Abstract
(1) Background: Thermal treatment of high-protein food may lead to the formation of mutagenic and carcinogenic compounds, e.g., polycyclic aromatic hydrocarbons and heterocyclic aromatic amines. Frequent consumption of processed meat was classified by the International Agency for Research on Cancer as directly carcinogenic for humans. (2) Methods: A literature review was carried out based on a search of online databases for articles on consuming thermally processed meat containing carcinogenic compounds versus a risk of cancers in humans published between 2001 and 2021. (3) Results: A review of the current literature on the participation of PAHs and HAA in the formation of certain neoplasms indicates a positive relationship between diet and the incidences of many cancers, especially colon cancer. A simple way to obtain dishes with reduced contents of harmful compounds is the use of spices and vegetables as meat additives. These seasonings are usually rich in antioxidants that influence the mechanism of HAA and PAH synthesis in food. (4) Conclusions: As there is a growing risk of a cancer tendency because of exposing humans to PAHs and HAAs, it is extremely vital to find a simple way to limit carcinogenic compound synthesis in a processed proteinaceous food. Disseminating the knowledge about the conditions for preparing dishes with a reduced content of carcinogenic compounds could become a vital element of cancer prevention programs.
Keywords: cancer, meat, PAH, HAA, cooking procedures
1. Introduction
It is assumed that 90–95% of cancers are caused by environmental factors. Even 30–35% of them are caused by a diet [1]. Food may contain many harmful chemical compounds left after the production process (nitrates, pesticides and dioxins). Compounds with mutagenic and carcinogenic activity may also be formed during storage or the thermal processing of high-protein food [2]. These compounds include products of lipid and protein oxidation, polycyclic aromatic hydrocarbons (PAHs) and heterocyclic aromatic amines (HAAs) and, also, nitroso compounds (NOCs) formed from the nitrates (III) added to meat products [3]. Carcinogenic NOCs may also be formed endogenously with the contribution of heme iron [3]. In 2015, the International Agency for Research on Cancer (IARC), based on a sufficient number of evidence for harmfulness for human health, classified red meat as “probably carcinogenic for humans” (group 2A) and processed red meat as “carcinogenic for humans” (group 1) [4]. To what extent the diet may cause a death from cancer depends on the type of cancer. Regular consumption of red and thermally treated meat is risky particularly in the case of the following cancers: colon, prostatic gland, breast, stomach, pancreas and oral cavity. In the present paper, a literature review on muta- and carcinogenic contributions of PAHs and HAAs contained in red meat in some cancer formations is presented.
2. Materials and Methods
2.1. Protocol Registration
In September 2021, the protocol for this review was developed. The review has been registered in the PROSPERO database (identification number 318707). For the methodological evaluation of the quality of this review, the authors used the AMSTER 2 checklist and the Preferred Reporting Items for Systematic Reviews and Meta-Analyzes (PRISMA) protocols (Figure 1).
Figure 1.
Protocol PRISMA flowcharts for the review.
2.2. Selection Criteria
The selection criteria were as follows: (1) case–control or cohort studies involving patients with specific cancers; (2) research works; (3) systematic reviews and meta-analyses; (4) research from the period 2001–2021; (5) research in English; (6) only studies involving humans were included in the analysis; (7) research about meat consumption that did not specifically contain red or processed meat were excluded from the analysis; and (8) excluded were also the articles describing other diet-dependent diseases. After applying the inclusion and exclusion criteria and analysis of all the abstracts, 140 articles were selected on the basis of which this work was written.
2.3. Search Strategy
A review of the literature was performed using the PubMed, Medline, Google Scholar, ProQuest, CINAHL and OpenGrey online databases. The following keywords were used to find the relevant articles: “red meat”, “polycyclic aromatic hydrocarbons”, “PAHs”, “heterocyclic aromatic amines”, ”HAA”, “HCA”, “cooking procedures”, “head and neck cancer”, “esophagus cancer”, “oesophagus cancer”, “pancreatic cancer”, “stomach cancer”, “colon cancer”, “prostate cancer”, “lymphoma”, “kidney cancer”, “bladder cancer”, “breast cancer”, “risk”, “prevention” and “diet”. The review concentrated on the publications from the period 2010–2021. In order to identify additional relevant literature, the databases were also searched manually. The sets of keywords were combined individually, and the eligibility of each study was judged independently by two authors.
3. Results
3.1. Polycyclic Aromatic Hydrocarbons (PAHs) in Food
Polycyclic aromatic hydrocarbons are a numerous group of over 200 organic compounds built of two or more fused aromatic rings [5]. PAHs are formed the during incomplete combustion of organic matter [6]. PAHs are slightly water-soluble. Due to a lipophilic character, they tend to gather in an alimentary chain [7].
Polycyclic aromatic hydrocarbons may get into food from the polluted environment and from the atmosphere adsorbed into particulate matter, as well as from water and soil. These compounds have been found in fruit and vegetables coming from the fields in industrial regions and the fields placed close to busy roads [8,9]. PAHs may be also formed during food processing. Protein products (fish and meat), which are smoked and dried or thermally cooked (grilled, roasted or fried), are a main source of polycyclic aromatic hydrocarbons [5,10,11,12,13,14,15]. Particles of organic components in food are easily fragmented under high temperatures during pyrolysis, and free radicals that are formed may create PAHs via pyrosynthesis [6,16]. Model testing showed that polycyclic aromatic hydrocarbons may be formed, among others, of aliphatic α-amino acids [17,18,19]. It was found that, in pork sausages containing more basic amino acids (L-lysine and L-arginine), more PAHs were formed than in the presence of acidic amino acids (L-glutamic and L-aspartate). Moreover, the addition of an aromatic amino acid generated fewer PAHs in the grilled product than by using other amino acids [20]. The addition of D-glucose can increase the PAH formation when compared with that of keto-based sugar (D-fructose) [18,20]. PAHs are also formed from fatty acids and fats [16,21]. The addition of different methyl esters of fatty acids (as lipid precursors) in heated meat model systems led significantly to an increase the PAH concentration [22,23]. PAHs may also be formed from the result of cholesterol and vegetable sterol pyrolysis [24].
In the European Union countries, there have been regulations for many years, and they define permissible concentrations of PAHs in some groceries. These regulations are updated all the time according to the results of numerous studies concerning the PAH determination in food. In 2006, one of the hydrocarbons—benzo(a)pyrene (BaP)—was pointed by the Scientific Committee on Food of the EU (SFC) as a marker for PAH presence and its carcinogenic activity in food [25]. The report of the European Food Safety Authority (EFSA) presenting PAH concentrations in about 10,000 different food samples showed that, in about 33% of the samples analyzed for the 15 SFC priority PAHs, other carcinogenic and genotoxic PAHs were detected, despite testing negative for BaP (concentration of BaP was below the limit of detection) [24]. Based on these data, the Scientific Panel on Contaminants in the Food Chain of EFSA concluded that benzo(a)pyrene is not a suitable marker for the occurrence of polycyclic aromatic hydrocarbons in food and that a system of four compounds (PAH4): benzo(a)pyrene (BaP), benz(a)anthracene (BaA), benzo(b)fluoranthene (BbFl) and chrysene (Chr) or eight compounds (PAH8): PAH4 + benzo(k)fluoranthene (BkF), benzo(ghi)perylene (BghiP), dibenzo(a,h)anthracene (DBahA) and indeno(1,2,3-cd)pyrene (IP) would be the most suitable indicators of PAHs in food. The formulas of these PAHs are presented in Table 1. The EFSA also concluded that a system of eight hydrocarbons (PAH8) would not provide much added value compared to a system of four compounds (PAH4) [26]. According to the regulations the concentration of BaP in smoked meat and smoked meat products should not exceed 5 µg/kg and PAH4 30 µg/kg, and since 1 September 2014, it should be reduced even to 2 µg and 12 µg/kg. Additionally, the regulations say that heat-treated meat and meat products (grilled and barbecued) sold to the final consumer cannot contain more than 5 µg/kg and PAH4 30 µg/kg. In many EU countries, in traditionally smoked meat and smoked meat products, the lower PAH levels (2 and 12 µg/kg) were not achievable by changing smoking practices, and that is why, since 2020, in some countries of the EU, higher acceptable levels: 5 µg/kg (for BaP) and 30 µg/kg (for PAH4) have been accepted again for local products [27].
Table 1.
Compounds of polycyclic aromatic hydrocarbons selected by EFSA as markers for the occurrence of PAHs in food [26].
| Name | Abbreviation | Structure | IARC Carcinogenic Group * | Classification | |
|---|---|---|---|---|---|
| Benzo(a)pyrene | BaP |

|
1 | PAH4 | PAH8 |
| Benz(a)anthracene | BaA |

|
2B | ||
| Benzo(b)fluoranthene | BbF |

|
2B | ||
| Chrysene | Chr |

|
2B | ||
| Benzo(k)fluoranthene | BkF |

|
2B | ||
| Benzo(ghi)perylene | BghiP |

|
3 | ||
| Dibenzo(a,h)anthracene | DB(ah)A |

|
2A | ||
| Indeno(1,2,3-cd)pyrene | IP |
|
2B | ||
* IARC classification groups: 1—carcinogenic to humans; 2A—probably carcinogenic to humans; 2B—possibly carcinogenic to humans; 3—not classifiable as to its carcinogenicity to humans.
3.2. Heterocyclic Aromatic Amines (HAAs) in Food
Heterocyclic aromatic amines are organic nitrogen compounds built from two or three condensed rings from which one is aromatic and the others are heterocyclic. All HAAs have one exocyclic amine group (-NH2), except for three compounds from this group [28,29,30]. Investigations on heterocyclic aromatic amines formed in high-protein food started in Japan in the 1970s of the 20th century [31,32]. Since then, the structures of over 30 amines have been determined [27,28,32,33,34,35].
HAAs are classified into two groups, depending on their formation temperature: polar (called also “thermic”), which are formed in temperatures from 100 °C to 250 °C (temperatures typical for the cooking, baking, frying and grilling of proteinaceous food), and non-polar, which are formed in higher temperatures. Polar compounds are formed in accordance with the Maillard reaction, from α-amino acids, reducing sugars (glucose, fructose and ribose) and creatine, all of them occurring naturally in meat [28,36]. This reaction occurs between the amine group of amino acids and the carbonyl group of sugars. The Maillard reaction involves both free radicals (pyridine and pyrazine radicals) and reactive carbonyl structures, so both the free radical pathway and a carbonyl pathway were proposed as mechanisms of HAA synthesis [29]. Non-polar HAAs (called also “pyrolytic”) are formed mainly from the result of the thermal decomposition of tryptophan and glutamic acid. The reactive fragments formed at high temperatures through radical reactions may condense to generate heterocyclic structures [35].
The concentrations of HAAs in different meat dishes range from 0 up to several dozen ng in 1 g of the product [28]. So far, no regulations have been introduced regarding the permissible content of HAAs in food. The kind and concentration of heterocyclic aromatic amines formed in food depend on many factors—first of all, on temperature, time of heating and kind of thermal processing [16,30,37,38]. Moreover, they also depend on the kind of meat, content of amino acids [39] and sugars [28] in it and on the kind of fats used for dish preparing [40] and the additives as well [28,30,36,41]. Heterocyclic aromatic amines are formed as early as after a few minutes of frying, and they occur even in slightly fried dishes. Small amounts of heterocyclic amines can also be found in cooked and stewed dishes [28,36].
The International Agency for Research on Cancer included one of HAA in the group 2A (probably carcinogenic to humans) and nine to the 2B group (possibly carcinogenic to humans). The names and formulas of these compounds are presented in Table 2.
Table 2.
