Abstract
Myocarditis and pericarditis are potential post-acute cardiac sequelae of COVID-19 infection, arising from adaptive immune responses. We aimed to study the incidence of post-acute COVID-19 myocarditis and pericarditis. Retrospective cohort study of 196,992 adults after COVID-19 infection in Clalit Health Services members in Israel between March 2020 and January 2021. Inpatient myocarditis and pericarditis diagnoses were retrieved from day 10 after positive PCR. Follow-up was censored on 28 February 2021, with minimum observation of 18 days. The control cohort of 590,976 adults with at least one negative PCR and no positive PCR were age- and sex-matched. Since the Israeli vaccination program was initiated on 20 December 2020, the time-period matching of the control cohort was calculated backward from 15 December 2020. Nine post-COVID-19 patients developed myocarditis (0.0046%), and eleven patients were diagnosed with pericarditis (0.0056%). In the control cohort, 27 patients had myocarditis (0.0046%) and 52 had pericarditis (0.0088%). Age (adjusted hazard ratio [aHR] 0.96, 95% confidence interval [CI]; 0.93 to 1.00) and male sex (aHR 4.42; 95% CI, 1.64 to 11.96) were associated with myocarditis. Male sex (aHR 1.93; 95% CI 1.09 to 3.41) and peripheral vascular disease (aHR 4.20; 95% CI 1.50 to 11.72) were associated with pericarditis. Post COVID-19 infection was not associated with either myocarditis (aHR 1.08; 95% CI 0.45 to 2.56) or pericarditis (aHR 0.53; 95% CI 0.25 to 1.13). We did not observe an increased incidence of neither pericarditis nor myocarditis in adult patients recovering from COVID-19 infection.
Keywords: COVID-19, myocarditis, pericarditis
1. Introduction
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is a leading cause of morbidity and mortality worldwide [1]. In addition to the clinical manifestations during the acute phase of the COVID-19 disease, there is an accumulating data regarding the subacute and long-term effects of COVID-19, also known as “post-acute COVID-19 syndrome” or “Long COVID”, defined by persistent symptoms several weeks after onset of COVID-19 infection [2]. The “Long-COVID” or “post-acute COVID-19 syndrome” is characterized by multi-organ sequelae or persistent symptoms after recovering from the acute COVID-19 phase, generally after 3 to 4 weeks from the onset of symptoms or the first PCR positive result test [3].
The pathogenesis of “Long-COVID” may result from several mechanisms, including direct viral toxicity, hypercoagulability, microvascular injury, and angiotensin-converting enzyme maladaptation [4]. While the underlying pathophysiological mechanisms leading to post-acute COVID-19 are yet to be fully understood, immune-mediated response [5,6] and immune dysregulation [4] are believed to play a major contributing role in the pathogenesis of this syndrome. There is no consensus as to which time point represents the transition from the acute COVID-10 infection and the recovery phase. As we were considering an indirect immune-mediated inflammation as the potential mechanism explaining delayed peri/myocarditis we reasoned that 10 days after infection is a relevant time point as this is valid with regard to pericarditis after myocardial infarction (Dressler syndrome) or cardiac surgery (postpericardiotomy syndrome).
Infectious causes have been shown to be an important inciting event in the pathophysiology of autoimmune diseases [7]. Viral infections have also been associated with the presence of autoimmune diseases such as systemic lupus disease, rheumatoid arthritis, and diabetes mellitus [8].
In viral infections, both direct contact and replication-induced injury and autoimmune mechanisms have been implicated in the pathogenesis of consequent myocarditis. Inappropriate regulation of T cells resulting from pathogen-related altered self -proteins or from molecular mimicry between the virus and the host or over-activation of B cells may lead to inappropriate immune-mediated damage to host tissue [9]. As such, this delayed inappropriate response may trigger autoimmune like myocarditis and pericarditis [10]. Accordingly, in a subset of patients with idiopathic dilated cardiomyopathy, prior myocarditis is considered causative in some cases and an example supportive of associating etiopathogenesis is the occurrence of anti-beta 1 adrenoreceptor antibodies [11].
Several autoimmune phenomena were linked to a previous COVID-19 infection including heparin-induced thrombocytopenia (HITT), Kawasaki-like syndromes (MIS-C and MIS-A), Guillain-Barre syndrome, vasculitis, and thyroiditis [8]. Thus, it can be postulated that the risk for autoimmune induced myocarditis and pericarditis is increased in recovering COVID-19 patients.
It has recently been reported that the incidence of myocarditis and pericarditis is increased in COVID-19 patients during the acute illness [12]. However; whether or not myocarditis and pericarditis after the recovery period are a part of the long COVID-19 syndrome is yet unknown. Herein, we studied the incidence of myocarditis and pericarditis in a large cohort of COVID-19 patients after recovering from the acute infection.
