Abstract
Background
Although autoantibodies are an important hallmark of systemic lupus erythematosus (SLE), most are not specific for SLE or any of its clinical manifestations. Autoantibodies against post-translationally modified (PTM) proteins have been studied extensively in rheumatoid arthritis and associate with disease progression. While PTMs have also been detected in patients with SLE, studies on anti-PTM antibodies remain scarce. We studied the presence of anti-PTM antibodies in SLE and neuropsychiatric SLE (NPSLE), a manifestation that lacks serological markers.
Methods
IgG antibody responses against six PTMs (malondialdehyde–acetaldehyde adducts (MAA), advanced glycation end-products (AGE), carbamylation (CarP), citrullination, acetylation and nitration) were tested using ELISA in sera of 349 patients with SLE (mean age 44±13 years; 87% female) and compared with 108 healthy controls. Levels and positivity were correlated with clinical features and SLE manifestations.
Results
Anti-MAA, anti-AGE and anti-CarP antibodies were more prevalent in SLE compared with controls (MAA: 29% vs 3%, AGE: 18% vs 4%, CarP: 14% vs 5%, all p≤0.0001). Anti-MAA and anti-AGE antibodies correlated with clinical manifestations and serological inflammatory markers. Patients with major NPSLE showed higher positivity of anti-MAA (39% vs 24%, p=0.01) and anti-CarP antibodies (20% vs 11%, p=0.04) than patients without major NPSLE. In addition, anti-PTM antibody levels correlated with brain volumes, an objective measure of nervous system involvement.
Conclusions
In our NPSLE cohort, a subset of patients with SLE have anti-PTM antibodies against MAA, AGE and CarP modified proteins. Interestingly, anti-MAA and anti-CarP were more prevalent in NPSLE, a manifestation for which no biomarkers exist.
Keywords: lupus erythematosus, systemic; autoantibodies; epidemiology
Key messages.
What is already known about this subject?
Post-translationally modified (PTM) proteins and anti-PTM antibodies are described in many diseases, such as rheumatoid arthritis, in which anti-PTM antibodies are associated with disease progression.
What does this study add?
We demonstrate the presence of several anti-PTM antibodies (anti-malondialdehyde–acetaldehyde adducts, anti-advanced glycation end-products and anti-carbamylation) in patients with systemic lupus erythematosus (SLE) and their association with different aspects of disease activity in SLE and neuropsychiatric SLE (NPSLE).
How might this impact on clinical practice or further developments?
As virtually no biomarkers exist for NPSLE, anti-PTM antibodies are a potential candidate. Future studies should further establish the potential role of anti-PTM antibodies in NPSLE.
Introduction
Systemic lupus erythematosus (SLE) is a heterogeneous autoimmune disease characterised by a global loss of self-tolerance. Although autoantibodies are an important hallmark of SLE, many autoantibodies are not specific for SLE or specific SLE manifestations, such as neuropsychiatric involvement (NPSLE).1
Many different types of biomarkers exist and may be used in different contexts for diagnostic, prognostic and predictive purposes.2 In rheumatoid arthritis (RA), the identification of anti-citrullinated protein antibodies (ACPAs), antibodies (Abs) directed against a post-translational modification (PTM), has facilitated the diagnostic process and created new insights in its pathophysiology.3 4 Noteworthy, the presence of specific anti-PTM Abs also facilitates discrimination between phenotypes within RA, as they associate with more severe RA.5–8 It is possible that Abs against PTMs may also contribute to the identification of specific phenotypes in patients with SLE.
PTMs can occur naturally, as part of physiological functions, or may be the result of enzymatic or chemical processes.9 10 SLE has been associated with a dysregulated metabolic state and elevated levels of reactive oxygen species,11 which enhances the formation of PTMs. In some situations, immune responses against PTMs can develop, leading to anti-PTM Abs.12 To date, anti-PTM Ab studies in SLE have mainly focused on ACPA and anti-carbamylated protein (anti-CarP) Abs, which associated with increased joint damage.13–16 Several anti-PTM Abs have been associated with general disease activity (SLE Disease Activity Index (SLEDAI)) in lupus.17–19 In addition, phospholipid β2-glycoprotein-1 is reported to be modified by PTMs making it more antigenic.20 Around 35% of all patients with SLE are positive for Abs against these phospholipids, which are associated with antiphospholipid syndrome.21 Overall, studies on anti-PTM Abs in patients with SLE remain limited and techniques to measure anti-PTM Abs vary greatly.18 19
Based on previous studies, we hypothesised that SLE activity can lead to the generation of PTMs on relevant antigens and that there is specificity in breaking tolerance towards these neoantigens. In this study, we focused on IgG antibodies against six different PTMs, selected based on their association with activity in other diseases and variation in location in the protein, configuration and reversibility. We aimed to first study the presence of these six anti-PTM Abs in patients with SLE using a standardised method to assess specific anti-PTM Ab reactivities. Second, we aimed to assess the association between anti-PTM Abs and clinical phenotypes of SLE, in particular NPSLE, for which virtually no biomarkers exist. Additionally, both the subjective clinical diagnosis of NPSLE and objective evidence of nervous system involvement, namely radiological measurements, were assessed.
Methods
Study design and population
Patients visiting the NPSLE clinic of the Leiden University Medical Center between 2007 and 2019 with the clinical diagnosis of SLE and signed informed consent were included in this study. The NPSLE clinic is a tertiary referral center in which patients with neuropsychiatric (NP) symptoms, potentially caused by SLE, are assessed multidisciplinary. This evaluation process has been described in detail previously.22 23 In short, NP symptoms attributed to SLE by multidisciplinary consensus requiring immunosuppressive or anticoagulant treatment are classified as ‘major NPSLE’. NP symptoms not attributed to SLE, mild NP symptoms that do not require additional treatment other than symptomatic treatment or NP symptoms due to other causes are classified as minor/non-NPSLE. Patients with major NPSLE are further classified as having an ischaemic, inflammatory or combined (both ischaemic and inflammatory) phenotype, based on the suspected pathogenetic mechanism.22 Major NPSLE diagnoses are classified according to the 1999 American College of Rheumatology (ACR) case definitions for NPSLE syndromes.24 Online supplemental figure 1 depicts the inclusion procedure.
rmdopen-2021-002079supp001.pdf (422.6KB, pdf)
Patient and public involvement
No patients were involved in the concept or design of this study.