Heterocyclic aromatic amines classified by IARC as carcinogenic [42].
| Name | Abbreviation | Structure | IARC Carcinogenic Group * |
|---|---|---|---|
| Polar HAAs (“thermic compounds”) | |||
| 2-amino-3-methylimidazo [4,5-f]quinolone |
IQ |

|
2A |
| 2-amino-3,4-dimethylimidazo [4,5-f]quinoline |
MeIQ |

|
2B |
| 2-amino-3,8-dimethylimidazo [4,5-f]quinoxaline |
MeIQx |

|
2B |
| 2-amino-1-methyl-6-phenylimidazo [4,5-b]pyridine |
PhIP |
|
2B |
| Non-polar HAAs (“pyrolytic compounds”) | |||
| 2-amino-9H-pyrido [2,3-b]indole |
AαC |
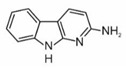
|
2B |
| 2-amino-3-methyl-9H-pyrido [2,3-b]indole |
MeAαC |

|
2B |
| 3-amino-1-methyl-5H-pyrido [4,3-b]indole |
Trp-P-2 |
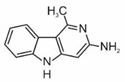
|
2B |
| 3-amino-1,4-dimethyl-5H-pyrido (4,3-b)indole |
Trp-P-1 |

|
2B |
| 2-aminodipyrido [1,2-a:3′,2′-d] imidazole |
Glu-P-2 |

|
2B |
| 2-amino-6-methyldipyrido [1,2-a:3′,2′ d] imidazole |
Glu-P-1 |

|
2B |
* IARC classification groups: 2A—probably carcinogenic to humans, 2B—possibly carcinogenic to humans.
3.3. Mechanisms of Bioactivation
3.3.1. PAHs
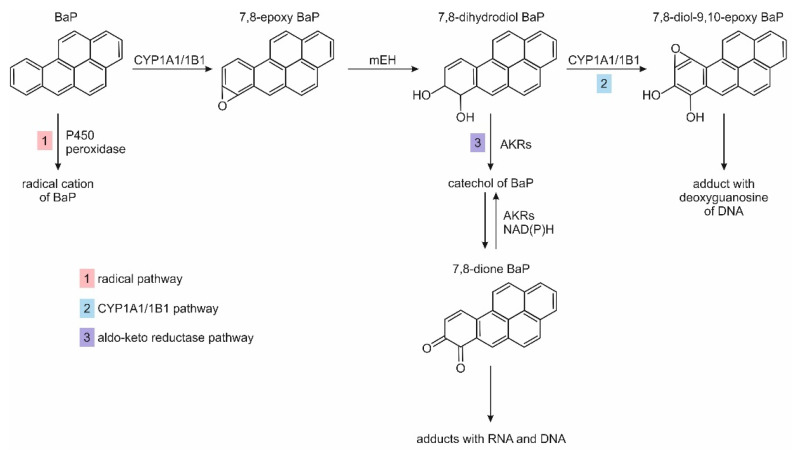
PAHs may enter the human body through the respiratory tract, digestive tract or the skin. As lipophilic compounds, they are transported in the blood connected with lipoproteins. To be removed from the body, they must undergo biotransformation to water-soluble compounds. The metabolism of PAHs proceeds in one or two phases with the participation of various liver enzymes. The reactions of phase I are catalyzed by cytochrome P450 (CYP) and leads to the formation of polar oxygen derivatives, amongst which epoxides are the primary products. The enzymatic processes of phase I include reactions of oxidations, reductions, hydrolyses and hydration. The phase II enzymes catalyze the conjugation of oxidized PAHs with compounds endogenously occurring in the body, such as sulphates, amino acids, glucuronic acid and glutathione (GSH). The conjugates (PAHs metabolites) as polar compounds may be excreted from the organism with bile and urine [43]. Compounds of carcinogenic activity can be generated from PAHs as a result of enzymatic reactions following three main pathways. The first occurs with the participation of cytochrome CYP1A1/1B1 and epoxide hydrolase, the second, undergone by CYP-peroxidase, is a radical pathway, and the third is catalyzed by aldo-keto reductases [44]. These three pathways for carcinogenic BaP are shown in Figure 2.
Figure 2.
PAH metabolism pathway BaP based on references [44,45]. Abbreviations: CYP—cytochrome P450; mEH—microsomal epoxide hydrolase; AKRs—aldo-keto reductases; NAD(P)H—quinone oxidoreductase.
The products of PAH metabolic activation, i.e., radical cations, diol-epoxides and o-quinones, may form adducts with DNA. This can lead to errors in DNA replication and disturbance of the promoter methylation process or promoter binding. DNA mutation or abnormal gene expression can, finally, lead to tumor formation [44].
PAHs metabolites may also form adducts with proteins in cells, which may influence their normal activity. In addition, reactive oxygen species generated by PAH metabolites can initiate carcinogenesis by modifying DNA, lipids and proteins [44].
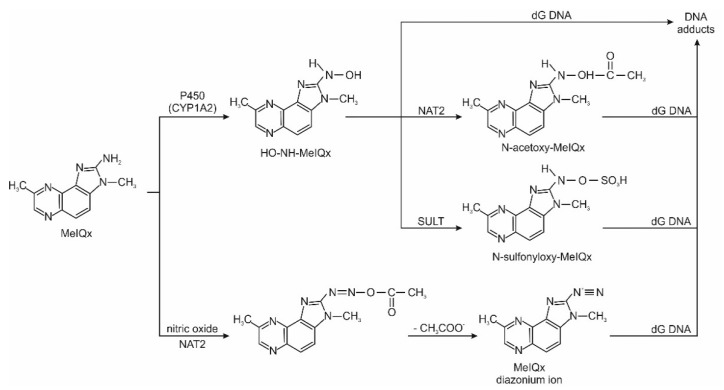
3.3.2. HAAs
Heterocyclic aromatic amines are metabolically activated by catalytic cytochrome P450. In the first phase of activation, the exocyclic amino group of this compound is N hydroxylated into hydroxylamine (-NHOH). Then, with the participation of enzymes from the group of N-acetyltransferases and sulfotransferases, highly active metabolites (esters and sulphates) are formed, which combine with deoxyguanosine (dG) of DNA molecules or with protein molecules to form stable adducts. Adducts can cause errors in DNA replication, which can lead to mutations and, subsequently, to cancer development. Figure 3 shows the scheme of metabolic activation of the polar heterocyclic amine MeIQx. Simultaneously with microsomal activation, metabolic detoxification takes place in the liver. It consists of the oxidation to hydroxyl derivatives with the participation of cytochrome P450 isoenzymes. Next, as result of the enzyme-catalyzed reaction, sulphate and glucuronide esters are formed. Direct N-glucuronidation of the exocyclic amino group of HAAs is also possible. Polar metabolites resulting from detoxification can be excreted from the body via the urinary system.
Figure 3.
HAA metabolism pathway of MeIQx based on references [46,47]. Abbreviations: NAT2—N-acetyltransferases; SULT—sulfotransferases; dG—deoxyguanosine.
3.4. Risk of Cancer
A high consumption of meat products is associated with an increased risk of cancer. The increased risk may be due to the high content of fat, protein or the formation of carcinogenic compounds, including heterocyclic aromatic amines and polycyclic aromatic hydrocarbons when processing meat at high temperatures [48]. In addition, heme iron, which is found in large quantities in red meat, may be involved in the endogenous formation of N-nitroso compounds from nitrates (III) [3,48]. These compounds can modify DNA synthesis, increase cell proliferation, affect hormone metabolism, increase insulin-like growth factors and contribute to the formation of free radicals, which leads to the development of cancer. [49].
3.4.1. Head and Neck Cancer
Head and neck cancers (HNC) include, among others, oral cavity (OCC), oropharyngeal (OHPC) and laryngeal (LC) cancers. About 90% are squamous cell carcinomas. While the effects of tobacco, alcohol or papillomavirus on the increased risk of head and neck cancer are well-understood, the role of diet in HNC etiology is less clear. In a Dutch cohort study, the consumption of processed meat was positively associated with overall HNC and the HNC subtype OCC but not with OHPC and LC [50]. The study by Xu et al. found that eating processed meat contributed to the formation of mouth and oropharyngeal cancer, but no association was found between red meat and oropharyngeal cancer [51]. Li et al. confirmed data suggesting that the high consumption of red or processed meat is associated with an increased risk of nasopharyngeal carcinoma (NPC) [52].
3.4.2. Gastrointestinal Cancer
Environmental factors, especially diet, play the most important role in the development of gastrointestinal neoplasms. Diet is estimated to contribute to 80% of colorectal cancer cases [53]. Liver is the major organ in the metabolism of PAHs. However, extrahepatic organs such as the gastrointestinal tract, spleen, lungs, heart, etc. may play a greater role. The underlying cause of gastrointestinal cancers is the information that human esophageal, duodenal and colon cells can metabolize PAHs and that microsomes from human gastric mucosa metabolize BaP [53]. Enzymes such as CYP1A1, CYP1A2, CYP1B1, glutathione S-transferase, UDP-glucuronosyl transferase and quinone oxidoreductase convert toxins into reactive metabolites that interact with cellular macromolecules, contributing to carcinogenesis [53].
Esophageal Cancer
Esophageal cancer (EC) is considered to be one of the most common types of cancer worldwide. It has been suggested that a high dietary protein intake increases the risk of EC [54]. Based on advanced case–control studies, Rostao et al. observed an increased risk of esophageal (squamous cell) cancer in people who have consumed large amounts of processed meat [55]. The above reports were confirmed by the meta-analysis by Choi et al., which showed an increase in the risk of esophageal cancer by 30% [56]. This association was stronger in esophageal adenocarcinoma than in squamous cell carcinoma [56]. Salehi et al. said that esophageal cancer is associated with the consumption of total red meat and processed meat but not with higher poultry consumption [57]. The study by Pournaghi et al. showed an association between the consumption of red meat, processed meat, poultry and the risk of EC. There was a positive relationship between the frequency of consuming red meat, processed meats (sausages), chicken with skin and the risk of EC; the use of lamb and fish showed no relationship [58]. In the study by Cross et al., high concentrations of two HAAs, MeIQx and PhIP, in meat consumed were associated with an increased risk of esophageal adenocarcinoma [59]. For esophageal neoplasms, the dose–response relationship between PAH concentration and EC risk is also important, suggesting a causal role of PAH exposure in the pathogenesis of EC [60].
Pancreatic Cancer
The relationship between the consumption of red and processed meat and the risk of pancreatic cancer is inconclusive. Malfatti et al. reported that mutagenic HAAs modify DNA molecules in pancreatic cells, indicating that heat-treated meat may be a risk factor for pancreatic cancer [61]. The study by Zhao et al. presented a case–control study that associated the consumption of red and processed meat with an increased risk of pancreatic cancer. Such a relationship was observed more often in men than in women [62]. Beaney et al. showed that the risk of pancreatic cancer, depending on the amount of meat consumed and the methods of its preparation, increases with age and concerns mainly people aged over 60 years [63].
Gastric Cancer
Gastric cancer is another cancer whose development is influenced by the PAHs and HAAs contained in food. The study by Cross et al. found a positive relationship between the consumption of 2-amino-3,4,8-trimethylimidazo[4,5-f]quinoxaline (DiMeIQx) and gastric carcinoma. Those with the highest consumption of DiMeIQx had an increased risk of gastric cardiac cancer, and benzo(a)pyrene showed no association [59]. The increased risk depends on the consumption of smoked, grilled and processed meat [64]. Additionally, the Western style of nutrition, which is dominated by a large amount of meat, increased the risk of gastric adenocarcinoma [65]. The association of an increased risk of gastric adenocarcinoma with high meat consumption was not demonstrated only in a study of the Netherlands population [66]. In addition, a meta-analysis by Zhao et al. suggested that there was no association between the consumption of red and processed meat and the risk of stomach cancer in cohort studies, although case–control studies have shown a positive correlation [67]. In conclusion, further well-designed prospective studies are needed to confirm the results of the influence of meat carcinogens on gastric cancer formation.
