||||
| Pair 9 | PD-0 | 30 | 5.67 | 0.84 | 0.15 | 3.50 | 28.10 | <0.001 |
| PD-2 | 30 | 2.17 | 0.38 | 0.07 | ||||
| Pair 10 | CAL-0 | 30 | 3.63 | 0.85 | 0.16 | 2.30 | 16.80 | <0.001 |
| CAL-1 | 30 | 1.33 | 0.80 | 0.15 | ||||
| Pair 11 | CAL-1 | 30 | 1.33 | 0.80 | 0.15 | 1.10 | 8.46 | <0.001 |
| CAL-2 | 30 | 0.23 | 0.43 | 0.08 | ||||
| Pair 12 | CAL-0 | 30 | 3.63 | 0.85 | 0.16 | 3.40 | 25.72 | <0.001 |
| CAL-2 | 30 | 0.23 | 0.43 | 0.08 |
There is significant change in all the four variables viz. PI, GBI, PD and CAL at all the time points with p-value less than 0.01. Bold signifies P< 0.05.
PI, plaque index; GBI: Gingival bleeding index; PD, pocket depth; CAL, clinical attachment level.
Table 4.
Paired T-test (group B).
| Groups | Periodontal parameters | N | Mean | Std. deviation | Std. error mean | Mean difference | t-value | p-value |
|---|---|---|---|---|---|---|---|---|
| Pair 1 | PI-0 | 30 | 2.57 | 0.50 | 0.09 | 1.47 | 11.00 | <0.001 |
| PI-1 | 30 | 1.10 | 0.55 | 0.10 | ||||
| Pair 2 | PI-1 | 30 | 1.10 | 0.55 | 0.10 | 0.27 | 2.28 | 0.03 |
| PI-2 | 30 | 0.83 | 0.46 | 0.08 | ||||
| Pair 3 | PI-0 | 30 | 2.57 | 0.50 | 0.09 | 1.73 | 16.28 | <0.001 |
| PI-2 | 30 | 0.83 | 0.46 | 0.08 | ||||
| Pair 4 | GBI-0 | 30 | 2.47 | 0.51 | 0.09 | 1.57 | 11.09 | <0.001 |
| GBI-1 | 30 | 0.90 | 0.61 | 0.11 | ||||
| Pair 5 | GBI-1 | 30 | 0.90 | 0.61 | 0.11 | 0.37 | 3.61 | 0.001 |
| GBI-2 | 30 | 0.53 | 0.57 | 0.10 | ||||
| Pair 6 | GBI-0 | 30 | 2.47 | 0.51 | 0.09 | 1.93 | 12.20 | <0.001 |
| GBI-2 | 30 | 0.53 | 0.57 | 0.10 | ||||
| Pair 7 | PD-0 | 30 | 5.57 | 0.90 | 0.16 | 2.17 | 14.99 | <0.001 |
| PD-1 | 30 | 3.40 | 0.93 | 0.17 | ||||
| Pair 8 | PD-1 | 30 | 3.40 | 0.93 | 0.17 | 0.90 | 6.92 | <0.001 |
| PD-2 | 30 | 2.50 | 0.68 | 0.12 | ||||
| Pair 9 | PD-0 | 30 | 5.57 | 0.90 | 0.16 | 3.07 | 22.71 | <0.001 |
| PD-2 | 30 | 2.50 | 0.68 | 0.12 | ||||
| Pair 10 | CAL-0 | 30 | 3.40 | 1.04 | 0.19 | 2.00 | 12.58 | <0.001 |
| CAL-1 | 30 | 1.40 | 0.97 | 0.18 | ||||
| Pair 11 | CAL-1 | 30 | 1.40 | 0.97 | 0.18 | 0.87 | 5.79 | <0.001 |
| CAL-2 | 30 | 0.53 | 0.68 | 0.12 | ||||
| Pair 12 | CAL-0 | 30 | 3.40 | 1.04 | 0.19 | 2.87 | 18.25 | <0.001 |
| CAL-2 | 30 | 0.53 | 0.68 | 0.12 |
There is significant change in all the four variables viz. PI, GBI, PD and CAL at all the time points with p-value less than 0.01. Bold signifies P< 0.05.
