Abstract
The COVID-19 pandemic has been suggested to have adverse impacts on psychiatric disorders. This study aimed to investigate the changes in medical visits due to a wide range of psychiatric disorders in children during the COVID-19 pandemic. The medical visits of all Korean children and adolescents (0–19 years old) due to the 12 following psychiatric disorders were investigated: autism; attention-deficit/hyperactivity disorder (ADHD); depressive disorder; bipolar disorder; primary insomnia; schizophrenia; panic disorder; hypochondriasis; posttraumatic stress disorder (PTSD); anxiety disorder; anorexia nervosa; and adephagia. The mean medical visits before and during the COVID-19 pandemic were compared. The mean number of clinical visits due to autism, ADHD, depressive disorder, bipolar disorder, panic disorder, hypochondriasis, PTSD, anxiety disorder, and anorexia nervosa was higher during the COVID-19 pandemic than before the COVID-19 pandemic (all p < 0.05). The higher mean number of medical visits due to psychiatric disorders was maintained in age and sex subgroups. The female and adolescent groups demonstrated a higher mean number of medical visits due to psychiatric disorders during the COVID-19 pandemic. The medical visits due to many psychiatric disorders were higher during the COVID-19 pandemic than before COVID-19 in children and adolescents in Korea. Women and adolescents were more susceptible to psychiatric disorders during the COVID-19 pandemic.
Keywords: COVID-19, depression, anxiety, child, adolescent, epidemiology
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic has been suggested to increase psychiatric burdens [1,2]. In particular, the COVID-19 pandemic could impose specific circumstances on children compared to adults. The closure of daycare centers or schools during the COVID-19 lockdown or social distancing acts may disrupt social support for susceptible children, such as those with low socioeconomic status, and increase the risk of abuse at home [3,4]. The widespread use of home-based online learning programs can increase the risk of internet addiction [5]. In addition, childhood is a period of development for both physical and psychiatric aspects and children are vulnerable to adverse or traumatic events [6,7]. Posttraumatic stress disorder (PTSD) in children is reported to be characterized by induced developmental abnormalities in the frontolimbic circuits, which result in increased threat reactivity and the loss of emotional control [7]. Children have an immature cognitive capacity and can experience hardships in coping with the COVID-19 pandemic [6]. Therefore, the psychiatric impacts of the COVID-19 pandemic on children need to be evaluated separately from the impacts on adults.
Several recent studies have reported the effect of COVID-19 on psychiatric wellbeing of children [8,9]. Our previous study estimated that self-reported stress and suicide-related behaviors were not increased in Korean adolescents during the COVID-19 pandemic [10]. However, this survey was based on self-report questionnaires, and the age range was restricted to the adolescent period (aged 12 to 18 years). Other prior studies have suggested increased anxiety and depression in children during the COVID-19 pandemic [8]. In a meta-analysis study, children and adolescents were exposed to an increased risk of anxiety, depression, sleep disturbances, and anorexia, which were related to containment actions, such as social distancing, school closures, and isolation [9]. Due to quarantine measures, social isolation and restrictions on physical activities can result in loneliness and mental distress. During the lockdown period, emotional and somatic symptoms, including depression, anxiety, uncontrolled emotional problems, and somatic complaints, increased in the 8- to 18-year-old population in Spain [11]. Because children are in developmental periods and have poorer coping skills for disasters than adults, various psychiatric disorders, in addition to depression and anxiety, could be influenced by the COVID-19 pandemic.
This study predicted that medical visits for a wide range of psychiatric disorders in youth would be changed during the COVID-19 pandemic compared to those before the COVID-19 pandemic. To test this hypothesis, all Korean children were investigated for mean medical visits due to psychiatric disorders during and before the COVID-19 pandemic.
2. Materials and Methods
2.1. Ethics
The analyses of the national health insurance data in Korea for this study were permitted by the Ethics Committee of Hallym University (2021-11-004). Written informed consent was not required in this study because the Ethics Committee permitted the exemption of the acquisition of written informed consent.
2.2. Participants and Measurements
This study included the entire Korean children and adolescent population (~8.7 million, 0–19 years old) without exception, as a single health insurance system mandatorily covers the whole country. Thus, we could gather the data of all Koreans, from primary clinics to tertiary hospitals. In this study, we analyzed Korea National Health Insurance Database medical claim code data from January 2018 through May 2021. The data were extracted for age, sex, and the diagnostic claim codes of psychiatric diseases. As the first COVID-19 cases in Korea were discovered on 20 January 2020, and disease prevention and control started in March 2020, we defined the period of ‘before COVID-19′ as until February 2020 and the period ‘during COVID-19′ from March 2020 onward.