2. Methods
2.1. Study Setting
We retrieved observational data from Clalit Health Services (CHS). CHS is the largest of four health maintenance organizations that offer mandatory health care coverage in Israel. CHS insures over 50% of the Israeli population (>4.4 million persons), and the CHS-insured population is approximately representative of the Israeli population at large [12,13]. CHS provides outpatient care, and inpatient care is divided between CHS and other hospitals. Research data can be retrieved from the central data warehouse using the CHS Secure Data Sharing Platform powered by MDClone (https://www.mdclone.com, accessed on 5 September 2021).
This study was approved by the institutional review board, and was exempt from the requirement for informed consent.
2.2. Study Design and Patient Population
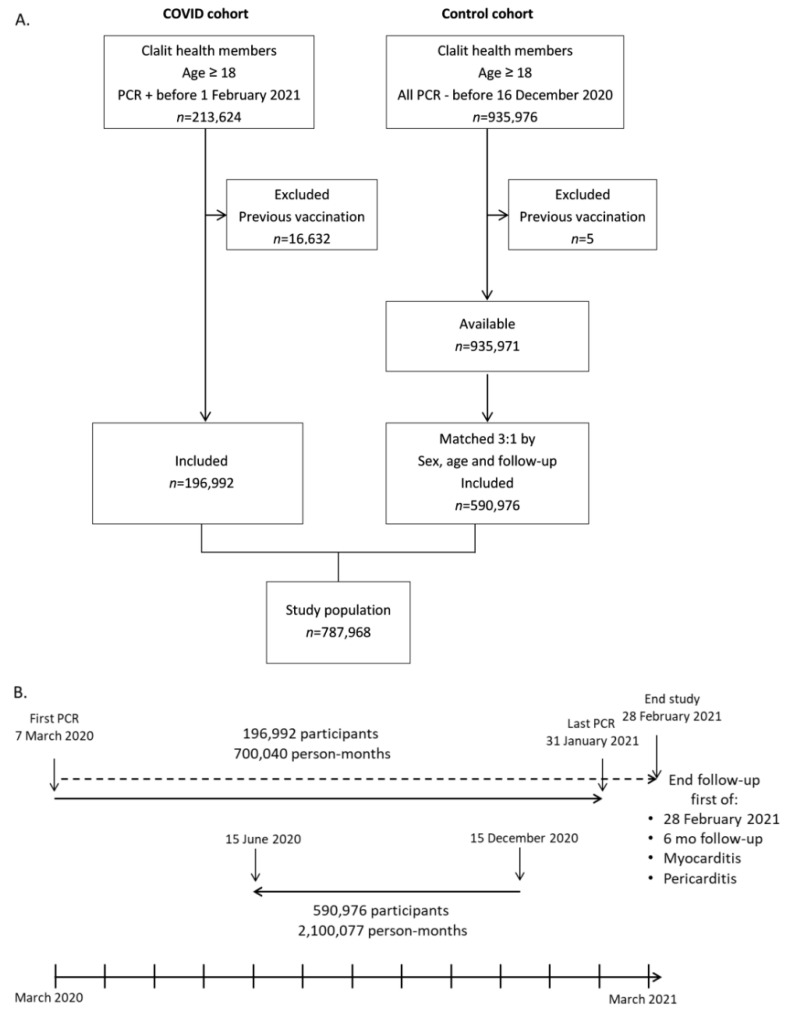
We retrieved records of all adult patients (age ≥ 18 years) who had a documented positive COVID-19 PCR test (n = 213,624) between 7 March 2020 and 31 January 2021 (Figure 1A). Records included demography and cardiovascular risk factors: smoking status, obesity, diabetes mellitus, hyperlipidemia, CKD (chronic kidney disease), PVD (peripheral vascular disease, ACS (acute coronary syndrome), essential hypertension, CVA (cerebrovascular accident), and heart failure (for the The International Classification of disease (ICD-10) code list for all diagnoses, see Table S1). Diagnostic inpatient codes for myocarditis (I40, I40.9, I51.4) and pericarditis (I30, I30.0, I30.9) were extracted between 10 days after COVID-19 infection and earliest between 6 months from infection or 28 February 2021. This was done to ensure a minimum follow-up period of 18 days and a maximum follow-up period of six months. Since data was retrieved during October 2021, we allowed for over 6 months delay in data transfer between hospitals that do not belong to the CHS and the CHS data warehouse. The post-COVID timeframe was defined from at least ten days after the date of positive PCR test contingent upon lack of symptoms related to COVID-19 infection, according to the definitions of the Israeli Ministry of Health. Patients with a first vaccination received before COVID-19 infection were excluded (n = 16,632), resulting in the final COVID-19 cohort (n = 196,992).
Figure 1.
Study profile, design and timelines. ‘clalit’ = Clalit Health Services. Vaccination = COVID-19 vaccination. PCR −/+ = negative/positive COVID-19 PCR. (A). Flowchart of patient selection in COVID and control cohorts. (B). Research timeline from first PCR in 7 March 2020 to the end of study (lower part). The COVID cohort is depicted in the upper part, and the matching period of the control cohort is depicted in the middle.
