Abstract
Purpose:
In the ophthalmology setting, given the close proximity required for the clinical exam, appropriate mask usage and fit is essential. This study aims to assess how a simple, cost-effective 3D-printed face mask ear protectors (EP) attachment may decrease discomfort, increase compliance, and improve fit in an academic institution’s Ophthalmology department.
Methods:
Face mask EPs were distributed to patients and providers in the Ophthalmology department. A validated questionnaire was administered before and 2 weeks after EP usage. The survey included questions on demographics and frequency of mask usage during a spectrum of activities. Descriptive statistics were performed with Fischer’s t test.
Results:
Post-EP responses demonstrated an increased likelihood of mask usage across all activities, although not statistically significant. The greatest change was during outdoor activities, with a 14.3% increase in highest utilization. Post-EP, all subjects were very likely to wear masks while shopping and 91.7% while in the workplace. EP usage decreased the number of noncompliant individuals while spending time with friends and family by 93.3%. Almost no subjects reported mask removal of >15 times per hour post-EP. The increase in mask compliance was greatest for low mask utilizers. 91.9% reported improved comfort, 91.9% reported improved fit, and 81.6% reported increased mask usage.
Conclusion:
Our results suggest that simple cost-effective 3D-printed ear protectors may improve fit, comfort, and overall mask compliance. The results of this study should drive broader public health efforts to further investigate whether mask attachments can improve overall mask compliance through better comfort and fit.
Keywords: 3D printing in ophthalmology, face mask ear protectors, infectious disease, mask compliance, mask fit, public health
In response to the COVID-19 epidemic, mask-wearing with cloth face coverings and surgical masks have become a social and in many cases a legal mandate across the US to dampen the spread of the virus. A Nature Medicine study found that if 95% of Americans correctly wore masks, the lives of more than 40,000 individuals could be saved.[1] Furthermore, widespread utilization of face masks combined with social distancing has been shown to increase the odds of controlling SARS-CoV-2 transmission.[2] As the pandemic continues, a growing share of Americans have begun to regularly wear a mask in stores and other businesses. Other studies have suggested that supplemental public health interventions, such as government mask mandates, may help increase mask adoption.[2] However, while 85% of Americans claim to wear a mask, a much lower percentage wear masks “regularly” or all the time when outside or in areas of potential transmission.[2] Furthermore, even if individuals are wearing masks, many struggle to wear the mask correctly, with both the nose and mouth covered, due to poor fit and discomfort.[3] A majority of individuals who endorse not wearing face masks when leaving their home cite discomfort as the main reason.[4] Discomfort has been specifically attributed to mask straps.[3] As cloth masks and face coverings become standard across the US, companies have made a variety of masks with varying goals of comfort and fit. However, there is little empirical evidence demonstrating the efficacy of such designs on mask compliance. Face masks have been associated with significant discomfort for healthcare workers.[4] Face mask ear protectors (EP) may reduce this discomfort by allowing earloop masks to be worn without tension and irritation.[5] These small extenders are easy to use and may improve subjective fit and comfort. Beyond the healthcare community, few individuals are aware of these options, and even within the healthcare community, there is a lack of data to suggest how these might impact mask usage. Even in subspecialties such as ophthalmology, which requires proximity contact to patients given the nature of the physical exam, mask extender use is limited. In a study by Breazzano et al.[6] among New York City physician residents, Ophthalmology residents were among the top three specialties with the highest proportion of confirmed COVID-19 disease burden. This study aims to assess how a simple, cost-effective, 3D-printed mask attachment may decrease mask discomfort and increase mask compliance in an academic institution’s ophthalmology department.
Methods
Materials
3D-printed face mask ear protectors were printed in-house, modeled after the available design 3DPX-013574 from the NIH 3D Print Exchange [Fig. 1a and b]. The ear protectors were 15.5-cm long, 2.5-cm wide, and 3-mm thick.
Figure 1.