We evaluated the monthly incidence of 12 psychiatric diseases that are common in primary clinics. The patients’ diseases were examined based on the histories of visiting clinics in person for each psychiatric disorder. The diagnosis of psychiatric diseases were based on the following ICD-10 codes: autism (F840, F841); ADHD (F900); depressive disorder (F32, F33); bipolar disorder (F31); primary insomnia (F510, G470); schizophrenia (F20, F21, F231, F232, F25); panic disorder (F400, F410); hypochondriasis (F452); posttraumatic stress disorder (F431); anxiety disorder (F40, F41); anorexia nervosa (F500, F501, F508); and bulimia nervosa (F502, F503, F504, F505). The diagnostic codes were registered by the physicians. The incidence of diseases was calculated without duplication, as we had the health insurance database of the entire hospitals or clinics, and patients were identified by their unique resident registration number.
2.3. Statistics
The differences in the mean medical visits for diseases before and during the COVID-19 pandemic were estimated using the Mann–Whitney U test for nonparametric values. The group difference in the variance in clinical visits due to psychiatric diseases before and during the COVID-19 pandemic was evaluated using Levene’s test for nonparametric values [12]. The participants were subgrouped according to age (0–4 years old, 5–9 years old, 10–14 years old, and 15–19 years old) and sex.
Two-tailed analyses were performed. Statistical significance was defined as p values < 0.05. SPSS version 22.0 was used for the statistical analyses (IBM, Armonk, NY, USA).
3. Results
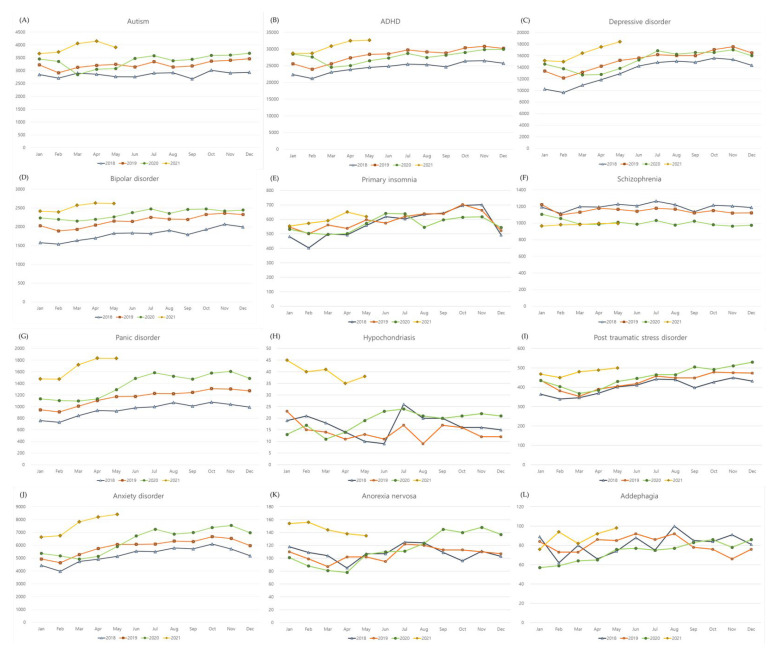
The number of mean clinical visits due to autism, ADHD, depressive disorder, bipolar disorder, panic disorder, hypochondriasis, PTSD, anxiety disorder, and anorexia nervosa was higher during the COVID-19 pandemic than before the COVID-19 pandemic (all p < 0.05, Table 1 and Figure 1). On the other hand, the mean number of clinical visits due to schizophrenia was lower during the COVID-19 pandemic than before the COVID-19 pandemic (p < 0.001). The variance in clinical visits due to primary insomnia and schizophrenia was lower during the COVID-19 pandemic than before the COVID-19 (SD = 48.5 vs. 77.9, p < 0.001 for primary insomnia, SD = 19.7 vs. 48.9, p < 0.001 for schizophrenia).
Table 1.