A control group was created from a cohort of adult patients with at least one negative COVID-19 PCR between 7 March 2020 and 15 December 2020, and with no prior positive COVID-19 PCR before retrieval of data in August 2021 (n = 935,976). 15 December 2020 was selected as the stop date, since the massive Israeli vaccination campaign was initiated on 20 December 2020. Still, five patients were excluded due to a previous COVID-19 vaccination. From this pool of patients (n = 935,971), the control cohort was created by 3:1 matching of age (±2 years) and sex (n = 590,976). The follow-up period of each of the three control patients was set to the exact same length of follow-up of the matched COVID-19 patient. The follow-up period was calculated backwards from 15 December 2020 (Figure 1B), in order to avoid the potential impact of COVID-19 vaccination on myocarditis and pericarditis. Although the COVID-19 patients’ drafting period was from March 2020 to January 2021, almost all COVID-19 cases occurred between July 2020 and January 2021 (Figure S1).
2.3. Statistical Analysis
We compared the baseline characteristics of the cohorts with the chi-square test. We used Kaplan-Meier cumulative incidence curves to assess the effect of post-COVID-19 infection on myocarditis and pericarditis up to a maximal follow-up of six months. Univariable and multivariable Cox proportional hazards regression models were used. Post-COVID infection, age, sex, BMI, diabetes, hyperlipidemia, obesity, chronic kidney injury, smoking status, peripheral vascular disease, acute coronary syndrome, and essential hypertension were introduced in the adjusted models. Both crude hazard ratio (HR) and adjusted HR (aHR) are presented with 95% confidence intervals. A p-value less than 0.05 was considered statistically significant. Statistical analyses were performed with R version 4.0.2, packages: survival, Survminer, ggplot2, and with SPSS version 26 (IBM).
3. Results
A total of 787,968 Clalit Health Services adult members (age ≥ 18) were included in the study (Figure 1), comprising of COVID-19 cohort (n = 196,992) and a sex and age 3:1 matched control cohort (n = 590,976). Total follow-up was 700,040 person-months in the COVID-19 cohort, and 2,100,077 person-months in the control cohort, with a median follow-up of 4.1 months [IQR 1.3–5.6 months]. The mean standard deviation (SD) age in both groups was 42.4 (17.7) years, and 45.7% were males (Table 1). There was a slightly higher BMI (mean (SD) 27.1 (7.1) vs. 26.1 (6.7) kg/m2) with higher prevalence of obesity (29.9% vs. 24.6%), diabetes mellitus (13% vs. 10.5%), essential hypertension (18.5% vs. 17%), cerebrovascular accidents (4% vs. 3.7%) and heart failure (2.6% vs. 2.2%) in the COVID-19 cohort. There was a lower prevalence of current and past smoking (11.3% vs. 18.4% and 10.8% vs. 12.3%) and peripheral vascular disease (1.2% vs. 1.4%) in the COVID-19 cohort.
Table 1.
Baseline Characteristics of the study population by COVID-19 infection status.
| Control | COVID-19 | |
|---|---|---|
| (n = 590,976) | (n = 196,992) | |
| Age (year) | 42.4 (17.7) | 42.4 (17.7) |
| Sex | ||
| Male | 270,210 (45.7) | 90,070 (45.7) |
| Female | 320,766 (54.3) | 106,922 (54.3) |
| BMI (kg/m2) | 26.1 (7.1) | 27.1 (6.7) |
| Sector | ||
| Arab | 109,759 (18.6) | 58,841 (29.9) |
| Bedouin | 19,956 (3.4) | 5306 (2.7) |
| Jewish | 436,986 (74.1) | 108,360 (55.0) |
| Other | 23,285 (3.9) | 24,475 (12.4) |
| Smoking | ||
| Never | 383,002 (69.3) | 137,079 (78.0) |
| Current | 101,475 (18.4) | 19,824 (11.3) |
| Past | 67,992 (12.3) | 18,917 (10.8) |
| Obesity | 145,537 (24.6) | 58,807 (29.9) |
| Diabetes | 61,978 (10.5) | 25,583 (13.0) |
| Hyperlipidemia | 183,704 (31.1) | 60,629 (30.8) |
| CKD | 18,593 (3.1) | 6725 (3.4) |
| PVD | 8016 (1.4) | 2448 (1.2) |
| Hypertension | 100,736 (17.0) | 36,502 (18.5) |
| ACS | 32,987 (5.6) | 11,027 (5.6) |
| CVA | 22,032 (3.7) | 7833 (4.0) |
| Heart failure | 13,228 (2.2) | 5132 (2.6) |
Variables were expressed as no. (%) or as mean (SD). CKD = chronic kidney disease. PVD = peripheral vascular disease, CVA = Cerebrovascular Accident. ACS = acute coronary syndrome.
During the study period, nine cases of myocarditis and 11 cases of pericarditis were detected in the COVID-19 cohort (Table 2). Twenty-seven cases of myocarditis and 52 cases of pericarditis were detected in the control cohort. Two out of the nine myocarditis patients were hospitalized due to severe COVID-19 infection with the need for mechanical ventilation, and myocarditis was diagnosed during the COVID-19 hospitalization at days 19 and 37 after infection, respectively. None of the patients who were diagnosed with pericarditis were hospitalized due to COVID-19 infection. The median (IQR) duration of hospitalization following myocarditis in the COVID-19 cohort was 5 (2–25) days vs. 3 (3–5) days in the control cohort (p = 0.291). The median (IQR) duration of hospitalization following pericarditis was 2 (2–3.5) days in the COVID-19 cohort and 3 (1.8–5.3) days in the control cohort (p = 0.272).
