Abstract
Introduction
To evaluate emergency medical services (EMS) professional response to escalating threats of violence during simulated patient encounters and describe differences in behaviors by characteristics.
Methods
EMS professionals of a large county‐based system participated in 1 of 4 standardized patient care scenarios. Each 8‐minute scenario included escalated threats of violence such that EMS personnel should escape the scene for safety. Trained evaluators recorded EMS professionals' performance using standardized data elements. Outcomes included EMS personnel escape and verbal de‐escalation attempts. Descriptive statistics and univariable odds ratios (OR) with 95% confidence intervals (95% CI) are reported.
Results
There were 270 EMS professionals evaluated as individual members of 2‐person crews. Overall, 54% escaped the unsafe scene and 54% made an adequate de‐escalation attempt; 20% did not make an adequate de‐escalation attempt nor escape the unsafe scene. Paramedics demonstrated lower odds of escaping compared to emergency medical technicians (OR: 0.40; 95% CI: 0.17–0.94), yet greater odds of adequate de‐escalation (OR: 3.17, 95% CI: 1.38–7.31). EMS professionals with more than 20 years of experience (OR: 0.32, 95% CI: 0.13–0.79, ref:2 years or less) and those with military experience (OR: 0.37; 95% CI: 0.17–0.81) demonstrated reduced odds of escaping. Crisis intervention team (CIT) training was associated with reduced odds of escape (OR: 0.38; 95% CI: 0.21–0.69), but increased odds of adequate de‐escalation (OR: 2.19; 95% CI: 1.19–4.04).
Conclusions
Nearly half of EMS professionals did not remove themselves from a simulated patient care scenario with an escalating threat of physical violence. EMS‐specific training for de‐escalation as a first‐line technique, recognizing imminent violence, and leaving a dangerous environment is needed.
Keywords: education, emergency medical services, occupational violence, simulation
1. INTRODUCTION
1.1. Background
Emergency medical services (EMS) professionals frequently encounter and must react to complex and high‐stress situations that result in increased risk for sustaining occupational injuries. 1 , 2 One source of injury that is of growing concern globally is work‐related violence. 3 , 4 Estimating how often EMS personnel are victims of assaults from patients or bystanders is complicated because of underreporting. However, surveys among EMS professionals suggest that between 53% and 93% have experienced at least 1 encounter involving physical or verbal violence in their careers. 4 , 5 , 6 In addition to physical injury, a growing body of literature has shown that assaults against EMS personnel have significant long‐term consequences including higher stress levels, loss of job satisfaction, anxiety, and negative effects on personal relationships. 7 , 8
1.2. Importance
The quality and depth of training EMS professionals receive related to the risk of violence on the job and how to respond to and mitigate this risk vary widely. 9 During initial EMS education programs, EMS professionals have traditionally been trained to confirm “scene safety” upon arriving at a response location. 10 , 11 If a scene becomes potentially unsafe, EMS personnel are instructed to remove themselves from the scene and wait for law enforcement to arrive. 10 Although verbal de‐escalation is an important first‐line skill for preventing assaults, there is no standardized de‐escalation training specifically for EMS professionals on a national level. Local training at EMS agencies varies. Some EMS systems provide education related to potentially violent encounters, such as the crisis intervention team (CIT) training designed for law enforcement personnel in encounters involving behavioral health emergencies. 12 However, unlike law enforcement personnel, the role of EMS personnel is not to confront or control offenders and the use of force by non‐law enforcement personnel is subject to legal limitations. The effects of EMS personnel undergoing training designed for professions with distinct roles such as law enforcement have not been thoroughly explored. Overall, little is known regarding how EMS professionals behave when experiencing escalating threats of violence during a response.
1.3. Goals of this investigation
The primary objective of this study was to describe EMS professionals’ responses to escalating threats of violence during simulated patient encounters, specifically in terms of de‐escalation attempts and leaving the unsafe environment. The secondary objective was to determine whether these behaviors differed by EMS professionals' characteristics. We hypothesized that personnel with greater EMS experience and previous CIT training would be more likely to escape the threatening situation and demonstrate adequate de‐escalation attempts during the encounter. Observing EMS professionals’ behaviors when faced with a potentially violent encounter is a first step toward understanding whether there is a need for training related to these unique situations designed specifically for EMS personnel.
2. METHODS
2.1. Study design and setting
We conducted a simulation‐based study of EMS professionals' reactions to patient encounters with threats of violence. These simulations were conducted as part of regularly scheduled EMS system‐wide continuing education sessions. This research project was deemed exempt by the Institutional Review Board of WakeMed Health and Hospitals.
The Bottom Line.
Violence against emergency medical services (EMS) professionals is not new but does appear to be growing. In this study 270 EMS professionals participated in simulated patients encounters involving threats of violence; 20% did not make an adequate de‐escalation or escape attempt. This study shows that EMS professionals need additional training to recognize and manage unsafe clinical situations.
Participants included EMS professionals working for a large county‐based system in North Carolina. At this agency, crews consist of 2 EMS professionals with the following possible configurations: dual paramedic, EMT/paramedic, or advanced EMT (AEMT)/paramedic. On duty EMS crews regularly participate in live‐action simulation‐based learning experiences using mannequins, standardized patients, and role players. As part of standard practice, simulations involve a facilitator and a simulation operations specialist. Sessions are audio‐video recorded for debriefing and teaching purposes. The scenarios for this study were incorporated into these regularly scheduled simulation training sessions.