Patient characteristics
Demographic and clinical patient characteristics were collected from electronic medical files of the visit to the NPSLE clinic: age, sex, smoking status, body mass index, 1997 SLE classification criteria,25 SLE duration, SLEDAI-2K,26 Systemic Lupus International Collaborating Clinic/ACR Damage Index,27 presence and phenotype of NPSLE and medication use. Active nephritis was defined as haematuria, proteinuria, urinary casts or pyuria as according to the SLEDAI-2K.26 The presence of active arthritis was established during physical assessment. Serum samples from each participant were collected at time of visit to the NPSLE clinic. In some patients with inflammatory NPSLE, immunosuppressive treatment was already initiated at this time point (median treatment duration: 1 month). Details of routine laboratory assessment are provided in online supplemental file II.
Assessment of anti-PTMs
Generation of antigens
Modified proteins and their corresponding control non-modified protein were produced by either enzymatic or chemical reactions as previously described with some adaptations.7 28–31 For more details, see online supplemental file II.
Detection of anti-PTM IgG antibodies by ELISA
Modified fetal calf serum (FCS) and non-modified FCS were coated at 10 µg/mL in 0.1 M carbonate–bicarbonate buffer pH 9.6 on Nunc Maxisorp plates (430341, Thermofisher) overnight at 4°C. In between each step, plates were washed with Phosphate Buffered Saline (PBS)/0.05% Tween (P1379, Sigma). After washing, plates were blocked using PBS/1% Bovine Serum Albumin (BSA) for 6 hours at 4°C. Following washing, wells were incubated with serum at a 1/50 dilution in PBS/0.05% Tween/1% BSA (PTB) for CarP, citrullination (Cit), acetylation (AL) and nitration (NT) and at a 1/100 or 1/1000 dilution in PTB for advanced glycation end-products (AGE) and malondialdehyde–acetaldehyde adducts (MAA), respectively. For each PTM, a standard of a pool of anti-PTM positive sera was taken along in serial dilutions on each plate. Sera was incubated overnight at 4°C. Human IgG was detected using rabbit anti-human IgG-HRP (P0214, Dako) diluted in PTB and incubated at 4°C for 3.5 hours. After the final wash, HRP enzyme activity was visualised using ABTS (A1888, Merck) with 0.05% H202 (107209, Merck) and absorbance at 415 nm was read using a microplate reader (Bio-Rad). Serum samples of 108 healthy controls (HCs) from the Leiden area were also tested.32 33 Absorbance was transformed to arbitrary units per millilitre (aU/mL) using a corresponding standard line for each PTM. Background aU/mL of FCS was subtracted from the aU/mL signal on FCS-PTM to analyse specific anti-PTM reactivity. Negative outcomes were changed to 0. Positivity for specific anti-PTM Abs was defined as a value larger than the mean plus two times the SD in the HCs. HCs with a value ≥10× the mean were excluded in calculating the cut-off.
Additionally, sera of 54 patients with NPSLE at their second visit (<2 years after first visit) were analysed for anti-PTM Ab reactivity.
Brain volume
Brain volume measurements were available for 182 patients visiting the NPSLE clinic between 2007 and 2015. An extensive description thereof has been published previously.34 35 In short, white matter volume (WMV), grey matter volume, white matter hyperintensity volume and total brain volume (TBV) were assessed using the CAT12 toolbox from the statistical parametric mapping software and the Lesion Segmentation Toolbox V.2.0.15.36
Statistical analysis
Differences in levels of anti-PTM Abs between HCs, patients with SLE and specific SLE manifestations were assessed using the Mann-Whitney test and Χ2 test. Median, median difference and 95% CIs were calculated using quantile regression. Further analyses were only performed if anti-PTM Ab positivity between HCs and SLE differed by at least a factor of two. Spearman rank analyses were used to assess correlation between anti-PTM Ab levels and all continuous clinical variables (including brain volumes). Point-biserial correlations were used to assess correlation between the level of anti-PTM Abs (continuous) and other Abs (dichotomous). As anti-PTM Ab level was non-normally distributed, the levels were natural log transformed for the point-biserial correlations. Kruskal-Wallis test was used to compare level of anti-PTM Abs in patients with different NPSLE phenotypes. Wilcoxon signed-rank test was used to compare anti-PTM Ab level at baseline versus follow-up. P values of ≤0.05 were considered significant.
All statistical analyses were performed using STATA statistical software V.16.
Results
Study cohort
In total, 349 patients with SLE were included in this study: 87% female and mean age 43.7±13.4 years. At time of enrolment, median disease duration was 4 years (IQR: 1–13) and median disease activity (SLEDAI-2K) was four (IQR: 2–8) (table 1). The most common ACR 1997 criteria were anti-nuclear Abs (ANA) positivity ever (97%), immunological disorder (76%) and non-erosive arthritis (59%). Major NPSLE was diagnosed in 104 patients (30%), of which 51 patients had an inflammatory, 28 patients an ischaemic and 25 patients a combined phenotype. NPSLE syndromes (1999 ACR case definitions) are presented in online supplemental table 1. Active nephritis and arthritis were present in 85 and 17 patients, respectively. Most patients were ANA positive at inclusion (89%) and complement consumption was present in 34% of patients (table 2).
Table 1.
Characteristics of study population with systemic lupus erythematosus (SLE) at time of inclusion
| Patient characteristics | SLE (n=349) |
| Female | 303 (87) |
| Age (years) | 43.7±13.4 |
| Duration of SLE (years) | 4 (1–13) |
| SLEDAI-2K | 4 (2–8) |
| SDI | 1 (0–2) |
| BMI | 24.9±5.1 |
| Current smoking | 99 (28) |
| Comorbidities | |
| Hypertension | 120 (35) |
| Diabetes | 17 (5) |
| ACR 1997 criteria for SLE | |
| Malar rash | 135 (39) |
| Discoid rash | 65 (19) |
| Photosensitivity | 179 (51) |
| Oral ulcers | 149 (43) |
| Non-erosive arthritis | 206 (59) |
| Pleuritis or pericarditis | 90 (26) |
| Renal disorder (ever) | 94 (27) |
| Neurological disorder (psychosis/epilepsy) | 43 (12) |
| Haematological disorder | 175 (50) |
| Immunological disorder | 265 (76) |
| Positive ANA | 340 (97) |
| Current immunosuppressive medication | |
| Hydroxychloroquine | 226 (65) |
| Prednisolone | 187 (54) |
| Azathioprine | 55 (16) |
| Methotrexate | 22 (6) |
| Belimumab | 2 (1) |
| Other* | 11 (3) |
| Current organ involvement | |
| Major NPSLE | |
| Inflammatory | 51 (15) |
| Ischaemic | 28 (8) |
| Combined | 25 (7) |
| Nephritis | 85 (24) |
| Arthritis | 17 (5) |
Results are presented as n (%), mean±SD or median (IQR).