(a) 3D-printed face mask ear protector (EP) distributed to survey participant (b) 3D-printed face mask ear protector (EP) worn by model
Data extraction
3D-printed face mask ear protectors were distributed to members of the Ophthalmology department in September 2020–January 2021 (during enforced universal masking policy and before the availability of vaccines). Before usage, individuals were asked to complete a brief validated questionnaire asking a series of questions on daily outings, underlying conditions, occupational exposure, and frequency and characteristics of mask usage.[7] Masks were distributed to physicians, administrative staff, technicians, and patients via the University City clinic in Philadelphia. Upon receiving the EP, users were shown a live tutorial by a resident physician on how to loop the ear loops over the hooks on the EP and how to take them off. Users then demonstrated understanding by placing their EP themselves and ensure proper fit. Participants were instructed to use mask extenders all the time (even outside of the workplace) and could be utilized with both surgical masks and cloth masks. Two weeks after the distribution of ear protectors, participants were asked to complete a follow-up survey modeled after previously validated mask comfort and compliance surveys,[7] including questions specific to the frequency of mask usage and the subjective perception of comfort, fit, and overall effect of mask extenders. The study was IRB exempt as a quality improvement project to improve mask compliance in the department.
Data analysis
Descriptive analyses were performed to characterize survey responses. Fishers Exact paired t test was used to perform statistical comparisons across groups to determine whether the ear protector had a significant effect on the frequency or characteristics of mask usage.
Results
In total, 48 participants completed pre- and post-surveys after wearing the face mask extender for 2 weeks. The average age of the population was 40.4 years old (SD = 12.2) with 31.3% female, 25% Caucasian, 22.9% African-American, and 43.8% Asian participants. Nine (16.8%) participants endorsed underlying conditions, including 14.6% with diabetes and 4.2% with asthma [Table 1].
Table 1.
Demographics
| Mean (n) | STH % | |
|---|---|---|
| Age (yrs) | 40.4 | 12.2 |
| Gender | ||
| Female | 15.0 | 31.3 |
| Male | 33.0 | 68.8 |
| Ethnicity | ||
| Asian | 21.0 | 43.8 |
| African-American | 11.0 | 22.9 |
| Caucasian | 12.0 | 25.0 |
| Hispanic | 2.0 | 4.2 |
| Education History | ||
| Post Graduate Degree | 17.0 | 35.4 |
| Associates Degree | 1.0 | 2.1 |
| College Graduate | 16.0 | 33.3 |
| Some College | 7.0 | 14.6 |
| High school or GED | 7.0 | 14.6 |
| Underlying Conditions | ||
| Diabetes | 7.0 | 14.6 |
| Asthma | 2.0 | 4.2 |
| Chronic Lung Disease | 0.0 | 0.0 |
| Chronic Heart Disease | 0.0 | 0.0 |
| Chronic Kidney Disease | 0.0 | 0.0 |
| Cancer in the Past year | 0.0 | 0.0 |
| Immunosuppressive Condition | 0.0 | 0.0 |
| None of the Above | 39.0 | 81.3 |
| Reasons Individuals choose not to wear a mask | ||
| Discomfort | 36 | 75.00 |
| Lack of Fit | 18 | 37.50 |
| Foggy Glasses | 1 | 2.08 |
| Do not want to | 3 | 6.25 |
| Difficulty breathing or hurts ears | 1 | 2.08 |
| Harder to Breathe when exercising | 1 | 2.08 |
When asked for reasons for not wearing masks, 75% of individuals listed discomfort as the main contributor, with 37.5% listing lack of fit [Table 1]. With respect to pre-mask extender mask usage, 72.9% of participants endorsed being “very likely” to wear masks while exercising or walking outside, with only 16.7% saying they were “not so likely” or “not likely at all” to wear masks. Furthermore, 95.8% of participants endorsed being “very likely” to wear masks while grocery shopping [Table 2]. Mask usage while visiting friends was more varied, with 52.1% of participants “very likely” to wear a mask, 31.5% “somewhat likely,” 4.2% “not so likely” and 12.5% “not likely at all.” Furthermore, 85.4% of participants endorsed masked usage while working at an office or workplace, with only 14.6% being “somewhat likely” or “not so likely” to wear masks [Table 2].
Table 2.