Mean, standard deviation of incidence of diseases before and during COVID-19, and their difference.
| Diseases | Before COVID-19 | During COVID-19 | p-Values of Difference | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | Variance | |
| Autism | 3070.6 | 243.1 | 3550.6 | 359.1 | <0.001 * | 0.936 |
| ADHD | 26498.2 | 2600.5 | 28667.8 | 2332.6 | 0.021 * | 0.480 |
| Depressive disorder | 14273.1 | 2036.9 | 15748.9 | 1656.6 | 0.021 * | 0.856 |
| Bipolar disorder | 1996.0 | 237.7 | 2416.7 | 138.2 | <0.001 * | 0.140 |
| Primary insomnia | 575.5 | 77.9 | 583.9 | 48.5 | 0.745 | 0.037 † |
| Schizophrenia | 1166.4 | 48.9 | 989.1 | 19.7 | <0.001 * | 0.014 † |
| Panic disorder | 1058.0 | 158.5 | 1507.1 | 213.1 | <0.001 * | 0.159 |
| Hypochondriasis | 15.5 | 4.3 | 26.3 | 10.6 | <0.001 * | 0.796 |
| Post traumatic stress disorder | 416.2 | 40.1 | 465.5 | 45.1 | 0.001 * | 0.766 |
| Anxiety disorder | 5536.6 | 675.1 | 6902.7 | 990.8 | <0.001 * | 0.739 |
| Anorexia nervosa | 106.4 | 10.8 | 127.1 | 24.8 | 0.003 * | 0.106 |
| Adephagia | 79.2 | 10.9 | 80.6 | 9.6 | 0.725 | 0.496 |
* Mann–Whitney U test, significance at <0.05, † Levene’s test in non-parametric data, significance at <0.05.
Figure 1.
Monthly incidence of psychiatric diseases in 2018, 2019, 2020, and 2021.
According to sex, the mean number of clinical visits due to autism, depressive disorder, bipolar disorder, panic disorder, hypochondriasis, and anxiety disorder were higher in both the male and female groups during the COVID-19 pandemic than before the COVID-19 pandemic (all p < 0.05, Table 2). In the female group, the mean number of clinical visits due to ADHD, PTSD, and anorexia nervosa was higher during the COVID-19 pandemic than before the COVID-19 pandemic (all p < 0.05). The mean number of clinical visits due to schizophrenia was lower during the COVID-19 pandemic than before the COVID-19 pandemic in both sexes (all p < 0.001).
Table 2.
Mean, Standard deviation of incidence of diseases before and during COVID-19, and their difference in the subgroup by sex.
| Diseases | Before COVID-19 | During COVID-19 | p-Values of Difference | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | Variance | |
| Men | ||||||
| Autism | 2595.8 | 201.1 | 2960.7 | 288.3 | <0.001 * | 0.892 |
| ADHD | 21881.1 | 2099.7 | 23093.9 | 1780.9 | 0.093 | 0.187 |
| Depressive disorder | 5427.6 | 630.5 | 5929.5 | 585.5 | 0.014 * | 0.709 |
| Bipolar disorder | 929.0 | 91.7 | 1054.8 | 44.4 | <0.001 * | 0.263 |
| Primary insomnia | 281.3 | 39.5 | 271.7 | 32.3 | 0.379 | 0.763 |
| Schizophrenia | 594.3 | 24.1 | 503.8 | 13.9 | <0.001 * | 0.014 † |
| Panic disorder | 469.8 | 58.6 | 643.7 | 78.8 | <0.001 * | 0.113 |
| Hypochondriasis | 10.0 | 3.4 | 14.1 | 3.4 | 0.001 * | 0.871 |
| Post traumatic stress disorder | 158.8 | 17.1 | 170.3 | 17.8 | 0.066 | 0.762 |
| Anxiety disorder | 2663.4 | 255.7 | 3186.3 | 411.4 | <0.001 * | 0.542 |
| Anorexia nervosa | 13.0 | 2.9 | 12.2 | 3.0 | 0.295 | 0.611 |
| Adephagia | 12.6 | 5.0 | 11.0 | 3.0 | 0.497 | 0.443 |
| Women | ||||||
| Autism | 474.8 | 44.6 | 589.9 | 71.8 | <0.001 * | 0.353 |
| ADHD | 4617.1 | 507.0 | 5573.9 | 562.3 | <0.001 * | 0.425 |
| Depressive disorder | 8845.5 | 1416.1 | 9819.5 | 1074.3 | 0.021 * | 0.973 |
| Bipolar disorder | 1067.0 | 148.0 | 1361.9 | 98.2 | <0.001 * | 0.101 |
| Primary insomnia | 294.2 | 44.3 | 312.2 | 21.9 | 0.159 | 0.003 † |
| Schizophrenia | 572.1 | 27.9 | 485.3 | 10.7 | <0.001 * | 0.017 † |
| Panic disorder | 588.2 | 100.7 | 863.4 | 137.4 | <0.001 * | 0.165 |
| Hypochondriasis | 5.6 | 2.4 | 12.2 | 8.1 | 0.006 * | 0.727 |
| Post traumatic stress disorder | 257.4 | 28.5 | 295.3 | 29.0 | <0.001 * | 0.777 |
| Anxiety disorder | 2873.2 | 422.4 | 3716.3 | 585.5 | <0.001 * | 0.898 |
| Anorexia nervosa | 93.4 | 10.0 | 114.9 | 23.4 | 0.003 * | 0.081 |
| Adephagia | 66.5 | 9.6 | 69.6 | 8.1 | 0.464 | 0.828 |
* Mann–Whitney U test, significance at <0.05, † Levene’s test in non-parametric data, significance at <0.05.