PI, plaque index; GBI: Gingival bleeding index; PD, pocket depth; CAL, clinical attachment level.
Discussion
Periodontitis is a chronic disease of the periodontium, characterised by the breakdown of tissues and, if not treated leads to tooth loss which can significantly hamper the quality of life. Periodontal disease is considered to be a major oral health burden as per epidemiological data and affects almost half of the global population.6 The etiopathogenesis of periodontal disease is explained by the formation of biofilm inhabited by periodontal pathogens inducing a periodontal inflammatory response. The host response to these pathogens eventually leads to bone loss and periodontal tissue destruction, which are the characteristic signs of periodontal disease.7 The bacterial aetiology however, is unable to explain various aspects of periodontitis, especially in cases where the amount of periodontal damage is inconsistent with the amount of local factors. Latest microbiological studies on periodontal disease have led researchers to believe that human viruses probably play a significant role in the pathogenesis of periodontitis.4,5,8, 9, 10, 11, 12
NaOCl is a chlorine-releasing agent and destroys microorganisms by oxidation of proteins, nucleotides and lipids. NaOCl at 0.5% was used effectively to manage infections in soldiers injured during World War I, before antibiotics. It is a highly efficient proteolytic and antimicrobial agent and is commonly used as irrigation solution for endodontic therapy.13 Jorgen Slots has been a pioneer in recommending antiviral therapy targeting viruses as periodontal pathogens and had introduced the concept of low cost periodontal therapy using NaOCl twicedaily rinses or povidone iodine irrigation.8 The most likely explanation of the excellent results obtained with this low-cost therapy is probably related to the absence of supragingival plaque, which can affect the subgingival ecology. The mouthwash reduces periodontal pathogen counts in pockets up to 5 mm in depth.14 The other possibility is that the subgingival irrigation with bleach suppresses periodontal herpesviruses, leading to a decreased subgingival bacterial counts and elimination of clinical signs of disease. The significant reduction of fusobacteria, an important periodontal pathogen, after irrigation with NaOCl might be due its antibacterial effect or due to its role in herpesvirus suppression.4,14, 15, 16
In this study, we have evaluated the effect of 0.05% NaOCl twice/day rinse and compared it with the gold standard 0.12% chlorhexidine gluconate twice/daily rinse in terms of improvement in periodontal parameters and reduction in GCF HSV-1 and CMV levels, if detected, in patients with chronic periodontitis. Earlier studies have reported significant reduction in supragingival biofilm formation, gingival inflammation and bleeding with oral rinsing with various concentrations of NaOCl twice/weekly.15,17, 18, 19, 20, 21 One study comparing NaOCl with hydrogen peroxide concluded that both the agents reduced plaque accumulation, but the effects of NaOCl persisted for 24 h.15 It has been reported in literature that by controlling the concentration of NaOCl used, it maybe possible to have a beneficial effect on the periodontium, by causing eliminating the soft tissue wall of the pocket without affecting the healing.13 In contrast, chlorhexidine gluconate in even low concentrations can interfere with healing due its ability to reduce the production of gingival proteins and being toxic to the fibroblasts in gingiva.7
A study carried out to investigate the persistence of antimicrobial action and plaque inhibitory properties of 3 Acidifed sodium chlorite mouthrinses with chlorhexidine 0.12% concluded that the chlorhexidine gluconate mouth rinse as and adjunct to mechanotherapy resulted in slightly greater reduction of probing than mechanotherapy alone.22 Another study comparing 0.2% NaOCl mouthwash and 0.2% chlorhexidine gluconate concluded that NaOCl mouthwash as an adjunct to mechanotherapy is as effective as chlorhexidine gluconate mouthwash for the treatment of gingivitis. Owing to enhanced safety due to less side effects such as staining, NaOCl can be used as a routine mouthwash.23
In our study, we found that there was a statistically significant difference in periodontal parameters between both groups, when evaluated six months following therapy with greater reduction in group A (NaOCl) as compared to group B (chlorhexidine gluconate)(p < 0.05){Table 3}. There was a marked change in all the four variables viz. PI, GBI, PD and CAL from baseline to one and six months after therapy in both the groups (p-value< 0.01) {Table 1, Table 2, Table 3, Table 4}. Previous reported literature on both NaOCl and chlorhexidine gluconate in the management of periodontitis have reported similar outcomes and both agents have been used worldwide as adjuncts to mechanotherapy. We agree the results of these earlier studies as both the groups showed improvement in clinical parameters following therapy. But in our study, NaOCl group showed a significant reduction in probing depth and an improvement in CALs as compared to the chlorhexidine gluconate group. We had tested the GCF samples for presence of viruses (HSV-1 and CMV) using a molecular analysis. HSV-1 was detected in 4 samples each at baseline evaluation in both the groups. None of the samples in either of the groups showed presence of HSV-1 at the time of assessment at one month and at six months after therapy. CMV was not detected in any of the baseline or post-therapy samples in both the groups.