*Other: includes cyclophosphamide (n=9) and tacrolimus (n=2).
ACR, American College of Rheumatology; ANA, anti-nuclear antibodies; BMI, body mass index; NPSLE, neuropsychiatric SLE; SDI, Systemic Lupus International Collaborating Clinics/ACR Damage Index; SLEDAI, SLE Disease Activity Index.
Table 2.
Routine laboratory assessment of study population with systemic lupus erythematosus (SLE) at time of inclusion*
| SLE (n=349) | |
| Nuclear antibodies | |
| ANA | 309 (89) |
| Anti-dsDNA | 91 (26) |
| Anti-ENA | 166 (48) |
| Anti-SSA | 131 (38) |
| Anti-SSB | 39 (11) |
| Anti-Sm | 24 (7) |
| Anti-RNP | 46 (13) |
| Antiphospholipid antibodies | |
| Lupus anticoagulant | 101 (29) |
| Anti-cardiolipin IgG | 46 (13) |
| Anti-β2-glycoprotein IgG | 40 (15) |
| Complement factors | |
| Low C1q | 42 (12) |
| Low C3 | 119 (34) |
| Low C4 | 86 (25) |
| Inflammation | |
| CRP | 0.8 (0.8–7) |
| ESR | 17 (9–39) |
Results are presented as n (%) or median (IQR).
*Missing data nuclear antibodies: ANA+anti-dsDNA: n=1, other: n=2; antiphospholipid antibodies: anti-β2-glycoprotein n=79, lupus anticoagulant: n=5, aCl=1; complement factors: n=2, inflammation: n=2. Percentages are given for the number of positive patients divided by the number of patients tested.
ANA, anti-nuclear antibodies; anti-dsDNA, anti-double-stranded DNA; anti-RNP, anti-ribonucleoprotein; anti-Sm, anti-Smith; anti-SSA/B, anti-Sjögren’s syndrome-related antigen A/B autoantibodies; CRP, C-reactive protein; ENA, extractable nuclear antigen antibodies; ESR, erythrocyte sedimentation rate.
Anti-MAA, anti-AGE and anti-CarP levels and positivity differ between HCs and patients with lupus
IgG Ab levels against six PTMs (MAA, AGE, CarP, Cit, AL and NT) from serum of all patients with SLE were compared with serum of 108 HCs (table 3 and online supplemental figure 2A–F). Median differences (95% CI) between Ab levels in patients with SLE versus HCs were 12 (95% CI: 7 to 18) for anti-MAA, 32 (3 to 60) for anti-AGE, 91 (60 to 123) for anti-CarP, 0 (−1 to 1) for anti-Cit, 4 (−2 to 9) for anti-AL and 33 (−1 to 67) for anti-NT.
Table 3.
Prevalence of antibodies against specific post-translational modifications in patients with systemic lupus erythematosus (SLE) (n=349) and healthy controls (n=108)
| SLE (n=349) | Healthy controls (n=108) | ||||
| aU/mL | n, % positive | aU/mL | n, % positive | Median difference (95% CI) | |
| Anti-MAA | 35 (23–52)* | 101 (29) | 23 (18–29) | 3 (3) | 12 (7 to18) |
| Anti-AGE | 112 (51–200)* | 63 (18) | 80 (41–122) | 4 (4) | 32 (3 to 60) |
| Anti-CarP | 126 (50–206)* | 49 (14) | 35 (0–111) | 5 (5) | 91 (60 to 123) |
| Anti-Cit | 3 (2–6) | 22 (6) | 3 (2 – 6) | 3 (3) | 0 (–1 to 1) |
| Anti-AL | 8 (0–23) | 29 (8) | 4 (0–19) | 8 (7) | 4 (–2 to 9) |
| Anti-NT | 44 (0–177) | 17 (5) | 11 (0–132) | 8 (7) | 33 (–1 to 67) |
Results are presented as n (%) or median (IQR).
*Statistically significant difference between patients with SLE and healthy controls (p≤0.0001).
AGE, advanced glycation end-product; AL, acetylated protein; aU/mL, arbitrary units per millilitre; CarP, carbamylated protein; Cit, citrullinated protein; MAA, malondialdehyde–acetaldehyde adduct; NT, nitrated protein.
Cut-off for anti-PTM positivity was defined as values larger than 2 times SD above the mean of HCs. Anti-MAA, anti-AGE and anti-CarP showed significant higher positivity in patients with SLE compared with HCs (table 3).
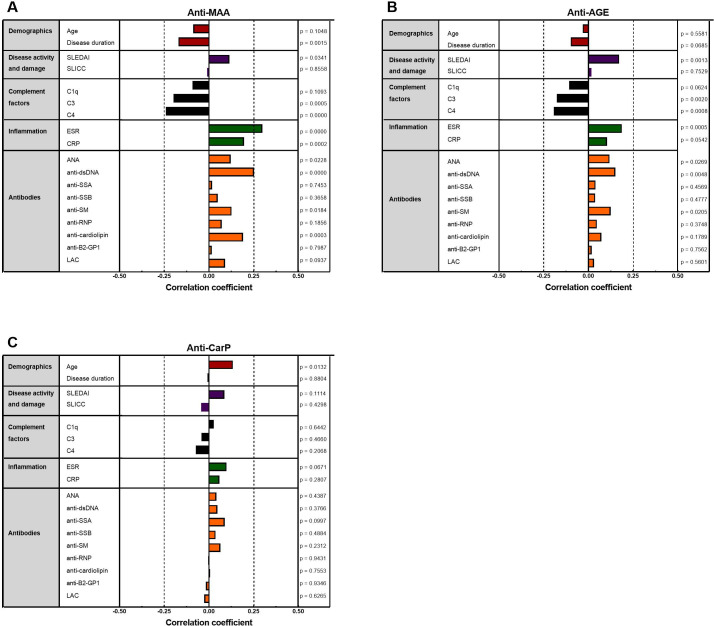
Anti-MAA and anti-AGE correlate with measures of systemic inflammation
Next, we sought to investigate whether these increased anti-PTM Abs correlated with clinical and serological markers (figure 1A–C and online supplemental table 2). Anti-MAA and anti-AGE both negatively correlated with levels of complement factors C3 and C4 (p≤0.002) and correlated positively with erythrocyte sedimentation rate (ESR) (p<0.001), ANA (p=0.02/0.03), anti-double-stranded DNA (p≤0.005) and anti-Smith (p=0.02). Anti-MAA negatively correlated with disease duration (p=0.03) and showed positive correlations with disease activity (p=0.03) and anti-cardiolipin (p=0.0003). Compared with anti-MAA, anti-AGE correlated slightly stronger with disease activity (p=0.001). All correlations found were modest (correlation coefficients ≤0.30). Anti-CarP only correlated significantly with age (p=0.01). There was no significant difference in anti-PTM Ab levels between patients with and without immunosuppressive treatment.