According to age, the 0–4-year-old group demonstrated higher mean number of clinical visits due to autism and ADHD during the COVID-19 pandemic than before the COVID-19 pandemic (all p < 0.05, Table 3). In the 5–9-year-old group, autism, depressive disorder, bipolar disorder, primary insomnia, anxiety disorder, and anorexia nervosa showed higher mean number of clinical visits during COVID-19 pandemic than before the COVID-19 pandemic (all p < 0.05). In the 10–14-year-old group, autism, ADHD, schizophrenia, panic disorder, hypochondriasis, anxiety disorder, and anorexia nervosa demonstrated higher mean number of clinical visits during the COVID-19 pandemic than before the COVID-19 pandemic (all p < 0.05). In the 15–19-year-old group, ADHD, depressive disorder, bipolar disorder, panic disorder, hypochondriasis, PTSD, anxiety disorder, and anorexia nervosa indicated higher mean number of clinical visits during the COVID-19 pandemic than before the COVID-19 pandemic (all p < 0.05). On the other hand, autism and schizophrenia showed lower mean number of clinical visits during the COVID-19 pandemic than before the COVID-19 pandemic (all p < 0.05).
Table 3.
Mean, Standard deviation of incidence of diseases before and during COVID-19, and their difference in the subgroup by age.
| Diseases | Before COVID-19 | During COVID-19 | p-Values of Difference | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | Variance | |
| Age 0–4 years old | ||||||
| Autism | 300.3 | 29.7 | 384.9 | 74.1 | <0.001 * | 0.526 |
| ADHD | 94.8 | 16.4 | 118.9 | 35.9 | 0.026 * | 0.380 |
| Depressive disorder | 14.2 | 4.7 | 8.5 | 2.5 | <0.001 * | 0.140 |
| Bipolar disorder | 2.1 | 1.3 | 2.3 | 1.3 | 0.592 | 0.651 |
| Primary insomnia | 12.6 | 3.9 | 14.5 | 5.1 | 0.187 | 0.562 |
| Schizophrenia | 0.6 | 0.6 | 0.4 | 0.5 | 0.433 | 0.142 |
| Panic disorder | 0.3 | 0.5 | 0.5 | 0.6 | 0.130 | 0.036 † |
| Hypochondriasis | 0.5 | 0.9 | 0.5 | 0.7 | 0.715 | 0.539 |
| Post traumatic stress disorder | 9.2 | 3.0 | 7.7 | 3.5 | 0.196 | 0.277 |
| Anxiety disorder | 52.8 | 9.1 | 62.1 | 16.9 | 0.136 | 0.432 |
| Anorexia nervosa | 2.7 | 2.1 | 3.1 | 1.9 | 0.473 | 0.803 |
| Adephagia | 4.3 | 4.3 | 3.9 | 1.7 | 0.663 | <0.001 † |
| Age 5–9 years old | ||||||
| Autism | 1141.3 | 143.2 | 1421.1 | 180.5 | <0.001 * | 0.560 |
| ADHD | 9660.0 | 1334.1 | 10395.3 | 915.3 | 0.074 | 0.010 † |
| Depressive disorder | 324.0 | 43.3 | 367.2 | 47.2 | 0.007 * | 0.343 |
| Bipolar disorder | 45.7 | 9.1 | 60.3 | 3.8 | <0.001 * | 0.135 |
| Primary insomnia | 9.6 | 3.7 | 12.4 | 4.4 | 0.009 * | 0.178 |
| Schizophrenia | 8.8 | 2.0 | 9.1 | 3.0 | 0.891 | 0.160 |
| Panic disorder | 7.3 | 2.6 | 6.8 | 1.5 | 0.564 | 0.102 |
| Hypochondriasis | 0.5 | 0.7 | 1.1 | 1.0 | 0.074 | 0.122 |
