Abstract
Background
Adult and immunocompromised patients suffering from varicella (chicken pox) are potential source of infection to healthcare workers. An outbreak of varicella among healthcare workers in a tertiary care centre was investigated, and preventive measures were implemented.
Methods
Cases of chicken pox between 05 Feb 2017 and 11 Feb 2017 in a tertiary healthcare establishment were investigated. An epidemiological investigation by developing case definitions, spot map and contact tracing was conducted. Eight cases were identified among healthcare workers. Suitable preventive measures including identification of susceptible contacts and vaccination of susceptible ones with two doses of varicella vaccine was undertaken.
Results
Index case was a 21-year-old nurse who was exposed to a 34-year-old male patient transferred from a secondary care hospital on 24 Jan 2017 as a case of acute liver failure and coagulopathy. Primary case was later diagnosed as case of varicella based on serological and clinical evidence. Among a total of 8 cases identified in the outbreak, the cases occurred among healthcare workers of secondary care centre, healthcare workers managing the primary case in the intensive care unit and who conducted the autopsy. A total of 181 contacts were identified in the epidemiological investigation, and 54 were susceptible to chicken pox. Two-dose immunization with varicella vaccination of susceptible ones was found to be effective in preventing further cases.
Conclusion
Two-dose vaccination of healthcare workers with varicella vaccine is an effective strategy to prevent nosocomial varicella among healthcare workers.
Keywords: Varicella, Outbreak, Healthcare workers, Vaccination
Introduction
Varicella (chickenpox) is a highly contagious disease, which is caused by the Varicella-Zoster Virus (VZV), a ubiquitous human α herpes virus.1 Infection due to the varicella-zoster or chickenpox virus has secondary attack rates nearing 90% and is among the most common infectious human diseases.2 The majority of primary chickenpox virus infections occur in childhood. Adult and immune-compromised subjects with chickenpox tend to have a more severe disease course than do children, and they are more likely to be hospitalized. They serve as potential sources of infection to nonimmune healthcare workers (HCWs) involved in their care.2 Nosocomial varicella in hospital employees can result in loss of productivity, entail cost to the hospital, and disruption to patient care.
An outbreak of varicella occurred amongst healthcare workers in an institutional setting of a tertiary care hospital from 05 Feb 2017 to 11 Feb 2017. The institution had an existing health surveillance mechanism, and prevention and control measures were initiated immediately after the reporting of the first case.
The tertiary healthcare institution had more than a thousand healthcare workers, including specialists, super-specialists, paramedical workers, and paramedical trainees. About half of the healthcare workers, especially paramedical workers and paramedical trainees, resided in barracks/hostels and were sharing rooms and dining facilities. This study was carried out with an aim to identify the source of the outbreak, factors responsible for the outbreak, and implement prevention and control measures.
Materials and methods
One case of chickenpox among the healthcare workers was reported and admitted to the hospital on 08 Feb 2017. A day later, another case of another healthcare worker occurred and was admitted to the hospital. An epidemiological investigation was undertaken, and notification was immediately issued. The possibility of an explosive outbreak in close settings is very high, and thus, aggressive control measures were instituted. In the present scenario, cases being healthcare staff employed in rotation to various units in the tertiary care institute, there was an impending risk of outbreak spilling over to patients and other staff in the hospital setting.
First, the susceptible population at risk was identified. “Susceptible individuals” were regarded as people without a prior history of chickenpox or no history of vaccination for varicella in the past.
Case definitions used in this outbreak were as under:
Probable case: A probable/clinical case was defined as an individual who developed acute onset diffuse (generalized) maculopapular vesicular rash having fever without apparent cause occurring from 2nd Feb 2017 to 23rd Feb 2017 at our healthcare facility.
Confirmed case: A confirmed case was defined as the case, which met the clinical case definition and was laboratory confirmed.
Close contact: Close contact was defined as an individual who had close indoor contact like residing in the same room/barrack or having face-to-face contact.
An epidemiological case sheet was prepared and the identification of cases was carried out. Line listing of all cases was done. A blood sample for VZ IgM antibodies was collected from all cases on admission. The search for the primary case for the index case was carried out. Mapping of cases and contacts was done using a spot map of the healthcare facility. Contact tracing of primary contacts, contacts of contacts (secondary contacts), and contacts of secondary contacts were done. History of contact, previous history of chickenpox disease, history of travel, and vaccination were recorded. All cases were admitted and kept in an isolation ward. All close contacts were identified, and quarantining was undertaken. Health education for case identification and reporting was imparted. Avoiding conglomeration and minimizing contact being the mainstay of spread of the disease, the meal timings of the healthcare workers staying in hostel/barracks were staggered, and other group gatherings were withheld.
Windows were kept open to improve ventilation of individual rooms/barracks. Screening drill for chickenpox was implemented every morning and evening for all individuals residing in hostels/barracks and at the time of reporting to the hospital for duty. The exposed healthcare workers not found susceptible to varicella were allowed to work in the hospital after implementing mask usage and observing standard precautions. Training activities in classrooms and hospital training visits were permitted. Among all the contacts, susceptible healthcare workers were identified and given two doses of varicella vaccine 4 weeks apart. Patient consent was obtained for all data disclosed and institutional ethical clearance was obtained for the epidemiological study.