Colorectal Cancer
The incidence of colorectal cancer (CRC) depends on lifestyle, environmental factors, genetics and diet [2]. Exposure to food-derived HAAs and PAHs is considered to be an important factor in the development of CRC. Studies by Helmus et al. have confirmed that HAAs (mainly MeIQx and DiMeIQx) and PAHs found in red meat dishes are important factors initiating colon cancer carcinogenesis [68]. In the study by Cross et al., both red and processed meat consumption correlated positively with the development of colorectal cancer. These dependencies may result not only from exposure to HAAs (MeIQx and DiMeIQx), which is raised in meat prepared at high temperatures, but also from exposure to heme iron and nitrates contained in meat [69]. Steck et al. found positive links between the consumption of thermally processed meat and its HAAs compounds and colon cancer [70]. In addition, they investigated how a specific genotype modifies the association between meat consumption and meat-derived carcinogens and colon cancer [70]. Different genotypes show different expressions of the arising HAA–DNA adducts. The occurrence of the so-called “at-risk” alleles, which are predisposed toward the occurrence of CRC, is associated with a high consumption of red meat, well-done red meat, pan-fried red meat and meat carcinogens MeIQx and DiMeIQx [70].
The risk of diet-related cancer is also gender-modified. In the study by Vulcan et al., a tendency towards an increased risk of CRC with a higher total consumption of processed meat among men was observed. High beef consumption was associated with an increased risk of rectal cancer in men. Additionally, high pork consumption was associated with an increased risk of colon cancer in women [71]. In another work, a high beef and lamb consumption was associated with colon cancer risk but not with rectal cancer [72].
The authors of this study found one case–control study that did not support the hypothesis that the risk of colorectal cancer increases with the increasing consumption of red meat [73]. Multiple results, depending on the type of meat, sex and tumor location, show the complexity of colorectal cancer.
3.4.3. Prostate Cancer
There is growing evidence that eating habits influence the incidence of prostate cancer. Heterocyclic amines are positively associated with the risk of prostate cancer in animal models [74]. However, the results are inconsistent in epidemiological studies. In the study by Sander et al., there was no association found between HAA consumption and advanced prostate cancer or between the high consumption of well-done meat and prostate cancer. Men showing the highest intake of PhIP, MeIQx and DiMeIQx did not have an increased risk of prostate cancer compared to men with the lowest intake [75]. On the other hand, in the study by John et al., an increased risk of prostate cancer was associated with the frequent consumption of grilled or well-done red meat. There was no increased risk of advanced prostate cancer with animal fat consumption, suggesting that the association between diets full of red meat and prostate cancer is not related to the fat content. It has been shown that the cooking method and the degree of roasting of the meat, affecting the concentration of carcinogenic HAAs and PAHs, determine the risk of prostate cancer [48]. Changes occur in the prostate gland that can induce DNA damage. Nakai et al. found that the all lobes of prostates are target tissues of PhIP-induced mutations. PhIP contributes to carcinogenesis by causing mutation and inflammation by acting as both an initiator and promoter of the tumor [76]. In the study by Bogen et al., the consumption of grilled red meat was associated with higher levels of PhIP–DNA adducts in prostate tumor cells in men who had undergone radical prostatectomy, and the consumption of PhIP from cooked meat determined increased prostatic-specific antigen (PSA) levels [77].
A meta-analysis by Fabiani et al. and a case–control study conducted in Argentina in 2008–2013 confirmed that eating patterns called “Western” and “carbohydrate”, characterized by high loads of red meat, processed meat, eggs, sweets, bread, pasta and rice, were significantly associated with an increased risk of PC [78,79]. It should be noted that the occurrence of PC is related not only to diet and lifestyle but also to family history.
3.4.4. Lymphatic Cancer
There are many reports of an increased risk of lymphatic cancers related to a high consumption of processed high-protein products. Diet can influence the development of lymphoma by antigenic stimulation of the lymphoid tissue in the digestive tract by the actions of specific nutrients, resulting in changes in the immune system’s response [80].
Despite reports of increasing risk [81], the results regarding the association of a high consumption of red meat are not convincing about its involvement in non-Hodgkin’s lymphoma (NHL) risk, irrespective of the cooking method and degree of deep-frying that led to the formation of HAA and PAH [82]. The exception is a significant upward trend depending on the frequency of consumption of grilled or roasted chicken, the daily consumption of which was associated with an 80% increase in the risk of NHL [82]. Studies by Rohrmann et al. showed a positive association of chronic lymphocytic leukemia (CLL) with a high consumption of processed meat [83]. This was not confirmed by the study by Solans et al. [84].
3.4.5. Renal and Bladder Cancer
Renal cell carcinoma (RCC), the most common kidney cancer in adults, originates in the lining of the proximal ileal tubule, where glucose, amino acids, uric acid and inorganic salts are reabsorbed into the filtrate [85]. Despite the role of the kidneys in the metabolism and urinary excretion of various compounds, studies of meat-derived mutagens and kidney cancer in humans are rare and limited by a small number of cases [86]. Daniel et al. examined the consumption of meat and meat-related mutagens in relation to RCC in a case–control study of US men and women. Exposure to PAH found in grilled meat was associated with a higher risk of kidney cancer. The risk of RCC increased with the consumption of grilled meat and PAHs, including benzo(a)pyrene. The risk of RCC was more than twice as high with the increasing BaP consumption [85].
The frequent consumption of processed meat increases the risk of bladder cancer, as shown in the National Institutes of Health (NIH) and the American Association of Retired Persons (AARP) Diet and Health Study. The results suggest a positive association between the frequent consumption of red meat and as dietary exposure to PhIP and bladder carcinogenicity [87].
3.4.6. Breast Cancer
Dietary factors may increase the risk of breast cancer by modifying the levels of estrogens and other hormones (e.g., insulin-like growth factor). There is a hypothesis that the fats, iron and products of food processing (including HAAs) contained in meat modify the risk of breast cancer [88]. In the study by Genkinger et al., the statistically significant association between breast cancer and the consumption of red meat, processed meat, white meat or fish was not observed [88]. However, other research suggests that different types of breast cancers may have different etiologies. The frequent consumption of fried meat may increase the risk of, for example, ER +/PR- breast cancer [89]. Additionally, in Nurses’ Health Study II, a higher consumption of red meat was associated with almost twice the risk of ER +/PR + breast cancer [90]. However, no association was observed with culinary practices, exposure to heterocyclic amines or heme iron from red meat consumption with a risk of breast cancer in the studies by Lo et al. [91], contrary to the reports of Anderson et al., who found that the consumption of processed meat may increase the overall breast cancer risk [92].
4. Reducing the Risk of Cancer by Supplementing the Diet with Plant Products
Diet is the major source of PAHs and HAAs for the nonsmoking population, contributing to over 90% of the total exposure to these chemical compounds [8,12]. According to the guidelines of the National Food Agency in Sweden, the consumption of red meat should not exceed 500 g per week [93]. Above this value, an increased cancer risk from red meat is observed [71].
Meat and meat products, despite their proven carcinogenic potential, have high nutritional value. In addition to the main ingredients (i.e., amino acids; proteins with high biological value and minerals such as iron, zinc, selenium, manganese, vitamin B12 and other B vitamins), meat is rich in bioactive ingredients such as taurine, L-carnitine, choline, alpha-lipoic acid, linoleic acid, glutathione, creatine, coenzyme Q10 and bioactive peptides [94]. A person using a normal diet is not able to completely avoid exposure to muta- and carcinogenic compounds formed during the thermal processing of food. Although the concentrations of heterocyclic aromatic amines and polycyclic aromatic hydrocarbons in meat dishes are low, all treatments and processes leading to the reduction of their formation in food deserve attention. In order not to give up the nutritional properties of meat, it is worth modifying the methods of its thermal processing and, also, composing the diet in such a way as to limit the exposure of a human body to carcinogenic and mutagenic substances present in meat products. Recently, several extensive literature reviews have been published, the authors of which have made an attempt to systematize the knowledge of the formation of PAHs and HAAs in food and the possibility of limiting human exposure to muta- and carcinogenic compounds [5,12,95,96,97].
Many cancers can be prevented by meeting the dietary guidelines of cancer societies and recommendations for cancer prevention by optimizing the consumption and combination of certain foods. Numerous scientific reports indicate the chemopreventive (anticancer) effects of a diet rich in vegetables and fruits [49,64,65,85,98,99,100]. Such diets are associated with a reduced risk of chronic disease, inflammation and mortality [99]. The protective effect of a diet based on plant-based products may be due to their anti-inflammatory and antioxidant effects [101].
Plant-based foods are a rich source of antioxidants, phytoestrogens and flavonoids, especially flavanones, which can help prevent cancer growth through anti-inflammatory action, scavenging free radicals or blocking the formation of carcinogens [49]. Other ingredients in these products, including fiber, folate, vitamin C, vitamin A and beta-carotene, may also have anticancer effects [49]. Research confirms that a greater consumption of fruits and vegetables is associated with a significant reduction in the risk of a variety of malignancies, including cancers of the esophagus, lung, stomach and colon [49]. It has been proven that the strict adherence to Mediterranean dietary patterns allows one to prevent, e.g., gastric adenocarcinoma [65].
Maximova et al. showed that a low consumption of vegetables and fruits, with the simultaneous frequent consumption of highly processed meat products, leads to an increase in the incidence of cancer and a shorter time for the development of this disease [98].
The results of studies by Mouss et al. confirmed that the nutritional profile based on fruit and vegetables was inversely correlated with the risk of hepatocellular carcinoma (HCC) [99], esophageal cancer (EC) [49] and renal cell carcinoma (RCC) [85]. There was no such clear correlation between the consumption of whole grains and fiber and red meat in terms of cancer development [98], although a study by Anderson et al. demonstrated that a high-fiber intake protects against colon cancer (CRC) in people genetically susceptible to IL10-related CRC [102].
In addition, the results of studies by Yang et al. indicate that the reduction of the risk of CRC positively correlates with a diet with an increased content of fiber [103]. The results from The World Cancer Research Fund International project have shown that a consumption of 90 g/day of whole grain is associated with a reduced risk of colon cancer, mainly due to the fiber content in whole grains [104]. The authors should discuss the results and how they can be interpreted from the perspective of previous studies and of the working hypotheses. The findings and their implications should be discussed in the broadest context possible. Future research directions may also be highlighted.
5. Influence of Vegetable Additives on the Synthesis of Carcinogenic PAHs and HAAs in Thermally Processed Meat Dishes
Vegetable additives not only improve the taste of meat dishes but also, as the latest scientific research shows, can decrease the contents of some xenobiotics. These additives, usually rich in antioxidants, can modify the free radical mechanisms of HAA and PAH synthesis in food [29,30,41,105,106].
The results of the investigations on the influence of the natural additives and antioxidants contained in them on PAH formation in meat dishes are presented in Table 3. Some studies tried not only to evaluate the possibility of the reduction of the compounds formation in meat dishes but to also know the processes that take place under the influence of antioxidants. To achieve this, the phenolic profiles, total antioxidant status or radical scavenging activity were determined [97,107,108,109].
Table 3.