2.2. Simulation environment and scenario development
All scenarios for this study were designed to be carried out in a modified simulation room operated by a public safety training program at a local community college. The simulation room contained a movable wall system that allowed configuration of divided spaces. The main room for each scenario was purposefully small at approximately 16 × 20 feet so that EMS professionals would be in close proximity with the patient and aggressor. The main room had 2 doors: the front door where EMS professionals entered the scenario and the rear door used by the aggressor to enter and leave the scenario at the indicated times. Evaluators observed the main room through a 2‐way mirrored window that did not allow participants to see evaluators. All furniture for scenarios was constructed out of tactical foam for safety. Appendix S1 contains images of scenario setups within the simulation room.
Using an iterative process, a work group of EMS physicians, EMS educators, and law enforcement training staff developed 4 simulation scenarios to assess EMS professionals responses to threatening situations. Each scenario included a patient (standardized patient or mannequin) and a non‐patient aggressor (role player). This study was focused entirely on EMS professionals behaviors and interpersonal interactions rather than patient care. All scenarios were designed to continue escalating independent of EMS professionals actions, such that they should remove themselves from the scenario location for safety. The 8‐minute scenarios were standardized for timing on 5 distinct phases of escalation: entry of a distractor, initiation of loud and distracting noise, aggressor gets louder and moves closer to crew members, aggressor makes physical contact with patient or other role player, and aggressor makes physical contact with 1 of the EMS professionals.
2.2.1. Scenario A: Possible overdose
EMS is dispatched to a residence for a reported sick person. Upon arrival, EMS is met by the caller (role player) who states that the patient (standardized patient) tried to commit suicide by overdosing with acetaminophen and shows an empty pill bottle. The patient refuses to speak with EMS and the caller continues to urge EMS to do something. The patient turns on loud music. The caller becomes more and more upset with EMS demanding that something be done for the patient and at the 7‐minute mark, the caller grabs or pushes an EMS crew member and screams, “Why aren't you doing anything?”
2.2.2. Scenario B: Intoxicated person
EMS is dispatched to an alley between 2 buildings for a reported sick person. Upon arrival, EMS sees a person (standardized patient) who appears to have just been awoken from sleep. A strong odor of alcohol is noted, and an empty alcohol container is tucked in the patient's clothing. A second person (role player) stumbles onto the scene and reports to be a friend of the patient. The friend also appears to be intoxicated. The friend tells EMS that he will take care of the patient and starts to interfere with patient care. Loud traffic noises begin. The friend gets louder and shouts at EMS that the patient “doesn't need to go to the hospital. He's just drunk!” At the 7‐minute mark the friend grabs an EMS crew member and shouts, “He's OK!”
2.2.3. Scenario C: Aggressive family member
EMS is dispatched to a residence for a reported sick person. Upon arrival, EMS is met by the patient's son (role player) who states that he called for his mother. He was unable to wake her up today. EMS sees a female, approximately 60 years old, lying in bed (mannequin). The patient is pulseless, apneic, and has signs of obvious death (rigor and lividity). The patient's other son arrives (role player) and demands to know why nothing is being done for his mother. A dog starts barking loudly in the other room. Becoming hysterical, the second son gets louder and begs the EMS crew do something for his mother. At the 7‐minute mark, the second son grabs an EMS crew member and shouts, “Do something now!”
2.2.4. Scenario D: Domestic violence
EMS is dispatched to a residence for a person with a traumatic injury. Upon arrival, EMS sees a patient (standardized patient) seated in the living room. The patient has redness, swelling, and a laceration on one side of the face. The patient reports that they fell and are fine. The patient's spouse (role player) enters the room carrying a bottle of beer. The spouse tells EMS that the patient is fine. A baby begins to cry loudly from the other room. The spouse gets louder and demands that the EMS crew leave and throws the beer bottle to the floor. At the 7‐minute mark, the spouse pushes an EMS crew member toward to door and shouts “Get out!”
Appendix S2 contains the complete scenario descriptions and timelines.
2.3. Evaluator rubric
Owing to the novel nature of these simulations, an evaluation rubric was specifically developed to assess EMS professionals' behaviors during the scenarios (see Appendix S3). De‐escalation attempts were rated using a 5‐point scale: (1) no attempt to deescalate the aggressor, (2) minimal effort made to calm the aggressor, (3) some reasonable effort made to calm the aggressor, (4) moderate effort made to calm the aggressor, and (5) great effort made to calm the aggressor. A separate data element was used to assess whether the EMS professional's behavior contributed to the escalation of the scenario using a similar 5‐point scale: (1) no attempt was made to deescalate, (2) no crew member remained neutral, (3) crew member's actions mildly escalated the situation; (4) crew member had some verbal engagement with the distractor, and (5) crew member actively engaged with distractor physically and verbally.