Results
Isolated cases of chickenpox occur among the hospital staff, and in the previous three years, not more than two cases had been reported in a month in any of the healthcare establishments under study. The first case was reported in a nurse on 06 Feb 2017. The inquiry into the case revealed that she had attended a case of “Acute Liver Failure with Coagulopathy” transferred from another hospital on 24 Jan 2017, and later, the patient had expired. The epidemiological investigation was extended to secondary healthcare facility from where this patient was transferred. The same case definitions were used except probable case definition, which was amended for the occurrence of cases from 31st Jan 2017 to 20th Feb 2017 at the secondary healthcare facility.
Index case: The 21-year-old nurse was exposed to a 34-year-old male who was transferred from a secondary care hospital on 24 Jan 2017 as a case of “Acute Liver failure with Coagulopathy.” She had close contact with the primary case in the form of intravenous cannulation, the suction of bronchial secretions, and assistance in providing ventilatory support to the patient.
Primary Case: The primary case was a 34-year-old male who was initially admitted to secondary care healthcare facility as a case of nasal polyp and underwent polypectomy on 04 Jan 2017. Three cases of chickenpox were under treatment in the secondary care hospital during the hospitalization of the primary case, and he probably acquired the disease from these cases. He was advised Tab Dexamethasone 4 mg twice a day after Polypectomy during the convalescence period. On 21 Jan 2017, he reported to the hospital with abdominal pain and fever. The patient's condition kept on deteriorating and he developed liver failure and coagulopathy (Raised Liver enzymes & INR-3.5). He was found to have a maculopapular rash, acute liver failure, and coagulopathy (Fig. 1). He was aggressively managed at the secondary healthcare facility and evacuated to a tertiary care institute on 24 Jan 2017. The patient succumbed to his illness on 24 Jan 2017 at the tertiary care healthcare institute. The post-mortem serology of this patient confirmed infection with varicella, verifying it to be a primary case.
Fig. 1.
Maculopapular rash in Primary Case.
The patient was initially managed by four healthcare workers at the tertiary care hospital. Three of the four healthcare workers who managed the case initially developed Varicella (Chickenpox).
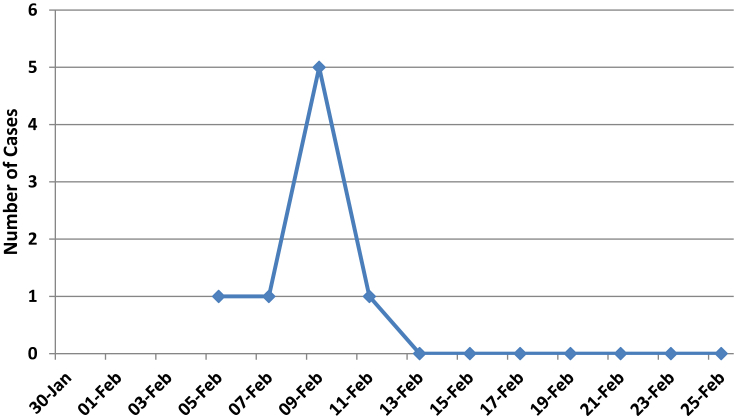
Two cases occurred in the secondary care healthcare institute, where the primary case was initially managed. Amongst all the cases reported, two cases were the female nurses who attended the patient. Three out of four healthcare workers who conducted the autopsy on the primary case developed the disease. All cases had close contact with the primary case in the form of contact with blood and body fluids, aerosols, etc. leading to the disease. The demographic and clinical characteristics of the cases are described in Table 1. The occurrence of cases is illustrated in the epidemic curve (Fig. 2). One of the cases who was previously vaccinated (Index case) had mild disease. None of the cases developed any complications, and all of them recovered fully.
Table 1.
Demographic/Clinical Characteristics of cases (n = 8).
| Characteristic | |
|---|---|
| Age (yrs) (Mean ± Std Dev) |
29.87 ± 12.49 |
| Gender | |
| Male | 6 (75.00%) |
| Female | 2 (25.00%) |
| Symptoms/Signs | |
| Fever | 7 (87.50%) |
| Chills | 2 (25.00%) |
| Malaise | 2 (25.00%) |
| Bodyache | 2 (25.00%) |
| Rash | 8 (100.00%) |
| Lesions < 50 | 2 (25.00%) |
| Lesions ≥ 50 | 7 (75.00%) |
| Lymphadenopathy | 5 (62.50%) |
Fig. 2.
Epidemic Curve.
The contact tracing at both (secondary care and tertiary care) healthcare institutes for primary contacts, secondary contacts, and contacts of secondary contacts revealed 181 contacts. The inquiry into the previous history of chickenpox infection or vaccination for chickenpox revealed that 54 (29.83%) contacts were susceptible to chickenpox, 59 susceptibles were vaccinated for chickenpox, and 68 had suffered chickenpox previously. All the susceptible contacts were identified and 52 were given two doses of chickenpox vaccine. Two susceptibles could not be vaccinated as one was pregnant, and the other was in the convalescence period post appendicectomy.