| Post traumatic stress disorder | 41.8 | 5.7 | 42.3 | 7.1 | 0.989 | 0.360 |
| Anxiety disorder | 372.1 | 32.7 | 454.5 | 70.0 | <0.001 * | 0.422 |
| Anorexia nervosa | 3.2 | 2.2 | 5.5 | 2.3 | 0.003 * | 0.956 |
| Adephagia | 3.3 | 2.9 | 2.5 | 1.6 | 0.618 | 0.594 |
| Age 10–14 years old | ||||||
| Autism | 752.3 | 87.2 | 974.3 | 104.1 | <0.001 * | 0.145 |
| ADHD | 10797.7 | 916.1 | 11839.2 | 1088.5 | 0.004 * | 0.978 |
| Depressive disorder | 2550.7 | 454.4 | 2366.9 | 338.9 | 0.110 | 0.023 † |
| Bipolar disorder | 272.1 | 39.0 | 294.3 | 28.7 | 0.113 | 0.047 † |
| Primary insomnia | 37.5 | 4.6 | 40.1 | 7.4 | 0.316 | 0.195 |
| Schizophrenia | 80.8 | 8.0 | 86.9 | 10.7 | 0.042 * | 0.019 † |
| Panic disorder | 84.2 | 13.7 | 122.1 | 31.4 | 0.001 * | 0.368 |
| Hypochondriasis | 2.2 | 1.0 | 5.1 | 3.0 | 0.001 * | 0.200 |
| Post traumatic stress disorder | 98.9 | 18.4 | 109.9 | 17.8 | 0.070 | 0.608 |
| Anxiety disorder | 920.1 | 110.7 | 1133.1 | 216.6 | 0.001 * | 0.206 |
| Anorexia nervosa | 41.8 | 6.1 | 49.9 | 13.0 | 0.030 * | 0.023 † |
| Adephagia | 7.0 | 1.9 | 8.3 | 3.8 | 0.557 | 0.055 |
| Age 15–19 years old | ||||||
| Autism | 876.7 | 33.9 | 770.3 | 25.8 | <0.001 * | 0.018 † |
| ADHD | 5945.7 | 388.1 | 6314.5 | 375.9 | 0.003 * | 0.776 |
| Depressive disorder | 11384.3 | 1574.8 | 13006.3 | 1292.9 | 0.002 * | 0.861 |
| Bipolar disorder | 1676.0 | 197.1 | 2059.7 | 110.6 | <0.001 * | 0.094 |
| Primary insomnia | 515.8 | 77.2 | 517.0 | 43.2 | 0.935 | 0.010 † |
| Schizophrenia | 1076.3 | 43.4 | 892.7 | 26.2 | <0.001 * | 0.014 † |
| Panic disorder | 966.2 | 146.9 | 1377.7 | 184.0 | <0.001 * | 0.127 |
| Hypochondriasis | 12.4 | 4.3 | 19.7 | 6.9 | 0.001 * | 0.417 |
| Post traumatic stress disorder | 266.3 | 25.4 | 305.7 | 23.0 | <0.001 * | 0.612 |
| Anxiety disorder | 4191.5 | 541.5 | 5252.9 | 716.8 | <0.001 * | 0.975 |
| Anorexia nervosa | 58.7 | 5.8 | 68.6 | 10.7 | 0.001 * | 0.168 |
| Adephagia | 64.5 | 10.2 | 65.5 | 6.4 | 0.818 | 0.087 |
* Mann–Whitney U test, significance at <0.05, † Levene’s test in non-parametric data, significance at <0.05.
4. Discussion
Many psychiatric disorders, including autism, ADHD, depressive disorder, bipolar disorder, panic disorder, hypochondriasis, PTSD, anxiety disorder, and anorexia nervosa, demonstrated a higher mean number of clinical visits in children during the COVID-19 pandemic than before the COVID-19 pandemic. Females and adolescents demonstrated a greater mean number of medical visits due to psychiatric disorders during the COVID-19 pandemic than before the COVID-19 pandemic. On the other hand, the mean number of clinical visits due to schizophrenia was lower in children during the COVID-19 pandemic than before the COVID-19 pandemic.