Figure 1.
Correlation between (A) anti-MAA IgG, (B) anti-AGE IgG, and (C) anti-CarP IgG and clinical and laboratory markers in patients with systemic lupus erythematosus (n=349), measured by Spearman correlation analyses (demographics–inflammation) and point-biserial correlation analyses after transformation (antibodies). AGE, advanced glycation end-product; ANA, anti-nuclear antibodies; anti-β2-GP1, anti-beta-2-glycoprotein; anti-dsDNA, anti-double-stranded DNA; anti-RNP, anti-ribonucleoprotein; anti-Sm, anti-Smith; anti-SSA/B, anti-Sjögren’s syndrome-related antigen A/B autoantibodies; CarP, carbamylated protein; CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; LAC, lupus anticoagulant; MAA, malondialdehyde–acetaldehyde adduct; SLEDAI, Systemic Lupus Erythematosus Disease Activity Index; SLICC, Systemic Lupus International Collaborating Clinic.
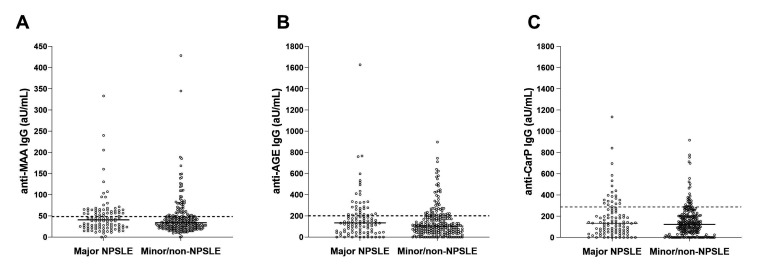
Anti-MAA and anti-CarP are more common in major NPSLE than in other SLE organ manifestations
Levels and positivity for different anti-PTM Abs were compared between patients with and without specific SLE manifestations (table 4 and figure 2A–C). As our cohort comprises patients visiting an expertise center for NPSLE, we primarily focused on this manifestation. Patients with major NPSLE more frequently harboured anti-MAA Abs (39% vs 24%, p=0.01) and anti-CarP Abs (20% vs 11%, p=0.04) compared with patients without major NPSLE, whereas the prevalence of anti-AGE Abs did not differ as clearly (23% vs 16%, p=0.13). In our cohort, for patients with active nephritis or active arthritis, differences in anti-PTM Ab positivity were less pronounced. Associations between the different anti-PTM Abs and ever having major organ manifestations are presented in online supplemental table 3.
Table 4.
The association between anti-PTM (IgG) antibodies and specific organ manifestations of systemic lupus erythematosus (n=349)
| NPSLE | Active nephritis | Arthritis | ||||
| Yes, n=104 | No, n=245 | Yes, n=85 | No, n=264 | Yes, n=17 | No, n=332 | |
| Anti-MAA | ||||||
| aU/mL | 41 (24–61) | 34 (23–48) | 36 (22–52) | 35 (23–52) | 30 (24–71) | 35 (22–51) |
| Positive | 41 (39)* | 60 (24) | 24 (28) | 77 (29) | 6 (35) | 95 (29) |
| Anti-AGE | ||||||
| aU/mL | 134 (48–217) | 103 (52–188) | 124 (70– 220) | 107 (50–187) | 115 (70–325) | 112 (50–198) |
| Positive | 24 (23) | 39 (16) | 20 (23) | 43(16) | 6 (35) | 57 (17) |
| Anti-CarP | ||||||
| aU/mL | 133 (52–245) | 123 (50–203) | 139 (55–261) | 121 (50–204) | 157 (65–258) | 126 (50–206) |
| Positive | 21 (20)** | 28 (11) | 16 (19) | 33 (13) | 3 (18) | 46 (14) |
Results are presented as n (%) or median (IQR).
Χ2 tests were used to assess the difference between the presence and absence of the specific manifestations.
NPSLE yes versus no: *p=0.01; **p=0.04, other values were not significant.
AGE, advanced glycation end-product; aU/mL, arbitrary units per millilitre; CarP, carbamylated protein; MAA, malondialdehyde–acetaldehyde adduct; NPSLE, neuropsychiatric systemic lupus erythematosus; PTM, post-translational modification.
Figure 2.
Levels of (A) anti-MAA, (B) anti-AGE, and (C) anti-CarP IgG in patients with (n=104) and without (n=245) major NPSLE. Reactivity was determined using ELISA and cut-off was calculated using mean plus two times the SD of the healthy controls (dashed line), as described in the Methods section. Reactivity is depicted as arbitrary units per millilitre (aU/mL). AGE, advanced glycation end-product; CarP, carbamylated protein; MAA, malondialdehyde–acetaldehyde adduct; NPSLE, neuropsychiatric systemic lupus erythematosus.
Anti-PTM Abs are similarly present in different major NPSLE phenotypes
As NPSLE has different pathophysiological origins, levels and positivity for different anti-PTM Abs were compared within specific phenotypes of major NPSLE (see online supplemental table 4). Patients with a combined NPSLE phenotype showed the most anti-PTM Ab positivity (anti-MAA=40%, anti-AGE=28%, anti-CarP=32%), followed by patients with an inflammatory phenotype (41%, 27% and 14%, respectively) and an ischaemic phenotype (36%, 11% and 21%, respectively). These differences were not statistically significant. In addition, no difference was observed in the presence of anti-PTM Abs between patients with inflammatory NPSLE who did and did not initiate immunosuppressive treatment prior to the clinic visit.