Influence of marinating and spices or natural plant additives on PAH concentrations in cooked meat. Concentration changes are presented as given in the publications, i.e., in % or ng/g.
| Additives | Sample Type and Heat Treatment Conditions | Influence on BaP Concentration | Influence on PAHs Concentration | Reference |
|---|---|---|---|---|
| Meat model system | ||||
| Epigallocatechin gallate (EGCG), (butylated hydroxyanisole (BHA), 3,5-di-tert-4-butylhydroxytoluene (BHT), α-tocopherol, sesamol (200 ng/g) |
Meat model system heated at 200 °C for 30 min (dry conditions) | Control 6.6 ng/g. Maximum decrease: to 4.1 ng/g (sesamol) |
PAH8 Control 22.3 ng/g. Decrease range: from 14.4 (EGCG) to 11.6 ng/g (sesamol) |
[22] |
| Marinades | ||||
| Three phenolic acid marinades with: protocatechuic acid (PA), gallic acid (GA) and ferulic acid (FA) (0.1–5 mg/mL) |
Charcoal-grilled chicken wings | Control 3.3 ng/g. Decrease range: 2.95 ng/g (0.1 mg/mL GA) to 2.1 ng/mL (3 mg/mL FA) |
PAH8 Control 12.83 ng/g. Decrease range: 12.3 (0.1 mg/mL FA) to 7.7 (3 mg/mL PA) |
[119] |
| Marinades with 8 phenolic compounds existing in green tea: (epigallocatechin gallate (EGCG), gallocatechin (GC), catechin (C), epicatechin gallate 107 (ECG), catechin gallate (CG), naringenin, and quinic acid (QA) |
Charcoal-grilled chicken wings | Control 1.5 ng/g. Reduction in the range from 20.5% (GC) to 71% (QA) |
PAH8 Control 2,5 ng/g. Reduction range from 15% (GC) to 54.5% (QA) |
[120] |
| Black beer, alcoholic and non-alcoholic pilsner beer marinades, | Charcoal-grilled pork | Control 2.7 ng/g. Decrease range: 2.2 ng/g (alcoholic beer) to 1.1 ng/g (black beer) |
PAH8 Control 20.7 ng/g. Decrease range: 17.8 ng/g (alcoholic beer) to 9.7 ng/g (black beer) |
[107] |
| Six brands of beer marinades and eleven phenolic compounds (e.g., gallic acid, hydroxycinnamic acids (ferulic acid), and flavonoids (catechin), Homovanillic acid (HVA) |
Charcoal-grilled chicken wings | Control 2.3 ng/g. Decrease to 0.5 ng/g (Heineken); Increase to 2.8 (Snow) All phenolic compounds decreased the BaP concentration. Maximum–HVA (67%) |
PAH8 Control 13.0 ng/g. Decrease to 4.3 (Heineken) Increase to 18.1 ng/g (Snow) All phenolic compounds decreased the PAH8 concentration. Maximum–HVA (48%) |
[109] |
| Tea marinade with green tea (GT) and yerba mate (YM) (1%) | Charcoal-grilled pork belly | Reduction: 24.5% (GT) and 31.5% (YM) |
- | [113] |
| Meat sprayed with vinegars: - white wine vinegar (WWV), - red wine vinegar (RWV), - apple cider vinegar (ACV), - elderberry vinegar (EV), - apple cider vinegar with raspberry juice (ACVR) |
Charcoal-grilled pork | Control 3.4 ng/g. Reduction in the range from 58.5 (ACVR) to 85.3% (WWV) |
PAH4 Control 31.5 ng/g. Reduction in the range from 55 (ACVR) to 82% (EV) |
[112] |
| Spices and natural plant additives | ||||
| Gochujang (Korean Red Pepper Paste) | Charcoal-Grilled Pork belly | Reduction by 32% | 16 PAH Reduction by (63.1%) |
[121] |
| Black pepper, garlic, ginger, onion, paprika (P), and red chilli (0.5%) | Fried beef and chicken meatballs | Reduction in the range from 44% (paprika in chicken) to 100% (ginger in beef) | 2 PAHs: BaA and BaP Reduction in the range from 47% (black pepper, beef) to 98% (ginger, beef) |
[111] |
| Garlic (0.05–0.15%, w/w); garlic essential oil (GEO) (0.002–0.006%, w/w) |
Charcoal-grilled pork sausages | Reduction: 37.2–62.3% (garlic); 29.1–57.1% (GEO) |
- | [108] |
| Garlic (15%); onion (30%) |
Pan fried pork (collars, chops) | Reduction: 55–71% (garlic); 44–74.5% (onion) |
6 PAHs (BaA, BaP, BbF, BghiP, BkF, DBahA) reduction 41–66% (garlic); 3.5–67% (onion) |
[100] |
An effective way to lower the PAH concentration in grilled dishes is to marinate the meat. Marinades containing lemon juice [110], as well as vitamins E and C [111], decreased the PAH levels by even 70% [110].
Marinating in beer significantly lowered the PAH contents in grilled meat, and the investigations showed that black beer had the highest inhibitory effect on the formation of PAH8 (53%) in charcoal-grilled pork, while pilsner alcoholic beer had the lowest (13%). The inhibitory effect of beer marinades on PAH increased with the increase of their radical scavenging activity [107,109] and the higher levels of the phenolic compounds [109].
A significant inhibitory effect of fruit/wine vinegars (sprayed on meat before grilling) on the formation of polycyclic aromatic hydrocarbons in charcoal-grilled pork was also shown. However, the mechanism of PAH reduction by vinegars is complex and probably depends on the phenolic profiles, pH and the interactions that can occur between meat and vinegar components [112].
The influence of green tea and yerba mate marinades on BaP formation in grilled and roasted meat was investigated [113,114]. Although benzo(a)pyrene was found in all samples, the tea marinades reduced the activity of the radicals and lipid oxidation [113,114].
It was proven that the addition of onion or garlic to pork meat being fried was able to decrease the PAH concentration [100]. Recent studies have shown that garlic and garlic essential oil added to charcoal-grilled pork sausages significantly decreased the BaP concentration [108], with inhibition being dependent on the number of sulfur (-S-) and thioallyl groups (–S–CH2–CH=CH2) in sulfide compounds. The mechanism of sulfides influencing BaP formation was related to the free radical reaction.
The addition of spices of high antioxidant capacity (i.e., paprika, ginger and black pepper) to thermally processed meat can decrease PAH and HAA contents, irrespective of the kind of meat [111]. It was also proven that the use of curcuma, lemon grass and curry leaves during meat roasting causes PAH and HAA concentrations to decrease [110,115,116].
Lately, a review of studies on the effects of cooking techniques and spiced marinades on the formation of PAHs, as well as heterocyclic amines in meats, has been published [97]. A meta-analysis of the results showed that the garlic and onion, pepper and other spices with phenolic compounds inhibited the formation of HAAs and PAHs due to the antioxidant and electron transfer mechanism.
The results of the studies on the effects of marinades, spices and additives often used for meat dish preparations on HAA synthesis are presented in Table 4. An effective way to lower the HAA concentrations in meat products is the use of natural additives containing flavonoids, vitamins C and E and catechin.
Table 4.
Influence of marinating and spices or natural plant additives on HAA concentrations in cooked meat. Concentration changes are presented as given in the publications, i.e., in % or ng/g.
| Additives | Sample Type and Heat Treatment Conditions | Reduction of HAAs Concentration | No Reduction or Increase of HAA Concentration | Reference |
|---|---|---|---|---|
| Marinades | ||||
| Marinade with 1% green tea extract | Pan-fried beef | PhIP reduction from 33.8 to 8.8 and AαC-from 14.7 ng/g to 2.2 |
4,8-DiMeIQx and MeIQx | [122] |
| Green (GT), oolong (OT) and white tea (WT) extracts (1%) |
Grilled chicken drumsticks | IQ, PhIP, AαC, Harman, norharman Reduction 23% (WT), 16–18% for GT and OT |
- | [114] |
| Beer (B) or red wine (RW) marinades | Pan-fried beef | PhIP–88% (B and RW); MeIQx–44% (B) and 33% (RW) AαC-7–77% (B, RW) |
- | [123] |
| Black beer (BB), alcoholic (AB) and nonalcoholic pilsner beer (NAB) marinades |
Charcoal-grilled pork | PhIP reduction from 6.1 ng/g to 1.6 (BB) Trp-P-1 from 5.9 ng/g to 0 ng/g (all marinades); AαC from 1.5 to 0.3 ng/g (BB); 4,8-DiMeIQx from 4.6 ng/g to 0 (BB) |
4,8-DiMeIQx, MeAαC (NAB) | [124] |
| Complex (purchased) marinades based on acerola, oregano and sumac, with many other ingredients |
Barbecued pork chops | Reduction by using each marinade: MeIQx from 1.11 to 0.73 ng/g; 4,8-DiMeIQx from 1.54 ng/g to 0.13 and PhIP from 11.35 to 0.13 ng/g |
Harman and norharman | [125] |
| Spices and natural plant additives | ||||
| Rosemary ethanolic extracts (0.05–0.5%) | Cooked beef patties | MeIQx (92%) and PhIP (85%) | - | [126] |
| Oregano (0.25% and 0.5%) |
Pan-fried ground beef patties | MeIQ (reduction 100%), MeIQx from 7.2 ng/g to 4.6 ng/g; PhIP from 2.3 ng/g to 1 ng/g |
- | [115] |
| Black cumin (1%) | Cooked meatballs (at 250 °C) |
MeIQx reduction from 1.53 ng/g to 0.86 ng/g; PhIP from 2.75 ng/g to 1.50 ng/g |
- | [127] |
| Basil (1%) | Cooked meatballs (at 250 °C) |
MeIQx reduction from 0.63 ng/g to 0.53 ng/g, MeIQ from 0.09 to 0.07 ng/g, 4,8-MeIQx, and PhIP–100% reduction |
- | [116] |
| Turmeric, curry leaf, torch ginger and lemon grass | Grilled beef | Total 9 HAAs (IQ, IQx, MeIQ, MeIQx, 7,8-DiMeIQx, PhIP, Harman, Norharman, AαC) reduction in the range from 21% (curry leaf) to 94.7% (turmeric and lemon grass) (50:50 w/w) |
- | [128] |
| Turmeric powder (0.5%) | Chicken meatballs | Total HAAs reduction by 72% | - | [129] |
| Black pepper (0.5; 1%, 1.5%) |
Fried tilapia fillets |
PhIP and MeIQx (reduction 100% by using 1% pepper) |
MeIQ and norharman |
[130] |
| Sichuan pepper (0.5%; 1%) |
Grilled ground beef patties | PhIP reduction (by using 0.5% pepper) 82%, IQx 61%, MeIQx 28% and 4,8-DiMeIQx 79% |
Harman and norharman | [131] |
| Black pepper, garlic, ginger, onion, paprika (P), and red chilli (0.5%) | Fried beef and chicken meatballs |
IQ, MeIQ,4,8-DiMeIQx, PhIP. Inhibitory efficiency of the 4 HAAs in the range from 43% (onion) to 87% (ginger). |
- | [111] |
| Chilli pepper (0.5%) | Roast beef patties |
PhIP reduction: 68%; Total 8HAAs reduction: 46% |
MeIQx, harman | [132] |
| Garlic (15%); onion (30%) | Pan fried pork (collars, chops) | IQ, MeIQ, MeIQx, 4,8-DiMeIQx, PhIP Total reduction in the range from 21 to 49.5% (onion) and 26–36 (garlic) |
[133] | |
| Beetroot juice (3%) | Meat-protein model system | PhIP reduction 60%, MeIQx 77% and IQ 87% |
- | [134] |
| Cherry tissue (11.5%) | Fried ground beef patties | PhIP reduction in the range from 87–93% | - | [135] |
| Dried apple peel extract (0.1, 0.15 and 0.3%) | Pan fried beef patties | MeIQx reduction 41- 68%; 4,8-DiMeIQx 21–56%; PhIP 60–83% |
- | [136] |
| Pomegranate seed extract (0.5%) |
Beef and chicken meatballs (oven roasted, pan cooked, charcoal-barbecued, deep-fat fried) | The highest reduction: PhIP 68–75%; norharman 24–57%; harman 18–28%; IQ 45–46%; MeIQx 49–57% |
Norharman and harman in beef oven roasted; IQ and MeIQx in chicken oven roasted and pan cooked |
[137] |
| Hawthorns extract (0.5, and 1%) |
Beef and chicken breast oven and pan-cooked | Total amount of 12 HAAs (Q, IQx, MeIQ, MeIQx, 4,8-DiMeIQx, 7,8-DiMeIQx, PhIP, harman, norharman, AαC, MeAαC, and Trp-P-2) reduced in the range of 12–100% | Harman | [138] |
| Apple skin and olive extracts, onion powder (1 and 3%) |
Ground beef patties-grilled | MeIQx 49–51% and PhIP 51–65% (olive and apple extracts); MeIQx and PhIP 47 and 80.7%, (onion powder) |
MeIQx (by using 1% onion) and PhIP (1% apple skin extract) | [139] |
A model study showed that the inhibitory effect of flavonoids depended mainly on their hydrophobicity, the position of the hydroxyl groups and topological structure. Catechin was the most effective inhibitor of HAA, followed by luteolin and genistein [105]. Other studies have shown that resveratrol was found to be the most efficient, as it totally inhibited MeIQ and reduced MeIQx and PhIP formation by 40 and 70%, respectively [115]. Antioxidants can inhibit various Maillard reaction pathways. They prevent the formation of HAAs through free radical quenching and scavenging. It was found that phenolic compounds are able to scavenge a wide range of reactive carbonyls formed during proteinaceous food thermal treating, even under common cooking conditions [29,105].