A higher burden of psychiatric diseases in youth during the COVID-19 pandemic has been suggested in a number of recent studies [9,13,14,15]. In a cross-sectional online survey, the three most common psychiatric symptoms in primary and secondary school students during school closures due to COVID-19 outbreaks were anxiety, depression, and stress [13]. Another prior study reported that the psychiatric symptoms of inattention (30.8%) and sleep disturbances (21.3%) were also high in youth during the COVID-19 pandemic [14]. Especially, the children with pre-existing psychiatric diseases were suggested to show higher incidence of the psychiatric symptoms during COVID-19 pandemic in recent studies [16]. For instance, in children with ADHD, the psychiatric symptoms were higher during the COVID-19 pandemic [16]. A few potential risk factors can be postulated for the higher incidence of psychiatric symptoms during COVID-19 pandemic. It was suggested that school closures and the increased burden of family conflicts due to increased online education and home care could mediate the higher psychiatric symptoms in children during the COVID-19 pandemic [14]. Moreover, the confinement and developmental vulnerabilities of children and adolescents may have contributed to the increased number of medical visits due to psychiatric disorders during the COVID-19 pandemic in this study.
In addition to the common affective disorders of anxiety and depression, other psychiatric disorders of ADHD, panic disorder, hypochondriasis, and anorexia nervosa were increased during the COVID-19 pandemic in the present study. The increased time spent on media use is thought to aggravate the risk of ADHD in youth [17]. In an online survey, the abuse of smartphones and the internet was associated with severe depression in children during the COVID-19 pandemic [18]. Fear or panic due to the COVID-19 pandemic may influence the increased number of medical visits due to panic disorder and hypochondriasis in children. Quarantine strategies and health-related education programs could encourage attention to health and could evoke hypochondriasis. Furthermore, the immature coping skills and developing neurocognitive functions of children could make them vulnerable to the pandemic crisis and may increase psychiatric disorders.
On the other hand, the number of clinical visits due to schizophrenia decreased during the COVID-19 pandemic. The clinical features of schizophrenia, such as psychosis and cognitive deficits and low sociodemographic status, may impair medical care in patients with schizophrenia [19]. Moreover, patients with schizophrenia were reported to show a high risk of COVID-19 infection [20,21]. Thus, infection with COVID-19 could hinder proper treatment for patients with schizophrenia. Telepsychiatry applications were proposed to support the medical management of patients with schizophrenia [22].
According to age and sex, the female and adolescent groups demonstrated more psychiatric disorders with a higher number of clinical visits during the COVID-19 pandemic in this study. In line with the current results, a few previous studies have suggested a higher susceptibility of adolescents and females to anxiety and depression during the COVID-19 pandemic [8,23]. A cross-sectional online survey reported that adolescents had the highest number of emotional problems during the lockdown period among youth (1-19 years) [23]. The higher incidence of affective disorders during the adolescent period could contribute to the significant association of medical visits due to these psychiatric disorders with the COVID-19 pandemic.
This study investigated data from all Korean children for the diagnosis of psychiatric disorders. Because all Koreans are legally registered for the health insurance system with their respective resident registration numbers, there was little concern on the missing or overlapping data. However, a few shortcomings need to be addressed when generalizing the current results. First, the cohort population was composed of one ethnic group: Korean children. Thus, regional or ethnic differences can exist for the changes in the cases of psychiatric disorders and the COVID-19 pandemic [24]. In addition, stratified social distancing policies from the Korean government were enacted without complete lockdown events. Thus, there was no restriction to visit clinics during study periods. Second, undiagnosed and subclinical cases could have been missed in the current study. Because this study analyzed health claims data, patients who did not visit clinics could not be included. Third, the severity and management of psychiatric disorders were heterogeneous in the current study. Lastly, there may have potential confounders, such as eating disorders, the increase in time spent at home, the increase in family meals and supermarket, and the stigma on the search for psychiatric visits or on access to clinical and rehabilitation facilities during COVID-19 [25,26,27] To elucidate the long-term consequences of the effects of the COVID-19 pandemic on psychiatric disorders, a long-term follow-up study with detailed treatment histories may be warranted.
5. Conclusions
The diagnoses of autism, ADHD, depressive disorder, bipolar disorder, panic disorder, hypochondriasis, PTSD, anxiety disorder, and anorexia nervosa were increased in children during the COVID-19 pandemic. Females and older children were more susceptible to diagnoses of psychiatric disorders during the COVID-19 pandemic.
Author Contributions
H.G.C. designed the study; D.M.Y. and H.G.C. analyzed the data; S.Y.K., N.-E.L., J.H.K., M.J.K., J.-H.K., W.J.B. and H.G.C. drafted and revised the paper; and H.G.C. drew the figures. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported in part by a research grant (2021-R1C1C1004986) from the National Research Foundation (NRF) of Korea and a research grant from Hallym University College of Medicine (HURF).