2.4. Role player and evaluator training
As simulations involving threatening behavior and physical violence are not common practice in EMS, maintaining safety throughout the scenario was top priority. Thus, certified law enforcement instructors with experience in threat‐based training served as role players. All evaluators were experienced EMS professionals with familiarity in simulation facilitation and evaluation. Role players and evaluators attended a week‐long course to standardize performance, data collection, and scoring for each scenario. During scenarios, role players were dressed in role‐appropriate attire. As practice scenarios were conducted with role players, evaluators practiced using the rubric. After each practice scenario, debriefings were held with role players to discuss any deviations from the script or other variations in performance. Debriefings were held with evaluators to discuss any scoring differences to reduce variability in scoring.
2.5. Simulation session logistics and data collection
To facilitate setup after each completed simulation session, a single scenario was preselected for each training day. Based on a predetermined condensed 14‐day training schedule, on‐duty EMS crews were called in by agency training staff to participate in the simulation as part of continuing education. EMS crews were scheduled to prevent overlap and exchange of information regarding the scenario. Crews were told that they would participate in a “patient care scenario” but otherwise blinded to the purpose of the simulation. Upon arriving at the simulation location, EMS professionals were asked to bring in all portable equipment from the ambulance including the stretcher, treatment bags, monitor/defibrillator, and oxygen tank. Before entering the scenario, basic demographic information was collected for each participant using a standardized paper questionnaire. This form included questions regarding gender, certification level, years of 911 EMS experience, military experience, law enforcement experience, and past crisis intervention training.
A staff member was designated as the safety officer for each simulation session. Before entering the scenario, all EMS professionals were asked to remove any sharp objects (eg, pocket knives, trauma shears, pens, keys, etc) from their person and the safety officer performed a secondary pat down to prevent injuries from unexpected EMS professionals' behavior. The designated safety officer was also responsible for monitoring the scenario and stopping the simulation in the event of any safety concerns for actors or EMS professionals. This was left to the discretion of the safety officer to determine that a true threat of physical injury was present. During the scenario, the safety officer was positioned outside the simulation space and used a long pole with a flag to discretely signal time cues for the role player to transition to each phase of the escalation.
Immediately before entering the scenario, a briefing was given to the EMS professionals that included safety instructions and scenario dispatch information (See Appendix S4). The 2‐person crew participated in the scenario as a team but were evaluated individually. Each crew member was assigned a number and letter for identification during the scenario. The number and letter were documented by the evaluator on the participant's evaluation form. One evaluator was assigned to each crew member.
Upon completion of the scenario, EMS professionals were administered a post‐simulation paper questionnaire. EMS professionals were asked to rate how realistic the scenario was using a 5‐point scale ranging from 1‐not at all to 5‐completely. The questionnaire also asked EMS professionals to rate whether they would have felt threatened had this scenario occurred in a real‐life situation using the same 5‐point scale. Before exiting the training session, participating crews were asked to avoid sharing any information related to the scenario or purpose of the simulation with other EMS professionals.
Collective debriefing sessions were conducted system‐wide during regularly scheduled continuing education sessions 30 days after the all scenarios were completed. These debriefing sessions were facilitated by EMS and law enforcement instructors using video recordings and data collected during the scenarios.
2.6. Measures
The primary outcome was whether or not the EMS professional escaped the unsafe scene before the 8‐minute scenario ended. Secondary outcomes were related to verbal de‐escalation attempts during the scenario. Professionals who received an evaluator rating of 3 (some reasonable effort to calm the aggressor) or higher on the 5‐point scale regarding their attempt to de‐escalate the aggressor were classified as having made an adequate de‐escalation attempt.
EMS professional responses to the post‐simulation questionnaire regarding the perceived degree of reality of the scenario were dichotomized to “realistic” (response options 4 and 5) and “not realistic” (response options 1, 2, and 3). Similarly, participant responses to the item assessing whether or not they would have felt threatened had this scenario occurred in real life were dichotomized to “threatening” (response options 4 and 5) and “not threatening” (response options 1, 2, and 3).
2.7. Statistical analysis
Descriptive statistics, including frequencies and proportions, were calculated. Differences in EMS professional characteristics across the 4 scenarios were assessed using chi‐square tests. Outcomes were also compared across EMS professional characteristics and training experience using chi‐square tests. For the ordinal categories of years of EMS experience, stepwise trends were assessed using a non‐parametric test for trend. Using logistic regression, univariable odds ratios (OR) and 95% confidence intervals (95% CI) were calculated to assess the association between EMS professional characteristics and the outcomes of escaping the unsafe scenario and making an adequate de‐escalation attempt.
3. RESULTS
A total of 270 EMS professionals were evaluated as individual members of 2‐person teams between November 23, 2015 and December 17, 2015. Most participants were certified at the paramedic level (79%, n = 204), 10% (n = 26) were AEMTs, 11% (n = 29) were EMTs. The majority were male (66%, n = 179). Nearly half of EMS professionals (45%, n = 118) reported 10 or more years of 911 EMS experience. A total of 13% (n = 34) of EMS professionals reported prior military experience and 10% reported experience in law enforcement. Nearly one quarter (23%, n = 59) had previously received CIT training (Table 1).
TABLE 1.