Effect of ear protector on likelihood of mask usage
| Pre | Post | % Usage Change | P | |||
|---|---|---|---|---|---|---|
|
|
|
|||||
| n | % | n | % | |||
| Exercise, Walking outside | ||||||
| Very Likely | 35.0 | 72.9 | 40.0 | 83.3 | 14.3 | 0.75 |
| Somewhat Likely | 5.0 | 10.4 | 7.0 | 14.6 | 40.0 | |
| Not so Likely | 6.0 | 12.5 | 1.0 | 2.1 | −83.3 | |
| Not Likely at all | 2.0 | 4.2 | 0.0 | 0.0 | −100.0 | |
| Grocery Shopping | ||||||
| Very Likely | 46.0 | 95.8 | 48.0 | 100.0 | 4.3 | 0.93 |
| Somewhat Likely | 2.0 | 4.2 | 0.0 | 0.0 | −100.0 | |
| Not so Likely | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | |
| Not Likely at all | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | |
| Visiting Friends | ||||||
| Very Likely | 25.0 | 52.1 | 25.0 | 52.1 | 0.0 | 0.95 |
| Somewhat Likely | 15.0 | 31.3 | 16.0 | 33.3 | 6.7 | |
| Not so Likely | 2.0 | 4.2 | 6.0 | 12.5 | 200.0 | |
| Not Likely at all | 6.0 | 12.5 | 1.0 | 2.1 | −83.3 | |
| Workplace | ||||||
| Very Likely | 41.0 | 85.4 | 44.0 | 91.7 | 7.3 | 0.89 |
| Somewhat Likely | 5.0 | 10.4 | 3.0 | 6.3 | −40.0 | |
| Not so Likely | 2.0 | 4.2 | 1.0 | 2.1 | −50.0 | |
| Not Likely at all | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | |
Although changes in mask usage were not statistically significant, post mask extender responses demonstrated increases in mask usage across all activities. After mask extender use, 83.3% of participants were very likely to wear a mask during exercise or walks, 100% of participants were very likely to wear a mask during grocery shopping, and 91.7% were very likely to wear a mask while working at an office or workspace [Table 2]. After mask extender usage, there was a decrease in the percentage of participants who had previously said they were “not likely at all” to wear a mask while visiting friends; however, there was no increase in participants “very likely” to wear masks while visiting friends [Table 2].
Frequency of mask removal during a variety of activities was also explored. Before the intervention, a majority of individuals (79.2%) endorsed removing their masks 0–5 times per hour (times/h), with 12.5% endorsing not wearing a mask at all or removing it >20 times/h while exercising or walking outside. The vast majority of participants (97.9%) endorsed removing masks only 0–5 times/h during grocery shopping [Table 3]. A smaller majority compared to the other activities (81.3%) reported removing masks 0–5 times/h while working at an office or workplace. In contrast, only 62.5% reported removing masks 0–5 times/h while visiting friends, with 16.7% reporting mask removal of greater than 20 times/h or not wearing a mask at all [Table 3].
Table 3.
Effect of mask extender on frequency of mask removal
| Pre | Post | % Usage Change | P | |||
|---|---|---|---|---|---|---|
|
|
|
|||||
| n | % | n | % | |||
| Exercise, Walking outside (removal/h) | ||||||
| 0-5 | 38.0 | 79.2 | 41.0 | 85.4 | 7.9 | 0.85 |
| 6-10 | 2.0 | 4.2 | 5.0 | 10.4 | 150.0 | |
| 10-15 | 1.0 | 2.1 | 1.0 | 2.1 | 0.0 | |
| 15-20 | 1.0 | 2.1 | 1.0 | 2.1 | 0.0 | |
| >20 or Noncompliant | 6.0 | 12.5 | 0.0 | 0.0 | −100.0 | |
| Grocery Shopping (removal/h) | ||||||
| 0-5 | 47.0 | 97.9 | 48.0 | 100.0 | 2.1 | 0.96 |
| 6-10 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | |
| 10-15 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | |
| 15-20 | 1.0 | 2.1 | 0.0 | 0.0 | −100.0 | |
| >20 or Noncompliant | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | |
| Visiting Friends (removal/h) | ||||||
| 0-5 | 30.0 | 62.5 | 30.0 | 62.5 | 0.0 | 0.98 |
| 6-10 | 9.0 | 18.8 | 12.0 | 25.0 | 33.3 | |
| 10-15 | 0.0 | 0.0 | 4.0 | 8.3 | 400.0 | |
| 15-20 | 1.0 | 2.1 | 0.0 | 0.0 | −100.0 | |
| >20 or Noncompliant | 8.0 | 16.7 | 2.0 | 4.2 | −75.0 | |
| Workplace (removal/h) | ||||||
| 0-5 | 39.0 | 81.3 | 41.0 | 85.4 | 5.1 | 0.89 |
| 6-10 | 6.0 | 12.5 | 7.0 | 14.6 | 16.7 | |