Institutional Review Board Statement
The ethics committee of Hallym University (2021-11-004) permitted this study following the guidelines and regulations.
Informed Consent Statement
Written informed consent was waived by the Institutional Review Board.
Data Availability Statement
Releasing of the data by the researcher is not legally permitted. All data are available from the database of the Korea Center for Disease Control and Prevention. The Korea Center for Disease Control and Prevention allows data access, at a particular cost, for any researcher who promises to follow the research ethics. The data of this article can be downloaded from the website after agreeing to follow the research ethics.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Dubey S., Biswas P., Ghosh R., Chatterjee S., Dubey M.J., Chatterjee S., Lahiri D., Lavie C.J. Psychosocial Impact of COVID-19. Diabetes Metab. Syndr. Clin. Res. Rev. 2020;14:779–788. doi: 10.1016/j.dsx.2020.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Park J.-H., Jang W., Kim S.-W., Lee J., Lim Y.-S., Cho C.-G., Park S.-W., Kim B.H. The Clinical Manifestations and Chest Computed Tomography Findings of Coronavirus Disease 2019 (COVID-19) Patients in China: A Proportion Meta-Analysis. Clin. Exp. Otorhinolaryngol. 2020;13:95–105. doi: 10.21053/ceo.2020.00570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee J. Mental Health Effects of School Closures During COVID-19. Lancet Child Adolesc. Health. 2020;4:421. doi: 10.1016/S2352-4642(20)30109-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ghosh R., Dubey M.J., Chatterjee S., Dubey S. Impact of COVID-19 on Children: Special Focus on the Psychosocial Aspect. Minerva Pediatr. 2020;72:226–235. doi: 10.23736/S0026-4946.20.05887-9. [DOI] [PubMed] [Google Scholar]
- 5.Zhu K., Xie X., Liu Q., Meng H., Song R. Internet Addiction: Prevalence and Relationship with Academic Burnout Among Undergraduates During Widespread Online Learning. Perspect. Psychiatr. Care. 2022 doi: 10.1111/ppc.13060. online ahead of print. [DOI] [PubMed] [Google Scholar]
- 6.Dalton L., Rapa E., Stein A. Protecting the Psychological Health of Children through Effective Communication about COVID-19. Lancet Child Adolesc. Health. 2020;4:346–347. doi: 10.1016/S2352-4642(20)30097-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Herringa R.J. Trauma, PTSD, and the Developing Brain. Curr. Psychiatry Rep. 2017;19:69. doi: 10.1007/s11920-017-0825-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meade J. Mental Health Effects of the COVID-19 Pandemic on Children and Adolescents. Pediatr. Clin. North Am. 2021;68:945–959. doi: 10.1016/j.pcl.2021.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meherali S., Punjani N., Louie-Poon S., Rahim K.A., Das J., Salam R., Lassi Z. Mental Health of Children and Adolescents Amidst COVID-19 and Past Pandemics: A Rapid Systematic Review. Int. J. Environ. Res. Public Health. 2021;18:3432. doi: 10.3390/ijerph18073432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim S.Y., Kim H.-R., Park B., Choi H.G. Comparison of Stress and Suicide-Related Behaviors Among Korean Youths Before and During the COVID-19 Pandemic. JAMA Netw. Open. 2021;4:e2136137. doi: 10.1001/jamanetworkopen.2021.36137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pizarro-Ruiz J.P., Ordóñez-Camblor N. Effects of Covid-19 Confinement on the Mental Health of Children and Adolescents in Spain. Sci. Rep. 2021;11:11713. doi: 10.1038/s41598-021-91299-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nordstokke D., Zumbo B.D. A New Nonparametric Levene Test for Equal Variances. Psicológica. 2010;31:401–430. [Google Scholar]
- 13.Tang S., Xiang M., Cheung T., Xiang Y.-T. Mental Health and Its Correlates Among Children and Adolescents During COVID-19 School Closure: The Importance of Parent-Child Discussion. J. Affect. Disord. 2021;279:353–360. doi: 10.1016/j.jad.2020.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Panda P.K., Gupta J., Chowdhury S.R., Kumar R., Meena A.K., Madaan P., Sharawat I.K., Gulati S. Psychological and Behavioral Impact of Lockdown and Quarantine Measures for COVID-19 Pandemic on Children, Adolescents and Caregivers: A Systematic Review and Meta-Analysis. J. Trop. Pediatr. 