Brain volume and anti-PTM Abs
Previous analyses were based on the distinction between major and minor NP involvement, of which the diagnosis was based on multidisciplinary assessment. As this has the risk for phenotypical misclassification, we sought to study the correlation between anti-PTM Abs and an objective marker of central nervous system (CNS) involvement in SLE. For 182 patients (52%), assessment of brain volumes was available (see online supplemental table 5). The strongest correlations were between anti-MAA and WMV and TBV (Spearman ρ=–0.20 and –0.18; both p<0.02) and anti-AGE and WMV and TBV (both Spearman ρ=–0.16; both p=0.03). Anti-CarP showed a significant association with white matter hyperintensity volume (Spearman ρ=0.19, p=0.03).
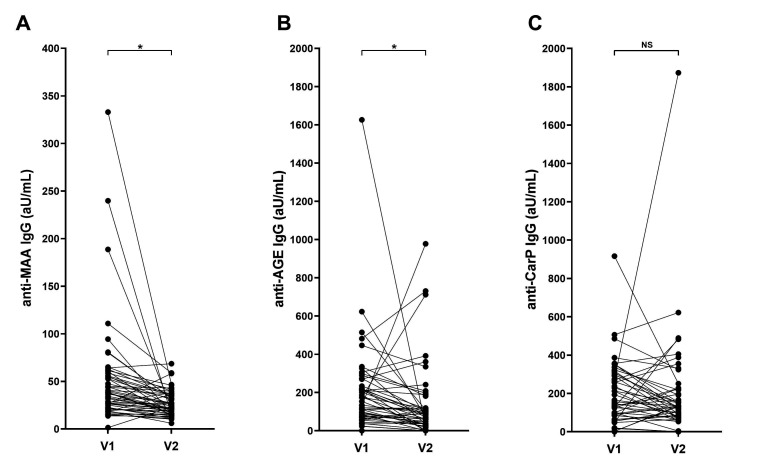
Longitudinal study comparing anti-PTM Ab responses over time
In order to study anti-PTM Abs over time, serum samples from 54 patients, that were taken within 2 years after the first visit, were analysed. Levels of anti-MAA, anti-AGE and anti-CarP Abs generally showed a decrease (figure 3A–C). This decrease was significant for anti-MAA and anti-AGE (p≤0.0001), but not for anti-CarP (p=0.20). Change in anti-MAA and anti-AGE Ab levels associated with change in SLEDAI-2K (both Spearman ρ: 0.29 and 0.28, p=0.04), respectively, but change in anti-CarP Ab level did not (Spearman ρ: 0.11, p=0.41).
Figure 3.
Levels of (A) anti-MAA, (B) anti-AGE and (C) anti-CarP in patients with NPSLE (n=54) over time within 2 years after first visit. Reactivity was determined using ELISA and cut-off was calculated using mean plus two times the SD of the healthy controls, as described in the Methods section. Reactivity is depicted as arbitrary units per millilitre (aU/mL). *P<0.01; NS, not significant. AGE, advanced glycation end-product; CarP, carbamylated protein; MAA, malondialdehyde–acetaldehyde adduct; NPSLE, neuropsychiatric systemic lupus erythematosus; V1, first visit; V2, second visit.
Discussion
We hypothesised that in SLE, there is generation of PTMs on relevant antigens and that the presence of anti-PTM autoantibodies may be associated with clinical presentation and/or disease activity. Therefore, we investigated the presence of Abs against six different PTMs on the same antigen backbone (FCS). We indeed observed that breaking of tolerance in SLE results in production of Abs against the PTMs, predominantly MAA, AGE and CarP, and less pronounced against Cit, AL and NT. Furthermore, anti-MAA Abs and anti-AGE Abs associated with markers of inflammation. Finally, we searched for Abs specific for NPSLE and observed that anti-MAA and anti-CarP Abs associated with major NPSLE.
Many different PTMs occur in both health and disease. Carbamylation and citrullination have been identified in patients with RA and Ab responses against these PTMs are nowadays used as a clinical measure.3 4 While it is currently unknown why a subset of the patients produce anti-PTM Abs, there is substantial insight into the processes that drive the PTM of proteins. Inflammation and oxidative stress can lead to formation of reactive oxygen species (ROS) or induction of enzymes, which may lead to the formation of PTMs. ROS can lead to malondialdehyde (MDA) following peroxidation of lipids from, for instance, cell membranes leading to MAA modification.37 Additionally, the ROS peroxynitrite is the reactive compound for nitration.38 Citrullination is the peptidyl arginine deiminase enzyme-mediated conversion of arginine.39 During carbamylation, the conversion of lysine into homocitrulline is driven by a chemical reaction with cyanate, a compound in equilibrium with urea and induced by smoking and inflammation.40 Excessive glycation is also a response to oxidative stress and inflammation leading to AGEs. AGEs in turn bind to AGE receptor leading to the perpetuation of inflammation.41 Excessive acetylation is a result of dysregulation of acetylation and deacetylation pathways.42 Taken together, specific PTMs are a consequence of inflammation and oxidative stress. It is therefore well possible that these modifications occur in patients with SLE in which widespread inflammation is going on. We previously observed that the PTM carbamylation is present in the joint of patients with RA, but also in the joint of HCs, while the anti-CarP Abs are only found in a subset of patients with RA.43 Why only a subset of patients with RA and SLE produce such anti-PTM Abs is still unknown. In our study, we demonstrated that three anti-PTM Abs are more prevalent in patients with SLE than in HCs, in increasing prevalence: anti-CarP, anti-AGE and anti-MAA. As only three out of six tested anti-PTMs showed increased reactivity, a specific induction process is implied. MAA, AGE and CarP are all modifications that occur on the lysine residue. However, AL is also a modification of lysine residue, but no difference in reactivity between patients with SLE and HCs was observed there. Whether a specific underlying pathological mechanism for reactivity against these three PTMs exists needs to be further investigated. As patients with SLE are known for their global loss of self-tolerance, it is plausible that PTMs, that are persistently or abundantly present, are targeted. However, other factors, such as genetics and environmental triggers, might play a role in breaking tolerance towards PTMs.44 45 In order to understand specific anti-PTM reactivities, the location of specific PTMs in different organ tissues in patients with SLE needs to be evaluated. Furthermore, studies on monoclonal Abs obtained from patients with SLE are required to further pinpoint specific reactivity.
