Abstract
Background:
The benefits of nonstandard work hours include increased production time and the number of jobs. While for some sectors, such as emergency services, around-the-clock work is a necessary and critical societal obligation, work outside of traditional daytime schedules has been associated with many occupational safety and health hazards and their associated costs. Thus, organizational- and policy-level decisions on nonstandard work hours can be difficult and are based on several factors including economic evaluation. However, there is a lack of systematic knowledge of economic benefits and costs associated with these schedules.
Methods:
We conducted a scoping review of the methodology and data used to examine the economic benefits and costs of nonstandard work hours and related interventions to mitigate risks.
Results:
Ten studies met all our inclusion criteria. Most studies used aggregation and analysis of national and other large datasets. Costs estimated include health-related expenses, productivity losses, and projections of future loss of earnings. Cost analyses of interventions were provided for an obstructive sleep apnea screening program, implementation of an employer-based educational program, and increased staffing to cover overtime hours.
Conclusions:
A paucity of studies assess nonstandard work hours using economic terms. Future studies are needed to expand economic evaluations beyond the employer level to include those at the societal level because impacts of nonstandard work go beyond the workplace and are important for policy analysis and formulation. We pose the opportunity for researchers and employers to share data and resources in the development of more analyses that fill these research gaps.
Keywords: economic benefits, economic costs, economic evaluation, long work hours, nonstandard shifts, scoping review, shift work
1 |. INTRODUCTION
Almost one quarter of American workers work nonstandard schedules such as shift work or long work hours.1 It has been suggested that the benefits of these types of schedules include the creation of more jobs and increased production.2 Work during nontraditional hours can allow for time for tasks (e.g., maintenance) that may not be possible during busier daytime hours when more activity is occurring. For some occupations, such as emergency services, providing around-the-clock-services is a critical societal necessity. From an worker’s perspective, benefits of nonstandard work hours include higher rates of pay, time for dependency care, or easier work commutes during times with lower traffic volume, with positive effects on worker well-being and health.3,4 However, these types of schedules are not without adverse occupational safety and health (OSH) risks. Working nonstandard hours requires workers to sleep during natural biological waking times and work during natural sleep times, and might impose erratic or irregular sleep schedules and routines on workers. This can disrupt sleep and increase the risk for OSH outcomes such as MVCs, workplace injuries, and chronic diseases such as cancer and cardiovascular disease.5–10
Multiple factors, such as regulations, safety and health risks, and worker acceptability come into play when making operational and policy decisions regarding shift scheduling or OSH interventions. Economic factors can provide additional insights throughout the decision-making process, both from the societal and employer’s perspectives. However, economic evaluation is rarely considered in OSH due to the lack of comprehensive surveillance and epidemiological data, and complex problem of identifying benefits and costs.11,12
The purpose of this study is to gain a better understanding of the current literature which describes the economic benefits and costs associated with nonstandard work hours, and the cost-effectiveness of interventions to mitigate related risks. We assessed the current literature for benefits and costs experienced by employers and workers. We also sought to describe external benefits or costs (i.e., “externalities”) which represent the effects on third parties (or society) financially, physically, or psychically.13 We sought to identify methods used in prior literature including data sources which can aid in decision making about shift scheduling and interventions in current operations; and identify directions for future research.
This manuscript is part of a series of papers developed following the NIOSH Working Hours, Sleep and Fatigue Forum in September 2019.14 The purpose of this series is to identify the research gaps in our understanding of working hours, sleep, and fatigue that are specific for industry sectors and working populations at higher risk for fatigue-related OSH events in the United States. Collectively, the papers provide overviews of the current state of research, identify safety and health risks, highlight effective interventions, and suggest future research directions.
2 |. METHODOLOGY
We conducted a scoping review to identify and describe the economic benefits and costs of nonstandard work schedules, such as shift work and long work hours, in the current literature. Scoping reviews aim to map key concepts in a research area and the main sources and types of evidence available.15 Unlike systematic reviews, scoping reviews do not “identify gaps, deficiencies and trends in the current evidence.” As such, “an assessment of methodological limitations… is generally not performed.”15 We followed existing review frameworks to systematically search, select, and synthesize existing knowledge.16–18 We identified literature search terms, databases, and seminal articles by consulting economists and researchers with expertise in nonstandard work hours, and by identifying terms from key articles. Terms related to nonstandard work hours, and economics were included in the search strategy (Supporting Information). We searched electronic databases including MEDLINE (OVID), EMBASE (OVID), PsycINFO, Scopus, EconLit, Business Source, National Safety Council, and the National Academies Press. We also included peer-reviewed literature and gray literature.
Articles were included if they were published in 1980 or later, written in English, involved an adult working population (18+ years old) who was exposed to nonstandard work hours such as shift work and long work hours. We included only studies among countries classified by the World Bank as “high income” which would be similar and generalizable to U.S. industry practices. Additionally, the outcome of interest had to be reported in economic terms. Descriptions of benefits, costs, or interventions were included.
Our search strategy, conducted in 2019, returned 12,600 articles. Six additional studies, identified by two authors (I. W. and M. B.) from sources outside of the search during study conceptualization, were added as potential articles to include in the review2,19–23 (Figure 1). Once all citations were merged and duplicates removed, 11,116 citations remained for title and abstract screening. This initial screening was completed by (I. W.) to identify studies which addressed the research question and fulfilled all inclusion criteria. From this, 66 articles remained for a full-text screening which was completed by three authors (I. W., B. Q., and E. I.). I. W. reviewed all articles, B. Q. and E. I. each reviewed half. Where there was a discrepancy between two authors on the inclusion or exclusion of an article, the third reviewer acted as a tiebreaker. Ten articles were identified to be included in the final step of data charting (Table 1). Two of these studies were among those initially identified from other sources.22,23 The reviewers met to discuss data to be charted (i.e., data sources used, benefits or costs described, and economic estimates). A pilot charting exercise was conducted with four articles to ensure consistency in capturing key aspects for evaluation and synthesis. Afterward, the reviewers met to compare results as a further assurance of consistency and discuss final results for all included articles and resolve any discrepancies.