| 10-15 | 2.0 | 4.2 | 0.0 | 0.0 | −100.0 | |
| 15-20 | 1.0 | 2.1 | 0.0 | 0.0 | −100.0 | |
| >20 or Noncompliant | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | |
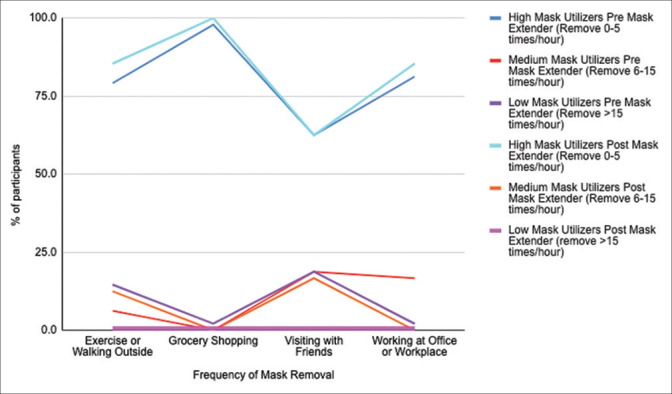
Although the effects were not statistically significant, the mask extender decreased the frequency of mask removal in all categories with almost no participants reporting mask removal of >15 times/h after using the mask extender. The effects of the mask extender while visiting friends showed a 100% reduction in participants reporting removing 15–20 times/h and 75% reduction for more than 20 times/h or complete mask noncompliance [Table 3 and Fig. 1]. The effect of the mask extender was greatest for low mask utilizers. In this low mask utilization cohort, there were no individuals reporting mask removal frequency of >15 times/h during any activity, and the greatest effects of increased usage occurred in activities including visiting friends or exercising or walking outside [Fig. 1].
Lastly, the subjective experience of the mask extender was queried among study participants: 91.9% of participants reported improved comfort, 91.9% reported improved fit, and 81.6% reported increased mask usage with the use of the mask extender [Table 4].
Table 4.
Subjective experience of mask extender use
| n | % | |
|---|---|---|
| Improved Comfort | ||
| Strongly Agree | 43.0 | 87.8 |
| Agree | 2.0 | 4.1 |
| Neither Agree nor Disagree | 3.0 | 6.1 |
| Disagree | 0.0 | 0.0 |
| Strongly Disagree | 0.0 | 0.0 |
| Improved Fit | ||
| Strongly Agree | 36.0 | 73.5 |
| Agree | 9.0 | 18.4 |
| Neither Agree nor Disagree | 2.0 | 4.1 |
| Disagree | 1.0 | 2.0 |
| Strongly Disagree | 0.0 | 0.0 |
| Increased Mask Usage | ||
| Strongly Agree | 37.0 | 75.5 |
| Agree | 3.0 | 6.1 |
| Neither Agree nor Disagree | 7.0 | 14.3 |
| Disagree | 1.0 | 2.0 |
| Strongly Disagree | 0.0 | 0.0 |
Of note, none of the participants reported mask strap breakage while engaging the ear protector with the mask strap. Additionally, every participant noted that the discomfort was related to the pressure on the ears and resultant headaches. Each participant used an elastic face mask that had loops around their ears. Surgical face masks that had ties were reserved only for surgical cases and their discomfort was not evaluated. N95 masks were reserved for the ICU and were not assessed.
Discussion
Medical face masks have been demonstrated to prevent transmission of COVID-19 in community and hospital settings.[8,9] However, while 85% of Americans claim to wear a mask,[10] a much lower percentage wear masks “regularly” or all the time when outside or in areas of potential transmission. This study aimed to investigate the perception of mask compliance, reasons for mask noncompliance, and the effect of a simple, cost-effective, 3D-printed mask attachment (EP) to decrease mask discomfort in the goals of increasing mask compliance in healthcare workers and patients in ophthalmology. Although the use of 3D-printed mask extenders have been reported in the literature,[5] to our knowledge, this is the first study that both implements 3D mask extenders and assesses the effect of extenders on mask usage and comfort in follow-up on a population with a relatively high risk of exposure.
The participants represented a diverse demographic, though they were also relatively healthy, with only 19.7% endorsing underlying chronic diseases, making them more susceptible to COVID-19 complications and thus more mask compliant. The majority of individuals reported discomfort and lack of fit to be the main reasons for choosing not to wear a mask, further supporting the need for simple measures such as the mask extender to ameliorate discomfort and fit to improve compliance. This discomfort was likely related to the ear loops on the ears given the resolution as the EP offset the pressure and most reported resolution of discomfort.