The three notable anti-PTM Ab responses have been studied to some degree in SLE before. Anti-CarP Abs, prevalent in 8%–53% of patients with SLE in other studies, have been associated with articular involvement, joint damage and disease activity (SLEDAI).13 16 17 Our study was unable to confirm these findings, possibly because of the low number of patients with arthritis in our cohort. We can however exclude that the observed association between the presence of certain anti-PTM Abs and major NPSLE is driven by the association between anti-PTM Abs and arthritis and the concurrent presence of arthritis and major NPSLE. An increase of anti-CarP Abs was observed in patients with major NPSLE, but the clinical meaning of this remains to be elucidated as limited correlation with other clinical markers was observed. Anti-AGE Abs have not been studied previously in SLE. However, increased amounts of AGEs have been identified in skin tissue of patients with SLE and increased AGEs in blood plasma are described, which correlated with disease activity.46 We demonstrated an association between anti-AGE Abs and different markers of systemic inflammation. In our study, anti-MAA associated most clearly with different markers of inflammation. Few previous studies have investigated the role of MDA, the unstable predecessor of MAA in SLE. One study demonstrated that anti-MDA IgG positively correlated with disease activity, ESR and C-reactive protein and negatively correlated with complement factors.19 This is in line with the results of our study. In this same study, an association with renal involvement was found, using a different definition for active nephritis (proteinuria >5 g per day or greater than 3 by dipstick, and/or cellular casts), whereas our study demonstrated an association with major NPSLE, a disease for which virtually no biomarker exists.
Several Abs have been suggested as biomarker for NPSLE.47 In particular, anti-ribosomal P and anti-N-methyl-D-aspartate receptor Abs have been implicated in the pathogenesis of NPSLE, although their exact role remains inconclusive and their clinical value limited.48–50 It is thought that breaches of the neuroimmune interface (among others, the blood–brain barrier) might enable neuropathic Abs in the serum of patients to enter the CNS.49 Interestingly, we demonstrated that several anti-PTM Abs are more prevalent in patients with major NPSLE. Discrimination between the presence and absence of NPSLE is important, as it influences treatment. The diagnosis is based on multiple clinical factors, and the presence or absence of anti-PTM Abs could give further direction. Additional studies need to clarify whether anti-PTM responses are specific enough for NPSLE or should be interpreted as part of a series of markers to point towards specific subgroups. The observed association between anti-PTM Abs and NPSLE is supported by the correlation between specific anti-PTM Abs and white matter and white matter hyperintensity brain volume, objective measures of CNS involvement linked to NPSLE. MAA has previously been linked to brain injury and neurodegenerative diseases.51 52 Furthermore, in ageing individuals, increased levels of MDA are seen in the temporal lobes, occipital lobes and hippocampus, underlying the potential relevance of anti-MAA Abs.53 We demonstrated that all three anti-PTM Abs (anti-MAA, anti-AGE and anti-CarP) showed a decrease in reactivity over time, of which anti-MAA and anti-AGE correlated with disease activity. To further uncover the role of anti-PTM Abs in NPSLE, future studies should assess the presence of anti-PTMs in cerebrospinal fluid.
Our study has several strengths: we used a standardised controlled ELISA set-up with one antigen backbone for each of the PTMs and a well-defined cohort of patients with SLE and specifically NPSLE.
There are also several limitations to our study. A relatively large number of patients were negative or weakly positive for ANA at inclusion, which was tested at a dilution of 1:40. Therefore, we repeated the analyses in the patients positive for ANA (see online supplemental file III), which led to similar results as the main analyses. Furthermore, as this study cohort is part of a tertiary referral for NPSLE, other clinical subsets (such as arthritis) are less prevalent. In this exploratory study within a well-defined cohort, we found anti-PTM Abs as potential biomarker for NPSLE and now additional studies need to be performed to determine the discriminative value of anti-PTM in different clinical settings, such as the outpatient clinic of a non-academic hospital. In addition, the clinical correlations identified in this study were modest and need further investigation. Lastly, the diagnosis of major NPSLE is made on clinical grounds. Although this is a clinically relevant phenotype, there still might be different underlying biological processes. Therefore, we used an objective marker (brain volumes) for CNS involvement and found an association with anti-PTM Abs.
In conclusion, we identified three anti-PTM Abs (anti-MAA, anti-AGE and anti-CarP) that are present more frequently in patients with SLE, of which anti-MAA and anti-AGE correlate with measurements of systemic inflammation. Furthermore, several anti-PTM Abs (anti-MAA and anti-CarP) were more prevalent in patients with major NPSLE, a disease manifestation currently lacking a suitable biomarker. In addition, all three anti-PTM Abs also correlated with brain volumes. Further research should confirm the role of anti-PTM Abs as well as its discriminative value for (NP)SLE.
Acknowledgments
We thank our colleagues from the Department of Radiology, especially Jeroen de Bresser and Francesca Inglese, for the data on brain volumes.
Footnotes
Contributors: All authors were involved in the design and interpretation of the study. (NP)SLE data collection and statistical analyses were performed by RCM under the supervision of GMS-B, TWJH and MK. Anti-PTM antibody analyses and interpretation were performed by MDvdB and NVB under the supervision of LAT. LAT is the guarantor for this study.
Funding: LAT has received funding from the European Research Council (ERC) under the European Union’s Horizon 2020 research and innovation programme (grant agreement no. 724517).
Competing interests: TWJH and LAT are listed as inventors on a patent describing the methods to detect anti-CarP antibodies.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. The research protocol and deidentified participant data are available upon reasonable request. Requests can be sent to l.a.trouw@lumc.nl.
Ethics statements
Patient consent for publication
Obtained.
Ethics approval
This study involves human participants and was approved by the Medical Ethical Committee of Leiden-The Hague-Delft (reference number: B18.040). Participants gave informed consent to participate in the study before taking part.