FIGURE 1.
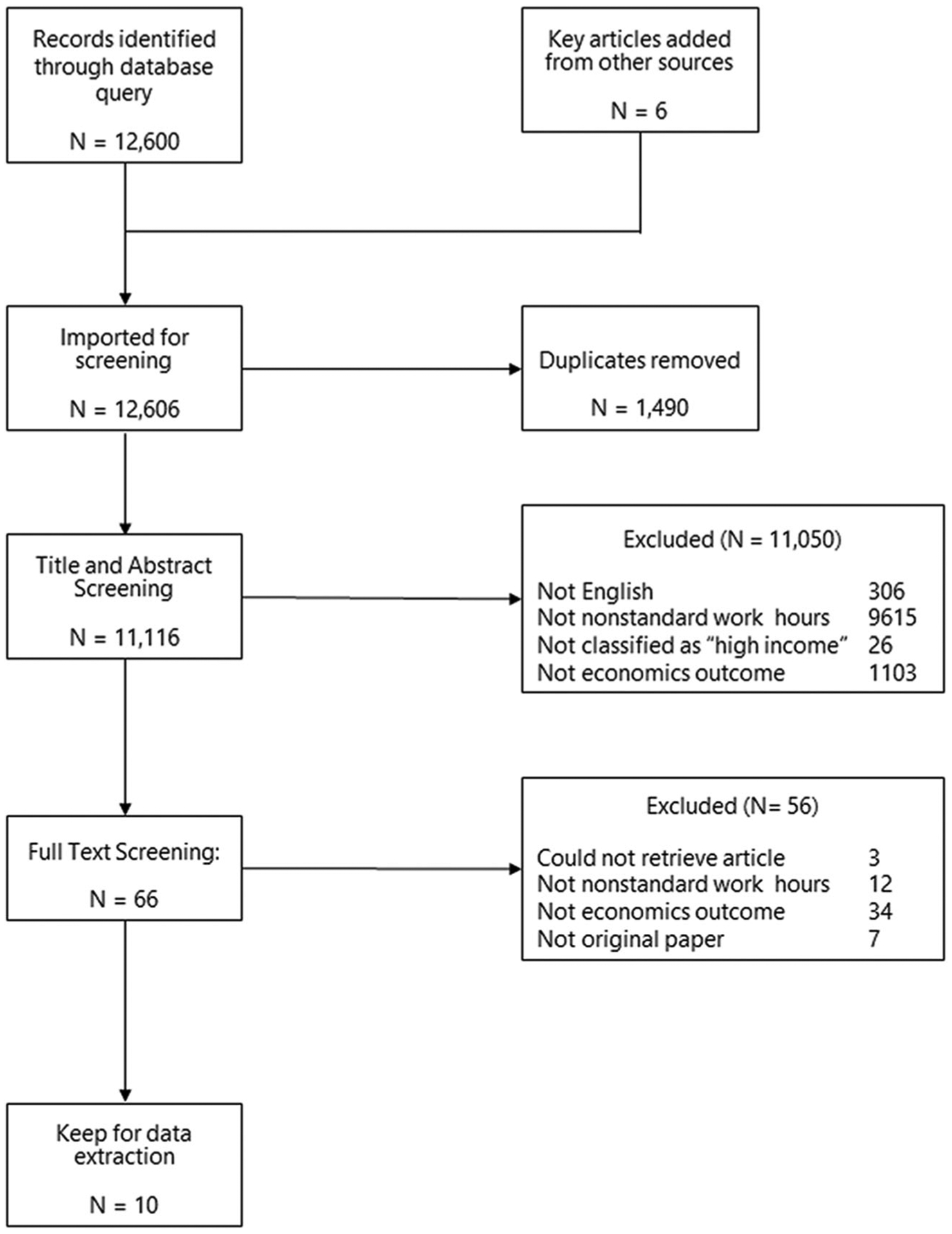
Overview of scoping methodology
TABLE 1.
Summary of articles included in scoping review
| Study reference, industry details and occupational groups; country | Type of article (peer-reviewed journal article, gray literature) | Type of nonstandard work hours benefits or costs described | Data source | Economic estimate(s) |
|---|---|---|---|---|
| Coburn (1997),24 no specific industry or occupation described; United States of America | Peer-reviewed journal | 24-h Shiftwork, rotating shiftwork. Two main categories of costs:
|
Information compiled from a variety of sources. Cost estimates were based on the portion of workers in shift work and the risk of outcome associated with shift work. Two main categories of costs:
|
The total annual cost of shiftworker fatigue: $77 billion ($157.31 billion in 2020 dollars) Breakdown (USD per year, in billions)
|
| Drebit et al. (2010),25 registered nurses; Canada | Peer-reviewed journal | Long work hours; overtime (>40 h/week). Overtime costs by employment category
|
Payroll data for registered nurses in acute care hospitals from 2005 to 2008 in a specific health care region in British Columbia, Canada. Each record represented one employee’s 2-week pay period and contained his/her number of regular hours and overtime hours worked, hourly wage rate as well as employment status (full time, part-time, casual), demographic characteristics (age, gender), and department | Overtime costs totaled $84 million CDN over the 4-year period and contributed 10%–12% of all costs to workers paid.
|
| Guruhagavatula et al. (2008),26 commercial truck drivers; United States of America | Peer-reviewed journal | Irregular shifts—e.g., shift work and long work hours. Cost analyses of obstructive sleep apnea (OSA) screening. Two methods examined:
|
Total cost of screening program: Summed cost of testing, treatment plus crashes.