Overall, participants in this study tended to be high mask utilizers, influencing the pre-intervention responses to conform to a skewed relatively high compliance of mask usage during activities. However, while the majority of participants stated they were “very likely” to wear masks while exercising, grocery shopping, visiting friends, and working, the numerical frequency of mask removal was more revealing. This is exemplified by the fact that while 85.4% of participants reported being likely to wear masks while visiting friends, 37.5% reported the frequency of mask removal to be >6 times/h, with 16.7% reporting wearing no mask at all. This suggests there was much room for improvement in mask compliance in situations of high transmission even among the healthcare worker population with presumably higher health literacy and compliance.
Although changes in mask usage after the introduction of mask extenders were not statistically significant, post-intervention responses demonstrated increases in the likelihood of mask usage across all activities with the greatest effects during exercise or walking outside. Mask extender usage also resulted in 100% of participants reporting being very likely to wear masks while grocery shopping and 91.7% (7.3% increase) while working at an office or workplace. Similarly, the mask extender decreased the frequency of mask removal in all categories, with almost no participants reporting mask removal of >15 times/h after using the mask extender. The effect of the mask extender was greatest for low mask utilizers, resulting in no individuals reporting mask removal frequency of >15 times/h during any activity and the greatest effects of increased usage while visiting friends (100% decrease in the frequency of mask removal >15 times/h) or exercising or walking outside in this relatively lower mask utilizer cohort. Overall, post-intervention, there were no noncompliant participants. Subjective experience of the mask extender was also promising. The vast majority reported improved comfort, improved fit, and increased mask usage, demonstrating that this simple extender may have real effects on improving mask compliance.
It is also important to further discuss the importance of facilitating appropriate mask usage and comfort in ophthalmology specifically. Among specialties, ophthalmology was one of the top three specialties with the highest proportion of confirmed COVID-19 disease burden,[6] likely explained by the often close exams. For example, during the slit-lamp exam, the distance between the ophthalmologist’s and patient’s face is often less than 1 foot. Beyond the proximity of the patient, certain ophthalmic diseases, including conjunctivitis, are known to be complications of the coronavirus and may serve as additional pathogenic routes for transmission.[11] Therefore, proper mask usage and comfort are important to prevent transmission in an ophthalmic exam that requires a very close working distance and contact with infectious secretions as in conjunctivitis. It is also important to note that the implications of 3D printing for ophthalmologists are far broader than just the creation of these ear protectors. Alongside these ear protectors, 3D printing has multiple other uses within ophthalmology.[12] For example, 3D printing has been used to create mounts for lenses that connect to imaging devices such as smartphones to allow for mobile fundus photography. Furthermore, it has been useful in surgical planning of orbital cases and is often used in fracture repairs.
While these results have implications for improvement of both compliance and the benefit of simple cost-effective mask attachments, this study is limited by several factors. First, this study represents a small subset of primarily healthcare workers with relatively high mask utilization prior to the introduction of the mask extenders. Therefore, this study may not be able to truly appreciate the effect of mask extenders on compliance in the general population, as suggested by the greater effects on low mask utilizers [Fig. 2]. In addition, it may be difficult to engage the mask in the ear protector and remove it, which may prove challenging for the average layperson and older age individual to use. Similarly, subjective measures of mask compliance derived from survey studies are inherently limited due to self-reporting bias and the inability to assess whether individuals are wearing masks correctly and/or whether the mask extender significantly improves the probability of “correct” mask usage. Third, this study is limited in its ability to draw prescriptive conclusions by the lack of a control group. Given the status of the COVID-19 crisis at the time, the authors wanted to supply the mask extender to as many individuals as possible and therefore did not have a control group without access to the mask extenders. In addition, subjects enrolled in the study may have been more likely to be compliant (or report compliance) as they knew they would be measured over the 2 week period. Therefore, it is difficult to quantitatively compare differences in compliance with extender usage.
Figure 2.