Table 2.
Baseline characteristics of patients with myocarditis and pericarditis patients in the COVID and no COVID cohorts.
| Myocarditis | Pericarditis | ||||||
|---|---|---|---|---|---|---|---|
| No COVID (n = 27) |
COVID (n = 9) |
p-Value | No COVID (n = 52) |
COVID (n = 11) |
p-Value | ||
| Days in hospital | 3 [3–5] | 5 [2–25] | 0.291 | 3 [1.8–5.3] | 2 [2–3.5] | 0.272 | |
| Age (year) | 39.1 (16.8) | 36.4 (19.7) | 0.695 | 49.1 (20.3) | 45.6 (19.3) | 0.609 | |
| Sex (male) | 20 (74.1) | 8 (88.9) | 0.643 | 31 (59.6) | 8 (72.7) | 0.637 | |
| BMI (kg/m2) | 27.3 (6.1) | 26.3 (6.9) | 0.713 | 26.5 (5.8) | 28.6 (3.8) | 0.319 | |
| Diabetes | 4 (14.8) | 1 (11.1) | 1.000 | 12 (23.1) | 1 (9.1) | 0.528 | |
| Hyperlipidemia | 6 (22.2) | 2 (22.2) | 1.000 | 25 (48.1) | 4 (36.4) | 0.708 | |
| Obesity | 14 (51.9) | 1 (11.1) | 0.079 | 15 (28.8) | 6 (54.5) | 0.197 | |
| CKD | 3 (11.1) | 1 (11.1) | 1.000 | 7 (13.5) | 1 (9.1) | 1.000 | |
| Smoking | Now | 6 (26.1) | 1 (12.5) | 0.602 | 9 (19.1) | 1 (9.1) | 0.777 |
| Past | 3 (13.0) | 2 (25.0) | 7 (14.9) | 1 (9.1) | |||
| PVD | 2 (7.4) | 0 (0.0) | 1.000 | 4 (7.7) | 2 (18.2) | 0.609 | |
| ACS | 3 (11.1) | 2 (22.2) | 0.781 | 9 (17.3) | 2 (18.2) | 1.000 | |
| Hypertension | 5 (18.5) | 2 (22.2) | 1.000 | 15 (28.8) | 3 (27.3) | 1.000 | |
| CVA | 3 (11.1) | 2 (22.2) | 0.781 | 5 (9.6) | 2 (18.2) | 0.769 | |
| HF | 5 (18.5) | 2 (22.2) | 1.000 | 6 (11.5) | 1 (9.1) | 1.000 | |
| Severe COVID | - | 2 (22.2) | NA | - | 0 (0.0) | NA | |
Variables were expressed as no. (%), median [IQR], or as mean (SD). CKD = chronic kidney disease. PVD = peripheral vascular disease. CVA = Cerebrovascular Accident, ACS = acute coronary syndrome. HF = Heart Failure. Days in hospital = length of stay of the hospitalization at which myocarditis/pericarditis were diagnosed.
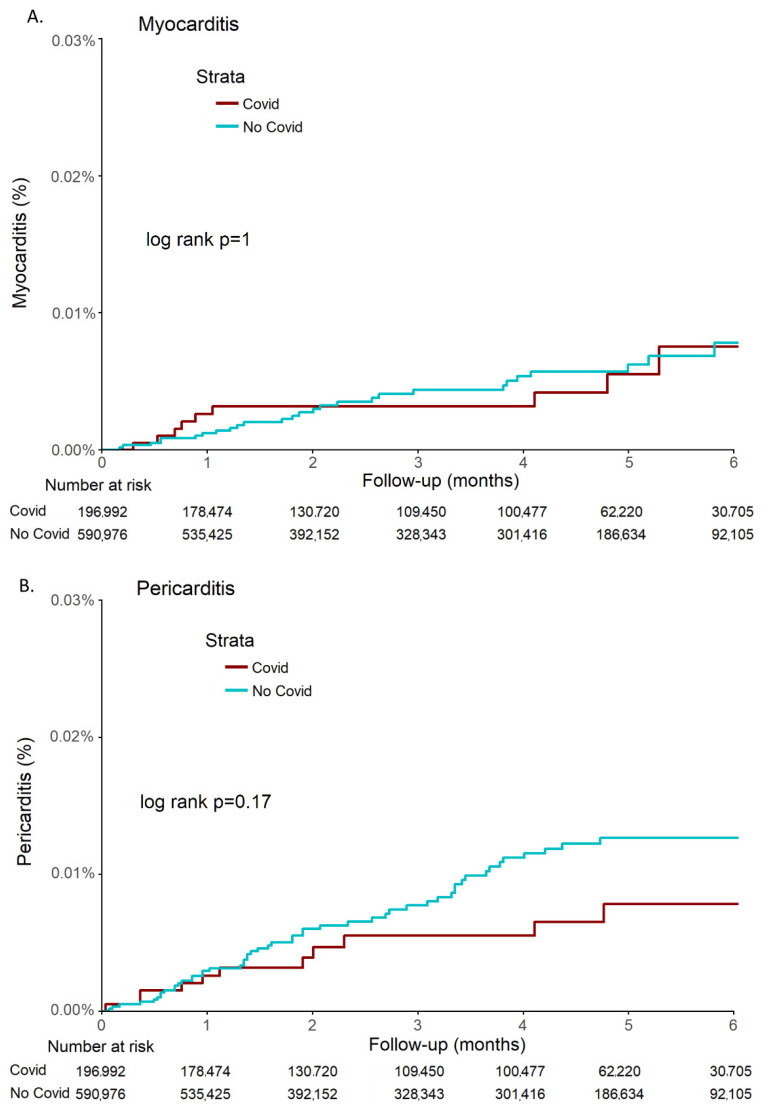
No statistical difference in the incidence rate of both myocarditis (p =1) and pericarditis (p =0.17) was observed between the COVID-19 cohort and the control cohort (Figure 2).