|
Cost of not screening commercial drivers: $689/driver (USD). In-laboratory polysomnography screening not cost effective: $920 (USD)/driver. This is 1/3 more expensive than not screening at all. Selective polysomnography is cost-effective: $358 (1-stage; sleep study to evaluate for OSA) to $372 (2-stage; sleep study to evaluate for OSA + oximetry)/driver. The survey was conducted from 1996 to 1998 so all costs are reported in 1997 dollars, where $1 = $1.64 in 2020 |
| Hafner et al. (2016),27 no specific industry or occupation described; five countries from the Organisation for Economic Co-operation and Development (OECD) countries (i.e., Japan, United States, United Kingdom, Germany, Canada) | White paper/report | Irregular hours (e.g., shift work). Objectives of the study:
|
Data were gathered from prior studies to estimate the association of short sleep with all-cause mortality, productivity losses at the employer level, and school achievement among adolescents. To determine losses for each OECD country described, additional national-level economic data (e.g., human/physical capital stock, capital/labor ratios, multifactor productivity, and total hours worked) were obtained from Penn World Tables, OECD, and the World Bank. Proportion of working population sleeping less than the recommended sleep duration was gathered from the National Sleep Foundation Survey (2013). Population projections were based on data from the United Nations (2014) and an adapted version of Chapin’s cohort-component model | Scenario 1: Short sleepers (<7 h/day) sleep longer and obtain recommended 7–9 h sleep/day. Costs/year for 2015–2030:
|
| Horwitz and McCall (2004),28 Hospital employees; United States of America | Peer-reviewed literature | Evening (12–7 p.m.) and night (8 p.m. –3 a.m.) shift work. Compensation for lost-time disability | Oregon workers’ compensation claim data from 1990 to 1997, restricted to hospital workers, hospital employment data from Oregon’s Labor Market Information System. Compensation data included: Claimant occupation and industry, claimant demographics (e.g., age, gender), nature of reported injury, body part affected, compensated days of lost work by claimant, claimant cost, and time claimant started work |
For all hospital employee claims, the average total amount per claim amounted to $6213 (SD = $13,382). An analysis of claim cost differences by shift shows that those working night shift had the highest claim costs, averaging $6715 (SD = $12,856), with day shift workers averaging $6187 (SD = $12,470), and evening shift employee claim costs averaging $6103 (SD = $15,338). Differences in total compensation were not statistically significant. Regression analyses showed night shift workers claimed significantly more lost-work time than day and evening shifts, while controlling for gender, age, event causing injury, nature of injury, occupation, year of injury and weekly wage of claimant The authors conclude that lower claim costs (medical, permanent partial disability, and vocational training) among night shift workers offset the lost-work time resulting in nonsignificant differences in total compensation |
| Iwasaki et al. (2006),29 no specific industry or occupation described; Japan | Peer-reviewed | Long work hours. Compensation for work or family of worker due to Karoshi—death or permanent disability attributed to cardiovascular disease caused by excessive work hours as defined by the Japanese Ministry of Health, Labor and Welfare as “100 h of overtime in the month before the death, or 80 h of overtime work in two or more consecutive months” | Data sources not provided | Compensation amount is provided for a single case: 45-year-old male, yearly income of 6.4 million yen (~$55,000 USD), with a wife and two children Total benefit awarded to survivors was approximately 88 million yen (~ $760,000 USD) composed of a lump-sum payment and a pension under the compensation system |
| Leger (1994),30 no specific industry or occupation described; United States of America | Peer-reviewed journal | Work occurring during times of circadian lows (2:00 and 7:00 a.m. and 2:00 and 5:00 p.m.) and overnight hours. Cost of work-related MVCs and accidents. Direct and indirect costs were provided:
|
Cost of work-related accidents and MVCs during circadian lows and overnight hours were calculated in two steps: Step 1: Direct and indirect cost of motor vehicle accidents from National Highway Transportation Safety Administration based on the severity of MVC in terms of injury/fatality per-victim or per-vehicle Cost of work-related MVCs and injuries obtained from National Safety Council. Provided direct and indirect costs for injury (incapacitating, nonincapacitating and possible injury) and fatalities Wage losses were determined using earnings data from the Bureau of Labor Statistics, adjusted for wage supplements such as social insurance, private pensions and welfare funds. Actual losses are used for nonfatal injuries and present value of all future earnings lost are considered for fatalities and permanent disabilities. Household work is also estimated using the market value of commercial household services Step 2: Proportion of work-related accidents and MVCs occurring during times of circadian lows and overnight hours were applied to total costs of work-related injuries and MVCs |
52.5% of all work-related injuries and fatalities during 1988 were estimated to be related to sleepiness due to work during circadian lows and overnight hours = $24.7 billion. ($55.57 billion in 2020 dollars) |
| National Safety Council (2019),23 all workers; United States of America | Gray literature | Night shifts, rotating shifts, or between midnight and 6 a.m. Costs related to sleep deficiencies (<7 h/night) and sleep disorders (e.g., insomnia, OSA, restless legs syndrome, shift work sleep disorder) are calculated by the NSC cost calculator for individual businesses based on user-provided information such as industry, workforce size, and geographical location Costs provided by the calculator include absenteeism, reduced productivity and health care expenses Intervention: Cost-saving estimates based on occupationally based sleep health education and sleep disorder screening programs |
Data about the specific organization is provided by the user into the Fatigue calculator Cost calculator determines cost of fatigue based on three types of information provided by the user: (workforce size, industry/occupation, workforce geographic location). Other data sources: American Time Use survey was used to determine prevalence of nonstandard work schedules for industry categories. Sleep duration was ascertained by state from the Behavioral Risk Factor Surveillance System. Adjustments for sleep problems among night shift workers were made using the National Sleep Foundation information. Costs related to sleep disorders, absenteeism and health disorders were gathered from prior studies. Presenteeism costs were obtained from the American Insomnia Survey and RAND Corporation reports |
