Abstract
Traumatic injuries to the axillary artery or subclavian artery along with a brachial plexus injury are infrequent. Although the traditional management has been conservative because of robust collaterals, the functional improvement of the limb depends on the degree of brachial plexus injury and on the revascularization status. We report three cases of endovascular repair post-traumatic axillo-subclavian artery injuries followed by brachial plexus injury with good functional outcomes. Endovascular repair of post-traumatic subclavian and axillary artery injuries followed by brachial plexus injury is safe and feasible, and improves limb outcomes.
Keywords: Endovascular repair, Axillo-subclavian artery injury, Brachial plexus injury, Trauma
Introduction
Upper extremity vascular injury is less common than lower extremity and accounts for 30% to 40% of extremity arterial trauma [1, 2]. The associated limb loss with upper extremity arterial injury ranges from 1 to 28% with amputation rates of less than 10% [2]. Blunt injuries tend to have more morbidity than penetrating injuries due to the associated concomitant injuries. Major penetrating vessel injuries involving either axillary or subclavian or both vessels are mostly associated with a clavicle fracture, rib fractures, and lung contusions, whereas vascular injuries along with brachial plexus are seen in blunt thoracic trauma in high-speed vehicular accidents, falling from a height, and gunshot injuries [2]. Despite the utilization of endovascular techniques in the setting of aneurysmal and atherosclerotic disease, reports remain limited in endovascular management of traumatic thoracic vascular injuries. However, with the uncertainty of the patient selection and optimal management algorithm, the role of endovascular treatment and timing of intervention of vascular injury and brachial plexus injury continues to evolve [2, 3]. The acute neurological injury tends to heal in the subacute phase and the remnant neuronal injury is apparent only after 12 weeks. Early revascularization of the injured vessel along with early brachial plexus repair has shown to have a better functional outcome [2–4]. We report three cases of post-traumatic subclavian and axillary artery injuries that were managed successfully in the subacute/chronic phase with endovascular revascularization followed by elective brachial plexus repair and had a partial functional outcome with improvement in Medical Research Council (MRC) grade of the muscle power to 2/3 in most of the muscle groups in the shoulder and elbow.
Case series
A 23-year-old male presented to us with pain and weakness in the right arm, forearm, and hand for 2 months following an alleged road traffic accident (RTA). He had sustained an injury to the right shoulder region following which he developed weakness in the same limb. He was managed conservatively elsewhere. There were no other associated injuries. At presentation, the motor examination showed MRC grade 2 power over trapezius muscle and MRC grade 0 power over serratus anterior, supra, and infraspinatus, deltoid, biceps, triceps, pronator teres, long flexors, and all other muscles supplied by medial ulnar and radial nerve. There was a sensory loss in all dermatomes from C5 to T1. Upper limb pulses (brachial/radial/ulnar) were not palpable. He was diagnosed to have complete right brachial plexus and subclavian artery injury. A magnetic resonance angiogram (MRA) was suggestive of short-segment stenosis of the right proximal subclavian artery distal to the origin of the right vertebral artery (Fig. 1a). He underwent endovascular recanalization with good results (Fig. 1b, c). Five months later, he underwent brachial plexus repair (Table 1). At 3 years follow-up, there was a partial functional improvement (MRC grade 2/3 in the upper limb).
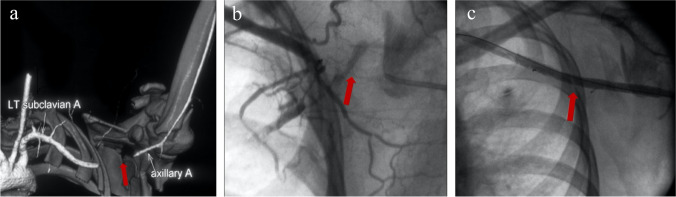
A 29-year-old male presented to us with a flail upper limb after RTA 7 months ago. He had wasting of the entire upper limb and periscapular region. Motor and sensory examination of the upper limb showed MRC grade 0 power in the median nerve, ulnar nerve, and radial nerve supplied regions. Tinel’s test was positive in the shoulder region. He was diagnosed to have a left total brachial plexus injury and left scapula-thoracic dissociation. Upper limb pulses (brachial/radial/ulnar) were not palpable. Computed tomography angiogram (CTA) confirmed the occlusion of the first part of the axillary artery with distal reformation through collaterals at the third part of the axillary artery (Fig. 2a). He underwent endovascular recanalization (Fig. 2b, c). All distal pulses were palpable post-procedure, and the hand was well perfused. Four months later, he underwent staged reconstruction of the brachial plexus and wrist arthrodesis (Table 1). At 5 years follow-up, he had partial functional improvement (MRC grade 2/3 in the upper limb).