Discussion
The present outbreak occurred among the healthcare workers indicating the easy vulnerability of acquiring the disease from patients. Nosocomial outbreaks in India are reported in the institutional setups involving healthcare workers.1,2 An outbreak among the nursing students in a tertiary healthcare center has been reported, and the index case transmitted the disease to eight other students.3 Fourteen health care workers in a tertiary care hospital in Rajasthan acquired the infection from a 23-year-old renal transplant recipient in another outbreak reported recently.1
In our setting, the affected healthcare workers had close contact with the primary case in the form of intravenous cannulation, ventilatory support, cardiopulmonary resuscitation, and conduct of autopsy. The close contact increases the vulnerability and has been reported in the outbreak in CMC Vellore when four healthcare workers acquired an infection after experiencing blood splash during the autopsy of a renal allograft recipient suffering from chickenpox.2
The primary case in our study was an immune-compromised adult who was administered steroids, and such adult immune-compromised subjects with chickenpox tend to have a more severe disease course, and chances of hospitalization are higher.4, 5, 6 They serve as potential sources of infection to nonimmune healthcare workers involved in their care. The minimization of this risk of health care transmission by the implementation of standard precautions in healthcare settings is successful to a limited extent. This reflects a need for a policy of vaccinating nonimmune healthcare workers against chickenpox and the use of personal protective measures like N95 mask in lieu of surgical mask and double gloves instead of single gloves in addition to other personal protective measures used in standard precautions. The index case in our study was vaccinated against chickenpox and had the mildest disease among all the cases. This emphasizes the fact that vaccination protects against severe disease; 52 susceptible contacts (healthcare workers) were administered two doses of the chickenpox vaccine, and none developed the disease. Cost-benefit analysis in developed countries like the United States and Spain has shown that a vaccination program to all children is justified.7, 8, 9 The findings of the study by Bhatti et al.3 have justified the benefit of vaccinating healthcare workers and need not be overemphasized. The formulation and strict implementation of policy on vaccination of healthcare workers against chickenpox are needed to develop herd immunity among healthcare workers and prevent disruption of healthcare to the patients.
Conclusion
Adulthood being a predisposing factor for visceral involvement and systemic complications of chickenpox, the vaccination of healthcare workers against chickenpox along with conventional preventive measures like isolation of cases, personal protection, disinfection, proper ventilation, etc. is the mainstay to interrupt transmission in healthcare settings.
Conflicts of interest
The authors have none to declare.
References
- 1.Sood Smita. Occupationally related outbreak of chicken pox in hospital staff: a learning experience. J Clin Diagn Res. 2013;7:2294–2295. doi: 10.7860/JCDR/2013/5780.3502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Paul Navin, Mini E., Jacob An outbreak of cadaver-acquired chickenpox in a Health Care Setting. Clin Infect Dis. 2006;43:599–601. doi: 10.1086/506569. [DOI] [PubMed] [Google Scholar]
- 3.Bhatti V.K., Lee Budhathoki, Mahadevan Kumar, et al. Use of immunization as strategy for outbreak control of varicella zoster in an institutional setting. Med J Armed Forces India. 2014;70:220–224. doi: 10.1016/j.mjafi.2014.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dits Hilde, Frans Eric, Wilmer Alexander, Van Ranst Marc, Fevery Johan, Bobbaers Herman. Clin Infect Dis. 1998;27:209–210. doi: 10.1086/514613. [DOI] [PubMed] [Google Scholar]
- 5.Bajaj N., Joshi J., Bajaj S. Chicken pox with multisystem complications. Med J Armed Forces India. 2010;66:280–282. doi: 10.1016/S0377-1237(10)80062-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anne-Marie Roque-Afonso, Bralet Marie-Pierre, Philippe Ichai, et al. Chickenpox-associated fulminant hepatitis that led to liver transplantation in a 63 year old woman. Liver Transplant. 2008;14:1309–1312. doi: 10.1002/lt.21514. [DOI] [PubMed] [Google Scholar]
- 7.Weekly Epidemiological Record WHO position paper on varicella vaccines. World Health Organ. 1998;73:241–248. [Google Scholar]
- 8.Diez Domingo J., Ridao M., Latour J., Ballester A., Morant A. A cost benefit analysis of routine varicella vaccination in Spain. Vaccine. 1999;17:1306–1311. doi: 10.1016/s0264-410x(98)00394-6. Mar 17. [DOI] [PubMed] [Google Scholar]
- 9.Gray A.M., Fenn P., Weinberg J., Miller E., McGuire A. An economic analysis of varicella vaccination for health care workers. Epidemiol Infect. 1997 Oct;119:209–220. doi: 10.1017/s0950268897007887. [DOI] [PMC free article] [PubMed] [Google Scholar]