It is worth saying that not only meat additives have an effect on the concentration of carcinogenic substances in food product but also the way of preparation, i.e., methods of smoking (direct or indirect), the heat source, the smoke generation process (pyrolysis and air flow temperature), the distance between the food and the heat source and the fat content in a product [117]. Some alternative technologies may be applied, such as high-pressure treatment, cold plasma and ultrasounds [118]. Moreover, to limit HAA formation in food, long high-temperature thermal processes for food preparation should be avoided and, also, the dripping of fat during meat grilling.
6. Conclusions
As there is a growing tendency for the consumption of processed food accompanied by the aging of the population, which means a longer exposure of humans to PAHs and HAAs, it is extremely vital to find a simple way of how to limit carcinogenic compound synthesis in a processed proteinaceous food.
The investigations that were reviewed showed that simple cooking processes when some additives rich in phenolic compounds are added to the food are a natural and effective way for the inhibition of the harmful compound formations, including PAHs and HAAs, in thermally treated meat.
The studies confirmed that a higher intake of total meat, red or processed meats is associated with a higher risk of cancer. Nevertheless, cohort studies are necessary in order to have a clear perspective for the long-term effect of a regular intake of xenobiotics formed during food processing on cancer generation. The consumption of vegetables even as meat additives demonstrates a protective activity against cancer. A diet rich in natural products (fruits and vegetables) may have a positive influence on one’s health due to antioxidants and their detoxifying properties [140].
Author Contributions
Conceptualization: S.B. and B.J.; methodology: S.B.; resources: S.B. and B.J. writing—original draft preparation: S.B. and B.J.; writing—review and editing: S.B. and B.J.; visualization: S.B.; and supervision: B.J. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the research grant for Young Scientists, PCN-2-038/N/1/Z, from the Medical University of Silesia in Katowice, Poland.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Dybing E., O’Brien J., Renwick A., Sanner T. Risk assessment of dietary exposures to compounds that are genotoxic and carcinogenic—An overview. Toxicol. Lett. 2008;180:110–117. doi: 10.1016/j.toxlet.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 2.Chiavarini M., Bertarelli G., Minelli L. Dietary Intake of Meat Cooking-Related Mutagens (HCAs) and Risk of Colorectal Adenoma and Cancer: A Systematic Review and Meta-Analysis. Nutrients. 2017;18:514. doi: 10.3390/nu9050514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nogacka A., Gómez-Martín M., Suárez A., González-Bernardo O., Reyes-Gavilán C., Gonzalez S. Xenobiotics Formed during Food Processing: Their Relation with the Intestinal Microbiota and Colorectal Cancer. Int. J. Mol. Sci. 2019;25:2051. doi: 10.3390/ijms20082051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.International Agency for Research on Cancer (IARC) Red Meat and Processed Meat. IARC Publication; Lyon, France: 2018. Monographs on the Evaluation of Carcinogenic Risks to Humans; p. 114. [Google Scholar]
- 5.Sampaio G.R., Guizellini G.M., da Silva S.A., de Almeida A.P., Pinaffi-Langley A.C., Rogero M., de Camargo A.C., Torres E. Polycyclic Aromatic Hydrocarbons in Foods: Biological Effects, Legislation, Occurrence, Analytical Methods and Strategies to Reduce Their Formation. Int. J. Mol. Sci. 2021;22:6010. doi: 10.3390/ijms22116010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sharma R.K., Chan W.G., Hajaligol M.R. Product compositions from pyrolysis of some aliphatic α-amino acids. J. Anal. Appl. Pyrolysis. 2006;75:2. doi: 10.1016/j.jaap.2005.03.010. [DOI] [Google Scholar]
- 7.Sobral M., Cunha S., Faria M., Ferreira I. Domestic Cooking of Muscle Foods: Impact on Composition of Nutrients and Contaminants. Food Sci. Food Saf. 2018;17:309–333. doi: 10.1111/1541-4337.12327. [DOI] [PubMed] [Google Scholar]
- 8.European Food Safety Authority (EFSA) Scientific opinion of the Panel on Contaminants in the Food Chain on a request from the European Commission on polycyclic aromatic hydrocarbons in food. EFSA J. 2008;724:1–114. [Google Scholar]
- 9.Paris A., Ledauphin J., Poinot P., Gaillard J. Polycyclic aromatic hydrocarbons in fruits and vegetables: Origin, analysis, and occurrence. Environ. Pollut. 2018;234:96–106. doi: 10.1016/j.envpol.2017.11.028. [DOI] [PubMed] [Google Scholar]
- 10.Singh L., Varshney J., Agarwal T. Polycyclic aromatic hydrocarbons’ formation and occurrence in processed food. Food Chem. 2016;199:768–781. doi: 10.1016/j.foodchem.2015.12.074. [DOI] [PubMed] [Google Scholar]
- 11.Rose M., Holland J., Dowding A., Petch S., White S., Fernandes A., Mortimer D. Investigation into the formation of PAHs in foods prepared in the home to determine the effects of frying, grilling, barbecuing, toasting and roasting. Food Chem. Toxicol. 2015;78:1–9. doi: 10.1016/j.fct.2014.12.018. [DOI] [PubMed] [Google Scholar]
- 12.Zhang Y., Chen X., Zhang Y. Analytical chemistry, formation, mitigation, and risk assessment of polycyclic aromatic hydrocarbons: From food processing to in vivo metabolic transformation. Compr. Rev. Food Sci. Food Saf. 2021;20:1422–1456. doi: 10.1111/1541-4337.12705. [DOI] [PubMed] [Google Scholar]
- 13.Sahin S., Ulusoy H., Alemdar S., Erdogan S., Ximba S. Benzo[a]pyrene and benzo[k]fluoranthene in some processed fish and fish products. Int. J. Environ. Res. Public Health. 2015;12:940–951. doi: 10.3390/ijerph120100940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oliveira M., Capelas S., Delerue-Matos C., Morais S. Grill workers exposure to polycyclic aromatic hydrocarbons: Levels and excretion profiles of the urinary biomarkers. Int. J. Environ. Res. Public Health. 2021;18:230. doi: 10.3390/ijerph18010230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mastanjevic K., Puljic L., Kartalovic B., Grbavac J., Grbavac M., Nadaždi H., Habschied K. Analysis of polycyclic aromatic hydrocarbons in heregovacki pršut—Traditionally smoked prosciutto. Int. J. Environ. Res. 2020;15:5097. doi: 10.3390/ijerph17145097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bao Y., Zhu Y., Ren X., Zhang Y., Peng Z., Zhou G. Formation and inhibition of lipid alkyl radicals in roasted meat. Foods. 2020;9:572. doi: 10.3390/foods9050572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Britt P., Buchanan A., Owens C., Skeen T. Dose glucose enhance the formation of nitrogen containing polycyclic aromatic compounds and polycyclic aromatic hydrocarbons in the pyrolysis of proline? Fuel. 2004;83:1417–1432. doi: 10.1016/j.fuel.2004.02.009. [DOI] [Google Scholar]
- 18.Sharma R., Chen W., Seeman J., Hajaligol M. Formation of low molecular weight heterocycles and polycyclic aromatic compounds(PACs) in the pyrolysis of α-amino acids. J. Anal. Appl. Pyrolysis. 2003;66:97–121. doi: 10.1016/S0165-2370(02)00108-0. [DOI] [Google Scholar]
- 19.Sharma R., Chan W., Wang J., Waymack B., Wooten J., Seeman J., Hajaligol M. On the role of peptides in the pyrolysis of amino acids. J. Anal. Appl. Pyrolysis. 2004;72:153–163. doi: 10.1016/j.jaap.2004.03.009. [DOI] [Google Scholar]
- 20.Nie W., Cai K., Li Y., Zhang S., Wang Y., Guo J., Chen C., Xu B. Small molecular weight aldose (D-Glucose) and basic amino acids (L-Lysine, L-Arginine) increase the occurrence of PAHs in grilled pork sausages. Molecules. 2018;19:3377. doi: 10.3390/molecules23123377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen B.H., Chen Y.C. Formation of polycyclic aromatic hydrocarbons in the smoke from heated model lipids and food lipids. J. Agric. Food Chem. 2001;49:5238–5243. doi: 10.1021/jf0106906. [DOI] [PubMed] [Google Scholar]
- 22.Min S., Patra J.K., Shin H.S. Factors influencing inhibition of eight polycyclic aromatic hydrocarbons in heated meat model system. Food Chem. 2018;239:993–1000. doi: 10.1016/j.foodchem.2017.07.020. [DOI] [PubMed] [Google Scholar]
- 23.Nie W., Cai K., Li Y., Tu Z., Hu B., Zhou C., Chen C., Jiang S. Study of polycyclic aromatic hydrocarbons generated from fatty acids by a model system. J. Sci. Food Agric. 2019;99:3548–3554. doi: 10.1002/jsfa.9575. [DOI] [PubMed] [Google Scholar]
- 24.Britt P., Buchanan A., Kidder M., Owens C. Influence of steroid structure on the pyrolytic formation of polycyclic aromatic hydrocarbons. J. Anal. Appl. Pyrolysis. 2003;66:71–95. doi: 10.1016/S0165-2370(02)00106-7. [DOI] [Google Scholar]
- 25.European Commission European Commission Regulation (EC) No. 1881/2006 of 19 December 2006 setting maximum levels for certain contaminants in foodstuffs. Off. J. Eur. Union. 2006;L364:5–24. [Google Scholar]
- 26.European Commission European Commission Regulation (EU) No 835/2011 of 19 August 2011 amending Regulation (EC) No 1881/2006 as regards maximum levels for polycyclic aromatic hydrocarbons in foodstuffs. Off. J. Eur. Union. 2011;L215:4–8. [Google Scholar]
- 27.European Commission European Commission Regulation (EU) 2020/1255 of 7 September 2020 Amending Regulation (EC) No 1881/2006 as regards maximum levels of polycyclic aromatic hydrocarbons (PAHs) in traditionally smoked meat and smoked meat products and traditionally smoked fish and smoked fishery products and establishing a maximum level of PAHs in powders of food of plant origin used for the preparation of beverages. Off. J. Eur. Union. 2020;L293:1–4. [Google Scholar]
- 28.Gibis M. Heterocyclic aromatic amines in cooked meat products: Causes, formation, occurrence, and risk assessment. Compr. Rev. Food Sci. Food Saf. 2016;15:269–302. doi: 10.1111/1541-4337.12186. [DOI] [PubMed] [Google Scholar]
- 29.Zamora R., Hidalgo F.J. Formation of heterocyclic aromatic amines with the structure of aminoimidazoazarenes in food products. Food Chem. 2020;313:126–128. doi: 10.1016/j.foodchem.2019.126128. [DOI] [PubMed] [Google Scholar]