Calculator provides estimates specific to user Total annual cost of fatigue is estimated for absenteeism, decreased productivity and healthcare The averted costs associated with an employer-initiated sleep health education program was also provided based on user-estimate of number of employees who would be engaged in the program |
| Sjølie and Bosely (2009),22 no specific industry or occupation described; Denmark | Gray literature | Night shifts. Compensation paid to women who had worked night shifts for more than 20 years at least one night per week | Danish National Board of Industrial Injuries | Thirty-eight women, all of whom have worked night shift patterns for more than 20 years, received compensation. Of those, seven who were nurses received between 30,000 and one million Danish kroner (US $4740–158,150) in compensation |
| Wong et al. (2011),31 no specific industry or occupation described; Canada | Peer-reviewed journal | Shift work: Regular nights, rotating shifts, other. The annual cost of lost-time claims due to risk of injury associated with shift work | Statistics Canada Data: Survey of Labour Income Dynamics. Includes information gathered from federal income tax returns, such as receipt of lost-time of work injury compensation benefits over the past year | Estimated cost of lost-time claims due to risk of injury associated with shift work: CA $50.5 million (US$ 43.3 million) |
3 |. RESULTS
Among the 10 articles included in this scoping review, seven were published in peer-reviewed journals (Table 1). Some of the articles estimated the economic benefits associated with interventions. While most examined costs among the general working population, two were focused on health care professionals25,28 and one focused on commercial truck drivers.26 Costs were reported for medical expenses (e.g., medical cost of treating heart disease), productivity losses, work-related motor vehicle crashes (MVCs), and health outcomes. Five studies reported costs from the employer’s perspective (i.e., internal costs),23–25,28,31 while four reported external costs from the perspective of the worker, his/her family, and society.26,27,29,30 These external costs included projected future loss of earnings and estimates of costs related to loss of ability to attend to household responsibilities. Cost of shiftwork and long work hours was described in five studies.24,27,28,30,31 Cost analyses—a method used to compare the costs of different interventions (including no intervention at all)—were provided for an obstructive sleep apnea (OSA) screening program, implementation of an employer-based sleep/fatigue educational program, and increased staffing to cover overtime hours.23,25,26 National compensation strategies to fund treatment of adverse health outcomes related to long work hours and shiftwork were also described.22,29 The majority of studies used data from multiple sources to estimate costs associated with nonstandard work hours.
We report the economic estimates in US dollars, converting from another currency when necessary. However, because most of the studies do not state the time frame or year for which the economic estimate is reported, we were unable to convert the estimates to constant dollars. Thus, the dollar values of the estimates are not commensurate.
3.1 |. Cost of shift work, long work hours, and related short sleep
Coburn24 provided an estimate of health-related expenses (i.e., cost of coronary heart disease [CHD]/heart attacks, MVCs, accidental deaths at work, and other medical and psychiatric illnesses) and costs related to reduced human productivity at work (i.e., manufacturing productivity, industrial accidents, employee turnover, and retraining costs) from the societal perspective. To calculate the cost of CHD, the risk of CHD among shift workers and prevalence of shift workers in the United States were applied to the cost of CHD from the national population as reported by National Health Care Financing Review. The cost of automobile accidents and workplace fatalities was obtained by applying the proportion of shift workers to total national costs of all accidents reported by the National Safety Council. Cost estimates related to medical and psychiatric illnesses, losses in manufacturing productivity, industrial accidents, and employee turnover and retraining were provided; however, it was unclear how these costs were estimated. The authors report health and reduced productivity costs attributed to shiftwork totaled $77 billion annually in the United States in the early 1990s.
Costs for on-the-job MVCs and work-related falls and fatalities associated with nonstandard work hours from the societal perspective were reported by Leger.30 Direct costs were defined as “monies to repair materials and rehabilitate people, such as medical and legal fees, and property damage repair cost.” Indirect costs “represent the loss of production and welfare for the individual and the nation due to premature death or disability,” which include costs of administration and human capital. Costs associated with work-related injuries/fatalities and MVCs were estimated by applying the percentage of work-related falls and on-the-job MVCs which occurred during daily circadian lows (02:00–07:00 and 14:00–17:00 h) and overnight hours, to national cost estimates from the National Safety Council. Leger estimated that a total of $24.7 billion in 1988 could be attributed to work-related injuries/fatalities and MVCs during periods of circadian lows and overnight hours. It is worth noting that these estimates include incidents occurring between 14:00 and 17:00 h, which does not fall into the typical definition of shift work. However, given the limited hours used in the analyses, it is possibile that chronic fatigue could widen the period of susceptibility for fatigue-related events.
Workers’ compensation (WC) costs for work-related injury among workers in nonstandard schedules were examined by Horwitz and McCall28 and Wong et al.31 using claims data. Horwitz and McCall28 examined the cost of lost work time—from the employer’s perspective—which may or may not have resulted in disability among hospital workers, using WC claim data from 1990 to 1997 from the Oregon Department of Consumer and Business Information and Management Division. Shift types were defined by work start time: night (8 p.m.–3 a.m.), evening (12–7 p.m.), and day shift workers (4–11 a.m.). While night shift workers claimed significantly more lost-work time compared to other shift types, and evening and night shift workers experienced a higher rate of injury than day shift, the average total cost per claim was not statistically different: night shift workers ($6715), day shift workers ($6187), and evening shift workers ($6103).