Figure 2.
Kaplan-Meier estimates of cumulative probability of myocarditis (A) and pericarditis (B) in COVID-19 and control cohorts during 6 months.
In the multivariable Cox proportional hazards regression model (Table 3, Tables S2 and S3), age (aHR 0.96; 95% CI 0.93 to 1.00, p =0.045) and the male sex (aHR 4.42; 95% CI 1.64 to 11.96, p = 0.003) were independently associated with myocarditis. Obesity was borderline associated with myocarditis (aHR 2.31; 95% CI 0.99 to 5.41, p = 0.053). Post COVID-19 infection was not associated with myocarditis (aHR 1.08; 95% CI 0.45 to 2.56, p = 0.869).
Table 3.
Adjusted HRs for myocarditis and pericarditis.
| Myocarditis | Pericarditis | |||
|---|---|---|---|---|
| aHR (95% CI) | p-Value | aHR (95% CI) | p-Value | |
| COVID-19 | 1.08 (0.45–2.56) | 0.869 | 0.53 (0.25–1.13) | 0.100 |
| Age | 0.96 (0.93–1.00) | 0.045 * | 1.01 (0.99–1.03) | 0.537 |
| Sex (male) | 4.42 (1.64–11.96) | 0.003 * | 1.93 (1.09–3.41) | 0.025 * |
| BMI | 1.00 (0.97–1.04) | 0.935 | 1.00 (0.94–1.06) | 0.897 |
| Diabetes | 1.15 (0.26–5.00) | 0.856 | 0.97 (0.43–2.21) | 0.950 |
| Hyperlipidemia | 0.33 (0.08–1.43) | 0.139 | 1.13 (0.54–2.38) | 0.749 |
| Obesity | 2.31 (0.99–5.41) | 0.053 | 1.32 (0.64–2.71) | 0.448 |
| CKD | 3.80 (0.82–17.66) | 0.088 | 1.91 (0.72–5.05) | 0.191 |
| Smoking (Now) | 1.62 (0.65–4.06) | 0.304 | 0.85 (0.42–1.74) | 0.661 |
| Smoking (Past) | 1.85 (0.61–5.64) | 0.277 | 0.73 (0.33–1.63) | 0.439 |
| PVD | 1.35 (0.14–12.84) | 0.793 | 4.20 (1.50–11.72) | 0.006 * |
| ACS | 3.93 (0.76–20.40) | 0.104 | 1.52 (0.61–3.80) | 0.366 |
| Hypertension | 1.46 (0.36–5.87) | 0.592 | 0.88 (0.38–2.06) | 0.770 |
CKD = chronic kidney disease. PVD = peripheral vascular disease. ACS = acute coronary syndrome. * Statistically significant results are highlighted in bold.
Male sex (aHR 1.93; 95% CI 1.09 to 3.41, p = 0.025) and peripheral vascular disease (aHR 4.20; 95% CI 1.50 to 11.72, p = 0.006) were associated with pericarditis (Table 3). Post COVID-19 infection was not associated with pericarditis (aHR 0.53; 95% CI 0.25 to 1.13, p = 0.1).
4. Discussion
In the current large population study of subjects, who were not vaccinated against SARS-CoV-2, we observed no increase in the incidence of myocarditis or pericarditis from day 10 after positive SARS-CoV-2.
Multivariable analysis did show male sex as associated with a higher risk of developing myocarditis or pericarditis, regardless of previous COVID-19 infection.
COVID-19 infection is responsible for considerable morbidity and mortality at an unprecedented scale globally. Cumulative scientific and clinical data is evolving on the sub-acute and long-term effects of COVID-19 infection, which can affect multiple organ systems. Recent studies suggest several mechanisms for the pathogenesis of the persistent and prolonged signs and symptoms associated with the cardiovascular system.
