Abstract
Sub-macular hemorrhage poses a potential threat to vision if left untreated. The preferred surgical technique to clear sub-macular hemorrhage includes vitrectomy followed by retinotomy using a 41G needle with subsequent injection of recombinant tissue plasminogen activator (r-tPA) followed by air/SF6 injection into the sub-retinal space. A malleable nature, increased resistance, and the cost of the 41G needle limit its use. We evaluated the safety and efficacy of a 26G needle for retinotomy as a supplement for the 41G needle in a series of six subjects with sub-macular hemorrhage. A slight modification in the procedure was done by injecting air into the sub-retinal space prior to the r-tPA injection. We found that our technique of using the 26G needle for retinotomy is safe and effective due to its stable nature and self-sealing properties. An air injection prior to r-tPA allows for increased bioavailability of the drug by preventing efflux due to its tamponading effect.
Keywords: 26G needle, recombinant tissue plasminogen activator (r-tPA), retinotomy, sub-macular hemorrhage
Sub-macular hemorrhage poses a threat to vision due to the toxic effects of accumulated blood between the photoreceptors and retinal pigment epithelial cells (RPE).[1,2] The available treatment options include conservative management such as observation alone,[3] minimal invasive procedures such as Anti- Vascular endothelial growth factor (anti-VEGF) monotherapy,[4] pneumatic displacement alone[2] or their combination.[5,6] The active intervention includes pars plana vitrectomy with sub-retinal r-tPA and anti-VEGF injection with pneumatic displacement.[7,8] The latter being the preferred technique involving retinotomy using the 41G needle. The malleable tip of the 41G needle with unsteadiness while passing through the 23G port (please refer to Clip 1 for our experience with the 41G needle causing inadvertent retinotomy extensions due to loose fit through the 23G pars plana cannula) and resistance for drug injection into the sub-retinal space are some drawbacks. In our case series, we describe retinotomy using the 26G needle instead of the 41G with unique advantages.
Surgical Technique
We describe our technique in six patients with sub-retinal hemorrhage of various etiologies. We performed chandelier-assisted four ports pars plana vitrectomy through the 23G system which included complete vitrectomy with Internal limiting membrane (ILM) peeling. After visualizing the sub-macular hemorrhage, retinotomy was performed using the readily available and cost-effective 1.5 in 26G needle. The injection of the air bubble was done through the retinotomy site into the sub-retinal space, followed by an injection of sub-retinal recombinant tissue plasminogen activator (r-tPA) 25 mg with the 26G needle in situ following which intravitreal anti-VEGF injection was done. An air bubble due to its buoyancy forces provides a uniform plane underneath it for the spread of r-tPA. Also, by tamponading the retinotomy site, the air prevents the efflux of the injected drug back into the vitreous cavity, and thus, increases its bioavailability in the sub-retinal space. Retinotomy with the 26G needle was self-sealing, hence, it did not require to be lasered.
For representation, we hereby showcase a 67-year-old male patient (case 1) with massive persistent sub-macular hemorrhage secondary to polypoidal choroidal vasculopathy (PCV) status post-multiple anti-VEGF injections. His best-corrected visual acuity (BCVA) was finger counting close to face [Fig. 1a and b]. The pneumatic displacement of the hemorrhage was done using the above technique with air gas injected into the sub-retinal space along with r-tPA, 1.25 mg/0.01 mL of bevacizumab was injected intravitreally. One month post-operative picture shows the heme to be displaced off the macula with the restoration of near-normal foveal contour with the BCVA improved up to 6/60 on the Snellen acuity chart [Clip 2 and Fig. 2a, b].
Figure 1.
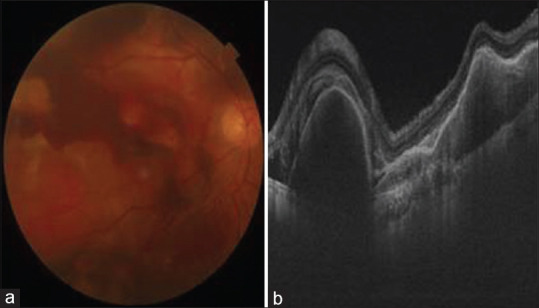
(a) Pre-operative color fundus photograph of case 1 showing the presence of sub-macular hemorrhage. (b) OCT image of Figure 1a showing sub-macular hemorrhage
Figure 2.
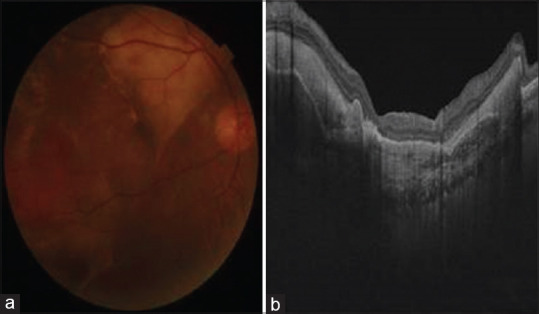
(a) Post-operative color fundus photo of case 1 showing the resolution of hemorrhage. (b) OCT image of Figure 2a showing displacement of heme from the foveal center
The second case was a 62-year-old female with breakthrough vitreous hemorrhage and sub-macular hemorrhage secondary to the neovascular age-related macular degeneration (n-AMD) with a BCVA of 6/60. A similar procedure to displace the heme was undertaken. A 1-month post-operative picture shows an inferiorly displaced heme with relative flattening of the foveal contour with improvement in the BCVA up to 6/24 on the Snellen visual acuity chart [Clip 3 and Fig. 3].