Wong et al.31 used data from the Survey of Labour and Income Dynamics, a nationally representative survey conducted by Statistics Canada which includes information gathered in federal tax returns including sources of income such as WC for work-related injuries, to assess costs from the employer’s perspective.32 Shift types were defined as: regular daytime schedule, regular night (evening and overnight shifts), rotating (between days and nights), and other (split shifts, irregular schedules, on-call, and other). Receipt of WC was used as a surrogate measure for work-related injury or disability. Population attributable fraction estimates, adjusted for demographic, socioeconomic, and occupational factors, were reported as the proportion of work injuries among the total workforce population that could be prevented if effective measures were implemented to reduce the risk of shift work on work injury. The authors found that the overall excess risk for work-related injury attributed to nonstandard schedules was 11.3%, with greater excess risk higher among women than men (14.4% vs. 8.2%, respectively). Estimates for lost-time claims due to risk of injury associated with shift work were estimated to be over CA$50.5 million (US$ 43.3 million, using conversion rate from December 30, 2005 since workers compensation was reported for 2005 for this study) by applying population attributable fraction calculations to total compensation claims from that year.
The cost of short sleep from the societal perspective, in part related to irregular work hours, was estimated by the RAND Corporation27 for five different countries (United States, Canada, United Kingdom, Germany, and Japan), as a function of a country’s lost economic output and labor productivity. A macroeconomic model of insufficient sleep was based on reduced labor force participation and resulting economic output due to higher mortality rates, prolonged periods of sickness and absenteeism, and reduced productivity. The authors also estimated the loss of future labor contributions among adolescents attributed to reduced skill development and lifetime earnings. Cost of insufficient sleep for 2015–2030 was estimated across various scenarios involving longer sleep duration. Simulation models were developed using findings from prior studies regarding losses due to mortality and reduced productivity related to short sleep. To estimate economic losses by country, macroeconomic data was used such as the capital stock (human and physical), capital-to-labor ratios, multifactor productivity and total hours worked, among others, from the Penn World Tables, the Organisation for Economic Co-operation and Development, and the World Bank. A unique aspect of these simulations were the projections of insufficient sleep among future generations and loss of economic contributions of future offspring due to early mortality losses among the current population of those with insufficient sleep. The estimated cost of short sleep for the United States ranged from $281 billion to $467 billion annually from 2015 to 2030.
3.2 |. Cost analyses of interventions
High prevalence of OSA, and working irregular schedules are common among commercial truck drivers.33–35 This increases the risk for falling asleep at the wheel and occupational crashes, necessitating the development of OSA diagnoses strategies. Gurubhagavatula et al.26 explored the tradeoffs of two (OSA) screening programs from the societal perspective: in-laboratory polysomnography for all drivers and polysomnography for only drivers with high risk of OSA (selective polysomnography) using OSA modeling algorithms as determined by body mass index, age, and gender. Employer costs in terms of testing, treatment, and MVCs were represented. The cost of MVCs attributable to OSA were estimated using US Department of Transportation data for large trucks, risk estimates of OSA-related crashes from prior studies, and reported costs from the Federal Motor Vehicle Carrier Safety Administration for large-truck and large-bus crashes which included costs of medical treatment, emergency services, property damage, lost productivity, and monetary value of the pain, suffering and reduced quality of life experienced by the victim and his or her family.
The authors estimated that the cost of no screening measures would result in $689/driver due to fixed costs of crashes attributed to missed cases of OSA. The cost of performing polysomnography on all drivers was estimated to be $920/driver. Selective polysomnography, using prescreening algorithms for OSA risk, was the most cost-effective measure and ranged from $358/driver to $372/driver, depending on the selection procedure.
A report from the National Safety Council outlined the methodology behind their “Cost of Fatigue Calculator” which estimates fatigue-related expenses—from the employer’s perspective—such as absenteeism, decreased productivity, and medical costs specific to each organization based on user-provided information such as industry, geographical location, and number of employees.23 Expenses were related to sleep deficiencies (<7 h of sleep/night) and sleep disorders (i.e., insomnia, OSA, restless legs syndrome, shift work sleep disorder). Prevalence of nonstandard schedules was identified by combining reported industry category with information from the American Time Use Survey. Proportion of all workers with sleep deficiencies was extracted from reported geographic location and linked to sleep duration by state from the Behavioral Risk Factor Surveillance System. Adjustments were made to reflect the proportion of nightshift workers with sleep deficiencies that was estimated using data from the National Health Interview Survey. Prevalence of sleep disorders was estimated using prior studies and adjusted for those working night shifts as described by the National Sleep Foundation. The number of workers with sleep deficiencies or sleep disorders was calculated by applying the proportions to user-reported organization size.
Cost per worker due to absenteeism related to sleep deficiencies and sleep disorders was derived from prior studies on insomnia. Further adjustments were made for night shift workers, based on higher absenteeism rates compared to regular daytime workers. Cost per worker attributed to reduced productivity was based on estimates of days lost to presenteeism due to insomnia and sleep deficiency (as reported by the America Insomnia Survey and the RAND Corporation) and multiplied by median hourly wage plus benefits for user-reported industry. Total health care costs due to chronic health conditions related to OSA and insomnia was determined using estimates of annual health care expenditures from prior studies and adjusted for inflation. Total organizational costs were derived by applying costs per employee to the number of employees estimated with sleep deficiencies and disorders.
The benefits associated with an employer-initiated sleep health education program was based on user estimates of the percentage of employees who would take the training. Employees who take the course might reduce the impact of sleep deficiencies and disorders, and consequently, related costs to the employer.
Drebit et al.25 explored the cost-savings of increasing nursing staff to offset overtime wages from the employer’s perspective. Costs for overtime wages among nurses from a southwest region in Canada were determined using payroll data from 2005 to 2008, which included employment status (full time, part time, casual), hourly wage rate and number of regular and overtime hours worked during each bi-weekly reporting period. Regular work hours for each employment status type and overtime pay rates were defined by pre-existing union agreements. Cumulative overtime pay was estimated to be $84.4 million CDN by the end of the 4-year follow-up period and represented 10%–12% of all wages. A simple cost analysis was conducted by converting the number of overtime hours into full-time equivalents (1879.2 h), which could have resulted in 910 full-time positions at a cost of $56.4 million. Thus, they estimated an increase in full-time staff could result in a net savings of $27.6 million. However, it is unclear if overhead and fringe benefit costs (e.g., healthcare) were included in these calculations.