A 48-year-old gentleman presented with an open fracture of the left clavicle involving the brachial plexus injury and subclavian artery following an RTA, 6 months ago. There was a loss of motor and sensory function involving the arm and forearm with a positive sulcus sign. There was no active range of movement over the shoulder, elbow, wrist, or fingers. The upper limb pulses (brachial/radial/ulnar) were not palpable. CTA showed complete occlusion at the first part of the left subclavian and reformation through collaterals at the third part of the subclavian artery (Fig. 3a). He underwent left subclavian artery recanalization and stenting (Fig. 3b, c). Two months later, he underwent brachial plexus repair (Table 1). At 3 years follow-up, he had partial functional improvement (MRC grade 2/3 in the upper limb).
Fig. 1.
a MRA showing occlusion of the first part of the axillary artery with distal reformation through collaterals at the third part of the axillary artery. b Diagnostic angiogram. c Right subclavian artery recanalization and stenting with balloon-expandable covered stent 6 × 38 mm (Advanta V12™, Getinge)
Table 1.
Demography, endovascular intervention, and brachial plexus repair details
| Case | Age Gender |
Cause of injury Hemodynamic stability |
Interval from trauma to neurological dysfunction | Diagnosis | Vascular repair | Interval from injury to vessel repair (months) | Brachial plexus repair | Interval from vessel repair to nerve surgery (months) | Functional outcome | Follow-up (years) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 |
23 M |
Road traffic accident Stable |
Immediately |
Total brachial plexus injury Right subclavian arterial occlusion |
Right subclavian artery recanalization and stenting with balloon-expandable covered stent 6 × 38 mm (Advanta V12™, Getinge) | 2 | Exploration, Hemi accessory nerve to suprascapular neurotization and right 3rd, 4th, and 5th intercostal nerve to musculocutaneous nerve (MCN) neurotization | 5 |
Partial (MRC grade 2/3) |
3 |
| 2 |
29 M |
Road traffic accident Stable |
Immediately | Left subclavian artery injury and total brachial plexus injury | Recanalization/percutaneous transluminal angioplasty with a 7 mm × 40 mm non-compliant (Mustang, Boston Scientific) balloon and stenting of the left axillary artery with a self-expandable 6 mm × 80 mm bare-metal stent (Life stent™, Bard) | 7 | Exploration of the infraclavicular plexus, musculocutaneous and median nerve identification, contralateral C7 anterior division harvest, reversed ulnar nerve harvest, micro neurorrhaphy C7 and median and MCN with ulnar nerve graft and total wrist arthrodesis | 4 |
Partial (MRC grade 2/3) |
5 |
| 3 |
48 M |
Road traffic accident Stable |
5 days later |
Left subclavian artery injury and total brachial plexus injury Clavicular fracture |
Left subclavian artery recanalization and stenting with balloon-expandable 6 × 55 mm bare-metal stent (Scuba™, Invatec) | 6 | Left brachial plexus exploration, upper trunk to MCN, and median nerve neurotization via sural and radial cutaneous grafts | 2 |
Partial (MRC grade 2/3) |
3 |
Fig. 2.
a CTA showing 4-cm occlusion at the first part of the left subclavian and reformation through collaterals at the third part of the subclavian artery. b Diagnostic angiogram. c Recanalization/percutaneous transluminal angioplasty with a 7 mm × 40 mm non-compliant (Mustang, Boston Scientific) balloon and stenting of the left axillary artery with a self-expandable 6 mm × 80 mm bare-metal stent (Life stent™, Bard)
Fig. 3.