Comparison of proportion of EMS professionals who escaped the unsafe scenario by personal characteristics
| Escaped (54%, n = 147) row % (n) | Did not escape (46%, n = 123) row % (n) | P value | |
|---|---|---|---|
| Certification level | 0.07 | ||
| EMT | 72% (21) | 28% (8) | |
| AEMT | 62% (16) | 38% (10) | |
| Paramedic | 51% (104) | 49% (100) | |
| Sex | 0.0 | ||
| Female | 63% (57) | 37% (34) | |
| Male | 50% (90) | 50% (89) | |
| Years of 911 EMS experience | 0.02 | ||
| 0 to 2 | 65% (22) | 35% (12) | |
| 2 to 5 | 58% (22) | 42% (16) | |
| 5 to 10 | 58% (41) | 42% (30) | |
| 10 to 20 | 57% (39) | 43% (30) | |
| 20+ | 37% (18) | 63% (31) | |
| Military experience | 0.01 | ||
| Yes | 33% (11) | 67% (22) | |
| No | 57% (130) | 43% (97) | |
| Law enforcement experience | 0.36 | ||
| Yes | 46% (12) | 54% (14) | |
| No | 56% (130) | 44% (104) | |
| Previous CIT training | |||
| Yes | 36% (21) | 64% (38) | <0.01 |
| No | 60% (119) | 40% (81) | |
| Scenario | 0.16 | ||
| A–possible overdose | 57% (54) | 43% (40) | |
| B–intoxicated person | 59% (26) | 41% (18) | |
| C–aggressive family member | 59% (39) | 41% (27) | |
| D–domestic violence | 42% (28) | 58% (38) | |
| Felt scenario was realistic | 0.30 | ||
| Yes | 53% (115) | 47% (104) | |
| No | 61% (28) | 39% (18) | |
| Felt threatened during scenario | 0.05 | ||
| Yes | 59% (100) | 41% (70) | |
| No | 46% (46) | 54% (53) |
Abbreviations: AEMT, advanced emergency medical technician; CIT, crisis intervention team, EMS, emergency medical services; EMT, emergency medical technician.
Approximately half of EMS professionals (54%, n = 147) escaped the unsafe scenario and separately approximately half of EMS professionals (54%, n = 147) made an adequate attempt to de‐escalate the threatening encounter. Total 29% (n = 79) of participants made an adequate de‐escalation attempt and escaped the unsafe scenario during the simulation. Meanwhile, 20% (n = 55) did not adequately attempt to de‐escalate the aggressor nor escape the unsafe scene (Figure 1).
FIGURE 1.
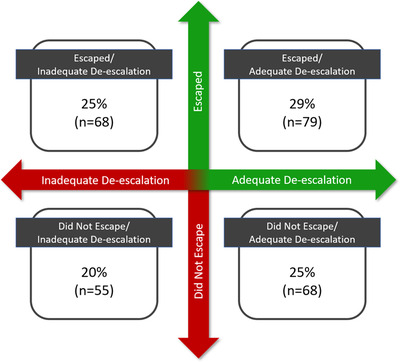
Participants classified by escaping the unsafe scene and attempted de‐escalation
For the primary outcome of escaping the unsafe scenario, there was a stepwise decrease in the proportion of EMS professionals who escaped as years of EMS experience increased (P‐trend = 0.02). One third (33%, n = 11) of those with previous military experience escaped compared to over half of those without military experience (57%, n = 130, P = 0.01). Similarly, a smaller proportion of those who had crisis intervention training did not escape compared to those without crisis intervention training (36% [n = 21] vs 60% [n = 119], P < 0.01). There was no difference in the proportion of EMS professionals who escaped by previous law enforcement experience (P = 0.36) (Table 1).
For the secondary outcome of de‐escalation, paramedics most frequently made an adequate de‐escalation attempt (59%, n = 118), followed by AEMTsiIntermediate (36%, n = 9) and EMTs (32%, n = 9) (P < 0.01). There was no difference in the proportion of male or female personnel who made an adequate de‐escalation attempt (P = 0.50). There was a stepwise increase in the proportion of EMS professionals who made an adequate de‐escalation attempt as years of EMS experience increased, though this trend was not statistically significant (P‐trend = 0.06). More of the EMS professionals who had crisis intervention training made an adequate attempt to de‐escalate the threatening situation compared to those without crisis intervention training (68% [n = 40] vs 50% [n = 96], P < 0.01). No statistical differences were observed for de‐escalation attempts by prior law enforcement experience (P = 0.67) (Table 2).
TABLE 2.
Comparison of proportion of EMS professionals who made an adequate de‐escalation attempt by personal characteristics
| Adequate De‐escalation (55%, n = 145) row % (n) | Inadequate De‐escalation (45%, n = 118) row % (n) | P value | |
|---|---|---|---|
| Certification level | <0.01 | ||
| EMT | 32% (9) | 68% (19) | |
| AEMT | 36% (9) | 64% (16) | |
| Paramedic | 59% (118) | 41% (81) | |
| Sex | 0.50 | ||
| Female | 51% (46) | 49% (44) | |
| Male | 55% (91) | 45% (73) | |
| Years of 911 EMS experience | 0.06 | ||
| 0 to 2 | 46% (32) | 54% (38) | |
| 2 to 10 | 53% (37) | 47% (33) | |
| 10 to 20 | 58% (39) | 42% (28) | |
| 20+ | 62% (29) | 38% (18) | |
| Military experience | 0.39 | ||
| Yes | 61% (19) | 39% (12) | |
| No | 53% (118) | 47% (104) | |
| Law enforcement experience | 0.67 | ||
| Yes | 58% (15) | 42% (11) | |
| No | 53% (121) | 47% (106) | |
| Previous CIT training | <0.01 | ||
| Yes | 68% (40) | 32% (19) | |
| No | 50% (96) | 50% (97) | |
| Scenario | 0.14 | ||
| A–possible overdose | 52% (49) | 48% (45) | |
| B–intoxicated person | 57% (25) | 43% (19) | |
| C–aggressive family member | 65% (43) | 35% (23) | |
| D–domestic violence | 45% (30) | 55% (36) | |
| Felt scenario was realistic | 0.30 | ||
| Yes | 56% (123) | 44% (96) | |
| No | 48% (22) | 52% (24) | |
| Felt threatened during scenario | 0.46 | ||
| Yes | 53% (90) | 47% (80) | |
| No | 58% (57) | 42% (42) |
Abbreviations: AEMT, advanced emergency medical technician; CIT, crisis intervention team, EMS, emergency medical services; EMT, emergency medical technician.