3.3 |. National compensation programs
Two national compensation programs for night shift workers and families of workers who died from long work hours were described by Iwasaki et al.29 and Sjølie and Boseley22 Iwasaki et al.29 reported on the compensation mechanism from the Japanese government for the workers who have been permanently disabled or families of workers who have died due to karoshi. Loosely defined as “death due to overwork,” it is recognized by the Japanese Ministry of Health, Labor and Welfare as the death or permanent disability from cerebrovascular diseases and ischemic heart disease attributed to overwork—defined as 100 overtime hours or more for the past 1 month, or 80 overtime hours or more per month for the past 2–6 months before the onset of disease.36 Compensation for karoshi began in the 1980s primarily as litigation through court cases and did not become formally recognized by the Japanese government until 2002 when the “Comprehensive Program for the Prevention of Health Impairment Due to Overwork” was formed.36 Benefits paid include a lump sum payment to the family, funeral expenses, a yearly pension for the surviving spouse, educational expenses for children, and a yearly pension for children until they graduate from university.37,38 Despite this information, there is little information in the English-language literature about the number of claims or the total compensation awarded since the inception of this compensation program. Iwasaki et al.29 reports on a single case of karoshi-related fatality (date unknown) of a male worker, 45 years old, married with children with an annual income of ~$55,000 USD. Surviving family members were awarded ~$760,000 USD.
Following the classification of shift work as a “probable human carcinogen” by the International Agency for Research on Cancer,5 the Danish government began awarding compensation benefits to women who worked for more than 20 years in night shift work and were diagnosed with breast cancer. Under Danish employment laws, all employers must insure their workers against industrial injuries and disease, and compensatory benefits are paid by the employer’s insurers.39 The Danish National Board of Industrial Injuries adjudicates claims decisions on a case-by-case basis and exposure to shift work is weighed against other cancer-risks such as smoking to determine if the risk of nonwork-related factors are greater. Economic compensation is based on loss of working capacity, potential lost lifespan and “pain.”40 Other than descriptive information, little information is reported about the number of claims and amount awarded since the inception of this compensatory measure. The compensation amount was only described in one article found in this scoping review. Sjølie and Boseley22 reported that in 2008, 38 women who worked night shifts for at least 1 night per week for more than 20 years and were diagnosed with breast cancer were awarded 30,000 to 1 million Danish kroner (US$4740–158,150).22
4 |. DISCUSSION
Nonstandard work hours remain a necessity in certain circumstances, such as emergency services or to accommodate job tasks that may not be feasible during traditional work hours. In addition, some workers prefer nonstandard work hours with benefits such as increased wages, time for other responsibilities (e.g., dependency care) or opportunities for secondary employment.41 However, working long hours or during traditional sleeping hours has been associated with an increased risk of adverse OSH outcomes. As such, the decision to redesign work schedules or employ OSH fatigue-mitigation interventions should include several factors such as feasibility, worker well-being and economic measures. Our scoping review aimed to answer the question “how has nonstandard work schedules been described in economic terms in the current literature?” by providing information such as monetary estimates, data sources and methodologies to assist future research and decision-making processes with respect to economic considerations.
Although we started with a broad range of gray and scientific literature, we found a paucity of economic estimates related to nonstandard work hours. Results of our scoping review found that studies only analyzed costs of nonstandard work hours and related interventions. Benefits of nonstandard schedules, in the context of OSH, were not described in any of the literature captured, suggesting that this is area has not yet been explored in the English-language scientific literature. Costs reported were mainly from the perspective of the employer, which are helpful for organizational decisions. Three main sources of data were used to determine costs: risk estimates from prior studies, prevalence of nonstandard work hours and sleep impairment from national surveys, and economic data. Types of costs ranged from proximal to the worker (e.g., salary, health care) or fatigue-related event (e.g., MVCs, work injuries), to distal measures requiring further assumptions (e.g., future lost earnings, reduced productivity). WC claims were the most frequent source of information used to estimate costs.
Cost analyses were used to compare the costs associated with increased staffing to cover overtime hours, OSA screening, educational programs, and increasing sleep duration. The benefits associated with OSH interventions outweighed the associated costs in all studies. However, this is based only on a small handful of studies and thus more research is needed to explore the benefit-cost of other types of interventions. Economic costs from national compensation systems for disease or disability related to shift work and long work hours were only reported in two sources in our scoping review. While both programs have been in place for over a decade, little has been presented in the English-language literature on how compensation is calculated and how much has been awarded since their inception. Knowledge of this type of information could be useful for other countries and compensation mechanisms.
Results from this scoping review suggest that there is room for more research in this area. Future studies are needed to expand economic evaluations beyond the employer perspective to the societal perspective, to consider all benefits and costs.42–45 Assessments restricted to the employer perspective ignore an important fact: the burden that employers create is borne by their workers, the community, and society—or taxpayers—overall. The impacts of nonstandard schedules extend beyond the workplace, affecting not only the well-being of the worker, but also the worker’s family, community, and society as a whole. For example, Leigh et al.46 estimated that workers compensation covers less than 25% of the costs of occupational injury and illness in the United States; the remainder of the costs fall on workers and taxpayers.46 Therefore, analyses at the societal level consider all costs and all benefits regardless of who pays and who benefits, and this points to “externalities,” or costs borne by people or entities who should not bear them. Concentrating only on employer-based perspectives will underestimate the true costs or benefits. Therefore, considerations from the societal perspective should be used when designing and economic evaluation whose insights might be helpful for decision-makers.