a CTA showing 3.5-cm stenosis in the second part of the subclavian artery. b Diagnostic angiogram. c Left subclavian artery recanalization and stenting with balloon-expandable 6 × 55 mm bare-metal stent (Scuba™, Invatec)
Discussion
The endovascular approach to the management of various vascular diseases has become the standard of care and the same has been used in the treatment strategy for vascular trauma [1, 2]. The use of catheter-based approaches to treat proximal upper extremity and thoracic vascular injuries may provide benefits in the acute environment, as well as less-urgent traumatic sequelae. This includes avoiding dissection near venous injuries and the brachial plexus, gaining rapid proximal control with balloon occlusion, and ensuring blood flow continuity [1, 3]. It can also be used as a bridge therapy for definitive treatment. In stable patients, endovascular repair of axillo-subclavian lesions has been performed with success rates of over 93% [2]. Open vascular repair is done mainly when there was a penetrating injury or extensive contaminated wound [3].
Multidisciplinary teams and staged procedures are required for the management of axillo-subclavian vessel injury in association with brachial plexus injury. Though these entities are very rare, often they are associated with high morbidity and mortality [2, 3, 5]. Initial experience with neurovascular injuries seemed to have poor outcomes and was done to facilitate functional rehabilitation of major limb amputations. However, in the later series, good outcomes were seen where early revascularization was followed by repair of brachial plexus injury was performed. A study from a single large trauma center by Kou et al. reported Glasgow Coma Scale (GCS) ≤ 12, Abbreviated Injury Scale (AIS) of head ≥ 3, and presence of clavicular or scapular fractures as independent risk factors for traumatic axillo-subclavian vessel injuries [5]. A systematic review and meta-analysis of open surgical and endovascular management of thoracic outlet vascular injuries by Sinha et al. showed that there was no difference in mortality ratio when compared between open surgical repair and endovascular repair; however, the endovascular repair had a lesser operating time [2], whereas Branco et al. in 153 patients showed significantly lower in-hospital mortality and surgical site infection in patients undergoing endovascular revascularization [6]. DuBose et al. showed the successful use of the endovascular revascularization process in 96.9% of patients. It also showed good follow-up results in terms of stent patency [7]. Once the perfusion of the limb is attained, brachial plexus repair yields better and faster outcomes. The outcomes of brachial plexus repair depend on the time of injury and surgical intervention, concomitant vascular injuries, the age of the patient, and the length of the nerve graft [2, 4, 5]. In our case series, all the three patients were managed conservatively elsewhere and then referred to us in the subacute or chronic phase.
Both self-expanding and balloon-expandable covered stents have been reported to be effective in managing thoracic vascular injuries [1–3, 7]. The self-expanding covered stents have good radial strength and are less likely to fracture or become compressed in this region; balloon-expandable stents provide a safer alternative with their more precise control of deployment if needs to be placed close to a major branch vessel like the vertebral artery [1, 3, 8, 9]. Uncovered or bare-metal stents are an excellent alternative to deal with small dissections or intimal flaps. In our case series, we used 1 balloon-expandable stent graft in the proximal subclavian artery as it required to be placed close to the vertebral artery, 1 self-expanding covered stent graft in the axillary artery, and 1 bare-metal balloon-expandable stent.
Brachial plexus injuries include a combination of neuropraxia, axonotmesis, neurotmesis, and root avulsions. Other than in open-cut injuries, the accepted practice is to wait for 3 months for possible nerve recovery. If no recovery is seen by this period, an elective exploration and definitive nerve surgery like nerve transfers or nerve grafting is done. Total brachial plexus avulsion injuries tend to have a poor prognosis [10]. We have also observed that double fascicular nerve transfer in traumatic upper brachial injuries gives superior results in the strength of elbow flexion [10]. In this report, the brachial plexus was repaired electively after the revascularization. There was a partial functional recovery in all the cases (MRC grade 2/3 power in the shoulder and elbow). The outcomes are superior to non-revascularized upper limbs which rely on collateral circulation rather than inline flow. The follow-up is usually done clinically at 3, 6, and 12 months and then annually for the next 5 years. In some cases, electromyography and nerve conduction tests are done to evaluate the recovery. All the patients were started on dual antiplatelets for 10 weeks followed by single antiplatelet for 1 year and usually, stopped 1 week before brachial plexus repair.