Several earlier studies on SARS-CoV infections have highlighted the possible link between types of coronavirus infections and immune-mediated responses [14,15].
Antibodies to Coronavirus-OC43 and 229E were found in patients diagnosed with multiple sclerosis [16]. High and sustained levels of anti-erythrocyte autoantibodies were found in mice infected with murine hepatitis Coronavirus [17].
Given the clinical similarities between SARS-CoV-2 and other coronaviruses [18,19], it is conceivable that immune-mediated tissue damage is also potentially induced by SARS-CoV-2 infection. Molecular mimicry, activation of specific T cells to virus altered self-proteins, and activation of B cells constitute a few examples of mechanisms mediating the potential occurrence of myocarditis and pericarditis that could play a role in triggering delayed cardiac inflammation [9]. Furthermore, in a recent study 309 COVID-19 patients were tested for the presence of six different autoantibodies, such as anti-nuclear antibodies and anti-Interferon-α2 antibodies, at least two months after the initial illness. In this study, autoantibodies were associated with a higher risk of developing post-acute sequelae of COVID-19 [20].
Early in the COVID-19 pandemic, it was evident that COVID-19 patients with cardiovascular comorbidities have worse prognosis and higher in-hospital mortality [21]. Individuals with underlying autoimmune diseases appear to be particularly vulnerable to severe sequelae resulting from COVID-19 infection [22]. Other studies demonstrated that severe COVID-19 disease is associated with robust inflammatory responses including type two and hyper four hypersensitivity responses, resulting from overactivation of T cells and a subsequent cytokine storm [23,24]. Immune-mediated manifestations of COVID-19 include mimicry of autoimmune diseases like Kawasaki disease, Guillain-Barre syndrome, vasculitis, myositis, and myocardial damage [25].
Puntmann et al. found a 78% cardiac involvement assessed by Cardiac Magnetic Resonance Imaging (MRI) among patients with a confirmed diagnosis of COVID-19 eight weeks before enrollment [26], most of whom were asymptomatic or had just mild symptoms. This study demonstrates cardiac inflammation independent of the severity of the initial illness nor the overall course of the acute illness. A recent study showed an increased risk of late cardiovascular outcomes in either symptomatic or asymptomatic SARS-CoV-2 infection [27]. Thus, we also sought to investigate whether cardiac damage may also occur regardless of the presence of corona-related symptoms. Further corroborating the potential late inflammatory pericardial and myocardial involvement is an additional cardiovascular magnetic resonance (CMR) guided study demonstrating myocardial edema, fibrosis, and impaired right ventricle function in 58% (16 of 25) patients recently recovering from COVID-19 [28]. These studies are supported by an autopsy study pointing to the occurrence of mononuclear infiltrates in patients with COVID-19 infection [29]. However, an important caveat to these studies is the lack of appropriate controls including patients with other intercurrent viral infections.
Similar to our study, Xie et al. showed that individuals with COVID-19 infection are at increased risk of cardiovascular complications 30 days after infection, including pericarditis and myocarditis regardless of the need for hospitalization [30]. Comparable with our study, the study population was tested for the risk of inflammatory heart diseases regardless of previous SRAS-COV-2 vaccination. Yet, in contrast, in the study by Xie et al., the tested cohort was homogenous, comprising of US Department of Veterans Affairs with male predominance and young age. The difference in the population characteristics may explain the dissimilarity between the results of the studies as young males are known to exhibit a higher incidence of myocarditis and pericarditis.
Higher risk of myocarditis (risk ratio, 18.28; 95% CI, 3.95 to 25.12; risk difference, 11.0 events per 100,000 persons; 95% CI, 5.6 to 15.8) and pericarditis was observed in a large population study of recently published by Barda et al. [12]. Although both our study and the study by Barda et al. are based on Clalit Health Service patients, there are several important differences between the studies. Barda et al. were focused on COVID-19 vaccination, and thus the matching was designed to neutralize vaccination-related factors, while our study is on a non-vaccinated population. Barda et al. studied the occurrence of myocarditis and pericarditis from positive PCR results up to 42 days, while we study recovering patients starting 10 days after infection and for a significantly more prolonged time. Barda et al.’s analysis also ignores the timing of myocarditis and pericarditis. Finally, while Barda et al. have included many causes of myocarditis and pericarditis, we only included acute myocarditis and pericarditis in hospitalized patients which is more likely to be accurate.
Our current study has several limitations. First, although the potential number of participants who were considered for inclusion was large, the number of cases of myocarditis and pericarditis was small. This was mainly attributed to the limitation of a relatively short follow-up period due to the initiation of the massive vaccination program. Second, we included only cases of hospitalized myocarditis or pericarditis patients, whereas outpatient medical records were excluded from the study. This could possibly omit a small number of patients with mild disease. Furthermore, we included a diagnosis of myocarditis and pericarditis according to the medical records, without access to patient-based information regarding confirmation of the diagnosis.
5. Conclusions
Our data suggest that there is no increase in the incidence of myocarditis and pericarditis in COVID-19 recovered patients compared to uninfected matched controls. Further longer-term studies will be needed to estimate the incidence of pericarditis and myocarditis in patients diagnosed with COVID-19.