Paramedics demonstrated 60% lower odds of leaving the unsafe scene compared to EMTs (OR: 0.40; 95% CI: 0.17–0.94). Compared to EMTs, paramedics demonstrated over 3‐fold greater odds of making an adequate de‐escalation attempt (OR: 3.17, 95% CI: 1.38–7.31) Those with 20 or more years of EMS experience exhibited 68% lower odds of escaping compared to those with 2 or fewer years of experience (OR: 0.32; 95% CI: 0.13–0.79). There was no statically significant association between years of experience and odds of an adequate de‐escalation attempt. Crisis intervention training (OR: 0.38; 95% CI: 0.21–0.69) was also associated with reduced odds of escaping but increased odds of adequately attempting de‐escalation (OR: 2.19, 95% CI: 1.19–4.04). Those with military experience demonstrated reduced odds of escaping (OR: 0.37, 95% CI: 0.17–0.81). No association was observed between military experience and de‐escalation attempts (OR: 1.40, 95% CI: 0.66–2.94). There was no significant association between law enforcement experience and escaping the unsafe scenario (OR: 0.69, 95% CI: 0.30–1.55) or making an adequate de‐escalation attempt (OR: 1.23, 95% CI: 0.54–2.79) (Table 3).
TABLE 3.
Univariable odds ratios for escaping the unsafe scenario or making an adequate de‐escalation attempt by EMS professional characteristics
| Escape Univariable OR (95% CI) | Adequate de‐escalation attempt Univariable OR (95% CI) | |
|---|---|---|
| Certification level | ||
| EMT | Referent | Referent |
| AEMT | 0.61 (0.20–1.90) | 1.18 (0.38–3.63) |
| Paramedic | 0.40 (0.17–0.94) | 3.17 (1.38–7.31) |
| Sex | ||
| Female | Referent | Referent |
| Male | 0.60 (0.36–1.01) | 1.27 (0.76–2.10) |
| Years of 911 EMS experience | ||
| 0 to 2 | Referent | Referent |
| 2 to 5 | 0.75 (0.29–1.95) | 0.58 (0.23–1.48) |
| 5 to 10 | 0.75 (0.32–1.74) | 0.97 (0.43–2.19) |
| 10 to 20 | 0.71 (0.30–1.67) | 1.16 (0.51–2.64) |
| 20+ | 0.32 (0.13–0.79) | 1.40 (0.58–3.40) |
| Military experience | ||
| No | Referent | Referent |
| Yes | 0.37 (0.17–0.81) | 1.40 (0.66–2.94) |
| Law enforcement experience | ||
| No | Referent | Referent |
| Yes | 0.69 (0.30–1.55) | 1.23 (0.54–2.79) |
| Previous CIT training | ||
| No | Referent | Referent |
| Yes | 0.38 (0.21–0.69) | 2.19 (1.19–4.04) |
Abbreviations: AEMT, advanced emergency medical technician; CI, confidence interval; CIT, crisis intervention team, EMS, emergency medical services; EMT, emergency medical technician; OR, odds ratio.
4. LIMITATIONS
The use of high‐fidelity simulation with standardized patients and role players provides a unique opportunity to evaluate critical decision making and observe human behavior during challenging situations when direct observation of EMS professionals in real time is not feasible. Nevertheless, simulated encounters in a training environment do not perfectly imitate real‐life scenarios and important limitations are introduced. The time constraints imposed by the simulated scenario design are artificial and EMS professionals may exhibit different behaviors with longer observation times. Further, it is possible that EMS professionals were less likely to escape in a simulated scenario knowing that they were being videorecorded within a training environment with a safety officer to ensure physical safety. Thus, this work may overestimate the number of EMS professionals who would remain on scene in a similar threatening real‐world situation. Most study participants reported that they felt that the simulated scenario represented a real situation, and nearly two thirds reported that they would have felt threatened had the scenario occurred in real life. Nevertheless, although data were collected anonymously, response bias may be present as EMS professionals knew they were providing feedback to their training program staff.