Conclusion
Endovascular repair of post-traumatic subclavian and axillary artery injuries with concomitant brachial plexus injury is safe and feasible, and improves limb outcomes.
Author contribution
Concept and design: DH, AAK, SPR.
Analysis and interpretation: DH, AAK, SA.
Data collection: DH, AAK.
Writing the article: DH, AAK.
Critical revision of the article: DH, AAK, PP, ADS, SA, BPT.
Final approval of the article: all authors.
Overall responsibility: AAK.
Funding
None.
Data availability
Not applicable.
Code availability
Not applicable.
Declarations
Ethical approval
As this was a case report with no experimental treatment, ethics committee approval was not obtained. There was no violation of human or animal rights.
Informed consent
As patient-identifiable information is not provided in the report, informed consent to publish was not obtained.
Conflict of interest
The authors declare no competing interests.
Footnotes
The author Professor Sunil Agarwal is deceased (04.02.2020).
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Darpanarayan Hazra, Email: drdarpahazra@gmail.com.
Albert Abhinay Kota, Email: albertkota@cmcvellore.ac.in.
Sam Pon Raj, Email: samdan81@gmail.com.
Prabhu Premkumar, Email: prabhupremkumar@yahoo.co.in.
Andrew Dheepak Selvaraj, Email: drdevdeepak2000@yahoo.com.
Sunil Agarwal, Email: agarwalcmcvellore@gmail.com.
Binu Prathap Thomas, Email: binu@cmcvellore.ac.in.
References
- 1.Starnes BW, Arthurs ZM. Endovascular management of vascular trauma. Perspect Vasc Surg Endovasc Ther. 2006;18:114–29. doi: 10.1177/1531003506293418. [DOI] [PubMed] [Google Scholar]
- 2.Sinha S, Patterson BO, Ma J, et al. Systematic review and meta-analysis of open surgical and endovascular management of thoracic outlet vascular injuries. J Vasc Surg. 2013;57:547–567.e8. [DOI] [PubMed]
- 3.Shalhub S, Starnes BW, Hatsukami TS, Karmy-Jones R, Tran NT. Repair of blunt thoracic outlet arterial injuries: an evolution from open to endovascular approach. J Trauma. 2011;71:E114–21. [DOI] [PubMed]
- 4.Martin E, Senders JT, DiRisio AC, Smith TR, Broekman MLD. Timing of surgery in traumatic brachial plexus injury: a systematic review. J Neurosurg. 2018 doi: 10.3171/2018.1.JNS172068. [DOI] [PubMed] [Google Scholar]
- 5.Kou H-W, Liao C-H, Huang J-F, et al. Eighteen years’ experience of traumatic subclavian vascular injury in a tertiary referral trauma center. Eur J Trauma Emerg Surg. 2019;45:973–978. doi: 10.1007/s00068-018-01070-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Branco BC, Boutrous ML, DuBose JJ, et al. Outcome comparison between open and endovascular management of axillosubclavian arterial injuries. J Vasc Surg. 2016;63:702–9. doi: 10.1016/j.jvs.2015.08.117. [DOI] [PubMed] [Google Scholar]
- 7.DuBose JJ, Rajani R, Gilani R, et al. Endovascular management of axillo-subclavian arterial injury: a review of published experience. Injury. 2012;43:1785–92. doi: 10.1016/j.injury.2012.08.028. [DOI] [PubMed] [Google Scholar]
- 8.Duerig TW, Wholey M. A comparison of balloon- and self-expanding stents. Minim Invasive Ther Allied Technol. 2002;11:173–8. doi: 10.1080/136457002760273386. [DOI] [PubMed] [Google Scholar]
- 9.Xenos ES, Freeman M, Stevens S, Cassada D, Pacanowski J, Goldman M. Covered stents for injuries of subclavian and axillary arteries. J Vasc Surg. 2003;38:451–4. doi: 10.1016/S0741-5214(03)00553-6. [DOI] [PubMed] [Google Scholar]
- 10.Srampickal GM, Mathew A, Raveendran S, Yadav BK, Thomas BP. Restoration of elbow flexion in adult traumatic brachial plexus injury - a quantitative analysis of results of single versus double nerve transfer. Injury. 2021;52:511–515. doi: 10.1016/j.injury.2020.10.090. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.
Not applicable.