- 30.Nadeem H., Akhtar S., Ismail T., Sestili P., Lorenzo J., Ranjha M., Jooste L., Hano C., Aadil R. Heterocyclic aromatic amines in meat: Formation, isolation, risk assessment, and inhibitory effect of plant extracts. Foods. 2021;10:1466. doi: 10.3390/foods10071466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nagao M., Honda M., Seino Y., Yahagi T., Sugimura T. Mutagenicities of smoke condensates and the charred surface of fish and meat. Cancer Lett. 1977;2:221–226. doi: 10.1016/S0304-3835(77)80025-6. [DOI] [PubMed] [Google Scholar]
- 32.Sugimura T., Wakabayashi K., Nakagama H., Nagao M. Heterocyclic amines: Mutagens /carcinogens produced during cooking of meat and fish. Cancer Sci. 2004;95:290–299. doi: 10.1111/j.1349-7006.2004.tb03205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barzegar F., Kamankesh M., Mohammadi A. Heterocyclic aromatic amines in cooked food: A review on formation, health risk-toxicology and their analytical techniques. Food Chem. 2019;280:240–254. doi: 10.1016/j.foodchem.2018.12.058. [DOI] [PubMed] [Google Scholar]
- 34.Chen X., Jia W., Zhu L., Mao L., Zhang Y. Recent advances in heterocyclic aromatic amines: An update on food safety and hazardous control from food processing to dietary intake. Compr. Rev. Food Sci. Food Saf. 2020;19:124–148. doi: 10.1111/1541-4337.12511. [DOI] [PubMed] [Google Scholar]
- 35.Dong H., Xian Y., Li H., Bai W., Zeng X. Potential carcinogenic heterocyclic aromatic amines (HAAs) in foodstuffs: Formation, extraction, analytical methods, and mitigation strategies. Compr. Rev. Food Sci. Food Saf. 2020;19:365–404. doi: 10.1111/1541-4337.12527. [DOI] [PubMed] [Google Scholar]
- 36.Jägerstad M., Skog K., Arvidsson P., Solyakov A. Chemistry, formation and occurrence of genotoxic heterocyclic amines identified in model systems and cooked foods. Z. Lebensm. Unters. Forsch. 1998;207:419–427. doi: 10.1007/s002170050355. [DOI] [Google Scholar]
- 37.Polak M., Demšar L., Zahija I., Polak T. Influence of temperature on the formation of heterocyclic aromatic amines in pork steaks. Czech J. Food Sci. 2020;38:248–254. doi: 10.17221/144/2019-CJFS. [DOI] [Google Scholar]
- 38.Knize M., Dolbeare F., Carroll K., Moore D., Felton J. Effect of cooking time and temperature on the heterocyclic amine content of fried beef patties. Food Chem. Toxicol. 1994;32:595–603. doi: 10.1016/0278-6915(94)90002-7. [DOI] [PubMed] [Google Scholar]
- 39.Linghu Z., Karim K., Taghvaei M., Albashabsheh Z., Houser T., Smith S. Amino acids effects on heterocyclic amines formation and physicochemical properties in pan-fried beef patties. J. Food Sci. 2020;85:1361–1370. doi: 10.1111/1750-3841.15078. [DOI] [PubMed] [Google Scholar]
- 40.Szterk A., Waszkiewicz-Robak B. Influence of selected quality factors of beef on the profile and the quantity of heterocyclic aromatic amines during processing at high temperature. Meat Sci. 2014;96:1177–1184. doi: 10.1016/j.meatsci.2013.11.019. [DOI] [PubMed] [Google Scholar]
- 41.Meurillon M., Engel E. Mitigation strategies to reduce the impact of heterocyclic aromatic amines in proteinaceous foods. Trends Food Sci. Technol. 2016;50:70–84. doi: 10.1016/j.tifs.2016.01.007. [DOI] [Google Scholar]
- 42.International Agency for Research on Cancer . Monographs on the Evaluation of Carcinogenic Risks to Humans. IARC Publications; Lyon, France: 1993. Some naturally occurring substances: Food items and constituents, heterocyclic aromatic amines and mycotoxins; p. 56. [Google Scholar]
- 43.Mielżyńska-Švach D., Błaszczyk E. Polycyclic aromatic hydrocarbons and PAH-related DNA adducts. J. Appl. Genet. 2017;58:321–330. doi: 10.1007/s13353-016-0380-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Moorthy B., Chu C., Carli D. Polycyclic aromatic hydrocarbons: From metabolism to lung cancer. Toxicol. Sci. 2015;145:5–15. doi: 10.1093/toxsci/kfv040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Barnes J., Zubair M., John K., Poirier M., Martin F. Carcinogens and DNA damage. Biochem. Soc. Trans. 2018;46:1213–1224. doi: 10.1042/BST20180519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Alaejos M.S., Afonso A.M. Factors that affect the content of heterocyclic aromatic amines in foods. Compr. Rev. Food Sci. Food Saf. 2011;10:52–108. doi: 10.1111/j.1541-4337.2010.00141.x. [DOI] [Google Scholar]
- 47.Gu D., McNaughton L., LeMaster D., Lake B., Googerham N., Kadlubar F., Turesky R. A comprehensive approach to the profiling of the cooked meat carcinogens 2-amino-3,8-dimethylimidazol[4,5-f]quinoxaline, 2-amino-1-methyl-6-phenylimidazo-[4,5-b]pyridine and their metabolites in human urine. Chem. Res. Toxicol. 2010;23:788–801. doi: 10.1021/tx900436m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.John E., Stern M., Sinha R., Koo J. Meat consumption, cooking practices, meat mutagens and risk of prostate cancer. Nutr. Cancer. 2011;63:525–537. doi: 10.1080/01635581.2011.539311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Salamat F., Semnani S., Honarvar M., Fazel A., Roshandel G. 10-Year trends in dietary intakes in the high- and low-risk areas for esophageal cancer: A population-based ecological study in Northern Iran. Middle East J. Dig. Dis. 2020;12:89–98. doi: 10.34172/mejdd.2020.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Perloy A., Maasland D., van den Brandt P., Kremer B., Schouten L. Intake of meat and fish and risk of head–neck cancer subtypes in the Netherlands Cohort Study. Cancer Caus. Control. 2017;28:647–656. doi: 10.1007/s10552-017-0892-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Xu J., Yang X., Wu Y., Li X., Bai B. Meat consumption and risk of oral cavity and oropharynx cancer: A meta-analysis of observational studies. PLoS ONE. 2014;9:e95048. doi: 10.1371/journal.pone.0095048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Li F., Duan F., Zhao X., Song C., Cui S., Dai L. Red meat and processed meat consumption and nasopharyngeal carcinoma risk: A dose-response meta-analysis of observational studies. Nutr. Cancer. 2016;68:1034–1043. doi: 10.1080/01635581.2016.1192200. [DOI] [PubMed] [Google Scholar]
- 53.Diggs D., Huderson A., Harris K., Myers J., Banks L., Rekhadevi P., Niaz M., Ramesh A. Polycyclic aromatic hydrocarbons and digestive tract cancers: A perspective. J. Environ. Sci. Health C Environ. Carcinog. Ecotoxicol. Rev. 2011;29:324–357. doi: 10.1080/10590501.2011.629974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Torre L., Bray F., Siegel R., Ferlay J., Lortet-Tieulent J., Jemal A. Global cancer statistics, 2012. CA Cancer J. Clin. 2015;65:87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 55.Rosato V., Kawakita D., Negri E., Serraino D., Garavello W., Montella M., Decarli A., La Vecchia C., Ferraroni M. Processed meat and risk of selected digestive tract and laryngeal cancers. Eur. J. Clin. Nutr. 2019;73:141–149. doi: 10.1038/s41430-018-0153-7. [DOI] [PubMed] [Google Scholar]
- 56.Choi Y., Song S., Song Y., Lee J.E. Consumption of red and processed meat and esophageal cancer risk: Meta-analysis. World J. Gastroenterol. 2013;19:1020–1029. doi: 10.3748/wjg.v19.i7.1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Salehi M., Moradi-Lakeh M., Salehi M.H., Nojomi M., Kolahdooz F. Meat, fish, and esophageal cancer risk: A systematic review and dose-response meta-analysis. Nutr. Rev. 2013;71:257–267. doi: 10.1111/nure.12028. [DOI] [PubMed] [Google Scholar]
- 58.Pournaghi S., Noveyri F., Doust H., Ahmadi A., Hamedi H., Rahimi J., Ghasemi M., Hamidi H., Gholamalizadeh M., Doaei S., et al. The association of consumption of animal proteins and the risk of esophageal cancer. Nutr. Cancer. 2019;71:1094–1099. doi: 10.1080/01635581.2019.1597903. [DOI] [PubMed] [Google Scholar]
- 59.Cross A., Freedman N., Ren J., Ward M., Hollenbeck A., Schatzkin A., Sinha R., Abnet C. Meat consumption and risk of esophageal and gastric cancer in a large prospective study. Am. J. Gastroenterol. 2011;106:432–442. doi: 10.1038/ajg.2010.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Abedi-Ardekani B., Kamangar F., Hewitt S., Hainaut P., Sotoudeh M., Abnet C., Taylor P., Boffetta P., Malekzadeh R., Dawsey S. Polycyclic aromatic hydrocarbon exposure in oesophageal tissue and risk of oesophageal squamous cell carcinoma in north-eastern Iran. Gut. 2010;59:1178–1183. doi: 10.1136/gut.2010.210609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Malfatti M., Kuhn E., Turteltaub K., Vickers S., Jensen E., Strayer L., Anderson K. Disposition of the dietary mutagen 2-Amino-3,8-dimethylimidazo[4,5-f]quinoxaline in healthy and pancreatic cancer compromised humans. Chem. Res. Toxicol. 2016;21:352–358. doi: 10.1021/acs.chemrestox.5b00495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zhao Z., Yin Z., Pu Z., Zhao Q. Association between consumption of red and processed meat and pancreatic cancer risk: A systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. 2017;15:486–493.e10. doi: 10.1016/j.cgh.2016.09.143. [DOI] [PubMed] [Google Scholar]
- 63.Beaney A., Banim P., Luben R., Lentjes M., Khaw K., Hart A. Higher meat intake is positively associated with higher risk of developing pancreatic cancer in an age-dependent manner and are modified by plasma antioxidants: A prospective cohort study (EPIC-Norfolk) using data from food diaries. Pancreas. 2017;46:672–678. doi: 10.1097/MPA.0000000000000819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lazarevic I., Nagorni A., Rancic N., Milutinovic S., Stosic L. Dietary factors and gastric cancer risk: Hospital-based case control study. J. BU ON. Off. J. Balk. Union Oncol. 2010;15:89–93. [PubMed] [Google Scholar]
- 65.Castelló A., Fernández de Larrea N., Martín V., Dávila-Batista V., Boldo E., Guevara M., Moreno V., Castaño-Vinyals G., Gómez-Acebo I., Fernández-Tardón G., et al. High adherence to the western, prudent, and mediterranean dietary patterns and risk of gastric adenocarcinoma: MCC-Spain study. Gastric Cancer. 2018;21:372–382. doi: 10.1007/s10120-017-0774-x. [DOI] [PubMed] [Google Scholar]
- 66.Keszei A., Schouten L., Goldbohm R., Beandt P. Red and processed meat consumption and the risk of esophageal and gastric cancer subtypes in the Netherlands cohort study. Ann. Oncol. 2012;23:2319–2326. doi: 10.1093/annonc/mdr615. [DOI] [PubMed] [Google Scholar]