Inherent in the rating system used for this investigation is a degree of subjectivity that should be considered. Owing to the novel nature of this pilot project, the Likert scale for de‐escalation was developed specifically for this situation, and, as such, it was not validated. Nevertheless, the EMS training team uses this type of scale for evaluating performance on a routine basis for other training purposes, and at minimum, this scale provides a subjective method to separate EMS professionals based on observation by training staff. All evaluators were previously trained simulation operators within the EMS system and were not members of the study design team. These evaluators went through a week‐long training session specifically related to this project with practice scenarios and debriefings related to scoring. Despite the training, evaluation of colleagues within their EMS system may have resulted in some bias and variability that could not be controlled. As only 1 evaluator assessed each crew member, there is a potential for variability in the reliability of ratings between reviewers that cannot be determined from this study. Further, in the categorization of de‐escalation attempts, the neutral category of 3 was included as adequate de‐escalation to err on the side of giving crew members credit for de‐escalation attempts. As such, the results of this analysis may overestimate the proportion adequate de‐escalation attempts. Future studies may attempt to further mitigate these limitations by validating a scoring system for these unique and dynamic encounters targeted for EMS professionals and EMS job roles.
The practical implications of training an entire EMS workforce using public safety partners also created some logistical limitations from a research consistency standpoint. For example, role players were rotated between training days because of other professional obligations including their shift work. Therefore, it was not possible to use the same role player for every iteration of every scenario over the weeks in which these sessions occurred. To limit this type of bias, all role players received the same week‐long training and practiced their roles before the project. There was also the possible effect of evaluator fatigue given the repetitive task of rating the same scenarios over multiple iterations. Additionally, although efforts were made to maintain the confidentiality of the scenarios during the training, it is possible that some EMS professionals discussed aspects of the training with colleagues who had not yet participated. Training duration was condensed to 14 days to reduce the disclosure risk as much as feasible.
Although we assessed a variety of EMS professional characteristics and experiences, there are possible additional variables associated with response to threatening encounters that were not assessed. For example, we did not collect data related to EMS professionals’ prior experiences with violence during patient care, and it is unclear how past experiences with violence on the job could have affected behaviors. Further, we did not assess prior training or experience specifically related to self‐defense or safe restraint techniques. Additionally, this study did not assess the effects of role player or participant characteristics (eg, gender, stature) on exhibited behaviors. EMS crew configurations in terms of characteristics, physical stature, gender concordance or discordance, and experience level of each EMS professional could affect how the crew operates with each other or behaves in threatening scenarios. Future research should explore these relationships as well as possible implicit biases.
The timing of this study should be considered as these simulations were conducted at the end of 2015. There have not been any major shifts in EMS education related to threat recognition and de‐escalation training on a large scale since the time these data were collected. This study was conducted at a single EMS agency necessitating further research to evaluate generalizability of these findings. The effects of local protocols, policies, and current industry focus on EMS professionals’ responses to threatening encounters warrant further investigation.
5. DISCUSSION
Using specially developed standardized simulation scenarios, we observed and described EMS professionals’ behaviors in situations involving escalating threats of violence. Half of EMS professionals removed themselves from the unsafe situations or made an adequate attempt to de‐escalate the threatening aggressor. Of concern, 1 in 5 EMS professionals failed to make an adequate de‐escalation attempt and did not leave the unsafe scene. Collectively, these findings highlight areas of opportunity for EMS education and training regarding how to effectively use de‐escalation techniques, how to recognize imminent violence when de‐escalation fails, and when to extricate oneself from a dangerous environment until the scene can be secured by appropriate personnel.
De‐escalation is an important first‐line intervention in a potentially threatening or aggressive situation. 13 , 14 , 15 Although natural skill at verbal de‐escalation exists on a continuum, there is evidence that verbal de‐escalation techniques can be learned and used effectively. 16 , 17 In the present study, a large proportion of EMS professionals did not adequately attempt to de‐escalate the aggressor, suggesting an opportunity for increased training and education related to verbal de‐escalation techniques. In a previous mixed‐methods study, EMS professionals who had been assaulted cited a lack of knowledge regarding how to prevent and manage aggressive behavior as a contributing factor to violence on the job. 18 Respondents also indicated that the communication style of the EMS professionals was a possible contributing factor in some violent attacks. 18 This study suggests that EMS professionals behavior may have worsened the threatening situation in some cases. Behaviors that plausibly escalated the threatening situation ranged from raised voices, outright yelling, and physically pushing or shoving the aggressor. Several EMS professionals attempted to re‐enter the scenario location after being pushed outside by the aggressor, an act that could potentially be considered trespassing in some real‐world settings. These observed behaviors further reinforce the need for formal, standardized de‐escalation training that is specific to the job functions of EMS professionals.
Our results did not confirm our hypothesis that greater EMS experience would predict escape from the violent situation. Greater years of experience, as well as paramedic‐level certification, and military background were associated with reduced odds of leaving the unsafe scene. Although these scenarios were designed to be non‐responsive to de‐escalation attempts, personnel with greater years of EMS experience may have witnessed more successful de‐escalations in their careers and may have felt more confident in their ability to verbally de‐escalate the situation. Further, personnel who worked in EMS longer have also likely had more EMS training experience overall simply due to career longevity. Previous training encounters are unlikely to have involved threatening or violent encounters and thus the progression of the present scenarios was likely unanticipated. More experienced EMS professionals and those with the higher level of certification (paramedic) often assume lead roles on calls. These EMS professionals may have felt a sense of duty or pressure to take control and protect their more junior counterparts. Previous research has shown that paramedics demonstrated nearly a 3‐fold increase in odds of physical violence compared to EMTs. 5 More years of experience was also associated with increased odds of experiencing violence on the job. 5 The tendency to remain on scene in a threatening environment observed in our study could represent a contributing factor to the greater odds of violence among paramedics and more experienced professionals.