2021;67:fmaa122. doi: 10.1093/tropej/fmaa122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee S.Y., Ro Y.S., Jeong J., Shin S.D., Moon S. Impact of the COVID-19 Pandemic on the Incidence and Characteristics of Patients with Psychiatric Illnesses Visiting Emergency Departments in Korea. J. Clin. Med. 2022;11:488. doi: 10.3390/jcm11030488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Colizzi M., Sironi E., Antonini F., Ciceri M.L., Bovo C., Zoccante L. Psychosocial and Behavioral Impact of COVID-19 in Autism Spectrum Disorder: An Online Parent Survey. Brain Sci. 2020;10:341. doi: 10.3390/brainsci10060341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shuai L., He S., Zheng H., Wang Z., Qiu M., Xia W., Cao X., Lu L., Zhang J. Influences of Digital Media Use on Children and Adolescents with ADHD During COVID-19 Pandemic. Glob. Health. 2021;17:48. doi: 10.1186/s12992-021-00699-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Duan L., Shao X., Wang Y., Huang Y., Miao J., Yang X., Zhu G. An Investigation of Mental Health Status of Children and Adolescents in China During the Outbreak of COVID-19. J. Affect. Disord. 2020;275:112–118. doi: 10.1016/j.jad.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kozloff N., Mulsant B.H., Stergiopoulos V., Voineskos A.N. The COVID-19 Global Pandemic: Implications for People with Schizophrenia and Related Disorders. Schizophr. Bull. 2020;46:752–757. doi: 10.1093/schbul/sbaa051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Correll C.U., Chepke C., Gionfriddo P., Parks J., Foxworth P., Basu A., Brister T.S., Brown D., Clarke C., Hassoun Y. The Post COVID-19 Healthcare Landscape and the Use of Long-Acting Injectable Antipsychotics for Individuals with Schizophrenia and Bipolar I Disorder: The Importance of an Integrated Collaborative-Care Approach. BMC Psychiatry. 2022;22:32. doi: 10.1186/s12888-022-03685-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fond G., Nemani K., Etchecopar-Etchart D., Loundou A., Goff D.C., Lee S.W., Lancon C., Auquier P., Baumstarck K., Llorca P.-M., et al. Association Between Mental Health Disorders and Mortality Among Patients With COVID-19 in 7 Countries. JAMA Psychiatry. 2021;78:1208. doi: 10.1001/jamapsychiatry.2021.2274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kahve A.C., Kaya H., Darben Y., Cakil A.G., Goka E. From Predictions to Evidence: Treatment Compliance, Disease Progression and Social Compliance of Patients with Schizophrenia in the COVID-19 Pandemic. Perspect. Psychiatr. Care. 2021;57:1991–1998. doi: 10.1111/ppc.12824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schmidt S.J., Barblan L.P., Lory I., Landolt M.A. Age-Related Effects of the COVID-19 Pandemic on Mental Health of Children and Adolescents. Eur. J. Psychotraumatol. 2021;12:1901407. doi: 10.1080/20008198.2021.1901407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim S.Y., Kim D.W. Does the Clinical Spectrum of Coronavirus Disease 2019 (COVID-19) Show Regional Differences? Clin. Exp. Otorhinolaryngol. 2020;13:83–84. doi: 10.21053/ceo.2020.00612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kurisu K., Matsuoka M., Sato K., Hattori A., Yamanaka Y., Nohara N., Otani M., Yoshiuchi K. Increased Prevalence of Eating Disorders in Japan since the Start of the COVID-19 Pandemic. Eat. Weight Disord. Stud. Anorexia Bulim. Obes. 2021:1–5. doi: 10.1007/s40519-021-01339-6. online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ransing R., Ramalho R., de Filippis R., Ojeahere M.I., Karaliuniene R., Orsolini L., da Costa M.P., Ullah I., Grandinetti P., Bytyçi D.G., et al. Infectious Disease Outbreak Related Stigma and Discrimination During the COVID-19 Pandemic: Drivers, Facilitators, Manifestations, and Outcomes across the World. Brain Behav. Immun. 2020;89:555–558. doi: 10.1016/j.bbi.2020.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Aamir A., Awan S., de Filippis R., Diwan M.N., Ullah I. Effect of COVID-19 on Mental Health Rehabilitation Centers. J. Psychosoc. Rehabil. Ment. Health. 2021;8:97–100. doi: 10.1007/s40737-020-00203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Releasing of the data by the researcher is not legally permitted. All data are available from the database of the Korea Center for Disease Control and Prevention. The Korea Center for Disease Control and Prevention allows data access, at a particular cost, for any researcher who promises to follow the research ethics. The data of this article can be downloaded from the website after agreeing to follow the research ethics.