- 67.Zhao Z., Zifang Y., Qingchuan Z. Red and processed meat consumption and gastric cancer risk: A systematic review and meta-analysis. Oncotarget. 2017;8:30563–30575. doi: 10.18632/oncotarget.15699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Drew L., Helmus S., Thompson C., Zelenskiy S., Tucker T. Red meat-derived heterocyclic amines increase risk of colon cancer: A population-based case-control study. Nutr. Cancer. 2013;65:1141–1150. doi: 10.1080/01635581.2013.834945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cross A., Ferrucci L., Risch A., Graubard B., Ward M., Park Y., Hollenbeck A., Schatzkin A. A large prospective study of meat consumption and colorectal cancer risk: An investigation of potential mechanisms underlying this association. Cancer Res. 2010;70:2406–2414. doi: 10.1158/0008-5472.CAN-09-3929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Steck S., Butler L., Keku T., Antwi S., Galanko J., Sandler R. Nucleotide excision repair gene polymorphisms, meat intake and colon cancer risk. Mutat. Res. 2014;762:24–31. doi: 10.1016/j.mrfmmm.2014.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Vulcan A., Manjer J., Ericson U., Ohlsson B. Intake of different types of red meat, poultry, and fish and incident colorectal cancer in women and men: Results from the Malmö Diet and cancer study. Food Nutr. Res. 2017;61:1341810. doi: 10.1080/16546628.2017.1341810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Carr P., Walter V., Brenner H., Hoffmeister M. Meat subtypes and their association with colorectal cancer: Systematic review and meta-analysis. Int. J. Cancer. 2015;138:293–302. doi: 10.1002/ijc.29423. [DOI] [PubMed] [Google Scholar]
- 73.Tabatabaei J., Fritschi L., Knuiman M., Boyle T., Iacopetta B., Platell C. Meat consumption and cooking practices and the risk of colorectal cancer. Eur. J. Clin. Nutr. 2011;65:668–675. doi: 10.1038/ejcn.2011.17. [DOI] [PubMed] [Google Scholar]
- 74.Bellamri M., Walmsley S., Turesky R. Metabolism and biomarkers of heterocyclic aromatic amines in humans. Genes Environ. 2021;43:29. doi: 10.1186/s41021-021-00200-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sander A., Linseisen J., Rohrmann S. Intake of heterocyclic aromatic amines and the risk of prostate cancer in the EPIC-Heidelberg cohort. Cancer Caus. Control. 2011;22:109–114. doi: 10.1007/s10552-010-9680-9. [DOI] [PubMed] [Google Scholar]
- 76.Nakai Y., Nelson W., de Marzo A. The dietary charred meat carcinogen 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine acts as both a tumor initiator and promoter in the rat ventral prostate. Cancer Res. 2007;67:1378–1384. doi: 10.1158/0008-5472.CAN-06-1336. [DOI] [PubMed] [Google Scholar]
- 77.Bogen K., Keating G., Chan J., Paine L., Simms E., Nelson D., Holly E. Highly elevated PSA and dietary PhIP intake in a prospective clinic-based study among African Americans. Prostate Cancer Prostatic Dis. 2007;10:261–269. doi: 10.1038/sj.pcan.4500941. [DOI] [PubMed] [Google Scholar]
- 78.Fabiani R., Minelli L., Bertarelli G., Bacci S. A western dietary pattern increases prostate cancer risk: A systematic review and Meta-Analysis. Nutrients. 2016;8:626. doi: 10.3390/nu8100626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Niclis C., Román M., Osella A., Eynard A., Díaz M. Traditional dietary pattern increases risk of prostate cancer in argentina: Results of a multilevel modeling and bias analysis from a case-control study. J. Cancer Epidemiol. 2015;2015:179562. doi: 10.1155/2015/179562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Shivappa N., Hébert J., Taborelli M., Montella M., Libra M., Zucchetto A., Crispo A., Grimaldi M., La Vecchia C., Serraino D., et al. Dietary inflammatory index and non-hodgkin lymphoma risk in an Italian case-control study. Cancer Caus. Control. 2017;28:791–799. doi: 10.1007/s10552-017-0905-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ollberding N., Aschebrook-Kilfoy B., Caces D., Smith S., Weisenburger D., Chiu B. Dietary patterns and the risk of non-hodgkin lymphoma. Public Health Nutr. 2014;17:1531–1537. doi: 10.1017/S1368980013001249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Campagna M., Cocco P., Zucca M., Angelucci E., Gabbas A., Latte G., Uras A., Rais M., Sanna S., Ennas G. Risk of lymphoma subtypes and dietary habits in a mediterranean area. Cancer Epidemiol. 2015;39:1093–1098. doi: 10.1016/j.canep.2015.09.001. [DOI] [PubMed] [Google Scholar]
- 83.Rohrmann S., Linseisen J., Jakobsen M., Overvad K., Raaschou-Nielsen O., Tjonneland A., Boutron-Ruault M., Kaaks R., Becker N., Bergmann M., et al. Consumption of meat and dairy and lymphoma risk in the european prospective investigation into cancer and nutrition. Int. J. Cancer. 2011;128:623–634. doi: 10.1002/ijc.25387. [DOI] [PubMed] [Google Scholar]
- 84.Solans M., Castelló A., Benavente Y., Marcos-Gragera R., Amiano P., Gracia-Lavedan E., Costas L., Robles C., Gonzalez-Barca E., de la Banda E., et al. Adherence to the western, prudent, and mediterranean dietary patterns and chronic lymphocytic leukemia in the MCC-Spain study. Haematologica. 2018;103:1881–1888. doi: 10.3324/haematol.2018.192526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Daniel C., Schwartz K., Colt J., Dong L., Ruterbusch J., Purdue M., Cross A., Rothman N., Davis F., Wacholder S., et al. Meat-cooking mutagens and risk of renal cell carcinoma. Br. J. Cancer. 2011;105:1096–1104. doi: 10.1038/bjc.2011.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Chow W., Dong L., Devesa S. Epidemiology and risk factors for kidney cancer. Nat. Rev Urol. 2010;7:245–257. doi: 10.1038/nrurol.2010.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ferrucci L., Sinha R., Ward M., Graubard B., Hollenbeck A., Kilfoy B., Schatzkin A., Michaud D., Cross A. Meat and components of meat and the risk of bladder cancer in the NIH-AARP diet and health study. Cancer. 2010;116:4345–4353. doi: 10.1002/cncr.25463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Genkinger J., Makambi K., Palmer J., Rosenberg L., Adams-Campbell L. Consumption of dairy and meat in relation to breast cancer risk in the black women’s health study. Cancer Caus. Control. 2013;24:675–684. doi: 10.1007/s10552-013-0146-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Larsson S., Bergkvist L., Wolk A. Long-term meat intake and risk of breast cancer by oestrogen and progesterone receptor status in a cohort of Swedish women. Eur. J. Cancer. 2009;45:3042–3046. doi: 10.1016/j.ejca.2009.04.035. [DOI] [PubMed] [Google Scholar]
- 90.Cho E., Chen W., Hunter D., Stampfer M., Colditz G., Hankinson S., Willett W. Red meat intake and risk of breast cancer among premenopausal women. Arch. Intern. Med. 2006;166:2253–2259. doi: 10.1001/archinte.166.20.2253. [DOI] [PubMed] [Google Scholar]
- 91.Lo J., Park Y.M., Sinha R., Sandler D. Association between meat consumption and risk of breast cancer: Findings from the sister study. Int. J. Cancer. 2020;146:2156–2165. doi: 10.1002/ijc.32547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Anderson J., Darwis N., Mackay D., Celis-Morales C., Lyall D., Sattar N., Gill J., Pell J. Red and processed meat consumption and breast cancer: UK Biobank cohort study and meta-analysis. Eur. J. Cancer. 2018;90:73–82. doi: 10.1016/j.ejca.2017.11.022. [DOI] [PubMed] [Google Scholar]
- 93.Bjerselius R., Konde Å.B., Färnstrand J.S. Konsumtion av Rött Kött och Charkuteriprodukter och Samband Med Tjock- Och Ändtarmscancer av-Risk-och Nyttohanteringsrapport. Livsmedelsverket; Uppsala, Sweden: 2014. [Google Scholar]
- 94.Kulczyński B., Sidor A., Gramza-Michałowska A. Characteristics of selected antioxidative and bioactive compounds in meat and animal origin products. Antioxidants. 2019;22:335. doi: 10.3390/antiox8090335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Singh L., Agarwal T., Simal-Gandara J. PAHs, diet and cancer prevention: Cooking process driven-strategies. Trends Food Sci. Tech. 2020;99:487–506. doi: 10.1016/j.tifs.2020.03.030. [DOI] [Google Scholar]
- 96.Duedahl-Olesen L., Ionas A. Formation and mitigation of PAHs in barbecued meat–a review. Crit. Rev. Food Sci. Nutr. 2021;7:1–16. doi: 10.1080/10408398.2020.1867056. [DOI] [PubMed] [Google Scholar]
- 97.Neves T., Cunha D., Rosso V., Domene S. Effects of seasoning on the formation of heterocyclic amines and polycyclic aromatic hydrocarbons in meats: A meta-analysis. Compr. Rev. Food Sci. Food Saf. 2021;20:526–541. doi: 10.1111/1541-4337.12650. [DOI] [PubMed] [Google Scholar]
- 98.Maximova K., Moez E., Dabravolskaj J., Ferdinands A., Dinu I., Lo Siou G., Rajabi A., Veugelers P. Co-consumption of vegetables and fruit, whole grains, and fiber reduces the cancer risk of red and processed meat in a large prospective cohort of adults from Alberta’s Tomorrow Project. Nutrients. 2020;12:2265. doi: 10.3390/nu12082265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Moussa I., Day R., Li R., Du X., Kaseb A., Jalal P., Daniel-MacDougall C., Hatia R., Abdelhakeem A., Rashid A., et al. Dietary patterns and hepatocellular carcinoma risk among US adults. Nutrients. 2021;13:2011. doi: 10.3390/nu13062011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Janoszka B. HPLC-fluorescence analysis of polycyclic aromatic hydrocarbons (PAHs) in pork meat and its gravy fried without additives and in the presence of onion and garlic. Food Chem. 2011;126:1344–1353. doi: 10.1016/j.foodchem.2010.11.097. [DOI] [Google Scholar]
- 101.Silveira B., Oliveira T., Andrade P., Hermsdorff H., Rosa C., Franceschini S. Dietary pattern and macronutrients profile on the variation of inflammatory biomarkers: Scientific update. Cardiol. Res. Pract. 2018;2018:4762575. doi: 10.1155/2018/4762575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Andersen V., Egeberg R., Tjønneland A. Interaction between interleukin-10 (IL-10) polymorphisms and dietary fibre in relation to risk of colorectal cancer in a Danish case-cohort study. BMC Cancer. 2012;17:12183. doi: 10.1186/1471-2407-12-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Yang J., Yu J. The association of diet, gut microbiota and colorectal cancer: What we eat may imply what we get. Protein Cell. 2018;9:474–487. doi: 10.1007/s13238-018-0543-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Vieira A., Abar L., Chan D., Vingeliene S., Polemiti E., Stevens C., Greenwood D., Norat T. Foods and beverages and colorectal cancer risk: A systematic review and meta-analysis of cohort studies, an update of the evidence of the WCRF-AICR Continuous Update Project. Ann. Oncol. 2017;28:1788–1802. doi: 10.1093/annonc/mdx171. [DOI] [PubMed] [Google Scholar]