The underlying factors for the association between military experience and lower likelihood of leaving the threatening scene are also likely multifactorial. EMS professionals with previous military experience possibly felt greater confidence managing hostile situations because of combat training and experience. The role of military personnel differs greatly from the role of EMS professionals. Military personnel are expected to remain in hostile situations rather than retreat to safety. Those with military backgrounds may have felt an increased sense of duty to protect others and not back down in a threatening situation. Future study is needed to explore how crew configuration characteristics (eg, mix of experience, prior training, gender, and age) affect behavior in threatening situations.
Also contrary to our hypothesis, previous CIT training was associated with decreased likelihood of leaving the unsafe scene. EMS professionals with CIT training demonstrated substantially lower odds of escaping the unsafe scenario and increased odds of verbal de‐escalation. Plausibly, those with CIT training overestimated their ability to verbally de‐escalate the situation and did not recognize the imminent threat of violence. The increased de‐escalation observed is in line with results from a study of law enforcement officers where this type of training was associated with a 2‐fold increase in odds of verbal engagement or negotiation being reported as the highest level of force used during encounters. 19 Of note, CIT training was designed specifically for law enforcement personnel who have different roles in managing violence compared to health care workers such as EMS personnel. Law enforcement personnel are expected to control violent situations whereas EMS personnel are expected to retreat to safety and allow law enforcement to control a violent situation. Future work is needed to create standardized training specifically for EMS professionals with de‐escalation techniques and recommended actions to take after recognition of imminent violence.
Barriers to EMS professionals removing themselves from threatening situations require further research. Ambiguity regarding ethical‐legal and agency policy considerations has been noted in prior work. In a national survey of EMS professionals, only one third reported that their EMS agency had written policies and procedures related to violence against EMS professionals. 9 A qualitative study of EMS professionals who had been assaulted highlighted perceptions that policies obligated EMS personnel to remain on scene even if they felt the scene could be dangerous. 18 The American College of Emergency Physicians’ policy statement on violence prevention and intervention in EMS systems recommended developing written operational protocols for violent situations in the EMS environment and adopting a zero‐tolerance policy for violence against EMS professionals. 20 EMS systems should ensure that personnel comprehend the legal framework (ie, case law and general statutes) that covers their agency. Furthermore, EMS systems should provide clear policies related to threatening encounters as guidance regarding when EMS personnel should leave a potentially unsafe scene.
Overall, this study provides support for the feasibility of using high‐fidelity simulation with standardized scenarios developed in collaboration with combative training subject‐matter experts to better understand EMS professionals’ responses to encounters with escalating threats of violence. Simulated scenarios provide a safe way to train and provide feedback to EMS personnel for encounters involving escalated threats of violence. In a simulation study among nurses, repetitive escalating and violent situations helped improve skills and feelings of preparation to deal with such scenarios. 21 Future work is needed to develop and evaluate the effectiveness of programs that effectively prepare EMS professionals to respond to threatening or violent situations.
In summary, this study, involving standardized simulated scenarios, revealed substantial variation in EMS professionals’ responses to situations involving escalating threats of violence, including some behaviors that may put them at greater risk of experiencing physical assault. EMS professionals with training designed for non‐health care roles, such as military or law enforcement, were less likely to remove themselves from the threatening situation. These findings suggest a need for specialized EMS training and education regarding de‐escalation as a first‐line technique, recognizing imminent violence, and leaving a dangerous environment.
CONFLICT OF INTEREST
The authors have no conflicts of interest to report.
AUTHOR CONTRIBUTIONS
Study conceptualization and design: Donald G. Garner, Mallory B. DeLuca, Jefferson G. Williams, and Jose G. Cabanas. Literature review: Donald G. Garner, Mallory B. DeLuca, and Remle P. Crowe. Data analysis: Remle P. Crowe. Interpretation of results: Donald G. Garner, Mallory B. DeLuca, Jefferson G. Williams, Jose G. Cabanas, Rebecca E. Cash, Madison K. Rivard, and Ashish R. Panchal. Manuscript development: Donald G. Garner, Mallory B. DeLuca, Remle P. Crowe, Rebecca E. Cash, Madison K. Rivard, Jefferson G. Williams, Ashish R. Panchal, and Jose G. Cabanas.
Supporting information
SUPPORTING INFORMATION
SUPPORTING INFORMATION
SUPPORTING INFORMATION
SUPPORTING INFORMATION
Biography
Donald G. Garner, Jr. is the Deputy Director/Chief of Professional Development for Wake County Emergency Medical Services (EMS) in Raleigh, North Carolina. He is responsible for all aspects of education and training for the EMS system.

Garner DG, DeLuca MB, Crowe RP, et al. Emergency medical services professional behaviors with violent encounters: A prospective study using standardized simulated scenarios. JACEP Open. 2022;3:e12727. 10.1002/emp2.12727
Funding and support: By JACEP Open policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
Supervising Editor: Juan March, MD.
Accepted for oral presentation at the 2018 Annual Meeting of the National Association of EMS Physicians. Awarded Best EMS Professional Research Presentation.