Figure 3.
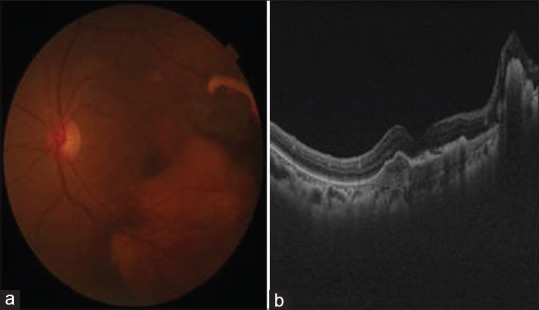
(a) Post-operative color fundus photo of case 2 showing inferiorly displaced heme. (b) OCT image of Figure 3a showing displaced heme
Furthermore, four more patients were evaluated using the same technique with a similar outcome, and none of the subjects required any lasering of the retinotomy site. None of them required a second procedure. The details of all the patients are enumerated in Table 1.
Table 1.
The details of the subjects who underwent the procedure with the comparison of the outcomes
| Case number | Cause of sub-macular hemorrhage | Pre-operative BCVA | Post-operative BCVA (at 1 month) |
|---|---|---|---|
| 1 | Polypoidal choroidal vasculopathy | CFCF | 6/60 |
| 2 | Neovascular AMD - type 2 MNV | 6/60 | 6/24 |
| 3 | Polypoidal choroidal vasculopathy | 1/60 | 6/60 |
| 4 | PEHCR | 6/60 | 6/18 |
| 5 | PEHCR | 1/60 | 6/60 |
| 6 | Neovascular AMD-MNV? type 2 | 4/60 | 6/24 |
BCVA - Best-corrected visual acuity; AMD - Age-related macular degeneration; CFCF - counting fingers close to face; MNV - macular neovascularization; PEHCR - peripheral exudative hemorrhagic chorioretinopathy
Conclusion
Using a 26G 1.5 in needle for retinotomy to inject r-tPA in the sub-retinal space is relatively easy due to its stable nature while passing through the 23G vitrectomy port, preventing inadvertent intraocular movements of the needle tip. Retinotomy is of the intended size and self-sealing; also, the 26G needle being cheaper and readily available is of great advantage in developing countries and can be used as a cheaper alternative to the 41G needle. The injection of the air bubble before the r-tPA injection provides increased bioavailability of the drug in the sub-retinal space by preventing the efflux into the vitreous cavity.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Video Available on: www.ijo.in
References
- 1.Fang IM, Lin YC, Yang CH, Yang CM, Chen MS. Effects of intravitreal gas with or without tissue plasminogen activator on sub-macular hemorrhage in age-related macular degeneration. Eye (Lond) 2009;23:397–406. doi: 10.1038/sj.eye.6703017. [DOI] [PubMed] [Google Scholar]
- 2.Casini G, Loiudice P, Menchini M, Sartini F, De Cillà S, Figus M, et al. Traumatic sub-macular hemorrhage:Available treatment options and synthesis of the literature. Int J Retina Vitreous. 2019;5:48. doi: 10.1186/s40942-019-0200-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Scupola A, Cosca G, Soubrane G, Balestrazzi E. Natural history of macular sub-retinal hemorrhage in age-related macular degeneration. Ophthalmologica. 1999;213:97–102. doi: 10.1159/000027400. [DOI] [PubMed] [Google Scholar]
- 4.Abdul-Salim I, Embong Z, Khairy-Shamel ST, Raja-Azmi MN. Intravitreal ranibizumab in treating extensive traumatic sub-macular hemorrhage. Clin Ophthalmol. 2013;7:703–6. doi: 10.2147/OPTH.S42208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de Silva SR, Bindra MS. Early treatment of acute sub-macular hemorrhage secondary to wet AMD using intravitreal tissue plasminogen activator, C3F8, and an anti-VEGF agent. Eye (Lond) 2016;30:952–7. doi: 10.1038/eye.2016.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grohmann C, Dimopoulos S, Bartz-Schmidt KU, Schindler P, Katz T, Spitzer MS, et al. Surgical management of sub-macular hemorrhage due to n-AMD:A comparison of three surgical methods. Int J Retina Vitreous. 2020;6:27. doi: 10.1186/s40942-020-00228-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kamei M, Misono K, Lewis H. A study of the ability of tissue plasminogen activator to diffuse into the sub-retinal space after intravitreal injection in rabbits. Am J Ophthalmol. 1999;128:739–46. doi: 10.1016/s0002-9394(99)00239-1. [DOI] [PubMed] [Google Scholar]
- 8.Singh RP, Patel C, Sears JE. Management of sub-retinal macular hemorrhage by direct administration of tissue plasminogen activator. Br J Ophthalmol. 2006;90:429–31. doi: 10.1136/bjo.2005.085001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