- 105.Zhao L., Pan F., Li Y., Hao S., Mehmood A., Wang Y., Wang C. Structure characteristics of flavonoids for heterocyclic aromatic amines inhibition using quantitative structure–activity relationship modeling. J. Food Biochem. 2020;44:e13390. doi: 10.1111/jfbc.13390. [DOI] [PubMed] [Google Scholar]
- 106.Cao H., Chen B., Inbaraj B., Chen L., Alvarez-Rivera G., Cifuentes A., Zhang N., Yang D., Simal-Gandara J., Wang M., et al. Preventive potential and mechanism of dietary polyphenols on the formation. Food Front. 2020;1:134–151. doi: 10.1002/fft2.30. [DOI] [Google Scholar]
- 107.Viegas O., Yebra-Pimentel I., Martínez-Carballo E., Simal-Gandara J., Ferreira I. Effect of beer marinades on formation of polycyclic aromatic hydrocarbons in charcoal-grilled pork. J. Agric. Food Chem. 2014;62:2638–2643. doi: 10.1021/jf404966w. [DOI] [PubMed] [Google Scholar]
- 108.Hu G., Cai K., Li Y., Hui T., Wang Z., Chen C., Xu B., Zhang D. Signifikant inhibition of garlic essential oil on benzo[a]pyrene formation in charcoal-grilled pork sausages relates to sulfide compounds. Food Res. Int. 2021;141:110127. doi: 10.1016/j.foodres.2021.110127. [DOI] [PubMed] [Google Scholar]
- 109.Wang C., Xie Y., Wang H., Bai Y., Dai C., Li C., Xu X., Zhou G. Phenolic compounds in beer inhibit formation of polycyclic aromatic hydrocarbons from charcoal-grilled chicken wings. Food Chem. 2019;294:578–586. doi: 10.1016/j.foodchem.2019.05.094. [DOI] [PubMed] [Google Scholar]
- 110.Hur S., Yoon Y., Jo C., Jeong J. Effect of dietary red meat on colorectal cancer risk—a review. Compr. Rev. Food Sci. Food Saf. 2019;18:1812–1824. doi: 10.1111/1541-4337.12501. [DOI] [PubMed] [Google Scholar]
- 111.Fei L., Kuhnle G., Cheng Q. The effect of common spices and meat type on the formation of heterocyclic amines and polycyclic aromatic hydrocarbons in deep-fried meatballs. Food Control. 2018;92:399–411. [Google Scholar]
- 112.Tânia C., Viegas O., Silva M., Martins Z., Fernandes I., Ferreira I., Pinho O., Mateus N., Calhau C. Inhibitory effect of vinegars on the formation of polycyclic aromatic hydrocarbons in charcoal-grilled pork. Meat Sci. 2020;167:108083. doi: 10.1016/j.meatsci.2020.108083. [DOI] [PubMed] [Google Scholar]
- 113.Park K., Pyo H., Kim W., Sun K. Effects of cooking methods and tea marinades on the formation of benzo[a]pyrene in grilled pork belly (Samgyeopsal) Meat Sci. 2017;129:1–8. doi: 10.1016/j.meatsci.2017.02.012. [DOI] [PubMed] [Google Scholar]
- 114.Yao M., Khan I., Cheng Y., Ang Y., Zhou X., Huang M. Effects of cooking methods and tea marinades on the formation of heterocyclicamines and benzo[a]pyrene in grilled drumsticks. J. Food Prot. 2020;83:365–376. doi: 10.4315/0362-028X.JFP-19-084. [DOI] [PubMed] [Google Scholar]
- 115.Meurillon M., Angénieux M., Mercier F., Blinet P., Chaloin L., Chevolleau S., Debrauwer L., Engel E. Mitigation of heterocyclic aromatic amines in cooked meat. Part I: Informed selection of antioxidants based on molecula. Food Chem. 2020;331:127264. doi: 10.1016/j.foodchem.2020.127264. [DOI] [PubMed] [Google Scholar]
- 116.Uzun I., Oz F. Effect of basil use in meatball production on heterocyclic aromatic amine formation. J. Food Sci. Technol. 2021;58:3001–3009. doi: 10.1007/s13197-020-04803-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Ledesma E., Rendueles M., Díaz M. Contamination of meat products during smoking by polycyclic aromatic hydrocarbons: Processes and prevention. Food Control. 2016;60:64–87. doi: 10.1016/j.foodcont.2015.07.016. [DOI] [Google Scholar]
- 118.Ursachi C., Perța-Crișan S., Munteanu F. Strategies to Improve Meat Products’ Quality. Foods. 2020;9:1883. doi: 10.3390/foods9121883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Wang H., Wang C., Li C., Xu X., Zhou G. Effects of phenolic acid marinades on the formation of polycyclic aromatic hydrocarbons in charcoal-grilled chicken wings. J. Food Protect. 2019;82:684–690. doi: 10.4315/0362-028X.JFP-18-420. [DOI] [PubMed] [Google Scholar]
- 120.Wang C., Xie Y., Wang H., Bai Y., Dai C., Li C., Xu X., Zhou G. The influence of natural antioxidants on polycyclic aromatic hydrocarbon formation in charcoal-grilled chicken wings. Food Control. 2019;98:34–41. doi: 10.1016/j.foodcont.2018.11.012. [DOI] [Google Scholar]
- 121.Kim H., Cho J., Kim D., Park T., Jin S., Hur S., Lee S., Jang A. Effects of gochujang (Korean Red Pepper Paste) marinade on polycyclic aromatic hydrocarbon formation in charcoal-grilled pork belly. Food Sci. Anim. Resour. 2021;41:481–496. doi: 10.5851/kosfa.2021.e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Quelhas I., Petisca C., Viegas O., Melo A., Pinho O., Ferreira I. Effect of green tea marinades on the formation of heterocyclicaromatic amines and sensory quality of pan-fried beef. Food Chem. 2010;122:98–104. doi: 10.1016/j.foodchem.2010.02.022. [DOI] [Google Scholar]
- 123.Melo A., Viegas O., Petisca C., Pinho O., Ferreira I. Effect of beer/red wine marinades on the formation of heterocyclic aro-matic amines in pan-fried beef. J. Agric. Food Chem. 2008;56:10625–10632. doi: 10.1021/jf801837s. [DOI] [PubMed] [Google Scholar]
- 124.Viegas O., Moreira P., Ferreira I. Influence of beer marinades on the reduction of carcinogenic heterocyclic aromaticamines in charcoal-grilled pork meat. Food Addit. Contam. Part A. 2015;32:315–323. doi: 10.1080/19440049.2015.1010607. [DOI] [PubMed] [Google Scholar]
- 125.Aaslyng M., Lund B., Jensen K. Inhibition of heterocyclic aromatic amines in pork chops using complex marinades with natural antioxidants. Food Nutr. Sci. 2016;7:1315–1329. doi: 10.4236/fns.2016.714120. [DOI] [Google Scholar]
- 126.Puangsombat K., Smith J. Inhibition of heterocyclic amine for-mation in beef patties by ethanolic extracts of rosemary. J. Food Sci. 2010;75:T40–T47. doi: 10.1111/j.1750-3841.2009.01491.x. [DOI] [PubMed] [Google Scholar]
- 127.Oz E. Inhibitory effect of black cumin on the formation of hetero-cyclic aromatic amines in meatball. PLoS ONE. 2019;14:e0221680. doi: 10.1371/journal.pone.0221680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Sepahpour S., Selamat J., Khatib A., Manap M., Razis A., Hajeb P. Inhibitory effect of mixture herbs/spices on formation of heterocyclic amines and mutagenic activity of grilled beef. Food Addit. Contam. Part A. 2018;35:1911–1927. doi: 10.1080/19440049.2018.1488085. [DOI] [PubMed] [Google Scholar]
- 129.Kilic S., Oz E., Oz F. Effect of turmeric on the reduction of heterocyclic aromatic amines and quality of chicken meatballs. Food Control. 2021;128:108189. doi: 10.1016/j.foodcont.2021.108189. [DOI] [Google Scholar]
- 130.Bao X., Miao J., Fan Y., Lai K. The effective inhibition of the formation of heterocyclic aromatic amines via adding black pepper in fried tilapia fillets. J. Food Process. Preserv. 2020;44:e14435. doi: 10.1111/jfpp.14435. [DOI] [Google Scholar]
- 131.Zeng M., Wang J., Zhang M., Chen J., He Z., Qin F., Xu Z., Cao D., Chen J. Inhibitory effects of Sichuan pepper (Zanthoxylum bungeanum) and sanshoamide extract on heterocyclic amine formation in grilled ground beef patties. Food Chem. 2018;239:111–118. doi: 10.1016/j.foodchem.2017.06.097. [DOI] [PubMed] [Google Scholar]
- 132.Zeng M., Zhang M., He Z., Qin F., Tao G., Zhang S., Gao Y., Chen J. Inhibitory profiles of chilli pepper and capsaicin on heterocyclic amine formation in roast beef patties. Food Chem. 2017;221:404–411. doi: 10.1016/j.foodchem.2016.10.061. [DOI] [PubMed] [Google Scholar]
- 133.Janoszka B. Heterocyclic amines and azaarenes in pan-fried meat and its gravy fried without additives and in the presence of onion and garlic. Food Chem. 2010;120:463–473. doi: 10.1016/j.foodchem.2009.10.039. [DOI] [Google Scholar]
- 134.Račkauskienė I., Pukalskas A., Venskutonis P., Fiore A., Troise A., Fogliano V. Effects of beetroot (Beta vulgaris) preparations on the Maillard reaction products in milk and meat-protein model systems. Food Res. Int. 2015;70:31–39. doi: 10.1016/j.foodres.2015.01.026. [DOI] [Google Scholar]
- 135.Britt C., Gomaa E., Gray J., Booren A. Influence of cherry tissue on lipid oxidation and heterocyclic aromatic amine formation in ground beef patties. J. Agric. Food Chem. 1998;46:4891–4897. doi: 10.1021/jf980233y. [DOI] [Google Scholar]
- 136.Sabally K., Sleno L., Jauffrit J., Iskandar M., Kubow S. Inhibitory effects of apple peel polyphenol extract on the formation of heterocyclic amines in pan fried beef patties. Meat Sci. 2016;117:57–62. doi: 10.1016/j.meatsci.2016.02.040. [DOI] [PubMed] [Google Scholar]
- 137.Keskekoglu H., Üren A. Inhibitory effects of pomegranate seed extract on the formation of heterocyclic aromatic amines in beef and chicken meatballs after cooking by four different methods. Meat Sci. 2014;96:1446–1451. doi: 10.1016/j.meatsci.2013.12.004. [DOI] [PubMed] [Google Scholar]
- 138.Tengilimoglu-Metin M., Hamzalioglu A., Gokmen V., Kizil M. Inhibitory effect of hawthorn extract on heterocyclic aromatic amine formation in beef and chicken breast meat. Food Res. Int. 2017;99:586–595. doi: 10.1016/j.foodres.2017.06.044. [DOI] [PubMed] [Google Scholar]
- 139.Rounds L., Havens C., Feinstein Y., Friedman M., Ravishankar S. Concentration-dependent inhibition of Escherichia coli O157: H7 and heterocyclic amines in heated ground beef patties by apple and olive extracts, onion powder and clove bud oil. Meat Sci. 2013;94:461–467. doi: 10.1016/j.meatsci.2013.03.010. [DOI] [PubMed] [Google Scholar]
- 140.Buja A., Pierbon M., Lago L., Grotto G., Baldo V. Breast cancer primary prevention and diet: An umbrella review. Int. J. Environ. Res. Public Health. 2020;17:4731. doi: 10.3390/ijerph17134731. [DOI] [PMC free article] [PubMed] [Google Scholar]