Mask utilization pre and post mask extender
Overall, this study demonstrates that there is room for improvement in mask compliance, driven by the need for better fit and comfort, even in a high compliance ophthalmology department at an academic institution. While mask extenders have been employed in certain healthcare worker populations, access to and use of them has been limited. Even among ophthalmologists, where the clinical exam necessitates close proximity to patients, almost no subjects had used an EPs before. Beyond the proximity of the patient, certain ophthalmic diseases, including conjunctivitis, are known to be complications of the coronavirus and may serve as additional pathogenic routes for transmission.[11] Along with proper face mask usage, comprehensive protection with eye shields has been shown to have a relative decrease in infection risk by 10.6%.[13] In addition, although not assessed in this study, the pediatric population may benefit greatly from these as their cranial circumference is much less than an adult and most of the widely available face masks are designed for adults. Further studies may assess its utility in children.
Conclusion
This study demonstrates that these simple cost effective extenders may improve fit, comfort, and overall mask compliance among healthcare workers, with potential implications for the population at large. We hope that this study will drive broad public health efforts to further investigate the effect and availability of these mask attachments to potentially improve mask compliance in the population through better fit and comfort.
Financial support and sponsorship
CARES grant to support the production of 3D-printed ear protectors.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We appreciate the help of the Biomedical Library 3D Printing Lab at the University of Pennsylvania for their assistance in the production of 3D-printed ear protectors.
References
- 1.IHME COVID-19 Forecasting Team. Reiner RC, Jr, Barber RM, Collins JK, Zheng P, Adolph C, et al. Modeling COVID-19 scenarios for the United States. Nat Med. 2021;27:94–105. doi: 10.1038/s41591-020-1132-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rader, Benjamin, White LF, Burns MR, Chen J, Brilliant J, et al. Mask wearing and control of SARS-CoV-2 transmission in the United States. medRxiv. 2020 [Google Scholar]
- 3.Zuo Y, Hua W, Luo Y, Li L. Skin reactions of N95 masks and medial masks among health-care personnel:A self-report questionnaire survey in China. Contact Dermatitis. 2020;83:145–7. doi: 10.1111/cod.13555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shenal BV, Radonovich LJ, Cheng J, Hodgson M, Bender BS. Discomfort and exertion associated with prolonged wear of respiratory protection in a health care setting. J Occup Environ Hyg. 2012;9:59–64. doi: 10.1080/15459624.2012.635133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O'Connor Z, Huellewig D, Sithiyopasakul P, Morris JA, Gan C, Ballard DH. 3D printed mask extenders as a supplement to isolation masks to relieve posterior auricular discomfort:An innovative 3D printing response to the COVID-19 pandemic. 3D Print Med. 2020;6:27. doi: 10.1186/s41205-020-00080-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Breazzano Mark P, Shen J, Abdelhakim AH, Glass LR, Horowitz JD, et al. New York City COVID-19 resident physician exposure during exponential phase of pandemic. The Journal of clinical investigation. 2020;9:130. doi: 10.1172/JCI139587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rader B, White LF, Burns MR, Chen J, Brilliant J, Cohen J, et al. Mask-wearing and control of SARS-CoV-2 transmission in the USA:A cross-sectional study. Lancet Digit Health. 2021;3:e148–57. doi: 10.1016/S2589-7500(20)30293-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chaabna K, Doraiswamy S, Mamtani R, Cheema S. Since January 2020 Elsevier has created a COVID-19 resource centre with free information in English and Mandarin on the novel coronavirus COVID- 19. The COVID-19 resource centre is hosted on Elsevier Connect, the company's public news and information. 2020 (January) [Google Scholar]
- 9.Cheng VC, Wong SC, Chuang VW, So SY, Chen JH, Sridhar S. The role of community-wide wearing of face mask for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. The Journal of infection. 2020;81:107–14. doi: 10.1016/j.jinf.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khubchandani J, Saiki D, Kandiah J. Masks, gloves and the COVID-19 pandemic:Rapid assessment of public behaviors in the United States. Epidemiologia. 2020;1:16–22. doi: 10.3390/epidemiologia1010004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Danesh-Meyer, Helen V, McGhee CN. Implications of COVID-19 for Ophthalmologists. American Journal of Ophthalmology. 2021;223:108–18. doi: 10.1016/j.ajo.2020.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Akkara JD, Kuriakose A. The magic of three-dimensional printing in ophthalmology. Kerala J Ophthalmol. 2018;30:209–15. [Google Scholar]
- 13.Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19:A systematic review and meta-analysis. Lancet. 2020;395:1973–87. doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]