References
- 1.Dema B, Charles N. Autoantibodies in SLE: specificities, isotypes and receptors. Antibodies 2016;5:2. 10.3390/antib5010002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Califf RM. Biomarker definitions and their applications. Exp Biol Med 2018;243:213–21. 10.1177/1535370217750088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Willemze A, Trouw LA, Toes REM, et al. The influence of AcpA status and characteristics on the course of RA. Nat Rev Rheumatol 2012;8:144–52. 10.1038/nrrheum.2011.204 [DOI] [PubMed] [Google Scholar]
- 4.Aletaha D, Neogi T, Silman AJ, et al. 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League against rheumatism collaborative initiative. Arthritis Rheum 2010;62:2569–81. 10.1002/art.27584 [DOI] [PubMed] [Google Scholar]
- 5.Kroot EJ, de Jong BA, van Leeuwen MA, et al. The prognostic value of anti-cyclic citrullinated peptide antibody in patients with recent-onset rheumatoid arthritis. Arthritis Rheum 2000;43:1831–5. [DOI] [PubMed] [Google Scholar]
- 6.van der Helm-van Mil AHM, Verpoort KN, Breedveld FC, et al. Antibodies to citrullinated proteins and differences in clinical progression of rheumatoid arthritis. Arthritis Res Ther 2005;7:R949–58. 10.1186/ar1767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shi J, Knevel R, Suwannalai P, et al. Autoantibodies recognizing carbamylated proteins are present in sera of patients with rheumatoid arthritis and predict joint damage. Proc Natl Acad Sci U S A 2011;108:17372–7. 10.1073/pnas.1114465108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Trouw LA, Rispens T, Toes REM. Beyond citrullination: other post-translational protein modifications in rheumatoid arthritis. Nat Rev Rheumatol 2017;13:331–9. 10.1038/nrrheum.2017.15 [DOI] [PubMed] [Google Scholar]
- 9.Pejaver V, Hsu W-L, Xin F, et al. The structural and functional signatures of proteins that undergo multiple events of post-translational modification. Protein Sci 2014;23:1077–93. 10.1002/pro.2494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bagwan N, El Ali HH, Lundby A. Proteome-Wide profiling and mapping of post translational modifications in human hearts. Sci Rep 2021;11:2184. 10.1038/s41598-021-81986-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lightfoot YL, Blanco LP, Kaplan MJ. Metabolic abnormalities and oxidative stress in lupus. Curr Opin Rheumatol 2017;29:442–9. 10.1097/BOR.0000000000000413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Navarro Quiroz E, Chavez-Estrada V, Macias-Ochoa K, et al. Epigenetic mechanisms and posttranslational modifications in systemic lupus erythematosus. Int J Mol Sci 2019;20:5679. 10.3390/ijms20225679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ceccarelli F, Perricone C, Colasanti T, et al. Anti-carbamylated protein antibodies as a new biomarker of erosive joint damage in systemic lupus erythematosus. Arthritis Res Ther 2018;20:126. 10.1186/s13075-018-1622-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Massaro L, Ceccarelli F, Colasanti T, et al. Anti-carbamylated protein antibodies in systemic lupus erythematosus patients with articular involvement. Lupus 2018;27:105–11. 10.1177/0961203317713141 [DOI] [PubMed] [Google Scholar]
- 15.Pecani A, Alessandri C, Spinelli FR, et al. Prevalence, sensitivity and specificity of antibodies against carbamylated proteins in a monocentric cohort of patients with rheumatoid arthritis and other autoimmune rheumatic diseases. Arthritis Res Ther 2016;18:276. 10.1186/s13075-016-1173-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ziegelasch M, van Delft MAM, Wallin P, et al. Antibodies against carbamylated proteins and cyclic citrullinated peptides in systemic lupus erythematosus: results from two well-defined European cohorts. Arthritis Res Ther 2016;18:289. 10.1186/s13075-016-1192-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li Y, Jia R, Liu Y, et al. Antibodies against carbamylated vimentin exist in systemic lupus erythematosus and correlate with disease activity. Lupus 2020;29:239–47. 10.1177/0961203319897127 [DOI] [PubMed] [Google Scholar]
- 18.Wang G, Pierangeli SS, Papalardo E, et al. Markers of oxidative and nitrosative stress in systemic lupus erythematosus: correlation with disease activity. Arthritis Rheum 2010;62:NA–72. 10.1002/art.27442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hardt U, Larsson A, Gunnarsson I, et al. Autoimmune reactivity to malondialdehyde adducts in systemic lupus erythematosus is associated with disease activity and nephritis. Arthritis Res Ther 2018;20:36. 10.1186/s13075-018-1530-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Buttari B, Profumo E, Capozzi A, et al. Post-translational modifications of proteins in antiphospholipid antibody syndrome. Crit Rev Clin Lab Sci 2019;56:511–25. 10.1080/10408363.2019.1650714 [DOI] [PubMed] [Google Scholar]
- 21.Ünlü O, Zuily S, Erkan D. The clinical significance of antiphospholipid antibodies in systemic lupus erythematosus. Eur J Rheumatol 2016;3:75–84. 10.5152/eurjrheum.2015.0085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Monahan RC, Fronczek R, Eikenboom J, et al. Mortality in patients with systemic lupus erythematosus and neuropsychiatric involvement: a retrospective analysis from a tertiary referral center in the Netherlands. Lupus 2020;29:1892–901. 10.1177/0961203320963815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zirkzee EJM, Steup-Beekman GM, van der Mast RC, et al. Prospective study of clinical phenotypes in neuropsychiatric systemic lupus erythematosus; multidisciplinary approach to diagnosis and therapy. J Rheumatol 2012;39:2118–26. 10.3899/jrheum.120545 [DOI] [PubMed] [Google Scholar]
- 24.The American College of rheumatology Nomenclature and case definitions for neuropsychiatric lupus syndromes. Arthritis Rheum 1999;42:599–608. [DOI] [PubMed] [Google Scholar]
- 25.Hochberg MC. Updating the American College of rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 1997;40:40:1725. 10.1002/art.1780400928 [DOI] [PubMed] [Google Scholar]
- 26.Gladman DD, Ibañez D, Urowitz MB. Systemic lupus erythematosus disease activity index 2000. J Rheumatol 2002;29:288–91. [PubMed] [Google Scholar]
- 27.Gladman D, Ginzler E, Goldsmith C, et al. The development and initial validation of the systemic lupus international collaborating Clinics/American College of rheumatology damage index for systemic lupus erythematosus. Arthritis Rheum 1996;39:363–9. 10.1002/art.1780390303 [DOI] [PubMed] [Google Scholar]