Conclusion
NaOCl mouthwash is recommended to be included in the protocol for management of periodontal disease in the Armed forces to offer the possibility of enhanced control of destructive periodontal disease reducing the rate of tooth loss improving form, function, esthetics and overall quality of life. It will be beneficial to troops stationed in remote areas to help control periodontal disease, during the maintenance phase in absence of regular recall visits to the dental centre.
Disclosure of competing interest
The authors have none to declare.
Acknowledgements
This article is based on Armed Forces Medical Research Committee Project No. 4851/2017 granted and funded by office of the Directorate General Armed Forces Medical Services and Defence Research Development Organization, Government of India.
References
- 1.Hugoson A., Sjódin B., Norderyd O. Trends over 30 years, 1973–2003, in the prevalence and severity of periodontal disease. J Clin Periodontol. 2008;35 doi: 10.1111/j.1600-051X.2008.01225.x. 405–414.88. [DOI] [PubMed] [Google Scholar]
- 2.Umeda M., Takeuchi Y., Noguchi K., Huang Y., Koshy G., Ishikawa I. Effects of non- surgical periodontal therapy on the microbiota. Periodontol 2000. 2004;36:98–120. doi: 10.1111/j.1600-0757.2004.03675.x. [DOI] [PubMed] [Google Scholar]
- 3.Beirne P., Forgie A., Worthington H.V., Clarkson J.E. Routine scale and polish for periodontal health in adults. Cochrane Database Syst Rev. 2005;1 doi: 10.1002/14651858.CD004625.pub2. [DOI] [PubMed] [Google Scholar]
- 4.Slots J. Herpesvirus periodontitis: infection beyond biofilm. J Calif Dent Assoc. 2011;39 393–399.5. [PubMed] [Google Scholar]
- 5.Slots J. Herpes viral-bacterial interactions in periodontal diseases. Periodontol 2000. 2010;52:117–140. doi: 10.1111/j.1600-0757.2009.00308.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kassebaum N.J., Bernabé E., Dahiya M., Bhandari B., Murray C.J.L., Marcenes W. Global burden of severe tooth loss: a systematic review and meta-analysis. J Dent Res. 2014;93:20S–28S. doi: 10.1177/0022034514537828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mariotti A.J., Rumpf D.A. Chlorhexidine induced changes to human gingival fibroblast collagen and non-collagen protein production. J Periodontol. 1999;70:1443–1448. doi: 10.1902/jop.1999.70.12.1443. [DOI] [PubMed] [Google Scholar]
- 8.Das S., Krithiga G.S., Gopalakrishnan S. Detection of human herpes viruses in patients with chronic and aggressive periodontitis and relationship between viruses and clinical parameters. J Oral Maxillofac Pathol. 2012;16:203–209. doi: 10.4103/0973-029X.98502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Slots J. Low-cost periodontal therapy. Periodontol 2000. 2012;60:110–137. doi: 10.1111/j.1600-0757.2011.00429.x. [DOI] [PubMed] [Google Scholar]
- 10.Luiz Fernando Noira Passos da Costa, Cristine da Silva Furtado Amaral, Davi da Silva Barbirato, Anna Thereza Thomé Leão, Mariana Fampa Fogacci Chlorhexidine mouthwash as an adjunct to mechanical therapy in chronic periodontitis: a meta analysis. J Am Dent Assoc (Ed Espñola) 2017;148:308–318. doi: 10.1016/j.adaj.2017.01.021. [DOI] [PubMed] [Google Scholar]