Acknowledgments
The authors would like to thank Galit Shefer for her assistance in research design, The Clalit Research Institute for their assistance in data analysis and the Kaplan Medical Center Heart team for their support.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm11082219/s1, Figure S1. Number of patients with positive PCR in the COVID-19 cohort by month during the study period. Table S1. ICD-10 codes for cardiac risk factors. Table S2. Crude and adjusted HRs for myocarditis. Table S3. Crude and adjusted HRs for pericarditis.
Author Contributions
Conceptualization, J.G.; Data curation, E.D.; Formal analysis, E.D. and R.R.H.; Investigation, S.T., O.T. and D.H.; Methodology—E.D. and G.S.; Project administration, J.G.; Supervision, A.A.; Validation, S.T. and J.G.; Writing–original draft, O.T.; Writing–review & editing, S.T. and J.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Kaplan Medical Center (KMC-123-2021), Date of approval 24 June 2021.
Informed Consent Statement
Patient consent was waived due to de-identified retrospective cohort study.
Data Availability Statement
The data presented in this study is available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Paules C.I., Marston H.D., Fauci A.S. Coronavirus Infections—More Than Just the Common Cold. JAMA. 2020;323:707–708. doi: 10.1001/jama.2020.0757. [DOI] [PubMed] [Google Scholar]
- 2.Lopez-Leon S., Wegman-Ostrosky T., Perelman C., Sepulveda R., Rebolledo P.A., Cuapio A., Villapol S. More than 50 long-term effects of COVID-19: A systematic review and meta-analysis. Sci. Rep. 2021;11:16144. doi: 10.1038/s41598-021-95565-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Raveendran A.V., Jayadevan R., Sashidharan S. Long COVID: An overview. Diabetes Metab. Syndr. Clin. Res. Rev. 2021;15:869–875. doi: 10.1016/j.dsx.2021.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shuwa H.A., Shaw T.N., Knight S.B., Wemyss K., McClure F.A., Pearmain L., Prise I., Jagger C., Morgan D.J., Khan S., et al. Alterations in T and B cell function persist in convalescent COVID-19 patients. Med. 2021;2:720–735.e4. doi: 10.1016/j.medj.2021.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McElvaney O.J., McEvoy N.L., McElvaney O.F., Carroll T.P., Murphy M.P., Dunlea D.M., Ni Choileain O., Clarke J., O’Connor E., Hogan G., et al. Characterization of the Inflammatory Response to Severe COVID-19 Illness. Am. J. Respir. Crit. Care Med. 2020;202:812–821. doi: 10.1164/rccm.202005-1583OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tang N., Li D., Wang X., Sun Z. Abnormal Coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J. Thromb. Haemost. 2020;18:844–847. doi: 10.1111/jth.14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ercolini A.M., Miller S.D. The role of infections in autoimmune disease. Clin. Exp. Immunol. 2009;155:1–15. doi: 10.1111/j.1365-2249.2008.03834.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yazdanpanah N., Rezaei N. Autoimmune complications of COVID-19. J. Med. Virol. 2021;94:54–62. doi: 10.1002/jmv.27292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fujinami R.S., von Herrath M.G., Christen U., Whitton J.L. Molecular Mimicry, Bystander Activation, or Viral Persistence: Infections and Autoimmune Disease. Clin. Microbiol. Rev. 2006;19:80–94. doi: 10.1128/CMR.19.1.80-94.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Caforio A.L.P., Mahon N., Baig M.K., Tona F., Murphy R.T., Elliott P.M., McKenna W.J. Prospective Familial Assessment in Dilated Cardiomyopathy: Cardiac autoantibodies predict disease development in asymptomatic relatives. Circulation. 2007;115:76–83. doi: 10.1161/CIRCULATIONAHA.106.641472. [DOI] [PubMed] [Google Scholar]
- 11.Matsui S., Fu M.L., Katsuda S., Hayase M., Yamaguchi N., Teraoka K., Kurihara T., Takekoshi N., Murakami E., Hoebeke J., et al. Peptides Derived from Cardiovascular G-protein-coupled Receptors Induce Morphological Cardiomyopathic Changes in Immunized Rabbits. J. Mol. Cell. Cardiol. 1997;29:641–655. doi: 10.1006/jmcc.1996.0307. [DOI] [PubMed] [Google Scholar]
- 12.Barda N., Dagan N., Ben-Shlomo Y., Kepten E., Waxman J., Ohana R., Hernán M.A., Lipsitch M., Kohane I., Netzer D., et al. Safety of the BNT162b2 mRNA COVID-19 Vaccine in a Nationwide Setting. N. Engl. J. Med. 2021;385:1078–1090. doi: 10.1056/NEJMoa2110475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marom T., Tshori S., Shefer G., Pitaro J. Pneumococcal Conjugated Vaccines Decreased Acute Otitis Media Burden: A Population-Based Study in Israel. J. Pediatr. 2021;235:233–238.e3. doi: 10.1016/j.jpeds.2021.04.025. [DOI] [PubMed] [Google Scholar]