REFERENCES
- 1. Reichard AA, Marsh SM, Tonozzi TR, Konda S, Gormley MA. Occupational injuries and exposures among emergency medical services workers. Prehosp Emerg Care. 2017;21(4):420‐431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Weaver MD, Patterson PD, Fabio A, Moore CG, Freiberg MS, Songer TJ. The association between weekly work hours, crew familiarity, and occupational injury and illness in emergency medical services workers. Am J Ind Med. 2015;58(12):1270‐1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Maguire BJ, Browne M, O'Neill BJ, Dealy MT, Clare D, O'Meara P. International survey of violence against EMS personnel: physical violence report. Prehosp Disaster Med. 2018;33(5):526‐531. [DOI] [PubMed] [Google Scholar]
- 4. Maguire BJ, O'Meara P, O'Neill BJ, Brightwell R. Violence against emergency medical services personnel: a systematic review of the literature. Am J Ind Med. 2018;61(2):167‐180. [DOI] [PubMed] [Google Scholar]
- 5. Gormley MA, Crowe RP, Bentley MA, Levine R. A national description of violence toward emergency medical services personnel. Prehosp Emerg Care. 2016;20(4):439‐447. [DOI] [PubMed] [Google Scholar]
- 6. Murray RM, Davis AL, Shepler LJ, et al. A systematic review of workplace violence against emergency medical services responders. New Solut. 2020;29(4):487‐503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Taylor JA, Barnes B, Davis AL, Wright J, Widman S, LeVasseur M. Expecting the unexpected: a mixed methods study of violence to EMS responders in an urban fire department. Am J Ind Med. 2016;59(2):150‐163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bigham BL, Jensen JL, Tavares W, et al. Paramedic self‐reported exposure to violence in the emergency medical services (EMS) workplace: a mixed‐methods cross‐sectional survey. Prehosp Emerg Care. 2014;18(4):489‐494. [DOI] [PubMed] [Google Scholar]
- 9. National Association of Emergency Medical Technicians Violence Against EMS Practitioners: 2019 National Survey. https://www.naemt.org/docs/default-source/2017-publication-docs/naemt-violence-report-web-10-02-2019.pdf?Status=Temp&sfvrsn=b700d792_2. Published 2019. Accessed February 14, 2020.
- 10. American Academy of Orthopaedic Surgeons . Nancy Caroline's Emergency Care in the Streets . 8th ed. Jones & Bartlett Learning; 2018. [Google Scholar]
- 11. National Highway Traffic Safety Administration . National Emergency Medical Services Education Standards: Paramedic Instructional Guidelines. https://www.ems.gov/pdf/education/National‐EMS‐Education‐Standards‐and‐Instructional‐Guidelines/Paramedic_Instructional_Guidelines.pdf. Published 2009. Accessed January 3, 2020.
- 12. Watson AC, Fulambarker AJ. The crisis intervention team model of police response to mental health crises: a primer for mental health practitioners. Best Pract Ment Health. 2012;8(2):71‐71. [PMC free article] [PubMed] [Google Scholar]
- 13. Hallett N, Dickens GL. De‐escalation of aggressive behaviour in healthcare settings: concept analysis. Int J Nurs Stud. 2017;75:10‐20. [DOI] [PubMed] [Google Scholar]
- 14. Beck JC, White KA, Gage B. Emergency psychiatric assessment of violence. Am J Psychiatry. 1991;148(11):1562‐1565. [DOI] [PubMed] [Google Scholar]
- 15. Blair EW, Woolley S, Szarek BL, et al. Reduction of seclusion and restraint in an inpatient psychiatric setting: a pilot study. Psychiatr Q. 2017;88(1):1‐7. [DOI] [PubMed] [Google Scholar]
- 16. Richmond JS, Berlin JS, Fishkind AB, et al. Verbal de‐escalation of the agitated patient: consensus statement of the American Association for Emergency Psychiatry Project BETA de‐escalation workgroup. West J Emerg Med. 2012;13(1):17‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kaufman G, McCaughan D. The effect of organisational culture on patient safety. Nurs Stand. 2013;27(43):50‐56. [DOI] [PubMed] [Google Scholar]
- 18. Maguire BJ, O'Neill BJ, O'Meara P, Browne M, Dealy MT. Preventing EMS workplace violence: a mixed‐methods analysis of insights from assaulted medics. Injury. 2018;49(7):1258‐1265. [DOI] [PubMed] [Google Scholar]
- 19. Compton MT, Bakeman R, Broussard B, et al. The police‐based crisis intervention team (CIT) model: II. Effects on level of force and resolution, referral, and arrest. Psychiatr Serv. 2014;65(4):523‐529. [DOI] [PubMed] [Google Scholar]
- 20. American College of Emergency Physicians . Violence prevention and intervention in emergency medical services systems. Ann Emerg Med. 2019;74(3):e29‐e30. [DOI] [PubMed] [Google Scholar]
- 21. Brown RG, Anderson S, Brunt B, Enos T, Blough K, Kropp D. Workplace violence training using simulation. Am J Nurs. 2018;118(10):56‐68. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
SUPPORTING INFORMATION
SUPPORTING INFORMATION
SUPPORTING INFORMATION
SUPPORTING INFORMATION