More work is needed to better understand the benefits of nonstandard schedules which could include employers’ cost savings when running maintenance tasks during slower activity times and societal benefits with 24-h services such as emergency care. While prior studies have alluded to some workers’ preferences for nonstandard work hours, estimates of economic benefits from a worker perspective could help provide a more balanced approach concerning workers’ health and well-being.3,4,41 Whether workers have the choice to work nonstandard hours, including specific schedules such as permanent night shifts or rotating shifts, should also be considered as control over work schedules is positively associated with worker well-being.47
Future research directions should include longitudinal designs to assess trends in benefits and costs related to nonstandard work hours or the effectiveness of interventions over time. Additionally, while studies have mainly concentrated on costs of either shift work or long work hours, our review did not find any which examined the interaction of shift timing with shift duration. This creates potential avenues to study this, and other, interactions. Studies included in this scoping review described nonstandard schedules in broad terms (e.g., irregular schedules, long work hours, night shift work), however, there is a need to refine epidemiological methods in shift work research to improve risk estimates, with cascading effects on economic estimates.48 This could include a sector-specific approach, with emphasis on unique work conditions or job tasks (e.g., fly-in/fly-out operations, turndowns in oil, and gas organizations). Other approaches may include comparisons of shift types, shift rotations, incorporation of rest breaks between- and within- work shifts. This would provide more detailed information that could be applied to decisions about work scheduling and other work-related fatigue-mitigation interventions.
Many of the studies included in this review were conducted by combining various datasets and making assumptions to determine cost estimates. Thus, multidisciplinary approaches involving epidemiology and economics are needed to provide the different skills and expertize. We pose the opportunity for researchers and employers to share data and resources in the development of more analyses that fill these research gaps.
Supplementary Material
Footnotes
CONFLICTS OF INTEREST
The authors declare that there are no conflicts of interest.
DISCLOSURE BY AJIM EDITOR OF RECORD
John Meyer declares that he has no conflict of interest in the review and publication decision regarding this article.
ETHICS STATEMENT
The work was performed at the National Institute for Occupational Safety and Health. Human subjects institutional review and approval was not required because the work did not involve human subjects.
Publisher's Disclaimer: DISCLAIMER
The findings and conclusions in this report are those of the authors and do not necessarily reflect the official position of the National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention.
REFERENCES
- 1.National Center for Health Statistics. National Health Interview Survey, 2015. Public-use data file and documentation. Accessed November 2019. https://www.cdc.gov/nchs/nhis/nhis_2015_data_release.htm [Google Scholar]
- 2.Sloane P Economic aspects of shift and night work in industrialized market economies. Int Lab Rev 1978:117–129. [Google Scholar]
- 3.NIOSH. NIOSH training for nurses on shift work and long work hours: benefits of shift work and long work hours. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication No. 2015-115 (Revised 04/2020). 2020. Accessed September 2021. https://www.cdc.gov/niosh/work-hour-training-for-nurses/longhours/mod1/04.html [Google Scholar]
- 4.Kim M Who works nonstandard schedules voluntarily?: the role of having children. J Fam Stud. 2020;29:1–8. [Google Scholar]
- 5.International Agency for Research on Cancer. Night shift work: IARC monographs on the identification of carcinogenic hazards to humans, Vol. 124. 2020. https://publications.iarc.fr/593 [PubMed] [Google Scholar]
- 6.Dembe AE, Erickson JB, Delbos RG, Banks SM. Nonstandard shift schedules and the risk of job-related injuries. Scand J Work Environ Health. 2006;32(3):232–240. doi: 10.5271/sjweh.1004 [DOI] [PubMed] [Google Scholar]
- 7.Caruso CC. Negative impacts of shiftwork and long work hours. Rehabil Nurs. 2014;39(1):16–25. doi: 10.1002/rnj.107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wagstaff A, Lie J. Shift and night work and long working hours-a systematic review of safety implications. Scand J Work Environ Health. 2011;37(3):173–185. [DOI] [PubMed] [Google Scholar]
- 9.Moreno C, Marqueze E, Sargent C, Wright K Jr., Ferguson S, Tucker P. Working Time Society consensus statements: evidence-based effects of shift work on physical and mental health. Ind Health. 2019;75(2):139–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wong I, Popkin S, Folkard S. Working Time Society consensus statements: a multi-level approach to managing occupational sleep-related fatigue. Ind Health. 2019;57(2):228–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tompa E, Dolinschi R, de Oliveira C. Practice and potential of economic evaluation of workplace-based interventions for occupational health and safety. J Occup Rehabil. 2006;16(3):375–400. doi: 10.1007/s10926-006-9035-2 [DOI] [PubMed] [Google Scholar]
- 12.Tompa E, Dolinschi R, de Oliveira C, Irvin E. A systematic review of occupational health and safety interventions with economic analyses. J Occup Environ Med. 2009;51(9):1004–1023. doi: 10.1097/JOM.0b013e3181b34f60 [DOI] [PubMed] [Google Scholar]
- 13.Tompa E, Culyer A, Dolinschi R. Economic Evaluation of Interventions for Occupational Health and Safety: Developing Good Practice. Oxford University Press; 2008. [Google Scholar]
- 14.Wong I, Swanson N. NIOSH working hours, sleep and fatigue forum: meeting the needs of American workers and employers. AJIM. 2020. [Google Scholar]