- 14.Lo A.W., Tang N.L., To K.-F. How the SARS coronavirus causes disease: Host or organism? J. Pathol. 2006;208:142–151. doi: 10.1002/path.1897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kyuwa S., Yamaguchi K., Toyoda Y., Fujiwara K. Induction of self-reactive T cells after murine coronavirus infection. J. Virol. 1991;65:1789–1795. doi: 10.1128/jvi.65.4.1789-1795.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Salmi A., Ziola B., Hovi T., Reunanen M. Antibodies to coronaviruses OC43 and 229E in multiple sclerosis patients. Neurology. 1982;32:292–295. doi: 10.1212/WNL.32.3.292. [DOI] [PubMed] [Google Scholar]
- 17.Lardans V., Godfraind C., Van Der Logt J.T.M., Heessen F.W.A., Gonzalez M.-D., Coutelier J.-P. Polyclonal B lymphocyte activation induced by mouse hepatitis virus A59 infection. J. Gen. Virol. 1996;77:1005–1009. doi: 10.1099/0022-1317-77-5-1005. [DOI] [PubMed] [Google Scholar]
- 18.Lu R., Zhao X., Li J., Niu P., Yang B., Wu H., Wang W., Song H., Huang B., Zhu N., et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet. 2020;395:565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Le Bert N., Tan A.T., Kunasegaran K., Tham C.Y.L., Hafezi M., Chia A., Chng M.H.Y., Lin M., Tan N., Linster M., et al. SARS-CoV-2-specific T cell immunity in cases of COVID-19 and SARS, and uninfected controls. Nature. 2020;584:457–462. doi: 10.1038/s41586-020-2550-z. [DOI] [PubMed] [Google Scholar]
- 20.Su Y., Yuan D., Chen D.G., Ng R.H., Wang K., Choi J., Li S., Hong S., Zhang R., Xie J., et al. Multiple early factors anticipate post-acute COVID-19 sequelae. Cell. 2022;185:881–895.e20. doi: 10.1016/j.cell.2022.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Late-Breaking Science Abstracts and Featured Science Abstracts From the American Heart Association’s Scientific Sessions 2020 and Late-Breaking Abstracts in Resuscitation Science From the Resuscitation Science Symposium 2020. Circulation. 2020;142:e470–e500. doi: 10.1161/cir.0000000000000940. [DOI] [PubMed] [Google Scholar]
- 22.Montero F., Martínez-Barrio J., Serrano-Benavente B., González T., Rivera J., Collada J.M., Castrejón I., Álvaro-Gracia J. Coronavirus disease 2019 (COVID-19) in autoimmune and inflammatory conditions: Clinical characteristics of poor outcomes. Rheumatol. Int. 2020;40:1593–1598. doi: 10.1007/s00296-020-04676-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tan C., Zheng X., Sun F., He J., Shi H., Chen M., Tu C., Huang Y., Wang Z., Liang Y., et al. Hypersensitivity may be involved in severe COVID-19. Clin. Exp. Allergy. 2021;52:324–333. doi: 10.1111/cea.14023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yu L., Feng Z. The Role of Toll-Like Receptor Signaling in the Progression of Heart Failure. Mediat. Inflamm. 2018;2018:9874109. doi: 10.1155/2018/9874109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saad M.A., Alfishawy M., Nassar M., Mohamed M., Esene I.N., Elbendary A. COVID-19 and Autoimmune Diseases: A Systematic Review of Reported Cases. Curr. Rheumatol. Rev. 2021;17:193–204. doi: 10.2174/1573397116666201029155856. [DOI] [PubMed] [Google Scholar]
- 26.Puntmann V.O., Carerj M.L., Wieters I., Fahim M., Arendt C., Hoffmann J., Shchendrygina A., Escher F., Vasa-Nicotera M., Zeiher A.M., et al. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19) JAMA Cardiol. 2020;5:1265–1273. doi: 10.1001/jamacardio.2020.3557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tereshchenko L.G., Bishop A., Fisher-Campbell N., Levene J., Morris C., Patel H., Khan A. Risk of Cardiovascular Events after COVID-19: A double-cohort study. medRxiv. 2021 doi: 10.1101/2021.12.27.21268448. [DOI] [Google Scholar]
- 28.Huang L., Zhao P., Tang D., Zhu T., Han R., Zhan C., Liu W., Zeng H., Tao Q., Xia L. Cardiac Involvement in Patients Recovered From COVID-2019 Identified Using Magnetic Resonance Imaging. JACC Cardiovasc. Imaging. 2020;13:2330–2339. doi: 10.1016/j.jcmg.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rali A.S., Ranka S., Shah Z., Sauer A.J. Mechanisms of Myocardial Injury in Coronavirus Disease 2019. Card. Fail. Rev. 2020;6:e15. doi: 10.15420/cfr.2020.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xie Y., Xu E., Bowe B., Al-Aly Z. Long-term cardiovascular outcomes of COVID-19. Nat. Med. 2022;28:583–590. doi: 10.1038/s41591-022-01689-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study is available on request from the corresponding author.