- 28.Ohmori H, Oka M, Nishikawa Y, et al. Immunogenicity of autologous IgG bearing the inflammation-associated marker 3-nitrotyrosine. Immunol Lett 2005;96:47–54. 10.1016/j.imlet.2004.07.004 [DOI] [PubMed] [Google Scholar]
- 29.Dekkers JS, Verheul MK, Stoop JN, et al. Breach of autoreactive B cell tolerance by post-translationally modified proteins. Ann Rheum Dis 2017;76:1449–57. 10.1136/annrheumdis-2016-210772 [DOI] [PubMed] [Google Scholar]
- 30.Guan K-L, Yu W, Lin Y, et al. Generation of acetyllysine antibodies and affinity enrichment of acetylated peptides. Nat Protoc 2010;5:1583–95. 10.1038/nprot.2010.117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Duryee MJ, Klassen LW, Schaffert CS, et al. Malondialdehyde-acetaldehyde adduct is the dominant epitope after MDA modification of proteins in atherosclerosis. Free Radic Biol Med 2010;49:1480–6. 10.1016/j.freeradbiomed.2010.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nagai R, Matsumoto K, Ling X, et al. Glycolaldehyde, a reactive intermediate for advanced glycation end products, plays an important role in the generation of an active ligand for the macrophage scavenger receptor. Diabetes 2000;49:1714–23. 10.2337/diabetes.49.10.1714 [DOI] [PubMed] [Google Scholar]
- 33.Verheul MK, Yee A, Seaman A, et al. Identification of carbamylated alpha 1 anti-trypsin (A1AT) as an antigenic target of anti-CarP antibodies in patients with rheumatoid arthritis. J Autoimmun 2017;80:77–84. 10.1016/j.jaut.2017.02.008 [DOI] [PubMed] [Google Scholar]
- 34.Inglese F, Kant IMJ, Monahan RC, et al. Different phenotypes of neuropsychiatric systemic lupus erythematosus are related to a distinct pattern of structural changes on brain MRI. Eur Radiol 2021;31:8208–17. 10.1007/s00330-021-07970-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Monahan RC, Inglese F, Middelkoop H, et al. White matter hyperintensities associate with cognitive slowing in patients with systemic lupus erythematosus and neuropsychiatric symptoms. RMD Open 2021;7:e001650. 10.1136/rmdopen-2021-001650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jenkinson M, Bannister P, Brady M, et al. Improved optimization for the robust and accurate linear registration and motion correction of brain images. Neuroimage 2002;17:825–41. 10.1006/nimg.2002.1132 [DOI] [PubMed] [Google Scholar]
- 37.Thiele GM, Duryee MJ, Anderson DR, et al. Malondialdehyde-acetaldehyde adducts and anti-malondialdehyde-acetaldehyde antibodies in rheumatoid arthritis. Arthritis Rheumatol 2015;67:645–55. 10.1002/art.38969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Beckman JS. Oxidative damage and tyrosine nitration from peroxynitrite. Chem Res Toxicol 1996;9:836–44. 10.1021/tx9501445 [DOI] [PubMed] [Google Scholar]
- 39.Vossenaar ER, Zendman AJW, van Venrooij WJ, et al. PAD, a growing family of citrullinating enzymes: genes, features and involvement in disease. Bioessays 2003;25:1106–18. 10.1002/bies.10357 [DOI] [PubMed] [Google Scholar]
- 40.Verheul MK, van Veelen PA, van Delft MAM, et al. Pitfalls in the detection of citrullination and carbamylation. Autoimmun Rev 2018;17:136–41. 10.1016/j.autrev.2017.11.017 [DOI] [PubMed] [Google Scholar]
- 41.Schmidt AM, Yan SD, Yan SF, et al. The multiligand receptor RAGE as a progression factor amplifying immune and inflammatory responses. J Clin Invest 2001;108:949–55. 10.1172/JCI200114002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Drazic A, Myklebust LM, Ree R, et al. The world of protein acetylation. Biochim Biophys Acta 2016;1864:1372–401. 10.1016/j.bbapap.2016.06.007 [DOI] [PubMed] [Google Scholar]
- 43.Verheul MK, Janssen GMC, de Ru A, et al. Mass-Spectrometric identification of carbamylated proteins present in the joints of rheumatoid arthritis patients and controls. Clin Exp Rheumatol 2021;39:570–7. [PubMed] [Google Scholar]
- 44.Han B, Diogo D, Eyre S, et al. Fine mapping seronegative and seropositive rheumatoid arthritis to shared and distinct HLA alleles by adjusting for the effects of heterogeneity. Am J Hum Genet 2014;94:522–32. 10.1016/j.ajhg.2014.02.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Raychaudhuri S, Sandor C, Stahl EA, et al. Five amino acids in three HLA proteins explain most of the association between MHC and seropositive rheumatoid arthritis. Nat Genet 2012;44:291–6. 10.1038/ng.1076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chen D-Y, Chen Y-M, Lin C-C, et al. The potential role of advanced glycation end products (AGEs) and soluble receptors for ages (sRAGE) in the pathogenesis of adult-onset still's disease. BMC Musculoskelet Disord 2015;16:111. 10.1186/s12891-015-0569-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sato S, Temmoku J, Fujita Y, et al. Autoantibodies associated with neuropsychiatric systemic lupus erythematosus: the quest for symptom-specific biomarkers. Fukushima J Med Sci 2020;66:1–9. 10.5387/fms.2020-02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Karassa FB, Afeltra A, Ambrozic A, et al. Accuracy of anti-ribosomal P protein antibody testing for the diagnosis of neuropsychiatric systemic lupus erythematosus: an international meta-analysis. Arthritis Rheum 2006;54:312–24. 10.1002/art.21539 [DOI] [PubMed] [Google Scholar]
- 49.Schwartz N, Stock AD, Putterman C. Neuropsychiatric lupus: new mechanistic insights and future treatment directions. Nat Rev Rheumatol 2019;15:137–52. 10.1038/s41584-018-0156-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wen J, Stock AD, Chalmers SA, et al. The role of B cells and autoantibodies in neuropsychiatric lupus. Autoimmun Rev 2016;15:890–5. 10.1016/j.autrev.2016.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lorente L, Martín MM, Abreu-González P, et al. Maintained high sustained serum malondialdehyde levels after severe brain trauma injury in non-survivor patients. BMC Res Notes 2019;12:789. 10.1186/s13104-019-4828-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Islam MT. Oxidative stress and mitochondrial dysfunction-linked neurodegenerative disorders. Neurol Res 2017;39:73–82. 10.1080/01616412.2016.1251711 [DOI] [PubMed] [Google Scholar]
- 53.Domínguez-González M, Puigpinós M, Jové M, et al. Regional vulnerability to lipoxidative damage and inflammation in normal human brain aging. Exp Gerontol 2018;111:218–28. 10.1016/j.exger.2018.07.023 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
rmdopen-2021-002079supp001.pdf (422.6KB, pdf)
Data Availability Statement
Data are available upon reasonable request. The research protocol and deidentified participant data are available upon reasonable request. Requests can be sent to l.a.trouw@lumc.nl.