- 15.Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18(1):143. doi: 10.1186/s12874-018-0611-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Colquhoun HL, Levac D, O’Brien KK, et al. Scoping reviews: time for clarity in definition, methods, and reporting. J Clin Epidemiol. 2014;67(12):1291–1294. doi: 10.1016/j.jclinepi.2014.03.013 [DOI] [PubMed] [Google Scholar]
- 17.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. doi: 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 18.Levac D, Colquhoun HL, O’Brien K. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69. doi: 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Belzer M, Rodriguez D, Sedo S. Paying for Safety: An Economic Analysis of the Effect of Compensation on Truck Driver Safety. Wayne State University; 2002. [Google Scholar]
- 20.Ju S Empirical study of basic violations, pay incentives, and safety: evidence from US Intrastate carriers. Wayne State University Dissertations; 2019. [Google Scholar]
- 21.Rodriguez D, Rocha M, Belzer M. The effects of trucking firm financial performance on driver safety. Transport Labor Issues Regul Reform. 2004;10:35–55. [Google Scholar]
- 22.Sjolie M, Boseley S. Breast cancer patients get landmark payout. The Guardian. March 16, 2009. [Google Scholar]
- 23.National Safety Council. Calculating the cost of poor sleep—methodology. 2017. Accessed November 2019. https://www.nsc.org/Portals/0/Documents/Fatigue%20Documents/Cost-Calculator-Methodology-Report.pdf
- 24.Coburn E Shiftwork fatigue: the $77 billion problem. Cost Eng. 1997;39(4). [Google Scholar]
- 25.Drebit S, Ngan K, Hay M, Alamgir H. Trends and costs of overtime among nurses in Canada. Health Policy. 2010;96(1):28–35. doi: 10.1016/j.healthpol.2009.12.016 [DOI] [PubMed] [Google Scholar]
- 26.Gurubhagavatula I, Nkwuo JE, Maislin G, Pack AI. Estimated cost of crashes in commercial drivers supports screening and treatment of obstructive sleep apnea. Accid Anal Prev. 2008;40(1):104–115. doi: 10.1016/j.aap.2007.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hafner M, Stepanek M, Taylor J, Troxel W, van Stolk C. Why sleep matters—the economic costs of insufficient sleep. 2016. Accessed November 2019. https://www.rand.org/pubs/research_reports/RR1791.html [PMC free article] [PubMed]
- 28.Horwitz IB, McCall BP. The impact of shift work on the risk and severity of injuries for hospital employees: an analysis using Oregon workers’ compensation data. Occup Med. 2004;54(8):556–563. doi: 10.1093/occmed/kqh093 [DOI] [PubMed] [Google Scholar]
- 29.Iwasaki K, Takahashi M, Nakata A. Health problems due to long work hours in Japan: working hours, workers’ compensation (Karoshi) and preventative measures. Ind Health. 2006;44(4):537–540. [DOI] [PubMed] [Google Scholar]
- 30.Leger D The cost of sleep-related accidents: a report for the National Commission on sleep disorders research. Sleep. 1994;17(1): 84–93. [DOI] [PubMed] [Google Scholar]
- 31.Wong IS, McLeod CB, Demers PA. Shift work trends and risk of work injury among Canadian workers. Scand J Work Environ Health. 2011;37(1):54–61. doi: 10.5271/sjweh.3124 [DOI] [PubMed] [Google Scholar]
- 32.Statistics Canada. SLID definitions, data sources and methods. Detailed information for 2008 Accessed May 2019. http://www.statcan.gc.ca/cgi-bin/imdb/p2SV.pl?Function=getSurvey%26SDDS=3889%26lang=en%26db=imdb%26adm=8%26dis=2
- 33.Gurubhagavatula I, Maislin G, Pack A. An algorithm to stratify sleep apnea risk in a sleep disorders clinic population. Am J Respir Crit Care Med. 2001;164(10 Pt 1):1904–1909. [DOI] [PubMed] [Google Scholar]
- 34.Howard ME, Desai AV, Grunstein RR, et al. Sleepiness, sleep disordered breathing and accident risk factors in commercial vehicle drivers. Am J Respir Crit Care Med. 2004;170:1014–1021. [DOI] [PubMed] [Google Scholar]
- 35.Stoohs R, Bingham L, Itoi A, Guilleminault C, Dement W. Sleep and sleep-disordered breathing in commercial long-haul truck drivers. Chest. 1995;107:1275–1282. [DOI] [PubMed] [Google Scholar]
- 36.Araki S Death due to overwork (Karoshi): causation, health service and life expectancy of Japanese males. JMAJ. 2005;48:92–98. [Google Scholar]
- 37.Ministry of Health Labour and Welfare LSB Industrial accident compensation insurance application guidance for foreign workers. 2014. https://www.mhlw.go.jp/new-info/kobetu/roudou/gyousei/kantoku/dl/161108-01.pdf Accessed July, 2020.
- 38.Takahashi M. Director, Research Center for Overwork-Related Disorders; Japanese Ministry of Health Labor and Welfare. (Personal communication, 2020). [Google Scholar]
- 39.Hansen J. Women with night shift work and breast cancer: the situtation in Denmark. J Epidemiol Commun Health. 2010;64(12): 1025–1026. [DOI] [PubMed] [Google Scholar]
- 40.Hansen J. Senior Researcher. Danish Cancer Society. (Personal communication, 2020). [Google Scholar]
- 41.Finn P. The effects of shift work on the lives of employees. Monthly Lab Rev. 1981;104:31–35. [Google Scholar]
- 42.Gramlich E. A Guide to Benefit-Cost Analysis. Waveland Press; 1997. [Google Scholar]
- 43.Gramlich E. Benefit-cost analysis in the public policy process. Econ Financ Rev. 2004;11(1):27–43. [Google Scholar]
- 44.Viscusi W. Pricing Lives: Guideposts for a Safer Society. Princeton University Press; 2018. [Google Scholar]
- 45.Haddix A, Teutsch S, Corso P. Prevention Effectiveness: A Guide to Decision Analysis and Economic Evaluation. 2nd Ed. Oxford University Press; 2003. [Google Scholar]
- 46.Leigh J, Markowitz S, Fahs M, Landrigan P. Costs of Occupational Injuries and Illnesses. University of Michigan Press; 2000. [Google Scholar]
- 47.Barton J. Choosing to work at night: a moderating influence on individual tolerance to shift work. J Appl Psychol. 1994;79(3):449–454. [DOI] [PubMed] [Google Scholar]
- 48.Knutsson A. Methodological aspects of shift-work research. Chronobiol Int. 2004;21(6):1037–1047. doi: 10.1081/cbi-200038525 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