- 11.Darveau R.P. Periodontitis: a polymicrobial disruption of host homeostasis. Nat Rev Microbiol. 2010;8:481–490. doi: 10.1038/nrmicro2337. [DOI] [PubMed] [Google Scholar]
- 12.Contreras A., Umeda M., Chen C. Relationship between herpesviruses and adult periodontitis and periodontopathic bacteria. J Periodontol. 1999;70:478–484. doi: 10.1902/jop.1999.70.5.478. [DOI] [PubMed] [Google Scholar]
- 13.Slots J. Selection of antimicrobial agents in periodontal therapy. J Periodontal Res. 2002;37:389–398. doi: 10.1034/j.1600-0765.2002.00004.x. [DOI] [PubMed] [Google Scholar]
- 14.Kalkwarf K.L., Tussing G.J., Davis M.J. Histologic evaluation of gingival curettage facilitated by sodium hypochlorite solution. J Periodontol. 1982;53:63–70. doi: 10.1902/jop.1982.53.2.63. [DOI] [PubMed] [Google Scholar]
- 15.Mohammadi Z. Sodium hypochlorite in endodontics: an update review. Int Dent J. 2008;5:329–341. doi: 10.1111/j.1875-595x.2008.tb00354.x. [DOI] [PubMed] [Google Scholar]
- 16.De Nardo R., Chiappe V., Gomez M., Romanelli H., Slots J. Effect of 0.05% sodium hypochlorite oral rinse on supragingival biofilm and gingival inflammation. Int Dent J. 2012;62:208–212. doi: 10.1111/j.1875-595X.2011.00111.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mombelli A. Microbial colonization of the periodontal pocket and its significance for periodontal therapy. Periodontol 2000. 2018;76:85–96. doi: 10.1111/prd.12147. [DOI] [PubMed] [Google Scholar]
- 18.Saygun I., Kubar A., Sahin S., Sener K., Slots J. Quantitative analysis of association between herpesviruses and bacterial pathogens in periodontitis. J Periodontal Res. 2008;43:352–359. doi: 10.1111/j.1600-0765.2007.01043.x. [DOI] [PubMed] [Google Scholar]
- 19.Gonzalez S., Cohen C.L., Galvan M., Alonaizan F.A., Rich S.K., Slots J. Gingival bleeding on probing: relationship to change in periodontal pocket depth and effect of sodium hypochlorite oral rinse. J Periodontal Res. 2014;50:397–402. doi: 10.1111/jre.12219. [DOI] [PubMed] [Google Scholar]
- 20.Jurczyk Karolina, Nietzsche Sandor, Ender Claudia, Sculean Anton, Eick Sigrun. In-vitro activity of sodium-hypochlorite gel on bacteria associated with periodontitis. Clin Oral Invest. 2016 doi: 10.1007/s00784-016-1711-9. s00784-016-1711-9. [DOI] [PubMed] [Google Scholar]
- 21.Ximénez-Fyvie L.A., Haffajee A.D., Som S., Thompson M., Torresyap G., Socransky S.S. The effect of repeated professional supragingival plaque removal on the composition of the supra- and subgingival microbiota. J Clin Periodontol. 2000 Sep;27 doi: 10.1034/j.1600-051x.2000.027009637.x. 637–647.19. [DOI] [PubMed] [Google Scholar]
- 22.Yates R., Moran J., Addy M., Mullan P.J., Wade W.G., Newcombe R. The comparative effect of acidified sodium chlorite and chlorhexidine mouthrinses on plaque re- growth and salivary bacterial counts. J Clin Periodontol. 1997;24:603–609. doi: 10.1111/j.1600-051x.1997.tb00236.x. [DOI] [PubMed] [Google Scholar]
- 23.Pourshahidi Sara, Rezazadeh Fahimeh, Motamedifar Mohammad, Davarmanesh Mahdi, Ebrahimi Hooman. In vitro comparative study on antiherpetic effect of chlorhexidine and persica mouthwashes with acyclovir. J Basic Appl Sci. 2012;8:286–290. [Google Scholar]